Abstract
Background:
Household air pollution (HAP) from combustion of biomass fuel, such as wood and animal dung, is among the leading environmental risk factors for preventable disease. Close to half of the world’s population relies on biomass cookstoves for their daily cooking needs. Understanding factors that affect HAP can inform measures to maximize the effectiveness of cookstove interventions in a cost-effective manner. However, the impact of kitchen and household characteristics, as well as the presence of secondary stoves, on HAP concentrations is poorly understood in Puno, Peru.
Objective:
To explore how household characteristics explain variability of kitchen area concentrations and personal exposures to CO, PM2.5 and BC from biomass cookstoves among women in rural Peru.
Methods:
Household characteristics (including kitchen materials and layout, wealth, and cooking behaviors) and HAP measurements were collected from 180 households in Puno, Peru, from baseline measurements of a randomized trial. Kitchen area concentrations and personal exposures to carbon monoxide (CO), fine particulate matter (PM2.5) and black carbon (BC) were sampled for 48 hours. We implemented simple and multivariable linear regression models to determine the associations between household characteristics and both kitchen area concentration and personal exposure to each pollutant.
Results:
Mean daily kitchen area concentrations and personal exposures to HAP were, on average, 48 times above World Health Organization indoor guidelines for PM2.5. We found that roof type explained the most variability in HAP and was strongly associated with both kitchen area concentrations and personal exposures for all pollutants after adjusting for other household variables. Personal exposures were 27% to 36% lower for PM2.5, CO and BC, in households with corrugated metal roofs, compared to roofs made of natural materials (straw, totora or reed) after adjusting for other factors. Higher kitchen area concentrations were also associated with less wealth, owning more animals, or sampling during the dry season in multivariable models. Having a liquefied petroleum gas (LPG) stove and having a chimney were associated with lower personal exposures, but were not associated with kitchen area concentrations. Personal exposures were lower by 21% for PM2.5 and 28% for CO and BC concentrations among participants who had both LPG and biomass stoves compared to those with only biomass cookstoves adjusting for other household factors.
Conclusions:
Characterizing HAP within different settings can help identify effective and culturally-relevant solutions to reduce HAP exposures. We found that housing roof type is strongly related to kitchen area concentrations and personal exposures to HAP, perhaps because of greater ventilation in kitchens with metal roofs compared to those with thatch roofs. Although HAP concentrations remained above guidelines for all households, promoting use of metal roof materials and LPG stoves may be actionable interventions that can help reduce exposures to HAP in high-altitude rural Peru and similar settings.
Keywords: Biomass cookstove, household air pollution, particulate matter, carbon monoxide, black carbon
1. Introduction
Household air pollution (HAP) from the combustion of biomass fuels (typically wood, animal dung, and agricultural crop waste) is among the leading environmental risk factors for preventable disease (Bruce et al., 2000; Cohen et al., 2017; Smith et al., 2014; World Health Organization, 2009). Close to half of the world’s population, mostly from low- and middle-income countries (LMICs), rely on biomass cookstoves for their daily cooking needs (Bonjour et al., 2013; Yadama, 2013). Exposure to HAP was estimated to be responsible for 1.6 million deaths in 2017 (Stanaway et al., 2018). HAP is known to contribute to lower respiratory infections, chronic respiratory disease, cardiovascular disease, and cancer, and is a leading risk factor for childhood pneumonia and low birthweight (Fullerton et al., 2008; Gordon et al., 2014; Miller et al., 2007; Sana et al., 2018).
The incomplete combustion of biomass fuels produces a wide range of gas and particulate pollutants. The most commonly measured pollutants from HAP are carbon monoxide (CO) and particulate matter (PM) (Pope et al., 2017; Quansah et al., 2017; Thomas et al., 2015). Fine PM consists of particles smaller than 2.5 micrometers in aerodynamic diameter (PM2.5), which are small enough to penetrate deep in the respiratory tract and reach the alveoli (Kulkarni et al., 2005; Xing et al., 2016). CO and PM2.5 from ambient air pollution have been strongly associated with increased risk of cardiopulmonary-related morbidity and mortality in adults and children (Beelen et al., 2014; Brook et al., 2010, 2004, 2002; Chan et al., 2015; Gold and Samet, 2013; Krewski et al., 2009; Miller et al., 2007; Mustafic et al., 2012; Newby et al., 2015; O’Neill et al., 2005; Pope et al., 2009, 2004; Rundell et al., 2007; World Health Organization, 2010). Black carbon (BC), one of the main constituents of combustion generated PM2.5, has been identified to play an important role in cardiovascular disease development (Kelly and Fussell, 2012; World Health Organization, 2012).
Understanding how different household characteristics impact indoor concentrations can inform measures to maximize the effectiveness of cookstove interventions in a cost-effective manner. Kitchen design and structure can affect ventilation, while different biomass fuels produce varying relative concentrations of specific pollutants. According to recent reviews and a WHO database, kitchen area 24-hr average PM2.5 concentrations range from 200 to 3,000 μg/m3 in households that use biomass in LMICs (Balakrishnan et al., 2014; Pope et al., 2017; Shupler et al., 2018). Households that use animal dung as the primary biomass fuel tend to have higher concentrations than households that use wood (Shupler et al., 2018). However, the relationship between household characteristics and HAP concentrations can also vary widely across different settings (Balakrishnan et al., 2013; Clark et al., 2010; Klasen et al., 2015). For example, a study that looked at improved and traditional biomass cookstoves in Honduras found that the presence of windows was most strongly associated with lower kitchen area HAP (Clark et al., 2010). In contrast, a previous study in Puno, Peru found that the number of windows, presence of chimney, or outdoor concentrations had no influence on indoor HAP concentrations in rural households (Pollard et al., 2014). Additionally, the authors acknowledged that chimney designs varied considerably across households, suggesting the need to include an additional category for chimney type.
Little is known about the impact of household characteristics on personal exposure, which may be more relevant when identifying relationships with health outcomes than area concentrations, particularly in regions where stoves are often left unattended (Clark et al., 2013; Northcross et al., 2015). Furthermore, recent governmental programs have contributed to an increase in co-ownership of liquefied petroleum gas (LPG) stoves among biomass users (Pollard et al., 2018) in the Puno region. Understanding household characteristics associated with HAP exposures among biomass users, as well as the impact of owning an LPG stove on HAP concentrations, is essential to develop and maximize the effectiveness of interventions to reduce HAP.
To address these gaps, we performed a detailed exposure assessment of PM2.5, CO, and BC to evaluate the influence of household characteristics on HAP exposures in Puno, Peru. We explored how household characteristics explain variability of kitchen area concentrations and personal exposures to CO, PM2.5 and BC from cookstoves in rural Peruvian households. We attempted to identify kitchen and participant characteristics that are common, culturally relevant, and could be targeted to reduce HAP.
2. Materials and Methods
2.1. Study settings and design
The data in this paper were collected as part of the baseline measurements for an ongoing biomass-to-LPG individually randomized, open-label controlled field trial (Fandiño-Del-Rio et al., 2017). HAP measurements were collected in rural communities surrounding the city of Puno, located around Lake Titicaca at 3,825 meters above sea level. Enrolled participants used traditional biomass-burning cookstoves for cooking daily. We enrolled 181 women aged 25–64 years. One participant withdrew from the study before completing follow-up evaluations of the main trial, which left a sample of 180 participants included in this study. Inclusion criteria included: being the primary cook of the household, using biomass fuels daily for cooking, and having the cooking area separate from the sleeping area (which is typical in the region). Each enrolled participant received a set of baseline, pre-intervention assessments that included one visit to measure 48-hour HAP measurements. Baseline assessments spanned 12 months, from February 2017 to February 2018, visiting approximately 15 participants each month. With approximately one third of samples taken during the rainy season (December, January, February, March). When we experienced issues with equipment and the sample was missing, we repeated sample collection when possible (limiting repetition for a household to no more than 2 attempts per household). During baseline visits we also collected basic socio-demographic information and observed household and kitchen characteristics. Additional information on enrollment and procedures has been previously published (Fandiño-Del-Rio et al., 2017).
We collected information on household characteristics relevant to HAP concentrations including number of permanently open windows, number of doors left permanently open, kitchen roof and wall materials, number of people living in the household, trash burning activities, typical cooking durations, and number of dogs and pigs (based on formative research we identified that participants often cook for their pigs and dogs). We collected information regarding potential additional exposures, including the use of candles, smoking, and sweeping. We also asked if participants owned an LPG stove as a secondary stove and if they participated in the national government LPG subsidy program. The program, called the Fondo de Inclusion Social Energetico (FISE), aims to reduce use of solid fuels by subsidizing LPG fuel for low income Peruvian households (Pollard et al., 2018). We also collected information about stove ventilation and type of chimney. We incorporated basic socioeconomic status indicators including income, education level and a wealth indicator wherein participants are placed in a wealth quintile relative to a representative sample of the Peruvian population. Participants in our study were assigned a score based on asset ownership and were grouped into one of the five national wealth quintiles depending on their total score. Additional information on the estimation of wealth quintiles has been previously published (Kephart et al., 2020).
2.2. Household air pollution measurements
We assessed HAP exposure by measuring kitchen concentrations and personal exposures over a 48-hour period. Kitchen concentrations were measured using PM2.5 and CO monitors located approximately one meter from the combustion zone of the traditional stove, 1.5 meters from the floor (representing the breathing zone), and at least one meter from doors and windows (when possible). Personal exposure was measured by placing a PM2.5 and CO monitor near each participant’s breathing zone in an adapted apron (commonly used by women in the study site) provided to the participants (Figure 1). Women were encouraged to wear the aprons throughout the duration of the sampling period and to keep the apron close by when sleeping or bathing. Direct-reading measures of both PM2.5 and CO were logged at 1-minute intervals. BC concentrations were later measured from the gravimetric samples collected on PM2.5 filters.
Figure 1.
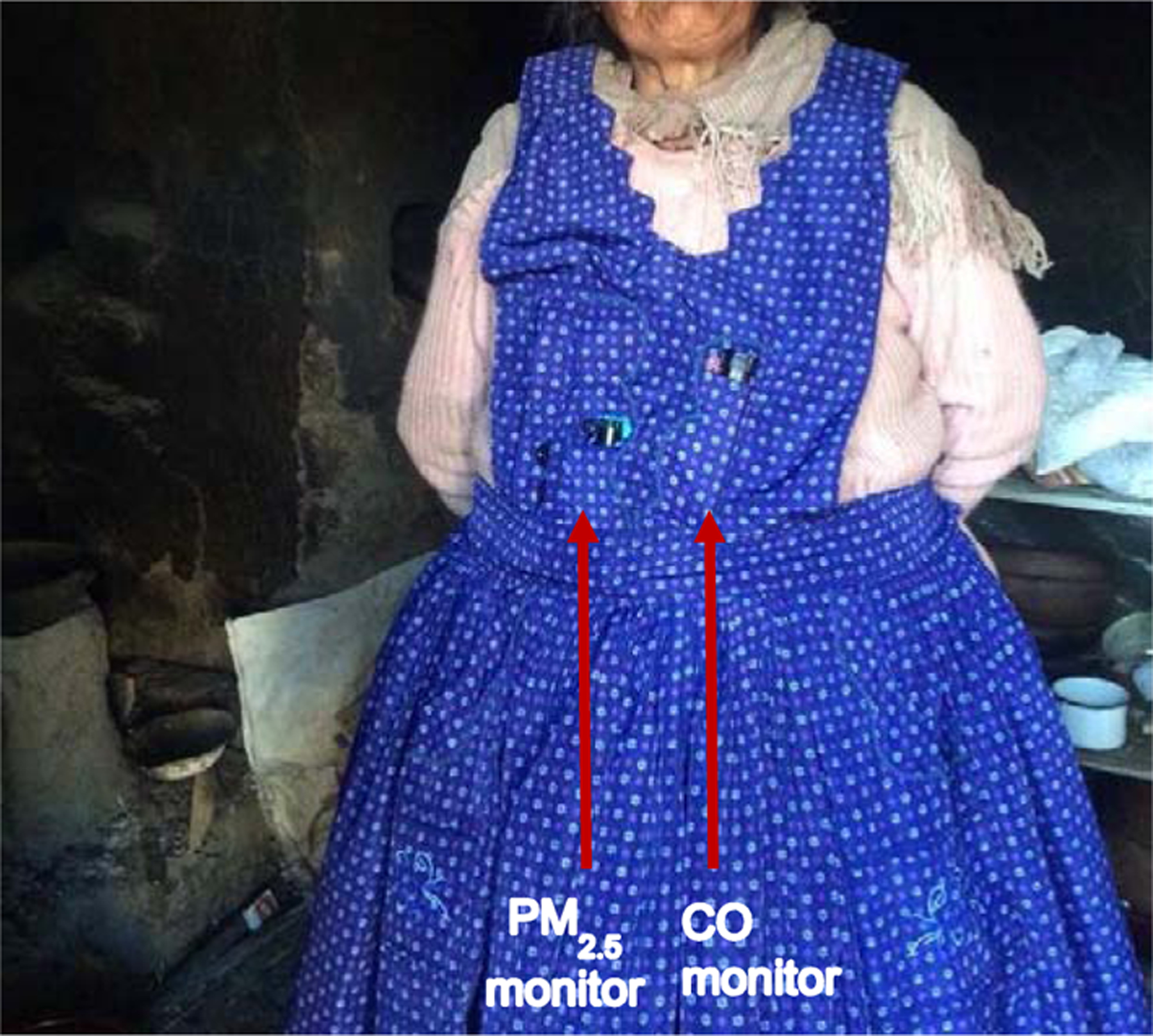
Personal exposure monitor placement on apron for household participants
We collected gravimetric and nephelometric PM2.5 mass concentration using the ECM, an active, direct-reading aerosol monitor (RTI Inc., Research Triangle Park, NC, USA). The ECM has a light-scattering laser for continuous-time nephelometric assessment of PM2.5, a pump operating at 0.3 L/minute that collects PM2.5 on a filter for gravimetric analysis, and an accelerometer to detect movement. We calibrated the ECM pumps daily and measured flow rate after sample collection with a TSI 4100 flowmeter (TSI Incorporated 500 Cardigan Road Shoreview, MN, USA). The nephelometric concentrations were calibrated using the concurrently sampled gravimetric time-weighted average filter sample. Gravimetric PM2.5 samples were collected on 15-mm Teflon filters with a 2-μm pore size (Measurement Technology Laboratories LLC, Minneapolis, MN, USA). Filters were pre-weighed and post-weighed at the Johns Hopkins Bloomberg School of Public Health in a humidity and temperature-controlled laboratory using a MT5 microbalance (Mettler Toledo, Columbus, OH, USA). To estimate the total volume of air sampled we used the flow rate logged by the ECMs, however, if the logged inlet pressure of the ECM was greater than 15 cm H2O for ≥10% of the time and the logged flow rate varied by more than ±3.5%, we used the average of the before and after sampling flow rates. We operated ECMs using duty cycles in order to avoid overloading the filters due to the high PM2.5 concentrations observed. These duty cycles operate the ECM pump at regular intervals. ECMs used for personal exposure samples operated for 30 consecutive seconds out of every 1-minute and devices for kitchen samples operated for 20 consecutive seconds out of every 3-minute period.
Direct-reading concentrations of CO were measured with the EL-USB-CO data logger (Lascar Electronics, Erie, PA, USA). BC concentrations were determined measuring optical attenuation on the PM2.5 gravimetric samples collected on filters (a cumulative measure per sample), using a Magee OT21 Sootscan transmissometer (Magee Scientific, Berkeley, CA). Attenuation units were converted to mass using the calibration algorithm provided by the Sootscan manufacturer for Teflon filters using standard equations (Chow et al., 2010). To estimate concentration, we used the volume sampled from the ECM monitor, as described above.
Kitchen samples of PM2.5 and CO included 10% duplicates. In addition, all PM2.5 samples included 10% blanks and all reported concentrations were blank-corrected. High correlations were observed for duplicate samples for the baseline measurements (0.94 for CO and 0.95 for BC and PM2.5, after excluding one outlier duplicate sample). The limits of detection (LOD) for BC and PM2.5 samples were estimated as three times the standard deviation of estimated mass from field blanks. All PM2.5 and BC samples with mass below the LOD were replaced by the LOD divided by the square root of two (Hornung and Reed, 1990). During the initial 6 months of the study the pre-weighed filters were loaded into the cassettes of the ECMs in the field site laboratory. For the remainder of the study, the filters were pre-loaded into individual ECM cassettes at the Johns Hopkins Bloomberg School of Public Health laboratory before being sent to the field site. Initially, the PM2.5 LOD was estimated to be 20 μg; after filter handling in the field laboratory was reduced, the LOD decreased to 9.8 μg. The LOD for BC was 1.4 μg throughout the study.
CO measurements were calibrated using correction factors derived by co-locating all CO monitors every 3–4 months in a sealed chamber. The monitors were exposed to clean air (nitrogen gas) and a known gas CO concentration of 100 ppm. Individual slopes and intercepts were estimated for each device and for each co-location timepoint to correct any existing drift on the devices. The LOD for the CO direct-reading instrument was estimated as three times the standard deviation of concentrations logged during the regular clean air calibration checks in the field; our estimate for CO LOD was 1 ppm. All direct-reading concentrations below the LOD were replaced by the LOD divided by the square root of two.
To provide context, we compared concentrations to WHO indoor guidelines (World Health Organization, 2010, 2006). The guideline used for CO in ppm (9.4 ppm) is based on temperature and pressure conditions representative of Puno (WHO guideline of 7 mg/m3 was converted to ppm assuming 10°C and 0.62 atm). We us ed the 24-hour guideline for PM2.5 of 25 μg/m3. The WHO does not have a BC guideline.
2.3. Statistical methods
To ensure that each 24-hour period was representative (i.e. capturing a typical number of cooking events), we excluded samples for which the sample day had a duration less than 20 hours (4% of CO samples and 1% of PM2.5 samples) for each pollutant. We estimated 48-hour mean concentrations as the mean of the two consecutive daily means for PM2.5 and CO when both sampling days had at least 20 hours of measurements. If the sample duration on the second day was less than 20 hours (total sample <44 hours), we used the initial 24-hours only. For BC, we estimated the integrated time-weighted average concentration from the time-integrated filter-based PM2.5 samples. We did not observe important differences in percent of awake time wearing the ECM monitors (differences<5%) comparing the first day to the second day of each sample. Most missing and short duration samples were due to battery issues with the CO and PM2.5 devices or technical issues with the device or the data download process (6% of CO samples and 1% of PM2.5 samples).
We fit single variable (univariate) and multivariable linear regression models to determine the association between household characteristics (explanatory variables) and each pollutant (CO, PM2.5, and BC; outcome variables) from both types of measurements (kitchen area concentrations and personal exposures). We used the log-transformed 48-hour average pollutant concentrations, which were highly skewed, to help meet linear regression assumptions. Our final exponentiated regression model coefficients represent the ratio of the geometric mean of the pollutant concentration in the specified category to that of the reference category. For example, a ratio of 1.1 translates to a 10% higher concentration and a value of 0.9 translates to a 10% lower concentration in pollutant concentration compared to the reference category.
Exploratory data analysis and single variable linear regression models were developed to make an initial selection of variables that might explain HAP variability. When evaluating single variable linear regression models, variables with a p-value less than 0.2 and partial correlation coefficients greater than 0.01 were included in the analysis. Among the variables selected we included rainy season (December, January, February, March) as a binary variable given its potential influence on availability of dry fuel. We included a binary indicator variable to account for whether the sample was for a 24-hour vs. 48-hour sample duration, as described above. This allowed us to adjust for potential differences between 24-hour and 48-hour samples. We assessed collinearity among all selected variables using variance inflation factors (Dupont, 2009). We excluded education level since it showed collinearity with the other variables selected, with variance inflation factors between 15 and 30. Variance inflation factors were approximately 1 for all other variables incorporated. Categorical variables were also examined for their potential relationship with other variables (see list of variables excluded in Table 1 footnote).
Table 1.
Baseline and household characteristics of study participants
| Household characteristics | Number (%) | |
|---|---|---|
| Total number of participants | 180 (100%) | |
| Number of bedrooms | 1 | 66 (37%) |
| 2 | 89 (49%) | |
| 3 | 16 (9%) | |
| 4 | 9 (5%) | |
| Kitchen roof material | ||
| Corrugated metal roof | 73 (41%) | |
| Natural: straw, totora, reed or similar | 107 (59%) | |
| Door or entrance in kitchen permanently open | 31 (17%) | |
| Windows permanently open | 0 | 72 (40%) |
| 1 | 26 (14%) | |
| 2 | 7 (4%) | |
| 5 | 2 (1%) | |
| Burn trash at home* | 147 (82%) | |
| Ventilation over traditional stove | ||
| Stove with no ventilation | 70 (39%) | |
| Stove with chimney | 19 (11%) | |
| Stove in recessed area | 91 (51%) | |
| Most common fuels used for cooking (can chose more than one) | ||
| Cow dung | 179 (99%) | |
| Wood | 75 (42%) | |
| Presence of secondary stove in addition to | No other | 48 (27%) |
| biomass stove | LPG gas | 132 (73%) |
| Electricity in household* | 175 (97%) | |
| Previously participated in FISE* | 88 (49%) | |
| Used FISE in last 3 months* | 76 (42%) | |
| Sleeps in the kitchen* | 6 (3%) | |
| Number of dogs | 0 | 57 (32%) |
| 1 | 92 (51%) | |
| 2 | 30 (17%) | |
| 3 | 1 (1%) | |
| Number of pigs | 0 | 74 (41%) |
| 1 to 2 | 52 (29%) | |
| 3 to 5 | 49 (27%) | |
| 6 to 9 | 5 (3%) | |
| Kitchen with adjacent walls with main | yes adjacent | 105 (58%) |
| residence | not adjacent | 75 (42%) |
| Number of samples during rainy season* | 62 (34%) | |
| Participant characteristics | Number (%) or Mean (SD) | |
| Age (years) | 48.3 (10.1) | |
| BMI (kg/m2) | 26.8 (4.2) | |
| Average years of education | 6.2 (3.3) | |
| Highest level of education achieved | ||
| Without education or preschool only | 7 (4%) | |
| Primary | 106 (59%) | |
| Secondary | 67 (37%) | |
| Non-university superior or university | 0 (0%) | |
| Wealth Quintile | 1 (lowest) | 101 (56%) |
| 2 | 69 (38%) | |
| 3 | 10 (6%) | |
| 4 and 5 (highest) | 0 (0%) | |
| Time cooking weekly (hours) | 0 – 20 | 31 (17%) |
| 20 – 30 | 137 (76%) | |
| 30 – 50 | 12 (7%) | |
Percentages shown are for “yes” response; the remainder of the percentage not shown are for “no” responses.
Other variables considered but not included in this table because they did not explain any of the variability or were not in any of the models include: wall material, floor material, number of entrances (permanently open and closed), number of windows (permanently open and closed), times cooking outside per week, number of household members, number of nights sleeping in kitchen per month, source of light (includes use of candles), years of education, hours cooking daily, and monthly income.
We developed multivariable linear regression models for each pollutant (CO, PM2.5, BC) and sample type (kitchen area, personal exposures) using a variable selection method. For each model (pollutant and sample type), we selected the group of variables (household characteristics) that were consistently chosen by backwards and forward variable selection methods (Dupont, 2009), using a p-value of 0.1 as a criterion for variable inclusion and removal. This process was repeated for each pollutant to select the set of variables that best described the variability in the data; each model was allowed to have a different set of household characteristics as explanatory variables. In addition, as a sensitivity analysis, we estimated the Akaike information criterion using a forward and backward variable selection method (AIC; using it as a criterion to compare models) (Wagenmakers and Farrell, 2004). All data analyses were conducted with MATLAB (The MathWorks, Inc., Natick, MA) and STATA (StataCorp., College Station, TX). Forest plots are used to summarize multivariable linear regression results (Clark and Djulbegovic, 2001).
3. Results
3.1. Household air pollutant kitchen area concentrations and personal exposures
We collected HAP samples in 180 households. Mean kitchen area 48-hour CO concentrations were 52 ppm (inter quartile range, IQR: 45–59 ppm), five times greater than the WHO indoor 24-hour guideline (9.4 ppm). Average daily kitchen area PM2.5 concentrations were 1,205 μg/m3 (422–1,824 μg/m3), approximately 50 times the WHO indoor daily guideline (25 μg/m3) and more than 15 times the most flexible interim WHO target of 75 μg/m3. Mean kitchen area BC concentration were 171 μg/m3 (84–282 μg/m3), which represents 16% of the estimated PM2.5 mass, on average (Figure 2).
Figure 2.
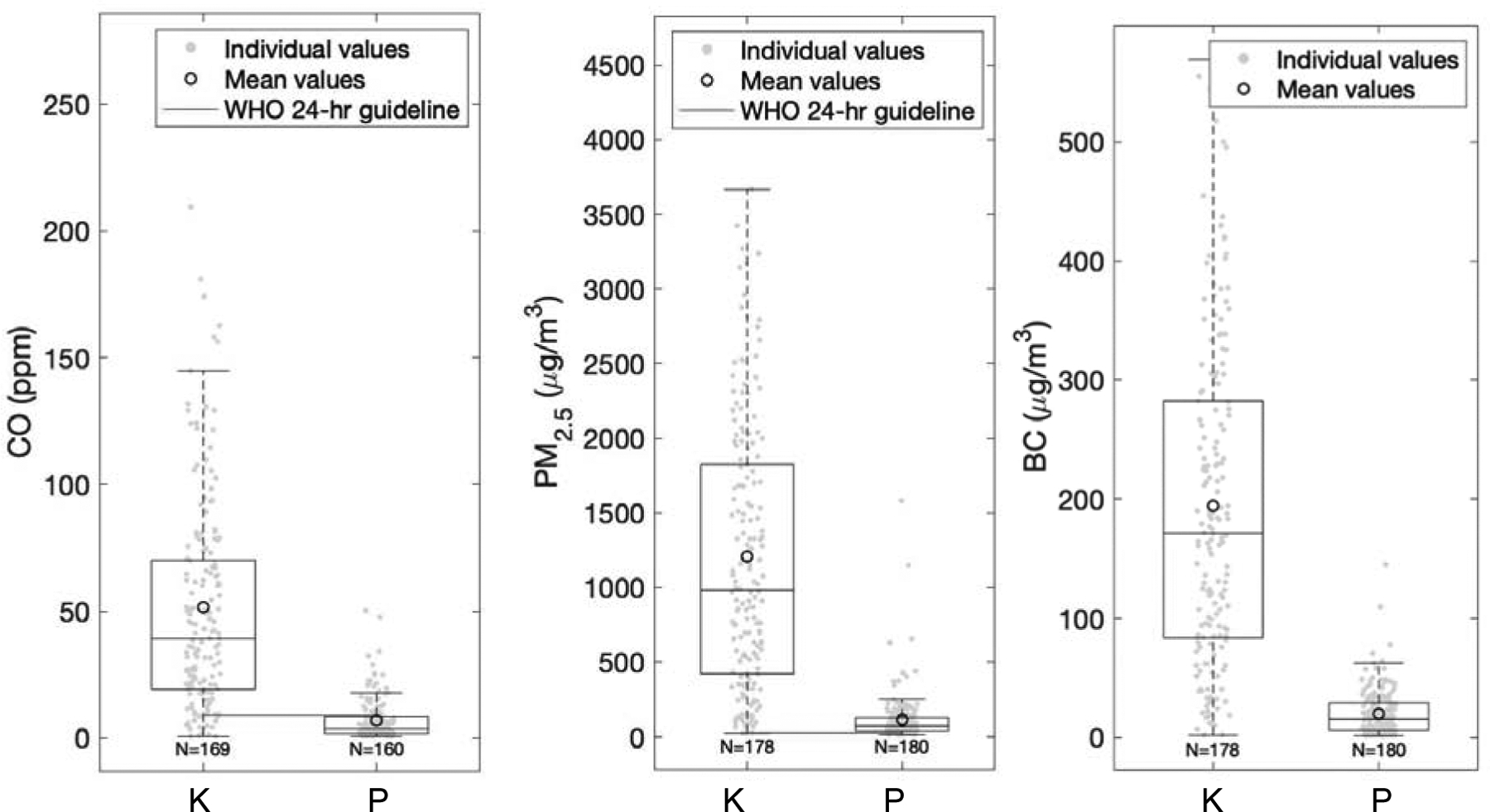
Baseline 48-hour mean kitchen area concentrations (K) and personal exposures (P) box plots for CO, PM2.5, and BC. Interquartile ranges of the box plots represent the 25th and the 75th percentiles of the 48-hr means for each group; the middle line of the box represents the 50th percentile; the circle represents the average of the group; the sample size is indicated under each box plot. The red lines represent the WHO indoor 24-hour guideline for CO (9.4 ppm) and PM2.5 (25 μg/m3). There is no WHO indoor guideline for BC. Acronyms: BC: black carbon; PM2.5: fine particulate matter; CO: carbon monoxide, WHO: World Health Organization.
Mean 48-hour personal exposures to CO were 6.9 ppm (IQR: 5.6 −8.2 ppm). Daily average personal exposures to PM2.5 were 115 μg/m3 (40–130 μg/m3), which is 5 times the WHO daily guideline. BC personal exposures were estimated to be, on average, 16 μg/m3 (6–29 μg/m3), which represents 17% of the estimated PM2.5 mass for personal exposure.
3.2. Household characteristics
We include variables that were associated with HAP in Table 1. All 180 households reported dung as their primary fuel and 42% of homes reported additionally using wood. Most households (73%) reported owning an LPG stove as a secondary stove for cooking (Figure 3 shows examples of different types of LPG stoves observed). We identified that for those households without a chimney, participants frequently positioned the stoves in a recessed area in the kitchen, which has an opening for the smoke to escape but does not directly funnel smoke from the stove (Figure 4A–B). This recessed structure was previously observed although not included in previous analyses within this setting (Pollard et al., 2014). Eleven percent of participants (19 households) had chimneys (Figure 4C–D includes examples of the types of chimneys observed) over their traditional stove and half of participants (91) had the stove in a recessed area with a simple opening in the roof (Figure 4A–B). Most of the households reported having electricity in their homes and using it as the primary method used for lighting the home (97%). All households had only one door and 17% reported leaving it permanently open. Most participants (82%) burn trash at home and only 3% reported sleeping in the kitchen.
Figure 3.

Examples of LPG stoves as secondary stoves for cooking used in the study area
Figure 4.

Examples of traditional stoves located in recessed areas in the kitchens of study participants (A, B) and chimneys used by study participants with traditional stoves (C, D).
3.3. Household characteristics associated with concentrations and exposures
We found strong associations between kitchen area HAP concentrations and the following characteristics: roof type, rainy season and wealth quintile in multivariable models. Variables that were associated with HAP personal exposure, after controlling for other household variables, included: having an LPG stove in addition to the traditional biomass stove, number of bedrooms, roof type, stove ventilation, and sample duration (24-hours versus 48-hours). The final multivariable models explained 14% of PM2.5, 24% of CO and 27% of BC kitchen concentration variability (21%, 6%, and 17% variability of personal exposures, respectively).
The kitchen characteristic that was consistently and significantly associated with HAP in the kitchen area and personal exposures was roof type. The associations were robust when controlling for other variables in the multivariable models for all pollutants. The effect of roof type was much larger than the effect of wealth quintile, which incorporates roof type in addition to the possession of other household materials related to higher wealth. The type of roof explained the most variability among univariate models for kitchen area PM2.5 (12%; Table S1) and CO (16%). We found that corrugated metal roof kitchens were significantly associated with lower kitchen concentrations and personal exposures for all pollutants compared to having roof of natural materials (straw, totora or reed). Concentrations in the kitchen were 50%, 58% and 37% lower for PM2.5, CO and BC, respectively, for corrugated metal roof kitchens compared to natural fiber roofs after adjusting for other household variables (Figure 5). Personal exposures were 27%, 27% and 36% lower for PM2.5, CO and BC, respectively, in households with corrugated metal roofs compared to natural roof material after adjusting for other household variables (Figure 6).
Figure 5.
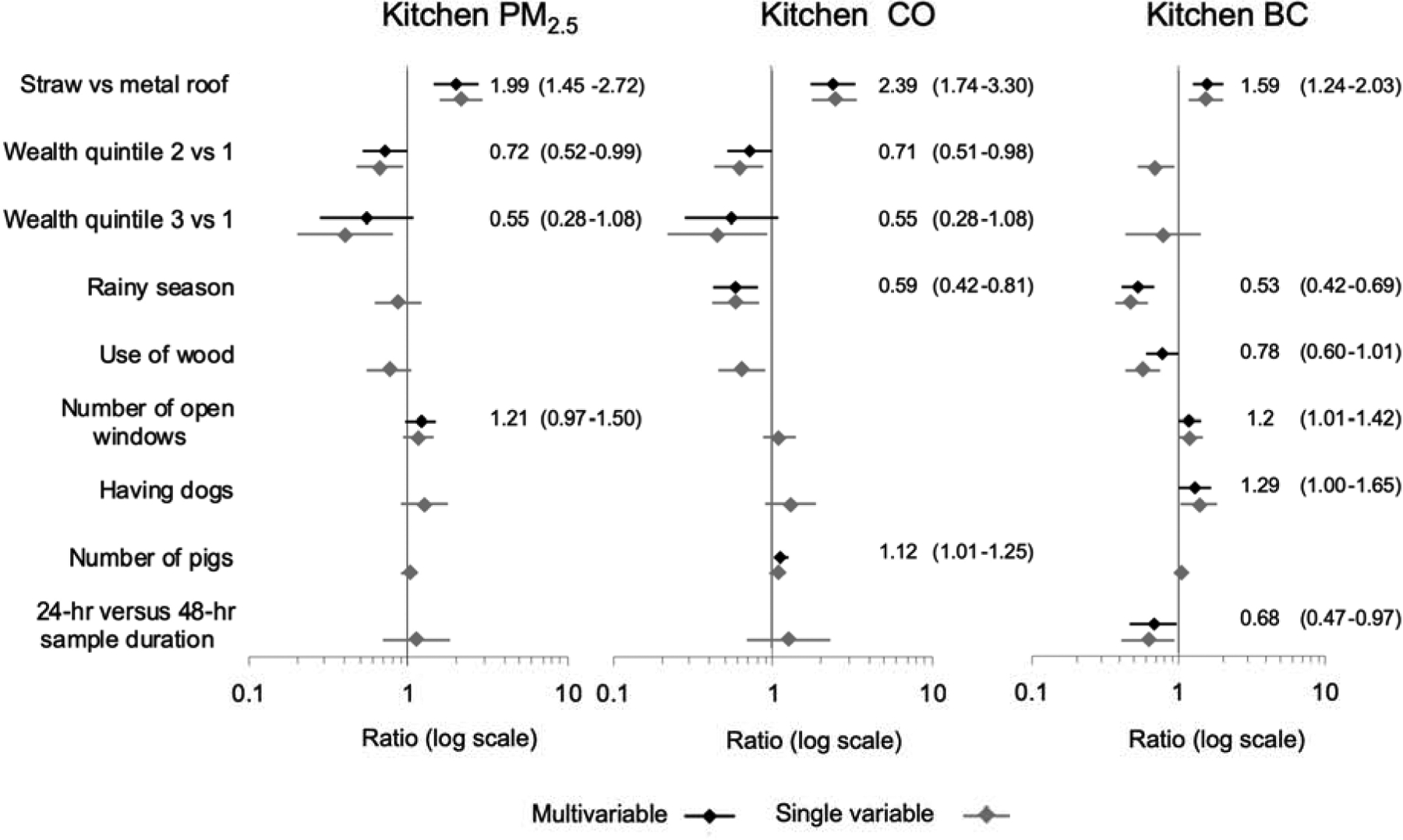
Forest plots of multivariable linear regression coefficients (with 95% confidence intervals) of the associations between household variables and kitchen area concentrations. Multivariable model results are shown in black with numeric coefficients and 95% CI; single variable regression coefficients are shown in lighter gray. Multivariable model covariates of each kitchen area pollutant: PM2.5 includes roof type, wealth quintile and number of open windows; CO covariates include roof type, wealth quintile, rainy season and number of pigs; BC covariates include: roof type, rainy season, use of wood, number of open windows, having dogs and samples with only the first 24 h. Each of the regression model estimates represents the ratio of the geometric mean on the pollutant compared to the reference category based on the final multivariable linear regression models. For example, a ratio of 1.1 translates to 10% higher concentrations and a value of 0.9 translates in a 10% lower concentration compared to the reference category. Abbreviations: PM2.5: fine particulate matter; CO: carbon monoxide; BC: black carbon.
Figure 6.
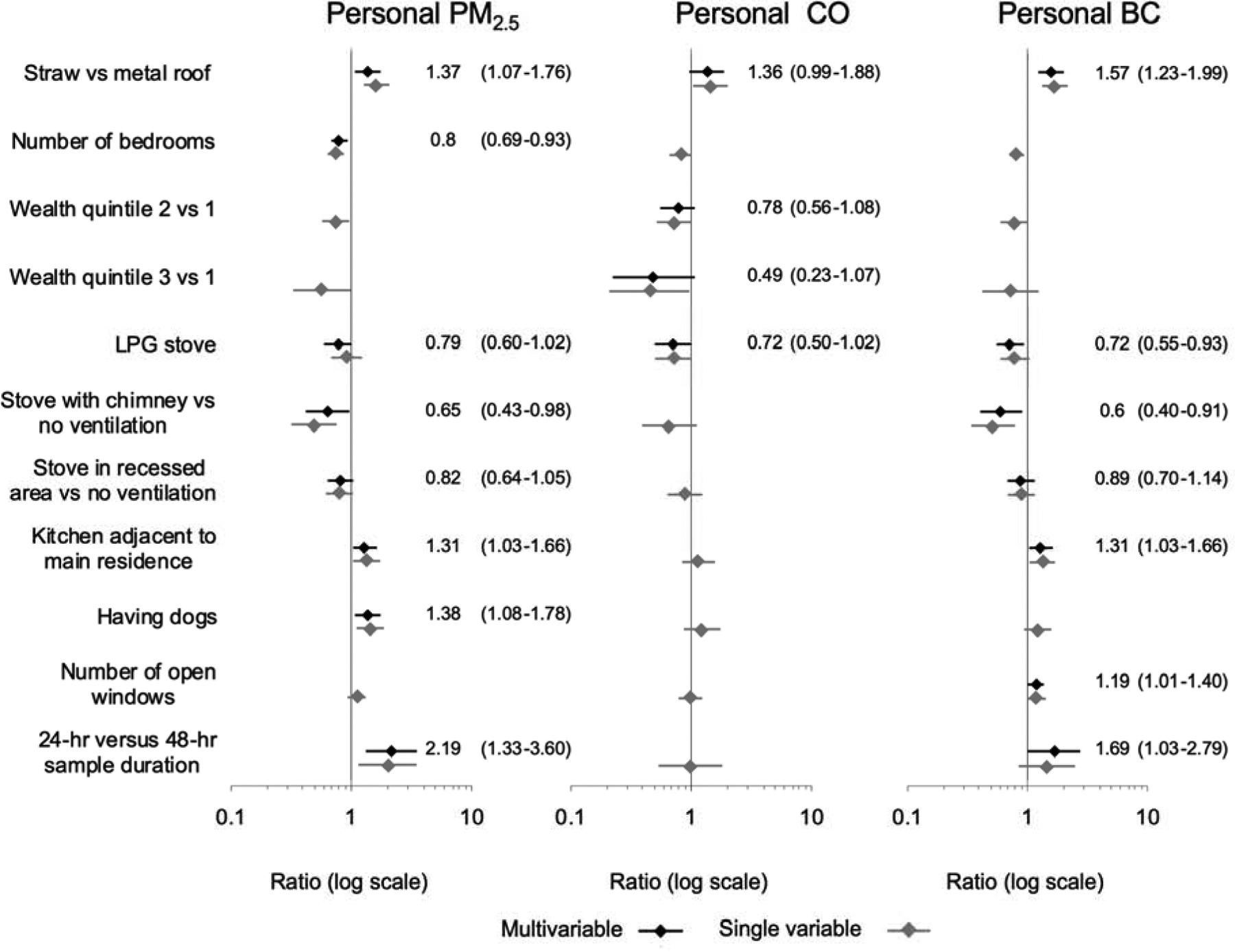
Personal exposure forest plots of linear regression coefficient results of multivariable linear regression models of household variables (with 95% confidence intervals). Multivariable model results are shown in black with numeric coefficients and 95% CI; single variable regression coefficients are shown in lighter gray. Multivariable model covariates of each personal exposure pollutant: PM2.5 includes roof type, number of bedrooms, LPG stove, stove ventilation, kitchen with adjacent wall to the main residence, having dogs and samples with only the first 24 h; CO covariates include roof type, wealth quintile and LPG stove; BC covariates include: roof type, LPG stove, stove ventilation, kitchen with adjacent wall to the main residence, number of open windows and samples with only the first 24 h. Each of the regression model estimates represents the ratio of the geometric mean on the pollutant compared to the reference category based on the final multivariable linear regression models. For example, a ratio of 1.1 translates to 10% higher concentrations and a value of 0.9 translates in a 10% lower concentration compared to the reference category. Abbreviations: PM2.5: fine particulate matter; CO: carbon monoxide; BC: black carbon.
The relationship of wealth to kitchen area concentrations was strong (showing concentration reductions for PM2.5 and CO of 45%, for the third quintile compared to the lowest quintile, and reductions of approximately 30% for the second quintile compared to the lowest quintile after adjusting for other household variables; Figure 5). Wealth was only associated with personal exposures for CO in multivariable models, having a similar impact to that of the kitchen area model for CO (reduction of 22% and 51% among those in the 2nd and 3rd quintiles, respectively, compared to the first quintile, indicating the least wealth; Figure 6) but not showing significance for particulate pollutants.
Owning an LPG stove in addition to a biomass cookstove did not impact kitchen area concentrations, but it did have an impact on personal exposures. Concentrations were lower by 21% for PM2.5 and 28% for CO and BC concentrations when participants reported having an LPG stove in multivariable models (Figure 6). In the kitchen area, the use of wood (in addition to dung used by all participants) was generally associated with reduced concentrations in univariate models of all pollutants and was a robust variable explaining variability in the multivariate model for BC.
Better stove ventilation was associated with a reduction of personal exposures, particularly for PM2.5 and BC in multivariable models (Figure 6). Concentrations in households with a chimney were 35% and 40% lower for PM2.5 and BC, respectively, compared to households with no stove ventilation. Having the stove in a recessed area did not significantly impact any of the pollutants measured (p-values>0.1). The physical structure of the home also influenced personal exposures. Having additional bedrooms reduced personal exposures of PM2.5 (−20% for every additional bedroom) in multivariable models. The number of open widows was associated with a slightly higher kitchen area concentrations (20% for PM2.5 and BC for each additional window) after controlling for other household variables.
Samples taken during the rainy season (December, January, February, March) had lower kitchen area concentrations compared to samples not taken during that season (Figure 6). Number of open windows and having pigs and dogs was associated with a slight increase in kitchen area concentrations (Table S1) although these variables contributed very little (< 3%) to explaining kitchen area concentration variability. Results of the single variable linear regression models along with the multivariable linear regression models are shown in Table S1 (kitchen area concentrations) and Table S2 (personal exposures).
4. Discussion
We found that the kitchen area concentrations of HAP were twice as high in households with natural roof material as opposed to households with corrugated metal roofs. When visiting participant homes, we observed that the natural straw or totora roof materials leave less space between the walls and the roof for smoke to leak out of the home compared to corrugated metal roofs, likely resulting in reduced ventilation for natural materials roofs (Figure S1). In addition, we observed more soot accumulation in the natural roof materials compared to corrugated metal roofs, possibly further reducing ventilation. In households with a corrugated metal roof type, participants had on average between 30% to 40% lower personal exposures compared to other households, after controlling for other household characteristics (including wealth, for CO). These reductions are comparable to what has been achieved for some improved stove interventions such as stoves with chimneys (Pope et al., 2017), although such concentrations are substantially above WHO guidelines (Clark et al., 2013; Pope et al., 2017; Thomas et al., 2015).
It is possible that the type of thatch roofs and the way they are built in this region are particularly good at insulating the kitchens. Several kitchen roofs are made of a type of reed called totora that grows in the Titicaca lake and that local communities often use to build boats and floating islands. This material has been shown to have unique insulating and water proof properties making it comparable to industrial materials (Aza et al., 2017; Fernando Hidalgo-Cordero and García-Navarro, 2017).
Although we did not find that having an LPG stove as a secondary stove impacted kitchen area concentrations, it did have an impact on personal exposures. We observed reductions of almost 30% in personal exposures among households with an LPG stove compared to no LPG stove. These reductions were consistent for all pollutants (PM2.5, CO and BC) after adjusting for other household variables. A previous paper describing the successes and challenges of the government program to promote the use of LPG stoves in Puno (Pollard et al., 2018) concluded that less than 5% of beneficiaries reported exclusively using LPG stoves, likely because the quantity of fuel provided by the program is insufficient to meet cooking needs. That study also used data from a subset of 95 of our CHAP households and found a slight reduction in PM2.5 personal exposures among households participating in the program (Pollard et al., 2018). Rural communities in Puno that have an LPG stove do not show the reductions in HAP concentrations that may be expected from switching from biomass cookstoves to exclusive LPG stove use (Balakrishnan et al., 2014). Kitchen area HAP might not be impacted because the main cooking events are probably still being done with biomass cookstoves and were not replaced with LPG stoves. It is possible that the reductions of personal exposures are detected because women move between the traditional and LPG stoves when cooking with both simultaneously. It is also possible that participants transition some cooking tasks to the LPG stove, though not enough to significantly impact HAP in the kitchen area. Interventions that impact personal exposures may have more meaningful impacts on health and should be prioritized.
Having more bedrooms was associated with lower PM2.5 personal exposures (approximately 20% lower for each additional bedroom). This could be because the participants spend more time in those bedrooms when available and less time in the kitchen. Having more open windows in the kitchen was associated with a slight increase in kitchen area BC concentrations. We would have expected open windows would be associated with lower concentrations due to increased ventilation. However, it is possible that participants open the windows more often when more highly visible smoke is generated. Given the distance between households (Fandiño-Del-Rio et al., 2017) and the lack of other outdoor air pollution sources in the region (Pollard et al., 2014), we don’t expect that increased infiltration of ambient pollution explains this association. The number of windows was not associated with HAP in previous studies in this area (Pollard et al., 2014), however, in other locations, studies have found that windows were important in explaining concentration variability (Clark et al., 2010). Households in rural Puno are at high altitude and in a cold climate, therefore windows may not be a major source of ventilation.
Compared with previous measurements in rural households in the same area by Pollard et al., the PM2.5 concentrations measured in this study were much higher (Pollard et al., 2014). This difference might be explained by the differences in sampling methods. Pollard et al. selected a smaller sample of households and collected passive nephelometric measurements on most households. That study used a calibration curve developed with a mixture of urban and rural households to adjust the nephelometric measurements. In contrast, we were able to calibrate every individual sample using simultaneous nephelometric and gravimetric data for all of our samples since our monitors used active sampling (air is sampled using a pump). Passive sampling has been shown to underestimate concentrations and to have different biases for different types of aerosol mixtures (Thorpe and Walsh, 2007).
Contrary to our results, Pollard et al. found that hours spent cooking was related to HAP in Puno. However, Pollard et al. also included urban participants that use cleaner fuels more often compared to rural participants. Rural households in Puno showed little variability in hours spent cooking (as opposed to urban households in the area) limiting our ability to see an effect. Most of our participants reported cooking for about 3 to 4 hours each day; compared to urban households that reported a wider range in time spent cooking (from 1 to 6 hours) (Pollard et al., 2014).
Household characteristics that provide ventilation and impact personal exposures can have different impacts on gases compared to particles. The presence of a chimney or having the stove in a recessed area explained variability of personal exposures for PM2.5 and BC but not CO. Households structures and air flow in and out of the kitchen might remove particles in a different way compared to gases given the mechanism by which they can interact with surfaces after being emitted. Particles have a tendency to impact and adhere to surfaces much more than gases (Hinds, 1999). We observed thick layers of soot accumulation on kitchen walls and roofs of participants. Gases such as CO are less influenced by kitchen surfaces.
The presence of a chimney reduced personal exposures of PM2.5 and BC but did not impact kitchen area concentrations. This result was unexpected. However, we observed that the construction of chimneys varied widely between households and that they often had leaks and cracks that allowed the smoke to escape back to the kitchen, likely limiting their effectiveness.
We also observed some other variables that explained either kitchen or personal exposures but not both. For example, rainy season impacted CO and BC kitchen concentrations but not personal exposures. During rainy seasons there is less dry fuel available, potentially reducing the amount of fuel used for cooking. This, however, might not impact personal exposures since the behavior of participants and the amount of time they spend close to the stove attending the fire may remain unchanged.
Sample duration, on the other hand, impacted PM2.5 personal exposures but not kitchen area concentrations. Most personal samples reached 48-hour duration and only 10 samples were only 24-hour duration. These shorter duration samples included an outlier sample with a high concentration, in which is it possible the monitor was left in the kitchen for a prolonged period of time while not worn. This explains the higher mean concentration for the 24-hour samples compared to 48-hour samples. However, our results and overall conclusions do not change when we restrict the models to the 48-hour duration samples. We did not observe important differences among the 48-hour duration samples in wearing compliance when comparing the first and second day of the sample. We also did not observe any consistent trends in individual concentrations differences when comparing first and second day concentrations among samples with a 48-hour duration. Thus, 48-hour samples likely better represent the “typical” personal exposures better than 24-hour duration samples.
This study has many strengths. We collected household characteristics of 180 participants and were able to quantify the impact of these household characteristics on HAP. We collected 48-hour samples for most of our participants, which allowed us to estimate typical exposures in this setting. We were able to collect simultaneous active gravimetric samples and direct-reading continuous measurements for PM2.5, which allowed for better precision in calibrating each sample. We also identified the impact of different fuel types on HAP concentrations and personal exposures for the first time in rural Peru. In particular, we quantified the impact of having an LPG stove and the use of wood on HAP concentrations. Being able to incorporate personal exposures in our analysis allowed us to identify associations that had not been previously identified. We developed models for three different pollutants, which was important to identify the consistency of the associations.
This study was also subject to several limitations. The variables included in the analysis explained less than 30% of the total variability in HAP concentrations. We did not collect other variables that may have an important impact on HAP and emissions such as amount of fuel used by household, household dimensions, and detailed fuel characteristics. We observed that participants use a mixture of fuels, therefore, we were not able to estimate the individual impact of different fuel types on HAP. We did not collect information regarding the size of the kitchens, chimney quality, roof quality, or roof age. The number of kitchens with chimneys was limited probably reducing our capacity to identify their potential impact on the pollutants measured. Even though samples were evenly spaced through an entire year of data collection, we would have been able to better estimate the impact of seasonality if each participant had received a baseline sample in both the rainy and dry seasons. However, we identified household characteristics that influenced personal exposures, which can be used in future studies or interventions to optimize interventions to reduce HAP exposures.
Despite identifying the impact of certain household characteristics on HAP, concentrations still remain substantially higher than WHO guidelines. When possible, cleaner fuel interventions such as exclusive use of LPG stoves should be prioritized. However, using LPG stoves non-exclusively, installing chimneys, and metal roofs types may reduce HAP personal exposures and be an actionable intervention in communities where the exclusive use of cleaner fuels such as LPG is not feasible. These actionable interventions identified could be used in conjunction with clean fuel interventions to promote ventilation in the kitchen, further reduce HAP, and reduce personal exposures.
5. Conclusions
Characterizing HAP in different settings can help identify culturally-relevant and effective local solutions to reduce HAP exposures. Improving kitchen ventilation, associated with having metal roof types and chimneys, and increasing use of LPG stoves could help reduce exposures to HAP in high-altitude rural Peru and similar settings where exclusive LPG stove use is not yet feasible. However, these measures in the absence of exclusive LPG use are unlikely to achieve the WHO guidelines for pollutant concentrations. Thus, efforts should continue to focus on promoting clean fuels in tandem with household modifications.
Supplementary Material
Highlights:
Kitchen concentrations in Puno were, on average, 48 times the PM2.5 recommended levels.
Kitchens with metal roofs had 50% lower PM2.5 compared to straw and reed roofs.
Women who owned LPG stoves had 21% lower personal exposures to PM2.5.
Personal exposures to PM2.5 were 35% lower in kitchens with a chimney.
LPG stoves and ventilation provided by metal roofs reduce personal exposures to HAP.
7. Acknowledgments
The authors would like to thank the field staff including Ida Luz Mamani, William Paucar, Julio Sucasaca, Edith Arocutipa, and Elena Morales (A.B. PRISMA, Puno, Peru), the study participants in Puno, Peru, Phabiola Herrera (Johns Hopkins University, Baltimore, MD, USA), David Danz (A.B. PRISMA, Puno, Peru), Juan Gabriel Espinoza (A. B. PRISMA, Lima, Peru), Lisa de las Fuentes (Washington University School of Medicine, St. Louis, MO, USA), Luke Naeher (University of Georgia, Athens, GA, USA), Ryan Chartier (RTI International, Chapel Hill, NC, USA), and Joshua Rosenthal (Fogarty International Center, National Institutes of Health, Bethesda, MD, USA) for their help providing technical assistance in data collection with this study.
Funding Sources: Research reported in this publication was supported by the United States National Institutes of Health through the following Institutes and Centers: Fogarty International Center, National Institute of Environmental Health Sciences, National Cancer Institute, National Institute for Occupational Safety and Health, and Centers for Disease Control under NIH Collaborative Grant 1U2RTW010114-01 and award number U01TW010107 (MPIs: Checkley, Gonzales, Naeher, Steenland). This trial was additionally supported in part by the Clean Cooking Alliance of the United Nations Foundation UNF-16-810 (PI: Checkley). Dr. Fandiño-Del-Rio was further supported by the Global Environmental and Occupational Health (GEOHealth) and the Fogarty International Center of the United States National Institutes of Health and by the David Leslie Swift Fund of the Bloomberg School of Public Health, Johns Hopkins University. Dr. Williams and Dr. Kephart were supported by United States National Institutes of Health Research Training Grant D43TW009340 (MPIs: Buekens, Checkley, Chi, Kondwani) funded by United States National Institutes of Health through the following Institutes and Centers: Fogarty International Center, National Institute of Neurological Disorders and Stroke, National Institute of Mental Health, National Heart, Lung, and Blood Institute and the National Institute of Environmental Health Sciences. Dr. Kephart, Dr. Williams, Dr. Fandiño-Del-Rio, were supported by a Global Established Multidisciplinary Sites award from the Center for Global Health at Johns Hopkins University (PI: Checkley). Dr. Kephart was further supported by the National Institute of Environmental Health Sciences of the National Institutes of Health under Award number T32ES007141 (PI: Wills-Karp). Dr. Williams was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number T32HL007534 (PI: Wise). Our Global Non-Communicable Disease Research and Training field center in Puno, Peru, also received generous support from Mr. William and Bonnie Clarke III and the COPD Discovery Award from Johns Hopkins University. The content is solely the responsibility of the authors and does not necessarily represent the official views of these organizations.
Abbreviations:
- BC
black carbon
- CHAP
Cardiopulmonary outcomes and Household Air Pollution
- CO
carbon monoxide
- LPG
liquefied petroleum gas
- PM2.5
fine particulate matter
- WHO
World Health Organization
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval and consent
The trial received approval by Johns Hopkins School of Public Health Institutional Review Board (IRB00007128), A.B. PRISMA Ethical Institutional Committee (CE2402.16), and Universidad Peruana Cayetano Heredia Institutional Review Board (SIDISI 66780). We requested verbal consent to participate from all participants at time of enrollment.
10. References
- Aza L, Palumbo M, Lacasta A, 2017. Totora used as thermal insulation: properties and potential. Acad. J. Civ. Eng 35, 416–421. 10.26168/icbbm2017.63 [DOI] [Google Scholar]
- Balakrishnan K, Ghosh S, Ganguli B, Sambandam S, Bruce N, Barnes DF, Smith KR, 2013. State and national household concentrations of PM2.5 from solid cookfuel use: Results from measurements and modeling in India for estimation of the global burden of disease. Environ. Health 12, 77 10.1186/1476-069X-12-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balakrishnan K, Mehta S, Ghosh S, Johnson M, Brauer M, Zhang J, Naeher L, Smith KR, 2014. WHO | Indoor air quality guidelines: household fuel combustion. Review 5: Population levels of household air pollution and exposures [WWW Document]. URL http://www.who.int/airpollution/guidelines/household-fuel-combustion/evidence/en/ (accessed 1.8.19). [Google Scholar]
- Beelen R, Stafoggia M, Raaschou-Nielsen O, Andersen ZJ, Xun WW, Katsouyanni K, Dimakopoulou K, Brunekreef B, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Houthuijs D, Nieuwenhuijsen M, Oudin A, Forsberg B, Olsson D, Salomaa V, Lanki T, Yli-Tuomi T, Oftedal B, Aamodt G, Nafstad P, De Faire U, Pedersen NL, Östenson C-G, Fratiglioni L, Penell J, Korek M, Pyko A, Eriksen KT, Tjønneland A, Becker T, Eeftens M, Bots M, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Krämer U, Heinrich J, de Hoogh K, Key T, Peters A, Cyrys J, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Dratva J, Ducret-Stich R, Vilier A, Clavel-Chapelon F, Stempfelet M, Grioni S, Krogh V, Tsai M-Y, Marcon A, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Vineis P, Hoek G, 2014. Long-term exposure to air pollution and cardiovascular mortality: an analysis of 22 European cohorts. Epidemiol. Camb. Mass 25, 368–378. 10.1097/EDE.0000000000000076 [DOI] [PubMed] [Google Scholar]
- Bonjour S, Adair-Rohani H, Wolf J, Bruce NG, Mehta S, Prüss-Ustün A, Lahiff M, Rehfuess EA, Mishra V, Smith KR, 2013. Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environ. Health Perspect 121, 784–790. 10.1289/ehp.1205987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F, 2002. Inhalation of Fine Particulate Air Pollution and Ozone Causes Acute Arterial Vasoconstriction in Healthy Adults. Circulation 105, 1534–1536. 10.1161/01.CIR.0000013838.94747.64 [DOI] [PubMed] [Google Scholar]
- Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Luepker R, Lipsett M, Mittleman M, Samet J, Smith S, Tager I, Expert Panel on Population and Preventative Science of the American Heart Association, 2004. Air Pollution and Cardiovascular Disease: A Statement for Healthcare Professionals From the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109, 2655–2671. [DOI] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S, Pope C, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker R, Mittleman M, Peters A, Siscovick D, Smith SC, Whitsel L, Kaufman JD, American Heart Association Council on Epidemiology and Prevention, Council on the Kidney in Cardiovascular Disease, and Council on Nutrition, Physical Activity and Metabolism, 2010. Particulate Matter Air Pollution and Cardiovascular Disease: An Update to the Scientific Statement From the American Heart Association. Circulation 121, 2331–2378. [DOI] [PubMed] [Google Scholar]
- Bruce N, Perez-Padilla R, Albalak R, 2000. Indoor air pollution in developing countries: a major environmental and public health challenge. Bull World Health Organ 78, 1078–1092. [PMC free article] [PubMed] [Google Scholar]
- Chan SH, Van Hee VC, Bergen S, Szpiro AA, DeRoo LA, London SJ, Marshall JD, Kaufman JD, Sandler DP, 2015. Long-Term Air Pollution Exposure and Blood Pressure in the Sister Study. Environ. Health Perspect 123, 951–958. 10.1289/ehp.1408125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow JC, Watson JG, Green MC, Frank NH, 2010. Filter Light Attenuation as a Surrogate for Elemental Carbon. J. Air Waste Manag. Assoc 60, 1365–1375. 10.3155/1047-3289.60.11.1365 [DOI] [PubMed] [Google Scholar]
- Clark ML, Peel JL, Balakrishnan K, Breysse PN, Chillrud SN, Naeher LP, Rodes CE, Vette AF, Balbus JM, 2013. Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environ. Health Perspect 121, 1120–1128. 10.1289/ehp.1206429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark ML, Reynolds SJ, Burch JB, Conway S, Bachand AM, Peel JL, 2010. Indoor air pollution, cookstove quality, and housing characteristics in two Honduran communities. Environ. Res 110, 12–18. 10.1016/j.envres.2009.10.008 [DOI] [PubMed] [Google Scholar]
- Clark O, Djulbegovic B, 2001. Forest plots in excel software(Data sheet). 2001. Available at www.evidencias.com.
- Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH, 2017. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet Lond. Engl 389, 1907–1918. 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupont WD, 2009. Statistical modeling for biomedical researchers: a simple introduction to the analysis of complex data, 2nd ed. Cambridge University Press, Cambridge, UK New York. [Google Scholar]
- Fandiño-Del-Rio M, Goodman D, Kephart JL, Miele CH, Williams KN, Moazzami M, Fung EC, Koehler K, Davila-Roman VG, Lee KA, Nangia S, Harvey SA, Steenland K, Gonzales GF, Checkley W, 2017. Effects of a liquefied petroleum gas stove intervention on pollutant exposure and adult cardiopulmonary outcomes (CHAP): study protocol for a randomized controlled trial. Trials 18. 10.1186/s13063-017-2179-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernando Hidalgo-Cordero J, García-Navarro J, 2017. Review on the Traditional Uses and Potential of Totora (Schoenoplectus Californicus) as Construction Material. IOP Conf. Ser. Mater. Sci. Eng 245, 022068 10.1088/1757-899x/245/2/022068 [DOI] [Google Scholar]
- Fullerton D, Bruce N, Gordon S, 2008. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans. R. Soc. Trop. Med. Hyg 102, 843–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold DR, Samet JM, 2013. Air Pollution, Climate, and Heart Disease. Circulation 128, e411–e414. 10.1161/CIRCULATIONAHA.113.003988 [DOI] [PubMed] [Google Scholar]
- Gordon SB, Bruce NG, Grigg J, Hibberd PL, Kurmi OP, Lam KH, Mortimer K, Asante KP, Balakrishnan K, Balmes J, Bar-Zeev N, Bates MN, Breysse PN, Buist S, Chen Z, Havens D, Jack D, Jindal S, Kan H, Mehta S, Moschovis P, Naeher L, Patel A, Perez-Padilla R, Pope D, Rylance J, Semple S, Martin WJ, 2014. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med 2, 823–860. 10.1016/S2213-2600(14)70168-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds WC, 1999. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. John Wiley & Sons. [Google Scholar]
- Hornung RW, Reed LD, 1990. Estimation of Average Concentration in the Presence of Nondetectable Values. Appl. Occup. Environ. Hyg 5, 46–51. 10.1080/1047322X.1990.10389587 [DOI] [Google Scholar]
- Kelly FJ, Fussell JC, 2012. Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos. Environ 60, 504–526. 10.1016/j.atmosenv.2012.06.039 [DOI] [Google Scholar]
- Kephart JL, Fandiño-Del-Rio M, Williams KN, Malpartida G, Steenland K, Naeher LP, Gonzales GF, Chiang M, Checkley W, Koehler K, 2020. Nitrogen dioxide exposures from biomass cookstoves in the Peruvian Andes. Indoor Air 30, 735–744. 10.1111/ina.12653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klasen EM, Wills B, Naithani N, Gilman RH, Tielsch JM, Chiang M, Khatry S, Breysse PN, Menya D, Apaka C, Carter EJ, Sherman CB, Miranda JJ, Checkley W, 2015. Low correlation between household carbon monoxide and particulate matter concentrations from biomass-related pollution in three resource-poor settings. Environ. Res 142, 424–431. 10.1016/j.envres.2015.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, Turner MC, Pope CA, Thurston G, Calle EE, Thun MJ, Beckerman B, DeLuca P, Finkelstein N, Ito K, Moore DK, Newbold KB, Ramsay T, Ross Z, Shin H, Tempalski B, 2009. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res. Rep. Health Eff. Inst 5–114; discussion 115–136. [PubMed] [Google Scholar]
- Kulkarni NS, Prudon B, Panditi SL, Abebe Y, Grigg J, 2005. Carbon loading of alveolar macrophages in adults and children exposed to biomass smoke particles. Sci. Total Environ 345, 23–30. 10.1016/j.scitotenv.2004.10.016 [DOI] [PubMed] [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD, 2007. Long-Term Exposure to Air Pollution and Incidence of Cardiovascular Events in Women. N. Engl. J. Med 356, 447–458. 10.1056/NEJMoa054409 [DOI] [PubMed] [Google Scholar]
- Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, Périer M-C, Marijon E, Vernerey D, Empana J-P, Jouven X, 2012. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA 307, 713–721. 10.1001/jama.2012.126 [DOI] [PubMed] [Google Scholar]
- Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, Forastiere F, Franchini M, Franco OH, Graham I, Hoek G, Hoffmann B, Hoylaerts MF, Künzli N, Mills N, Pekkanen J, Peters A, Piepoli MF, Rajagopalan S, Storey RF, 2015. Expert position paper on air pollution and cardiovascular disease. Eur. Heart J 36, 83–93. 10.1093/eurheartj/ehu458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northcross AL, Hwang N, Balakrishnan K, Mehta S, 2015. Assessing Exposures to Household Air Pollution in Public Health Research and Program Evaluation. Ecohealth 12, 57–67. 10.1007/s10393-014-0990-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill MS, Veves A, Zanobetti A, Sarnat JA, Gold DR, Economides PA, Horton ES, Schwartz J, 2005. Diabetes Enhances Vulnerability to Particulate Air Pollution–Associated Impairment in Vascular Reactivity and Endothelial Function. Circulation 111, 2913–2920. 10.1161/CIRCULATIONAHA.104.517110 [DOI] [PubMed] [Google Scholar]
- Pollard SL, Williams DL, Breysse PN, Baron PA, Grajeda LM, Gilman RH, Miranda JJ, Checkley W, CRONICAS Cohort Study Group, 2014. A cross-sectional study of determinants of indoor environmental exposures in households with and without chronic exposure to biomass fuel smoke. Environ. Health Glob. Access Sci. Source 13, 21 10.1186/1476-069X-13-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard SL, Williams KN, O’Brien CJ, Winiker A, Puzzolo E, Kephart JL, Fandiño-Del-Rio M, Tarazona-Meza C, Grigsby MR, Chiang M, Checkley W, 2018. An evaluation of the Fondo de Inclusión Social Energético program to promote access to liquefied petroleum gas in Peru. Energy Sustain. Dev 10.1016/j.esd.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C, Burnett R, Krewski D, Jerrett M, Shi Y, Calle E, Thun M, 2009. Cardiovascular Mortality and Exposure to Airborne Fine Particulate Matter and Cigarette Smoke: Shape of the Exposure-Response Relationship. Circulation 120, 941–948. [DOI] [PubMed] [Google Scholar]
- Pope CA, Burnett RT, Thurston GD, Thun MJ, Callee EE, Krewski D, Godleski JJ, 2004. Cardiovascular Mortality and Long-Term Exposure to Particulate Air Pollution: Epidemiological Evidence of General Pathophysiological Pathways of Disease. Circulation 109, 71–77. [DOI] [PubMed] [Google Scholar]
- Pope D, Bruce N, Dherani M, Jagoe K, Rehfuess E, 2017. Real-life effectiveness of ‘improved’ stoves and clean fuels in reducing PM2.5 and CO: Systematic review and meta-analysis. Environ. Int 101, 7–18. 10.1016/j.envint.2017.01.012 [DOI] [PubMed] [Google Scholar]
- Quansah R, Semple S, Ochieng CA, Juvekar S, Armah FA, Luginaah I, Emina J, 2017. Effectiveness of interventions to reduce household air pollution and/or improve health in homes using solid fuel in low-and-middle income countries: A systematic review and meta-analysis. Environ. Int 103, 73–90. 10.1016/j.envint.2017.03.010 [DOI] [PubMed] [Google Scholar]
- Rundell K, Hoffman J, Caviston R, Bulbulian R, Hollenbach A, 2007. Inhalation of Ultrafine and Fine Particulate Matter Disrupts Systemic Vascular Function. Inhal. Toxicol. 19, 133–140. [DOI] [PubMed] [Google Scholar]
- Sana A, Somda SMA, Meda N, Bouland C, 2018. Chronic obstructive pulmonary disease associated with biomass fuel use in women: a systematic review and meta-analysis. BMJ Open Respir. Res 5 10.1136/bmjresp-2017-000246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shupler M, Godwin W, Frostad J, Gustafson P, Arku RE, Brauer M, 2018. Global estimation of exposure to fine particulate matter (PM2.5) from household air pollution. Environ. Int 120, 354–363. 10.1016/j.envint.2018.08.026 [DOI] [PubMed] [Google Scholar]
- Smith KR, Bruce N, Balakrishnan K, Adair-Rohani H, Balmes J, Chafe Z, Dherani M, Hosgood HD, Mehta S, Pope D, Rehfuess E, 2014. Millions Dead: How Do We Know and What Does It Mean? Methods Used in the Comparative Risk Assessment of Household Air Pollution. Annu. Rev. Public Health 35, 185–206. 10.1146/annurev-publhealth-032013-182356 [DOI] [PubMed] [Google Scholar]
- Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, Abbafati, 2018. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 392, 1923–1994. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas E, Wickramasinghe K, Mendis S, Roberts N, Foster C, 2015. Improved stove interventions to reduce household air pollution in low and middle income countries: a descriptive systematic review. BMC Public Health 15, 650 10.1186/s12889-015-2024-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe A, Walsh PT, 2007. Comparison of Portable, Real-Time Dust Monitors Sampling Actively, with Size-Selective Adaptors, and Passively. Ann. Occup. Hyg 51, 679–691. 10.1093/annhyg/mem047 [DOI] [PubMed] [Google Scholar]
- Wagenmakers E-J, Farrell S, 2004. AIC model selection using Akaike weights. Psychon. Bull. Rev 11, 192–196. 10.3758/BF03206482 [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2012. Health effects of black carbon (2012) [WWW Document]. URL http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/2012/health-effects-of-black-carbon-2012 (accessed 9.25.17).
- World Health Organization, 2010. WHO guidelines for indoor air quality: selected pollutants [WWW Document]. URL http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/2010/who-guidelines-for-indoor-air-quality-selected-pollutants (accessed 1.23.18). [PubMed]
- World Health Organization, 2009. Global Health Risks: mortality and burden of disease attributable to selected major risks WHO Press, Geneva. [Google Scholar]
- World Health Organization, 2006. Air quality guidelines global update 2005: particulate matter, ozone, nitrogen dioxide. and sulfur dioxide [WWW Document]. WHO. URL http://www.who.int/phe/health_topics/outdoorair/outdoorair_aqg/en/ (accessed 1.23.18). [PubMed]
- Xing Y-F, Xu Y-H, Shi M-H, Lian Y-X, 2016. The impact of PM2.5 on the human respiratory system. J. Thorac. Dis 8, E69–E74. 10.3978/j.issn.2072-1439.2016.01.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadama GN, 2013. Fires, Fuel, and the Fate of 3 Billion: The State of the Energy Impoverished. Oxford University Press, Oxford, New York. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


