When COVID‐19 struck Washington state in January 2020, most U.S. hospitals were unprepared. In March, the pandemic arrived in the New York metropolitan area, overwhelming hospitals 1 and causing significant mortality, 2 , 3 particularly in older adults. This experience continues in U.S. hospitals despite accumulating experience, research, and governmental support. 4 Emergency operations plans, 5 , 6 required for hospitals, may be insufficient for COVID‐19. Challenges and successful interventions must be shared to improve outcomes. This editorial describes how one system, Hackensack Meridian Health (HMH), in New Jersey, one of the early and hardest hit states, developed a comprehensive plan, the COVID 2.0 Playbook, 7 for the future.
COVID‐19 is devastating for older adults. Their hospitalization risk is eight‐fold higher at the age of 75 to 84 years compared with 18 to 29 years, 13‐fold higher for age 85 years and older, with a horrifying 220‐fold higher mortality rate for ages 75 to 84 years, and 630‐fold for age 85 years and older. 8 COVID‐19 amplifies hazards of hospitalization for older adults: 9 functional decline, delirium, polypharmacy, sleep disturbance, falls, weight loss, pressure injury, and infection. Some evidence‐based interventions, such as Acute Care for Elders units, 10 comprehensive geriatric consultation, 11 the Hospital Elder Life Program, 12 and Institute for Healthcare Improvementʼs Age‐Friendly Health System recommendations, 13 were suspended during the pandemic due to staffing.
On March 2, 2020, the first COVID‐19 patient was admitted to HMHʼs university hospital. 14 HMH mandated universal masking and testing of long‐term care frontline workers before Health Department requirements. Within 6 weeks, confirmed COVID‐19 cases at HMH peaked at 7,069 patients (5,109 hospitalized). HMH has now cared for greater than 13,000 COVID‐19 patients (Figure 1), including many older adults. The human and financial toll has been immense.
Figure 1.
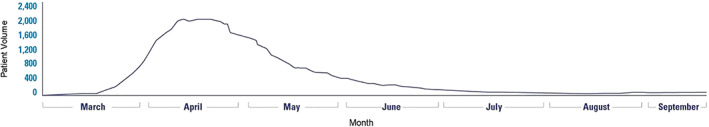
Hackensack Meridian Network Covid‐19 hospitalization volume, March to September 2020.
During this local pandemic nadir, team members from HMHʼs 17 hospitals, 16 post‐acute care facilities, 500+ ambulatory offices, home care, hospice, dialysis, and the Hackensack Meridian School of Medicine contributed challenges and innovations (examples in Table 1). The Playbook outlines future system actions across settings, facility and capacity management, infection control, safety, administration, human resources, clinical management, laboratory, pharmacy, patient experience, research, ethics, and supply chain.
Table 1.
Selected COVID 2.0 Playbook Challenges, Innovations, and Future Preparedness Plans
| Challenges | Innovations | Preparedness plans |
|---|---|---|
| Clinical Disease Management | ||
| Community MDs uncertain about referrals for admission, testing, treatment | MD education via live, internet‐based webinars; Command Center internet information; e‐mail blasts; chairpersonʼs virtual meetings | Develop process for earlier preparation and command center activation based on analysis of admission rates and percentage positivity; earlier communication |
| Clinical treatment uncertainty | HMH Clinical Guidelines interdisciplinary team development; dissemination | Expand rounding in clinical locations |
| HMH School of Medicine students review and summarize new research for clinicians | Develop standing literature search functionality to inform guidelines and practice | |
| Expand clinical guidelines | coaching program for infection prevention best practices | |
| Clinical site inexperience | Partner new and experienced nurses and physicians | Improving online COVID‐19 resource center for team members |
| Delays in discharge due to family and post‐acute care infection concerns | Discharge NP to assist complex family, post‐acute care issues | Simplify processes |
| Patients with hypoxia | Proning Service; clinical guidance on management | |
| Unusual pressure injury from proning | Additional clinical guidance on proning, pressure injury prevention | Conduct prediction models for local second COVID‐19 and influenza surge |
| Complexity of admissions for redeployed physicians | Hospitalist admission workup for all COVID‐19 patients; then assignment to ward teams | |
| Complex medical decision‐making and methods of family communication | iPad use, family communication teams, increased patient visibility | |
| Infection prevention | Multidisciplinary workgroup review and response for team members, patients, family | Update protocols |
| Delirium | Increase patient visibility, case review, geriatrics consultation | Add training and guideline section for delirium protocols |
| Ethics | ||
| Concern about allocation of resources | Rapidly developed HMH policy and infrastructure to adapt and implement state policy for Allocation of Critical Care Resources During a Public Health Emergency | Strengthen ethics education and training regarding clinical decision‐making |
| Partnered with Learning and Development to extend bioethics education to ensure fair allocation of resources | ||
| Ensure that relevant policies are collaboratively developed provide COVID‐19–relevant bioethics | ||
| Issues regarding advance directives | Temporary addendum Do Not Attempt Resuscitation policy to meet the unique demands of the pandemic. | |
| Adapt procedures for Do Not Attempt Resuscitation orders to meet the challenges of the pandemic | ||
| Staff and physician anxiety, illness | Departmental support, institutional webinars, website information | Partner with Wellness to expand opportunities for moral distress debriefs for frontline providers |
| Research ethics: projects and enrollment | Bioethics participation in research committee to support, guide, and collaborate in COVID‐19–related research protocol development | Incorporate learning in larger research ethics framework |
| Personal Protective Equipment | ||
| Variability in PPE use | Infection prevention team assessment of PPE effectiveness | Standing guidance, reassessments with types of infections (influenza, COVID‐19) |
| Clinical Disease Management standardize protocols across settings, institutions, incorporate CDC guidance | Stockpile critical PPE and supplies; enhance PPE education, oversight, and enforcement processes | |
| Staff/MD education by webinars, video, in‐person PPE training hourly | Standardizing local oversight of PPE distribution, management, and procurement | |
| Network procurement, monitoring, distribution | Create a new Value Analysis Rapid Response Team to evaluate new sources of PPE | |
Abbreviations: HMH, Hackensack Meridian Health; MD, doctor of medicine; NP, nurse practitioner; PPE, personal protective equipment.
HMHʼs Clinical Disease Management team led patient care, disease transmission prevention, and analytics, monitoring emerging literature, troubleshooting problems, and sharing best practices and policies in real time. Infection prevention collaborated with purchasing and materials management to acquire, distribute, and maintain personal protective equipment (PPE) supplies. Extensive COVID‐19 clinical guidelines were developed and disseminated, with continuing updates. Local experience included a March recommendation for steroid treatment for patients with COVID‐19 inflammatory respiratory failure, long before published data. Guidelines included advance directive, state law changes, and treatment and imaging recommendations, among others.
Hospital surge staffing is challenging. At the university hospital, more than 100 physicians were redeployed from ambulatory practice to assist during the surge. The Department of Medicine provided just‐in‐time clinical training, including hypoxia management, off‐label medication use, clinical trial eligibility, an electronic medical record refresher, and training for PPE use. Experienced physicians and nurses partnered with redeployed staff to support practice. Increased rounding, case discussions, and coaching to disseminate best practices are planned.
Despite a Hospital Elder Life Program, delirium presented with COVID‐19, compounded by isolation. iPads were provided for communication. The 74‐bed temporary COVID‐19 unit was built with transparent walls, enabling rapid responses to alterations in status and providing a reassuring presence of nurses and physicians. Windows in hospital room doors were enlarged to achieve the same capability.
Serious illness conversations about goals of care, clinical trial risks and benefits, and advance directives were held with families by video call. With geriatrics and palliative care service support, cliniciansʼ ability to hold these discussions improved rapidly. In intensive care units, a “Family Communication Team” of redeployed physicians provided telesupport for families. The physicians were grateful to participate “when it really counts.”
HMHʼs research program contributed the first‐approved COVID‐19 test, reducing result wait times from days to hours. An HMH COVID Recovery Center started to address persistent symptoms and support research. The Hackensack Meridian COVID‐19 2.0 Playbook is a leading example of rapid reflection and analysis needed by hospitals during COVID‐19, which will improve care now and for a postpandemic future.
ACKNOWLEDGMENTS
There is no extramural sponsor for this editorial. The manuscript was prepared by the first author, Dr Jacobs, based on the COVID 2.0 Reboot white paper written by the Hackensack Meridian team under the direction of the second author. The second author edited and commented on the content in the manuscript.
Conflict of Interest
The first author is an employee, and the second, the Chief Executive Officer, of Hackensack Meridian Health, discussed in the editorial.
Author Contributions
The first author developed the initial draft manuscript with content and ideas from the second author, who edited the manuscript.
Sponsor's Role
There is no sponsor for this work.
REFERENCES
- 1.Hosted by Michael Barbaro, produced by Neena Pathak, Austin Mitchell, and Andy Mills, and edited by Lisa Chow and Lisa Tobin. The Mistakes New York Made. The Daily (podcast). The New York Times July 27, 2020. https://www.nytimes.com/2020/07/27/podcasts/the-daily/new-york-hospitals-covid.html. Accessed September 12, 2020.
- 2.New York City Covid Map and Case Count. https://www.nytimes.com/interactive/2020/nyregion/new-york-city-coronavirus-cases.html. Accessed September 13, 2020.
- 3. Chilimuri S, Sun H, Alemam A, et al. Predictors of mortality in adults admitted with COVID‐19: retrospective cohort study from New York City. West J Emerg Med. 2020;21(4):779‐784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nuzzo JB, Bell JA, Cameron EE. Suboptimal US response to COVID‐19 despite robust capabilities and resources. JAMA. 2020. 10.1001/jama.2020.17395. Epub ahead of print. PMID: 32936215. [DOI] [PubMed] [Google Scholar]
- 5.Emergency Preparedness Rule. Center for Medicare and Medicaid Services. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertEmergPrep/Emergency-Prep-Rule. Accessed September 12, 2020.
- 6.Emergency Preparedness Rule. Appendix Z. Center for Medicare and Medicaid Services. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/som107ap_z_emergprep.pdf. Accessed September 12, 2020.
- 7. Weinstock M. "Q&A; 'How could we make Hackensack Meridian more efficient?'." Modern Healthcare, vol. 50, no. 32, 31 Aug. 2020, p. 0026. Gale OneFile: Health and Medicine, Accessed September 12, 2020.
- 8.COVID‐19 hospitalization and death by age. Centers for Disease Control (CDC). https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-age.html. Accessed September 12, 2020.
- 9. Creditor M. The hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219‐223. [DOI] [PubMed] [Google Scholar]
- 10. Flood KL, Booth K, Vickers J, et al. Acute care for elders (ACE) team model of care: a clinical overview. Geriatrics (Basel). 2018;3(3):50 10.3390/geriatrics3030050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ellis G, Gardner M, Tsiachristas A, et al. Comprehensive geriatric assessment for older adults admitted to the hospital. Cochrane Database Syst Rev. 2017;9:CD006211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669‐676. [DOI] [PubMed] [Google Scholar]
- 13.What is an age‐friendly health system? Institute for Healthcare Improvement. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx. Accessed September 12, 2020.
- 14. Dominus S. How New Jerseyʼs first coronavirus patient survived. New York Times April 5, 2020. https://www.nytimes.com/2020/04/05/magazine/first-coronavirus-patient-new-jersey.html. Accessed September 12, 2020.


