Abstract
Objective
Posttraumatic stress disorder (PTSD) treatment delivery by peer specialist providers could increase access to and engagement with PTSD treatment in low resource settings. The current pilot study tested the feasibility, acceptability, and initial effectiveness of a peer-delivered, brief cognitive behavioral therapy for PTSD.
Method
Four certified peer specialists delivered the intervention to 18 participants with probable PTSD. We assessed PTSD symptoms weekly and administered surveys and interviews at baseline and post-treatment.
Results
Our mixed-methods approach suggests that the intervention was feasible and acceptable, demonstrating high client satisfaction. We also found significant improvements in PTSD, depressive, anxiety, and general stress symptoms.
Conclusions
Peer-delivered interventions may be a good fit for addressing posttraumatic stress symptoms for people accessing care in low resource settings. Future research should evaluate peer-delivered PTSD treatment as a strategy for both reducing symptoms and improving access and engagement in professional care.
Keywords: posttraumatic stress disorder (PTSD), peer delivery, task-sharing, cognitive-behavioral therapy, skills training, urban community, implementation science, feasibility, acceptability, mixed methods
1. Introduction
As many as 94% of low-income, urban primary care patients report exposure to interpersonal violence, with 33% to 46% meeting diagnostic criteria for posttraumatic stress disorder (PTSD; Alim et al., 2006; Gillespie et al., 2009; Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). Yet, only 13% of these patients with PTSD receive any type of behavioral health treatment (Alim et al., 2006). Low access to behavioral healthcare (Institute of Medicine, 2003) is driven by a shortage of behavioral health specialists (Alegría et al., 2007; Dinwiddie, Gaskin, Chan, Norrington, & McCleary, 2013; Lê Cook, McGuire, & Zaslavsky, 2012). Based on national data, the Health Resources and Services Administration (HRSA) and Substance Abuse and Mental Health Services Administration (SAMHSA) estimated a national provider shortage of about 20% of behavioral health service needs in 2013 and predicted shortages of more than 10,000 full-time equivalents (FTEs) for psychiatrists, psychologists, social workers, and other counselors by the year 2025 (HRSA & SAMHSA, 2015), creating barriers to accessing PTSD treatment. Low engagement in behavioral healthcare in low income, urban communities is also common due to high mental health stigma or shame related to receiving mental health treatment (Fox et al. 2012; Próspero & Vohra-Gupta, 2008; Rüsch, Angermeyer, & Corrigan, 2005; Valentine, Dixon, Borba, Shtasel, & Marques, 2016) and mistrust of medical providers or medical models of care (Kaltman, Hurtado de Mendoza, Gonzales, & Serrano, 2014; Valentine et al., 2016).
The use of lay (or “paraprofessional”) counselors has been put forth as one strategy for addressing workforce shortages and mitigating engagement barriers associated with behavioral health stigma and medical mistrust (Ekers, Richards, McMillan, Bland, & Gilbody, 2011). In recent years, there has been increased interest in the use of lay counselors to deliver behavioral health interventions for various physical and behavioral health conditions (Dias et al. 2019; Glenton et al., 2013; Jarero, Rake & Givaudan, 2017; Stanley et al., 2014). A meta-analysis of findings related to the delivery of depression and anxiety interventions by lay counselors found that client outcomes did not differ from those of professional providers (Boer, Wiersma, Russo, & Bosch, 2005). A recent qualitative synthesis of lay-delivered interventions to improve maternal and child physical health symptoms or behaviors indicated that lay health workers were not only effective interventionists, but were preferred by clients over professionals (Glenton et al., 2013). Despite growth in this field of research, the role of the lay counselor in most studies is limited to supplemental support for self-management programs focused on health, functioning, and wellbeing, or for clinician-delivered behavioral health services, rather than as primary interventionists targeting behavioral health symptoms (Chinman, Young, Hassell, & Davidson, 2006; Salzer, Schwenk, & Brusilovskiy, 2010; SAMHSA-HRSA Center for Integrated Health Solutions, 2016; Solomon, 2004).
Peer specialists are a subset of paraprofessionals who are selected for their role because they share a specified type of lived experience with clients. Shared lived experience can mean a match based on age, gender, race, ethnicity, recovery from mental health or substance use conditions, or any other factor relevant to the clinical services provided. Peer specialists work in a wide range of settings and go by a range of titles, such as “peers,” recovery coaches, and community health workers (Salzer et al., 2010). Through mutual and reciprocal helping relationships (Scott, Doughty, & Kahi, 2011; Watson, 2019), peer specialists have the capacity to reduce stigma related to behavioral health (Austin, Ramakrishnan, & Hopper, 2014; Corrigan, Torres, Lara, Sheehan, & Larson, 2017; Davidson, Bellamy, Guy, & Miller, 2012). Traditional peer-led services align with client preferences for person-centered, informal care (Dixon, Holoshitz, & Nossel, 2016), and represent a community-based alternative to professional behavioral health services. Additionally, clients may more readily trust peer providers, thereby facilitating service engagement (Chinman et al., 2008).
Despite the promise of peers and other lay counselors in engaging hard-to-reach clients (Chinman et al., 2008; Chinman et al. 2006), limited research has been conducted in the U.S. to test the ability of peer specialists to deliver manualized behavioral interventions. Expanding this body of research is vitally important given professional provider concerns related to the safety and efficacy of peer specialists as behavioral health care providers (Chinman et al., 2008; Gates & Akabas, 2007). A recent randomized non-inferiority trial tested the effectiveness of a trauma-focused cognitive behavioral group treatment (Seeking Safety) for PTSD and substance use disorder delivered by peer versus professional providers. Both clinicians and peers demonstrated high fidelity to the intervention, and participants in both groups improved similarly in both PTSD symptoms and coping skill use (Crisanti, Murray-Krezan, Reno, & Killough, 2019). In a pilot study, Najavits et al. (2014) also evaluated peer delivery of Seeking Safety, but for trauma-exposed residential patients struggling with substance use, finding high satisfaction and fidelity, as well as positive trauma-related and mental health symptoms, function, and skill use outcomes. One randomized controlled pilot study found that peer delivery of a suicide prevention program was feasible and acceptable in terms of peer specialist fidelity to treatment protocol, participant recruitment and retention, and participant satisfaction (Pfeiffer et al., 2019).
The current study leveraged community-based participatory research (CBPR) strategies to inform the selection and adaptation of an intervention prior to feasibility testing. Our aims extend the research on peer specialist-delivered manualized PTSD treatments by testing preliminary effectiveness of a cognitive behavioral therapy (CBT) intervention while gathering information on implementation process and outcomes. Specifically, we conducted a nonrandomized hybrid 1 effectiveness-implementation pilot trial (Curran, Bauer, Mittman, Pyne, & Stetler, 2012) to (a) assess the initial feasibility and acceptability of and client satisfaction with a peer-delivered manualized treatment for PTSD—Skills Training in Affective and Interpersonal Regulation (STAIR), abbreviated to five sessions for primary care setting (STAIR-PC), and (b) assess the initial effectiveness of the intervention on clinical outcomes (PTSD, depression, anxiety, and general stress) and quality of life.
2. Methods
2.1. Research Setting in Context
As a safety-net hospital, our affiliated medical centers serve a highly diverse population of individuals struggling with low socioeconomic status, housing and food instability, language barriers, and chronic physical and mental health issues and disabilities, with a large proportion of our patients representing historically underserved communities (Health Resources in Action, 2016). A significant percent of patients seen in primary care clinics at our affiliated medical centers report one or more social needs, including housing instability, food insecurity, inability to afford medications, and lack of transportation to medical appointments (Johnson, 2019). We expected our sample to report similar demographics and barriers to care that characterize the population served within the safety-net hospital we recruited from.
2.2. Participant Recruitment and Assessment Procedures
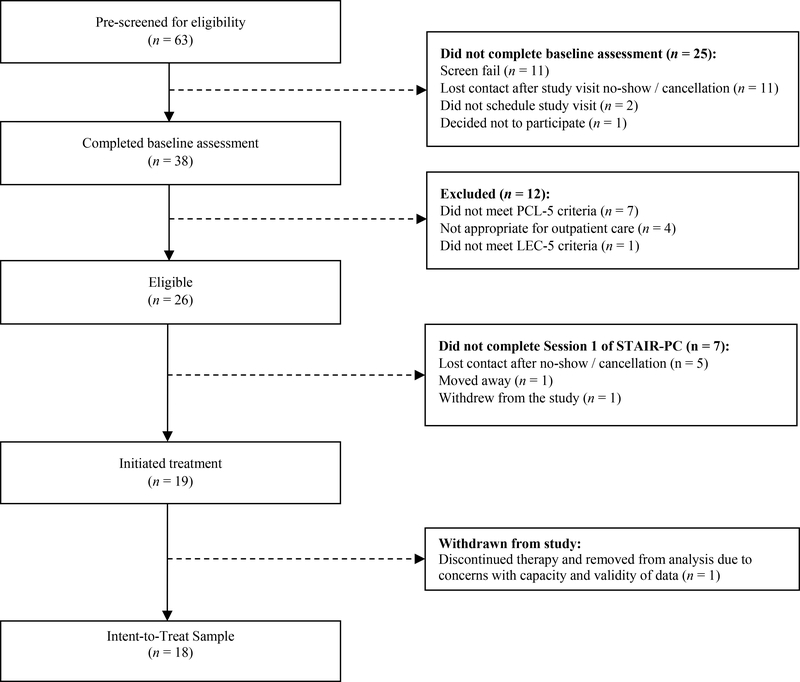
Participants were recruited between July 2018 and April 2019 via flyers distributed by certified peer specialists at our community partner organization—a local peer-led organization overseen by our academic medical center’s department of psychiatry. Peer specialist providers also distributed study flyers during outreach to community-based organizations, including inpatient hospital units, homeless shelters, and outpatient service settings. We also used a departmental registry to reach out to individuals who endorsed an interest in studies related to “stress and trauma.” A total of 19 people received at least one session of STAIR-PC, of whom 18 were included in our final analytic sample; one person’s data were excluded from the analyses due to validity concerns due to onset of psychosis (see Figure 1 for a flow chart presenting participant recruitment, attrition, and inclusion).
Figure 1.
Flow chart of participant recruitment, attrition, and inclusion. PCL-5, Posttraumatic stress disorder Checklist for the DSM-5; LEC-5, Life Events Checklist for the DSM-5; STAIR-PC, Skills Training in Affective and Interpersonal Regulation for Primary Care.
Potential participants were pre-screened by phone using the Primary Care PTSD Screen for the DSM-5 (PC-PTSD-5; Prins et al., 2016). A score of 3 indicates possible PTSD based on symptom endorsement across clusters (intrusions, avoidance, hyperarousal, and cognitive/mood symptoms; Prins et al., 2016). Those who pre-screened positive were invited to an in-person, one-hour baseline visit to obtain written informed consent, and complete surveys and an audio-recorded interview. During this visit, inclusion criteria were further verified by a licensed psychologist (senior author, SEV). We intentionally utilized broad inclusion and narrow exclusion criteria so that our sample most closely resembles clients typically served by our peer specialists. Study inclusion criteria were as follows: (a) endorsement of at least one potentially traumatic event (PTE), as assessed by the Life Events Checklist for the DSM-5 (LEC-5; Weathers et al., 2013a); (b) self-report of current elevated PTSD symptoms, indicated by scoring greater than or equal to 33 (U.S. Department of Veterans Affairs, 2019) on the PTSD Checklist for the DSM-5 (PCL-5; Weathers et al., 2013b) or by re-evaluation and clinical judgement of SEV that client would benefit from PTSD treatment; (c) 18 years of age or older; and (d) participant judgment of their ability to engage in treatment in English. Participants were excluded if (a) they needed a higher than outpatient level of care (i.e., treatment in detox, inpatient, or residential settings) based on clinician (SEV) judgment; or (b) they were unable to provide informed consent without a legally appointed representative present.
If all eligibility criteria were met, participants were assigned to a certified peer specialist based on scheduling availability and participant preferences for the peer specialist’s gender. Participants then received the STAIR-PC intervention, which includes five 45- to 60-minute therapy sessions. We aimed to schedule these weekly, but were flexible. Participants completed a second one-hour study visit after completing STAIR-PC during which they were again asked to complete surveys and an audio-recorded interview.
All study visits and therapy sessions took place in a clinical research unit. Participants were compensated for baseline and post-treatment study visits, but not for therapy sessions. All procedures were approved by the Institutional Review Board at the affiliated university, and conducted in compliance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) and the National Institute of Health. Informed consent was obtained from participants after study staff explained study procedures.
2.2. Skills Training Intervention for Peer Delivery
The original version of STAIR is an empirically-supported and face-valid intervention for PTSD that has demonstrated effectiveness (Cloitre et al., 2010; Cloitre, Koenen, Cohen, & Han, 2002), when delivered in safety-net settings (Trappler & Newville, 2007) and by non-specialists (MacIntosh, Cloitre, Kortis, Peck, & Weiss, 2016). By emphasizing self-care, coping skills, and client-driven goal setting, STAIR features an approach that particularly fits the needs of those experiencing symptoms of PTSD (Charuvastra & Cloitre, 2008), and seems to align with the type of support our peer specialists already provide through group work (i.e., teaching coping skills).
STAIR was recently abbreviated to improve implementation in VA primary care (STAIR-PC; Jain et al., in press). STAIR-PC is an individual, 5-session, low-intensity, CBT intervention for PTSD that focuses on functional improvement in emotion regulation and interpersonal effectiveness skills, and does not require clients to revisit the trauma memory. General session format includes review of weekly PCL-5, interactive psychoeducation, coping skill demonstration, and homework setting. STAIR-PC utilizes the three-channel conceptualization of emotion regulation (i.e., emotion, thought, and behavior channels) to structure the incorporation of coping skills throughout the program, and integrates skills relying on cognitive reappraisal, behavioral activation, mindfulness, and distress tolerance for each channel (Jain et al., in press).
Pilot data from a randomized controlled trial at the VA suggest that veterans engaged in STAIR-PC (n = 13) demonstrated significant improvements in PTSD symptoms, depressive symptoms, emotion regulation, and social engagement with moderate to large effect sizes, while those referred to brief psychotherapy and/or medication management (n = 13) did not show improvements. Thirteen providers, ranging from licensed psychologists or social workers to psychology technicians or care coordinators, delivered STAIR-PC as part of this VA trial (Jain et al., in press).
2.3. Overview of Community-based Participatory Procedures
In November 2017, we began meeting with the five members of the executive leadership team of the peer-led service organization who oversee the training and implementation of programming by peer specialists. The executive team served as a working group to assist with intervention selection and to advise adaptations to the manual prior to the trial. We hosted a series of meetings, where we presented and received feedback. Topics included 1) overview of manualized treatments for PTSD, including presentation of various interventions—resulting in the selection of STAIR-PC as the perceived best fit; 2) nomination of certified peer specialists within the organization who they believed were a good fit as study interventionists; 3) presentation of details of the STAIR-PC intervention to identify needed adaptations; 4) presentation of a summary of pre-training interviews with certified peer specialists (manuscript submitted for publication); 5) proposal and approval of any additional changes to the manual prior to trial; and 6) presentation of the modified STAIR-PC manual, tailored to the peer model (e.g., reduction in literacy level, simplification of educational materials, removal of clinical language that could be perceived as pathologizing). The above topics are further discussed in a forthcoming publication (manuscript submitted for publication). The executive team was also helpful in monitoring study progress and interpreting findings.
2.4. Provider Characteristics & Training
For our study, peer specialists were individuals who 1) endorsed having lived experience with mental health or substance use conditions; 2) reported exposure to at least one potentially traumatic event; 3) were employed as a certified peer specialist by our partner peer-led organization; and 4) engaged in STAIR-PC training and consultation. Peer specialist providers’ average age was 64.25 years (SD = 8.06) and a majority identified as men (75%). Two peer specialist providers had graduate-level education and the other two attended some college but did not receive a degree; none were practicing therapists. All four peer specialist interventionists had completed the state-wide peer specialist certification program (The Transformation Center, 2020) offered by a Department of Mental Health (DMH)-affiliated institution called The Transformation Center. The certification program is a series of courses designed to enhance trainees’ peer support skills, for example those related to recovery-oriented mental health care, cross-cultural competency, group facilitation and self-help, and disclosure of their recovery narrative (The Transformation Center, 2020). Peer specialists employed by our partner organization frequently run skills-based groups, one example being Wellness Recovery Action Planning (WRAP) courses that teach skills on self-management to promote recovery from mental health symptoms (Copeland, 2002).
All four certified peer specialists received a one day, 5-hour didactic training in STAIR-PC, which was facilitated by two licensed psychologists, including the principal investigator (senior author, SEV) and a certified national trainer in STAIR-PC (Dr. Christie Jackson). Weekly group consultation was provided by SEV for the duration of STAIR-PC implementation. Consultation focused on review of formal (written) feedback that highlighted specific examples of strengths and weaknesses of the peer specialist’s delivery of that session. Consultation also included supplemental training on topics such as case conceptualization, PTSD diagnosis and other treatment approaches, managing difficult clients, and targeting avoidance in sessions. Full detail on our approach to consultation and feedback is detailed elsewhere (manuscript submitted for publication).
2.3. Measures
2.3.1. Demographic and Sample Characteristics
Participants completed a demographic questionnaire that asked about their age, gender, race, and education level. In addition, participants completed the Health Services Utilization Form (HSUF) that was adapted from the National Latino and Asian American Survey (Alegría et al., 2004). The HSUF assessed for prior experiences with behavioral health services including utilization of psychiatric medication, therapy, CBT or dialectical behavioral therapy, and recent psychiatric hospitalization. Lifetime exposure to childhood or adulthood psychological abuse was assessed using the psychological abuse subscale of the Abuse Assessment Screen (Parker & McFarlane, 1991). Participants also self-reported the behavioral diagnoses they had received from a professional provider.
Consumer Experiences of Stigma Questionnaire (CESQ)
We used the 9-item stigma subscale of the Consumer Experiences of Stigma Questionnaire (CESQ; Wahl, 1999) to characterize our samples’ experiences of perceived behavioral health stigma. Items assessed participants’ stigmatizing experiences (e.g., “I have been shunned or avoided when it was revealed I am a consumer”). Scores range from 1 to 5 (never to very often) with higher scores indicating more frequent stigmatizing experiences. Following Dickerson, Sommerville, Origoni, Ringel, & Parente (2002), we modified the wording of the original measure for clarity based on advice from the workgroup, replacing “consumer” with “person served.”
2.3.2. Exposure to PTEs
Life Events Checklist for the DSM-5 (LEC-5)
The LEC-5 (Weathers et al., 2013a) was used to assess exposure to PTEs. Participants indicate what level of exposure (i.e., experienced, witnessed, or learned about) they experienced on a 6-point Likert scale for a total of 16 events. Although psychometric properties are not yet available for the LEC-5, the very similar previous version (based on the DSM-IV) has shown temporal stability and strong test-retest reliability (r = 0.82, p < 0.001; Gray, Litz, Hsu, & Lombardo, 2004).
2.3.3. Effectiveness Outcomes
PTSD Checklist for the DSM-5 (PCL-5)
We used the PCL-5 (Weathers et al., 2013b) to assess for PTSD symptoms. The measure includes 20 items that map onto DSM-5 criteria. Items are anchored to an index (Criterion A) event, as recommended by evaluations of past versions of the PTSD Checklist (Blevins, Weathers, Davis, Witte, & Domino, 2015). Items are assessed with a 5-point Likert scale (not at all to extremely) with a possible total score range of 0 to 80. We used a score of 33 or greater as our clinical cut off and a 10-point drop in total score as an indicator of clinically meaningful improvement (U.S. Department of Veterans Affairs, 2019). The PCL-5 includes four subscales per the DSM-5 symptom clusters for PTSD, including intrusion (5 items), avoidance (2 items), negative thoughts and feelings (7 items), and hyperarousal (6 items). The PCL-5 has been validated in a sample of individuals experiencing severe mental illness (SMI) with good-to-excellent internal consistency (α = 0.72 – 0.94), moderate-to-good test-retest reliability (ICC = 0.66), and moderate-to-good convergent validity with a gold-standard clinician-administered diagnostic interview for PTSD (κ = 0.67 – 0.85, 83% - 93% agreement; Mueser et al., 2001). In the current study, the PCL-5 demonstrated good internal consistency across time points (α = 0.88).
Depression, Anxiety, Stress, Scale-21 (DASS-21)
We used the 21-item Depression, Anxiety, Stress Scale (S. Lovibond & P. Lovibond, 1995) to measure depression, anxiety, and stress symptoms. Each item is assessed on a 4-point Likert scale. Scores on the DASS-21 range from 0 to 42 for each subscale with higher scores indicating greater symptoms. Score less than 9 on the depression subscale (7 items) indicate normal level, scores between 9 and 21 indicate outpatient level, and scores greater than 21 indicate inpatient level. For the anxiety subscale (7 items), scores less than 6 indicate normal level, scores between 6 and 14 indicate outpatient level, and scores greater than 14 indicate need inpatient. For the stress subscale (7 items), scores less than 12 indicate normal level, scores between 12 and 21 indicate outpatient level, and scores greater than 21 indicate inpatient level (Ronk, Korman, Hooke, & Page, 2013). The DASS-21 has shown adequate validity and reliability in a general adult population (α = 0.88 – 0.93; Henry & Crawford, 2005). In the current study, the DASS-21 including all subscales demonstrated good internal consistency (α = 0.87). The DASS-21 depression and stress subscales demonstrated good internal consistency (α = 0.88 and .074, respectively), while the anxiety subscale demonstrated poor internal consistency (α = 0.57).
Schwartz Outcome Scale-10 (SOS-10)
We used the 10-item Schwartz Outcome Scale (Blais et al., 1999) to measure of quality of life. Items are scored on a 7-point Likert scale with higher scores indicating greater quality of life. The SOS-10 includes items that assess psychological (e.g., “I feel hopeful about my future”) and physical well-being (e.g., “Given my current physical condition, I am satisfied with what I can do”). The SOS-10 has shown good reliability and validity in samples of inpatients, outpatients, and nonpatients (α = 0.96; Blais et al., 1999). In the current study, the SOS-10 demonstrated excellent internal consistency (α = 0.93).
2.3.5. Implementation Process and Outcomes
Feasibility
Feasibility was assessed using participant attendance and retention rates, as well as certified peer specialist fidelity to the intervention manual. All therapy sessions were reviewed to rate adherence and competence. STAIR-PC included session checklists to track adherence to the protocol. A percentage of adherence was calculated by dividing the components completed in session by the peer specialist by the total number of components listed in the session checklist. Competence assessed by the Cognitive Therapy Scale-Revised (CTS-R; Blackburn, et al., 2001). Study staff reviewed therapy sessions to calculate adherence and rate competence. Adherence and competency were double-coded by two raters until consensus was reached. Once raters attained an average inter-rater reliably above 75%, sessions were reviewed by only one rater.
Acceptability
Acceptability is the perception that an intervention is satisfactory, agreeable, or palatable, as evaluated based on its content, complexity, or comfort, to stakeholders (Proctor et al., 2011), We assessed participant acceptability related to the intervention by analyzing audio-recorded, semi-structured interviews conducted with clients at baseline and post-intervention (provider acceptability is published elsewhere; manuscript submitted for publication). Interviews at both time points were approximately 30 minutes in length. During the baseline interview, participants were asked open-ended questions related to their motivation for participating in the program and how they felt about receiving an intervention delivered by a peer specialist rather than a professional. The post-intervention interview included open-ended questions pertaining to perceived benefits or harms of the intervention, overall satisfaction, and recommendations for intervention improvement. To aide in further adaptations, participants were asked which skills they found most/least helpful and for any other feedback that could help us improve peer-delivered STAIR-PC. Interviews were transcribed, de-identified, and verified for accuracy by study staff. Qualitative analysis is described in later sections.
Client Satisfaction Questionnaire-8 (CSQ-8)
As a quantitative measure of acceptability, we assessed service satisfaction using the Client Satisfaction Questionnaire-8 (CSQ-8; Larsen, Attkisson, Hargreaves, & Nguyen, 1979), which includes 8-items eliciting opinions on a delivered service/intervention (e.g., “How would you rate the quality of the service you received?”). Items on the CSQ-8 are on a 1 to 4 Likert scale with the total score ranging from 8 to 32, and higher scores indicating greater satisfaction. The CSQ-8 has shown good reliability and validity in samples of urban behavioral health center patients (α = 0.91; Attkisson & Zwick, 1982) and general therapy patients (α = 0.93; Nguyen, Attkisson, & Stegner, 1983). Mean satisfaction scores for samples similar to ours range from 24.2 to 27.1 (Attkisson & Zwick, 1982; Nguyen, Attkisson, & Stegner, 1983).
2.4. Data Analysis
2.4.1. Quantitative
Data were analyzed using SPSS version 24 (IBM Corp., 2016). Results from the intent-to-treat (N = 18) and per-protocol sample (N = 17) were compared and no significant differences were found, so the intent-to- treat sample was used for analyses. To assess the normality of the data, skewness and kurtosis were examined. The data was not normally distributed for the total number of events on the LEC-5, baseline and post-intervention DASS-21 scores, and CSQ-8. Cronbach’s alphas were calculated to demonstrate the internal consistency of the measures utilized. Descriptive statistics were calculated for all variables. Due to the small sample size and lack of normality, non-parametric Wilcoxon signed-rank tests were used to compare measures assessed at baseline and post-intervention (including the PCL-5, DASS-21, and SOS-10). In addition, Friedman’s test was used to analyze change in PCL-5 score across seven time points (including baseline, sessions 1–5, and post-intervention), and post-hoc Wilcoxon signed-rank tests were conducted to assess at which time point the change in PCL-5 score became significant.
2.4.2. Qualitative
Baseline and post-intervention participant interview transcripts (n = 36) were coded using thematic analysis (Bernard, 2006; Hsieh & Shannon, 2005). Two study staff created initial coding categories derived directly from the same set of transcripts (Hsieh & Shannon, 2005), and met consistently while reviewing transcripts to discuss discrepancies and create new codes if necessary. This process continued until saturation was reached (at n = 10 [5 baseline & 5 post-intervention interviews]). A preliminary codebook was agreed upon. In cases where new themes arose in interviews after the preliminary codebook was created, new coding categories were added and staff re-coded previously coded transcripts using the revised codebook. Once achieving an inter-rater reliability above 80%, subsequent transcripts were coded independently, aside from those double-coded to calculate inter-rater reliability. Study staff double-coded 22.2% (n = 8) of participant interviews (n = 36) and achieved an inter-rater reliability rate above 80% for each transcript (M = 93.2%). Discrepancies within the double-coded transcripts were then reviewed, and a consensus was reached by a third rater. Lastly, codes were reviewed for accuracy and collapsed (if co-occurring). Themes were organized using axial coding in which related codes were grouped and nested within major categories to reflect themes about the program’s feasibility, acceptability, and initial effectiveness. Study staff utilized NVivo 12 (QSR International, 2018) for qualitative data management.
3. Results
3.1. Sample Characteristics
The intent-to-treat sample included 12 (66.7%) women and 13 (72.2%) participants who identified themselves as a race other than White. The mean age of the sample was 51.11 (SD = 9.80). Additionally, all participants endorsed having previous therapy, 13 (72.2%) reported an inpatient hospitalization in their lifetime, and 16 (88.9%) endorsed being prescribed psychiatric medication. See Table 1 for additional details.
Table 1.
Sample characteristics (N=18)
| n (%) | |
|---|---|
| Sex | |
| Female | 12 (66.7) |
| Male | 6 (33.3) |
| Age (Mean ± SD) | 51.11 ± 9.80 |
| Race | |
| White | 5 (27.8) |
| Black or African American | 8 (44.4) |
| Asian | 1 (5.6) |
| American Indian or Alaskan Native | 1 (5.6) |
| Other | 3 (16.7) |
| Ethnicity | |
| Hispanic or Latino | 1 (5.6) |
| Not Hispanic or Latino | 17 (94.4) |
| Education | |
| Attended some college or higher | 14 (77.8) |
| Completed high school or GED | 2 (11.1) |
| Attended high school, but did not receive diploma | 2 (11.1) |
| Lifetime inpatient stay | |
| Yes | 13 (72.2) |
| No | 5 (27.8) |
| Lifetime inpatient stay for emotional problems related to “trauma” | |
| Yes | 12 (66.7) |
| No | 6 (33.3) |
| Contact with a therapist | |
| Yes | 16 (88.9) |
| No | 2 (11.1) |
| Previous therapy | |
| Yes | 18 (100) |
| Previous CBT or DBT | |
| Yes | 11 (61.1) |
| No | 7 (38.9) |
| Prescribed psychiatric medication | |
| Yes | 16 (88.9) |
| No | 2 (11.1) |
Abbreviations: CBT, cognitive-behavioral therapy; DBT, dialectical-behavioral therapy; GED, general education diploma; SD, standard deviation.
Depressive disorders were the most commonly self-reported diagnosis received from a provider (n = 14; 77.8%), followed by trauma and stressor-related disorders (n = 11; 61.1%), and anxiety disorders (n = 10; 55.6%). Additionally, 13 (72.2%) participants reported receiving multiple diagnoses, with an average of 4.5 diagnoses (SD = 4.38). Eight (44.4%) participants reported receiving a diagnosis of a psychosis-related or bipolar disorder. The average number of PTEs endorsed was 5.56 (SD = 2.09). The most commonly reported events were physical assault (n = 15; 83.3%), other unwanted sexual experience (n = 13; 72.2%), and sexual assault (n = 12; 66.7%). Additionally, 12 (66.7%) participants reported experiencing childhood emotional or psychological abuse, and 14 (77.8%) reported adult emotional or psychological abuse. See Table 2 for the full list of PTEs endorsed and their respective proportions.
Table 2.
Rates of exposure to potentially traumatic events and psychological abuse (N=18)
| Participant exposure | |
|---|---|
| Potentially traumatic events (PTEs) | n (%) |
| Physical assault | 15 (83.3) |
| Other unwanted sexual experience | 13 (72.2) |
| Sexual assault | 12 (66.7) |
| Assault with a weapon | 10 (55.6) |
| Transportation accident | 10 (55.6) |
| Any other very stressful experience | 9 (50.0) |
| Sudden violent deatha | 7 (38.9) |
| Life threatening illness or injury | 6 (33.3) |
| Severe human suffering | 6 (33.3) |
| Captivity | 4 (22.2) |
| Fire or explosion | 3 (16.7) |
| Serious accident at home, work, or during recreation | 2 (11.1) |
| Sudden accidental deatha | 2 (11.1) |
| Natural disaster | 1 (5.6) |
| Serious harm, injury, or death you caused to someone else | 1 (5.6) |
| Combat | 0 (0.0) |
| Exposure to toxic substance | 0 (0.0) |
| Number of PTEs endorsed on the LEC-5 (Mean ± SD) | 5.56 ± 2.09 |
| Childhood emotional/psychological abuseb | 12 (66.7) |
| Adult emotional/psychological abuseb | 14 (77.8) |
Note: PTE exposure is based on participant endorsement of experiencing item on the Life Events Checklist for the DSM-5 (LEC-5) unless otherwise noted.
Includes participant endorsement of witnessing item
Emotional/psychological abuse is measured by participant endorsement of the psychological abuse item on the Abuse Assessment Scale (AAS; Parker & McFarlane, 1991) asked across two time periods (before and after 18th birthday).
Abbreviations: PTE, potentially traumatic event; LEC-5, Life Events Checklist for the DSM-5; SD, standard deviation.
Participants’ experiences of perceived behavioral health stigma were examined as a sample characteristic. At baseline participants reported an average score of 2.70 (SD = 0.66) on the CESQ indicating that they “seldom” (2) or “sometimes” (3) encountered stigmatizing experiences as behavioral health service consumers. Per item average values reported by participants are similar to those found in clinical samples (Wahl, 1999; Dickerson et al., 2002).
3.2. Effectiveness Outcomes
3.2.1. PTSD Symptoms
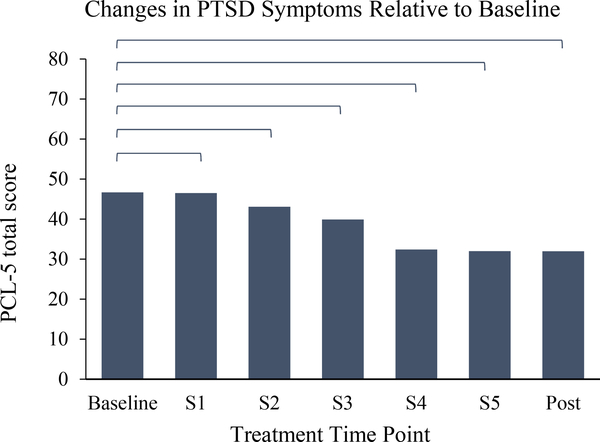
The mean PCL-5 score was 46.67 (SD = 14.47) at baseline and 31.94 (SD = 20.97) at post-intervention for the intent-to-treat sample. There was a statistically significant improvement between baseline and post-intervention PCL-5 scores (z = −3.15, p < .001) as seen in Table 3. Additionally, there were significant improvements on all subscales of the PCL-5 including intrusion (z = −2.92, p < 0.01), avoidance (z = −2.51, p < 0.05), negative thoughts and feelings (z = −2.38, p < 0.05), and hyperarousal (z = −3.01, p < 0.01). Median and range statistics are reported in Table 3, along with results from the baseline to post-intervention Wilcoxon signed-rank analyses. Results of the Friedman’s test (Figure 2) revealed a significant decrease in PTSD symptoms across time points (χ2 = 37.07, df = 6, p = < .001). Post-hoc tests showed that significant improvements in PTSD symptoms were seen by session three (z = −2.42, p < 0.05) and maintained until post-intervention (z = −3.15, p < 0.01). The average change in PCL-5 score was 14.72 (SD = 15.28862, Mdn = 19.00, range = −18.0 – 43.0). Twelve (66.7%) participants attained clinically meaningful improvement as indicated by a 10 point or higher decrease in PCL-5 score between baseline and post-intervention assessments (U.S. Department of Veterans Affairs, 2019). Of note, one participant’s scores showed an 18-point increase in PCL-5 score pre-post. Relative to all other participants, this person only attended two sessions of STAIR-PC before being referred out for a higher level of care (i.e., in need of substance use detox). After stabilizing, this participant returned to complete the post-implementation assessment and interview based on their engagement in the two sessions they completed, but was unable to complete the remaining STAIR-PC sessions due to end of study.
Table 3.
Summary of Wilcoxon signed-rank analyses evaluating baseline to post-intervention change in outcome assessments (N=18)
| Measure | Pre-Intervention | Post-Intervention | Wilcoxon Signed-Rank | |||
|---|---|---|---|---|---|---|
| Median | Range | Median | Range | Z | p | |
| PCL-5 | ||||||
| Intrusion | 11.0 | 7 – 20 | 7.50 | 0 – 20 | −2.92 | 0.004 |
| Avoidance | 6.00 | 3 – 8 | 4.00 | 1 – 8 | −2.51 | 0.012 |
| Negative thoughts and feelings | 16.0 | 0 – 28 | 9.00 | 0 – 28 | −2.38 | 0.017 |
| Hyperarousal | 13.0 | 8 – 24 | 7.50 | 0 – 24 | −3.01 | 0.003 |
| Total score | 44.0 | 27 – 80 | 28.5 | 9 – 80 | −3.15 | 0.002 |
| DASS-21 | ||||||
| Depression | 23.0 | 2 – 40 | 13.0 | 0 – 40 | −2.88 | 0.004 |
| Anxiety | 21.0 | 6 – 36 | 14.0 | 0 – 32 | −2.84 | 0.005 |
| Stress | 23.0 | 10 – 40 | 17.0 | 2 – 34 | −2.57 | 0.010 |
| SOS-10 | 27.0 | 9 – 58 | 30.0 | 10 – 60 | −1.09 | 0.276 |
Abbreviations: PCL-5, Posttraumatic Stress Disorder Checklist for the DSM-5; DASS-21, Depression Anxiety Stress Scales-21 item version; SOS-10, Schwartz Outcome Scale; CESQ, Consumer Experiences of Stigma Questionnaire.
Figure 2.
Changes in PTSD symptoms relative to baseline. PTSD, Posttraumatic stress disorder; PCL-5, PTSD Checklist for the DSM-5; S1, session 1; S2, session 2; S3, session 3; S4, session 4; S5, session 5; Post, post-assessment.
* p<0.05
** p<0.01
3.2.2. Depression, Anxiety, and Stress Symptoms
Significant improvements were seen for the DASS-21 depression subscale from baseline (M = 20.33, SD = 11.63) to post-intervention (M = 14.78, SD = 12.67; z = −2.88, p < 0.01), anxiety subscale from baseline (M = 21.0, SD = 8.124) to post-intervention (M = 14.11, SD = 8.55; z = −2.84, p < 0.01), and stress subscale from baseline (M = 23.56, SD = 8.133) to post-intervention (M = 17.44, SD = 9.79; z = −2.57, p < 0.01) as seen in Table 3.
3.2.3. Quality of Life
Between baseline (M = 30.94, SD = 14.48) and post-intervention (M = 32.83, SD = 14.56) there was not a significant improvement in quality of life (z = −1.09, p = 0.276) as seen in Table 3.
3.3. Implementation Outcomes
3.3.1. Feasibility
Overall, certified peer specialists demonstrated high adherence (M = 93.7%; SD = 12.3%) to intervention session checklists. On average, peer specialists demonstrated adequate competence assessed by the Cognitive Therapy Scale-Revised (CTS-R; Blackburn, et al., 2001; M = 3.70; SD = 0.508).
Of the intent-to-treat sample (N = 18), 17 (94.4%) completed the intervention. On average participants completed the five sessions in 6.98 weeks (SD = 2.47) despite the expected completion time of 5 weeks. The maximum amount of time it took for a participant to complete the five sessions was 12.29 weeks and the minimum was 3.43 weeks. Out of 106 scheduled sessions, 14 (13.2%) sessions did not occur due to a participant no-show. This is less than half of typical no-show rates (31%) reported by socio-demographically similar outpatient behavioral health clinics (Gajwani, 2014).
3.3.2. Acceptability
Client satisfaction
The average score on the CSQ-8 was 25.6 (SD = 5.98) which is similar to levels of satisfaction in populations such as general therapy patients (Nyguen, Attkisson, & Stegner, 1983) and those served by a community behavioral health center (Attkisson & Zwick, 1982). This suggests that the intervention was comparably acceptable to care received in similar settings.
Interview themes
Overall, themes pulled from interviews with participants suggest that they found the intervention acceptable. Sixteen (88.9%) participants reported they would recommend the program to friends or family. Participants mentioned improvements in a wide variety of areas, including PTSD symptoms, emotion regulation, relationships/interpersonal skills, coping, general functioning, confidence, hope, self-care, stress, anger management, happiness, and depression symptoms.
As one participant described,
“The fog of depression seems to have left. [...] It’s like I’m getting hopeful again, […] re-energized, enthusiastic about life. [...] It’s teaching me that I can be selective about what I put my attention to, and I want to put my attention to something that’s helpful, constructive. […] You know, when the astronaut gets out of his spacesuit, and- and is just being a regular person. I feel like I’m letting go, and I’m climbing out of that which has kept me from moving forward.” (63-year-old woman)
Similarly, another participant noted,
“I mean, my symptoms are still there but I mean, I’m more aware of them. […] When I’m starting to feel a certain way, I know- I immediately assess my surroundings, and determine do I want to take a different route or do I want to try to cope through it? […] I’m more willing to try coping skills before I merely run away […] it makes me more willing to stay within, like- stay within an environment I wouldn’t normally want to stay in.” (50-year-old man)
Participants described how they saw the intervention as helpful for depression and anxiety as well as PTSD, as one participated stated,
“I feel like this program would be a lot, um—it would work on people’s, not only just PTSD, but like depression and anxiety and like all the other stuff that’s going within a person’s life and what’s going on externally and internally. […] Cause this is all a mental health situation. […] A mental and physical health situation.” (33-year-old woman)
Interestingly, some participants noticed an initial increase in PTSD symptoms, but said that the skills presented in the program helped them manage these symptoms. As one participant put,
“It stirred up a lot of stuff […] and you know I’ve lost sleep, had nightmares again, but at least I know how to handle it […] I know I had to open the wound to learn how to apply first aid.” (59-year-old woman)
In terms of the intervention content, participants liked that the intervention was present-focused and trauma-focused:
“And the techniques, you know, the […] current-day approach as opposed to, um, digging up the past […] that’s what’s important to me right now […] I have to move forward.” (63-year-old woman)
“Here we just focus on the… PTSD- and there [in supportive therapy] I can focus on all kinds of stuff with her [therapist], but here it’s just, you know, that and I- I’m glad I dealt with just that [PTSD], because I needed to, for me […] to grow and heal.” (51-year-old woman)
All but one participant reported find the skills useful and practical. Participants mentioned one or two skills they did not understand or that could have been explained better by their certified peer specialist. Several participants also expressed that even if they already knew the skill, learning it as part of the intervention reinforced skill use. Most participants mentioned at least one skill they used regularly.
One participant was particularly eloquent when describing how various skills in the program helped him cope:
“I was able to apply a lot of things we learned, especially the, um, evidence technique, where I was able to identify what the real issues are and not just what I’m imagining is going on, and trying to you know rise above them, and other things like that, as well as the thought shifting. […] Actually, out of the behaviors it was basically taking a break. It helped me take a break and just sit back and then once I’ve accomplished that I could then look at my thoughts, and kind of work on what’s really bothering me, as opposed to what I’m feeling, you know, trying to get to the root of the emotions […] And it’s nice to have tools I can use that will actually get me to that level.” (50-year-old man)
Overall, the themes drawn from our analysis of interviews with participants suggests that the peer-delivered intervention had high acceptability, generally and in terms of skills usability, and has the potential to improve mental health symptoms and functioning. Participants recommended a few recommendations for intervention improvement, which primarily focused on providing more in-depth explanations of skills.
4. Discussion
4.1. Main Findings
We aimed to test the feasibility and acceptability of a brief, peer-delivered CBT intervention for PTSD, and to examine the initial effect of the intervention on clinical outcomes. Our findings suggest that peer delivery of STAIR-PC for PTSD is feasible and acceptable to participants, as evidenced by high client retention (94.4% of the intent-to-treat sample completed all 5 sessions), high therapist fidelity to the intervention (93.7% overall adherence), and positive feedback in post-treatment interviews. Despite some recommendations for improvement, participants reported high satisfaction with the intervention based on survey and interview feedback and commented on symptom and functional improvements. We also found preliminary support for the intervention’s clinical effectiveness with regard to PTSD, depressive, anxiety, and general stress symptoms. Surprisingly, we found no improvements in overall quality of life.
Similar to evidence provided by Crisanti et al. (2019), we found that a peer-delivered trauma-focused CBT intervention significantly improved PTSD symptoms. In fact, we found greater improvements in PTSD symptoms in our study compared to those found in the peer-delivered arm of Crisanti et al.’s (2019) study (z = −2.24, p < .05). Our mixed methods evaluation takes the field a step closer to real-world implementation of peer-delivered interventions. Specifically, our study deployed a CBPR strategy to adapt an intervention for peer-delivery, and our peers were directly involved in the development of best practices for implementation. Qualitative interviews with participants were also incredibly helpful in understanding how the intervention led to improvements in overall behavioral health symptomatology, coping, and engagement in services. Our study extends previous findings suggesting that peer specialists can deliver structured interventions with adequate fidelity (Crisanti et al. 2019; Najavits et al., 2014; Pfieffer et al., 2019), and good clinical outcomes (Crisanti et al. 2019; Najavits et al. 2014). Together, this body of research suggests that concerns related to the safety of peer-delivered interventions to high-risk populations (e.g., those struggling with trauma-exposure and substance use [Crisanti et al. 2019, Najavits et al. 2014], suicide risk [Pfieffer et al., 2019], or homelessness [Crisanti et al., 2019]) may be unwarranted.
Our results suggest that peer-delivered, brief, trauma-focused treatment may be a good fit for clients served in our urban academic medical center. As noted earlier, our research procedures were implemented within the department of psychiatry in a safety-net hospital that serves a highly diverse population of individuals struggling with financial, housing, and food insecurity, as well as chronic physical and mental health issues and disabilities (Health Resources in Action, 2016; Johnson, 2019). Therapy session review and discussions in consultation suggested that our participants were similar to those typically served at our hospital as they reported concurrently managing (a) chronic physical health conditions, and (b) significant ongoing or current external stressors, such as housing instability, substance use, and domestic violence, although we did not assess these systematically.
Participants in our study reported exposure to multiple PTEs (an average of 5 to 6 types). Our sample also seems to be characterized by high rates of SMI (psychotic or bipolar disorders), depression, anxiety, and substance use disorder, although it should be noted that this data was self-reported by participants and not verified in participants’ medical records. Most participants experienced improvements in PTSD, depression, anxiety, and stress symptoms. Therefore, the significant improvements we found in our sample suggest that 1) clients with multiple or repeated PTEs and those representing the clinically complex populations typically served in safety-net hospitals may benefit from a low-intensity approach to treatment, 2) stability in terms of socioeconomic resources, comorbid symptomatology, and ongoing trauma exposure may not be necessary to effectively treat PTSD symptoms, 3) peer-delivered services may be safe and beneficial for these populations, and 4) since significant PTSD symptoms improvement began at session 3, participants may receive benefits from brief interventions like this, even if they are unable to complete all sessions. Of note, the participant who only completed two sessions did become significantly worse based on the 10-point marker for clinical meaningful change. However, this participant completed only two sessions, because they required a higher level of care (i.e., detox for alcohol use) and also needed to resolve housing stability concerns. We maintained contact with this participant, connected them to treatment and housing resources, and ensured they accessed the necessary services. Further, this participant was willing to re-engage in STAIR-PC, but not in time to complete the study—we instead completed the post-assessments and referred them to an outpatient therapist who could continue STAIR-PC.
It is also important to note that despite participant desire for a longer intervention, 11 (61.1%) participants fell below the clinical cut-off for PTSD by the end of the program, indicating that, even if they would likely continue participation, an extended program or stepped-up PTSD treatment may not be warranted.
We did not find significant improvements in overall quality of life, which may be expected given the lack of follow up data. In addition to this reason, STAIR-PC was developed to target PTSD, yet PTSD is just one diagnosis among many, and symptom reduction may have only a small immediate impact on perceived quality of life. Previous studies suggest that PTSD symptom reduction may lead to improvements in other life domains at longer-term follow-up (Berle et al., 2018; Rapaport, Endiocott, & Clary, 2002; Schnurr, Hayes, Lunney, McFall, & Uddo, 2006). Therefore, our post-intervention assessment may not have captured changes in quality of life that may be present at follow-up data. Moreover, even participants who did not report improvements on survey measures described improvements during post-intervention interviews, and there is some data to suggest that follow-up assessments may be especially important for brief treatments where change (skills acquisition, clinically meaningful symptom reductions) may not be seen until follow-up (Sloan, Marx, Lee, & Resick, 2018).
Our study did not include any assessment of skills acquisition or skills practice, and because these are central to functional improvement, assessing skill use could have determined whether the lack of change in quality of life was due to limited practice. Participants who continue to practice skills learned in the intervention and improve in terms of behavioral health symptomology may see improvements in managing external stressors related to quality of life. Future studies should assess for skills usage to better understand how the skills presented in STAIR-PC may generalize to other contexts (e.g., managing life stressors such as homelessness, coping with medical illness) that may largely contribute to overall quality of life.
4.2. Implementation Challenges
We found that the main challenges to the feasibility of this intervention were the amount of administrative (schedule coordination, appointment reminders, travel vouchers, preparing materials) and technical support (consultation, audio-review and written feedback to therapists) needed to support real-world implementation. Barriers and facilitators related to peer delivery of the intervention are discussed in a forthcoming publication (manuscript submitted for publication).
Session scheduling also required an inordinate amount of effort and time from study staff. Although the session no-show rate for participants was relatively low, session cancellations and rescheduling were common. Finding overlap between participant and certified peer specialist schedules was also challenging, which contributed to the length of time it took participants to complete all 5 intervention sessions. Our study staff reported spending an average of 16 hours on administrative support and 8 hours on technical support per week, suggesting that staffing would be a barrier if the intervention were rolled out to scale.
Per expert recommendations (Blevins, Weathers, Davis, Witte, & Domino, 2015), our protocol required study staff to validate that participants linked PCL-5 responses to a Criterion A event. In order to administer the PCL-5 using this method, study staff received training and supervision around how to guide participants to identify the most appropriate index event to link to PCL-5. This was critical as participants often linked PTSD symptomology to non-Criterion A events (e.g., homelessness, unemployment, uncomplicated bereavement). Providers in real-world settings may experience similar difficulties when identifying appropriate PTEs to link to PCL-5 responses. This is of particular concern to peer specialists, who typically shy away from diagnostic labeling and tend to validate however their peer describes their lived experiences. Despite potential challenges, we recommend training peer specialists to administer the PCL-5 at the beginning of sessions, because 1) in clinician-administered STAIR-PC, PCL-5 administration and review is integrated into sessions; 2) peer specialists frequently requested information in consultation related to symptom management and improvement, indicating a need for increased familiarity with PTSD symptom assessment; and 3) peer specialist administration of the PCL-5 would increase visit efficiency and could decrease stigma associated with reporting behavioral health symptomatology. Ultimately, in real-world peer-based service settings, peer specialists play a vital role in helping persons access to PTSD treatment.
Related to peer specialist training needs, it is important to note that leadership within the organization nominated our peer specialist interventionists, indicating that they may have a higher skill level or are a better fit for intervention delivery than the average peer specialist. There is limited knowledge in the field concerning peer specialist training and supervision, and they may demonstrate varying levels of efficacy and clinical skill. Therefore, future research should be mindful of training and supervision needs of peer providers. There is also a need to develop best practices for selecting peer specialist interventionists. These needs are further discussed in an anticipated publication (manuscript submitted for publication).
Only one of the 26 participants who met our criteria for probable PTSD declined participation. We had a large drop between those eligible at their baseline visit and those participating in the first STAIR-PC session (73.1%). We imagine that this was primarily a function of how we remunerated participants, rather than an indication of unacceptability of the intervention, because once participants completed session 1, they typically completed the intervention in full. That said, large differences in participation between baseline assessment visits and initial sessions are commonly seen in cognitive-behavioral therapies for PTSD (Gutner, Gallagher, Baker, Sloan, & Resick, 2016). Our STAIR-PC completion rate was very high (94.4%). Of note, in a similar trial of peer delivery of a brief trauma-focused outpatient therapy, Crisanti et al. (2019) found 6-month completion rates of 54% and 58% for their study’s respective clinician- and peer-delivered exposure-based interventions, despite the addition of several engagement supports (transportation to and from sessions, childcare, and monetary incentive mid-treatment).
Higher completion rates in our study, compared to other outpatient treatment studies (Crisanti et al., 2019), suggests that our protocol may be more feasible and acceptable. We posit several reasons why this could be: 1) our brief, low-intensity, and low-commitment intervention may have promoted engagement compared to longer treatments requiring discussion of trauma memories, 2) our manual and program were adapted using CBPR to fit the peer model, which may be more acceptable to participants compared to the medical model, and 3) group delivery, like that employed by Crisanti et al. (2019), may inhibit the ability of participants to engage compared to individual delivery. The significant implementation support provided by the research team during this study is important to consider when attempting to disseminate this intervention in real-world settings, particularly as the purpose of training peer specialist providers in interventions like this is to reduce burden. For example, each session was reviewed by the study team and consultation was provided weekly by a licensed clinician. While session review may not be necessary in clinical settings where feasibility does not need to be examined, weekly consultation is arguably integral to appropriate care and clinicians may not be readily available in peer-based settings. Theses and additional needs to adapt the implementation of the intervention as well as the intervention itself are discussed in an anticipated publication (manuscript submitted for publication).
4.3. Study Limitations
There are some notable limitations associated with the nature of a hybrid implementation and initial effectiveness pilot, including our small sample size, lack of a comparison group, and lack of follow-up assessment. Additionally, our measures were not sufficient to capture the full breadth of improvements experienced by participants, as evidenced by our qualitative data. The alphas calculated for measures of effectiveness are also limited in their accuracy due to our small sample size. We also did not systematically assessment for sociodemographic and other factors that would directly characterize our sample as clinically complex, therefore making any generalizations of our findings tentative.
Although we used validated instruments to assess symptoms of PTSD, depression, anxiety, and stress, our evaluation of mental health diagnoses was based on self-report of which DSM-5 diagnoses they had been given by a professional provider. We observed that participants did not always know what they had been diagnosed with, and sometimes disagreed with their providers’ diagnoses. Only 11 (61.1%) participants reported having received a diagnosis of PTSD by a behavioral health professional despite meeting inclusion criteria of “probable PTSD,” providing further evidence that PTSD under-recognized, even by professionals (Roberts et al., 2011; Schwartz et al., 2005). Of course, clinician-administered assessment would be necessary to provide substantiating evidence of this claim. Future research should include clinician-administered diagnostic assessment for PTSD and other mental health diagnoses to validate these secondary findings. As mentioned above, we recommend research to assess the feasibility of peer-administered assessments for PTSD, as this would be necessary for real-world implementation of a peer-delivered intervention for PTSD.
Further study of STAIR-PC delivered by peer specialists and other informal support providers is warranted, given the current study’s promising findings related to improvements in PTSD and other behavioral health symptomatology in a population that represents a high rate of SMI and level of complexity. We recommend replication of the current study in a larger sample of participants, as well as similar research using typical peer-provided support services as a control. Future research should also compare the effectiveness of peer-delivered STAIR-PC to clinician-delivered STAIR-PC, similar to Crisanti et al. (2019). The acceptability of peers as an extension of behavioral health services to increase engagement and the feasibility of stepped approaches, in which peer-delivered services act as a point of entry into the behavioral health service system, should also be explored.
4.4. Conclusions
Due to the high prevalence of trauma-exposure and PTSD, as well as low access to evidence-based treatments, research that integrates implementation and effectiveness outcomes is important to address the lack of access to effective treatment for PTSD in low-income, diverse, urban communities. The current study demonstrated the feasibility, acceptability, and initial effectiveness of a brief, cognitive-behavioral, PTSD treatment. Our findings add to the growing body of literature suggesting that peer providers can effectively deliver treatments to persons experiencing behavioral health conditions, including PTSD. Further research is required to understand symptoms in the follow-up period and to establish best practices for peer delivery. We recommend future randomized controlled trials to further evaluate the promise of peer-delivered PTSD treatments to improve access, engagement, and behavioral health disparities in low-income, diverse, urban communities.
Acknowledgements
This study was funded by Boston University Clinical and Translational Science Institute (BU-CTSI) Integrated Pilot Grant Program and the National Institute of Health [NIH: 1UL1TR001430]. Dr. Valentine’s time was supported by the National Institute of Mental Health [NIMH: K23MH117221]. We would like to thank Dr. Christie Jackson who provided training to study therapists and consultation to study staff. Her support was instrumental in manual revision.
Footnotes
Disclosures
Authors have no conflicts of interest, financial or otherwise, related to this work to disclose at this time.
References
- Alegría M, Mulvaney-Day N, Woo M, Torres M, Gao S, & Oddo V (2007). Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American Study. American Journal of Public Health, 97(1), 76–83. 10.2105/AJPH.2006.087197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Vila D, Woo M, Canino G, Takeuchi D, Vera M, … Shrout P (2004). Cultural relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods in Psychiatric Research, 13, 270–288. 10.1002/mpr.181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, & Charney DS (2006). Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association, 98(10), 1630–1636. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2569763/ [PMC free article] [PubMed] [Google Scholar]
- Attkinson CC & Zwick R (1982). The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning 5(3), 233–237. 10.1016/0149-7189(82)90074-X [DOI] [PubMed] [Google Scholar]
- Austin E, Ramakrishnan A, & Hopper K (2014). Embodying recovery: A qualitative study of peer work in a consumer-run service setting. Community Mental Health Journal, 50(8), 879–885. 10.1007/s10597-014-9693-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berle D, Hilbrink D, Russell-Williams C, Kiely R, Hardaker L, Garwood N, … Steel Z (2018). Personal wellbeing in posttraumatic stress disorder (PTSD): association with PTSD symptoms during and following treatment. BMC Psychology, 6(1), 7 10.1186/s40359-018-0219-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard HR (2006). Research methods in anthropology: Qualitative and quantitative approaches (4th ed.). Lanham, MD: AltaMira Press. [Google Scholar]
- Blackburn IM, James IA, Milne DL, Baker C, Standart S, Garland A, & Reichelt FK (2001). The revised cognitive therapy scale (CTS-R): Psychometric properties. Behavioural and Cognitive Psychotherapy, 29, 431–446. 10.1017/s1352465801004040 [DOI] [Google Scholar]
- Blais MA, Lenderking WR, Baer L, deLorell A, Peets K, Leahy L, & Burns C (1999). Development and initial validation of a brief mental health outcome measure. Journal of Personality Assessment, 73, 359–373. 10.1207/S15327752JPA7303_5 [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. Journal of Traumatic Stress, 28(6), 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Boer PC, Wiersma D, Russo S, Bosch RJ, & Boer PC (n.d.). Paraprofessionals for anxiety and depressive disorders. Cochrane Database of Systematic Reviews, 2(CD004688). 10.1002/14651858.CD004688.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinman M, Lucksted A, Gresen R, Davis M, Losonczy M, Sussner B, & Martone L (2008). Early experiences of employing consumer-providers in the VA. Psychiatric Services, 59(11), 1315–1321. 10.1176/appi.ps.59.11.1315 [DOI] [PubMed] [Google Scholar]
- Chinman M, Young AS, Hassell J & Davidson L (2006). Toward the implementation of mental health consumer provider services. The Journal of Behavioral Health Services and Research, 33(2), 176–195. 10.1007/s11414-006-9009-3 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, & Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. 10.1037/0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, … Petkova E (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. The American Journal of Psychiatry, 167(8), 915–924. 10.1176/appi.ajp.2010.09081247 [DOI] [PubMed] [Google Scholar]
- Copeland ME (2002). Wellness Recovery Action Plan: A system for monitoring, reducing, and eliminating uncomfortable or dangerous physical symptoms and emotional feelings. Occupational Therapy in Mental Health, 17(3–4), 127–150. 10.1300/J004v17n03_09 [DOI] [Google Scholar]
- Corrigan PW, Torres A, Lara JL, Sheehan L, & Larson JE (2017). The healthcare needs of Latinos with serious mental illness and the potential of peer navigators. Administration and Policy in Mental Health and Mental Health Services Research, 44(4), 547–557. 10.1007/s10488-016-0737-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crisanti AS, Reno J, Salvador JG, Killough C, & Greene RN (2019). Perceived helpfulness of peer-delivered trauma specific treatment: A randomized controlled trial. Psychological Services, 16(3), 425–432. 10.1037/ser0000281 [DOI] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C (2012). Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50(3), 217–226. https://dx.doi.org/10.1097%2FMLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L, Bellamy C, Guy K, & Miller R (2012). Peer support among persons with severe mental illnesses: A review of evidence and experience. World Psychiatry, 11(2), 123–128. 10.1016/j.wpsyc.2012.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias A, Azariah F, Anderson SJ, Sequeira M, Cohen A, Morse JQ, … Reynolds CF III. (2019). Effect of a lay counselor intervention on prevention of major depression in older adults living in low- and middle-income countries: A randomized clinical trial. JAMA Psychiatry, 76(1), 13–20. 10.1001/jamapsychiatry.2018.3048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson FB, Sommerville J, Origoni AE, Ringel NB, & Parente F (2002). Experiences of stigma among outpatients with schizophrenia. Schizophrenia Bulletin, 28(1), 143–155. 10.1093/oxfordjournals.schbul.a006917 [DOI] [PubMed] [Google Scholar]
- Dinwiddie GY, Gaskin DJ, Chan KS, Norrington J, & McCleary R (2013). Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Social Science & Medicine, 80, 67–75. 10.1016/j.socscimed.2012.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon LB, Holoshitz Y, & Nossel I (2016). Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry, 15(1), 13–20. 10.1002/wps.20306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekers D, Richards D, McMillan D, Bland JM, & Gilbody S (2011). Behavioural activation delivered by the nonspecialist: Phase II randomised controlled trial. The British Journal of Psychiatry, 198(1), 66–72. 10.1192/bjp.bp.110.079111 [DOI] [PubMed] [Google Scholar]
- Fellowship and Residency at Boston Medical Center. (2019). Diverse patients need diverse providers. Developmental & Behavioral Pediatrics. Retrieved March 26, 2020, from https://www.bmc.org/sites/default/files/Patient_Care/Specialty_Care/Pediatrics-Developmental-Behavioral/Diverse-Patients-Need-Diverse-Providers.pdf
- Fox J, Desai MM, Britten K, Lucas G, Luneau R, & Rosenthal MS (2012). Mental-health conditions, barriers to care, and productivity loss among officers in an urban police department. Connecticut Medicine, 76(9), 525–531. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4089972/ [PMC free article] [PubMed] [Google Scholar]
- Gates LB, & Akabas SH (2007). Developing strategies to integrate peer providers into the staff of mental health agencies. Administration and Policy in Mental Health and Mental Health Services Research, 34(3), 293–306. 10.1007/s10488-006-0109-4 [DOI] [PubMed] [Google Scholar]
- Gajwani P (2014). Can what we learned about reducing no-shows in our clinic work for you? Current Psychiatry, 13(9), 13–15. Retrieved from https://www.mdedge.com/psychiatry/article/86564/practice-management/can-what-we-learned-about-reducing-no-shows-our-clinic [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, … Ressler KJ (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, & Rashidian A (2013). Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. The Cochrane Database of Systematic Reviews, 2(CD010414). 10.1002/14651858.CD010414.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray M, Litz B, Hsu J, & Lombardo T (2004). Psychometric properties of the Life Events Checklist. (PDF) Assessment, 11, 330–341. 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Gutner CA, Gallagher MW, Baker AS, Sloan DM, & Resick PA (2016). Time course of treatment dropout in cognitive–behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 115–121. 10.1037/tra0000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration & Substance Abuse and Mental Health Services Administration. (2015). National Projections of Supply and Demand for Behavioral Health Practitioners: 2013–2025. Rockville, MD: Health Resources and Services Administration; Retrieved from https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/behavioral-health2013-2025.pdf [Google Scholar]
- Health Resources in Action. (2016, July). Boston Medical Center community health needs assessment final report. https://www.bmc.org/sites/default/files/About_Us/Commitment_to_Our_Community/field_Attachments/BMC-Community-HealthNeedsAssessment-HNA.pdf
- Henry JD, & Crawford JR (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44(2), 227–239. [DOI] [PubMed] [Google Scholar]
- Hsieh H-F, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- IBM Corp. (2016). IBM SPSS Statistics for Windows, Version 24.0 [computer software]. Armonk, NY: IBM Corp. [Google Scholar]
- Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. 10.17226/12875 [DOI] [PubMed] [Google Scholar]
- Jain S, Ortigo K, Baldor DA, Weiss BJ, & Cloitre M (in press). A randomized controlled trial of brief skills training in affective and interpersonal regulation (STAIR) for veterans in primary care. Journal of Traumatic Stress. [DOI] [PubMed] [Google Scholar]
- Jarero I, Rake G, & Givaudan M (2017). EMDR therapy program for advanced psychosocial interventions provided by paraprofessionals. Journal of EMDR Practice and Research, 11(3), 122–128. 10.1891/1933-3196.11.3.122 [DOI] [Google Scholar]
- Johnson SR (2019, May 16). Study: EHRs can help address social needs in primary care. Modern Healthcare. Retrieved March 26, 2020, from https://www.modernhealthcare.com/technology/study-ehrs-can-help-address-social-needs-primary-care
- Kaltman S, Hurtado de Mendoza A, Gonzales FA, & Serrano A (2014). Preferences for trauma-related mental health services among Latina immigrants from Central America, South America, and Mexico. Psychological Trauma: Theory, Research, Practice, and Policy, 6(1), 83–91. 10.1037/a0031539 [DOI] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, and Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2, 197–207. 10.1016/0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- Lê Cook B, McGuire TG, & Zaslavsky AM (2012). Measuring racial/ethnic disparities in health care: Methods and practical issues. Health Services Research, 47(3, Pt2), 1232–1254. 10.1111/j.1475-6773.2012.01387.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond SH & Lovibond PF (1995). Manual for the Depression Anxiety & Stress Scales. (2nd Ed.) Sydney: Psychology Foundation. [Google Scholar]
- Mueser KT, Rosenberg SD, Fox L, Salyers MP, Ford JD, & Carty P (2001). Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychological Assessment, 13(1), 110–117. 10.1037/1040-3590.13.1.110 [DOI] [PubMed] [Google Scholar]
- Najavits LM, Hamilton N, Miller N, Griffin J, Welsh T, & Vargo M (2014). Peer-led seeking safety: Results of a pilot outcome study with relevance to public health. Journal of Psychoactive Drugs, 46(4), 295–302. 10.1080/02791072.2014.922227 [DOI] [PubMed] [Google Scholar]
- Nguyen TD, Attkisson C, & Stegner BL (1983). Assessment of patient satisfaction: Development and refinement of a Service Evaluation Questionnaire. Evaluation and Program Planning, 6(3–4), 299–313. 10.1016/0149-7189(83)90010-1 [DOI] [PubMed] [Google Scholar]
- Ogbeide SA, Landoll RR, Nielsen MK, & Kanzler KE (2018). To go or not go: Patient preference in seeking specialty mental health versus behavioral consultation within the primary care behavioral health consultation model. Families, Systems, & Health, 36(4), 513–517. 10.1037/fsh0000374 [DOI] [PubMed] [Google Scholar]
- Parker B, & McFarlane J (1991). Identifying and helping battered pregnant women. Journal of Maternal Child Nursing, 16, 161–164. 10.1097/00005721-199105000-00013 [DOI] [PubMed] [Google Scholar]
- Pfeiffer PN, King C, Ilgen M, Ganoczy D, Clive R, Garlick J, … Valenstein M (2019). Development and pilot study of a suicide prevention intervention delivered by peer support specialists. Psychological Services, 16(3), 360–371. 10.1037/ser0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Mark BP, Kimerling R, Jenkins-Guarnieri MA, … Tiet QQ (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and evaluation within a Veteran primary care sample. Journal of General Internal Medicine, 31, 1206–1211. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, … Hensley M (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38(2), 65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Próspero M, & Vohra-Gupta S (2008). The use of mental health services among victims of partner violence on college campuses. Journal of Aggression, Maltreatment & Trauma, 16(4), 376–390. 10.1080/10926770801926450 [DOI] [Google Scholar]
- QSR International. (2018). NVivo 12 Pro (Version 12.5) [computer software]. Available from https://www.qsrinternational.com/nvivo/nvivo-products/nvivo-12-pro
- Rapaport MH, Endicott J, & Clary CM (2002). Posttraumatic stress disorder and quality of life: Results across 64 weeks of sertraline treatment. The Journal of Clinical Psychiatry, 63(1), 59–65. 10.4088/JCP.v63n0112 [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83. 10.1017/S0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers ES, Maru M, Johnson G, Cohee J, Hinkel J, & Hashemi L (2016). A randomized trial of individual peer support for adults with psychiatric disabilities undergoing civil commitment. Psychiatric Rehabilitation Journal, 39(3), 248–255. https://doi.org10.1037/prj0000208 [DOI] [PubMed] [Google Scholar]
- Ronk FR, Korman JR, Hooke GR, & Page AC (2013). Assessing clinical significance of treatment outcomes using the DASS-21. Psychological Assessment, 25(4), 1103–1110. 10.1037/a0033100 [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, & Corrigan PW (2005). The stigma of mental illness: concepts, forms, and consequences. Psychiatrische Praxis, 32(5), 221–32. 10.1016/j.eurpsy.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Rutt BT, Oehlert ME, Krieshok TS, & Lichtenberg JW (2018). Effectiveness of Cognitive Processing Therapy and Prolonged Exposure in the Department of Veterans Affairs. Psychological Reports, 121(2), 282–302. 10.1177/0033294117727746 [DOI] [PubMed] [Google Scholar]
- Salzer MS, Schwenk E, & Brusilovskiy E (2010). Certified peer specialist roles and activities: Results from a national survey. Psychiatric Services, 61(5), 520–523. 10.1176/appi.ps.61.5.520 [DOI] [PubMed] [Google Scholar]
- SAMHSA-HRSA Center for Integrated Health Solutions. (2016). Peer Providers. Retrieved from http://www.integration.samhsa.gov/workforce/team-members/peer-providers
- Schnurr PP, Hayes AF, Lunney CA, McFall M, & Uddo M (2006). Longitudinal analysis of the relationship between symptoms and quality of life in veterans treated for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74(4), 707–713. 10.1037/0022-006X.74.4.707 [DOI] [PubMed] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, & Ressler KJ (2005). Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services, 56(2), 212–215. 10.1176/appi.ps.56.2.212 [DOI] [PubMed] [Google Scholar]
- Scott A, Doughty C, & Kahi H (2011). ‘Having those conversations’: The politics of risk in peer support practice. Health Sociology Review, 20(2), 187–201. 10.5172/hesr.2011.20.2.187. [DOI] [Google Scholar]
- Sloan DM, Marx BP, Lee DJ, & Resick PA (2018). A brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: A randomized noninferiority clinical trial. JAMA Psychiatry, 75(3), 233–239. 10.1001/jamapsychiatry.2017.4249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon P (2004). Peer support/peer provided services: Underlying processes, benefits, and critical ingredients. Psychiatric Rehabilitation Journal, 27(4), 392–401. 10.2975/27.2004.392.401 [DOI] [PubMed] [Google Scholar]
- Stanley MA, Wilson NL, Amspoker AB, Kraus SC, Wagener PD, Calleo JS, … Kunik ME (2014). Lay providers can deliver effective cognitive behavior therapy for older adults with generalized anxiety disorder: A randomized trial. Depression and Anxiety, 31(5), 391–401. 10.1002/da.22239 [DOI] [PubMed] [Google Scholar]
- The Transformation Center. (2020). Massachusetts Certified Peer Specialist (CPS) Training Program. Retrieved March 25, 2020, from https://transformation-center.org/home/training/certified-peer-specialists/
- U.S. Department of Veterans Affairs. (2019). Using the PTSD Checklist for the DSM-5 (PCL-5). National Center for PTSD; Retrieved from http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp. [Google Scholar]
- Valentine SE, Dixon L, Borba CPC, Shtasel DL, & Marques L (2016). Mental illness stigma and engagement in an implementation trial for cognitive processing therapy at a diverse community health center: A qualitative investigation. International Journal of Culture and Mental Health, 9(2), 139–150. 10.1080/17542863.2015.1123742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl OF (1999). Mental health consumers experience of stigma. Schizophrenia Bulletin, 25(3), 467–478. 10.1093/oxfordjournals.schbul.a033394 [DOI] [PubMed] [Google Scholar]
- Watson E (2019). The mechanisms underpinning peer support: A literature review. Journal of Mental Health, 28(6), 677–688. 10.1080/09638237.2017.1417559 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013a). The Life Events Checklist for DSM-5 (LEC-5) – Standard. [Measurement instrument]. Available from http://www.ptsd.va.gov/
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, … Marx BP (2017). Clinician-Administered PTSD Scale for DSM-5. PsycTESTS. 10.1037/t71324-000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013b). The PTSD Checklist for DSM-5 (PCL-5) – Standard [Measurement instrument]. Available from https://www.ptsd.va.gov/