Abstract
Background:
The Center for Medicare and Medicaid Innovation (CMMI) launched the Bundled Payments for Care Initiative (BPCI) in 2013. Its effect on payments and outcomes for percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) is unknown.
Methods and Results:
We used Medicare inpatient files to identify index admissions for PCI and CABG from 2013 through 2016 at BPCI hospitals and matched control hospitals, and difference in differences (DID) models to compare the two groups. Our primary outcome was the change in standardized Medicare allowed payments per 90-day episode. Secondary outcomes included changes in patient selection, discharge to post-acute care (PAC), length of stay (LOS), emergency department use, readmissions, and mortality. 42 hospitals joined BPCI for PCI and 46 for CABG. There were no differential changes in patient selection between BPCI and control hospitals. Baseline Medicare payments per episode for PCI were $20,164 at BPCI hospitals, and $19,955 at control hospitals. For PCI, payments increased at both BPCI and control hospitals during the intervention period, such that there was no significant difference-in-difference (BPCI hospitals + $673, p=0.048; control hospitals + $551, p=0.022; DID $122, p=0.768). For CABG, payments at both BPCI and control hospitals decreased during the intervention period (BPCI baseline, $36,925, change −$2,918, p<0.001; control baseline, $36,877, change −$2,618, p<0.001; DID, $300; p=0.730). For both PCI and CABG, BPCI participation was not associated with changes in mortality, readmissions, or LOS. Among BPCI hospitals, ED use differentially increased for patients undergoing PCI and decreased for patients undergoing CABG.
Conclusions:
Participation in episode-based payment for PCI and CABG was not associated with changes in patient selection, payments, LOS, or clinical outcomes.
Keywords: Medicare, PCI, CABG, bundled payment
Health care delivery is often fragmented and poorly coordinated, contributing to unnecessarily high spending and adverse clinical outcomes. In 2013, the Center for Medicare and Medicaid Innovation (CMMI) launched the Bundled Payments for Care Initiative (BPCI) in an effort to use a novel payment model to incentivize improvements in care.1 In contrast to the traditional fee-for-service model, which reimburses each provided service independently, in bundled payments, hospitals assume the financial responsibility for an entire “episode” of care, from admission through post-acute care. The BPCI program had four tracks; in Model 2, the topic of this analysis, the episode of care included the inpatient hospital stay plus all related services 30-, 60-, or 90 days after discharge. Enrolling hospitals selected to participate in one or more of 48 different clinical episodes. Total payments for the given care episode were then compared to target prices determined by the CMMI. Target prices are determined based on based historical data and risk adjustment models of patients and hospital peers.1,2 If the actual payments were below target payments, hospitals were able to keep a portion of the savings; if hospitals exceeded targets, they were required to reimburse Medicare for some of the difference.
Bundled payment models continue to expand. BPCI Advanced, which is a related bundled payments model encompassing both inpatient and outpatient care, began in October, 2018, and will run through October, 2023; 1299 participating hospitals and physician groups have already signed up for BPCI Advanced.2 Despite growing prevalence of these care models, there remains a paucity of information regarding their ability to reduce costs or whether they lead to any unintended consequences, such as compensatory increases in procedural volumes, restrictions in care for patients with high levels of comorbidity, or worsening clinical outcomes. The few completed studies have shown inconsistent results. For example, in studies of lower extremity joint replacement, bundled payments were associated with reduced payments without any apparent adverse outcomes.3–7 However, a prior study of the 5 most common medical conditions requiring hospitalization in Medicare patients (acute myocardial infarction, congestive heart failure, pneumonia, sepsis, and chronic obstructive pulmonary disease) demonstrated no association between participation in bundled payments for these conditions and reduced payments, readmission, mortality, or other major outcomes.8
Organizations participating in bundling may find it easier to alter clinical pathways for patients receiving procedures than for patients with medical problems. In this study we focused on percutaneous coronary intervention (PCI) and coronary bypass graft (CABG) surgery, two very common procedures. Cardiac procedures are not as elective as major joint replacement, but they are often planned, scheduled events that might be amenable to care redesign. While annual federal reports produced under contract with CMS have examined all conditions in the BPCI,3–6 to our knowledge there is nothing in the peer-reviewed literature examining changes in Medicare payments and clinical outcomes for cardiac procedures under BPCI.
Our goal was to evaluate the association of hospital participation in BPCI for percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) with changes in 1) patient selection for these procedures; 2) mean Medicare allowed payments per episode; and 3) clinical outcomes including length of stay, emergency department (ED) visits, mortality, readmission, and discharge to institutional post-acute care.
METHODS
The National Heart, Lung, and Blood Institute of the National Institutes of Health, which provided funding for the study, had no role in its design or conduct; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The requirement for informed consent was waived because the data were deidentified. The study was approved by the Human Research Protection Office at Washington University School of Medicine. Due to the sensitive nature of the data for this study, the authors are not authorized to share the data. Requests to access Medicare data must be requested at resdac.org
Data
We obtained publicly available lists of participating hospitals in Model 2 of BPCI from CMMI, which provided their start date for financial incentives, and the date they planned to terminate participation. From these lists, we identified hospitals enrolled by July 1, 2016, in bundles for PCI and CABG. These data were linked both to hospital characteristics, obtained from the 2014 American Hospital Association file, and to market characteristics such as availability of post–acute care services and median income levels, obtained from the Area Resource File. For each hospital, market share was calculated as the proportion of all admissions in the county for the condition of interest. Market competitiveness was calculated using the Herfindahl–Hirschman Index, which consists of the sum of squares of each hospital’s market share such that an HHI of zero represents a perfectly competitive market and an HHI of one represents a monopoly.9
Using propensity scores based on market and hospital characteristics, as well as trends in baseline rates of discharge to skilled nursing facilities and of readmissions, each hospital participating in BPCI was matched without replacement with up to three control hospitals whose log-odds propensity scores were within 0.515 of the log-odds propensity score for the BPCI hospital. We chose this difference of 0.515 to be consistent with the previous work in this area, which is based on the pooled standard deviation of our log-odds propensity scores multiplied by 0.2. Hospitals were excluded from consideration for the control group if they were not paid through the inpatient prospective-payment system (e.g. critical access hospitals) or if they participated in BPCI for any other condition, in case there was care redesign spillover.
We used Medicare inpatient files to identify index admissions for PCI (Medicare Severity Diagnosis-Related Groups [MS-DRGs] 246, 247, 248, 249, 250, 251, 273, 274) and CABG (MS-DRGs 231, 232, 233, 234, 235, 236) from January 1, 2013, through September 30, 2016 at participating hospitals and matched control hospitals. We included only beneficiaries who were continuously enrolled in Medicare Parts A and B during their episode of care and excluded those with Medicare eligibility because of end-stage renal disease. Claims contained demographic characteristics, principal discharge diagnoses, coexisting conditions, and service use.
For each index hospitalization, standardized Medicare-allowed payments for episodes of care (defined as the hospitalization plus 90 days after discharge) were calculated using 100% files for inpatient care, skilled nursing facility care, home health agency services, and durable medical equipment. These payments comprise approximately 85% of all payments including institutional post-acute care, which has been found to be most sensitive to the incentives in bundling.8, 10 Physician services and other outpatient care are not included as Medicare makes claims available for only a 20% sample of patients. Standardized payments specified by the Centers for Medicare and Medicaid Services (CMS) reflect a process that removes differences in payment according to a wage index, as well as differences with respect to payments for indirect costs of medical education, payments to disproportionate-share hospitals (i.e., hospitals providing a disproportionate share of care to Medicaid beneficiaries and uninsured patients), and other special payments. Total payments were Winsorized at the 95th percentile of national episode payments and adjusted for inflation to prices in 2015. Because fewer than 5% of hospitals chose 30- or 60-day episodes, we analyzed only 90-day episodes, which is consistent with prior evaluations.3–8, 11, 12
We considered the baseline period to be 9 months to 3 months (a 6-month period) before each hospital’s start date, with the intervention period starting immediately after the start date. The length of the intervention period ranged according to the enrollment date. For example, hospitals that started in January 2015 had a 2-year intervention period; those that started in April 2016 had only a 6-month intervention period. The mean intervention period was 16 months in our main analyses. Hospitals were included in this “intent-to-treat” analysis regardless of whether they elected to drop out of the program after enrollment.
Our primary outcome was the change in standardized allowed Medicare payments per episode. Secondary outcomes included changes in hospital case mix (based on the mean Chronic Conditions Warehouse score [a Medicare-provided comorbidity index that ranges from 0 to 27, with higher scores indicating more coexisting conditions]), discharge to post-acute care, per-hospital case volume, proportion of patients dually enrolled in Medicare and Medicaid (as an indicator of poverty), proportion of patients with disabling conditions, changes in the individual components of payment), and changes in length of stay, emergency department use, readmissions, and mortality.
Analyses
Hospital and market characteristics were compared between BPCI hospitals and matched control hospitals with the use of chi-square and t-tests, as appropriate. We used a difference-in-differences approach to examine changes in each outcome from the baseline period to the intervention period, and then to compare these changes between BPCI hospitals and controls. For each control hospital, the time periods were identical to those of the matched BPCI hospital. Analyses were run at the patient level, with each outcome in a separate model. Time was the primary predictor, coded as a binary variable for baseline versus intervention periods, along with BPCI status, and the interaction term between these indicators. The significance of the interaction term determined whether there had been a greater change in any outcome in patients at BPCI hospitals than in patients at control hospitals. Marginal models that use generalized estimating equations (PROC GLIMMIX in SAS) were used to account for correlation among patients within hospitals, and a match group fixed effect was included in all models to account for other unobserved differences. We risk-adjusted all models by including indicator variables for DRGs and individual Chronic Conditions Warehouse scores to control for coexisting conditions. For our primary outcome (total Medicare payments for each condition), we considered p<0.05 to be significant. Secondary endpoints and analyses should be considered exploratory.
RESULTS
Hospital Characteristics
A total of 42 hospitals participated in the program for PCI and 46 for CABG (Table 1). As compared with the sample of all eligible U.S. hospitals, BPCI hospitals for both PCI and CABG were more likely to be a teaching facility, have a larger number of beds, have higher median household incomes in their market and be located in the Northeast region. BPCI hospitals participating in PCI bundles were also more likely to be for-profit in ownership. Matched control hospitals were similar to BPCI hospitals on each of these elements, however. BPCI hospitals had higher mortality, higher readmission rates, and higher Medicare payments for PCI in 2013 than both controls and the broader all-hospital group. These parameters were more similar across BPCI, control, and all hospitals for CABG. However, slopes for the 15-month period before the intervention between BPCI hospitals and control hospitals were similar for Medicare payments and clinical outcomes for both BPCI and CABG, as these were a key part of the matching algorithm for our difference-in-differences approach (Supplemental Tables 1, 2, and 3).
Table 1.
Hospital Characteristics
| PCI | CABG | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BPCI | Matched Non-BPCI | P value | All Non-BPCI | p value | BPCI | Matched Non-BPCI | P value | All Non-BPCI | p value | |
| N of Hospitals | 42 | 115 | 1472 | 46 | 122 | 918 | ||||
| N conditions joined | 17.3 | 14.4 | ||||||||
| N of cases | 108.1 | 81.8 | 0.085 | 84.3 | 0.100 | 51.5 | 54.5 | 0.677 | 40.5 | 0.042 |
| Nonprofit | 64.3% | 62.6% | 0.847 | 69.5% | 0.470 | 84.8% | 78.7% | 0.374 | 69.6% | 0.027 |
| Public | 0.0% | 1.7% | 0.389 | 11.2% | 0.021 | 4.3% | 6.6% | 0.589 | 10.8% | 0.164 |
| For Profit | 35.7% | 35.7% | 0.994 | 19.3% | 0.008 | 10.9% | 14.8% | 0.513 | 19.6% | 0.140 |
| Urban Location | 100.0% | 100.0% | 1.000 | 99.1% | 0.540 | 100.0% | 100.0% | 1.000 | 99.5% | 0.616 |
| Teaching Hospital | 42.9% | 43.5% | 0.945 | 45.8% | 0.708 | 80.4% | 74.6% | 0.427 | 52.9% | <0.001 |
| DSH percent | 26.1% | 27.3% | 0.659 | 28.6% | 0.312 | 29.1% | 27.1% | 0.354 | 29.0% | 0.994 |
| Total Beds, Mean | 321 | 307 | 0.695 | 315 | 0.870 | 512 | 450 | 0.179 | 371 | <0.001 |
| Northeast | 21.4% | 20.0% | 0.844 | 14.1% | 0.182 | 43.5% | 38.5% | 0.558 | 11.7% | <0.001 |
| Midwest | 11.9% | 12.2% | 0.964 | 26.1% | 0.037 | 17.4% | 19.7% | 0.737 | 27.4% | 0.134 |
| South | 40.5% | 39.1% | 0.879 | 39.8% | 0.929 | 28.3% | 29.5% | 0.874 | 39.2% | 0.134 |
| West | 26.2% | 28.7% | 0.757 | 19.3% | 0.263 | 10.9% | 10.7% | 0.968 | 21.0% | 0.096 |
| Market Characteristics | ||||||||||
| Median Income | $59,557 | $58,854 | 0.819 | $53,312 | 0.003 | $55,728 | $55,716 | 0.996 | $52,688 | 0.102 |
| % Medicare Advantage | 27.7 | 28.1 | 0.858 | 27.9 | 0.931 | 29.1 | 28.5 | 0.795 | 29.0 | 0.973 |
| SNF Total Beds | 4945 | 6717 | 0.281 | 4529 | 0.723 | 7436 | 6311 | 0.458 | 5123 | 0.061 |
| Hospital Market Share | 0.41 | 0.37 | 0.484 | 0.45 | 0.575 | 0.46 | 0.48 | 0.683 | 0.46 | 0.961 |
| HHI | 0.15 | 0.13 | 0.401 | 0.13 | 0.267 | 0.14 | 0.14 | 0.838 | 0.13 | 0.640 |
| Pre-intervention | ||||||||||
| 90-day mortality | 7.1% | 4.1% | 0.059 | 3.91% | 0.006 | 2.2% | 4.7% | 0.237 | 4.2% | 0.216 |
| 90-day readmissions | 26.9% | 19.2% | 0.005 | 22.61% | 0.118 | 15.7% | 19.5% | 0.267 | 19.7% | 0.210 |
| 90-day payments | $25,574 | $22,332 | 0.003 | $22,685 | 0.006 | $48,346 | $49,425 | 0.663 | $48,273 | 0.972 |
All market characteristics are from 2013.
SNF – Skilled nursing facility; MA – Medicare Advantage; HHI - Herfindahl–Hirschman Index
Patient Selection
For PCI, there were 2,054 patients (episodes) in BPCI hospitals and 4,339 in control hospitals during the baseline period. During the intervention period for PCI, there were 3,799 patients (episodes) in BPCI hospitals and 8,657 in control hospitals (Table 2). There were no differential changes in procedural volume for PCI in BPCI hospitals versus matched control hospitals during the study period (decrease of 3.9 procedures per quarter versus decrease of 3.7 procedures per quarter, difference in differences [DID] 0.3, p=0.957, Table 2). There were also no differential changes over time for patients in BPCI hospitals undergoing PCI versus matched comparison hospitals with respect to demographics or measures of clinical risk.
Table 2.
Patient Selection for PCI
| BPCI | CONTROL | Differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Intervention | Difference | P value | Baseline | Intervention | Difference | P value | Differences | P value | |
| Episode, N | 2,054 | 3,799 | 4,339 | 8,657 | ||||||
| D/C per quarter | 24.2 | 20.3 | 3.9 | 0.316 | 24.6 | 20.9 | 3.7 | 0.210 | 0.3 | 0.957 |
| Age 64 and under | 10.9% | 12.5% | 1.7% | 0.206 | 10.0% | 10.7% | 0.7% | 0.205 | 1.0% | 0.488 |
| Age 65–79 | 60.4% | 59.4% | −1.1% | 0.470 | 59.8% | 59.8% | 0.0% | 0.983 | −1.1% | 0.526 |
| Age 80+ | 28.7% | 28.1% | −0.6% | 0.576 | 30.1% | 29.4% | −0.7% | 0.392 | 0.1% | 0.948 |
| Female | 39.6% | 39.4% | −0.2% | 0.861 | 39.2% | 39.3% | 0.1% | 0.905 | −0.3% | 0.833 |
| Medicaid | 19.2% | 19.8% | 0.5% | 0.730 | 16.7% | 16.8% | 0.1% | 0.865 | 0.4% | 0.816 |
| Disabled | 22.7% | 25.3% | 2.6% | 0.153 | 23.0% | 23.0% | −0.1% | 0.911 | 2.7% | 0.172 |
| Frail | 10.2% | 9.0% | −1.2% | 0.193 | 9.7% | 9.0% | −0.7% | 0.163 | −0.5% | 0.667 |
| Race | ||||||||||
| White | 87.1% | 85.0% | −2.1% | 0.104 | 88.5% | 88.7% | 0.2% | 0.750 | −2.3% | 0.107 |
| Black | 6.0% | 7.2% | 1.3% | 0.215 | 6.2% | 5.4% | −0.8% | 0.069 | 2.1% | 0.060 |
| Hispanic | 2.1% | 1.9% | −0.2% | 0.687 | 1.3% | 1.6% | 0.3% | 0.304 | −0.5% | 0.427 |
| Unknown/other | 4.7% | 5.8% | 1.1% | 0.184 | 3.9% | 4.3% | 0.4% | 0.325 | 0.7% | 0.442 |
| CCW mean | 7.69 | 7.89 | 0.20 | 0.008 | 7.73 | 7.87 | 0.14 | 0.015 | 0.06 | 0.500 |
| Billing level | ||||||||||
| DRG with MCC | 24.8% | 26.6% | 1.8% | 0.254 | 26.9% | 26.5% | −0.39% | 0.708 | 2.2% | 0.246 |
| DRG without CC | 75.2% | 73.4% | −1.8% | 0.254 | 73.1% | 73.5% | 0.39% | 0.708 | −2.2% | 0.246 |
| Admitted for MI | 51.8% | 60.6% | 8.9% | 0.004 | 51.9% | 63.3% | 11.34% | <0.001 | −2.5% | 0.467 |
| % of stays with outlier payments | 3.9% | 3.5% | −0.4% | 0.543 | 3.8% | 4.4% | 0.59% | 0.390 | −1.0% | 0.299 |
CCW – Chronic Conditions Warehouse; CABG – Coronary Artery Bypass Grafting
For CABG, there were 1,245 patients (episodes) in BPCI hospitals and 2,254 in control hospitals during the baseline period. During the intervention period for CABG, there were 3,898 patients (episodes) in BPCI hospitals and 7,744 in control hospitals (Table 3). For CABG, there were similarly no differential changes in procedural volume, and no significant differential changes in patient characteristics in BPCI hospitals vs. comparison hospitals with the exception that BPCI hospitals saw a greater increase over time in the proportion of patients who qualified for Medicare on the basis of a disability (Table 3).
Table 3.
Patient Selection for CABG
| BPCI | CONTROL | Differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Intervention | Difference | P value | Baseline | Intervention | Difference | P value | Differences | P value | |
| Episode, N | 1,245 | 3,898 | 2,254 | 7,744 | ||||||
| D/C per quarter | 13.0 | 13.2 | −0.2 | 0.925 | 13.0 | 13.3 | −0.3 | 0.867 | 0.1 | 0.981 |
| Age 64 and under | 8.0% | 9.5% | 1.5% | 0.076 | 8.5% | 8.7% | 0.1% | 0.838 | 1.3% | 0.216 |
| Age 65–79 | 76.5% | 73.3% | −3.2% | 0.031 | 75.3% | 75.0% | −0.3% | 0.793 | −2.9% | 0.108 |
| Age 80+ | 15.5% | 17.3% | 1.7% | 0.179 | 16.2% | 16.3% | 0.1% | 0.877 | 1.6% | 0.310 |
| Female | 28.8% | 28.3% | −0.5% | 0.742 | 26.4% | 25.1% | −1.3% | 0.148 | 0.8% | 0.630 |
| Medicaid | 15.0% | 15.4% | 0.4% | 0.776 | 11.7% | 11.4% | −0.4% | 0.639 | 0.8% | 0.632 |
| Disabled | 18.3% | 21.0% | 2.7% | 0.046 | 19.8% | 19.1% | −0.7% | 0.430 | 3.4% | 0.037 |
| Frail | 12.9% | 13.9% | 1.0% | 0.352 | 10.9% | 11.6% | 0.7% | 0.390 | 0.3% | 0.796 |
| Race | ||||||||||
| White | 85.1% | 87.9% | 2.8% | 0.078 | 91.1% | 89.9% | −1.2% | 0.110 | 4.0% | 0.023 |
| Black | 7.1% | 5.2% | −2.0% | 0.093 | 4.6% | 4.5% | −0.1% | 0.828 | −1.8% | 0.151 |
| Hispanic | 1.4% | 1.6% | 0.3% | 0.604 | 0.9% | 0.8% | −0.1% | 0.704 | 0.3% | 0.530 |
| Unknown/other | 6.5% | 5.4% | −1.1% | 0.257 | 3.4% | 4.8% | 1.4% | 0.004 | −2.5% | 0.021 |
| CCW mean | 7.75 | 7.94 | 0.19 | 0.001 | 7.59 | 7.80 | 0.21 | <0.001 | −0.02 | 0.786 |
| Billing level | ||||||||||
| DRG with MCC | 31.5% | 35.0% | 3.5% | 0.125 | 31.8% | 31.9% | 0.1% | 0.956 | 3.4% | 0.191 |
| DRG without CC | 68.5% | 65.0% | −3.5% | 0.125 | 68.2% | 68.1% | −0.1% | 0.956 | −3.4% | 0.191 |
| Admitted for MI | 24.3% | 27.1% | 2.8% | 0.082 | 23.9% | 25.8% | 1.88% | 0.034 | 0.9% | 0.609 |
| % of stays with outlier payments | 7.8% | 8.7% | 0.9% | 0.460 | 9.5% | 10.2% | 0.66% | 0.477 | 0.3% | 0.864 |
CCW – Chronic Conditions Warehouse; CABG – Coronary Artery Bypass Grafting
Medicare Payments per Episode
At baseline, the mean Medicare payment per episode in PCI for BPCI hospitals was $20,164, which increased during the intervention period (+$673; p= 0.048). Control hospitals for PCI had a mean Medicare payment of $19,955 per episode at baseline, which also increased during the intervention period (+$551; p=0.022, DID $122, p=0.768, Figure 1 and Table 4). Changes in individual components of Medicare payments, including payments for the index hospitalization, long-term care hospitals, readmissions, skilled nursing facilities, inpatient rehabilitation, and home health care, did not differ significantly between BPCI and control hospitals.
Figure 1: Total Medicare Payments, BPCI versus Control.
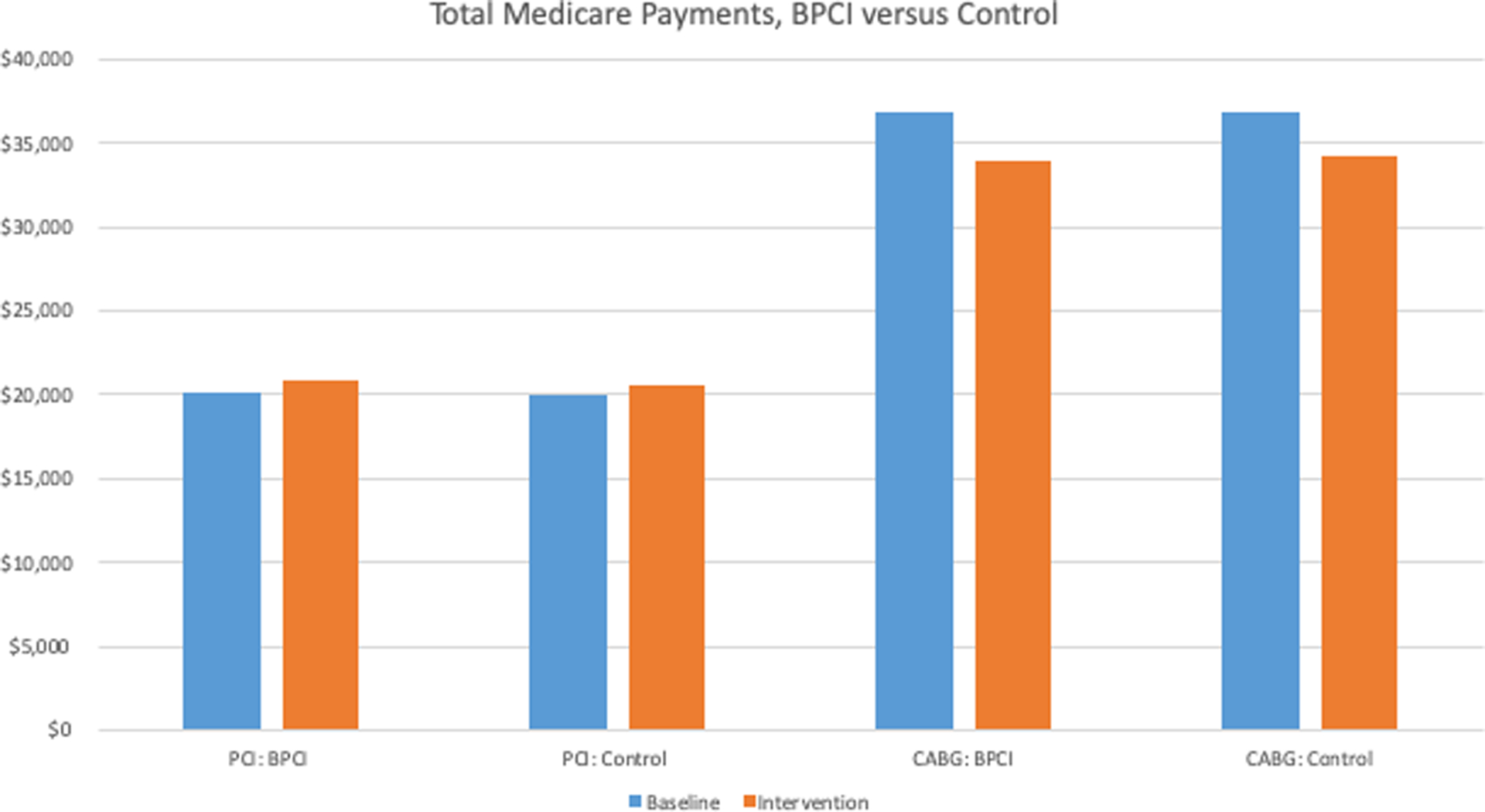
PCI – Percutaneous coronary intervention; CABG – Coronary Artery Bypass Grafting
Table 4.
Medicare Payments per Episode
| BPCI | CONTROL | Diff-in-Diff | P Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Intervention | Difference | P | Baseline | Intervention | Difference | P | |||
| PCI | ||||||||||
| Total payments | $20,164 | $20,836 | $673 | 0.048 | $19,955 | $20,506 | $551 | 0.022 | $122 | 0.768 |
| Index hospitalization | $13,825 | $14,067 | $242 | <0.001 | $13,864 | $14,074 | $210 | <0.001 | $32 | 0.619 |
| Readmission | $3,639 | $3,958 | $319 | 0.111 | $3,522 | $3,813 | $291 | 0.118 | $28 | 0.919 |
| SNF | $1,490 | $1,421 | −$69 | 0.612 | $1,395 | $1,415 | $20 | 0.856 | −$90 | 0.607 |
| IRF | $213 | $323 | $111 | 0.133 | $294 | $278 | −$16 | 0.797 | $127 | 0.192 |
| LTCH | $90 | $221 | $131 | 0.092 | $57 | $105 | $48 | 0.205 | $83 | 0.301 |
| Home health agency | $614 | $587 | −$26 | 0.498 | $557 | $534 | −$23 | 0.331 | −$3 | 0.950 |
| DME | $293 | $259 | −$34 | 0.296 | $266 | $287 | $20 | 0.225 | −$55 | 0.140 |
| CABG | ||||||||||
| Total payments | $36,925 | $34,007 | −$2,918 | <0.001 | $36,877 | $34,259 | −$2,618 | <0.001 | −$300 | 0.730 |
| Index hospitalization | $27,167 | $25,593 | −$1,574 | 0.021 | $27,248 | $25,505 | −$1,743 | <0.001 | $169 | 0.834 |
| Readmission | $3,325 | $3,114 | −$211 | 0.397 | $3,578 | $3,216 | −$362 | 0.034 | $151 | 0.623 |
| SNF | $3,355 | $2,584 | −$771 | 0.003 | $2,723 | $2,434 | −$288 | 0.030 | −$482 | 0.097 |
| IRF | $1,019 | $959 | −$60 | 0.742 | $1,201 | $1,212 | $11 | 0.923 | −$71 | 0.749 |
| LTCH | $182 | $92 | −$90 | 0.261 | $198 | $109 | −$90 | 0.195 | $0 | 0.997 |
| Home health agency | $1,702 | $1,500 | −$202 | 0.007 | $1,768 | $1,624 | −$144 | <0.001 | −$57 | 0.502 |
| DME | $174 | $163 | −$11 | 0.359 | $160 | $160 | $0 | 0.962 | −$11 | 0.480 |
SNF – Skilled nursing facility; IRF – Inpatient rehabilitation facility; DME – Durable medical equipment; PCI – Percutaneous coronary intervention; CABG – Coronary Artery Bypass Grafting
For CABG, the mean Medicare payment for BPCI hospitals was $36,925, which decreased to $34,007 during the intervention period (−$2,918, p<0.001). Control hospitals for CABG had a mean Medicare payment of $36,877, which also decreased during the intervention period (change −$2,618, p<0.001; DID, $300, p=0.730, Figure 1 and Table 4). The decline in payments was mostly driven by the index admission, however, there were significant reductions in payments for SNF as well as home health agencies in both BPCI and control hospitals. The decline in payments for index admissions was largely driven by a decline in both index and outlier payments (payments for exceedingly costly cases) among the costliest hospitalizations for both BPCI and control hospitals (Supplemental Table 4). Histograms of hospital-level changes in total payments are shown in Supplemental Figure 1.
Clinical Outcomes
In PCI, there were no differential changes between BPCI hospitals and controls in 30 and 90-day mortality, readmissions, length of stay, or discharge to institutional post-acute care. In BPCI hospitals, there were significant increases in both 30 and 90 day ED use in comparison to controls (Table 5).
Table 5.
Clinical Outcomes
| BPCI | CONTROL | Diff-in-Diff | P Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Intervention | Difference | P | Baseline | Intervention | Difference | P | |||
| PCI | ||||||||||
| Length of stay | 3.97 | 3.73 | −0.25 | 0.020 | 3.89 | 3.68 | −0.21 | 0.001 | −0.04 | 0.760 |
| ED Use | ||||||||||
| 30 Day | 18.6% | 23.5% | 4.9% | 0.038 | 22.0% | 19.3% | −2.8% | 0.107 | 7.7% | 0.010 |
| 90 Day | 29.3% | 34.0% | 4.6% | 0.128 | 32.0% | 29.4% | −2.6% | 0.192 | 7.2% | 0.045 |
| Readmission | ||||||||||
| 30 Day | 12.4% | 12.3% | −0.2% | 0.842 | 13.1% | 12.8% | −0.3% | 0.654 | 0.1% | 0.912 |
| 90 Day | 24.0% | 22.9% | −1.2% | 0.176 | 22.9% | 22.8% | −0.1% | 0.918 | −1.1% | 0.367 |
| Mortality | ||||||||||
| 30 Day | 2.4% | 3.2% | 0.8% | 0.103 | 3.4% | 3.3% | 0.0% | 0.955 | 0.8% | 0.170 |
| 90 Day | 4.1% | 4.8% | 0.7% | 0.173 | 5.5% | 5.2% | −0.4% | 0.333 | 1.1% | 0.099 |
| DC to inst PAC | 7.0% | 7.1% | 0.0% | 0.978 | 8.0% | 7.2% | −0.8% | 0.057 | 0.8% | 0.201 |
| CABG | ||||||||||
| Length of stay | 9.5 | 9.5 | −0.1 | 0.778 | 9.8 | 9.4 | −0.4 | 0.010 | 0.3 | 0.277 |
| ED Use | ||||||||||
| 30 Day | 18.0% | 14.2% | −3.8% | 0.134 | 10.8% | 16.5% | 5.7% | <0.001 | −9.5% | 0.001 |
| 90 Day | 28.3% | 22.8% | −5.6% | 0.091 | 19.9% | 26.4% | 6.6% | 0.001 | −12.1% | 0.002 |
| Readmission | ||||||||||
| 30 Day | 12.8% | 10.8% | −2.0% | 0.098 | 13.3% | 11.2% | −2.1% | 0.004 | 0.1% | 0.939 |
| 90 Day | 19.9% | 18.2% | −1.7% | 0.166 | 19.9% | 17.8% | −2.1% | 0.007 | 0.4% | 0.785 |
| Mortality | ||||||||||
| 30 Day | 2.1% | 1.8% | −0.3% | 0.496 | 2.3% | 1.7% | −0.6% | 0.045 | 0.2% | 0.691 |
| 90 Day | 3.0% | 2.7% | −0.3% | 0.643 | 3.0% | 2.3% | −0.6% | 0.055 | 0.4% | 0.554 |
| DC to inst PAC | 34.5% | 29.7% | −4.8% | 0.008 | 30.8% | 29.2% | −1.7% | 0.082 | −3.1% | 0.100 |
PCI – Percutaneous coronary intervention; CABG – Coronary Artery Bypass Grafting; ED – Emergency Department; DC to inst PAC – Discharge to institutional post-acute care
In CABG, there were no significant differential changes between BPCI hospitals and controls in 30 and 90-day mortality, readmissions, or length of stay (Table 5). There were differential reductions in ED use over time, with BPCI hospitals decreasing 30- and 90-day ED use more than controls.
DISCUSSION
We found that hospital participation in BPCI for PCI and CABG was not associated with significant changes in total or component Medicare payments, patient characteristics, or outcomes such as readmission, mortality or length of stay. In CABG, BPCI participation was associated with reductions in ED use, while after PCI, BPCI participation was associated with increases in ED use. Prior studies have shown that hospital participation in BPCI for any of the 5 most common medical conditions requiring hospitalization among Medicare patients was not associated with changes in payments or in clinical outcomes,8 while many have found reduced payments, without adverse outcomes, in hospitals participating in BPCI for joint replacement.3–7, 11 We had hypothesized that since both PCI and CABG are procedural, they might follow a pattern more like joint replacement, but we did not find this to be the case.
One potential reason for the differences between total joint replacement and cardiac procedures may be due to the nature of the procedures themselves. In most cases, joint replacement is an elective surgery. It is possible that planned, elective procedures or procedures with highly variable use of costly post-acute resources, such as rehab services, may be more amenable to cost reductions under episode-based payment models than urgent or emergent procedures such as PCI or CABG. For instance, in joint replacement, up to 92% of the variation in post-discharge spending is due to differences in PAC spending. Unsurprisingly, the reduction in payments with joint replacement in the BPCI program was largely driven by lower utilization of PAC.10 This is in contrast to inpatient PCI, which contains a large proportion of unplanned procedures that occur in the setting of an acute coronary syndrome (55% of our cohort). In this population, it has previously been found that readmissions account for the majority of hospital variation in payments.13, 14 Despite tremendous resources expended under the Hospital Readmissions Reduction Program, it has struggled to meaningfully impact readmission rates.15 Accordingly, it was not surprising to us that we failed to see a change in readmissions among BPCI participating hospitals. Also in comparison with total joint replacement, where the index hospitalization comprises around 48–50% of total payments, in both PCI and CABG, the index hospitalization accounted for at least 67% of total payments. As payments for inpatient stays are predominantly based on a standard DRG scale, it is possible there is less ability to reduce payments for this phase of care, rather than post-acute care (e.g. readmissions, rehabilitation services, etc.), given the variability in the use of these services.
Why BPCI participation was associated with increased ED use after PCI but the opposite after CABG is not readily apparent. There were no other consistent signals of harm for BPCI participation for PCI. The baseline ED use during the run-in period was lower in BPCI hospitals participating for PCI, so it is possible this amplified the differences observed between participating and control hospitals during the intervention period. For CABG, there were similar observations in the control hospitals, which may have led to the opposite result we observed.
Notably, we observed a significant decline in total Medicare payments in CABG for both BPCI and control hospitals. This decline was largely driven by a reduction in index and outlier payments among the costliest patients undergoing CABG for both BPCI and control hospitals during the study period. The factors driving this decline are unclear, but may be related to care improvements in both groups leading to reductions in complications and their associated extended hospitalizations, or in differential patient selection in ways that were not picked up in our models. There were also significant declines in payments for skilled nursing facilities for both BPCI and control hospitals after CABG. This is consistent with the decline in discharge to PAC we observed for BPCI participating hospitals. This is also in line with prior data which observed similar findings after total joint replacement, suggesting that hospitals may be changing behavior in regard to SNF utilization after a variety of surgeries.7
This study should be interpreted in the context of other work on bundled payments for cardiac procedures. One prior study looked at differences between hospitals that joined BPCI for cardiac bundles more broadly versus those that did not (finding that participants were higher-volume and provided higher-level cardiac services like PCI and cardiac transplant),16 but did not examine changes in costs or outcomes under the program. As noted above, federal reports from the Lewin Group, produced under contract with CMS, have been released annually, and examine all conditions within the program;3–6 our findings are qualitatively similar to those reported in their Year 5 report, in that they also find no significant differential change in 90-day episode payments made by Medicare for BPCI hospitals compared to controls for either condition. Minor differences in matching approaches and outpatient data availability likely explain quantitative differences. The Lewin report differs from our findings in some of the secondary outcomes, including mortality; they note an increase in CABG mortality for BPCI hospitals relative to controls, however, this finding did not remain robust after further sensitivity analysis using a matching strategy more similar to ours.3
Our study has a number of limitations. First, BPCI is a voluntary program, so generalizability to mandatory models is uncertain. Second, as with any administrative data research, there are unmeasured variables and confounders, which in this study, could have biased the results toward the null. Third, it is important to remember that this is a study of inpatients only, and so does not apply to outpatient PCI, which is becoming increasingly common. Fourth, we used a relatively short baseline period due to data availability, during which hospitals were likely aware they would soon be entering the bundled payments program and have already been preparing to redesign care; this could have biased us to the null. Fifth, we had a relatively short follow-up period and longer follow-up may be necessary to see if differences would develop between intervention and control hospitals.17 Sixth, there were a relatively small number of hospitals that participated in BPCI for PCI and CABG, and it is possible this biased us toward the null as well. Seventh, we were unable to control for whether hospitals were concurrently participating in other alternative payment models including bundled payment programs in the private setting. Eighth, we had no data on spending targets, penalties, or bonuses under the program. Therefore, our findings represent the effect of the program on Medicare payments, but we cannot estimate its impact on financial performance, nor whether hospitals that received penalties or bonuses had differential changes in outcomes over time.
In summary, we found that participation in episode-based payment for PCI and CABG was not associated with changes in patient selection, payments, LOS, or improved outcomes such as mortality or readmission. Bundled payments have demonstrated an ability to reduce payments for joint replacement, but our findings suggest their efficacy may not generalize across all procedures. As BPCI-Advanced is rolled out for a number of inpatient and outpatient diagnoses and procedures, continued monitoring will be important to ensure that the program is effective and does not have unintended consequences.
Supplementary Material
What is known:
The Bundled Payments for Care Improvement (BPCI) initiative has shown mixed results, with success in reducing costs for joint replacement, but not for common medical conditions including myocardial infarction and heart failure.
What this study adds:
For PCI episodes, payments increased at both BPCI and control hospitals during the intervention period, such that there was no significant differential change between the groups.
For CABG episodes, payments at both BPCI and control hospitals decreased during the intervention period, again indicating no differential change between the groups.
For both PCI and CABG, BPCI participation was not associated with differential changes in clinical outcomes such as mortality or readmissions.
Bundled payments may not be as successful for cardiac procedures as they have been for orthopedic ones.
SOURCES OF FUNDING
The National Heart, Lung, and Blood Institute (R01HL143421).
DISCLOSURES
Dr. Joynt Maddox receives research support from the National Heart, Lung, and Blood Institute (R01HL143421), National Institute on Aging (R01AG060935), and Commonwealth Fund, and previously did contract work for the US Department of Health and Human Services. Dr. Orav does contract work for the US Department of Health and Human Services. The other authors have no disclosures.
References
- 1.Centers for Medicare and Medicaid Services. Bundled Payments for Care Improvement (BPCI) Initiative: General Information. http://innovation.cms.gov/initiatives/bundled-payments/. Accessed May 8, 2017.
- 2.Center for Medicare & Medicaid Innovation. BPCI Advanced. 2017. https://innovation.cms.gov/initiatives/bpci-advanced. Accessed January 9, 2018.
- 3.Dummit L, Marrufo G, Marshall J, Ackerman T, Bergman S, Bradley A, Cherry R, Chung A, Cintina I, Cooper D, Dennen S, Fannoun A, Gerding G, Gregory D, Hyland M, Johnson A, Joy S, Kahn J, Kelly J, Lampert A, Lopez de Nava K, Maughan B, Melin C, Negrusa S, Sheahan W, Somers J, Subramanian A, Swanson K, Tan E, Than K-S, Wiedner P, Williams A, Yang G, Zhang D, Farley D, Breunig I, Hassol A, Gu Q, McClellan S, Trombley M, LaRocca C, Blystone B and Kummet C. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 5 Evaluation & Monitoring Annual Report. 2018.
- 4.Dummit L, Marrufo G, Marshall J, Ackerman T, Bergman S, Bradley A, Cherry R, Cintina I, Cooper D, Dennen S, Dishuck P, Fannoun A, Hyland M, Gerding G, Gregory D, Griffin C, Johnson A, Joy S, Kahn J, Kelly J, Lampert A, Lopez de Nava K, Maughan B, Melin C, Negrusa S, Somers J, Strubler D, Swanson K, Tan E, Than K-S, Wiedner P, Williams A, Yang G, Zhang D, Farley D, Breunig I, Hassol A, Gu Q, McClellan S, Trombley M, LaRocca C, Blystone B and Kummet C. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 4 Evaluation & Monitoring Annual Report. 2018.
- 5.Dummit L, Marrufo G, Marshall J, Maughan B, Ackerman T, Bergman S, Bradley A, Cherry R, Cintina I, Cooper D, Dennen S, Dishuck P, Fannoun A, Hyland M, Gerding G, Gregory D, Griffin C, Johnson A, Joy S, Kahn J, Kelly J, Lampert A, Lopez de Nava K, Melin C, Negrusa S, Somers J, Strubler D, Swanson K, Tan E, Than K-S, Wiedner P, Williams A, Yang G, Zezza M, Zhang D, Farley D, Breunig I, Hassol A, Gu Q, McClellan S, Trombley M, LaRocca C, Kirsch L, Kummet C and Roozeboom M. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 3 Evaluation & Monitoring Annual Report. 2017.
- 6.Dummit L, Marrufo G, Marshall J, Tan E, Bradley A, Hall C, Lee Y, Kelly J, Hyland M, Cherry R, Melin C, Maughan B, Fannoun A, Johnson A, Zurbey G, Joy S, Tucker S, Negrusa S, Davidson M, Alesci N, Glenn I, Gregory D, Smith L, Zhang D, Lampert A, Morgan N, Gordon G, Steier J, Farley D, Gu Q, Breunig I, Trombley M, Hassol A, LaRocca C and Kirsch L. CMS Bundled Payments for Care Improvement Initiative Models 2–4: Year 2 Evaluation & Monitoring Annual Report. 2016.
- 7.Dummit LA, Kahvecioglu D, Marrufo G, Rajkumar R, Marshall J, Tan E, Press MJ, Flood S, Muldoon LD, Gu Q, Hassol A, Bott DM, Bassano A and Conway PH. Association Between Hospital Participation in a Medicare Bundled Payment Initiative and Payments and Quality Outcomes for Lower Extremity Joint Replacement Episodes. JAMA. 2016;316:1267–78. [DOI] [PubMed] [Google Scholar]
- 8.Joynt Maddox KE, Orav EJ, Zheng J and Epstein AM. Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018;379:260–269. [DOI] [PubMed] [Google Scholar]
- 9.Antitrust Division of the United States Department of Justice. Herfindahl-Hirschman Index. 2015. https://www.justice.gov/atr/herfindahl-hirschman-index. Accessed May 2, 2018.
- 10.Barnett ML, Wilcock A, McWilliams JM, Epstein AM, Joynt Maddox KE, Orav EJ, Grabowski DC and Mehrotra A. Two-Year Evaluation of Mandatory Bundled Payments for Joint Replacement. N Engl J Med. 2019;380:252–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joynt Maddox KE, Orav EJ, Zheng J and Epstein AM. Post-Acute Care After Joint Replacement in Medicare’s Bundled Payments for Care Improvement Initiative. Journal of the American Geriatrics Society. 2019;67:1027–1035. [DOI] [PubMed] [Google Scholar]
- 12.Maughan BC, Kahvecioglu DC, Marrufo G, Gerding GM, Dennen S, Marshall JK, Cooper DM, Kummet CM and Dummit LA. Medicare’s Bundled Payments For Care Improvement Initiative Maintained Quality Of Care For Vulnerable Patients. Health Aff (Millwood). 2019;38:561–568. [DOI] [PubMed] [Google Scholar]
- 13.Sukul D, Seth M, Dupree JM, Syrjamaki JD, Ryan AM, Nallamothu BK and Gurm HS. Drivers of Variation in 90-Day Episode Payments After Percutaneous Coronary Intervention. Circulation Cardiovascular interventions. 2019;12:e006928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huckfeldt PJ, Mehrotra A and Hussey PS. The Relative Importance of Post-Acute Care and Readmissions for Post-Discharge Spending. Health Serv Res. 2016;51:1919–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ody C, Msall L, Dafny LS, Grabowski DC and Cutler DM. Decreases In Readmissions Credited To Medicare’s Program To Reduce Hospital Readmissions Have Been Overstated. Health Aff (Millwood). 2019;38:36–43. [DOI] [PubMed] [Google Scholar]
- 16.Oseran AS, Howard SE and Blumenthal DM. Factors Associated With Participation in Cardiac Episode Payments Included in Medicare’s Bundled Payments for Care Improvement Initiative. JAMA Cardiol. 2018;3:761–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dundon JM, Bosco J, Slover J, Yu S, Sayeed Y and Iorio R. Improvement in Total Joint Replacement Quality Metrics: Year One Versus Year Three of the Bundled Payments for Care Improvement Initiative. J Bone Joint Surg Am. 2016;98:1949–1953. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


