Key Points
Question
Among SPRINT participants self-identified as Black, what are the associations of global genetic West African ancestry with response to antihypertensive medication, blood pressure control, and cardiovascular outcomes?
Findings
Global West African ancestry proportion was not significantly associated with response to antihypertensive medication, blood pressure control, or kidney function changes over time. A higher proportion of West African ancestry was associated with a modestly lower risk for cardiovascular events.
Meaning
These findings highlight the greater importance of nonbiological risk factors—including socioeconomic status, environmental factors, educational attainment, behavioral characteristics, structural racism, and access to health care—in existing disparities in hypertension control and downstream adverse cardiovascular risk.
This post hoc analysis of data from the Systolic Blood Pressure Intervention Trial determines the association between the proportion of West African ancestry with response to antihypertensive medication, blood pressure control, kidney function, and risk of adverse cardiovascular events among self-identified Black individuals.
Abstract
Importance
Self-identified Black race is associated with higher hypertension prevalence and worse blood pressure (BP) control compared with other race/ethnic groups. The contribution of genetic West African ancestry to these racial disparities appears not to have been completely determined.
Objective
To determine the association between the proportion of West African ancestry with the response to antihypertensive medication, BP control, kidney function, and risk of adverse cardiovascular (CV) events among self-identified Black individuals in the Systolic Blood Pressure Intervention Trial (SPRINT).
Design, Setting, and Participants
This post hoc analysis of the SPRINT trial incorporated data from a multicenter study of self-identified Black participants with available West African ancestry proportion, estimated using 106 biallelic autosomal ancestry informative genetic markers. Recruitment started on October 20, 2010, and ended on August 20, 2015. Data were analyzed from May 2020 to September 2020.
Main Outcomes and Measures
Trajectories of BP and kidney function parameters on follow-up of the trial were assessed across tertiles of the proportion of West African ancestry using linear mixed-effect modeling after adjustment for potential confounders. Multivariable adjusted Cox models evaluated the association of West African ancestry with the risk of composite CV events (nonfatal myocardial infarction, CV death, and heart failure event).
Results
Among 2466 participants in the current analysis (1122 women [45.5%]; median West African ancestry, 81% [interquartile range, 73%-87%]), there were 120 composite CV events (4.9%) over a mean (SD) of 3.2 (0.9) years of follow-up. At baseline, mean (SD) high-density lipoprotein cholesterol levels were higher (tertile 3: 56.5 [15.0] mg/dL vs tertile 1: 54.2 [14.9] mg/dL; P = .006), smoking prevalence (never smoking: tertile 3: 367 [47.9%] vs tertile 1: 372 [42.2%]; P = .009) and mean (SD) Framingham Risk scores (tertile 3: 16.7 [9.7] vs tertile 1: 18.1 [10.2]; P = .01) were lower, and baseline BP was not different across increasing tertiles of West African ancestry. On follow-up, there was no evidence of differences in longitudinal trajectories of BP, kidney function parameters, or left ventricular mass (Cornell voltage by electrocardiogram) across tertiles of West African ancestry in either intensive or standard treatment arms. In adjusted Cox models, higher West African ancestry was associated with a lower risk of a composite CV event after adjustment for potential confounders (adjusted hazard ratio per 5% higher West African ancestry, 0.92 [95% CI, 0.85-0.99]).
Conclusions and Relevance
Among self-reported Black individuals enrolled in SPRINT, the trajectories of BP, kidney function, and left ventricular mass over time were not different across tertiles of the proportion of West African ancestry. A higher proportion of West African ancestry was associated with a modestly lower risk for CV events. These findings suggest that extrinsic and structural societal factors, more than genetic ancestry, may be the major drivers of the well-established racial disparity in cardiovascular health associated with hypertension.
Introduction
The Black-White difference in the prevalence and control of hypertension in the United States has been well described. Self-identified Black adults experience up to a 2-fold greater burden of cardiovascular and kidney disease, as well as significantly higher rates of uncontrolled hypertension, compared with White counterparts.1 Within the past 3 years, troubling trends demonstrate a decline in blood pressure (BP) control in all racial groups and especially among Black adults.2 Furthermore, Black adults exhibit higher rates of premature, severe, and resistant hypertension phenotypes and in turn experience more downstream cardiovascular and kidney complications.1,3
Currently, mechanisms of observed disparities by self-reported race are not well understood and have been broadly attributed to a complex interplay of genetic, environmental, societal, and behavioral factors.4 Because racial identity itself is a social rather than biological construct, it is vulnerable to confounding because of the effects of structural racism, socioeconomic inequality, environmental disparities, and unequal access to care, limiting its interpretability. In this setting, however, novel techniques that allow for the quantification of geographic ancestry provide unique tools for disentangling genetic contributors to excess risk from known social and environmental drivers.5 In the US, individuals of self-identified Black race represent a convergence of predominantly West African and European geographic ancestries, with West African geographic ancestry heterogeneously distributed within the population.5 As a result, the measured proportion of geographic West African ancestry in this population can serve as a proxy for race-specific risks attributable to genetic factors, allowing for genetic risk to be directly measured in the population.
Observational studies evaluating the contribution of biological and genetic factors to the high burden of poorly controlled hypertension and cardiovascular risk in Black individuals have been limited by inadequate capture of societal and environmental factors that contribute to disparities in access to care.2 In this study, we evaluated the contribution of West African genetic ancestry proportion to measures of BP control and clinical outcomes in the setting of the randomized, controlled Systolic Blood Pressure Intervention Trial (SPRINT), which by its design provided participants with similar access to clinicians and therapies, diminishing the effects of social and environmental disparities.
Methods
Study Population
For this study, we used publicly available, deidentified data from SPRINT. Data were obtained from the National Institutes of Health and National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC). The study design, treatment protocol, and primary outcomes from SPRINT have been reported previously and are detailed in the eMethods in the Supplement.6,7
Global West African ancestry estimates were available on a subset of 2569 SPRINT participants based on specialized consent to collect genetic information.8,9 The present study included self-reported Black participants with available data on genetic West African ancestry (n = 2569). Individuals who were outliers for their genetic ancestry (ie, individuals for whom self-reported race/ethnicity was not consistent with their genetic ancestry estimates; West African ancestry <30% [n = 13]) or with significant missingness in their baseline data (n = 90) were excluded from the present analysis. All SPRINT study participants provided written informed consent at the time of study enrollment. The institutional review boards approved the study at each participating study site. The University of Texas Southwestern institutional review board approved the current analysis.
Clinical Covariates and Laboratory Assessment
Demographic, clinical, and laboratory data were collected at baseline and follow-up by trained study personnel using standardized protocols, as described previously6 and detailed in the eMethods in the Supplement. Recruitment for SPRINT was begun on October 20, 2010, and completed on August 20, 2015.
Genotyping and Global West African Ancestry Assessment
Genetic samples were obtained from consenting SPRINT participants to assess genetic West African ancestry. Investigators identified 106 biallelic ancestry informative markers (AIMs), which were genotyped to provide the proportion of West African ancestry. Prior reports show that the correlation coefficient between estimated ancestry scores and true individual ancestral proportions is greater than 0.9 when the estimated ancestry scores are derived from approximately 100 AIMS.10,11 Using 44 Yoruba individuals in the HapMap database (representing West African ancestry) and 39 European American control participants serving as parental reference populations, per SPRINT protocol, a maximum likelihood approach was used to estimate individual ancestry using frequentist estimation of individual ancestry proportion, which has been previously validated to estimate the individual proportion of West African and European ancestry.9,12,13 The AIMs for Yoruba individuals in Ibadan, Nigeria, represent markers specific to West and Central African individuals, in that genetic and historical record data indicate that most Black American individuals derive their ancestry from these areas.14,15
Outcomes of Interest
Our primary outcome of interest was BP trajectory during the 3-year study period. Following randomization, participant antihypertensive regimens were adjusted to achieve new target BP with trends in BP and medication adjustments made monthly for the first 3 months, then every 3 months after that. Our secondary outcomes of interest included the primary composite outcome of the trial (composite of myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute decompensated heart failure, or cardiovascular death), trajectories of kidney function parameters (estimated glomerular filtration rate [eGFR], blood urea nitrogen [BUN], and urine albumin-creatinine ratio), and all-cause mortality. Outcome events were adjudicated by members of the SPRINT Clinical Outcomes Adjudicator Subcommittee, who were masked to treatment assignments using a previously described protocol.7
Statistical Analysis
The study cohort was categorized into tertiles of genetic West African ancestry proportion. The baseline characteristics were reported across the study groups as means (SDs) or medians (interquartile ranges [IQRs]) for continuous variables and percentages for categorical variables and compared using 1-way analysis of variance for continuous variables and χ2 tests for categorical variables. Changes in systolic blood pressure (SBP), diastolic blood pressure (DBP), number of antihypertensive medications, and other clinical parameters, including BUN, eGFR, urine microalbumin-creatinine ratio, and Cornell voltage, were assessed over time using linear mixed effect models for repeated measures. Two slopes were computed with a cut point at 6 months or less or more than 6 months after randomization and designed to reflect the short-term and long-term trajectories in these parameters in response to the study intervention. Since only 1 electrocardiogram (EKG) was regularly obtained before 6 months, only 1 slope was computed to assess trajectories in Cornell voltage over the duration of the trial. Differences in slopes between tertiles were compared using the Wald test. Given the differences in hemodynamic outcomes between treatment groups, the intensive and standard BP treatment arms were analyzed separately. Each model was adjusted for age, sex, history of cardiovascular disease, education level, trial site, and APOL1 risk count. A sensitivity analysis was also performed stratifying by APOL1 risk count (0 vs 1 or 2).
The association between continuous West African ancestry and risk of adverse cardiovascular events on follow-up was assessed using multivariable Cox proportional hazard models and restricted cubic splines with adjustment for the following covariates: model 1: no adjustments; model 2: adjustments for age, sex, treatment arm, eGFR, smoking status, education level, trial site, and APOL1 risk count; and model 3: the adjustments of model 2, plus SBP, total cholesterol, and high-density lipoprotein cholesterol. Separate models were constructed for the composite outcome and all-cause mortality. The interaction between treatment arm and West African ancestry proportion for the risk of primary and secondary outcomes of interest was assessed by including a multiplicative treatment interaction term in the most adjusted models. The intensive BP control treatment effect on the primary outcome was also evaluated using cumulative incidence curves and unadjusted and adjusted Cox models (with same covariates as in model 3) across tertiles of West African ancestry. All analyses were performed using R version 3.6.0 (R Foundation for Statistical Computing) from May 2020 to September 2020.
Results
The final study population included 2466 self-reported Black adults (of whom 1122 were women [45.5%]). The proportion of West African ancestry ranged from 30% to 100% in the study cohort (median, 81% [IQR, 73%-87%]; eFigure 1 in the Supplement). At baseline, we observed no meaningful difference in mean age or sex distribution across West African ancestry-based tertiles (Table 1). Participants exhibited similar baseline SBP and prevalence of clinical and subclinical cardiovascular disease (CVD) across tertiles. Among CVD risk factors, mean high-density lipoprotein cholesterol levels were higher (tertile 3: 56.5 [15.0] mg/dL vs tertile 1: 54.2 [14.9] mg/dL; P = .006; to convert to millimoles per liter, multiply by 0.0259), rates of never smoking were higher (tertile 3: 367 [47.9%] vs tertile 1: 372 [42.2%]; P = .009), and the mean Framingham Risk Score was lower (tertile 3: 16.7 [9.7] vs tertile 1: 18.1 [10.2]; P = .01) across study groups with increasing West African ancestry proportion. In contrast, the mean (SD) amount of proteinuria (tertile 3: 45.9 [140.8] μg/mg vs tertile 1: 36.7 [113.8] μg/mg; P = .02), mean (SD) serum creatinine level (tertile 3: 1.2 [0.4] mg/dL vs tertile 1: 1.1 [0.4] mg/dL; P = .009; to convert to micromoles per liter, multiply by 88.4), and prevalence of left ventricular hypertrophy assessed by Cornell voltage (tertile 1: 95 [10.8%] vs tertile 3: 120 [15.6%]; P = .01) increased with increasing West African ancestry, and the mean (SD) eGFR decreased (tertile 3: 74.0 [22.8] mL/min/1.73 m2 vs tertile 1: 77.9 [23.1] mL/min/1.73 m2; P = .003). Notably, modest but statistically significant differences in social risk factors were noted across the West African ancestry–based groups, with lower rates of college education (tertile 3: 381 [49.7%] vs tertile 1: 532 [60.2%]; P < .001) and a higher proportion of participants without insurance (tertile 3: 144 [18.8%] vs tertile 1: 135 [15.3%]; P = .02) in groups with higher West African ancestry.
Table 1. Baseline Characteristics of Study Participants by Tertile West African Ancestry.
| Characteristic | Patients, No. (%) | P value for trend | ||
|---|---|---|---|---|
| Tertile 1 (n = 882) | Tertile 2 (n = 817) | Tertile 3 (n = 767) | ||
| West African ancestry, % (IQR) | 69 (63-74) | 81 (79-83) | 89 (87-92) | |
| APOL1 risk count | <.001 | |||
| 0 | 411 (46.6) | 326 (39.9) | 274 (35.7) | |
| 1 | 385 (43.7) | 376 (46.0) | 343 (44.7) | |
| 2 | 86 (9.8) | 115 (14.1) | 150 (19.6) | |
| Intensive treatment arm | 436 (49.4) | 386 (47.2) | 388 (50.6) | .40 |
| Age, mean (SD), y | 65.2 (9.1) | 63.2 (8.7) | 64.3 (9.0) | <.001 |
| Female | 393 (44.6) | 368 (45.0) | 361 (47.1) | .57 |
| College education | 532 (60.2) | 435 (53.2) | 381 (49.7) | <.001 |
| No insurance | 135 (15.3) | 168 (20.6) | 144 (18.8) | .02 |
| Blood pressure, mm Hg | ||||
| Systolic | 140 (16.4) | 140 (16.0) | 140 (16.1) | .84 |
| Diastolic | 80 (12.7) | 82 (12.2) | 81 (12.2) | .01 |
| BMI | 31 (6.1) | 31 (6.4) | 31 (6.5) | .19 |
| Chronic kidney disease | 187 (21.2) | 185 (22.6) | 201 (26.2) | .05 |
| Clinical cardiovascular disease | 101 (11.5) | 84 (10.3) | 76 (9.9) | .56 |
| Atrial fibrillation | 44 (5.0) | 35 (4.3) | 30 (3.9) | .55 |
| Heart failure | 31 (3.5) | 37 (4.5) | 37 (4.8) | .38 |
| Peripheral vascular disease | 43 (4.9) | 34 (4.2) | 41 (5.4) | .53 |
| Stroke | 3 (0.3) | 7 (0.9) | 4 (0.5) | .36 |
| Diabetes | 13 (1.5) | 10 (1.2) | 21 (2.7) | .05 |
| Hypertension | 832 (94.3) | 775 (94.9) | 721 (94.0) | .76 |
| Depression | 149 (16.9) | 138 (16.9) | 127 (16.6) | .98 |
| Alcohol abuse | 51 (5.8) | 44 (5.4) | 42 (5.5) | .93 |
| Family history of heart disease | ||||
| No | 323 (36.7) | 323 (39.5) | 302 (39.5) | .43 |
| Yes | 486 (55.2) | 428 (52.4) | 390 (51.0) | |
| Unknown | 72 (8.2) | 66 (8.1) | 73 (9.5) | |
| Smoking | ||||
| Never | 372 (42.2) | 348 (42.6) | 367 (47.9) | .01 |
| Former | 320 (36.3) | 259 (31.7) | 225 (29.4) | |
| Current | 189 (21.5) | 210 (25.7) | 174 (22.7) | |
| Blood urea nitrogen, mean (SD), mg/dL | 17.3 (6.6) | 17.2 (6.4) | 17.6 (7.2) | .37 |
| Cholesterol, mean (SD), mg/dL | 195.6 (41.9) | 197.5 (42.4) | 195.7 (38.7) | .57 |
| Chloride, mean (SD), mEq/L | 103.1 (2.7) | 103.3 (2.9) | 103.1 (2.7) | .49 |
| Bicarbonate, mean (SD), mEq/L | 26.3 (2.8) | 26.3 (2.8) | 26.5 (2.6) | .39 |
| Urine creatinine, mean (SD), mmol | 155.5 (94.1) | 155.2 (88.2) | 155.2 (89.8) | .99 |
| Glucose, mean (SD), mg/dL | 97.9 (13.9) | 97.7 (16.0) | 97.6 (17.5) | .94 |
| High-density lipoprotein cholesterol, mean (SD), mg/dL | 54.2 (14.9) | 54.8 (15.1) | 56.5 (15.0) | .01 |
| Potassium, mean (SD), mEq/L | 4.1 (0.4) | 4.0 (0.4) | 4.1 (0.4) | .20 |
| Low-density lipoprotein cholesterol, mean (SD), mg/dL | 118.9 (35.0) | 121.1 (37.0) | 118.4 (34.8) | .26 |
| Sodium, mean (SD), mEq/L | 140.4 (2.3) | 140.4 (2.2) | 140.5 (2.2) | .26 |
| Triglycerides, mean (SD), mg/dL | 115.2 (115.6) | 112.7 (131.7) | 105.9 (69.5) | .21 |
| Urine microalbumin-creatinine ratio, mean (SD), μg/mg | 36.7 (113.8) | 61.6 (263.8) | 45.9 (140.8) | .02 |
| Creatinine, mg/dL | 1.1 (0.4) | 1.1 (0.4) | 1.2 (0.4) | .01 |
| Estimated glomerular filtration rate, mean (SD), mL/min/1.73 m2 | 77.9 (23.1) | 76.7 (22.8) | 74.0 (22.8) | .003 |
| QRS duration, mean (SD), ms | 92.7 (16.1) | 92.0 (16.1) | 91.8 (16.0) | .50 |
| Cornell voltage, mean (SD), mV | 1701.5 (715.3) | 1677.5 (733.8) | 1739.9 (724.2) | .23 |
| Left ventricular hypertrophy by Cornell voltage (baseline) | 95 (10.8) | 103 (12.6) | 120 (15.6) | .01 |
| Framingham 10-y cardiovascular disease risk, mean (SD) | 18.1 (10.2) | 17.2 (9.9) | 16.7 (9.7) | .01 |
| No. of antihypertensive drugs at start, mean (SD), % | 2.0 (1.1) | 2.0 (1.0) | 2.0 (1.0) | .73 |
| Aspirin | 373 (42.4) | 317 (38.8) | 317 (41.3) | .32 |
| Statin | 323 (36.8) | 260 (32.0) | 243 (31.9) | .05 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range.
SI conversion factors: To convert blood urea nitrogen to mmol/L, multiply by 0.357; high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, and total cholesterol to mmol/L, multiply by 0.0259; chloride, bicarbonate, potassium, and sodium to mmol/L, multiply by 1.0; glucose to mmol/L, multiply by 0.0555; triglycerides to mmol/L, multiply by 0.0113; creatinine to μmol/L, multiply by 88.4.
Association of West African Ancestry and Follow-up Trends in Blood Pressure
On follow-up, we observed no significant differences in BP trends across ancestry tertiles in both the standard and intensive therapy arms (Figure 1A). In the adjusted linear mixed-model analysis, West African ancestry categories were not significantly associated with the initial (≤6 months) or long-term (>6 months) changes in SBP over time in both the standard and intensive treatment arms (Table 2; eFigure 2 in the Supplement). Consistent patterns were also observed for the outcome of DBP measures over time, using continuous measures of West African ancestry, and in a stratified analysis by APOL1 risk count (eTables 1 and 2 in the Supplement). There was no significant interaction between the randomized treatment group and West African ancestry proportion for longitudinal changes in systolic or diastolic BP over time. Similarly, we observed no differences in the number of antihypertensive medications or medication classes over time between West African ancestry–based study groups (Figure 1B; eTables 3 and 4 in the Supplement).
Figure 1. Trajectories of Systolic Blood Pressure, Number of Antihypertensive Medications, and Kidney Function Parameters Across West African Ancestry Based Study Groups in the Intensive Treatment and Standard Arms.
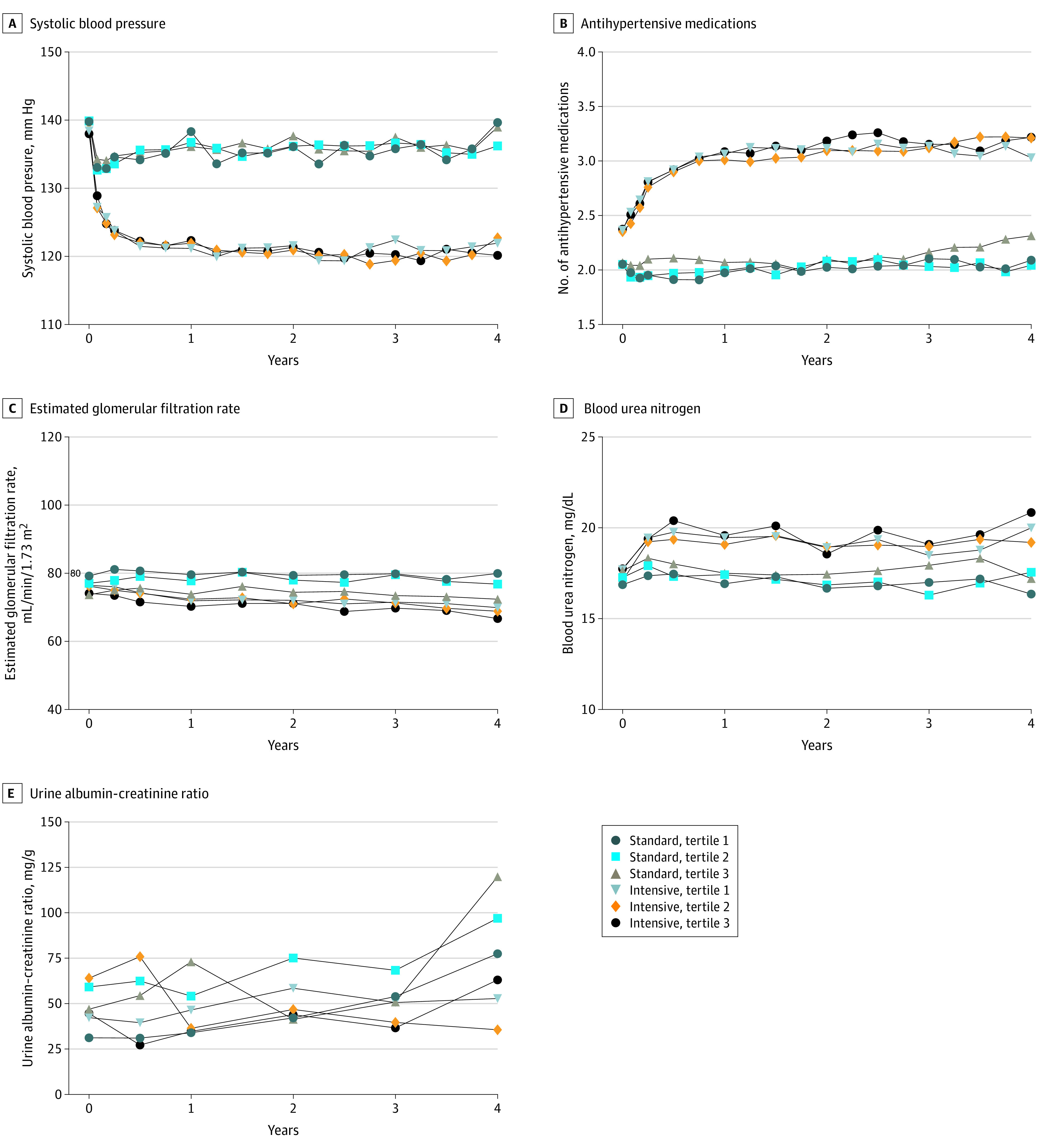
A, Mean systolic blood pressure. B, Mean number of antihypertensive medications. C, Mean estimated glomerular filtration rate. D, Mean blood urea nitrogen. E, Mean urine albumin-creatinine ratio over time by treatment group and ancestry tertile.
Table 2. Slopes of Linear Mixed Models of Blood Pressure Over Time by West African Ancestry Tertilesa.
| Period | Tertile 1 slope (95% CI) | Tertile 2 slope (95% CI) | Tertile 3 slope (95% CI) | Overall P valueb |
|---|---|---|---|---|
| Standard treatment arm | ||||
| SBP | ||||
| ≤6 mo | 6.92 (2.77 to 11.07) | 4.47 (0.09 to 8.85) | 2.11 (−2.65 to 6.86) | .33 |
| >6 mo | 0.00 (−0.41 to 0.42) | 0.22 (−0.20 to 0.63) | 0.26 (−0.22 to 0.74) | .68 |
| DBP | ||||
| ≤6 mo | 3.76 (0.73 to 6.80) | 3.69 (0.68 to 6.70) | 0.38 (−2.81 to 3.58) | .24 |
| >6 mo | −0.55 (−0.86 to −0.24) | −0.50 (−0.80 to −0.19) | −0.56 (−0.89 to −0.22) | .94 |
| Intensive treatment arm | ||||
| SBP | ||||
| ≤6 mo | −12.26 (−16.67 to −7.84) | −11.27 (−16.23 to −6.31) | −14.38 (−19.48 to −9.27) | .67 |
| >6 mo | −0.11 (−0.54 to 0.32) | −0.62 (−1.10 to −0.14) | −0.49 (−0.97 to −0.01) | .19 |
| DBP | ||||
| ≤6 mo | −7.98 (−10.99 to −4.97) | −6.03 (−9.32 to −2.75) | −8.17 (−11.37 to −4.97) | .60 |
| >6 mo | −0.47 (−0.77 to −0.17) | −1.05 (−1.38 to −0.72) | −0.34 (−0.66 to −0.02) | .003 |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
Models were adjusted for age, sex, education level, estimated glomerular filtration rate, history of cardiovascular disease, trial site, and APOL1 risk count.
Overall P value from analysis of variance using the Wald test for comparison of slopes across the 3 groups.
Association of West African Ancestry and Trajectories in Kidney Function Parameters
A consistent decline was noted in eGFR levels across all West African ancestry–based study groups over time, with a more significant reduction noted in the group with the highest West African ancestry proportion (Figure 1C). However, in adjusted linear mixed models, West African ancestry proportion was not associated with levels of eGFR on follow-up after accounting for other baseline covariates, including the presence of APOL1 variants (Table 3; eFigure 3 in the Supplement). No significant interaction was observed between the treatment arm and ancestry-based study groups for the trajectory of eGFR over time. Consistent patterns of results were observed in subgroup analyses stratified by APOL1 risk count (eTable 2 in the Supplement). The temporal trends in levels of BUN and the urine microalbumin-creatinine ratio were also not significantly different between the ancestry-based study groups (Figure 1D and E; eFigure 3 in the Supplement). Additionally, we observed no significant associations between trajectories of eGFR, BUN, or urine microalbumin-creatinine ratio over time and continuous measures of West African ancestry (eTable 5 in the Supplement).
Table 3. Slopes of Linear Mixed Models of Kidney Function Parameters Over Time by West African Ancestry Tertilesa.
| Period | Tertile 1 slope (95% CI) | Tertile 2 slope (95% CI) | Tertile 3 slope (95% CI) | Overall P valueb |
|---|---|---|---|---|
| Standard treatment arm | ||||
| Estimated glomerular filtration rate | ||||
| ≤6 mo | 3.01 (−2.82 to 8.84) | 3.84 (−2.47 to 10.15) | 4.15 (−2.10 to 10.40) | .96 |
| >6 mo | −0.32 (−1.36 to 0.72) | −0.27 (−1.36 to 0.81) | 0.04 (−1.47 to 1.54) | .83 |
| Blood urea nitrogen | ||||
| ≤6 mo | 1.21 (−0.41 to 2.84) | 0.23 (−1.57 to 2.03) | 0.77 (−1.12 to 2.66) | .72 |
| >6 mo | −0.04 (−0.35 to 0.27) | −0.17 (−0.50 to 0.16) | 0.19 (−0.20 to 0.58) | .34 |
| Urine albumin-creatinine ratio | ||||
| ≤6 mo | 0.04 (−0.27 to 0.35) | 0.08 (−0.29 to 0.45) | −0.21 (−0.59 to 0.18) | .93 |
| >6 mo | 0.05 (−0.03 to 0.12) | 0.08 (0.01 to 0.16) | 0.01 (−0.08 to 0.10) | .66 |
| Intensive treatment arm | ||||
| Estimated glomerular filtration rate | ||||
| ≤6 mo | −4.03 (−10.22 to 2.16) | −4.55 (−10.81 to 1.71) | −4.96 (−11.56 to 1.64) | .98 |
| >6 mo | −0.59 (−1.59 to 0.42) | −1.06 (−2.14 to 0.02) | −0.87 (−0.20 to 0.25) | .83 |
| Blood urea nitrogen | ||||
| ≤6 mo | 4.11 (2.09 to 6.12) | 4.72 (2.77 to 6.67) | 5.28 (2.87 to 7.70) | .75 |
| >6 mo | −0.18 (−0.51 to 0.15) | −0.04 (−0.43 to 0.35) | 0.05 (−0.39 to 0.49) | .72 |
| Urine albumin-creatinine ratio | ||||
| ≤6 mo | −0.29 (−0.62 to 0.03) | −0.23 (−0.62 to 0.15) | −0.57 (−0.92 to −0.22) | .51 |
| >6 mo | 0.08 (0.01 to 0.15) | 0.01 (−0.07 to 0.08) | 0.03 (−0.05 to 0.11) | .86 |
Models were adjusted for age, sex, education level, estimated glomerular filtration rate, history of cardiovascular disease, trial site, and APOL1 risk count.
Overall P value from analysis of variance using the Wald test for comparison of slopes across the 3 groups.
Association of West African Ancestry and Trajectories in EKG Measures of LV Mass
A decline was also noted in Cornell voltage on EKG over time in the intensive treatment arm (mean estimate for change in slope over time: tertile 3: −75.2 [95% CI, −105.2 to −45.2] vs tertile 1: −56.9 [95% CI, −87.5 to −26.3]; P = .69), with no difference across the levels of West African ancestry–based tertiles (eTable 6 and eFigure 4 in the Supplement). In the standard treatment arm, the decrease in EKG-based LV mass measures (Cornell voltage) was not significant over time but was comparable across the West African ancestry-based tertiles. Similarly, we observed no significant association between continuous measures of West African ancestry and repeated measures of Cornell voltage on EKG over time (eTable 6 in the Supplement).
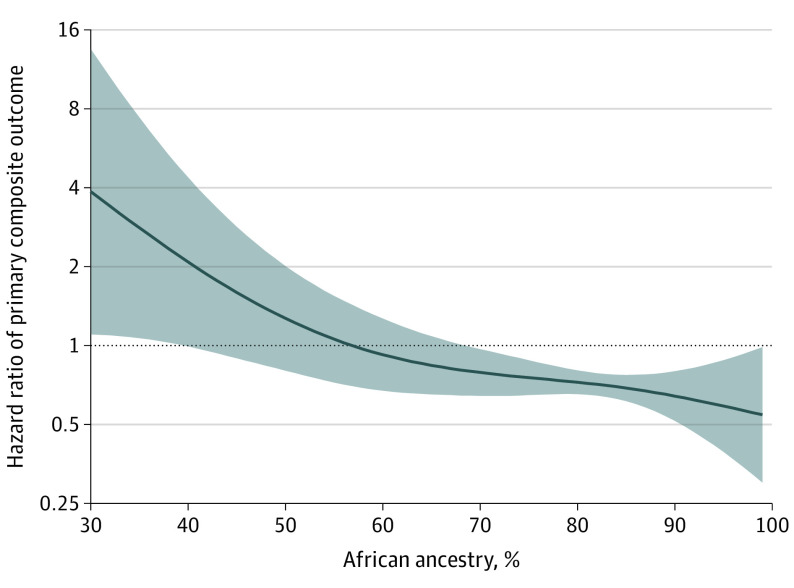
Association of West African Ancestry and the Risk of Primary Composite Outcome
Over a mean (SD) of 3.2 (0.9) years of follow-up, 120 participants (4.9%) and 91 participants (3.7%) experienced a primary composite outcome and all-cause mortality, respectively. In unadjusted analysis, higher continuous measures of West African ancestry proportion were associated with a modestly lower risk of the composite clinical outcome (model 1: hazard ratio per 5% increase, 0.92 [95% CI, 0.86-0.99]; eTable 7 in the Supplement). This association remained significant after adjustment for potential confounders including demographic characteristics, baseline CVD risk factors, and kidney function (model 3: hazard ratio, 0.92 [95% CI, 0.85-0.99]; eTable 7 in the Supplement; Figure 2).
Figure 2. Association of West African Ancestry Proportions With Risk of Primary Composite Outcome.
Continuous association (solid blue line) and 95% CIs (shaded region) between West African ancestry and risk of primary composite outcome using restricted cubic splines. The model was adjusted for age, sex, treatment arm, smoking status, education level, estimated glomerular filtration rate, systolic blood pressure, smoking status, total cholesterol, high-density lipoprotein cholesterol, APOL1 count, and trial site. Primary composite outcome is a composite of myocardial infarction, non–myocardial infarction acute coronary syndrome, stroke, acute decompensated heart failure, or cardiovascular death.
There was no significant interaction between the treatment arm and continuous measures of West African ancestry proportion for the risk of primary composite outcome in the most adjusted model. Similarly, in categorical analysis stratified by West African ancestry–based tertiles, the association between intensive (vs standard) treatment arm and risk of primary composite outcome was comparable across the 3 groups (eFigure 5 in the Supplement).
Association of West African Ancestry and the Risk of All-Cause Mortality
West African ancestry was not significantly associated with the risk of all-cause mortality in unadjusted and adjusted analysis (eTable 7 and eFigure 6 in the Supplement). There was no significant interaction between treatment arm and West African ancestry for the risk of all-cause mortality in the most-adjusted model.
Discussion
In a study of self-identified Black participants in SPRINT, trajectories in BP levels were not different in either study arm by tertile of West African ancestry. There was no difference in the number of antihypertensive agents required to achieve target BP control across the West African ancestry distribution. We observed no differences in temporal trends in kidney function parameters or LV mass (assessed by Cornell voltage) across tertiles of West African ancestry. Finally, a higher proportion of West African ancestry was associated with lower baseline CV risk and a modest but statistically significant lower risk of adverse CV events on follow-up after accounting for potential confounders. To our knowledge, this is the first study to evaluate the association between West African ancestry proportion and longitudinal trends in BP and kidney function in response to treatment and the downstream risk of adverse CV events among self-identified Black US adults.
Disentangling the contributions of genetic, societal, and environmental factors toward disparities in hypertension has important clinical and public health implications for improving care and reducing the morbidity and mortality attributed to hypertension among Black individuals.16 Hypertension affects nearly 1 in 2 Black adults, who additionally experience higher rates of severe, nocturnal, and nondipping phenotypes, as well as reduced responsiveness to standard BP regimens, contributing to notions of an innate biological risk associated with Black race.17,18 In SPRINT, prior studies reported racial differences in the risk of adverse outcomes and the number of antihypertensive medications required to reach the intensive SBP goal. Although no evidence of effect modification was observed by self-reported racial groups for the primary CVD composite outcome, there were race-based differences in the treatment effect for all-cause mortality risk (intensive vs standard BP control: hazard ratios: non-Hispanic Black individuals, 0.92 [95% CI, 0.63-1.35]; non-Hispanic White individuals, 0.61 [95% CI, 0.47-0.80]; P = .008 for the interaction of race and treatment arm). Furthermore, non-Hispanic Black (vs non-Hispanic White) individuals required more antihypertensive agents to achieve BP control.7,19 Although more pronounced racial differences in BP control and CVD events have been described in observational studies, such studies do not entirely account for the societal drivers of disparities. For example, studies of Black participants in the Health and Retirement Study and Family Blood Pressure Program20,21 found that previously observed associations between African ancestry and hypertension prevalence largely disappeared after adjustment for downstream societal risk factors, including low socioeconomic status and access to education. However, 1 factor that is not able to be adjusted for in these analyses is the adverse lived experience of Black adults attributable to systemic racism in a society based on social racial/ethnic groups. In the present study, we observed no association between the proportion of African ancestry and longitudinal changes in BP in response to therapy in a randomized clinical trial setting in which the study design mitigated disparities in treatment access. These findings add to the existing body of literature implicating societal and environmental risk, including socioeconomic factors, educational attainment, access to health care, and structural racism, in the existing disparities in hypertension control and downstream adverse CV events.22
Monogenic variants associated with self-identified Black race and genetic West African ancestry have previously been implicated in the biology of hypertension and downstream risk of LV hypertrophy. Sequence variations involving the Corin I555 allele, for example, have been shown to be associated with salt-sensitive hypertension, and lower circulating levels of natriuretic peptides among Black adults have been linked with higher SBP.23,24 However, known genetic variants cumulatively explain less than 3% of individual variations in BP.20,21,25,26 Although limited to assessment of West African ancestry, our findings suggest that differences in genetic ancestry proportions may not be predominant drivers of population-level disparities in BP control among self-reported Black individuals in the setting of adequate access to antihypertensive therapies.
We also observed a significant but modestly lower risk of adverse cardiovascular events among individuals with higher genetic West African ancestry after adjusting for potential confounders, including traditional CVD risk factors. Prior cohort studies have identified a lower burden of subclinical CVD among individuals with higher West African ancestry proportions.27,28,29 Consistent with these observations, the CVD risk profile was slightly worse among the study participants with lower genetic West African ancestry (ie, higher European ancestry). Our study findings suggest that the higher disproportionate burden of CVD in Black American individuals noted in the community may be more influenced by environmental and societal risk factors than genetic factors.30 Future studies among cohorts of Black individuals with a comprehensive assessment of societal confounders are needed to clarify the mechanisms that might underlie the observed lower risk of adverse CV events among individuals with higher West African ancestry proportions.
We also did not observe any significant associations between genetic West African ancestry and LV mass changes over time after adjustment for other confounders. Prior studies have linked West African ancestry with higher LV mass.31 In an analysis from the Dallas Heart Study, Alame et al31 observed a modest association between higher West African ancestry proportion and higher LV mass and greater prevalence of LV hypertrophy. Consistent with this observation, we noted significantly higher measures of LV mass, as assessed by Cornell voltage on electrocardiogram, at baseline among participants with a higher proportion of West African ancestry. However, LV mass decreased consistently among the intensive control arm participants, with no meaningful differences across West African ancestry–based categories. These findings suggest that the higher LV mass among Black individuals may be largely modifiable across the spectrum of genetic West African ancestry proportion with favorable changes in risk factors, including better control of BP.
Our study findings have important clinical implications. The lack of any adverse association between West African ancestry and clinical outcomes observed in our study adds to the existing evidence against the genetic basis for population-level racial disparities. These findings highlight the continued need to focus on extrinsic and societal factors shown in a growing body of literature to affect hypertension disparities among Black individuals, including structural racism, low socioeconomic status, lack of education, lack of access to care, and experiences of racial segregation and discrimination.22,32 Along these lines, intervention studies aimed at improving access to care among Black individuals, such as the GoodNEWS and Barbershop trials, have demonstrated significant improvements in BP control and cardiovascular risk profile.33,34 Future efforts focused on implementing innovative approaches, including use of mobile technology, to improve access to care, engage disadvantaged communities, and reduce racial biases in public health policies and care delivery are needed to lower the existing disparities in cardiovascular health.33,34,35
Strengths
Our study has several strengths, including the use of a randomized clinical trial population with a standardized, prospective assessment of BP and kidney function outcomes, and blinded clinical adjudication of cardiovascular outcomes. Moreover, although our analysis was limited to a subset of the SPRINT population for whom genetic information was collected, we report findings in more than 2500 patients with elevated cardiovascular risk, representing a larger sample than in previously reported studies from other population-based cohorts.18,31
Limitations
Our study also has some noteworthy limitations. First, there was limited capture of societal and environmental factors that may have influenced the observed associations between West African ancestry and clinical outcomes. Thus, observed associations may be subject to unmeasured and residual confounding. Second, BP assessment was limited to in-office measurements and did not include ambulatory measurements, which have been associated with the risk of LV hypertrophy and downstream complications of hypertension among Black adults in other cohorts.36 Third, we observed a relatively small number of cardiovascular events in our sample, limiting the interpretability of associations between ancestry and cardiovascular outcomes. Fourth, we had only 106 AIMS available for analysis. Prior studies show that the correlation coefficient between estimated ancestry and true individual ancestral proportions is greater than 0.9 when the ancestry is estimated from at least 100 AIMS.10,11 In the current analysis, we used genetic samples of the Nigerian population from HapMap (ie, Yoruba individuals in Ibadan, Nigeria), which serve as a proxy for West and Central African ancestry.37 While these markers vary widely across continental populations, West African genetic ancestry markers are consistent within West and Central African populations. However, this is not a major limitation when assessing the genetic ancestry of African American individuals because the genetic makeup of modern-day African American people has been influenced by admixture during approximately the past 500 years among European settlers, West African individuals who survived the trans-Atlantic slave trade, and Native American people. The literature is consistent in showing that more than 95% of the gene pool of modern-day African American individuals is from West and Central Africa.38,39,40 This is additionally consistent with historical data showing that about 90% of Africans brought to the new world in the trans-Atlantic slave trade were taken from areas in what is now Senegal to Angola. Fifth, local ancestry could not be assessed in the present study; therefore, rarer genetic markers associated with hypertension or new markers could not be evaluated. Finally, we did not have data on the place of birth of study participants and thus could not evaluate differences in BP response and risk of adverse outcomes based on acculturation status or time spent in the US (first generation vs foreign born) among Black American individuals. The current analysis represents an initial step in evaluating the association of genetic ancestry and BP response, and future studies will benefit from a more comprehensive and detailed genetic assessment.
Conclusions
In conclusion, among self-identified Black individuals with elevated cardiovascular risk who participated in the SPRINT trial, we found no significant association between the proportion of West African ancestry and BP, kidney function, and LV mass changes in response to antihypertensive therapy. Furthermore, a higher proportion of West African ancestry was associated with a modest but statistically significant lower risk of adverse cardiovascular outcomes. Although we cannot exclude the role of all genetic variants, our study findings highlight that the racial disparities in hypertension control and associated cardiovascular risk may not be predominantly associated with genetic factors and are more likely driven by extrinsic, societal factors.
eMethods. Study design and clinical covariates and laboratory assessment in SPRINT.
eTable 1. Estimates of linear mixed effect models of blood pressure over time by 5% increase in continuous measures of African ancestry.
eTable 2. Sensitivity analysis of slopes of linear mixed models of systolic blood pressure and eGFR over time by African ancestry categories stratified by APOL1 risk count.
eTable 3. Slopes of linear mixed models of number of anti-hypertensive medications over time by African ancestry categories.
eTable 4. Differences in medication use by classes over time by African ancestry categories in both the standard and intensive blood pressure treatment arms.
eTable 5. Estimates of linear mixed effect models of kidney function parameters over time by 5% increase in continuous measures of African ancestry.
eTable 6. Estimates of linear mixed effect models of Cornell Voltage over time by tertiles of African ancestry and 5% increase in continuous measures of African ancestry.
eTable 7. Adjusted association between continuous measures of African ancestry (per 5% increase) and risk of adverse clinical outcomes as assessed by Cox proportional hazard models.
eFigure 1. Histogram of the percentage of African ancestry in self-reported Black SPRINT participants (n=2,466) in the current analysis.
eFigure 2. Adjusted A) systolic blood pressure and B) diastolic blood pressure over time by treatment group and ancestry tertile.
eFigure 3. Adjusted A) estimated glomerular filtration rate (eGFR), B) blood urea nitrogen (BUN), and C) urine microalbumin/creatinine ratio over time by treatment group and ancestry tertile.
eFigure 4. Adjusted Cornell Voltage over time by treatment group and ancestry tertile.
eFigure 5. Cumulative incidence curves of the primary composite outcome (MI, ACS, stroke, HF and CV death) among intensive vs. standard BP control arms across West African ancestry tertiles with associated hazard ratio.
eFigure 6. Continuous association (solid black line) and 95% confidence interval (dashed red lines) between African ancestry and risk of all-cause mortality using restricted cubic splines.
eReferences.
References
- 1.Thomas SJ, Booth JN III, Dai C, et al. Cumulative incidence of hypertension by 55 years of age in Blacks and Whites: the CARDIA study. J Am Heart Assoc. 2018;7(14):e007988. doi: 10.1161/JAHA.117.007988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190-1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spence JD, Rayner BL. Hypertension in Blacks: individualized therapy based on renin/aldosterone phenotyping. Hypertension. 2018;72(2):263-269. doi: 10.1161/HYPERTENSIONAHA.118.11064 [DOI] [PubMed] [Google Scholar]
- 4.Kaufman JS, Dolman L, Rushani D, Cooper RS. The contribution of genomic research to explaining racial disparities in cardiovascular disease: a systematic review. Am J Epidemiol. 2015;181(7):464-472. doi: 10.1093/aje/kwu319 [DOI] [PubMed] [Google Scholar]
- 5.Mensah GA, Jaquish C, Srinivas P, et al. Emerging concepts in precision medicine and cardiovascular diseases in racial and ethnic minority populations. Circ Res. 2019;125(1):7-13. doi: 10.1161/CIRCRESAHA.119.314970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ambrosius WT, Sink KM, Foy CG, et al. ; SPRINT Study Research Group . The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials. 2014;11(5):532-546. doi: 10.1177/1740774514537404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright JT Jr, Williamson JD, Whelton PK, et al. ; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. doi: 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freedman BI, Rocco MV, Bates JT, et al. ; SPRINT Research Group . APOL1 renal-risk variants do not associate with incident cardiovascular disease or mortality in the Systolic Blood Pressure Intervention Trial. Kidney Int Rep. 2017;2(4):713-720. doi: 10.1016/j.ekir.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langefeld CD, Divers J, Pajewski NM, et al. ; Systolic Blood Pressure Intervention Trial (SPRINT) . Apolipoprotein L1 gene variants associate with prevalent kidney but not prevalent cardiovascular disease in the Systolic Blood Pressure Intervention Trial. Kidney Int. 2015;87(1):169-175. doi: 10.1038/ki.2014.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kosoy R, Nassir R, Tian C, et al. Ancestry informative marker sets for determining continental origin and admixture proportions in common populations in America. Hum Mutat. 2009;30(1):69-78. doi: 10.1002/humu.20822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tsai HJ, Choudhry S, Naqvi M, Rodriguez-Cintron W, Burchard EG, Ziv E. Comparison of three methods to estimate genetic ancestry and control for stratification in genetic association studies among admixed populations. Hum Genet. 2005;118(3-4):424-433. doi: 10.1007/s00439-005-0067-z [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Nyunoya T, Leng S, Belinsky SA, Tesfaigzi Y, Bruse S. Softwares and methods for estimating genetic ancestry in human populations. Hum Genomics. 2013;7:1. doi: 10.1186/1479-7364-7-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang H, Peng J, Wang P, Risch NJ. Estimation of individual admixture: analytical and study design considerations. Genet Epidemiol. 2005;28(4):289-301. doi: 10.1002/gepi.20064 [DOI] [PubMed] [Google Scholar]
- 14.Zakharia F, Basu A, Absher D, et al. Characterizing the admixed African ancestry of African Americans. Genome Biol. 2009;10(12):R141. doi: 10.1186/gb-2009-10-12-r141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Micheletti SJ, Bryc K, Ancona Esselmann SG, et al. ; 23andMe Research Team . Genetic consequences of the transatlantic slave trade in the Americas. Am J Hum Genet. 2020;107(2):265-277. doi: 10.1016/j.ajhg.2020.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gu A, Yue Y, Desai RP, Argulian E. Racial and ethnic differences in antihypertensive medication use and blood pressure control among US adults with hypertension: the National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10(1):e003166. doi: 10.1161/CIRCOUTCOMES.116.003166 [DOI] [PubMed] [Google Scholar]
- 17.Carnethon MR, Pu J, Howard G, et al. ; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council . Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393-e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 18.Booth JN III, Li M, Shimbo D, et al. West African ancestry and nocturnal blood pressure in African Americans: the Jackson Heart Study. Am J Hypertens. 2018;31(6):706-714. doi: 10.1093/ajh/hpy038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Still CH, Rodriguez CJ, Wright JT Jr, et al. ; SPRINT Writing Group . Clinical outcomes by race and ethnicity in the Systolic Blood Pressure Intervention Trial (SPRINT): a randomized clinical trial. Am J Hypertens. 2017;31(1):97-107. doi: 10.1093/ajh/hpx138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marden JR, Walter S, Kaufman JS, Glymour MM. African ancestry, social factors, and hypertension among Non-Hispanic Blacks in the Health and Retirement study. Biodemography Soc Biol. 2016;62(1):19-35. doi: 10.1080/19485565.2015.1108836 [DOI] [PubMed] [Google Scholar]
- 21.Non AL, Gravlee CC, Mulligan CJ. Education, genetic ancestry, and blood pressure in African Americans and Whites. Am J Public Health. 2012;102(8):1559-1565. doi: 10.2105/AJPH.2011.300448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3(2):173-180. doi: 10.1161/CIRCOUTCOMES.109.860841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dries DL, Victor RG, Rame JE, et al. Corin gene minor allele defined by 2 missense mutations is common in blacks and associated with high blood pressure and hypertension. Circulation. 2005;112(16):2403-2410. doi: 10.1161/CIRCULATIONAHA.105.568881 [DOI] [PubMed] [Google Scholar]
- 24.Gupta DK, de Lemos JA, Ayers CR, Berry JD, Wang TJ. Racial differences in natriuretic peptide levels: the Dallas Heart Study. JACC Heart Fail. 2015;3(7):513-519. doi: 10.1016/j.jchf.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Tassell JC, Shimbo D, Hess R, et al. Association of West African ancestry and blood pressure control among African Americans taking antihypertensive medication in the Jackson Heart Study. J Clin Hypertens (Greenwich). 2020;22(2):157-166. doi: 10.1111/jch.13824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Munroe PB, Barnes MR, Caulfield MJ. Advances in blood pressure genomics. Circ Res. 2013;112(10):1365-1379. doi: 10.1161/CIRCRESAHA.112.300387 [DOI] [PubMed] [Google Scholar]
- 27.Shendre A, Irvin MR, Wiener H, et al. Local ancestry and clinical cardiovascular events among African Americans From the Atherosclerosis Risk in Communities study. J Am Heart Assoc. 2017;6(4):e004739. doi: 10.1161/JAHA.116.004739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wassel CL, Pankow JS, Peralta CA, Choudhry S, Seldin MF, Arnett DK. Genetic ancestry is associated with subclinical cardiovascular disease in African-Americans and Hispanics from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Genet. 2009;2(6):629-636. doi: 10.1161/CIRCGENETICS.109.876243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gebreab SY, Riestra P, Khan RJ, et al. Genetic ancestry is associated with measures of subclinical atherosclerosis in African Americans: the Jackson Heart Study. Arterioscler Thromb Vasc Biol. 2015;35(5):1271-1278. doi: 10.1161/ATVBAHA.114.304855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cené CW, Roter D, Carson KA, Miller ER III, Cooper LA. The effect of patient race and blood pressure control on patient-physician communication. J Gen Intern Med. 2009;24(9):1057-1064. doi: 10.1007/s11606-009-1051-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alame AJ, Garg S, Kozlitina J, et al. Association of African ancestry with electrocardiographic voltage and concentric left ventricular hypertrophy: the Dallas Heart Study. JAMA Cardiol. 2018;3(12):1167-1173. doi: 10.1001/jamacardio.2018.3804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thorpe RJ Jr, Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study. Soc Sci Med. 2008;67(10):1604-1611. doi: 10.1016/j.socscimed.2008.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeHaven MJ, Ramos-Roman MA, Gimpel N, et al. The GoodNEWS (Genes, Nutrition, Exercise, Wellness, and Spiritual Growth) Trial: a community-based participatory research (CBPR) trial with African-American church congregations for reducing cardiovascular disease risk factors—recruitment, measurement, and randomization. Contemp Clin Trials. 2011;32(5):630-640. Correction published in Contemp Clin Trials. 2012;33(6):1321. doi: 10.1016/j.cct.2011.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in Black barbershops. N Engl J Med. 2018;378(14):1291-1301. doi: 10.1056/NEJMoa1717250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bakken S, Marden S, Arteaga SS, et al. Behavioral interventions using consumer information technology as tools to advance health equity. Am J Public Health. 2019;109(S1):S79-S85. doi: 10.2105/AJPH.2018.304646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rader F, Franklin SS, Mirocha J, Vongpatanasin W, Haley RW, Victor RG. Superiority of out-of-office blood pressure for predicting hypertensive heart disease in non-Hispanic Black adults. Hypertension. 2019;74(5):1192-1199. doi: 10.1161/HYPERTENSIONAHA.119.13542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.International HapMap Consortium . The International HapMap Project. Nature. 2003;426(6968):789-796. doi: 10.1038/nature02168 [DOI] [PubMed] [Google Scholar]
- 38.Tishkoff SA, Reed FA, Friedlaender FR, et al. The genetic structure and history of Africans and African Americans. Science. 2009;324(5930):1035-1044. doi: 10.1126/science.1172257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salas A, Carracedo A, Richards M, Macaulay V. Charting the ancestry of African Americans. Am J Hum Genet. 2005;77(4):676-680. doi: 10.1086/491675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parra EJ, Marcini A, Akey J, et al. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet. 1998;63(6):1839-1851. doi: 10.1086/302148 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Study design and clinical covariates and laboratory assessment in SPRINT.
eTable 1. Estimates of linear mixed effect models of blood pressure over time by 5% increase in continuous measures of African ancestry.
eTable 2. Sensitivity analysis of slopes of linear mixed models of systolic blood pressure and eGFR over time by African ancestry categories stratified by APOL1 risk count.
eTable 3. Slopes of linear mixed models of number of anti-hypertensive medications over time by African ancestry categories.
eTable 4. Differences in medication use by classes over time by African ancestry categories in both the standard and intensive blood pressure treatment arms.
eTable 5. Estimates of linear mixed effect models of kidney function parameters over time by 5% increase in continuous measures of African ancestry.
eTable 6. Estimates of linear mixed effect models of Cornell Voltage over time by tertiles of African ancestry and 5% increase in continuous measures of African ancestry.
eTable 7. Adjusted association between continuous measures of African ancestry (per 5% increase) and risk of adverse clinical outcomes as assessed by Cox proportional hazard models.
eFigure 1. Histogram of the percentage of African ancestry in self-reported Black SPRINT participants (n=2,466) in the current analysis.
eFigure 2. Adjusted A) systolic blood pressure and B) diastolic blood pressure over time by treatment group and ancestry tertile.
eFigure 3. Adjusted A) estimated glomerular filtration rate (eGFR), B) blood urea nitrogen (BUN), and C) urine microalbumin/creatinine ratio over time by treatment group and ancestry tertile.
eFigure 4. Adjusted Cornell Voltage over time by treatment group and ancestry tertile.
eFigure 5. Cumulative incidence curves of the primary composite outcome (MI, ACS, stroke, HF and CV death) among intensive vs. standard BP control arms across West African ancestry tertiles with associated hazard ratio.
eFigure 6. Continuous association (solid black line) and 95% confidence interval (dashed red lines) between African ancestry and risk of all-cause mortality using restricted cubic splines.
eReferences.