Abstract
Low back pain (LBP) continues to be a challenging condition to manage effectively. Recent guideline recommendations stress providing non-pharmacological care early, limiting diagnostic testing, and reducing exposure to opioid pain medications. However, there has been little uptake of these guideline recommendations by providers, patients or health systems, resulting in care that is neither effective nor safe. This paper describes the framework for an evidence-based pathway that would transform service delivery for LBP in the United States by creating changes that facilitate the delivery of guideline adherent care. An evidence informed clinical service pathway would be intentionally structured to include; a) direct linkages to community and population based resources that facilitate self-management, b) foundational LBP care that is appropriate for all seeking care, c) individualized LBP care for those who have persistent symptoms, and d) specialized LBP care for instances when advanced diagnostics and intensive treatments are indicated. There is an urgent need to transform LBP care by optimizing clinical care pathways focused on multiple opportunities for non-pharmacological treatments, carefully considering escalation of care, and facilitating self-management. Such approaches have the potential to increase patient access to guideline adherent LBP care as an alternative to opioids, unwarranted diagnostic tests, and unnecessary surgery.
Background
Low back pain (LBP) is a nearly ubiquitous human experience second to only upper respiratory infection as a reason for a primary care office visit in the United States (US).[26] Back pain is the leading cause of disability worldwide and in the US,[1] and rates of chronic LBP and resultant disability continue to increase.[30],[55] The societal impact of LBP cannot be attributed to under-treatment. LBP and neck pain were the costliest health condition in the US for 2016, with an estimated $134.5 billion spending paid across private (57%), public (34%), and out of pocket payers.[22] Surgical management of LBP is costly but incurred by a relatively small percentage of LBP cases, while the majority of costs are still incurred by those receiving care in the ambulatory setting.[47] Current ambulatory care practices are characterized by over-utilization of low-value services including advanced imaging, opioid medication and spinal injections.[61; 62] Ineffective LBP management is a significant contributor to the opioid crisis as the most common diagnosis for prescriptions,[69] despite no evidence of sustained benefit.[16; 48] Furthermore, when opioids are prescribed for LBP the risk of chronic opioid use is greater compared to other musculoskeletal pain conditions.[56] Low-value care (i.e. treatments or procedures with little or no evidence of effectiveness, have the potential to cause harm, and are costly) often occurs early in the course of care-seeking for LBP frequently accelerating the escalation of care to more costly services.[24; 47; 53; 70] Perpetuating these care patterns comes at the expense of evidence-based, non-pharmacologic options focused on physical activity and promoting self-management.[27; 37; 47; 53; 70]
The paradox of rapidly increasing resource utilization for LBP with no change in outcomes represents a failure of health care delivery on the part of relevant stakeholders, including patients, payers, health systems and clinicians. LBP evidence-practice gaps have been recognized for many years but have proven difficult to overcome.[21] Improvement efforts in the US, such as the Choosing Wisely campaign, targeted towards both patients and clinicians, focuses on practices within a particular care setting (e.g., primary care, emergency department) leading to varying impact.[42; 59] Given the multitude of practitioners and settings involved in LBP care, it can be argued that the need to transform delivery models spans across and between disciplines[29] with the goal of creating pathways that better align with guideline recommended care.[27] Individuals with a misperception of the need for identifying a definitive cause of LBP contribute to this paradox by increasing resource utilization for imaging.[13; 50] Therefore, existing pathways often facilitate unwarranted, premature escalation of care for LBP due to converging forces from provider, patient, and health system stakeholders. This occurs despite mounting evidence that opioid pain management, invasive procedures and advanced imaging should be limited to the small proportion of patients with very specific indications.[53; 54]
In a “call to action” article published in Lancet, priority was given to improve clinical pathways that focus initial care towards non-pharmacologic approaches and facilitate uptake of self-management strategies.[10] Such alternative pathways have been advocated and implemented in various delivery settings worldwide.,[10; 66] Although designed with the common objective of improving the quality of care provided to individuals with LBP, differing health care policies, practices and resources necessitate adaptations of existing models to local context. The purpose of this Topical Review is to provide the framework for an evidence-based clinical pathway that can transform service delivery for LBP in the US. This Review is intentionally focused on transformation in the context of one country’s health care, but there are general principles described in the proposed framework that are likely to be relevant for the delivery of health care in other countries.
What Do Recent Practice Guidelines Recommend?
The Centers for Disease Control and Prevention Guideline for Prescribing Opioids for Chronic Pain,[23] the American College of Physicians (ACP) Low Back Pain Guideline,[58] and the Federal Pain Research Strategy[2] all provide convergent, updated guidance for pain management. For example, the ACP guideline emphasizes the importance of non-pharmacological treatments as a first care option for acute, sub-acute, and chronic LBP and discourages use of diagnostic imaging, prescription medications, steroid injections, and spinal surgery as early care options.
Why Hasn’t Guideline Adherent LBP Care Already Been Implemented?
There are several barriers that prevent guideline adherent care from being delivered. First, the persistence of fee-for-service payment models and insurance reimbursement policies in the US have incentivized provision of low-value care while simultaneously restricting non-pharmacologic services.[66],[12] Concerns about the costs of LBP care and overreliance on opioid medications has led many to call for changes to payment models to incentivize guideline adherent, non-pharmacologic therapies.[2; 35; 38].
Second, the high prevalence of LBP represents its own challenge. If recommended non-pharmacologic treatments were consistently offered to those seeking care, it is feared that available providers would be overwhelmed by the sheer number of patients. Connections with community services and a consistent focus on promoting self-management are critical considerations for any sustainable pathway.
Finally, existing care pathways create a mismatch between the care appropriate for a patient’s LBP condition, and the type of care typically provided in the setting where a patient accesses care. Patients initiate care for LBP through multiple entry points with notable variability in provider type for a first encounter.[45] As a result, the type of care initially received corresponds with the typical practices of the initial provider. Primary care providers note short consultation times and lack of training on non-pharmacologic treatments as barriers to guideline adherence in their setting.[6; 63] Emergency department providers focus on diagnostic triage and amelioration of acute symptoms, predictably leading to overuse of imaging and opioids in this setting.[52] Furthermore, practice guideline dissemination at the provider level is ineffective in modifying practice behaviors as guidelines are often viewed as being restrictive of practice.[63] LBP is an inherently multi- and trans-disciplinary condition, and thus efforts targeted at individual settings and/or providers are unlikely to have a transformative impact. Transformation will require strategies that range from adjusting the behaviors of individual providers to altering operational patterns of service delivery. It is important that such strategies specifically focus on the needs of multiple stakeholders. For example, payers must be willing to invest in high value care (i.e. treatments or procedures with evidence of effectiveness or prevention, low potential for harm, and are affordable), clinicians require knowledge and skills that are reflective of our contemporary understanding of LBP and existing evidence-based treatment approaches, and patients need increased pain literacy and awareness of high value care options.[8]
Are There Models Available for Informing LBP Clinical Care Pathway Transformation?
Service models for LBP have been reviewed in PAIN, including stepped and stratified care delivery.[51] Each service model has inherent advantages and disadvantages with limited evidence on effectiveness and scalability.[51]
Stepped care begins with all patients receiving low cost, evidence-based options first, with more complex and costly care reserved for those who iteratively fail to respond to preceding steps.[67] Stepped care was first implemented in the US for pain management in the VA Medical System[46] and has been adopted by the Military Health System.[60] Stepped care is advocated for conditions with high prevalence and multiple low intensity intervention strategies that are effective and acceptable to many patients.[7] Stepped care is therefore an attractive service model for LBP. Stepped care has supporting evidence for effectiveness in managing chronic pain and depressive symptoms,[5; 49] however it lacks risk stratification and treatment tailoring that might be beneficial. We draw the following lessons from stepped care:
For recent onset LBP, the lowest cost, yet effective interventions include education and remaining physically active.[3] These interventions can be provided prior to any formal contact with the health system.
Patients with LBP have expectations of treatment that are not evidence-based.[13] The acceptability of patients to effective, low cost interventions must be balanced with their expectations.
Structured, sequential care that considers escalation in a systematic manner can be an effective way to limit exposure to low-value care.
Stratified care exists for many medical conditions, including LBP. Stratified care has the potential to expeditiously direct necessary care to patients in high-risk sub-groups, and reduce over-use for low risk patients. However, the impact of stratification is dependent on the accuracy and stability over time of tools used for initial triage,[51] and the ability to implement the triage step into existing clinical work flows.[11] An example of risk stratification for LBP that is gaining increasing acceptance is the Start Back Screening Tool .[39] Patients are screened with a questionnaire and triaged to follow-up care tailored to decrease that person’s risk for persistent disability.[28; 40] A clinical trial in the US using this tool found no difference in patient outcomes or health utilization. [11] In a process evaluation of the trial, providers had positive ratings for stratified care training, there were no changes in primary care referral rates for matched treatments.[43] These findings highlight the limitation of provider level interventions for changing practice patterns. We draw the following lessons from stratified care:
Care management decisions based on risk for poor outcome instead of diagnostic-based findings is patient-centered and has the potential to be useful for limiting overuse of imaging.
Patients with LBP express concerns when not provided a physiologic diagnosis and when care is perceived as lacking individualization.[4; 18] Patient communication around risk stratification must be considered as a way to alleviate these concerns.
Risk-based triaging provides opportunities to address over-use of low-value care as well as under-use in administering effective high value care for appropriate patients.
How Can Guideline Adherent Care be Delivered at Scale?
In the US, delivering deliberate care for LBP has largely been hampered by limited options between minimal and specialty care; and when such options do exist they are poorly defined, highly variable, and difficult to access. Therefore, there is an opportunity to combine best practice elements from existing models to create a pathway framework specifically designed to improve delivery of guideline adherent care for LBP.[41] The transformed LBP clinical care pathway framework is depicted in Figure 1 and summarized in Table 1. Information in Figure 1 and Table 1 provide guidance on “what” needs to happen to restructure care pathways. Further research in specific settings and systems is required to determine “how” this restructuring will occur.
Figure 1. Framework for a Transformed Low Back Pain Clinical Care Pathway.
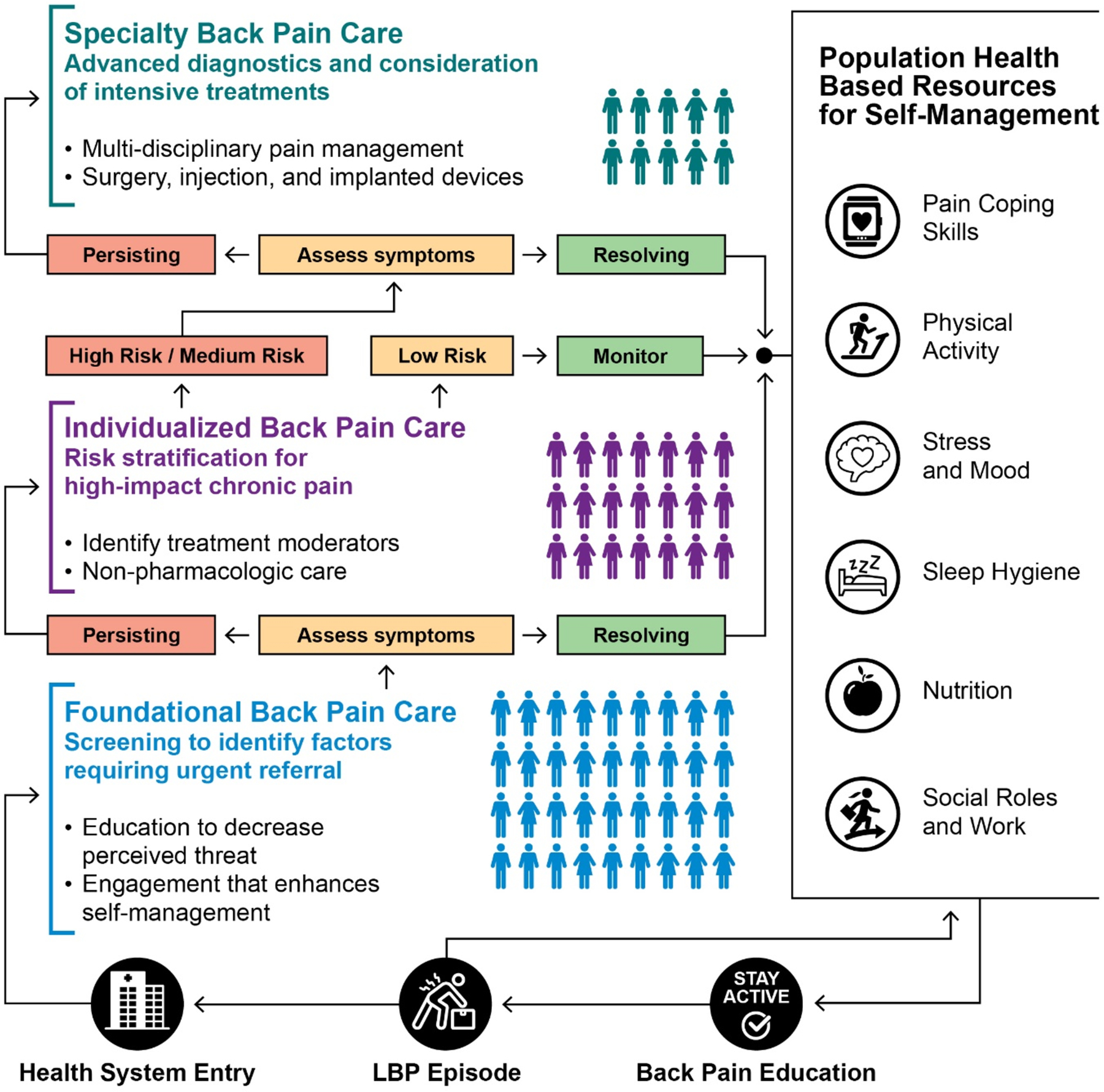
This framework is structured to support guideline adherent care for LBP by aligning the needs of the patient at different phases of care with the type of care received. The pathway is designed to avoid unwarranted care variation by embedding elements of a stepped progression through each phase. Each phase of the pathway includes an aspect of risk stratification and tailoring to a patient’s individual needs. This framework is not designed for a specific provider setting and meant to be tailored based on available resources.
Table 1.
Comparison of Current Clinical Practices and Transformed Care Pathway for Management of Low Back Pain Care
| Current Clinical Practices | Transformed Care Pathway |
|---|---|
Before Care Seeking
|
Before Care Seeking
|
Care Seeking
|
Care Seeking
|
Care Delivery
|
Care Delivery
|
Before Care Seeking:
Population health-based resources for self-management may be a critical element of a transformative LBP pathway because a large proportion of individuals with LBP do not seek health care.[25] Information empowering more people to self-manage an episode of LBP instead of entering the health care system is an important strategy to reduce over-utilization of low value services. Broad-based dissemination of evidence-based information on self-management may help those experiencing a LBP episode to improve beliefs and reduce disablement. For example, a media campaign conducted in Australia was successful in modifying expectations regarding the decision to seek health care[9] and campaigns with similar goals have been tested in other countries.[65] In the US, the Choosing Wisely campaign was designed to change provider and patient attitudes towards low-value care, such as diagnostic imaging for LBP but it was never intended to support patient uptake of self-management options.[65] However, there are education models available that could seed the next wave of media campaigns in the US. For example, healthy US military trainees receiving psychosocial education about back pain reported improved beliefs about consequences and management [34] and reduced back pain related health care seeking over the next 2 years.[33] A similar approach could be implemented in US primary and secondary education. Population health resources can also facilitate self-management in individuals who exit the health system following LBP treatment, consistent with recommendations from the Institute of Medicine and Department of Health and Human Services Interagency Pain Strategy.[17; 44] Health system exit is a critical part of a transformative pathway because there is a critical need for intentional efforts to enhance self-management. Although population health resources will be developed outside the health system, community based partnerships can be created to ensure effective and sustainable strategies are implemented.
Care Seeking:
Foundational back pain care is necessary for every individual who elects to seek health care for LBP. The point of entry is the opportunity for initial risk stratification and tailoring of treatment to guide subsequent care and insure that rare cases needing urgent medical attention are immediately identified. Evidence-based elements of foundational back care include education on the favorable long-term prognosis of LBP without imaging or invasive procedures, maintaining physical activity and building self-management skills.[57; 58; 64] These components can reduce the overall perceived threat of having LBP, enhance confidence in the ability to self-manage the condition and reduce patient perceptions of the need for imaging or early initiation of specialist care. The primary spine practitioner model provides an example of desired provider skills for delivering foundational back pain care.[36] There is flexibility in implementing this model because primary spine care can be delivered by a variety of professionals who are appropriately trained in spine care delivery, including physical therapists, physicians, or chiropractors. Many people who seek health care for LBP do not receive care beyond the initial entry visit.[31] Consistent provision of foundational care is likely to increase the likelihood that a new consulter for LBP will receive the information and reassurance needed to appropriately manage their condition.
Care Delivery:
For those identified as likely to benefit from additional care or those who experience persistent symptoms, individualized back pain care is indicated. The emphasis in this part of the pathway is to fill the existing void between minimal and specialty care by structuring evidence-based non-pharmacologic options. The distinction between care seeking and care delivery is intended to focus attention on the decision to escalate care. In many cases, the provider who performed the initial triage examination described in foundational back pain care will provide individualized, non-pharmacological care. The determination of the specific type and intensity of individualized care should be made with consideration of the patient’s risk stratification and preferences for non-pharmacologic options. Risk stratification should help identify patients at high risk for developing high impact chronic LBP, characterized by persistent pain intensity and lower functional levels.[20] Tailoring treatment to these individuals may require addressing psychosocial risk factors through evidence-based behavioral health strategies such as cognitive behavioral therapy.[20],[15] Systematic reviews of non-pharmacologic interventions for LBP have identified several effective strategies (spinal manipulative therapy, various forms of exercise, etc.) but fail to find substantial differences when these interventions are compared head-to-head.[14] This creates the opportunity for a shared decision-making process in determining specific non-pharmacologic options. Alternatively, this process could be used to consider intensive and/or invasive options when necessary. The overall goal of individualized back care is to limit development of high impact chronic LBP, provide controlled escalation of care, and facilitate self-management upon exit from the health system.
Escalation to specialty back pain care is appropriate for the relatively few individuals whose signs, symptoms, and disablement indicate the need for intensive and/or invasive approaches (e.g. cauda equina syndrome or risk of malignancy). In existing clinical practice, LBP care is often escalated to intensive approaches without clear reason or full consideration of the risks and benefits. A transformed pathway limits reflexive escalation by providing care in a manner that allows patients multiple opportunities to respond to non-pharmacological approaches before intensive approaches are considered. Specialty care may include referral for multi-disciplinary pain management, interventional pain procedures and/or surgical consultation. The goal of specialty care does not differ from the objectives at preceding phases of care; namely to limit the risk for developing or persisting in high impact chronic LBP, and facilitate self-management upon exit from the health system.
What Examples Already Exist in the US?
This framework has yet to be fully implemented within the US, however, there are examples from health systems and medical centers to inform future development. At an overall system level, the VA has initiated a Whole Health approach to care emphasizing many aspects of this framework including self-activation of the person towards improving overall health, making resources available in non-clinical settings, and direct provision of complementary and integrative health services such as acupuncture and chiropractic care.[32] In South Carolina (Greenville Health System) a first provider patient choice model for spine pain resulted in no difference in patient outcomes but lower total costs when seeing a physical therapist first (compared to primary care physician).[19] This example supports provider flexibility in providing foundational spine care. In Washington (Virginia Mason Medical Center) a multidisciplinary team recommended non-operative care for 58% of those already recommended for lumbar spine fusion.[68] This example supports team approaches for specialty back pain care.
Conclusion
Multiple practice guidelines recommend LBP care starts with limited diagnostic imaging and focuses on non-pharmacological treatments. Little progress has been made in improving care delivery for LBP perhaps due to barriers in changing individual provider behavior. In the US transformative progress for LBP care requires changes in service delivery that structure multiple opportunities to receive non-pharmacologic care and facilitate self-management within and outside the health system. A transformed clinical pathway has the potential to increased patient access to high value care for LBP; a change that is likely to improve functional outcomes while decreasing LBP related expenditures.
Funding Acknowledgments:
SZG and SNH were supported by the NIH/NCCIH while writing this paper (UG3AT00970). CG was supported by the NIH/NCCIH while writing this paper (UG3AT009761). JMF was supported by the NIH/NCCIH while writing this paper (UG3AT009763). The Communications Team from the Duke Clinical Research Institute assisted with the development of Figure 1.
Footnotes
Conflict of Interest: The authors have no conflict of interests to report.
Contributor Information
Christine Goertz, Department of Orthopaedic Surgery and Duke Clinical Research Institute Duke University.
S. Nicole Hastings, Geriatrics Division, Department of Medicine Center of the Study of Aging and Human Development, Duke University Durham Center of Innovation to Accelerate Discovery and Practice Transformation Geriatrics Research, Education, and Clinical Center Durham VA Health Care System.
Julie M. Fritz, Department of Physical Therapy & Athletic Training, College of Health University of Utah.
References
- [1].Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London, England) 2016;388(10053):1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].National Institute of Health Intraagency Pain Research Coordinating Committee. Federal Pain Research Strategy., Vol. 2018 Washington, DC: Health and Human Services, 2018. [Google Scholar]
- [3].Abdel Shaheed C, Maher CG, Williams KA, McLachlan AJ. Interventions available over the counter and advice for acute low back pain: systematic review and meta-analysis. J Pain 2014;15(1):2–15. [DOI] [PubMed] [Google Scholar]
- [4].Allvin R, Fjordkvist E, Blomberg K. Struggling to be seen and understood as a person - Chronic back pain patients’ experiences of encounters in health care: An interview study. Nurs Open 2019;6(3):1047–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bair MJ, Ang D, Wu J, Outcalt SD, Sargent C, Kempf C, Froman A, Schmid AA, Damush TM, Yu Z, Davis LW, Kroenke K. Evaluation of Stepped Care for Chronic Pain (ESCAPE) in Veterans of the Iraq and Afghanistan Conflicts: A Randomized Clinical Trial. JAMA internal medicine 2015;175(5):682–689. [DOI] [PubMed] [Google Scholar]
- [6].Bishop FL, Dima AL, Ngui J, Little P, Moss-Morris R, Foster NE, Lewith GT. “Lovely pie in the sky plans”: a qualitative study of clinicians’ perspectives on guidelines for managing low back pain in primary care in England. Spine (Phila Pa 1976) 2015;40(23):1842–1850. [DOI] [PubMed] [Google Scholar]
- [7].Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry 2005;186:11–17. [DOI] [PubMed] [Google Scholar]
- [8].Briggs AM, Slater H, Hsieh E, Kopansky-Giles D, Akesson KE, Dreinhofer KE, March LM, Woolf AD. System strengthening to support value-based care and healthy ageing for people with chronic pain. Pain 2019;160(6):1240–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Buchbinder R, Jolley D. Effects of a media campaign on back beliefs is sustained 3 years after its cessation. Spine 2005;30(11):1323–1330. [DOI] [PubMed] [Google Scholar]
- [10].Buchbinder R, van Tulder M, Oberg B, Costa LM, Woolf A, Schoene M, Croft P. Low back pain: a call for action. Lancet (London, England) 2018;391(10137):2384–2388. [DOI] [PubMed] [Google Scholar]
- [11].Cherkin D, Balderson B, Wellman R, Hsu C, Sherman KJ, Evers SC, Hawkes R, Cook A, Levine MD, Piekara D, Rock P, Estlin KT, Brewer G, Jensen M, LaPorte AM, Yeoman J, Sowden G, Hill JC, Foster NE. Effect of Low Back Pain Risk-Stratification Strategy on Patient Outcomes and Care Processes: the MATCH Randomized Trial in Primary Care. Journal of general internal medicine 2018;33(8):1324–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cherkin DC, Deyo RA, Goldberg H. Time to align coverage with evidence for treatment of back pain. J Gen Intern Med 2019;34(9):1910–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chou L, Ranger TA, Peiris W, Cicuttini FM, Urquhart DM, Sullivan K, Seneviwickrama M, Briggs AM, Wluka AE. Patients’ perceived needs for medical services for non-specific low back pain: A systematic scoping review. PloS one 2018;13(11):e0204885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S, Brodt E. Noninvasive Treatments for Low Back Pain. Comparative Effectiveness Review No. 169. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2012-00014-I.) AHRQ Publication No 16-EHC004-EF. Rockville, MD: Agency for Healthcare Research and Quality;, February 2016. [PubMed] [Google Scholar]
- [15].Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S, Brodt ED. Nonpharmacologic therapies for low back pain: Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017;166(7):493–505. [DOI] [PubMed] [Google Scholar]
- [16].Chou R, Deyo R, Friedly J, Skelly A, Weimer M, Fu R, Dana T, Kraegel P, Griffin J, Grusing S. Systemic pharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med 2017;166(7):480–492. [DOI] [PubMed] [Google Scholar]
- [17].Committee IPRC. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. In: Services UDoHaH editor. Washington, DC, 2016. [Google Scholar]
- [18].De Ruddere L, Goubert L, Stevens MA, Deveugele M, Craig KD, Crombez G. Health care professionals’ reactions to patient pain: impact of knowledge about medical evidence and psychosocial influences. J Pain 2014;15(3):262–270. [DOI] [PubMed] [Google Scholar]
- [19].Denninger TR, Cook CE, Chapman CG, McHenry T, Thigpen CA. The Influence of Patient Choice of First Provider on Costs and Outcomes: Analysis From a Physical Therapy Patient Registry. The Journal of orthopaedic and sports physical therapy 2018;48(2):63–71. [DOI] [PubMed] [Google Scholar]
- [20].Deyo RA, Dworkin SF, Amtmann D, Andersson G, Borenstein D, Carragee E, Carrino J, Chou R, Cook K, DeLitto A, Goertz C, Khalsa P, Loeser J, Mackey S, Panagis J, Rainville J, Tosteson T, Turk D, Von Korff M, Weiner DK. Report of the NIH Task Force on research standards for chronic low back pain. The journal of pain : official journal of the American Pain Society 2014;15(6):569–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, Horst C, Kaldjian A, Matyasz T, Scott KW, Bui AL, Campbell M, Duber HC, Dunn AC, Flaxman AD, Fitzmaurice C, Naghavi M, Sadat N, Shieh P, Squires E, Yeung K, Murray CJL. US Health Care Spending by Payer and Health Condition, 1996–2016. Jama 2020;323(9):863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. Jama 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Feldman DE, Carlesso LC, Nahin RL. Management of Patients with a Musculoskeletal Pain Condition that is Likely Chronic: Results from a National Cross Sectional Survey. The journal of pain : official journal of the American Pain Society 2019. [DOI] [PubMed] [Google Scholar]
- [25].Ferreira ML, Machado G, Latimer J, Maher C, Ferreira PH, Smeets RJ. Factors defining care-seeking in low back pain--a meta-analysis of population based surveys. European journal of pain (London, England) 2010;14(7):747.e741–747. [DOI] [PubMed] [Google Scholar]
- [26].Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, Eurich DT, Lindblad AJ, Vandermeer B, Allan GM. What are the most common conditions in primary care? Can Fam Phys 2018;64:832–840. [PMC free article] [PubMed] [Google Scholar]
- [27].Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet (London, England) 2018;391(10137):2368–2383. [DOI] [PubMed] [Google Scholar]
- [28].Foster NE, Mullis R, Hill JC, Lewis M, Whitehurst DG, Doyle C, Konstantinou K, Main C, Somerville S, Sowden G, Wathall S, Young J, Hay EM. Effect of stratified care for low back pain in family practice (IMPaCT Back): a prospective population-based sequential comparison. Annals of family medicine 2014;12(2):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Fourney DR, Dettori JR, Hall H, Hartl R, McGirt MJ, Daubs MD. A systematic review of clinical pathways for lower back pain and introduction of the Saskatchewan Spine Pathway. Spine 2011;36(21 Suppl):S164–171. [DOI] [PubMed] [Google Scholar]
- [30].Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Archives of internal medicine 2009;169(3):251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fritz JM, Brennan GP, Hunter SJ. Physical therapy or advanced imaging as first management strategy following a new consultation for low back pain in primary care: associations with future health care utilization and charges. Health Serv Res 2015;50:1927–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gaudet T, Kligler B. Whole Health in the Whole System of the Veterans Administration: How Will We Know We Have Reached This Future State? Journal of alternative and complementary medicine (New York, NY) 2019;25(S1):S7–s11. [DOI] [PubMed] [Google Scholar]
- [33].George SZ, Childs JD, Teyhen DS, Wu SS, Wright AC, Dugan JL, Robinson ME. Brief psychosocial education, not core stabilization, reduced incidence of low back pain: results from the Prevention of Low Back Pain in the Military (POLM) cluster randomized trial. BMC medicine 2011;9:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].George SZ, Teyhen DS, Wu SS, Wright AC, Dugan JL, Yang G, Robinson ME, Childs JD. Psychosocial education improves low back pain beliefs: results from a cluster randomized clinical trial (NCT00373009) in a primary prevention setting. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2009;18(7):1050–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Goertz CM, George SZ. Insurer Coverage of Nonpharmacological Treatments for Low Back Pain-Time for a Change. JAMA Netw Open 2018;1(6):e183037. [DOI] [PubMed] [Google Scholar]
- [36].Goertz CM, Weeks WB, Justice B, Haldeman S. A proposal to improve health-care value in spine care delivery: the primary spine practitioner. The spine journal : official journal of the North American Spine Society 2017;17(10):1570–1574. [DOI] [PubMed] [Google Scholar]
- [37].Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ, Underwood M. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–2367. [DOI] [PubMed] [Google Scholar]
- [38].Heyward J, Jones CM, Compton WM, Lin DH, Losby JL, Murimi IB, Baldwin GT, Ballreich JM, Thomas DA, Bicket MC, Porter L, Tierce JC, Alexander GC. Coverage of Nonpharmacologic Treatments for Low Back Pain Among US Public and Private Insurers. JAMA Netw Open 2018;1(6):e183044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE, Hay EM. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum 2008;59(5):632–641. [DOI] [PubMed] [Google Scholar]
- [40].Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason E, Somerville S, Sowden G, Vohora K, Hay EM. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet (London, England) 2011;378(9802):1560–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Hodges PW. Hybrid Approach to Treatment Tailoring for Low Back Pain: A Proposed Model of Care. The Journal of orthopaedic and sports physical therapy 2019;49(6):453–463. [DOI] [PubMed] [Google Scholar]
- [42].Hong AS, Ross-Degnan D, Zhang F, Wharam JF. Small decline in low-value back imaging associated With The ‘Choosing Wisely’ Campaign, 2012–14. Health Aff (Millwood) 2017;36(4):671–679. [DOI] [PubMed] [Google Scholar]
- [43].Hsu C, Evers S, Balderson BH, Sherman KJ, Foster NE, Estlin K, Levine M, Cherkin D. Adaptation and Implementation of the STarT Back Risk Stratification Strategy in a US Health Care Organization: A Process Evaluation. Pain medicine (Malden, Mass) 2019;20(6):1105–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Institute of Medicine. Committee on Advancing Pain Research C, Education Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, DC: National Academies Press, 2011. [PubMed] [Google Scholar]
- [45].Kazis LE, Ameli O, Rothendler J, Garrity B, Cabral H, McDonough C, Carey K, Stein M, Sanghavi D, Elton D, Fritz J, Saper R. Observational retrospective study of the association of initial healthcare provider for new-onset low back pain with early and long-term opioid use. BMJ open 2019;9(9):e028633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Kerns RD, Philip EJ, Lee AW, Rosenberger PH. Implementation of the veterans health administration national pain management strategy. Translational behavioral medicine 2011;1(4):635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, Faterni P, Feng A, Varshneya K, Desai M, Veeravagu A, Ratliff JK. Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA Network Open 2019;2(5):e193676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, Kronenke K, Bair MJ, Noorbaloochi S. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the SPACE randomized clinical trial. JAMA 2018;319:872–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Kroenke K, Bair MJ, Damush TM, Wu J, Hoke S, Sutherland J, Tu W. Optimized antidepressant therapy and pain self-management in primary care patients with depression and musculoskeletal pain: a randomized controlled trial. Jama 2009;301(20):2099–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Lim YZ, Chou L, Au RT, Seneviwickrama KMD, Cicuttini FM, Briggs AM, Sullivan K, Urquhart DM, Wluka AE. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. Journal of physiotherapy 2019;65(3):124–135. [DOI] [PubMed] [Google Scholar]
- [51].Linton SJ, Nicholas M, Shaw W. Why wait to address high-risk cases of acute low back pain? A comparison of stepped, stratified, and matched care. Pain 2018;159(12):2437–2441. [DOI] [PubMed] [Google Scholar]
- [52].Machado GC, Rogan E, Maher CG. Managing non-serious low back pain in the emergency department: time for a change? Emerg Med Australas 2018;20(2):279–282. [DOI] [PubMed] [Google Scholar]
- [53].Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA internal medicine 2013;173(17):1573–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine 2019;44(5):369–376. [DOI] [PubMed] [Google Scholar]
- [55].Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A, Werdecker A, Carter A, Zipkin B, Sartorius B, Serdar B, Sykes BL, Troeger C, Fitzmaurice C, Rehm CD, Santomauro D, Kim D, Colombara D, Schwebel DC, Tsoi D, Kolte D, Nsoesie E, Nichols E, Oren E, Charlson FJ, Patton GC, Roth GA, Hosgood HD, Whiteford HA, Kyu H, Erskine HE, Huang H, Martopullo I, Singh JA, Nachega JB, Sanabria JR, Abbas K, Ong K, Tabb K, Krohn KJ, Cornaby L, Degenhardt L, Moses M, Farvid M, Griswold M, Criqui M, Bell M, Nguyen M, Wallin M, Mirarefin M, Qorbani M, Younis M, Fullman N, Liu P, Briant P, Gona P, Havmoller R, Leung R, Kimokoti R, Bazargan-Hejazi S, Hay SI, Yadgir S, Biryukov S, Vollset SE, Alam T, Frank T, Farid T, Miller T, Vos T, Barnighausen T, Gebrehiwot TT, Yano Y, Al-Aly Z, Mehari A, Handal A, Kandel A, Anderson B, Biroscak B, Mozaffarian D, Dorsey ER, Ding EL, Park EK, Wagner G, Hu G, Chen H, Sunshine JE, Khubchandani J, Leasher J, Leung J, Salomon J, Unutzer J, Cahill L, Cooper L, Horino M, Brauer M, Breitborde N, Hotez P, Topor-Madry R, Soneji S, Stranges S, James S, Amrock S, Jayaraman S, Patel T, Akinyemiju T, Skirbekk V, Kinfu Y, Bhutta Z, Jonas JB, Murray CJL. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 2018;319(14):1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Moshfegh J, George SZ, Sun E. Risk and Risk Factors for Chronic Opioid Use Among Opioid-Naive Patients With Newly Diagnosed Musculoskeletal Pain in the Neck, Shoulder, Knee, or Low Back. Annals of internal medicine 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Pangarkar SS, Kang DG, Sandbrink F, Bevevino A, Tillisch K, Konitzer L, Sall J. VA/DoD clinical practice guideline: diagnosis and treatment of low back pain. J Gen Intern Med 2019;34:2620–2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of internal medicine 2017. [DOI] [PubMed] [Google Scholar]
- [59].Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y, Li C, DeVries A. Early trends among seven recommendations from the choosing wisely campaign. JAMA internal medicine 2015;175(12):1913–1920. [DOI] [PubMed] [Google Scholar]
- [60].Ryu J, Lee TH. The waiting game - why providers may fail to reduce wait times. The New England journal of medicine 2017;376:2309–2311. [DOI] [PubMed] [Google Scholar]
- [61].Schwartz AL, Jena AB, Zaslavsky AM, McWilliams JM. Analysis of physician variation in provision of Low-value services. JAMA internal medicine 2019;179(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Schwartz AL, Zaslavsky AM, Landon BE, Chernew ME, McWilliams JM. Low-value service use in provider organizations. Health Serv Res 2018;53(1):87–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Slade SC, Kent P, Patel S, Bucknall T, Buchbinder R. Barriers to Primary Care Clinician Adherence to Clinical Guidelines for the Management of Low Back Pain: A Systematic Review and Metasynthesis of Qualitative Studies. The Clinical journal of pain 2016;32(9):800–816. [DOI] [PubMed] [Google Scholar]
- [64].Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, Andersen MO, Fournier G, Hojgaard B, Jensen MB, Jensen LD, Karbo T, Kirkeskov L, Melbye M, Morsel-Carlsen L, Nordsteen J, Palsson TS, Rasti Z, Silbye PF, Steiness MZ, Tarp S, Vaagholt M. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J 2018;27(1):60–75. [DOI] [PubMed] [Google Scholar]
- [65].Suman A, Armijo-Olivo S, Deshpande S, Marietta-Vasquez J, Dennett L, Miciak M, Reneman M, Werner EL, Straube S, Buchbinder R, Gross DP. A systematic review of the effectiveness of mass media campaigns for the management of low back pain. Disability and rehabilitation 2020:1–29. [DOI] [PubMed] [Google Scholar]
- [66].Traeger AC, Buchbinder R, Elshaug AG, Croft PR, Maher CG. Care for low back pain: can health systems deliver? Bulletin of the World Health Organization 2019;97(6):423–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Von Korff M, Moore JC. Stepped care for back pain: activating approaches for primary care. Ann Intern Med 2001;134:911–917. [DOI] [PubMed] [Google Scholar]
- [68].Yanamadala V, Kim Y, Buchlak QD, Wright AK, Babington J, Friedman A, Mecklenburg RS, Farrokhi F, Leveque JC, Sethi RK. Multidisciplinary Evaluation Leads to the Decreased Utilization of Lumbar Spine Fusion: An Observational Cohort Pilot Study. Spine 2017;42(17):E1016–e1023. [DOI] [PubMed] [Google Scholar]
- [69].Young JC, Jonsson Funk M, Dasgupta N. Medical use of long-term extended-release opioid analgesics in commercially insured adults in the United States. Pain medicine (Malden, Mass) 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Zheng P, Kao MC, Karayannis NV, Smuck M. Stagnant physical therapy referral rates alongside rising opioid prescription rates in patients with low back pain in the United States 1997–2010. Spine 2017;42(9):670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]


