Abstract
Introduction
Aphasia is a common language disorder acquired after stroke that reduces the quality of life of affected patients. The impairment is frequently accompanied by a deficit in cognitive functions. The state-of-the-art therapy is speech and language therapy but recent findings highlight positive effects of high-frequency therapy. Telerehabilitation has the potential to enable high-frequency therapy for patients at home. This study investigates the effects of high-frequency telerehabilitation speech and language therapy (teleSLT) on language functions in outpatients with aphasia compared with telerehabilitative cognitive training. We hypothesise that patients training with high-frequency teleSLT will show higher improvement in language functions and quality of life compared with patients with high-frequency tele-rehabilitative cognitive training (teleCT).
Methods and analysis
This study is a randomised controlled, evaluator-blinded multicentre superiority trial comparing the outcomes following either high-frequency teleSLT or teleCT. A total of 100 outpatients with aphasia will be recruited and assigned in a 1:1 ratio stratified by trial site and severity of impairment to one of two parallel groups. Both groups will train over a period of 4 weeks for 2 hours per day. Patients in the experimental condition will devote 80% of their training time to teleSLT and the remaining 20% (24 min/day) to teleCT, vice versa for patients in the control condition. The primary outcome measure is the understandability of verbal communication on the Amsterdam Nijmegen Everyday Language Test and secondary outcome measures are intelligibility of the verbal communication, impairment of receptive and expressive language functions, confrontation naming. Other outcomes measures are quality of life and acceptance (usability and subjective experience) of the teleSLT system.
Ethics and dissemination
This study is approved by the Ethics Committee Bern (ID 2016-01577). Results will be submitted to a peer-reviewed journal.
Trial registration number
Keywords: rehabilitation medicine, stroke, neurological injury, neurology, telemedicine
Strengths and limitations of this study.
The multicentric nature of the study increases the generalisability of results.
Recruitment in multicentric sites promotes easier access to larger sample size.
Evaluators measuring outcomes are blinded to the allocation.
Lack of compliance to the training time over a 4-week duration might result in bias.
Person-centric outcomes (quality of life, speech improvements) may limit generalisation.
Introduction
According to the global health estimates by the WHO, stroke is a leading cause of disability and death worldwide.1 Approximately one-third of stroke patients develop aphasia.2 Aphasia is an acquired language disorder and affects speaking, verbal comprehension, reading and writing.3 Although spontaneous recovery is possible, 19% of patients who had stroke still suffer from severe chronic aphasia 1 year post stroke.4 There is evidence that aphasia has the highest negative impact on health-related quality of life compared with non-infectious as well as infectious disorders.5 In particular, the language impairments of aphasia result in major negative consequences for participation in social life.
Speech and language therapy (SLT) is the gold standard in aphasia treatment and is recommended by the current clinical guidelines in stroke management.6 The aim of SLT is to maximise the patients’ communication abilities and participation. There is evidence that SLT improves functional communication as well as receptive and expressive language,3 including patients with chronic aphasia.7 8 Intensive SLT enhances their verbal communication abilities.9 Dosage is a key factor for successful aphasia therapy, but it remains unclear whether dose frequency (eg, training time per day) or intervention duration (eg, number of weeks) is more crucial.6
From a practical point of view, providing high-dose frequency SLT to patients depends on the availability of qualified speech and language therapists and reimbursement by insurance companies. One way to lessen the reliance on face-to-face SLT services and to provide intensive SLT for patients with aphasia is the use of telemedicine technology. Telemedicine by using tablet computers offers the possibility for patients to exercise at a high frequency independently at home, while being remotely monitored by therapists. There is evidence that additional tablet-based training to SLT improves language functions and thus decreases impairment severity.10 Telerehabilitation speech and language therapy (teleSLT) was also demonstrated to be effective in patients who had chronic stroke.11 Although tablet-based aphasia treatment has been reported in a number of studies,10 12–14 there is little detail as to how the efficacy of the exercises was optimised for study participants. Assignment of exercises adapted to patient needs is time consuming and requires evaluation of performance and adaptation of exercise levels by speech and language therapists. Furthermore, there are lack of studies investigating the effect of teleSLT over a prolonged time. Therefore, there is a high need of new validated telerehabilitation applications including facilitated exercise assignment methods to deliver efficient SLT to persons with aphasia.
Additionally, aphasia following a stroke can be accompanied by deficits in cognitive abilities such as attention,15 speed of processing, working memory and other executive functions.16 It has been shown that these cognitive deficits impact recovery and rehabilitation of aphasia.17–19 These cognitive abilities are also known to be involved in sentence comprehension and speech production.20–22 Sentences with ambiguous syntactic structure can be interpreted in more than one way. Previous research has shown that the ability of patients with aphasia to reinterpret ambiguous sentences was proportional to their executive functions (eg, processing speed).23 It has also been shown that comprehension of syntactically ambiguous material is related to demanding working memory.24 Recent studies suggest that working memory, processing speed and other executive skills can be enhanced with cognitive training (CT).25 26
The authors thus suggest that SLT should be accompanied with CT. It remains, however, unclear what percentage of the training time should be devoted to SLT and CT, respectively. For the current study, we will use two combinations of teleSLT and telerehabilitation cognitive training (teleCT), where one combination will have a higher percentage of time devoted to teleSLT and the other a higher percentage devoted to teleCT. The latter will serve as the control group to examine the effect of teleSLT. The teleSLT application which started as a master thesis27 was evaluated for usability by 15 healthy controls, 5 patients with aphasia, and 5 speech therapists. Results from the usability study28 (patient’s subjective experience, enjoyment and stress experienced) showed excellent usability, high acceptability and motivation for training independently by 15 patients. The usability of the teleCT used in this study has already been demonstrated for participants of different age groups.29 30 The two games used in the teleCT application address processing speed, visual attention and executive compounds such as inhibition and planning.29 30
Therefore, the purpose of this study is to investigate the effects of prolonged high-frequency teleSLT on language functions in patients who had chronic stroke with diagnosed aphasia. In the experimental condition, patients will devote more time to teleSLT compared with a control task (teleCT). We hypothesise that patients training with high-dose teleSLT (and low-dose teleCT) show higher improvements in the outcome of language functions, and thus the quality of life, compared with patients with high-dose teleCT (and low-dose teleSLT) as measured by standard language tests.
Methods
Trial design and study setting
This study is designed as a randomised controlled, evaluator-blinded multicentre superiority trial comparing the outcomes following either high-dose frequent teleSLT or teleCT and has been developed following the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines as explained in the SPIRIT guidelines.31 The study is conducted at the University Hospital Bern (Inselpital) and the Central Hospital Lucerne in Switzerland.
Enrolled patients are randomly assigned to the experimental or control group. In both cases, patients will exercise on a tablet-computer for 4 weeks (7 days per week), 2 hours a day independently at home by using the teleSLT and teleCT application (figure 1). The selection of training frequency and duration was based on literature that reports intensive therapy over a short period of time has better outcome.6 9 32 The training frequency and duration was set, based on the clinical experience of the local speech and language therapists who were involved in the usability study27 28 guaranteeing its feasibility for the participants. The usability study27 28 provided a rough estimate of teleSLT usage if the patients could decide for themselves. The intervention duration of 4 weeks was selected from patient feedback collected during face-to-face SLT sessions with an aim to reduce dropout rates. The intervention period differs in the time devoted to teleSLT and teleCT. The distribution of training time (80% vs 20%) is based on a Cochrane Review3 to reflect the high-intensity SLT (4–15 hours/week) and low-intensity SLT (1.5–5 hours/week) interventions. Patients in the experimental condition will devote 80% of their self-paced training time to teleSLT (96 min/day=11.2 hours/week) and the remaining 20% (24 min/day=2.8 hours/week) to teleCT, vice versa for patients in the control condition (24 min/day teleSLT +96 min/day teleCT). In case of teleSLT intervention, the exercises get updated weekly during the intervention using a computerised adaptive testing algorithm. Outcome measures which will include severity and effectiveness of teleSLT and teleCT on language functions are assessed at different time points (before and after intervention, follow-up 6 weeks).
Figure 1.
Standard Protocol Items: Recommendations for Interventional Trials—schedule of enrolment, allocation, intervention and outcome measures. ANELT, Amsterdam Nijmegen Everyday Language Test; BNT, Boston Naming Test; CG, Control Group; EG, Experimental Group; IMI, Intrinsic Motivation Inventory; SAPS, Sprachsystematisches APhasie Screening; SAQOL, Stroke and Aphasia quality of life; SLT, Speech and Language Therapy; SUS, System Usability Scale.
Patient and public involvement
The public was not directly involved in the development of the research question or design of this study. Subjective experiences of the participants will be collected at the end of the intervention allowing them to express their opinion and experience.
Recruitment and participants
Speech and language therapists at both study sites will recruit patients and evaluate their eligibility (table 1). The study population will consist of native German speakers aged 18 years or older who have been diagnosed with aphasia. Study participants will be at least 1 year post onset of their stroke. Furthermore, eligible patients need to retrieve at least 10% but not more than 80% of words on the Boston Naming Test33 and patients must have the ability (sufficient vision and cognition) to work using tablet-computer applications. Patients with any other premorbid speech and language disorder caused by a deficit other than stroke and not German speaking will be excluded. All patients receive an information sheet and a consent form (online supplemental appendix A). The local speech and language therapists will guide the patients through the information and consent sheet, to ensure that they can make an informed decision on participation in the study.
Table 1.
Overview of eligibility criteria
| Inclusion criteria | Exclusion criteria |
| Aged equal to or greater than 18. | Any other premorbid speech and language disorder caused by a deficit other than stroke. |
| At least 1 year post onset of stroke. | Requirement for treatment in language other than German. |
| Diagnosis of aphasia due to stroke. | |
| Ability to retrieve 10%–80% of words on the Boston Naming Test. | |
| Completed therapy for 2 months. | |
| Sufficient vision and cognitive ability to work with the used tablet-computer applications (for assessment, sample exercises during the instruction of patients are used). |
bmjopen-2020-037702supp001.pdf (105KB, pdf)
The required sample size to reject the null hypothesis that word finding ability is significantly higher in the experimental than in the control group is 78 patients. For this calculation, a t-test with a 5% one-sided significance level, a power of 80% and an estimated effect size of 0.57 were chosen. The estimation of effect size is based on a previous pilot study as the applied telerehabilitative system consisted of similar training modalities to the system used in the current study.34 To ensure that at least 78 patients participate in the study with an assumed dropout rate of 20%, we chose a total sample size of 100 subjects.
Allocation
Blinding of participants in psychological interventions is practically impossible35 and therefore, this study uses an evaluator-blinded design. Allocation is performed by an independent data manager who is not involved in the evaluation and assessment of patients by using Research Electronic Data Capture which is a certified clinical and translational research database.36 Allocation is 1:1 stratified by study site (University Hospital Bern and Central Hospital Lucerne, Switzerland) and by severity of word retrieval deficit at baseline by the Boston Naming Test (severe=10%–33%, and mild=58%–80%). After allocation, the intervention group is revealed via the web interface of the clinical and translational research database exclusively to study personnel who are not collecting or evaluating outcome measures.
Outcome measures
All primary and secondary outcomes are measured at the beginning, at the end (post-test), and 6 weeks after the intervention (follow-up). The primary outcome is the understandability of verbal communication which is assessed with the A-scale of the Amsterdam Nijmegen Everyday Language Test (ANELT).37 During the test, an investigator presents 10 different everyday life situations and asks patients what they would say in this moment. The answer is judged with respect to the understandability (A-scale) and intelligibility (B-scale) of the verbal communication. The ANELT was already used in previous studies.3 38 It has been validated for use in a population with language impairments and has been shown to have good test parallel reliability and internal consistency for both versions (parallel versions ANELT I and ANELT II).39 ANELT I is used as pretest as well as follow-up, whereas ANELT II is used as post-test.
The secondary outcomes consist of intelligibility of the verbal communication, impairment of receptive and expressive language functions, comprehension of verbal commands of increasing complexity, and word retrieval in confrontation naming. Intelligibility of the verbal communication is measured with the B-scale of the ANELT (eg, by judging the utterance independent of the meaning). The impairment of receptive and expressive abilities assessed by using the ‘Sprachsystematisches Aphasie Screening’ comprises comprehension and production abilities in different domains (eg, morphology and syntax) and difficulty levels (eg, naming of pictures visualising high/low frequency words). Since a range of domains is assessed, this measure allows evaluation of disorder specific treatments. Reliability of both scales (receptive and expressive abilities) had estimates close to 1.39
In addition to previous measures, the Token Test40 and a 30-item version of the Boston Naming Test are used to detect comprehension of verbal commands of increasing complexity41 and to assess the word retrieval in confrontation naming,33 respectively. The Boston Naming Test is the most frequently used test for assessment of visual naming ability and its psychometric properties were demonstrated in several ways (ie, reliability coefficients, congruent validity).42 Similarly, the Token Test yields a good test–retest reliability43 and has been validated for use in patients with aphasia in which a relationship between the test performance and the level of severity of aphasia was demonstrated.44
Other outcomes which are assessed 6 weeks after the intervention comprise of perceived quality of life (ie, Stroke and Aphasia Quality Of Life,44 as well as usability and subject experience of the intervention (ie, System Usability Scale45 and the Intrinsic Motivation Inventory46).
Intervention
Both telerehabilitation applications will be preinstalled on a 12.9-inch iPad Pro tablet-computer (Apple, Cupertino, California, USA). An investigator will familiarise participants with the applications and instruct them not to use other sources of rehabilitation (eg, applications installed on a private computer) for the duration of the study.
teleSLT
The teleSLT application (Bern Aphasia App) is designed as an add-on to standard speech and language therapy running on a tablet computer developed by the University of Bern.27 28 By providing a set of interfaces, patients can train independently at home while therapists can assign exercises, track the performance and implement patient specific new exercises remotely. In a usability study, it was shown that the app is well accepted by patients and therapists.28
Patients are provided with an overview of exercise collections assigned by a speech and language therapist. Collections are intended to train a specific language impairment (eg, semantically categorising items). Patients are free to select specific collections from among the assigned ones. As soon as the limit of the training time is reached, access to assigned collections is prohibited until the next day.
Once patients start to solve exercises, therapists are provided with information regarding the performance of the patient. Analysing the performance remotely, therapists can adapt the training by either increasing or lowering the difficulty level of collections or replacing assigned collections with new ones of the same difficulty level. However, during the current study, difficulty levels of collections have been adjusted using a criterion-based computerised adaptive testing algorithm.
Exercises
The application in total provides ten different exercise types with more than 30 000 validated exercises (table 2), which allow for the adaptation of the exercises to the patient’s needs (ie, varying the difficulty of the exercise). The exercise types cover all levels of language organisation, that is, phonology, grammar (consisting of morphology and syntax) and semantics.28
Table 2.
Description of exercise types adapted from Gerber et al28
| Exercise type | Level | Description | Additional media | Metadata |
| Single picture-word matching | Phonology | Selecting the correct word from phonematically resp. semantically related distractors | Audio, video | Part of speech (eg, noun) of correct word, level of distractor (eg, phonological), number of distractors |
| Semantic | ||||
| Single word-picture matching | Phonology | Selecting the correct picture from phonematically resp. semantically related distractors | Audio, video | Part of speech of presented word, level of distractor, number of distractors |
| Semantic | ||||
| Multiple Matching | Semantic | Match all objects (word-picture, picture-picture, word-word) | – | Type of match (eg, synonyms) |
| Word completion | Phonology | Selecting the correct letter(s) (from distractors) and inserting them into the correct position(s) | Audio, image, video | Number of syllables, part of speech, number of elements to be inserted, sound (eg, consonant) of correct letter(s), number of distractors, sound of distractors |
| Sentence completion | Grammar | Selecting the correct word(s) (from grammatically resp. semantically related distractors) and inserting them into the correct position(s) | Audio, image, video | Level of distractor (eg, semantical), syntax, number of elements to be inserted, part of speech of correct word(s), number of distractors, frequency, inflection |
| Semantic | ||||
| Anagram | Phonology | Bringing the letters into the correct order | Audio, image, video | Number of syllables, part of speech (eg, noun), inflection (eg, past tense) |
| Sentence ordering | Grammar | Bringing the words into the correct order | Audio, image, video | Number of words, syntax, REST part of speech, inflection, |
| Word repetition | Phonology | Repeating the audio-visually recorded spoken word by a speech and language therapist | Variety (eg, dialect), first ordering principle (eg, number of syllables), secondary ordering principle (eg, initial sound) | |
| Copy and recall | Phonology | Copying and recalling presented words by typing or writing | Frequency (eg, high) | |
| Semantic | ||||
| Lexical | ||||
| Comprehension | Auditory | Selecting the correct answer to a question about the auditory, audio-visual, text-based resp. image-based information | Difficulty (eg, easy), text type (eg, narrative) | |
| Audio-visual | ||||
| Reading | ||||
| Visual |
Exercises consist of fixed (eg, written language, placeholders), supportive (eg, videos, audio tracks, images) and response elements (eg, unarranged letters), except exercises of the type word repetition which exclusively provide videos as fixed elements. Unmovable and required elements to solve the exercise are referred to as fixed elements.
A help button provides part of the solution to solve the exercise. Besides that, supportive components such as videos, audio tracks or images yield further facilitation of exercises by providing information through different sensory modalities (eg, an image of a pullover). Movable or clickable elements which operationalise a patient’s response and/or the feedback that follows after a response are referred to as response elements. To illustrate the components, an exercise of the type Anagram is shown in figure 2, where the goal is to arrange letters to create a meaningful word.
Figure 2.

Exercise of the type anagram. (A) Screen appearing when exercise was selected. (B) Solving the exercise using drag and drop on touchscreen. (C) Feedback after incorrect response. (D) Feedback after correct response.
In order to improve language functions effectively, exercises should be adapted to the needs of each patient. Therefore, the scaling of difficulty and classification of exercises is crucial. To classify the exercises, linguistic (eg, semantic similarity between target and distractors) or non-linguistic measures (eg, number of distractors) were considered (table 2).
Computerised adaptive testing algorithm for exercise adjustment
The algorithm, as shown in figure 3, adapts the difficulty level of exercises by analysing whether the present performance exceeds a predefined threshold or not (see online supplemental appendix B for a detailed description).
Figure 3.
Steps of the computerised adaptive testing algorithm used to adapt task difficulty.
bmjopen-2020-037702supp002.pdf (434.6KB, pdf)
In a first step to calculate the performance, data of a single collection are used as input. Afterwards, the algorithm decides whether the collection contains exercises of a specific type that allows for analysis of the performance (eg, word repetition exercises have no valid classification of the response as being correct or false). Data are analysed using the sequential probability ratio test47 and binomial CIs. Criterion-based comparisons indicate the difficulty level of exercises in relation to the patient’s performance and adapt the difficulty level accordingly.
teleCT
Custom-made versions of two casual puzzle video games are used as teleCT: Flow Free (Big Duck Games LLC), a remake of the Numberlink puzzle (Nikoli Co.), and Bejeweled (PopCap Games).48
Flow free
The objective of flow free is to connect same-coloured dots by drawing ‘pipes’ via tap and drag movements in order to create a ‘flow’ in a squared grid (figure 4). A puzzle is solved when the entire grid is covered with non-overlapping flows. Task difficulty is adjusted by grid-size and number of dots.29 49 50 Both puzzles will be played each day with the same duration.
Figure 4.

Procedure of the flow free puzzle game.
Match three
The objective of match three is to swap one gem with one of the cardinally neighboured gems resulting in three or more, vertically or horizontally adjacent, identical gems. Matched gems get repeatedly replaced by new ones until no more matches are possible (figure 5). Task difficulty is adjusted by grid-size, number of gems and possible match patterns.30
Figure 5.
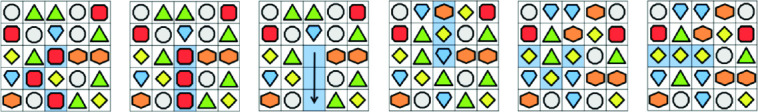
Procedure of the match three puzzle game.
Data collection and management
The ARTORG Center for Biomedical Engineering Research in Bern, which has extensive experience in handling processes for data entry, provides the data management. State-of-the art processes promote data integrity (eg, double data entry, range checks). The ARTORG Center will use one of its web-based electronic data capturing systems (REDCap) to set up the clinical study database.
Data analysis
The planned analysis will include all outcome measures collected throughout the study using linear mixed-effect models including transformation of data if normality assumptions are violated. All variables concerning one outcome will be examined simultaneously in one model. This approach considers the longitudinal nature of the data, numeric variables and the multilevel structure with two superior levels. To analyse the primary objective (eg, whether patients in the experimental group have increased their understandability of verbal communication more than patients in the control group at the end of the intervention), a linear mixed-effect model with ‘group’ as between-subject factor (eg, experimental and control group) and ‘time point’ as within-subject factor (eg, pretest, post-test and follow-up) with an appropriate post-hoc test will be applied. The same analysis will be used for secondary outcome variables. Significant effects will be further analysed by direct comparisons between different groups or different time points using means of post-hoc tests (eg, Holm-Bonferroni correction). Although missing data are expected to be rare, multiple imputation assuming random missing would be used.
Monitoring
A data monitoring committee is not needed because known risks are minor for both interventions.51 In case of adverse events (eg, stroke-related events) due to which participants are withdrawn from the study, the time of onset, duration to resolve, counter measures, as well as the severity of the event and its relation to the study intervention will be recorded and documented. Affected patients will receive paid medical care.
Ethics and dissemination
Ethics
The study will be compliant to the protocol approved by the Ethics Committee Bern (ID 2016-01577, Version 5.0, 11 July 2018) and Ethics Committee Northwest/Central Switzerland. It is also registered in ClinicalTrials.gov (NCT03228264). The study will be carried out in accordance to the protocol and follow the current version of the Declaration of Helsinki, the guidelines of Good Clinical Practice. When protocol amendments are needed (eg, to include another participating centre), ethical approval will be obtained first. After having obtained this approval, relevant adaptations will be made in the relevant clinical trial registry databases.
Dissemination
The study protocol was presented to clinicians and at national conferences. After completing recruitment, according to the inclusion and exclusion criteria, statistical analyses are planned. Obtained results will be submitted to peer-reviewed journals and will be presented at national as well as international scientific congresses. The list and order of authors will be established according to the International Committee of Medical Journal Editors.
Supplementary Material
Acknowledgments
The authors thank Narayan Schütz for his advice with the software and particularly acknowledge Alvin Chesham for providing the adapted version of FreeFlow and Match3 teleCT for this study.
Footnotes
Twitter: @prabithaUrwyler
Contributors: ASU and SMG wrote the first draft of the manuscript. SMG was involved in the development of the teleSLT application. NS, CR and ASU are trained researchers in the current study and populated the database of the Bern Aphasia App. PW, PU and TN drafted the application for ethics approval. SS, CW and MK-B are the involved speech and language therapists and were involved in the conception of the study together with PU, TV, TB, TNy, RM and TN. TNy is the principal investigator at trial site Lucerne, RM, PU are principal investigators at trial site Bern, and TN is the sponsor investigator.
Funding: The present study is partially funded by the Interdisciplinary Grants at the University of Bern (UniBE ID Grants 2018), Switzerland.
Competing interests: SMG was involved in the development of the Bern Aphasia App. NS, CR and ASU were involved in populating (exercises) the Bern Aphasia App.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.WHO Global health estimates 2016: deaths by cause, age, sex, by country and by region, 2000-2016. Geneva: World Health Organisation, 2018. [Google Scholar]
- 2.Engelter ST, Gostynski M, Papa S, et al. Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke 2006;37:1379–84. 10.1161/01.STR.0000221815.64093.8c [DOI] [PubMed] [Google Scholar]
- 3.Brady MC, Kelly H, Godwin J, et al. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev 2016;24:CD000425 10.1002/14651858.CD000425.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dijkerman HC, Wood VA, Hewer RL. Long-term outcome after discharge from a stroke rehabilitation unit. J R Coll Physicians Lond 1996;30:538–46. [PMC free article] [PubMed] [Google Scholar]
- 5.Lam JMC, Wodchis WP. The relationship of 60 disease diagnoses and 15 conditions to preference-based health-related quality of life in Ontario hospital-based long-term care residents. Med Care 2010;48:380–7. 10.1097/MLR.0b013e3181ca2647 [DOI] [PubMed] [Google Scholar]
- 6.Teasell RW, Foley NC, Bhogal SK, et al. An evidence-based review of stroke rehabilitation. Top Stroke Rehabil 2003;10:29–58. 10.1310/8YNA-1YHK-YMHB-XTE1 [DOI] [PubMed] [Google Scholar]
- 7.Code C, Torney A, Gildea-Howardine E, et al. Outcome of a one-month therapy intensive for chronic aphasia: variable individual responses. Semin Speech Lang 2010;31:021–33. 10.1055/s-0029-1244950 [DOI] [PubMed] [Google Scholar]
- 8.Kendall DL, Oelke M, Brookshire CE, et al. The influence of phonomotor treatment on word retrieval abilities in 26 individuals with chronic aphasia: an open trial. J Speech Lang Hear Res 2015;58:798–812. 10.1044/2015_JSLHR-L-14-0131 [DOI] [PubMed] [Google Scholar]
- 9.Breitenstein C, Grewe T, Flöel A, et al. Intensive speech and language therapy in patients with chronic aphasia after stroke: a randomised, open-label, blinded-endpoint, controlled trial in a health-care setting. Lancet 2017;389:1528–38. 10.1016/S0140-6736(17)30067-3 [DOI] [PubMed] [Google Scholar]
- 10.Des Roches CA, Balachandran I, Ascenso EM, et al. Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform. Front Hum Neurosci 2014;8:1015. 10.3389/fnhum.2014.01015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aftonomos LB, Steele RD, Wertz RT. Promoting recovery in chronic aphasia with an interactive technology. Arch Phys Med Rehabil 1997;78:841–6. 10.1016/S0003-9993(97)90197-0 [DOI] [PubMed] [Google Scholar]
- 12.Hoover EL, Carney A. Integrating the iPad into an intensive, comprehensive aphasia program. Semin Speech Lang 2014;35:25–37. 10.1055/s-0033-1362990 [DOI] [PubMed] [Google Scholar]
- 13.Kurland J, Wilkins AR, Stokes P. iPractice: piloting the effectiveness of a tablet-based home practice program in aphasia treatment. Semin Speech Lang 2014;35:51–64. 10.1055/s-0033-1362991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szabo G, Dittelman J. Using mobile technology with individuals with aphasia: native iPad features and everyday apps. Semin Speech Lang 2014;35:5–16. 10.1055/s-0033-1362993 [DOI] [PubMed] [Google Scholar]
- 15.Spaccavento S, Marinelli CV, Nardulli R, et al. Attention deficits in stroke patients: the role of lesion characteristics, time from stroke, and concomitant neuropsychological deficits. Behav Neurol 2019;2019:7835710. 10.1155/2019/7835710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonçalves APB, Mello C, Pereira AH, et al. Executive functions assessment in patients with language impairment a systematic review. Dement Neuropsychol 2018;12:272–83. 10.1590/1980-57642018dn12-030008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brownsett SLE, Warren JE, Geranmayeh F, et al. Cognitive control and its impact on recovery from aphasic stroke. Brain 2014;137:242–54. 10.1093/brain/awt289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fridriksson J, Nettles C, Davis M, et al. Functional communication and executive function in aphasia. Clin Linguist Phon 2006;20:401–10. 10.1080/02699200500075781 [DOI] [PubMed] [Google Scholar]
- 19.Schumacher R, Halai AD, Lambon Ralph MA. Assessing and mapping language, attention and executive multidimensional deficits in stroke aphasia. Brain 2019;142:3202–16. 10.1093/brain/awz258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caplan D, Waters G. Memory mechanisms supporting syntactic comprehension. Psychon Bull Rev 2013;20:243–68. 10.3758/s13423-012-0369-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crotty M, George S. Retraining visual processing skills to improve driving ability after stroke. Arch Phys Med Rehabil 2009;90:2096–102. 10.1016/j.apmr.2009.08.143 [DOI] [PubMed] [Google Scholar]
- 22.Zakariás L, Keresztes A, Marton K, et al. Positive effects of a computerised working memory and executive function training on sentence comprehension in aphasia. Neuropsychol Rehabil 2018;28:369–86. 10.1080/09602011.2016.1159579 [DOI] [PubMed] [Google Scholar]
- 23.Engelhardt PE, Nigg JT, Ferreira F. Executive function and intelligence in the resolution of temporary syntactic ambiguity: an individual differences investigation. Q J Exp Psychol 2017;70:1263–81. 10.1080/17470218.2016.1178785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoo H, Dickey MW. Aging effects and working memory in Garden-Path recovery. Clin Arch Commun Disord 2017;2:91–102. 10.21849/cacd.2017.00122 [DOI] [Google Scholar]
- 25.Nouchi R, Taki Y, Takeuchi H, et al. Brain training game boosts executive functions, working memory and processing speed in the young adults: a randomized controlled trial. PLoS One 2013;8:e55518. 10.1371/journal.pone.0055518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salis C, Hwang F, Howard D, et al. Short-term and working memory treatments for improving sentence comprehension in aphasia: a review and a replication study. Semin Speech Lang 2017;38:29–39. 10.1055/s-0036-1597262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Januth S. Development and Evaluation of a New Tablet Computer Application for the Therapy of Brain-Injured Patients with Aphasia [Master]. Bern: University of Bern, 2015. [Google Scholar]
- 28.Gerber SM, Schütz N, Uslu AS, et al. Therapist-Guided tablet-based Telerehabilitation for patients with aphasia: proof-of-concept and usability study. JMIR Rehabil Assist Technol 2019;6:e13163. 10.2196/13163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nef T, Chesham A, Schütz N, et al. Development and evaluation of Maze-Like puzzle games to assess cognitive and motor function in aging and neurodegenerative diseases. Front Aging Neurosci 2020;12:87. 10.3389/fnagi.2020.00087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chesham A, Gerber SM, Schütz N, et al. Search and match task: development of a Taskified Match-3 puzzle game to assess and practice visual search. JMIR Serious Games 2019;7:e13620. 10.2196/13620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bhogal SK, Teasell R, Speechley M. Intensity of aphasia therapy, impact on recovery. Stroke 2003;34:987–93. 10.1161/01.STR.0000062343.64383.D0 [DOI] [PubMed] [Google Scholar]
- 33.Kaplan EL, Goodglass H, Weintraub S. The Boston naming test. Philadelphia: Lea & Febiger, 1983. [Google Scholar]
- 34.Palmer R, Enderby P, Cooper C, et al. Computer therapy compared with usual care for people with long-standing aphasia poststroke: a pilot randomized controlled trial. Stroke 2012;43:1904–11. 10.1161/STROKEAHA.112.650671 [DOI] [PubMed] [Google Scholar]
- 35.Green CS, Strobach T, Schubert T. On methodological standards in training and transfer experiments. Psychol Res 2014;78:756–72. 10.1007/s00426-013-0535-3 [DOI] [PubMed] [Google Scholar]
- 36.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blomert L, Buslach DC. Amsterdam-Nijmegen Everyday Language Test(ANELT) - Deutsche Fassung. Lisse, The Netherlands: Swets & Zeitlinger, 1994. [Google Scholar]
- 38.Blomert L, Kean ML, Koster C, et al. Amsterdam—Nijmegen everyday language test: construction, reliability and validity. Aphasiology 1994;8:381–407. 10.1080/02687039408248666 [DOI] [Google Scholar]
- 39.Blömer F, Pesch A, Willmes K, et al. Das sprachsystematische Aphasiescreening (SAPS): Konstruktionseigenschaften und erste Evaluierung. Zeitschrift für Neuropsychologie 2013;24:139–48. 10.1024/1016-264X/a000101 [DOI] [Google Scholar]
- 40.De Renzi E, Vignolo LA. The Token test: a sensitive test to detect receptive disturbances in aphasics. Brain 1962;85:665–78. 10.1093/brain/85.4.665 [DOI] [PubMed] [Google Scholar]
- 41.Fastenau PS, Denburg NL, Mauer BA. Parallel short forms for the Boston naming test: psychometric properties and norms for older adults. J Clin Exp Neuropsychol 1998;20:828–34. 10.1076/jcen.20.6.828.1105 [DOI] [PubMed] [Google Scholar]
- 42.Gallaher AJ. Temporal reliability of aphasic performance on the Token test. Brain Lang 1979;7:34–41. 10.1016/0093-934X(79)90004-X [DOI] [PubMed] [Google Scholar]
- 43.Orgass B, Poeck K. Clinical validation of a new test for aphasia: an experimental study on the Token test. Cortex 1966;2:222–43. 10.1016/S0010-9452(66)80005-9 [DOI] [Google Scholar]
- 44.Hilari K, Byng S, Lamping DL, et al. Stroke and aphasia quality of life scale-39 (SAQOL-39). Stroke 2003;34:1944–50. 10.1161/01.STR.0000081987.46660.ED [DOI] [PubMed] [Google Scholar]
- 45.Brooke J. Jordan PW, Thomas B, Weerdmeester BA, et al., SUS-A quick and dirty usability scale. London: Taylor & Francis, 1996: 189–94. [Google Scholar]
- 46.Ryan RM. Control and information in the intrapersonal sphere: an extension of cognitive evaluation theory. J Pers Soc Psychol 1982;43:450–61. 10.1037/0022-3514.43.3.450 [DOI] [Google Scholar]
- 47.Wald A. Sequential analysis. New York: Wiley, 1947. [Google Scholar]
- 48.Chlond MJ. Puzzle-IP satisfied. INFORMS Transactions on Education 2014;14:140–2. [Google Scholar]
- 49.Cunningham R, Alex L, Frederick C. Studying human relatedness through a shared gaming experience. Paper presented at the Proceedings of the Human Factors and Ergonomics Society Annual Meeting, 2015. [Google Scholar]
- 50.Oei AC, Patterson MD. Enhancing cognition with video games: a multiple game training study. PLoS One 2013;8:e58546. 10.1371/journal.pone.0058546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sydes MR, Spiegelhalter DJ, Altman DG, et al. Systematic qualitative review of the literature on data monitoring committees for randomized controlled trials. Clin Trials 2004;1:60–79. 10.1191/1740774504cn004rr [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037702supp001.pdf (105KB, pdf)
bmjopen-2020-037702supp002.pdf (434.6KB, pdf)




