Abstract
The health issue addressed is the unmet need to universally screen and treat depression, which is one of the most common mental health disorders among adults in the United States. The US Preventive Services Task Force recommends screening adults for depression in primary care and using evidence-based protocols. This quality improvement project implemented VitalSign6, a measurement-based care program, to improve depression screening and treatment of adults in primary care at an academic medical center. A pre-post design was used to determine effectiveness of changes in screening, outcomes, and satisfaction. Of 1200 unique adult patients, 95.4% received initial screening. Providers diagnosed and administered measurement-based care to 236 patients. After 14 weeks, 27.5% returned for at least 1 follow-up. Results showed a statistically significant decrease in self-reported depression scores from baseline to follow-up. VitalSign6 was effective in improving identification and management of depression in primary care.
Keywords: depression, screening, primary care, community health
Background
Depression is one of the most common mental disorders in the United States. The prevalence of at least 1 major depressive episode among US adults aged 18 years or older, was 17.3 million, representing 7.1% of all US adults.1 Depression is disabling and costly,2-9 with an estimated $210 billion annual medical care and lost productivity cost.3,10 Untreated depression causes emotional suffering, reduced productivity, lost wages, impaired relationships, and increased comorbidity risk.3,5,11 With the inextricable link between mental and physical health,4,8,12 evidence shows depression concomitant with serious chronic diseases.4,6,7
A strong body of evidence supports depression screening and treatment in primary care to provide early identification and intervention.13-20 The US Preventive Services Task Force (USPSTF) recommends screening adults, 18 years of age and older, for depression and combining screening with support systems and evidence-based protocols.5,11,21-25 The American Academy of Family Physicians endorses USPSTF’s recommendations.5,24,25 The Centers for Medicare & Medicaid Services (CMS) new value-based payment models further emphasize USPSTF screening recommendations.26 Accountable care organizations participating in CMS’s Medicare Shared Savings Program must meet quality performance benchmarks for depression screening, follow-up planning, and remission rates to earn shared savings.26,27
The largest prospective randomized clinical trial of depression, the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) supported screening for and treating depression in primary care.28-34 This landmark trial was implemented over 5 years, across 41 primary care and specialty sites, included 4041 adults, 18 to 75 years of age, and represented a broad range of socioeconomic and ethnic groups.29,34,35 The STAR*D trial found depression treated in primary care produced quality outcomes on par with specialty care.28,30,36 The results of this study are widely published and provide guidance and clinical implications for managing patients with moderate depressive disorder in primary care.30-32,35,36,37 However, despite increased attention to depression screening and treatment from research and national guidelines over 50% of patients in primary care still are unrecognized and undertreated.5,20,38,39 The national depression screening rate from 2005 to 2015 was 1.4%, and 2.2% of primary care physician office visits included depression screening for adults, 18 years of age and older.4,14,38,40,41
Efforts to improve depression identification and treatment in primary include increased use of screening tools. The Patient Health Questionnaire (PHQ)–2 and PHQ-9 are the most commonly used adult depression screening tools and demonstrate clinical utility and diagnostic accuracy.5,18,20,23,38,42-44 The PHQ-2 was designed to be used as the first step in the screening process and if positive, to be followed with the more comprehensive PHQ-9.20,45 The PHQ-2 tool consists of 2 questions about frequency of depressed mood and anhedonia, scoring each as 0 (“not at all”) to 3 (“nearly every day”).45 A PHQ-2 score ≥3 was shown to have a sensitivity of 83% and a specificity of 92% for detecting major depression.45,46 The PHQ-9 consists of 9-items based on the 9 DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, fifth edition) criteria for major depressive disorder.47 Scores of 5, 10, 15, and 20 represent mild, moderate, moderately severe, and severe depression respectively.46-48
Meta-analysis of pooled data from 14 760 primary care adults with depressive disorder found both PHQ-2 and PHQ-9 to be effective, valid, and reliable for detecting depression in primary care.5 Meta-analysis and systematic reviews indicate the best outcomes and long-term remission in depression care comes from combining screening with systems of care.5,11,17,18,23 The American College of Preventive Medicine specifies that systems of care include standardized screening tools, treatment protocols, and established specialty referral systems.31 Measurement-based care (MBC) is a comprehensive guideline offering validated screening tools, standard symptom measurements, treatment effects and adherence monitoring, and evidence-based decision tools to support primary care physicians with diagnosis, treatment, follow-up, and referrals.20,28,37,49-54 Future efforts must optimize technology innovation to equip primary care providers with tools to seamlessly integrate screening and MBC with existing workflow. The University of Texas Southwestern Medical Center for Depression Research and Clinical Care (CDRCC) developed an MBC program called VitalSign6 and built an application programming interface enabling interoperability with the electronic health record (EHR).
Purpose and Specific Aims
The purpose of this quality improvement project was to implement VitalSign6, an evidence-based MBC program, to improve identification and management of depression in adult patients, 18 years and older, at the University of Texas Southwestern Medical Center (UTSW), Department of Family and Community Medicine. The specific aims were to
Screen 75% of unique patients for depression using PHQ-2.
Screen 85% of PHQ-2 positive patients for depression using PHQ-9.
Administer MBC to 75% of patients diagnosed with depression and schedule follow-up in 4 to 6 weeks.
Monitor responses, treatment effects, and remission using VitalSign6 MBC.
Assess satisfaction of physicians and staff with theVitalSign6 and EHR integration.
The rates for screening and MBC intervention were adopted from the VitalSign6 Primary Care First Model for depression screening and MBC.20
Methods
A pre-post intervention design to improve screening rates and subsequent referrals was used to assess screening effectiveness, clinical outcomes, and satisfaction. The setting was UTSW Department of Family and Community Medicine. The study was reviewed and approved by the Institutional Review Board of UTSW Medical Center with a waiver of the need to obtain informed consent from individual patients.
The clinic has a residency program, a broad payor mix, and monthly volume of 585 patient visits. The project began on February 6, 2019, and initial screening continued through May 31. Patients diagnosed with depression and administered MBC were followed for 14 additional weeks.
Evidence-Based Innovation
There is convincing evidence supporting the use of MBC to drive evidence-based care when treating depression in primary care.36,37,44 The CDRCC developed VitalSign6, a web-based MBC program that offers primary care providers tools for standard measures and systematic assessment of symptom severity, antidepressant side effects, adherence behavior, and tailored medication selection using algorithm-based dosing with decision support and consultation.6,20,55-57 Primary care providers using VitalSign6 can tailor their treatment approach to the individual patient by selecting appropriate medications, adequate dosing, appropriate referrals, and follow-up that adhere to evidence-based guidelines.20
The VitalSign6 software utilizes a web-based application to administer depression questionnaires on an iPad, in both English and Spanish. The application allows patients to complete self-reported measures of depression symptoms during check-in within the clinic’s existing workflow and allows the provider to review results in real-time, document diagnosis and begin tailored treatment planning using clinical decision support (CDS).20,55 If the patient screens negative for depression, VitalSign6 software triggers rescreening in 1 year.
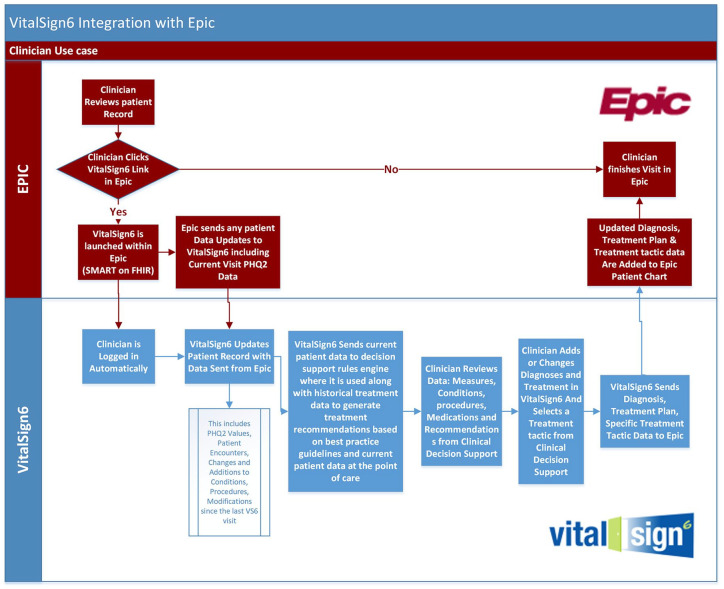
VitalSign6 has been successfully implemented in community-based clinics affiliated with UTSW6,20,51,55,57 but has not been implemented in the Department of Family Medicine and Community Health. Greenhalgh’s diffusion of innovation theory58 addresses complexity of healthcare information systems and identification of barriers and facilitators to new technologies and system changes. Barriers and facilitators to implementing VitalSign6 in the faculty practice clinics centered on interoperability with the EHR. To address this issue, a UTSW technology team developed an application programming interface, using Fast Healthcare Interoperability Resources (FHIR) and Substitutable Medical Apps Reusable Technology (SMART), enabling VitalSign6 integration in real-time directly into the EHR Epic database. These tools enabled physicians to trigger a context-sensitive launch of VitalSign6 within Epic Hyperspace window, review patient measures, clinical decision support data, and then send specific treatment tactics in VitalSign6 to the patient chart in real time. Figure 1 shows VitalSign6 integration with Epic.
Figure 1.
VitalSign6 integration with Epic.
Clinic Training and Stakeholder Engagement
The authors demonstrated the innovation with departmental leadership and worked with clinical staff to assess current operations and workflow integration to minimize disruption. Two-hour in-person training sessions were held for 25 physicians and residents, and 20 clinic staff. Training included depression education, screening, standard measures for symptom severity, diagnosis, and best treatment practices, medication and dosing, and referrals. VitalSign6 expert trainers remained onsite for 2 weeks to provide immediate assistance.
Procedure
Initial Screening
An approved Patient Acknowledgement Form was developed by the CDRCC and acknowledged by patients prior to screening. Patients presenting for an initial visit were given the Epic Welcome tablet to complete the 2-item PHQ-2. Epic Welcome electronically transferred PHQ-2 values to patient’s EHR. PHQ-2 scores range from 0 to 6, if the patient screened negatively with a score of 2 or less and had no history of depression or depression treatment documented in the EHR, staff proceeded with routine workflow.
If the patient screened positive for depression, or screened negative, but had a history of depression or antidepressant medication documented in the EHR, the Best Practice Advisor (BPA) opened to advise the nurse to have patient complete screening with the 9-item PHQ-9 using VitalSign6 iPad to assess if the patient’s symptoms were mild, moderate, or severe. The patient’s self-reported scores were electronically added to the EHR in real-time. Self-report of depression symptoms reduces stigma attached to depression screening and promotes truthful reporting of symptoms.20,55
Self-reported depression measures were presented in Epic allowing the physician to review scores, update conditions, procedures, and medications. VitalSign6 included a checklist for diagnosis and decision support to allow tailoring a patient-specific treatment plan. Treatment plan options available to the providers were pharmacological treatment using MBC, behavioral treatment such as psychotherapy with behavioral health providers integrated in the clinic, exercise plans, continue symptomatic monitoring, referral to a specialist, or no further follow-up. Program functionality supported scheduling follow-up in 4 to 6 weeks to evaluate patient’s progress.
Follow-up Visit
During check-in at follow-up, the patient completed PHQ-9 and other standard measures. Based on patient’s self-reported measures and the physician’s clinical assessment, decision support tools were available to continue or modify treatment, schedule follow-up, or refer a patient to a specialist or for counseling. The MBC program equipped the physician with tools to systematically manage, treat, and refer based on symptom response.
Provider and Staff Satisfaction
A Likert-type scale survey tool developed by the CDRCC was administered pre and post project implementation for a qualitative assessment of provider and staff satisfaction with and perceptions of depression care. Physicians and staff were asked questions about their knowledge of depression, comfort level talking with patients about depression, where they thought depression screening and treatment should occur, and perceptions of the most and least valuable aspects of VitalSign6. Mann-Whitney U tests were used for paired, Likert-type scale items. At the end of the post-survey, providers and staff were asked 2 open-ended questions about the most challenging and the most valuable aspects of using VitalSign6. Qualitative analysis was used to identify themes from the provider and staff written responses.
Outcome Measures and Analysis
Outcome measures were developed using the Specific, Measurable, Achievable, Relevant, and Time-Bound framework.59 Descriptive statistics were used for measurement of program fidelity. Fidelity was measured by the number of patients screened for depression relative to the total number of unique patient visits, the number of patients with positive screens relative to the total patients screened, and the number of patients with a positive depression screen who were administered MBC and scheduled follow-up. A clinical outcome measured changes in patients’ baseline and follow-up self-reported PHQ-9 scores. A paired t test was used to compare baseline and follow-up scores. A process outcome measured physician and staff beliefs and satisfaction with VitalSign6. Mann-Whitney U tests were used for paired, Likert-type scale items. Data were collected using the EHR and UTSW’s REDCap survey database. All statistical tests were conducted using IBM SPSS v.25 with alpha set to .05.
Results
Sample and Screening Rates
Between February 6 and May 31, 2019, 1200 unique adult patients, 18 years and older, were seen in the clinic: 44.5% (n = 534) were male and 55.5% (n = 666) female; ages ranged from 18 to 94 years with the average being 46.7 years.
Of 1200 patients, 95.4% (n = 1145) were screened with PHQ-2 and 18.2% (n = 208) screened positive (PHQ-2 >2). Of patients with positive PHQ-2 screens, 89.4% (n = 186) were screened with the PHQ-9. As a result of technical issues, software failed to record positive PHQ-2 screens and associated PHQ-9 assessment in 10.5% (n = 22) patients.
Of patients screened with the PHQ-2 (n = 1145), 18.6% (n = 214) had a negative screen, but had a history of depression or antidepressant medication documented in the EHR, triggering the BPA to advise the nurse to have patient continue screening. Additionally, 7.1% (n = 81) of patients with negative PHQ-2 scores and no history of depression or antidepressant medication were screened with PHQ-9 per physician request.
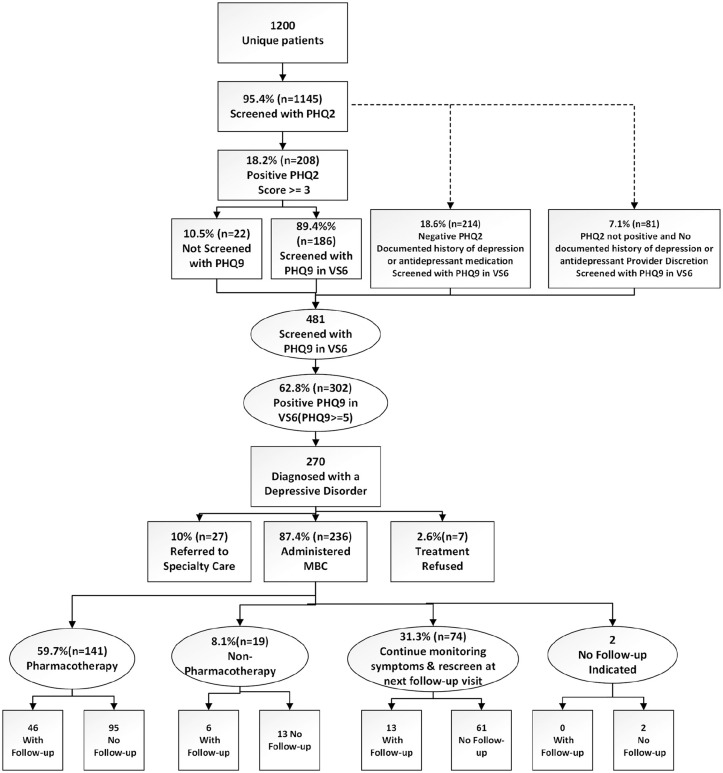
A total of 481 patients were screened with PHQ-9, 62.8% (n = 302) screened positive with a score of >4, and of those, 89.4% (n = 270) were diagnosed with a depressive disorder. Of 270 patients diagnosed, 10% (n = 27) were referred to specialty care, 2.6% (n = 7) refused treatment, and 87.4% (n = 236) began MBC with personalized treatment plans.
Depression Follow-up
Patients diagnosed with depressive disorder and started on a personalized treatment plan were scheduled for a follow-up visit in 4 to 6 weeks. Of the patients (n = 236) diagnosed with a depressive disorder and administered MBC, 59.7% (n = 141) received pharmacological treatment, 8.1% (n = 19) received nonpharmacological treatment, 31.3% (n = 74) were recommended for symptomatic monitoring and rescreening at next follow-up appointment, and 2 patients had no follow-up indicated. Patients diagnosed with depression and started on a treatment plan were followed for 14 weeks. A CONSORT (Consolidated Standards of Reporting Trials) flow diagram of the progress through treatment and follow-up is shown in Figure 2.
Figure 2.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
Changes in Depression Scores at Follow-up
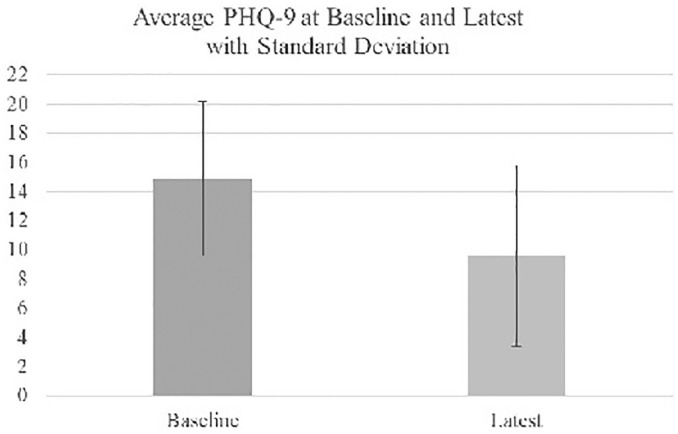
To measure changes in patients’ baseline and follow-up self-reported PHQ-9 scores, a paired t test was conducted on 65 patients with complete data. These were patients diagnosed with a depressive disorder, receiving individualized treatment and had at least 1 follow-up visit within the 14-week period. Patients demonstrated changes in self-reported depression scores with the mean score dropping from 14.89 to 9.58. These scores reflect a statistically significant decrease in self-reported PHQ-9 score from baseline. Figure 3 shows comparison of PHQ-9 scores at baseline and follow-up. Of those patients, 23.1% (n = 15/65) reached remission with a PHQ-9 score <5. No PHQ-9 <5 remissions were documented in the clinic prior to VitalSign6 implementation.
Figure 3.
The 9-item Patient Health Questionnaire (PHQ-9) self-reported scores at baseline and follow-up.
Physician and Staff Satisfaction
Physician Survey Results
Twenty-five physicians completed the pre-survey and 56% (n = 14) completed the post-survey. A statistically significant (P = .002) difference was found in physicians’ perceived importance of depression screening and MBC, surprisingly, was lower post project implementation. Physician survey results are shown in Table 1.
Table 1.
Provider Survey Results.a
| Provider survey items | Provider | P | |
|---|---|---|---|
| Pre, median (min, max) | Post, median (min, max) | ||
| How frequently are you currently treating depression?b | 4.5 (3, 5) | 4 (3, 5) | .466 |
| My current understanding of depression is:c | 4 (3, 5) | 4.5 (3, 5) | .912 |
| Depression is a chronic medical illness.d | 5 (3, 5) | 4.5 (3, 5) | .217 |
| Depression in primary care patients is common.d | 5 (4, 5) | 5 (4, 5) | .287 |
| Depression should mostly be treated by psychiatrists.d | 1 (1, 5) | 2 (1, 3) | .494 |
| Primary care is the best setting to screen for depression.d | 5 (3, 5) | 4 (3, 5) | .051 |
| When treating depression, it is important to use measures to assess symptoms.d | 5 (4, 5) | 4 (3, 5) | .002 |
| I believe that it is important to screen patients for depression in my clinic.d | 5 (4, 5) | 4 (4, 5) | .002 |
| I can accurately diagnose patients who screen positive for depression.d | 4 (3, 5) | 4 (4, 5) | .328 |
| I am very familiar with how to use antidepressant medications.d | 4 (2, 5) | 4 (1, 5) | .471 |
| I feel confident in knowing when to change antidepressant medications.c | 4 (2, 5) | 4 (1, 4) | .270 |
| I know what medications can be used to augment an antidepressant medication.d | 4 (2, 5) | 4 (1, 4) | .562 |
| I feel comfortable talking with my patients about their mental health.d | 5 (3, 5) | 4.5 (4, 5) | .474 |
| How easy is the VitalSign6 software program to use with your daily workflow?e | na | 2.5 (1,4) | nc |
| How easy is the VitalSign6 software program to use in the presence of patients?e | na | 2.5 (1, 4) | nc |
| Overall, how easy is the VitalSign6 software program to use?e | na | 3 (2, 4) | nc |
| How useful is the VitalSign6 software program in following a patient’s status over time?f | na | 3.5 (1, 4) | nc |
| How useful do you find the treatment recommendations (clinical decision support) provided by the VitalSign6 software program?f | na | 1.5 (1, 4) | nc |
| Overall, how useful is the VitalSign6 software program?f | na | 3 (1, 4) | nc |
| How often does the VS6 software program draw your attention to issues or problems the patient is having that need to be addressed?g | na | 3.5 (2, 5) | nc |
| To what extent has the VitalSign6program as a whole (training + VitalSign6 software + access to consulting clinicians) improved the quality of patient care that you are able to provide?h | na | 3 (1, 4) | nc |
Abbreviations: na, nc.
Mann-Whitney U tests were used for paired, Likert-type scale items.
Response scale: 1 = Never to 5 = Very Frequently.
Response scale: 1 = Very Poor to 5 = Very Good.
Response scale: 1 = Strongly Disagree to 5 = Strongly Agree.
Response scale: 1 = Very Difficult to 5 = Very Easy.
Response scale: 1 = Not Useful to 5 = Very Useful.
Response scale: 1 = Never to 5 = Often.
Response scale: 1 = Not at all Improved to 5 = Very Much Improved.
Staff Survey Responses
Twenty staff completed the pre-survey and 40% (n = 8) completed the post-survey. Results showed a significant difference (P = .044) in staff’s comfort level talking with patients about their mental health. Staff survey results are shown in Table 2.
Table 2.
Staff Survey Results.a
| Staff survey items | Staff | P | |
|---|---|---|---|
| Pre, median (min, max) | Post, median (min, max) | ||
| My current understanding of depression is:b | 3 (3, 5) | 4 (3, 5) | .362 |
| Depression is a chronic medical illness.c | 4 (3, 5) | 4.5 (2, 5) | .935 |
| Depression in primary care patients is common.c | 4 (3, 5) | 4 (4, 5) | .622 |
| Depression should mostly be treated by psychiatrists.c | 3 (2, 5) | 2 (1, 5) | .057 |
| Primary care is the best setting to screen for depression.c | 4 (2, 5) | 4.5 (3, 5) | .080 |
| I believe that it is important to screen patients for depression in my clinic.c | 4 (3, 5) | 4.5 (3, 5) | .083 |
| I feel comfortable talking with my patients about their mental health.c | 3 (1, 4) | 4 (1, 5) | .044 |
| How easy is the VitalSign6 software program to use with your daily workflow?d | — | 2.5 (1, 5) | — |
| Overall, how easy is the VitalSign6 software program to use?d | — | 3 (2, 5) | — |
| Overall, patients are receptive to depression screening using the VitalSign6 software program.c | — | 2 (1, 4) | — |
| To what extent does your role contribute to patients receiving quality care for depression?e | — | 3.5 (2, 5) | — |
Mann-Whitney U tests were used for paired, Likert-type scale items.
Response scale: 1 = Very Poor to 5 = Very Good.
Response scale: 1 = Strongly Disagree to 5 = Strongly Agree.
Response scale: 1 = Very Difficult to 5 = Very Easy.
Response scale: 1 = Not at All to 5 = Very Much.
Post-Survey Open-Ended Questions
Two open-ended questions were posed to physicians and staff. Of 14 physicians completing the post-survey, 64.3% (n = 9) provided written responses. Of eight staff completing the post survey, 100% provided written responses. The first question asked, “Based on your experience, what are the 3 most difficult/challenging aspects of using VitalSign6?” Results showed 55.6% of physicians found VitalSign6 slowed clinic workflow, 55.6% experienced technical issues with interoperability and lack of bidirectional information flow with the EHR, and 11.1% requested more robust decision support tools. For the staff, 100% found VitalSign6 slowed workflow.
The second question asked, “Based on your experience, what are the three most valuable aspects of using VitalSign6?” Of physicians, 55.6% noted EHR integration to be most valuable, 33.3% commented that VitalSign6 improved screening and increased mental health awareness, and 11.1% found clinical decision support most valuable. Of staff, 87.5% noted the most valuable aspects were increased mental health awareness and improved screening, 50% noted EHR integration, and 12.5% found the VitalSign6 team on-site support most valuable.
Discussion
The ultimate outcome of depression care is patient remission.20,52,60 Studies report a depression remission rate of <6% for patients treated in primary care,52,61 Results of this quality improvement study showed patient remission rates improved from 0% to 23.1% post-intervention. We contribute this finding to the combination of screening, diagnosing, and treating patients using principles of measurement-based care with evidence-based CDS tools interoperable with the EHR. Electronic health records equipped with CDS systems may be an effective mechanism to increase depression screening and remission rates in primary care.20,41,60
Physicians and staff noted on post-surveys that VitalSign6 improved mental health awareness and depression screening in the clinic. The 2-step screening process, first screening with the PHQ-2 and confirming with the PHQ-9, along with real-time integration of VitalSign6 and the EHR was effective. Depression screening rates improved from 85% to over 95%. Over 89% of patients with positive PHQ-9 screens were diagnosed with a depressive disorder. The PHQ-2 and PHQ-9 are preferred screening tools for primary care patients based on their validity, reliability, and brevity.40 An external factor contributing to the clinic’s high screening rate prior to the project was the Delivery System Reform Incentive Payment (DSRIP) program.62 Since the department of family medicine was participating in the DSRIP program, efforts were focused on improving depression screening and documentation in the performance year. Evidence suggests an association between depression screening and participation in federal programs that provide financial incentives.41,55
Study findings support approaching depression care as a triage issue and not as a mental health access issue.20 VitalSign6 technology equipped providers with evidence-based tools and CDS to effectively manage 87.4% of patients they diagnosed with depression using personalized treatment plans and MBC, with referring only 10% to specialty care. Personalized treatment included pharmacological therapy, behavioral treatment such as psychotherapy with behavioral health providers integrated in the clinic, exercise plans, and continued symptomatic monitoring. This approach to treatment complemented the primary care physician’s professional clinical judgment. Our findings are comparable to a study implementing VitalSign6 across 16 primary care clinics across north Texas. Studies show an integrated, collaborative treatment approach to be effective in treating depression in primary care, managing specialty referrals, and improving remission rates.20,60
Pre- and post-survey analysis found many items to have a “ceiling effect” with high pre-implementation values, making it difficult to significantly improve post-implementation. There was a statistically significant difference in physicians’ perceived importance of depression screening and MBC, with lower post-project implementation values. Technology problems slowing workflow likely contributed to this finding. Impact on clinic workflow and technical issues with interoperability were the most reported concerns. The original technology design required the PHQ-2 be completed using the Epic Welcome tablet to enable bidirectional exchange with VitalSign6. Prior to project implementation, the clinic did not use Welcome tablets. Therefore, the clinic was simultaneously learning to integrate Epic Welcome and VitalSign6 into their workflow. Physicians also expressed problems transferring data into their notes, closing notes, re-signing in and logging out. The 2019 Epic upgrade will introduce changes to enhance VitalSign6 interoperability.
Significant improvement was seen in clinic staff’s comfort level talking with patients about their mental health. We believe this was a positive outcome of the 2-hour, in-person training sessions on depression and measurement-based care provided to all clinic staff and the on-site support provided during project implementation.
Limitations
The quality improvement project was conducted in a single clinic site with a residency program, thus limiting generalizability. Also, the project focused on PHQ-2 and PHQ-9 measures and did not analyze other measures available withVitalSign6 for anxiety, treatment side effects, and treatment adherence. Furthermore, there was a high attrition rate—70.2% of patients did not return for follow-up. Further study is needed to identify contributing factors and strategies to improve retention such as care coordination, care navigation, patient engagement, and teletherapy. Evidence shows patient engagement, care coordination and teletherapy interventions reduce logistical and financial barriers and improve follow-up rates.63,64
Conclusion
Implementation science investigates methods, interventions, and variables influencing individual and organizational adoption of evidence-based practices to improve outcomes and care delivery.65-67 Implementation of VitalSign6 provided primary care physicians with evidence-based practice tools allowing depression identification, treatment, and referral management. Additional work is needed to create integrated, multidisciplinary care team models, to streamline workflow, and improve reporting methods and sustainment policies. These results add to a growing body of evidence that VitalSign6 is an effective adjunct in the identification and management of depression in primary care.20,52,55
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kimberly A. Siniscalchi  https://orcid.org/0000-0002-7129-0821
https://orcid.org/0000-0002-7129-0821
References
- 1. National Institute of Mental Health. Major depression among adults. Accessed May 15, 2020 https://www.nimh.nih.gov/health/index.shtml
- 2. Baik SY, Crabtree BF, Gonzales JJ. Primary care clinicians’ recognition and management of depression: a model of depression care in real-world primary care practice. J Gen Intern Med. 2013;28:1430-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76:155-162. [DOI] [PubMed] [Google Scholar]
- 4. HealthyPeople 2020. Mental health and mental disorders. Published October 6, 2019. Accessed January 5, 2020 https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Mental-Health
- 5. Smithson S, Pignone MP. Screening adults for depression in primary care. Med Clin North Am. 2017;101:807-821. [DOI] [PubMed] [Google Scholar]
- 6. Howe-Martin L, Jester B, Walker R, et al. A pilot program for implementing mental health screening, assessment, and navigation in a community-based cancer center. Psychooncology. 2018;27:683-686. [DOI] [PubMed] [Google Scholar]
- 7. Watson LC, Amick HR, Gaynes BN, et al. Practice-based interventions addressing concomitant depression and chronic medical conditions in the primary care setting: a systematic review and meta-analysis. J Prim Care Community Health. 2013;4:294-306. [DOI] [PubMed] [Google Scholar]
- 8. Trivedi MH. The link between depression and physical symptoms. Prim Care Companion J Clin Psychiatry. 2004;6(suppl 1):12-16. [PMC free article] [PubMed] [Google Scholar]
- 9. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10:e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Network of Depression Centers. Get the facts. Published 2018. Accessed May 15, 2020 https://nndc.org/facts/
- 11. Siu AL, US Preventive Services Task Force (USPSTF), Bibbins-Domingo K, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315:380-387. [DOI] [PubMed] [Google Scholar]
- 12. Smith RC, Lyles JS, Gardiner JC, et al. Primary care clinicians treat patients with medically unexplained symptoms: a randomized controlled trial. J Gen Intern Med. 2006;21:671-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mojtabai R, Feder KA, Kealhofer M, et al. State variations in Medicaid enrollment and utilization of substance use services: results from a National Longitudinal Study. J Subst Abuse Treat. 2018;89:75-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bhattacharjee S, Goldstone L, Vadiei N, Lee JK, Burke WJ. Depression screening patterns, predictors, and trends among adults without a depression diagnosis in ambulatory settings in the United States. Psychiatr Serv. 2018;69:1098-1100. [DOI] [PubMed] [Google Scholar]
- 15. Nease DE, Jr, Nutting PA, Graham DG, Dickinson WP, Gallagher KM, Jeffcott-Pera M. Sustainability of depression care improvements: success of a practice change improvement collaborative. J Am Board Fam Med. 2010;23:598-605. [DOI] [PubMed] [Google Scholar]
- 16. Grazier KL, Smiley ML, Bondalapati KS. Overcoming barriers to integrating behavioral health and primary care services. J Prim Care Community Health. 2016;7:242-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grochtdreis T, Brettschneider C, Wegener A, et al. Cost-effectiveness of collaborative care for the treatment of depressive disorders in primary care: a systematic review. PLoS One. 2015;10:e0123078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mulvaney-Day N, Marshall T, Piscopo KD, et al. Screening for behavioral health conditions in primary care settings: a systematic review of the literature. J Gen Intern Med. 2018;33:335-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Symons L, Tylee A, Mann A, et al. Improving access to depression care: descriptive report of a multidisciplinary primary care pilot service. Br J Gen Pract. 2004;54:679-683. [PMC free article] [PubMed] [Google Scholar]
- 20. Trivedi MH, Jha MK, Kahalnik F, et al. VitalSign6: a Primary Care First (PCP-First) model for universal screening and measurement-based care for depression. Pharmaceuticals (Basel). 2019;12:E71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315:388-406. [DOI] [PubMed] [Google Scholar]
- 22. O’Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151:793-803. [DOI] [PubMed] [Google Scholar]
- 23. O’Connor E, Rossom RC, Henninger M, et al. US Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. In: Screening for Depression in Adults: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force. Agency for Healthcare Research and Quality; 2016. [PubMed] [Google Scholar]
- 24. American Academy of Family Physicians. Clinical preventive services recommendation. Depression. Accessed September 9, 2019 https://www.aafp.org/patient-care/clinical-recommendations/all/depression.html
- 25. American Academy of Family Physicians. Summary of recommendations for clinical preventive services. Published 2016. Accessed May 15, 2020 https://www.aafp.org/dam/AAFP/documents/patient_care/clinical_recommendations/cps-recommendations.pdf
- 26. Centers for Medicare and Medicaid Services. MEDICARE Shared Savings Program quality measure benchmarks for the 2019 performance year. Published December 2018. Accessed September 8, 2019 https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2019-quality-benchmarks-guidance.pdf
- 27. Centers for Medicare and Medicaid Services. Next generation ACO Model. Accessed May 15, 2020 https://innovation.cms.gov/innovation-models/next-generation-aco-model
- 28. Gaynes BN, Rush AJ, Trivedi MH, Wisniewski SR, Spencer D, Fava M. The STAR*D study: treating depression in the real world. Cleve Clin J Med. 2008;75:57-66. [DOI] [PubMed] [Google Scholar]
- 29. Gaynes BN, Warden D, Trivedi MH, Wisniewski SR, Fava M, Rush AJ. What did STAR* D teach us? Results from a large-scale, practical, clinical trial for patients with depression. Psychiatr Serv. 2009;60:1439-1445. [DOI] [PubMed] [Google Scholar]
- 30. Huynh NN, McIntyre RS. What are the implications of the STAR*D Trial for primary care? A review and synthesis. Prim Care Companion J Clin Psychiatry. 2008;10:91-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nimalasuriya K, Compton MT, Guillory VJ; Prevention Practice Committee of the American College of Preventive Medicine. Screening adults for depression in primary care: a position statement of the American College of Preventive Medicine. J Fam Pract. 2009;58:535-538. [PubMed] [Google Scholar]
- 32. Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905-1917. [DOI] [PubMed] [Google Scholar]
- 33. Trivedi MH, Rush AJ, Gaynes BN, et al. Maximizing the adequacy of medication treatment in controlled trials and clinical practice: STAR(*)D measurement-based care. Neuropsychopharmacology. 2007;32:2479-2489. [DOI] [PubMed] [Google Scholar]
- 34. ClinicalTrials.gov. Sequenced treatment alternatives to relieve depression (STAR*D). Published July 23, 2001. Accessed May 15, 2020 https://clinicaltrials.gov/ct2/show/study/NCT00021528
- 35. Sinyor M, Schaffer A, Levitt A. The sequenced treatment alternatives to relieve depression (STAR*D) trial: a review. Can J Psychiatry. 2010;55:126-135. [DOI] [PubMed] [Google Scholar]
- 36. Gaynes BN, Rush AJ, Trivedi MH, et al. Primary versus specialty care outcomes for depressed outpatients managed with measurement-based care: results from STAR*D. J Gen Intern Med. 2008;23:551-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Trivedi MH. Tools and strategies for ongoing assessment of depression: a measurement-based approach to remission. J Clin Psychiatry. 2009;70(suppl 6):26-31. [DOI] [PubMed] [Google Scholar]
- 38. Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the United States. JAMA Intern Med. 2016;176:1482-1491. [DOI] [PubMed] [Google Scholar]
- 39. Kato E, Borsky AE, Zuvekas SH, Soni A, Ngo-Metzger Q. Missed opportunities for depression screening and treatment in the United States. J Am Board Fam Med. 2018;31:389-397. [DOI] [PubMed] [Google Scholar]
- 40. Ferenchick EK, Ramanuj P, Pincus HA. Depression in primary care: part 1—screening and diagnosis. BMJ. 2019;365:I794. [DOI] [PubMed] [Google Scholar]
- 41. Akincigil A, Matthews EB. National rates and patterns of depression screening in primary care: results from 2012 and 2013. Psychiatr Serv. 2017;68:660-666. [DOI] [PubMed] [Google Scholar]
- 42. Doraiswamy PM, Bernstein IH, Rush AJ, et al. Diagnostic utility of the Quick Inventory of Depressive Symptomatology (QIDS-C16 and QIDS-SR16) in the elderly. Acta Psychiatr Scand. 2010;122:226-234. [DOI] [PubMed] [Google Scholar]
- 43. Katzelnick D, Duffy FF, Chung H, Regier DA, Rae DS, Trivedi MH. Depression outcomes in psychiatric clinical practice: using a self-rated measure of depression severity. Psychiatr Serv. 2011;62:929-935. [DOI] [PubMed] [Google Scholar]
- 44. Kurian BT, Grannemann B, Trivedi MH. Feasible evidence-based strategies to manage depression in primary care. Curr Psychiatry Rep. 2012;14:370-375. [DOI] [PubMed] [Google Scholar]
- 45. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284-1292. [DOI] [PubMed] [Google Scholar]
- 46. Fuchs CH, Haradhvala N, Hubley S, et al. Physician actions following a positive PHQ-2: Implications for the implementation of depression screening in family medicine practice. Fam Syst Health. 2015;33:18-27. [DOI] [PubMed] [Google Scholar]
- 47. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kroenke K, Spitzer RL, Williams JB, Lowe B. The patient health questionnaire somatic, anxiety and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345-359. [DOI] [PubMed] [Google Scholar]
- 49. Waitzfelder B, Stewart C, Coleman KJ, et al. Treatment initiation for new episodes of depression in primary care settings. J Gen Intern Med. 2018;33:1283-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lewis CC, Scott K, Marti CN, et al. Implementing measurement-based care (iMBC) for depression in community mental health: a dynamic cluster randomized trial study protocol. Implement Sci. 2015;10:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sanchez K, Eghaneyan BH, Trivedi MH. Depression screening and education: options to reduce barriers to treatment (DESEO): protocol for an educational intervention study. BMC Health Serv Res. 2016;16:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jha MK, Grannemann BD, Trombello JM, et al. A structured approach to detecting and treating depression in primary care: VitalSign6 Project. Ann Fam Med. 2019;17:326-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Guo T, Xiang YT, Xiao L, et al. Measurement-based care versus standard care for major depression: a randomized controlled trial with blind raters. Am J Psychiatry. 2015;172:1004-1013. [DOI] [PubMed] [Google Scholar]
- 54. Zimmermann T, Puschmann E, van den Bussche H, et al. Collaborative nurse-led selfmanagement support for primary care patients with anxiety, depressive or somatic symptoms: cluster-randomised controlled trial (findings of the SMADS study). Int J Nurs Stud. 2016;63:101-111. [DOI] [PubMed] [Google Scholar]
- 55. Kahalnik F, Sanchez K, Faria A, et al. Improving the identification and treatment of depression in low-income primary care clinics: a qualitative study of providers in the VitalSign6 program. Int J Qual Health Care. 2018;31:57-63. [DOI] [PubMed] [Google Scholar]
- 56. Sanchez K, Eghaneyan BH, Killian MO, Cabassa L, Trivedi MH. Measurement, Education and Tracking in Integrated Care (METRIC): use of a culturally adapted education tool versus standard education to increase engagement in depression treatment among Hispanic patients: study protocol for a randomized control trial. Trials. 2017;18:363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Trombello JM, South C, Cecil A, et al. Efficacy of a behavioral activation teletherapy intervention to treat depression and anxiety in Primary Care VitalSign6 Program. Prim Care Companion CNS Disord. 2017;19:17m02146. [DOI] [PubMed] [Google Scholar]
- 58. Greenhalgh T, Stramer K, Bratan T, Byrne E, Mohammad Y, Russell J. Introduction of shared electronic records: multi-site case study using diffusion of innovation theory. BMJ. 2008;337:a1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Centers for Disease Control and Prevention. Develop SMART objectives. Accessed August 31, 2019 https://www.cdc.gov/phcommunities/resourcekit/evaluate/smart_objectives.html
- 60. Ramanuj P, Ferenchick EK, Pincus HA. Depression in primary care: part 2—management. BMJ. 2019;365:l835. [DOI] [PubMed] [Google Scholar]
- 61. Pence BW, O’Donnell JK, Gaynes BN. The depression treatment cascade in primary care: a public health perspective. Curr Psychiatry Rep. 2012;14:328-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Texas Health and Human Services. Waiver renewal: Health Information Technology (Health IT) Strategic Plan. Accessed June 22, 2019 https://hhs.texas.gov/laws-regulations/policies-rules/waivers/medicaid-1115-waiver/waiver-renewal
- 63. Schaeffer AM, Jolles D. Not missing the opportunity: improving depression screening and follow-up in a multicultural community. Jt Comm J Qual Patient Saf. 2019;45:31-39. [DOI] [PubMed] [Google Scholar]
- 64. Trombello JM, South C, Sánchez A, Kahalnik F, Kennard BD, Trivedi MH. Two trajectories of depressive symptom reduction throughout Behavioral Activation teletherapy among underserved, ethnically-diverse, primary care patients: a VitalSign6 Report [published online January 11, 2020]. Behav Ther. doi: 10.1016/j.beth.2020.01.002 [DOI] [PubMed] [Google Scholar]
- 65. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Titler MG, Everett LQ, Adams S. Implications for implementation science. Nurs Res. 2007;56(4 suppl):S53-S59. [DOI] [PubMed] [Google Scholar]
- 67. Agency for Healthcare Research and Quality. Improving primary care practice. Accessed May 15, 2020 https://www.ahrq.gov/professionals/prevention-chronic-care/improve/index.html [DOI] [PubMed]