Abstract
Background
Outlet obstruction constipation accounts for about 30% of chronic constipation (CC) cases in a referral practice.
Aims
To assess the proportion of patients with CC diagnosed with descending perineum syndrome (DPS) by a single gastroenterologist; to compare clinical, radiological and associated features in DPS compared to patients with constipation.
Methods
We conducted a review of records of 300 consecutive patients evaluated for constipation by a single gastroenterologist from 2007–2019, including medical, surgical, and obstetrics history, digital rectal examination, anorectal manometry, defecation proctography (available in 15/23 with DPS), treatment and follow-up. DPS was defined as >3cm descent of anorectal junction on imaging or estimated perineal descent on rectal examination. Logistic regression with univariate and multivariate analysis compared factors associated with DPS to non-DPS patients.
Results
23/300 (7.7%, all female) patients had DPS; these patients were older, had more births [including more vaginal deliveries (84.2% vs. 31.2% in non-DPS, p<0.001)], more instrumental or traumatic vaginal deliveries, more hysterectomies, more rectoceles on proctography (86.7% vs. 28.6% non-DPS, p=0.014), lower squeeze anal sphincter pressures (p<0.001), and lower rectal sensation (p=0.075) than non-DPS. On univariate logistic regression, history of vaginal delivery, hysterectomy, and Ehlers-Danlos syndrome increased the odds of developing DPS. Vaginal delivery was confirmed as a risk factor on multivariate analysis.
Conclusions
DPS accounts for almost 10% of tertiary referral patients presenting with constipation. DPS is associated with age, female gender and number of vaginal (especially traumatic) deliveries.
Keywords: pelvic floor retraining, vaginal deliveries, rectal examination
Introduction
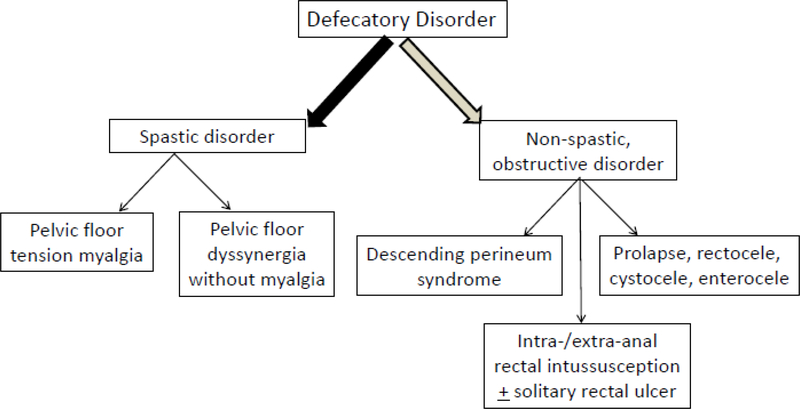
Chronic constipation affects 20% of adults based on epidemiological studies [1] and contributes to significant morbidity and decreased quality of life [2] for the patient, as well as increased healthcare utilization leading to increased societal costs [3]. The differential diagnosis of constipation includes obstruction to defecation by a mucosal lesion such as a polyp or stricture, normal transit, slow transit, and outlet obstruction constipation. After excluding rectal or colonic obstruction by a mucosal lesion, outlet obstruction constipation accounts for about 50% of referrals to a tertiary care practice [4] and can be further divided into three main categories: spastic pelvic floor disorders (pelvic tension myalgia, pelvic floor dyssynergia), anatomical rectal obstruction disorders (including mucosal prolapse, rectocele/cystocele, intra- and extra-anal rectal intussusception with or without solitary rectal ulcer syndrome), and descending perineum syndrome (DPS) (Figure 1). DPS is generally recognized as a form of constipation occurring in the context of pelvic organ prolapse and the need for consideration of pelvic floor repair; therefore, many scholarly articles and contributions in the field are provided by colorectal or urogynecological surgeons, as illustrated elsewhere [5]. However, there is a need for gastroenterologists, who see the majority of patients with chronic constipation not responding to first line therapy, to recognize and manage patients with DPS. The hallmark symptom of DPS is frequent and excessive straining accompanied by incomplete evacuation. The repetitive straining may also lead to mucus discharge and perineal discomfort, which is often deep and poorly localized [6,7].
Figure 1.
Classification of defecatory disorders, after exclusion of rectal or colonic obstruction (e.g. by mucosal lesions or strictures).
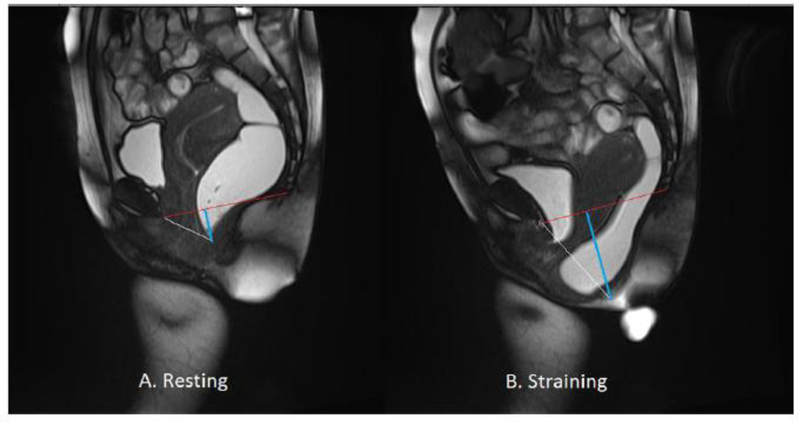
Descending perineum syndrome was first described in 1966 by Parks et al. [8] and was initially defined as a caudal movement of the anorectum at least 4 cm below the pubococcygeal line or ischial tuberosity, based on imaging studies [9]. This caudal movement of the anorectum with straining pulls the rectum downwards around the puborectalis muscle leading to outlet obstruction during attempted defecation (Figure 2). Descending perineum syndrome likely develops as a consequence of excessive straining and incomplete defecation leading to further straining. A second contributing factor is pelvic floor weakness [10]. Predictive factors recognized for development of DPS include female gender, multiparity with vaginal delivery, obstructed labor, rectoceles, prior pelvic floor surgery, and hysterectomy or cystocele/rectocele repair [7,11,12].
Figure 2.
Magnetic resonance proctogram of patient with descending perineum syndrome. MR proctogram pictures obtained at (A) rest and (B) strain. Red line delineates pubococcygeal line (PCL); white line delineates anorectal junction (ARJ); thick blue line measures descent of the ARJ below PCL; A) Rest image shows a 1.2cm descent of ARJ. B) During simulated evacuation, there is 6.4cm descent of the ARJ below the PCL.
Prolonged DPS in patients with constipation may lead to neuropathic injury resulting in denervation of the external anal sphincter and puborectalis and, possibly, sensory loss that may manifest as reduced rectal sensation and an abnormal rectoanal inhibitory reflex [13]. All of these features appear to result from stretch injury to the terminal portion of the pudendal nerve (which supplies the external anal sphincter) and the sacral roots (which supply the puborectalis), and, ultimately, neuropathic injury may lead to fecal incontinence [13,14].
The prevalence of DPS ranges from 5.7 to 73.3% of patients with constipation, depending on the cohort studied [15–17]. Descending perineum syndrome predominantly affects females; however, one study of 100 patients with severe idiopathic constipation reported DPS in 87% of men in the cohort. The wide range of prevalence and gender distribution suggests there is referral or specialty bias in the cohorts from which the data emanate. There are still questions regarding DPS in gastroenterology practices focused on functional gastrointestinal and motility disorders, specifically, “What is the proportion of patients with constipation who are diagnosed with DPS?” and “What are the associated features?”
The aim of our study was to evaluate patients diagnosed with DPS and compare their clinical and radiological features and associated factors to those of patients with constipation without DPS. We evaluated a consecutive cohort of 300 patients evaluated by a single gastroenterologist. We also reviewed any treatments and surgical repairs undertaken for DPS and associated features, as described in the literature [18–20].
Methods
A retrospective review was conducted of medical records of 300 consecutive patients who were evaluated for constipation from 2007–2019 by a single gastroenterologist. The study was exempt from requiring patient consent by the Mayo Clinic Institutional Review Board. Only patients who had previously authorized consent to use their records for research purposes were included. Databases containing electronic medical records were screened and data were collected via the Mayo Clinic Advanced Cohort Explorer (ACE) in order to identify patients with constipation and DPS. ACE is a clinical data repository maintained by the Unified Data Platform and uses natural language processing for data retrieval.
Medical, surgical, and obstetrics histories, digital rectal exam, anorectal manometry in all patients, and defecating proctography reports, if available, were extracted. Review of associated urinary symptoms was undertaken, given previously reported increase in urinary symptoms in patients with defecatory disorders (21). Treatment and follow-up information were obtained when available. Diagnosis of DPS was determined either by proctogram, defined as anorectal junction descent of >3 cm below the pubococcygeal plane during strain, or on clinical evaluation by a single experienced observer (MC) by estimated excessive (>3 cm) perineal descent on rectal exam. Defecography was performed in 65% of the patients with clinically-diagnosed DPS when there was suspicion of other complicating anatomical defects; MRI defecography was the modality of choice except when it was contraindicated in 1 patient. Defecography was performed in 4% of the patients with constipation in whom DPS was not suspected clinically.
Descriptive statistics were utilized to compare characteristics between the DPS vs. non-DPS patients with constipation. Continuous variables were evaluated with t-tests assuming unequal variance. Nominal variables were evaluated using Fisher’s exact tests. All p-values are two-tailed and a cut-off of 0.05 was utilized for statistical significance. Analysis for predictors of DPS was based on the factors that were nominally significant (p<0.05) in the comparisons between DPS and non-DPS constipation (as identified in Tables 1, 2 and 3). Logistic regression with univariate and multivariate analysis (the latter based on factors that were nominally significant on univariate analysis) was performed to evaluate variables that may predict DPS as a contributor to constipation.
Table 1.
Demographics and Obstetrics History
| DPS | Other Constipation | P-value | |
|---|---|---|---|
| Total (N) | 23 | 277 | |
| Female (N, %) | 23 (100%) | 223 (80.5%) | 0.02 |
| Age (years) (mean, 95% CI) | 50.2 (43.4–57.0) | 41.7 (39.7–43.7) | 0.03 |
| BMI (kg/m2) (mean, 95% CI) | 22.1 (20.0–24.3) | 22.9 (22.3–23.6) | 0.34 |
| Ehlers-Danlos syndrome (N, %) | 5 (21.7%) | 7 (2.5%) | 0.0009 |
| Obstetrics History | |||
| Percent who had at least one delivery (N, %) |
17 (77%) | 85 (41.5%) | 0.0015 |
| Percent who had at least one vaginal delivery (N, %) | 16 (84.2%) | 64 (31.4%) | <0.001 |
| Percent who had at least one traumatic vaginal delivery* (N, %) | 5 (26.3%) | 23 (11.3%) | 0.071 |
| Average number of births (mean, 95% CI) (median, IQR) |
2.24 (1.72–2.75) 2 (1.5–3) |
0.94 (0.78–1.10) 0 (0–2) |
0.0006 |
| Hysterectomy (N, %) | 8 (42.1%) | 27 (16.2%) | 0.012 |
episiotomy, tear, forceps or vacuum used
Table 2.
Proctogram Findings (Fluoroscopic and MRI)
| DPS | Other Constipation | P-value | |
|---|---|---|---|
| Proctograms performed Fluoroscopic MRI Nuclear Medicine |
65.2% (n=15) 6.67% (n=1) 93.3% (n=14) 0 |
3.97% (n=11) 54.5% (n=6) 9.1% (n=1) 36.4% (n=4) |
<0.0001 |
| ARJ maximal descent (cm) below PCL median (IQR) |
7.5 (2.9) | 2.7 (4.3) | 0.019 |
| Rectocele | 86.7% (n=13) | 28.6% (n=2) | 0.014 |
| Enterocele* | 13.3% (n=2) | 0 | |
| Cystocele* | 53.3% (n=8) | 14.29% (n=1) | 0.106 |
medium or large included and small (<2cm) ignored; ARJ=anorectal junction; MRI=magnetic resonance imaging; PCL=pubococcygeal line
Table 3.
Anorectal Manometry and Rectal Exam [data show mean (SD) or %]
| DPS Constipation | Non-DPS Constipation | P-value | |
|---|---|---|---|
| N | 20 | 275 | |
| Anorectal Manometry | |||
| Maximum pressure at rest (mmHg) | 83.2 (69.60–96.80) | 95.0 (91.4–98.7) | 0.051 |
| Maximum pressure with squeeze (mmHg) | 138.8 (106.9–170.7) | 174.5(165.9–183.1) | 0.0006 |
| Volume to first rectal sensation (mL) | 41.67 (28.86–54.5) | 37.03 (33.7–40.4) | 0.53 |
| Volume to rectal urge sensation (mL) | 93.33 (67.75–118.9) | 71.9 (65.2–78.6) | 0.27 |
| Volume to rectal discomfort sensation (mL) | 154.12 (119.5–88.7) | 111.3 (102.4–120.2) | 0.075 |
| Digital Rectal Examination | |||
| Estimated mean pelvic floor descent (cm) | 3.38 | 2.15 | 0.0023 |
| Puborectalis tenderness (%) | 13.4 | 34.6 | 0.038 |
| Increased resting anal sphincter tone (%) | 8.7 | 31.6 | 0.03 |
| Paradoxical contraction (%) | 22.7 | 50.8 | 0.014 |
Results
Demographics and prevalence
A total of 300 charts were evaluated; 23 (7.7%) patients had DPS, diagnosed by either defecating proctogram or clinical features. A higher proportion of DPS patients were female (100%) compared to 80.5% of patients with constipation without DPS (p=0.02). Patients with DPS were older at diagnosis (mean: 50 years of age vs. 42 years of age; p=0.03) compared to non-DPS patients. BMI was similar between the two groups (Table 1). In addition, 22% of the patients with DPS and only 2.5% of patients with other constipation had a diagnosis of or clinical suspicion of having Ehlers-Danlos syndrome hypermobility type, a collagen vascular disorder associated with increased flexibility of joints and elasticity in soft tissues (p=0.0009) (Table 1).
Obstetrics history
A larger proportion of DPS patients had delivered at least one child (by vaginal delivery or Cesarian section) compared to non-DPS patients (77% vs. 41.5%; p=0.0015). DPS patients had more vaginal deliveries compared to non-DPS (84.2% in DPS vs. 31.4% in non-DPS; p<0.001) with more instrumental deliveries (defined as forceps or vacuum assisted) or traumatic deliveries defined by history of episiotomy and/or tears associated with deliveries, although this was not statistically significant (26.3% in DPS vs.11.3% in non-DPS; p=0.071). Overall, patients with DPS gave birth to more children (mean 2.24±1.47 vs. 0.94±1.17; p=0.0006) and underwent more hysterectomies (42.1% vs. 16.2%; p=0.012) (Table 1).
Urinary symptoms
Urinary symptoms were separated into day time frequency/urgency, nocturia, urinary incontinence, incomplete emptying/retention/hesitancy with bladder emptying, recurrent urinary tract infections (≥2 in women, ≥1 in men), urinary pain. Presence of symptoms in any category was considered positive for urinary symptoms for analysis and each category was analyzed separately. Overall, 60.9% of patients with DPS had at least one urinary symptom compared to 48.7% of non-DPS, though this was not statistically significant (p=0.29). However, patients with DPS had significantly higher rates of daytime frequency/urgency, with 43.5% reporting this symptom compared to 22.2% of non-DPS patients (p=0.038). Mean number of urinary symptoms did not differ significantly between the two groups.
Defecation proctography findings
Fluoroscopic, MRI, or nuclear medicine based proctograms were performed in 65% of the DPS patients (15/23) and in 4% of non-DPS patients (Table 2). Patients with DPS had a greater median anorectal junction descent at maximal strain (7.5 cm) compared to patients with constipation without DPS (2.7 cm, p=0.019). A higher proportion of DPS patients had anterior rectoceles (86.7% vs. 28.6%) and more medium or large enterocele and/or cystoceles compared to non-DPS patients, although this numerical difference was not statistically significant due to low numbers or absence of enteroceles in the non-DPS group.
Rectal exam and anorectal manometry findings
On digital rectal exam, DPS patients had less puborectalis tenderness (p=0.039), lower prevalence of elevated resting sphincter tone (p=0.03), and paradoxical contraction of the pelvic floor or anal sphincters (p=0.015) (Table 3).
On anorectal manometry, there was numerically lower anal sphincter pressure at rest (p=0.051) and significantly lower anal sphincter pressure during squeeze (p=0.0008) in DPS patients compared to non-DPS patients. Balloon distension in the rectum showed overall similar volumes to sensation between the two groups (to first sensation, and sensation of urge to defecate); however, there was a numerically increased threshold volume for rectal discomfort in patients with DPS (p=0.075), suggesting reduced rectal sensation to discomfort (Table 3).
Treatment
Of the 23 patients with DPS, 6 (26.1%) underwent medical management only, 4 (17.4%) underwent surgical procedures, and 12 (52.2%) were referred for pelvic floor rehabilitation with 1 (4.3%) patient undergoing both ventral rectopexy and pelvic floor retraining. The 4 surgical procedures performed in 4 patients were: colectomy with loop ileostomy, fibroid removal, repair of rectocele enterocele, hysterectomy with bilateral salpingo-oophorectomy along with endometriosis excision and hysterectomy with sacropexy, rectocele, cystocele repair, and bladder sling.
Among the patients who underwent pelvic floor rehabilitation, 6/12 (50%) had improvement in symptoms, although these were predominantly assessed during the time of training and long-term follow-up was not available. Two (16.67%) patients undergoing medical management had improved results. The patient with retraining and surgical treatment had short-term improvement, but had recurrence of symptoms after 6 months. The improvement rate among conservative versus surgical management strategies was not significantly different.
Among the patients who underwent surgical procedures, three of the four procedures resulted in improvement of symptoms, although the fourth patient experienced complications including vaginal bleeding and urinary retention which required repeat operation and adjustment of the urethral sling. The one patient who underwent colectomy did not have symptomatic improvement.
Factors associated with DPS on univariate and multivariate analysis
On univariate analysis, age and abnormal findings on anorectal manometry were weak predictors of DPS. History of delivery was associated with a 4.8 times higher odds of DPS; moreover, vaginal delivery was associated with an 11.7 times higher odds of DPS. There was a 2 times increase in odds in DPS for every childbirth. History of hysterectomy had a 3.7 times higher odds of DPS, and presence of a rectocele was associated with 16.3 times higher odds of DPS. Patients with a diagnosis of Ehlers-Danlos syndrome (hypermobility type) had a 10.7 times higher odds of having DPS (Table 4).
Table 4.
Univariate Regression for Predictors of DPS
| Predictor | Odds Ratio | 95% CI | P-value |
|---|---|---|---|
| Age (odds per unit change) | 1.03 | 1.004–1.06 | 0.02 |
| Presence of rectocele | 16.25 | 1.78–148.8 | 0.0066 |
| History of delivery | 4.8 | 1.7–13.5 | 0.003 |
| History of vaginal delivery | 11.67 | 3.38–41.5 | <0.0001 |
| Total number of births (odds per unit change) | 2.07 | 1.5–2.9 | <0.001 |
| Hysterectomy | 3.71 | 1.4–10.1 | 0.0132 |
| Maximum squeeze pressure on ARM | 0.99 | 0.98–0.999 | 0.024 |
| Volume to discomfort | 1.006 | 1.0–1.01 | 0.036 |
| Puborectalis tenderness (%) | 0.28 | 0.08–0.98 | 0.023 |
| Increased resting tone (%) | 0.21 | 0.05–0.92 | 0.012 |
| Paradoxical contraction (%) | 0.28 | 0.10–0.79 | 0.009 |
| Diagnosis of Ehlers-Danlos syndrome | 10.7 | 3.09–37.1 | 0.0007 |
ARM = anorectal manometry
However, on multivariate analysis, the only significant, independent predictor was history of vaginal delivery which conferred a 6.49 times higher odds of DPS (95% CI, 1.17–36.1; p=0.03), controlling for age, history of hysterectomy and delivery trauma.
Discussion
In our cohort of patients with constipation seen at a tertiary care center, 7.7% of patients were found to have descending perineum syndrome. This experience may be limited by the tertiary referral nature of the practice, which represents patients with refractory constipation. Our evaluation of risk factors supports prior studies of the pathophysiology and development of this condition. Rectal exam findings differentiated spastic pelvic floor conditions (high resting anal pressures, paradoxical contraction and pelvic tension myalgia) from descending perineum syndrome in a significant number of patients. It is interesting to note that the resting and squeeze sphincter pressures were lower in comparison with the rest of the constipation group among whom, 31.6% had increased resting anal sphincter tone and 50.8% had paradoxical contraction of the pelvic floor on DRE. The lower anal sphincter pressure during squeeze is consistent with the 100% female gender and 77% with at least one child delivered. Among the patients with DPS, a minority had manometric evidence of dyssynergic defecation on DRE (e.g. 22.7% paradoxical contraction or 13.4% puborectalis tenderness) and on anorectal manometry.
Proctography identified increased propensity for associated rectoceles compared to constipated patients without DPS. The findings on proctography illustrate the obstructed defecation resulting from prolapse or laxity leading to excessive straining and further pressure on the anterior rectal wall. This increased pressure results from the vector of forces associated with straining that starts from a relatively acute rectoanal angle. Enteroceles and cystoceles were also numerically increased in the DPS cohort compared to patients without DPS and constipation. One patient with mutations in COL1A1 gene with constipation associated with DPS and Ehlers-Danlos syndrome had also been reported elsewhere [19].
History of hysterectomy and vaginal delivery, as well as a history of Ehlers-Danlos syndrome hypermobility type were predictive for DPS on univariate analysis, particularly, the history of vaginal deliveries (which was also significant on multivariate analysis). This corroborates prior studies showing pelvic surgeries and vaginal deliveries as risk factors for development of DPS [11,18]. History of vaginal delivery was more predictive for DPS development than history of instrumentation or trauma during vaginal delivery, and remained significant on multivariate analysis which controlled for history of hysterectomy, age, and delivery trauma. It is unclear how these factors interact to lead to development of DPS, and future research is required, including assessment of the impact of avoidance of instrumental or traumatic vaginal deliveries to prevent the morbidity with constipation and fecal incontinence associated with DPS in later years.
Diagnosis of DPS during the assessment of patients with chronic constipation is important for appropriate management; however, treatment options for DPS are limited. The clinical significance of pelvic organ prolapse seen on imaging is not always correlated to size (e.g., mucosal prolapse, rectocele) or length (e.g., perineal or recto-anal angle descent) of the radiographic finding. Involvement of colleagues in urogynecology and colorectal surgery when appropriate is important to guide treatment plans. While pelvic floor rehabilitation is the mainstay for pelvic floor dyssynergia, this treatment had limited success in improving pelvic floor laxity once DPS is established. Harewood et al. reported 30% of DPS patients who underwent pelvic floor rehabilitation and responded to follow-up questionnaires had resolution of constipation, and those patients who responded to pelvic floor retraining showed lesser degrees of pelvic floor descent compared to those who did not respond to rehabilitation [7]. Prior studies recommend conservative management focused on targeting symptom improvement, with less emphasis given to improving pelvic laxity [12]. Although 50% of patients reported improvement with pelvic floor rehabilitation in short-term follow-up, it is unclear if this improvement persisted beyond completion of the period of rehabilitation. Conservative management (separate from pelvic floor rehabilitation) was also associated with limited improvement in constipation symptoms [12].
Our experience with outcomes related to surgical management of DPS is limited. The literature suggests that, when DPS is associated with pelvic organ prolapse, sacral colpoperineopexy (with mesh placed between the bladder and vagina, rectum and sacral concavity, vaginal and rectum, and posteriorly for uterosacral fixation if rectocele is present) has shown cure rates of 95% for low stage pelvic organ prolapse, with 77% subjective patient satisfaction. However, 7% of patients reported worsening symptoms after surgery [19]. Less aggressive procedures with a smaller amount of mesh placement have been proposed with good short-term outcomes in small cohorts, although long-term effects have not been reported [20,22].
It is important to note that, as of April 2019, the FDA has ordered all manufacturers to discontinue distribution of surgical mesh intended for transvaginal repair of pelvic organ prolapse in the anterior compartment (cystoceles) due to concerns regarding safety and efficacy. This order followed on the FDA’s prior order in July 2018 to discontinue use of surgical mesh in the posterior compartment for rectocele repair. Therefore, further surgical management of both pelvic organ prolapse and DPS will likely require new techniques and further study to determine efficacy.
Strengths and limitations
A major strength of this analysis is that it is based on clinical appraisal by the same experienced gastroenterologist, and the diagnosis was based on standard digital rectal examination in the left lateral position, with confirmation on defecography which was performed using the same supine method (MRI defecography) in 14/15 patients of the 23 with DPS. This standardization of DRE and 14/15 MR defecography virtually excludes any risk of misclassification.
Limitations are reflected in the tertiary referral nature of the patient cohort with probably refractory constipation and the fact that 4% of the patients with constipation without clinical evidence of DPS underwent defecography. However, the exclusion of defecography in the evaluation of all patients with chronic constipation is consistent with expert assessment that the diagnostic value of defecography is unclear, and its utility greatest when ARM and balloon expulsion test are equivocal, or inability to evacuate a balloon is associated with ability to relax the pelvic floor normally during simulated defecation [23]. A third limitation is that the proportion of non-DPS patients undergoing defecography was only 4% and therefore the percentages of patients with rectoceles or enteroceles in these two different groups may be inaccurate particularly because the DPS group underwent almost exclusively MRI defecography, whereas, the non-DPS group underwent predominantly barium or nuclear medicine defecography. The literature has identified discrepancies in the accuracy of different imaging methods in these diagnoses [24]. Our cohort consists of patients treated by a single physician at a tertiary care referral center, which limits the number of patients and the gender diversity. In such a medical records study, the lack of standardization among providers in documentation of associated symptoms ( such as urological symptoms) and the limited recognition of descending perineum syndrome as a component of pelvic floor dysfunction prevented examination of the same observations in medical records from patients treated by other providers to allow for meaningful comparison of data for review. A final limitation is that the rationale for the different treatments cannot be deciphered in such a retrospective study, and the outcomes observed are not generalizable. Future prospective cohorts may need to be identified to study a larger number of patients of both genders and collect more imaging data.
Conclusions
Descending perineum syndrome accounts for almost 10% of tertiary referral constipation patients and is associated with concomitant rectoceles, older age, more pregnancies, more vaginal deliveries, and Ehlers-Danlos syndrome hypermobility type. A larger number of vaginal deliveries is a significant predictor, even on multivariate analysis adjusted for confounders. Patients with DPS can be considered for pelvic rehabilitation if there is limited laxity, whereas patients with concomitant pelvic organ prolapse may require surgical repair, although efficacy without the use of transvaginal mesh (following FDA recall) is unclear.
Acknowledgement
The authors thank Mrs. Cindy Stanislav for excellent secretarial assistance.
Grant support: Michael Camilleri is supported by grant R01-DK115950 from National Institutes of Health.
Conflicts of interest: Michael Camilleri receives research support unrelated to this manuscript from Allergan and Takeda. The other authors have no conflicts of interest.
References
- 1.Choung RS, Locke GR 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Cumulative incidence of chronic constipation: a population-based study 1988–2003. Aliment Pharmacol Ther 2007;26:1521–1528. [DOI] [PubMed] [Google Scholar]
- 2.Koloski NA, Jones M, Wai R, Gill RS, Byles J, Talley NJ. Impact of persistent constipation on health-related quality of life and mortality in older community-dwelling women. Am J Gastroenterol 2013;108:1152–1158. [DOI] [PubMed] [Google Scholar]
- 3.Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 2019;156:254–272, e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Surrenti E, Rath DM, Pemberton JH, Camilleri M. Audit of constipation in a tertiary referral gastroenterology practice. Am J Gastroenterol 1995;90:1471–1475. [PubMed] [Google Scholar]
- 5.Payne I, Grimm LM Jr. Functional disorders of constipation: paradoxical puborectalis contraction and increased perineal descent. Clin Colon Rectal Surg 2017;30:22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andromanakos N, Skandalakis P, Troupis T, Filippou D. Constipation of anorectal outlet obstruction: pathophysiology, evaluation and management. J Gastroenterol Hepatol 2006;21:638–646. [DOI] [PubMed] [Google Scholar]
- 7.Harewood GC, Coulie B, Camilleri M, Rath-Harvey D, Pemberton JH. Descending perineum syndrome: audit of clinical and laboratory features and outcome of pelvic floor retraining. Am J Gastroenterol 1999;94:126–130. [DOI] [PubMed] [Google Scholar]
- 8.Parks AG, Porter NH, Hardcastle J. The syndrome of the descending perineum. Proc R Soc Med 1966;59:477–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim AY. How to interpret a functional or motility test - defecography. J Neurogastroenterol Motil 2011;17:416–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lembo A, Camilleri M. Chronic constipation. N Engl J Med 2003;349:1360–1368. [DOI] [PubMed] [Google Scholar]
- 11.Snooks SJ, Setchell M, Swash M, Henry MM. Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet 1984;2:546–50. [DOI] [PubMed] [Google Scholar]
- 12.D’Amico DF, Angriman I. Descending perineum syndrome: iatrogenic or spontaneous pathology? Chir Ital 2000;52:625–630. [PubMed] [Google Scholar]
- 13.Bartolo DC, Read NW, Jarratt JA, Read MG, Donnelly TC, Johnson AG. Differences in anal sphincter function and clinical presentation in patients with pelvic floor descent. Gastroenterology 1983;85:68–75. [PubMed] [Google Scholar]
- 14.Bartolo DC, Jarratt JA, Read MG, Donnelly TC, Read NW. The role of partial denervation of the puborectalis in idiopathic faecal incontinence. Br J Surg 1983;70:664–667. [DOI] [PubMed] [Google Scholar]
- 15.Karasick S, Karasick D, Karasick SR. Functional disorders of the anus and rectum: findings on defecography. AJR Am J Roentgenol 1993;160:777–782. [DOI] [PubMed] [Google Scholar]
- 16.Andrade LC, Correia H, Semedo LC, Ilharco J, Caseiro-Alves F. Conventional videodefecography: Pathologic findings according to gender and age. Eur J Radiol Open 2014;1:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rafiei R, Bayat A, Taheri M, Torabi Z, Fooladi L, Husaini S. Defecographic findings in patients with severe idiopathic chronic constipation. Korean J Gastroenterol 2017;70:39–43. [DOI] [PubMed] [Google Scholar]
- 18.Pucciani F, Boni D, Perna F, Bassotti G, Bellini M. Descending perineum syndrome: are abdominal hysterectomy and bowel habits linked? Dis Colon Rectum 2005;48:2094–2099. [DOI] [PubMed] [Google Scholar]
- 19.Nessi A, Kane A, Vincens E, Salet-Lizée D, Lepigeon K, Villet R. Descending perineum associated with pelvic organ prolapse treated by sacral colpoperineopexy and retrorectal mesh fixation: preliminary results. Front Surg 2018;5:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petros PE. Tissue fixation system perineal body repair: a minimally invasive method for repair of descending perineal syndrome. Dis Colon Rectum 2016;59:e455. [DOI] [PubMed] [Google Scholar]
- 21.Brandler J, Camilleri M. Pretest and post-test probabilities of diagnoses of rectal evacuation disorders based on symptoms, rectal exam, and basic tests: A systematic review. Clin Gastroenterol Hepatol 2019. December 4 pii: S1542–3565(19)31389–8. doi: 10.1016/j.cgh.2019.11.049. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Renzi A, Brillantino A, Di Sarno G, et al. Transverse perineal support: a novel surgical treatment for perineal descent in patients with obstructed defecation syndrome. Dis Colon Rectum 2016;59:557–564. [DOI] [PubMed] [Google Scholar]
- 23.Rao SS, Bharucha AE, Chiarioni G, et al. Functional anorectal disorders. Gastroenterology 2016;150:1430–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Gruting IMA, Stankiewicz A, Kluivers K, et al. Accuracy of four imaging techniques for diagnosis of posterior pelvic floor disorders. Obstet Gynecol 2017;130:1017–1024. [DOI] [PubMed] [Google Scholar]