Abstract
Background
Preeclampsia and gestational hypertension are hypertensive disorders of pregnancy (HDP) that identify an increased risk of developing chronic hypertension and cardiovascular disease later in life. Postpartum follow‐up may facilitate early screening and treatment of cardiovascular risk factors. Our objective is to describe patterns of postpartum visits with primary care and women's health providers (eg, family medicine and obstetrics) among women with and without HDP in a nationally representative sample of commercially insured women.
Methods and Results
We conducted a retrospective cohort study using insurance claims from a US health insurance database to describe patterns in office visits in the 6 months after delivery. We identified 566 059 women with completed pregnancies between 2005 and 2014. At 6 months, 13% of women with normotensive pregnancies, 18% with HDP, and 23% with chronic hypertension had primary care visits (P<0.0001 for comparing HDP and chronic hypertension groups with control participants). Only 58% of women with HDP had 6‐month follow‐up with any continuity provider compared with 47% of women without hypertension (P<0.0001). In multivariable analysis, women with severe preeclampsia were 16% more likely to have postpartum continuity follow‐up (adjusted odds ratio, 1.16; 95% CI, 1.2–1.21). Factors associated with a lower likelihood of any follow‐up included age ≥30 years, Black race, Hispanic ethnicity, and having multiple gestations.
Conclusions
Rates of continuity care follow‐up after a pregnancy complicated by hypertension were low. This represents a substantial missed opportunity to provide cardiovascular risk screening and management to women at increased risk of future cardiovascular disease.
Keywords: hypertension, preeclampsia, primary prevention, women's health
Subject Categories: Pregnancy, Women, Primary Prevention
Nonstandard Abbreviations and Acronyms
- AHA
American Heart Association
- CPT
Current Procedural Terminology
- HDP
hypertensive disorders of pregnancy
- ICD-9
International Classification of Diseases, Ninth Revision
Clinical Perspective
What Is New?
Women with hypertensive disorders of pregnancy are more likely than women with normotensive pregnancies to follow‐up with a primary care or women's health provider within 6 months after delivery; however, follow‐up rates remain extremely low.
Patient characteristics associated with lower rates of 6-month follow‐up include age ≥30 years, Black race, Hispanic ethnicity, and multiple gestations.
What Are the Clinical Implications?
Improving postpartum care transitions, especially for women with pregnancy complications, may facilitate early cardiovascular risk screening and management for women at increased risk of future cardiovascular disease.
Hypertension is a common medical complication of pregnancy that affects >10% of all pregnancies. 1 Hypertensive disorders of pregnancy (HDP), including gestational hypertension and preeclampsia, are important contributors to maternal morbidity and mortality. In the immediate postpartum period, hypertensive disorders confer a greater risk of hypertensive crisis and stroke. 2 , 3 , 4 In the year after delivery, women with preeclampsia and gestational hypertension are at 12‐ to 25‐fold greater risk of developing chronic hypertension and remain at greater risk of ischemic heart disease, stroke, and heart failure later in life, especially among women with severe preterm preeclampsia. 5 , 6 , 7 , 8
The American Heart Association (AHA) recognizes HDP as a major risk factor for cardiovascular and cerebrovascular disease in women, and the 2019 AHA and American College of Cardiology Guideline on the Primary Prevention of Cardiovascular Disease identifies preeclampsia as a risk‐enhancing factor. 9 , 10 , 11 Pregnancy serves as a natural “stress test” to identify at‐risk women who may benefit from risk‐factor screening and lifestyle counseling earlier in life. 10 , 11 Nevertheless, most women are unaware of the association between HDP and future cardiovascular risk, which represents an unmet need for education and primary prevention. 12 , 13 Increasing attention has been given to the “fourth trimester,” the 3 months after delivery, during which time there is a high need for coordinated health care, including cardiovascular prevention efforts, to prevent future maternal complications and to improve long‐term cardiovascular health. 14 , 15
The postpartum obstetric care visit, historically scheduled within 6 weeks of delivery, is currently recommended to occur within 3 weeks of delivery for all women with the transition to well‐woman care occurring within 12 weeks postpartum. 14 This visit represents an opportunity to provide cardiovascular preventive care and to transition to a primary care provider for ongoing follow‐up. Despite this, ≈40% of women do not attend the recommended postpartum visit. 1 , 14 The transition to primary care has been shown to be suboptimal in selected populations, ranging from 13% among a nationwide sample of women with gestational diabetes mellitus to 50% among women with commercial insurance living in Maryland. 16 , 17 Rates of primary care follow‐up among women with hypertensive disorders, who may particularly benefit from cardiovascular preventive care, have not been well studied in a nationally representative population.
Ambulatory care visits with a women's health provider (eg, obstetrics or family medicine) or primary care provider in the months following delivery do not ensure that cardiovascular preventive care is provided; understanding patterns of care can provide insight into opportunities to improve counseling for those at risk. Our objective is to describe patterns in postpartum continuity care follow‐up and factors associated with follow‐up among women with and without HDP who have commercial insurance. We hypothesized that women with hypertensive disorders would have higher rates of follow‐up but that overall rates would be suboptimal, highlighting the need for improved delivery of cardiovascular risk screening and treatment.
METHODS
The data that support the findings of this study are not publicly available at this time. We conducted a retrospective cohort study of women to evaluate rates of postpartum continuity care follow‐up in the 6 months after a hospital discharge for delivery, using health insurance claims data. Because all women are recommended to follow up with their women's health provider shortly after delivery, we evaluated follow‐up with women's health (eg, obstetrics or family medicine) and primary care providers. This study was deemed exempt by the University of Pennsylvania's institutional review board.
Cohort
Our study cohort consisted of commercially insured women whose medical and prescription drug insurance claims are included in the OptumInsight Clinformatics Data Mart, a US commercial health insurance database that includes >15 million commercially insured individuals annually and located in all 50 states. Using administrative claims from January 2005 through September 2014, we included patients aged 12 to 55 years with a delivery indicated by Current Procedural Terminology (CPT) and/or International Classification of Diseases, Ninth Revision, (ICD-9) procedure codes reported on medical service claims. 18 Date of last menstrual period (LMP) was calculated using a validated algorithm based on whether the delivery was coded as preterm. 19 We required patients to have continuous enrollment in the database for the 180 days before start of pregnancy, as defined by the date of last menstrual period, to be able to evaluate clinical data before pregnancy. Women were required to be enrolled through 180 days after the delivery date for a total time period of ≈600 days for a full‐term delivery. We restricted our cohort to the first pregnancy during this time period.
Using ICD-9, Clinical Modification (ICD-9-CM) codes, we stratified our cohort into 3 exposure groups: (1) patients with no history of a hypertensive disorder either before or during pregnancy (normotensive control participants); (2) patients who developed HDP, including gestational hypertension, preeclampsia or eclampsia (with or without severe features), and chronic hypertension with superimposed preeclampsia; and (3) patients with chronic hypertension diagnosed before pregnancy but no HDP (Table S1 for CPT and ICD codes). 20 Patients with HDP were analyzed regardless of chronic hypertension status, given the possibility that patients with chronic hypertension may have been misclassified as not having chronic hypertension as a result of limited clinical encounters before pregnancy, in addition to inappropriate coding of chronic hypertension among women being worked up for HDP. Because patients with a diagnosis of chronic hypertension before pregnancy may be more likely to have an established primary care provider, we analyzed patients with chronic hypertension separately from patients without chronic hypertension (normotensive control participants).
Covariates
We evaluated baseline patient characteristics in the 6‐month period before the start of pregnancy (ie, before the last menstrual period date) and during pregnancy (ie, last menstrual period date to delivery date). Demographic variables were collected from the enrollment files at time of delivery. Race/ethnicity and educational attainment data were provided by Optum. We assessed clinical comorbidities (eg, diabetes mellitus, lipid disorder, heart failure) using ICD‐9 diagnosis codes at any time before or during pregnancy with the exception of gestational diabetes mellitus, which was assessed only during pregnancy. Obstetrics variables were assessed with CPT and ICD‐9 procedure codes (eg, cesarean delivery) and diagnosis codes (eg, preterm delivery and multiple gestations). We assessed medication use using the National Drug Code reported on pharmacy claims.
Outcomes
The primary outcome was the proportion of women with an office visit in the 6 months (180 days) after hospital discharge for delivery with a women's health provider, primary care provider, or both. Patients were censored after the first visit within a provider type (women's health and primary care). Women's health providers provide prenatal and postpartum care and include family medicine providers, obstetricians, nurse midwives, and maternal fetal medicine specialists. We included cardiologists with primary care providers because some women with HDP will be referred to cardiology postpartum. We assessed visits using a previously published algorithm with modifications as needed for our data set. 16 Visits were identified by physician claims having an eligible CPT code (eg, ambulatory provider visit) with a corresponding provider specialty code.
Statistical Analysis
We used χ2 tests to assess the proportion of women who attended follow‐up visits among those with HDP and those with chronic hypertension compared with those with normotensive pregnancies. Multivariable logistic regression models were conducted in the entire cohort. We included variables that could plausibly affect ambulatory follow‐up, including demographics (age, race, education level, geographical region), obstetrics history (cesarean delivery, preterm delivery, multiple gestations, gestational diabetes mellitus), hypertensive disorders (gestational hypertension, nonsevere and severe preeclampsia, and chronic hypertension), medical comorbidities (diabetes mellitus, lipid disorder, coronary artery disease, kidney disease, and heart failure), and healthcare utilization (emergency department visits before delivery, blood pressure medication use before pregnancy). We chose a 6‐month follow‐up period for our primary analysis because we hypothesized that visits occurring ≥6 months after delivery are less likely to reflect pregnancy‐related complications.
Sensitivity Analysis
Given our anticipated low follow‐up rates during this time frame, we conducted a sensitivity analysis among patients with continuous insurance enrollment for 12 months postpartum and calculated follow‐up rates within 6 and 12 months after delivery.
RESULTS
Baseline Characteristics
We identified 566 059 completed pregnancies, including 483 562 (85%) normotensive women, 63 216 (11%) women with HDP, and 19 281 (4%) women with chronic hypertension alone (Figure 1). This represents an estimated 1.3% of all deliveries in the United States during the 10‐year study period. Among the HDP group, 23% were documented as having severe preeclampsia or eclampsia. Baseline demographics are presented in Table 1. Women with normotensive pregnancy were of similar age to those with HDP (31.2 years) but younger than women with chronic hypertension (31.2 versus 32.5 years, P<0.0001). Many statistically significant demographic and clinical differences were present among the 3 cohorts. Compared with normotensive women, women with HDP and chronic hypertension were more likely to be Black and to live in the southern United States. Women with HDP or chronic hypertension had significantly higher rates of cesarean section and preterm birth compared with normotensive women. Women with HDP and chronic hypertension were more likely to have diabetes mellitus, lipid disorder, coronary artery disease, kidney disease, or heart failure compared with normotensive women.
Figure 1.
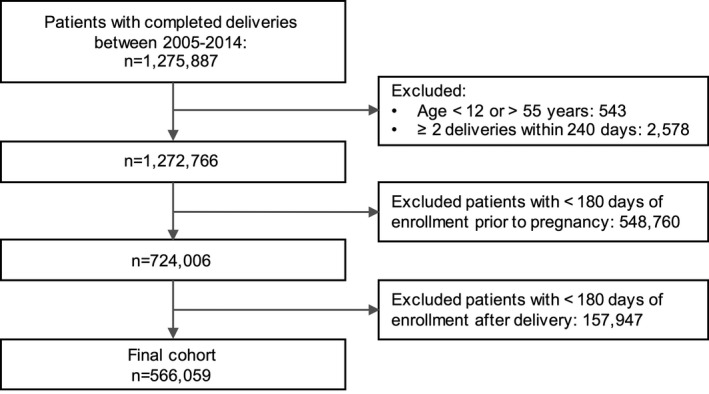
CONSORT diagram of patients included in the analysis.
Table 1.
Baseline Characteristics of Women With Completed Pregnancies According to Hypertensive Status
|
Normotensive Control Participants (n=483 562) |
HDP (n=63 216) |
Chronic Hypertension (n=19 281) |
|
|---|---|---|---|
| Demographics | |||
| Age, mean (SD), y | 31.2 (5.3) | 31.2 (5.7)*, * | 32.5 (5.5) |
| Age <30 y | 170 582 (35) | 23 572 (37) | 5568 (29) |
| Race/ethnicity | |||
| White | 313 392 (65) | 43 065 (68) | 11 942 (62) |
| Black | 38 844 (8) | 7172 (11) | 2888 (15) |
| Hispanic | 61 792 (13) | 7074 (11) | 2445 (13) |
| Other | 69 534 (14) | 5905 (9.3) | 2006 (10) |
| HS graduate or less | 100 299 (21) | 16 109 (26) | 5349 (28) |
| Geographic region | |||
| Midwest | 127 674 (26) | 16 365 (26) | 4332 (23) |
| Northeast | 50 000 (10) | 5756 (9.1) | 2444 (13) |
| South | 203 041 (42) | 30 692 (49) | 9670 (50) |
| West | 101 813 (21) | 10 339 (16) | 2810 (15) |
| Obstetrics history | |||
| Cesarean delivery | 155 692 (32) | 31 298 (50) | 8813 (46) |
| Preterm delivery | 93 717 (19) | 19 930 (32) | 4906 (25) |
| Multiple gestations | 10 421 (2.2) | 3563 (5.6) | 570 (3.0) |
| Gestational diabetes mellitus | 62 961 (13) | 11 884 (19) | 3541 (18) |
| Medical comorbidities | |||
| Diabetes mellitus | 15 906 (3.3) | 5451 (8.6) | 2568 (13) |
| Lipid disorder | 15 149 (3.1) | 3898 (6.2) | 3083 (16) |
| Coronary artery disease | 966 (0.2) | 267 (0.4) | 305 (1.6) |
| Kidney disease | 513 (0.1) | 419 (0.7) | 218 (1.1) |
| Heart failure | 424 (0.1) | 249 (0.4) | 156 (0.8) |
| Healthcare utilization | |||
| Prior ED visit † , † | 0.4 (0.9) | 0.6 (1.2) | 0.7 (1.4) |
| Prior BP medication use‡ | 4668 (1) | 5742 (9.1) | 4550 (24) |
All values represent number (percentage) except as indicated. All comparisons of HDP and control participants and chronic hypertension and control participants are significant at P<0.0001, except as indicated. BP indicates blood pressure; ED, emergency department; HDP, hypertensive disorders of pregnancy; and HS, high school.
P>0.05.
Before delivery.
Before pregnancy.
Ambulatory Care Follow‐up After Delivery
Postpartum follow‐up rates with primary care providers within 6 months of delivery were low in all groups but higher in women with HDP (18%) and chronic hypertension (22%) compared with normotensive women (13%; P<0.0001 for both comparisons to control participants), as shown in Table 2. Only 40% of women had a follow‐up visit with a women's health provider within 6 months of delivery, including 48% of women with HDP and chronic hypertension and 39% of normotensive women (P<0.0001 for both comparisons to control participants). As shown in Figure 2, a minority of women had postpartum follow‐up with both primary care and women's health providers within 6 months of delivery (<10% in all groups). Among women who followed up with a women's health provider within 6 months, only 12% of normotensive women, 17% of women with HDP, and 20% of women with chronic hypertension also followed up with a primary care provider.
Table 2.
Postpartum Ambulatory Care Follow‐up Within 6 Months of Delivery Among Women With and Without Hypertensive Disorders
| Provider Type |
Normotensive Control Participants (n=483 562) |
HDP (n=63 216) |
P Value* |
Chronic Hypertension (n=19 281) |
P Value* |
|---|---|---|---|---|---|
| Primary care | 60 447 (13) | 11 463 (18) | <0.0001 | 4218 (22) | <0.0001 |
| Women's health | 188 161 (39) | 30 612 (48) | <0.0001 | 9244 (48) | <0.0001 |
| Any provider | 225 217 (47) | 36 789 (58) | <0.0001 | 11 620 (60) | <0.0001 |
All values represent number (percentage). HDP indicates hypertensive disorders of pregnancy.
Compared with normotensive controls.
Figure 2. Postpartum ambulatory care follow‐up within 6 months after delivery according to provider type.
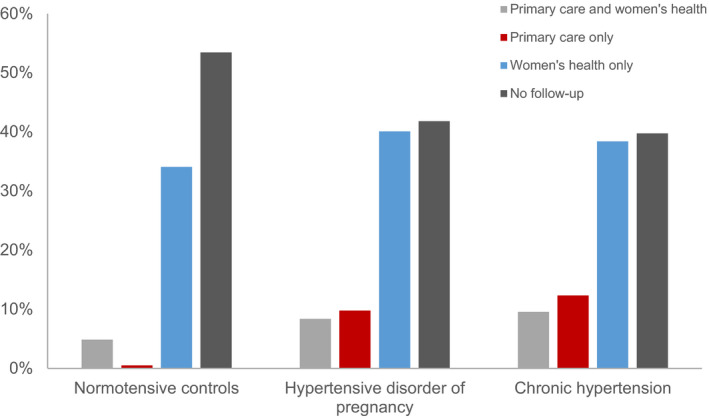
By 6 months after delivery, 53% of normotensive women, 42% of women with HDP, and 40% of women with chronic hypertension had no ambulatory care visits with a continuity provider (P<0.0001 for both comparisons to control participants). Among the 464 003 women (82% of the original cohort) with continuous enrollment through 12 months postpartum, follow‐up rates at 12 months with primary care and women's health providers improved but remained suboptimal: 35% of normotensive women, 26% of women with HDP, and 23% of women with chronic hypertension had no postpartum follow‐up with any continuity provider (P<0.0001 for both comparisons to control participants; see Table S2).
Characteristics Associated With Postpartum Follow‐Up
Hypertensive disorders were associated with a small but significantly increased likelihood of follow‐up with primary care and women's health providers in age‐adjusted models and adjusting for demographics, clinical conditions, and healthcare utilization before delivery in multivariable analysis (Table 3) compared with women without hypertension. Specifically, in multivariable models, women with gestational hypertension (odds ratio [OR], 1.14; 95% CI, 1.12–1.17), nonsevere preeclampsia (OR, 1.16; 95% CI, 1.13–1.19), severe preeclampsia (OR, 1.16; 95% CI, 1.12–1.21), or chronic hypertension (OR, 1.23; 95% CI, 1.2–1.26) were more likely to follow up with any provider within 6 months of delivery than women without those conditions.
Table 3.
Effect of HDP and Chronic Hypertension on Postpartum Ambulatory Care Follow‐up Within 6 Months After Delivery According to Provider Type
| Primary Care | Women's Health | Any Provider | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Hypertensive disorders | ||||||
| Gestational hypertension | ||||||
| Model 1 | 1.09 (1.06–1.13) | <0.0001 | 1.18 (1.16–1.21) | <0.0001 | 1.19 (1.16–1.22) | <0.0001 |
| Model 2 | 1.1 (1.07–1.13) | <0.0001 | 1.13 (1.11–1.16) | <0.0001 | 1.14 (1.12–1.17) | <0.0001 |
| Nonsevere preeclampsia | ||||||
| Model 1 | 1.1 (1.06–1.14) | <0.0001 | 1.2 (1.16–1.23) | <0.0001 | 1.2 (1.16–1.23) | <0.0001 |
| Model 2 | 1.09 (1.05–1.13) | <0.0001 | 1.16 (1.13–1.19) | <0.0001 | 1.16 (1.13–1.19) | <0.0001 |
| Severe preeclampsia | ||||||
| Model 1 | 1.29 (1.24–1.35) | <0.0001 | 1.23 (1.19–1.27) | <0.0001 | 1.32 (1.28–0.37) | <0.0001 |
| Model 2 | 1.15 (1.1–1.21) | <0.0001 | 1.1 (1.06–1.14) | <0.0001 | 1.16 (1.12–1.21) | <0.0001 |
| Chronic hypertension | ||||||
| Model 1 | 1.73 (1.69–1.78) | <0.0001 | 1.37 (1.35–1.4) | <0.0001 | 1.61 (1.57–1.64) | <0.0001 |
| Model 2 | 1.24 (1.20–1.28) | <0.0001 | 1.14 (1.12–1.17) | <0.0001 | 1.23 (1.2–1.26) | <0.0001 |
Model 1 is adjusted for age, chronic hypertension, and HDP. Model 2 is fully adjusted with all variables listed in Table 4. HDP indicates hypertensive disorders of pregnancy; and OR, odds ratio.
The effect of other baseline characteristics on postpartum follow‐up are presented in Table 4. Women with preterm delivery were 29% more likely to follow up with any provider than women with full‐term delivery (OR, 1.29; 95% CI, 1.27–1.3), an effect that was largely driven by women's health provider follow‐up. Chronic medical conditions, including diabetes mellitus, lipid disorders, coronary artery disease, and heart failure, were associated with a significantly greater likelihood of any provider follow‐up, largely driven by a greater likelihood of follow‐up with primary care providers. Women with an emergency department visit before delivery were 25% and 33% more likely to follow‐up with primary care (OR, 1.25; 95% CI, 1.23–1.28) and women's health providers (OR, 1.33; 95% CI, 1.31–1.34), respectively. Women who were prescribed an antihypertensive medication before pregnancy were 49% more likely to follow up with primary care (OR, 1.49; 95% CI, 1.41–1.58) and 22% more likely to follow‐up with women's health providers (OR, 1.22; 95% CI, 1.16, 1.28). Characteristics associated with a lower likelihood of postpartum follow‐up with any provider included women aged ≥30 years (OR, 0.94; 95% CI, 0.93–0.95), Black race/ethnicity (OR, 0.92; 95% CI, 0.9–0.94), Hispanic race/ethnicity (OR, 0.85; 95% CI, 0.84–0.87), and multiple gestations (OR, 0.85; 95% CI, 0.82–0.88).
Table 4.
Characteristics Associated With Postpartum Ambulatory Care Follow‐up Within 6 Months After Delivery According to Provider Type in Multivariable Analysis
| Primary Care | Women's Health | Any Provider | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Demographics | ||||||
| Age ≥30 y | 1.24 (1.22–1.26) | <0.0001 | 0.86 (0.85–0.87) | <0.0001 | 0.94 (0.93–0.95) | <0.0001 |
| Race/ethnicity | ||||||
| Black | 1.05 (1.02–1.08) | 0.0006 | 0.91 (0.89–0.93) | <0.0001 | 0.92 (0.9–0.94) | <0.0001 |
| Hispanic | 0.89 (0.87–0.91) | <0.0001 | 0.87 (0.86–0.89) | <0.0001 | 0.85 (0.84–0.87) | <0.0001 |
| White | Ref | Ref | Ref | |||
| HS graduate or less | 0.91 (0.89–0.92) | <0.0001 | 1.03 (1.02–1.05) | <0.0001 | 0.99 (0.98–1.0) | 0.1366 |
| Geographic region | ||||||
| Northeast | 2.5 (2.43–2.57) | <0.0001 | 0.95 (0.93–0.97) | <0.0001 | 1.34 (1.31–1.36) | <0.0001 |
| Midwest | 1.12 (1.09–1.15) | <0.0001 | 1.2 (1.18–1.22) | <0.0001 | 1.25 (1.23–1.27) | <0.0001 |
| South | 1.51 (1.48–1.55) | <0.0001 | 1.17 (1.15–1.18) | <0.0001 | 1.31 (1.29–1.33) | <0.0001 |
| West | Ref | Ref | Ref | |||
| Obstetrics history | ||||||
| Cesarean delivery | 1.1 (1.08–1.11) | <0.0001 | 1.12 (1.11–1.14) | <0.0001 | 1.15 (1.13–1.16) | <0.0001 |
| Preterm delivery | 1.14 (1.12–1.16) | <0.0001 | 1.28 (1.27–1.3) | <0.0001 | 1.29 (1.27–1.3) | <0.0001 |
| Multiple gestations | 0.91 (0.87–0.95) | 0.0001 | 0.86 (0.84–0.9) | <0.0001 | 0.85 (0.82–0.88) | <0.0001 |
| Gestational diabetes | 1.07 (1.04–1.09) | <0.0001 | 1.07 (1.05–1.09) | <0.0001 | 1.09 (1.07–1.1) | <0.0001 |
| Hypertensive disorders | ||||||
| Gestational hypertension | 1.1 (1.07–1.13) | <0.0001 | 1.13 (1.11–1.16) | <0.0001 | 1.14 (1.12–1.17) | <0.0001 |
| Nonsevere preeclampsia | 1.09 (1.05–1.13) | <0.0001 | 1.16 (1.13–1.19) | <0.0001 | 1.16 (1.13–1.19) | <0.0001 |
| Severe preeclampsia | 1.15 (1.1–1.21) | <0.0001 | 1.1 (1.06–1.14) | <0.0001 | 1.16 (1.12–1.21) | <0.0001 |
| Chronic hypertension | 1.24 (1.20–1.28) | <0.0001 | 1.14 (1.12–1.17) | <0.0001 | 1.23 (1.2–1.26) | <0.0001 |
| Medical comorbidities | ||||||
| Diabetes mellitus | 1.19 (1.13–1.24) | <0.0001 | 1.11 (1.07–1.16) | <0.0001 | 1.17 (1.13–1.21) | <0.0001 |
| Lipid disorder | 1.79 (1.73–1.85) | <0.0001 | 1.23 (1.2–1.27) | <0.0001 | 1.56 (1.52–1.61) | <0.0001 |
| Coronary artery disease | 1.75 (1.56–1.96) | <0.0001 | 1.08 (0.98–1.2) | 0.1398 | 1.42 (1.27–1.58) | <0.0001 |
| Kidney disease | 1.21 (1.05–1.39) | 0.0078 | 0.86 (0.76–0.97) | 0.0134 | 0.99 (0.87–1.12) | 0.8262 |
| Heart failure | 2.57 (2.22–2.97) | <0.0001 | 1.04 (0.91–1.2) | 0.5615 | 1.55 (1.33–1.81) | <0.0001 |
| Healthcare utilization | ||||||
| Prior ED visit*, * | 1.25 (1.23–1.28) | <0.0001 | 1.33 (1.31–1.34) | <0.0001 | 1.36 (1.34–1.38) | <0.0001 |
| Prior BP medication use † , † | 1.49 (1.41–1.58) | <0.0001 | 1.22 (1.16–1.28) | <0.0001 | 1.43 (1.36–1.5) | <0.0001 |
BP indicates blood pressure; ED, emergency department; HS, high school; OR, odds ratio; and Ref, referent.
Before delivery.
Before pregnancy.
DISCUSSION
Among postpartum women with commercial insurance, only 58% of women with HDP followed up with a continuity care provider within 6 months of delivery. Up to 350 000 women in the United States are diagnosed with preeclampsia or gestational hypertension every year. 21 If our results are generalized to the broader US population, an estimated 147 000 women will lack postpartum follow‐up in the 6 months after delivery. By 12 months postpartum, 1 in 4 affected women will still not have followed up with a continuity care provider, including primary care, obstetrics, or family medicine. These low follow‐up rates highlight a substantial missed opportunity to provide counseling, screening, and treatment to women who are at increased risk of developing short‐ and long‐term cardiovascular sequelae.
Women with HDP have 12‐ to 25‐fold higher risk of being diagnosed with chronic hypertension in the year after delivery and 2‐fold increased lifetime risk of heart failure, coronary heart disease, and cardiovascular death compared with women with normotensive pregnancies. 5 , 7 , 8 , 22 Up to 77% of the excess cardiovascular risk associated with HDP may be explained by modifiable risk factors, such as hypertension and obesity, that are amenable to early treatment. 23 The potential benefit of postpartum primary care follow‐up is multifactorial and includes the opportunity to provide blood pressure, lipid, and diabetes mellitus screening; to manage hypertension; and to reinforce the importance of healthy lifestyle changes to improve interconception and future cardiovascular health, as recommended by the AHA and the American College of Obstetricians and Gynecologists. 15 In addition to longer term cardiovascular health benefits, postpartum blood pressure control and weight loss can reduce the risk of developing recurrent preeclampsia in subsequent pregnancies. 9 , 24 , 25
Our analysis demonstrates that patients diagnosed with chronic medical conditions, such as chronic hypertension, diabetes mellitus, lipid disorders, coronary artery disease, and heart failure, are more likely to have postpartum ambulatory care follow‐up, largely driven by follow‐up with primary care providers. This results suggests that the postpartum care transition may be facilitated by women having a preexisting relationship with a healthcare provider or that women who are motivated to seek out care before pregnancy may simply be motivated to seek out care postpartum. In addition, women with preexisting relationships with primary care providers may be more likely to have been previously diagnosed with a chronic condition (eg, chronic hypertension or lipid disorder).
Several barriers exist to facilitating follow‐up care for patients with HDP. First, women face unique challenges in the postpartum period that complicate follow‐up care, including fatigue, pain, infant caregiving and feeding demands, exacerbation of mental health disorders, and inconvenience. 26 , 27 , 28 Second, the lack of communication between maternity providers and primary care providers about pregnancy complications may complicate timely follow‐up. 29 Third, specific postpartum preventive care guidelines are lacking, which may lead to clinical inertia in prioritizing the scheduling or emphasizing the importance of attending postpartum ambulatory care visits. 11 , 30 , 31 Finally, awareness of HDP as a risk factor for chronic hypertension and future cardiovascular disease is lacking among primary care providers and may affect the successful transition of care, as well the delivery of appropriate cardiovascular risk counseling. 32 , 33 , 34
The intense focus on women's health prenatally is not sustained in the postpartum period. The 12 weeks after delivery have been described as the fourth trimester to reflect the ongoing physical, mental, and emotional challenges that many women face. 35 The opportunity to optimize interconception and long‐term health during this period is limited by low follow‐up rates, as demonstrated in our study. The majority of postpartum visits in our analysis were with women's health providers, who are more likely to recognize future health risks of pregnancy complications but less likely to perform preventative cardiovascular risk assessment. 32 , 34 More systematic and persistent outreach is needed. Comprehensive care is more likely to appeal to women rather than highly specialized visits. 36 Monitoring and treatment delivered remotely by text messages can improve blood pressure control in the immediate postpartum period in high‐risk women and may offer insight into engaging women who are more remote from delivery in healthy behaviors. 37 Finally, enrolling postpartum women into chronic disease screening and management pathways may offer standardization of screening and treatment during this period of transition.
The primary care follow‐up rates in our study are similar to those reported among a nationally representative sample of women with gestational diabetes mellitus 17 but lower than those reported among women with pregnancies complicated by gestational diabetes mellitus or hypertensive disorders in Maryland. 16 This variation may represent geographical variation or definitional differences of claims‐based outcomes. We categorized postpartum follow‐up with family medicine providers as receiving obstetric care. To account for family medicine providers and obstetricians serving as both maternity and continuity providers, we also analyzed our data to reflect follow‐up with any of these providers. Postpartum visits with women's health providers may be underreported in claims data because of the global billing of pregnancy care, which includes prenatal care, inpatient delivery, and routine postpartum care within 6 weeks of delivery. 38 However postpartum visits for the treatment of pregnancy complications, such as preeclampsia, and all follow‐up visits beyond 6 weeks postpartum are typically billed outside of the global payment for pregnancy care. Consequently, the follow‐up rates with primary care providers in our study should not be affected by the global billing system for pregnancy care.
Our analysis has a number of limitations. First, the documentation of postpartum follow‐up does not guarantee that cardiovascular risk factor counselling was provided; therefore, the receipt of preventative risk assessment is likely overestimated. Second, we adjusted for socioeconomic status using race and educational attainment, but we lacked more granular detail on social determinants of health. Third, certain clinical factors that may affect clinical outcomes and healthcare utilization are not well captured in claims‐based data sets, such as smoking, substance abuse, and obesity. 39 Fourth, although we relied on validated algorithms for identifying pregnancies and hypertensive disorders within claims data, we may have incorrectly identified some cases because of incorrect billing codes and codes for postpartum ambulatory care have not yet been validated. There may be some misclassification of chronic hypertension given potentially insufficient clinical encounter data before pregnancy. Fifth, our data extend until 2015 and may not represent more recent changes in healthcare utilization. Finally, our findings may not be generalizable to a more diverse population given that our cohort is older and more likely to be White than the general US population of pregnant nulliparous women. Furthermore, our cohort has continuous commercial insurance coverage extending from 6 months before pregnancy until at least 6 months after delivery, suggesting fewer barriers to accessing care. Given these restrictions, our findings are even more striking given the overall low rates of follow‐up among a relatively socioeconomically advantaged population.
CONCLUSIONS
Among a nationally representative cohort of women with commercial insurance, women with HDP had a significantly higher likelihood of follow‐up with primary care providers at 6 months after delivery compared with women without HDP; however, overall rates of follow‐up remained low. This represents a missed opportunity to provide important cardiovascular risk assessment in a population of women at increased risk of future cardiovascular disease. Further study is needed to understand barriers to continuity care transition in the postpartum period and to assess for the role of interventions designed to improve risk factor control.
Sources of Funding
This study was supported by grants K12 HD085848 (Lewey) and R56 575508 (Levine) from the National Institutes of Health.
Disclosures
None.
Supporting information
Tables S1–S2
(J Am Heart Assoc. 2020;9:e05459 DOI: 10.1161/JAHA.120.016357.)
Supplementary Materials for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.016357
For Sources of Funding and Disclosures, see page 9.
References
- 1. American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy . Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–1131. [DOI] [PubMed] [Google Scholar]
- 2. Miller EC, Gatollari HJ, Too G, Boehme AK, Leffert L, Marshall RS, Elkind MSV, Willey JZ. Risk factors for pregnancy‐associated stroke in women with preeclampsia. Stroke. 2017;48:1752–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bateman BT, Schumacher HC, Bushnell CD, Pile‐Spellman J, Simpson LL, Sacco RL, Berman MF. Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology. 2006;67:424–429. [DOI] [PubMed] [Google Scholar]
- 4. Sharma KJ, Kilpatrick SJ. Postpartum hypertension: etiology, diagnosis, and management. Obstet Gynecol Surv. 2017;72:248–252. [DOI] [PubMed] [Google Scholar]
- 5. Mongraw‐Chaffin ML, Cirillo PM, Cohn BA. Preeclampsia and cardiovascular disease death: prospective evidence from the child health and development studies cohort. Hypertension. 2010;56:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bellamy L, Casas J‐P, Hingorani AD, Williams DJ. Pre‐eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta‐analysis. BMJ. 2007;335:974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, Zaman A, Fryer AA, Kadam U, Chew‐Graham CA, et al. Preeclampsia and future cardiovascular health: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2017;10:ee003497 DOI: 10.1161/CIRCOUTCOMES.116.003497. [DOI] [PubMed] [Google Scholar]
- 8. Behrens I, Basit S, Melbye M, Lykke JA, Wohlfahrt J, Bundgaard H, Thilaganathan B, Boyd HA. Risk of post‐pregnancy hypertension in women with a history of hypertensive disorders of pregnancy: nationwide cohort study. BMJ. 2017;358:j3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger GZ, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, Howard VJ, Lichtman JH, Lisabeth LD, Piña IL, et al. Guidelines for the prevention of stroke in women a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014:45:1545–1588. DOI: 10.1161/01.str.0000442009.06663.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd‐Jones DM, Newby LK, Piña IL, Roger VL, Shaw LJ, et al.; American Heart Association . Effectiveness‐based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57:1404–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brown MC, Bell R, Collins C, Waring G, Robson SC, Waugh J, Finch T. Women’s perception of future risk following pregnancies complicated by preeclampsia. Hypertens Pregnancy. 2013;32:60–73. [DOI] [PubMed] [Google Scholar]
- 13. Seely EW, Rich‐Edwards J, Lui J, Nicklas JM, Saxena A, Tsigas E, Levkoff SE. Risk of future cardiovascular disease in women with prior preeclampsia: a focus group study. BMC Pregnancy Childbirth. 2013;13:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McKinney J, Keyser L, Clinton S, Pagliano C. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet Gynecol. 2018;132:784–785. [DOI] [PubMed] [Google Scholar]
- 15. Brown HL, Warner JJ, Gianos E, Gulati M, Hill AJ, Hollier LM, Rosen SE, Rosser ML, Wenger NK. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137:e843–e852. [DOI] [PubMed] [Google Scholar]
- 16. Bennett WL, Chang H‐Y, Levine DM, Wang L, Neale D, Werner EF, Clark JM. Utilization of primary and obstetric care after medically complicated pregnancies: an analysis of medical claims data. J Gen Intern Med. 2014;29:636–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bernstein JA, Quinn E, Ameli O, Craig M, Heeren T, Lee‐Parritz A, Iverson R, Jack B, McCloskey L. Follow‐up after gestational diabetes: a fixable gap in women’s preventive healthcare. BMJ Open Diabetes Res Care. 2017;5:e000445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Palmsten K, Huybrechts KF, Mogun H, Kowal MK, Williams PL, Michels KB, Setoguchi S, Hernández‐Díaz S. Harnessing the Medicaid Analytic eXtract (MAX) to evaluate medications in pregnancy: design considerations. PLoS One. 2013;8:e67405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Margulis AV, Setoguchi S, Mittleman MA, Glynn RJ, Dormuth CR, Hernández‐Díaz S. Algorithms to estimate the beginning of pregnancy in administrative databases. Pharmacoepidemiol Drug Saf. 2013;22:16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol. 2009;113:1299–1306. [DOI] [PubMed] [Google Scholar]
- 21. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67:1–50. [PubMed] [Google Scholar]
- 22. Levine LD, Nkonde‐Price C, Limaye M, Srinivas SK. Factors associated with postpartum follow‐up and persistent hypertension among women with severe preeclampsia. J Perinatol. 2016;36:1079–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Haug EB, Horn J, Markovitz AR, Fraser A, Klykken B, Dalen H, Vatten LJ, Romundstad PR, Rich‐Edwards JW, Åsvold BO. Association of conventional cardiovascular risk factors with cardiovascular disease after hypertensive disorders of pregnancy: analysis of the Nord‐Trøndelag Health Study. JAMA Cardiol. 2019;4:628–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population‐based study. Lancet. 2006;368:1164–1170. [DOI] [PubMed] [Google Scholar]
- 25. Lapolla A, Marangon M, Dalfrà MG, Segato G, De Luca M, Fedele D, Favretti F, Enzi G, Busetto L. Pregnancy outcome in morbidly obese women before and after laparoscopic gastric banding. Obes Surg. 2010;20:1251–1257. [DOI] [PubMed] [Google Scholar]
- 26. Henderson V, Stumbras K, Caskey R, Haider S, Rankin K, Handler A. Understanding factors associated with postpartum visit attendance and contraception choices: listening to low‐income postpartum women and health care providers. Matern Child Health J. 2016;20:132–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Walker LO, Murphey CL, Nichols F. The broken thread of health promotion and disease prevention for women during the postpartum period. J Perinat Educ. 2015;24:81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bernstein JA, McCloskey L, Gebel CM, Iverson RE, Lee‐Parritz A. Lost opportunities to prevent early onset type 2 diabetes mellitus after a pregnancy complicated by gestational diabetes. BMJ Open Diabetes Res Care. 2016;4:e000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. MacDonald SE, Walker M, Ramshaw H, Godwin M, Chen X, Smith G. Hypertensive disorders of pregnancy and long‐term risk of hypertension: what do Ontario prenatal care providers know, and what do they communicate? J Obstet Gynaecol Can. 2007;29:705–710. [DOI] [PubMed] [Google Scholar]
- 30. Julia S, Louis P, Marc S, Mark B. Cardiovascular risk management after a hypertensive disorder of pregnancy. Hypertension. 2012;60:1368–1373. [DOI] [PubMed] [Google Scholar]
- 31. ACOG Practice Bulletin No. 202: gestational hypertension and preeclampsia. Obstet Gynecol. 2019;133:e1–e25. [DOI] [PubMed] [Google Scholar]
- 32. Wilkins‐Haug L, Celi A, Thomas A, Frolkis J, Seely EW. Recognition by womenʼs health care providers of long‐term cardiovascular disease risk after preeclampsia. Obstet Gynecol. 2015;125:1287–1292. [DOI] [PubMed] [Google Scholar]
- 33. Young B, Hacker MR, Rana S. Physicians’ knowledge of future vascular disease in women with preeclampsia. Hypertens Pregnancy. 2012;31:50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. van Kesteren F, Visser S, Hermes W, Teunissen PW, Franx A, van Pampus MG, Mol BW, de Groot CJM. Counselling and management of cardiovascular risk factors after preeclampsia. Hypertens Pregnancy. 2016;35:55–61. [DOI] [PubMed] [Google Scholar]
- 35. Tully KP, Stuebe AM, Verbiest SB. The fourth trimester: a critical transition period with unmet maternal health needs. Am J Obstet Gynecol. 2017;217:37–41. [DOI] [PubMed] [Google Scholar]
- 36. Smith GN, Louis JM, Saade GR. Pregnancy and the postpartum period as an opportunity for cardiovascular risk identification and management. Obstet Gynecol. 2019;134:851–862. [DOI] [PubMed] [Google Scholar]
- 37. Hirshberg A, Downes K, Srinivas S. Comparing standard office‐based follow‐up with text‐based remote monitoring in the management of postpartum hypertension: a randomised clinical trial. BMJ Qual Saf. 2018;27:871–877. [DOI] [PubMed] [Google Scholar]
- 38. Coding for Postpartum Services (The Fourth Trimester). Available at: https://www.acog.org/en/Practice‐Management/coding/Coding‐Library/Coding‐for-Postpartum-Services‐The-4th‐Trimester. Accessed March 21, 2020.
- 39. Triebwasser JE, Kamdar NS, Langen ES, Moniz MH, Basu T, Syrjamaki J, Thomason AC, Smith RD, Morgan DM. Hospital contribution to variation in rates of vaginal birth after cesarean. J Perinatol. 2019;39:904–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


