Abstract
The 2019 coronavirus (COVID‐19), also known as SARS‐CoV‐2, is highly pathogenic and virulent, and it spreads very quickly through human‐to‐human contact. In response to the growing number of cases, governments across the spectrum of affected countries have adopted different strategies in implementing control measures, in a hope to reduce the number of new cases. However, 5 months after the first confirmed case, countries like the United States of America (US) seems to be heading towards a trajectory that indicates a health care crisis. This is in stark contrast to the downward trajectory in Europe, China, and elsewhere in Asia, where the number of new cases has seen a decline ahead of an anticipated second wave. A data‐driven approach reveals three key strategies in tackling COVID‐19. Our work here has definitively evaluated these strategies and serves as a warning to the US, and more importantly, a guide for tackling future pandemics. Also see the video abstract here https://youtu.be/gPkCi2_7tWo
Keywords: COVID‐19, data‐driven, data science, policy decisions, SARS‐CoV‐2, strategy
Don't take socioeconomic risks with this one! A data‐driven approach serves as a warning to the US and a guide for dealing with new pandemics. Three key strategies in tackling COVID‐19 emerge from this comparative analysis of new case numbers between China, the European nations, and the US, and a timeline of the measures taken in response to the outbreaks.
INTRODUCTION TO A GLOBAL PANDEMIC
A pandemic is a global outbreak of a new virus that is very different from current and previously circulating human viruses. As viruses are constantly mutating, on rare occasions, it is possible for non‐human viruses to change in such a way that can infect humans easily. This may be exacerbated by the ease of spread when it becomes contagious through person to person contact. Beginning in December 2019, in the region of Wuhan, the People's Republic of China, a novel coronavirus appeared and began to spread in human beings.[ 1 ] The coronavirus disease of 2019 (COVID‐19) is a new virus that spreads quickly between people. Although it was initially perceived as an epidemic in China, the virus soon spread worldwide within months. The World Health Organisation (WHO) declared COVID‐19 a pandemic in March, 2020, and by the end of that month, the world saw more than a 7.5 million people infected and nearly 35,000 deaths,[ 1 ] according to WHO Situation Report 71. As of the end of June, 2020, the virus has spread beyond 10 million individuals, with half a million deaths reported worldwide 6 months since the first reported case in Wuhan.
Coronaviruses are a group of related RNA viruses that cause diseases in groups of mammals and birds. When humans are infected by these viruses, these viruses cause respiratory tract infections that can range from mild respiratory deficiencies to severe effects, leading to death. Unlike COVID‐19, the outbreak of severe acute respiratory syndrome (SARS) in 2002–2003 in Asia never reached the level of a pandemic.[ 2 ] This coronavirus is not as contagious as the one responsible for COVID‐19. The spread of SARS was mainly restricted to hospitals and other settings where people came in close contact with body fluids of the infected patients.[ 3 ] At the end of the SARS epidemic in June, 2003, the incidence was 8422 cases with a case fatality rate of 11%, and no new cases of SARS had been reported worldwide since 2004.[ 4 ] The other major coronavirus outbreak, since 2000, is the Middle East respiratory syndrome (MERS). The first identified case of MERS occurred in 2012 in Saudi Arabia and most outbreaks have occurred in the Arabian Peninsula.[ 5 ] This virus is not as contagious as COVID‐19, but has proven to be much deadlier than both SARS and COVID‐19. About 2500 cases have been reported as of January, 2020, with a case fatality rate of about 35%.
A key feature that sets the 2019 coronavirus apart from previous epidemics is the far‐reaching extent of the virus, having spread to 216 countries and territories after just 6 months of it being first detected and classified.[ 6 ] As an indication of the potential widespread of the virus, epidemiologist will estimate the basic reproductive number, . This gives an indication of the spread of a disease. If the , infections will continue to spread. If , the infection will eventually diminish. The of COVID‐19 based on early studies from initial data from China is estimated at 1.4–6.5, with an average of 3.3, median of 2.8 and interquartile range of 1.2, with other studies indicating the same range of values.[ 7 , 8 ] More recent research using data from the outbreak in Italy puts the numbers in the range of 2.4–3.1.[ 9 ] This range of values is due to various factors, among which, transparency, decisive leadership, effective communication, solidarity and accountability are some of the key factors that influence . Most countries would not be returning to the open and connected global economy they had before anytime soon. While it is also too early to say that the worst is over, we can certainly identify some key lessons that can inform our responses to future crises.[ 10 , 11 ] In this paper, we attempt to study and compare the spread of COVID‐19 in the United States (US) of America (comprising the 50 States, including the District of Columbia (D.C.)) and the group of European nations (comprising the members of the European Union, the countries in the Schengen area and United Kingdom), with comparisons to the situation in Mainland China, Japan, and South Korea. We first introduce some key concepts that will aid in our analysis. Our methodology pertaining to the data collection and its analysis are then discussed. Finally, we provide caution and give our conclusion in the last section.
WHAT IS THE GLOBAL RESPONSE?
Timeline and response
As with on‐going epidemics and pandemics, the situation is evolving with new discoveries each day. For the purpose of this paper, we discuss the COVID‐19 pandemic from the period of December 31, 2019 (when the the alert was first announced by the WHO) to June 30 2020, 6 months after.
Retrospective studies consider the emergence of the SARS‐CoV‐2 strain to have evolved in November 2019.[ 12 ] Apprehension of a pending epidemic started at the Hubei Provincial Hospital of Integrated Chinese and Western Medicine in Wuhan, in the days between December 27 and 29 2019. On December 31, 2019, the Wuhan Health authorities issued a case statistic of 27 infected individuals. On the same day, the WHO also received the information.[ 13 ] There was swift action by the scientific community in China that resulted in the publication of the genomic sequence of the virus on January 11. Since January 20, there have been reports confirming human‐to‐human transmission after initial suspicion of transmission to medical workers. In this section, we first summarize the responses given by the different governments at key junctures of their pandemic milestones.
COVID‐19 in the US
The US Centre for Disease Control received its first reported case on January 22 and confirmed its first local transmission case in the same month.[ 14 ] In response to the early outbreaks in Hubei province in China, the US President suspended entry of foreigners who have been physically in mainland China during the preceding 14‐day period, effective February 2. Following which, the 26 European countries that comprise the Schengen Area adopted the same travel restrictions, effective March 13 and were joined by the United Kingdom and Ireland on March 16. The early closure of the border to China meant that many of the first cases detected in the US are arrivals from Europe.[ 15 ] European travel preceded the index cases in at least 13 states and territories, compared to only six from China, with Italy accounting for at least 10 of the first COVID‐19 cases.
By the end of March, cases were recorded in all 50 US states and D.C., with early outbreaks concentrated at key major cities. In the same month, New York alone accounted for the highest number of cases. The state saw 56% of all confirmed US cases on March 25.[ 16 ] With stricter measures of stay‐at‐home orders and curfew in place, some states have managed to significantly decrease the spread of the coronavirus within their state borders. This was subsequently followed by most states in the following week, however these orders were imposed with a diverse scope and severity. Figure 1 shows the efforts by each state of the union, and D.C., in its efforts to limit the spread of the virus.
FIGURE 1.
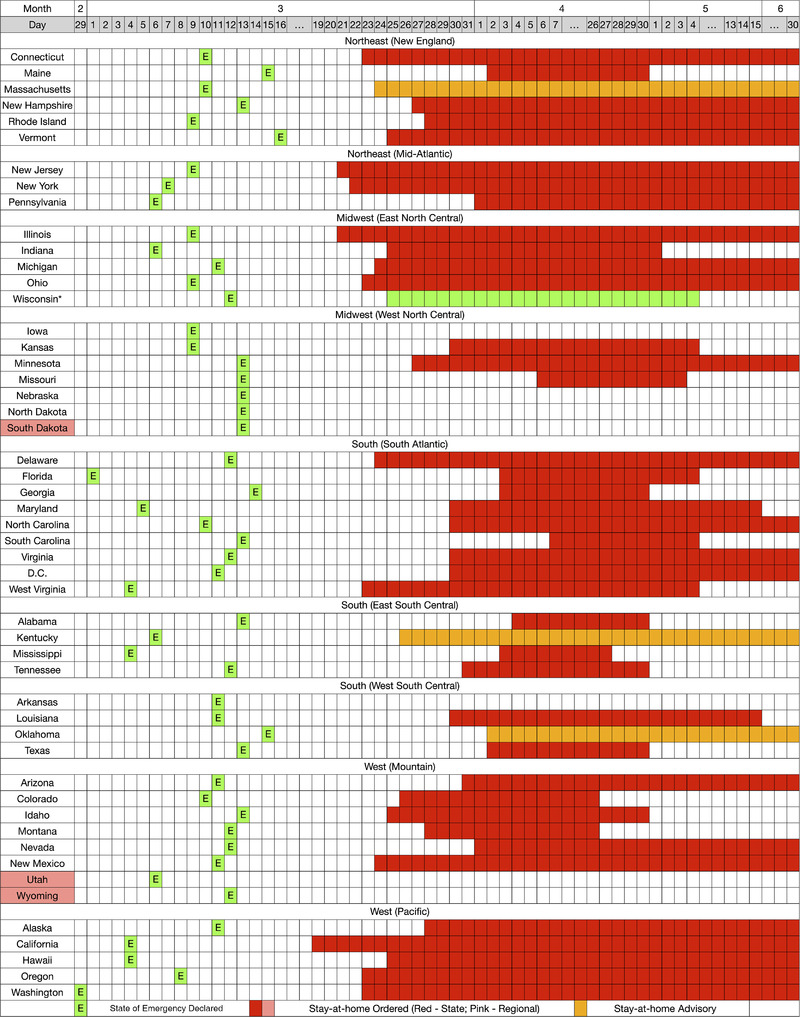
The efforts by the States of the US and D.C., grouped according to regions. *Wisconsin's State court declared the “stay‐at‐home” order unconstitutional.
A second peak1 of infections began in June 2020, primarily driven by relaxed restrictions in several states, mainly among the Southern states, including Arizona, South Carolina, Florida, Texas, and Arkansas, among others.
COVID‐19 in Europe
Under the European Union subsidiarity principle, the EU does not have the legal powers to impose health management policy or actions, such as quarantine measures or closing schools, on member states. However, the EU and its member states have been taking resolute and coordinated action to mitigate the socio‐economic impact due to the COVID‐19 outbreak. The EU is coordinating efforts and mobilising resources available to help member states in their national responses. The EU has laid out key principles in its fight against the spread of the virus[ 17 , 18 ]:
limiting the spread of the virus
ensuring the provision of medical equipment
boosting research for treatments and vaccines
supporting jobs, businesses and the economy
helping citizens stranded in third countries.
On March 16, the EU Commission recommended member states to urge their citizens to remain within the EU to avoid spreading the virus to other countries. Each country is responsible for their external borders and many have limited entry for non‐EU citizens. In the initial stages, the EU was reluctant to close internal borders as a form of EU solidarity. However, as the spread of the virus became more serious, the EU, in consolidation of efforts, has also allowed countries to—for a limited period—introduce border checks at their internal borders if there is a serious threat to public policy or internal security.[ 19 ] France and Germany planned to reopen their internal borders on June 15 and their external border on July 1 to selected non‐Schengen countries.[ 20 , 21 ] Figure 2 shows the efforts by the major countries of the EU and the United Kingdom (UK) in its efforts to arrest the spread of the virus.
FIGURE 2.
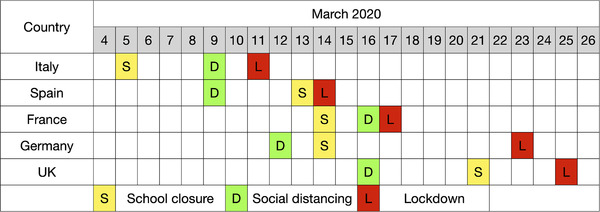
The efforts by Italy, Spain, France, Germany, and the UK in limiting the spread of the virus through internal control strategies such as closure of schools, social distancing, and lockdown
COVID‐19 in East Asia
In China, Wuhan authorities shut down the city's Huanan Seafood Wholesale Market, in response to the reporting of 27 cases, widely believed to be the first cluster of COVID‐19. Following the closure of the seafood market, the following actions were then taken by Hubei Province in response to the outbreak[ 22 , 23 ]:
January 23: transport in Wuhan, Huanggang, and Ezhou was severely restricted, including closure of public transit, trains, airports, and major highways into and out of these regions. Residents were also restricted from leaving. Further travel restrictions were enacted in 12 additional prefecture‐level cities in the province of Hubei.
February 13: the Chinese government issued extension of order to shut down all non‐essential companies, including manufacturing plants, in Hubei province until at least February 20. This was extended a week later to last until at least March 10.
March 13: With the situation improving in areas outside of the epicenter, Wuhan, local governments relax some controls and permits on road traffic.
March 14: Hubei Sanitation and Health Committee announces that only Wuhan remains a high‐risk area, with the rest of the Hubei province considered medium‐ or low‐risk areas. Any low‐risk township‐level divisions, in addition to those medium‐ and high‐risk divisions with no confirmed active cases, could lift their blockades and other mobility controls. This kick started a series of easing of controls over the rest of the province.
March 22: Wuhan loosens its 2‐month lockdown.
March 25: Hubei lifts the lockdown outside of Wuhan, although people will still need to confirm their “Green Code” health classification, designated by Alipay's monitoring system, to travel.
April 8: Wuhan lifts its lockdown, resumes all transportation, with residents intending to leave the city to adhere to similar “Green Code” requirement as those in the rest of the province.
Outside the Hubei province, there were various degrees of control imposed at Prefecture, District and County level. This system of ”closed management” was implemented on a community‐basis, where local communities championed their own COVID‐19 management by adopting guidelines provided by the authorities. China's aggressive strategy has seen a sharp decrease in new cases. Despite the aggressive strategy, as the country opens up, there have been threats of a second wave, most notably in the capital city, Beijing.[ 24 ] In some cases, control measures had to be implemented again at the local level because of localised outbreaks, two examples include Suifenhe county in Heilongjiang province, a county bordering Russia[ 25 ] and Anxin county in Hebei, near Beijing after a small surge in cases.[ 26 ]
In Japan, the initial response was to adopt the strategy of containment. Japan focused on preventing the infected cases from entering and treating those that are within its borders. Japan adopted a policy of containment that focused on the repatriation of Japanese citizens from Wuhan, and the introduction of new border control regulations. Some of the border controls included enacting restrictions to deny entry, on February 1, to foreign citizens who had visited Hubei province within 14 days and to those with a Chinese passport issued from Hubei province.[ 27 ] This was later extended to Zhejiang Province. This on top of having to handle an outbreak onboard the Diamond Princess under quarantine in Yokohama.[ 28 ] Japan adopted a revised strategy in late February when local cases started to increase exponentially. A state of emergency was declared and the following took place[ 29 ]:
April 7: Prime Minister Shinzo Abe declared a 1‐month state of emergency for Tokyo and the prefectures of Kanagawa, Saitama, Chiba, Osaka, Hyogo, and Fukuoka. 9 days later, the declaration was extended to the rest of the country for an indefinite period.
May 14: Japan relieves the nationwide state of emergency COVID‐19 in 39 of Japan's 47 prefectures, but it is still in place for major cities including Tokyo, Osaka, Kyoto, Hyogo, Hokkaido, Chiba, Kanagawa, and Saitama.
May 25: Japan ended the state of emergency in all of Japan.
Japan has seen increasing cases in Tokyo from late May into June, but fears of it being a second wave has been dismissed by Governor Yuriko Koike.[ 30 , 31 ] Japan managed to bring down the number of new reported cases during the period of the state‐of‐emergency without implementing the stringent lockdown as seen in Wuhan and Northern Italy.[ 32 ]
The response in South Korea has been the center of praise from the international community. South Korea introduced what was considered as one of the largest and best‐organized epidemic control programs in the world. South Korea is the only country outside of the Arabian peninsula that recorded an outbreak of MERS within their borders, which may have prepared the country for another of such outbreak.[ 33 ] The country reported its first COVID‐19 case on January 20. The government takes the view that dealing with the COVID‐19 outbreak requires focusing efforts on early testing and global cooperation instead of implementing a lockdown. Different measures have been taken to screen the mass population for the virus, and isolate any infected people as well as trace and quarantine those who contacted them, without further lockdown.[ 34 ] Community locations that may lead to extended social interactions were also shuttered, and only reopened when South Korea saw sequential days of recording single digit of new cases in late April. Aggressive testing and a data‐driven approach to performing contact tracing for isolation and quarantine created the environment needed for social distancing, which significantly reduced the number of new cases in South Korea.[ 35 ] By the end of June, South Korea recorded 12,800 cases, with a case fatality rate of about 2.19%, which is significantly lower than the WHO's reported global case fatality rate of slightly under 5%.[ 36 ] The rapid and extensive tests taken by South Korea have been judged successful in limiting the spread of the outbreak, without using the drastic measure of quarantining entire cities. South Korea began easing social distancing rules on May 6.[ 37 ] However, despite a sustained period of low reported cases, a new cluster emerged in Seoul in mid May. Persistent local counts of infections in the greater Seoul area continued, which the government hinted as a second wave of infections.[ 38 ]
Testing for COVID‐19
Testing gives an indication of the infection status as lab‐confirmed infection are counted as confirmed cases. This means that the number of confirmed cases is a function of how much testing is being carried out. With the possibility of asymptomatic transmission, it becomes increasingly important in carrying out testing.[ 39 , 40 , 41 , 42 ]
Testing also provides a window into the pandemic and how it is spreading. Without such data, we have no way of understanding the dynamics of the spreading and severity of the pandemic. Without which, it will lead to under‐reporting of infected cases and death counts. To interpret any data on confirmed cases and evaluating policies in relation to the curbing of the virus, it becomes crucial to know how much testing for COVID‐19 is being carried out by individual country. The lack of access or reporting of such data will prevent anyone from having a full understanding of the spread of COVID‐19.
There are two kinds of tests available for COVID‐19, namely, the viral tests and antibody tests. A viral test indicates current infection. Any individual who is currently infected with COVID‐19 will be tested as positive on a viral test. An antibody test is a retrospective test. It indicates a past infection. An antibody test may not show if an individual has a current infection because it can take 1 to 3 weeks after infection for the body to produce antibodies.[ 43 , 44 ]
Immunity to COVID‐19
Based on current knowledge, it is not known if having antibodies to the virus that causes COVID‐19 may provide protection from getting infected with the virus again. Furthermore, if it does, one does not know how much protection the antibodies may provide, or for how long this protection may last.[ 45 , 46 , 47 , 48 ]
A DATA‐DRIVEN APPROACH TO ANALYZE EFFECTIVENESS OF STRATEGIES
We used two data sets in this paper. The first data set contains raw data on confirmed cases, by country, extracted from Our World in Data.[ 49 ] The information used in this data set is sourced from the European Centre for Disease Prevention and Control (ECDC). The first data set was extracted on July 1, 2020, 0000 hours Universal Coordinated Time. The second data set contains raw data of confirmed cases (according to the states of the US), extracted from Centre of Disease Control and Prevention (CDC).
It is worth noting that case numbers are highly dependent on truthful reporting and efficient testing. The CDC acknowledges that COVID‐19 can cause mild illness where symptoms may not appear immediately, as such, there will be delays in reporting and testing. Furthermore, there are individuals who are infected, but do not get tested or seek medical care, and there may be differences in how jurisdictions confirm numbers. Thus, any conclusions drawn from this analysis is highly dependent on the reporting. It is also possible that the number of cases reported is different between data sets. This largely boils down to the different reporting jurisdiction's health departments. This will not affect our conclusion as our analyses are pertaining to the observed trends and not specific to individual case numbers. The data sets used in this paper are also cross‐referenced to ensure accuracy in recorded information.
Data analysis
In this section, we have compiled the data according to the second higher administrative division of the US and Europe, namely the states and countries, respectively. The graphs generated capture the number of new cases reported each day since the first reported case in the US and Europe, respectively.
With regards to the US, we have seen that the main strategy adopted by the states is the stay‐at‐home order or advisory implemented at varying degrees, at different timelines. Their implementation are largely reactionary, rather than cautionary. Figure 3 shows the number of new COVID‐19 cases per day, by state including D.C., and the total number of new COVID‐19 cases per day reported by the United States Centre of Disease Control and Prevention.
FIGURE 3.
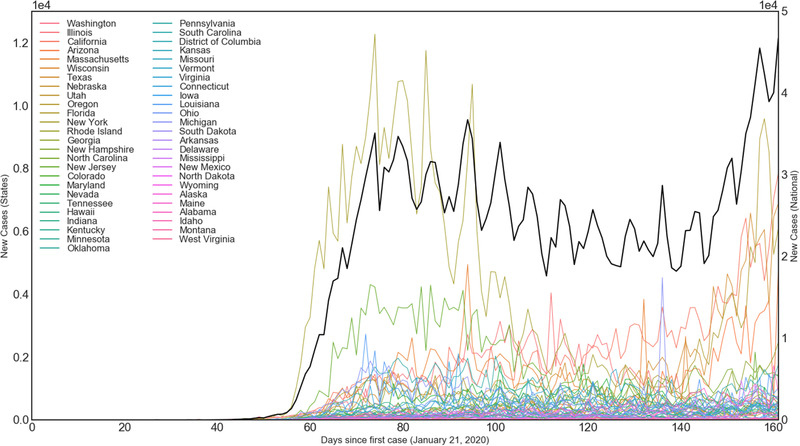
Number of new COVID‐19 cases per day, by state including the District of Columbia, and the total number of new COVID‐19 cases per day reported by the United States Centerfor Disease Control and Prevention
In Figure 4, the graphs show the different trajectories categorised according to the main features of the spread of COVID‐19. The graphs in green show the states of New York and New Jersey, these states were severely hit by the early waves of COVID‐19, but have since brought the spread under control after the early peak. Cases in these states continue to fester, and are often still higher than other states, but this is largely attributed to their high population density. The graphs in orange (Pennsylvania, Illinois and Massachusetts) highlight the states that have an early to mid peak of COVID‐19 cases, and similar to the states highlighted in green, these states have brought the number of new cases under control. The states highlighted in orange have significantly lower number of case counts compared to the states highlighted in green. These five states continue to be under stay‐at‐home orders or advisories. These states continue to see a decrease in new cases each day.
FIGURE 4.
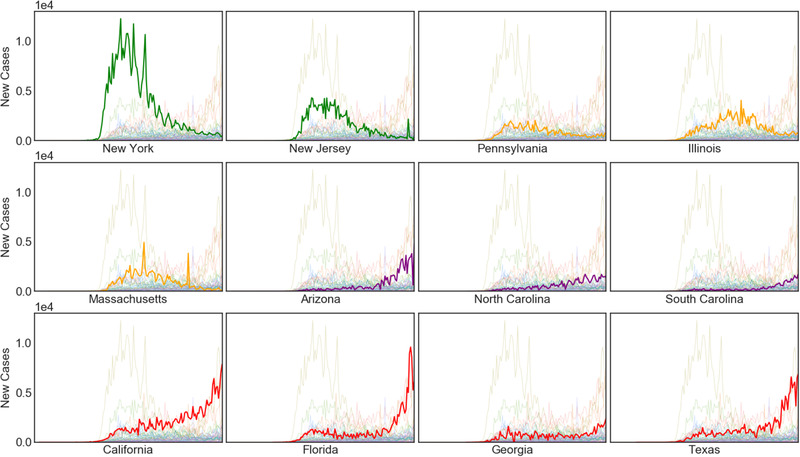
Graph showing the number of cases of COVID‐19 in different states. Different color categories indicate the different stages of the COVID‐19 wave. The horizontal axis is in days since the first recorded case in the US (January 21, 2020)
On the other hand, the graphs in red show states (California, Florida, Georgia and Texas) that have experienced an early first wave, similar to those observed for the states highlighted in orange, but have not fully recovered. These states are experiencing a second wave that is significantly worse than the first wave. The graphs in purple show states (Arizona, North and South Carolina) that have experienced late first waves that coincide with the second wave of the states highlighted in red. Of these seven states, four of them, namely Florida (May 4), Georgia (April 30), South Carolina (May 4) and Texas (April 30) have lifted their stay‐at‐home orders, and are now seeing a surge in infection numbers. After two weeks of lifting the stay‐at‐home orders, these states are now experiencing another peak in the number of newly recorded COVID‐19 cases. We note that this is not unique only to the seven states mentioned in Figure 4, in fact, 20 other states have seen an increase in the number of new cases in the final week of June, compared to the week before. However, with no re‐introduction of stay‐at‐home orders or advisories, estimates indicate that the number of new cases will continue to increase beyond 100,000 new cases a day.[ 50 ]
In comparison to Europe, which has a larger population over a smaller land area than the US, we see that most of the countries in the EU, Schengen Area and the UK were hit by the coronavirus at around the same time, with a lead or lag by about two weeks. This is largely attributed to the fact that these countries, though belonging to the EU, have major airports that connect to the rest of the world. This would likely bring the virus into its borders at around the same time. Figure 5 shows the number of cases, by country.
FIGURE 5.
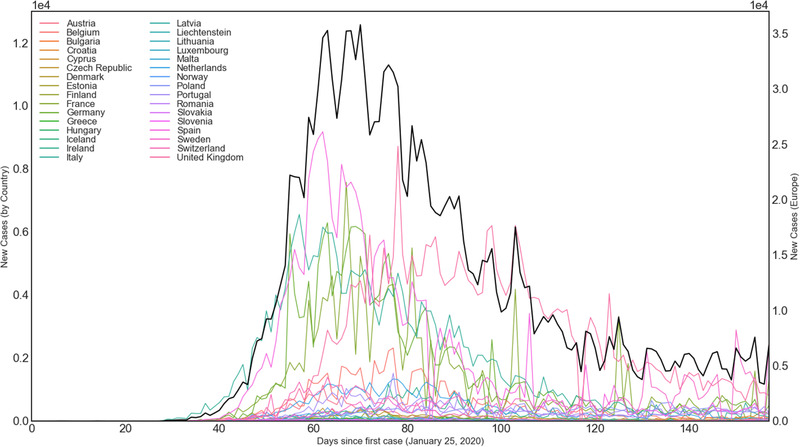
Number of new COVID‐19 cases per day, by the member countries of the European Union, Schengen Area and the United Kingdom, and the total number of new COVID‐19 cases per day reported by the European Centre for Disease Prevention and Control
Unlike the trend observed in the US, the countries in the European block have recorded a decrease in the number of new cases in the last week of June as compared to the previous week. A comparison of the trend observed in the US, Europe and China is given in Figure 6A. The comparison shown in in the graph indicates the effectiveness of a lockdown (in any form) as a viable strategy in reducing the number of new COVID‐19 cases. It also reveals the effectiveness of the stringent lockdown implemented by China. Despite and in spite of China being hit early by the novel coronavirus and not having prior knowledge of the RNA sequencing of the virus and its classification,[ 51 ] swift action to close localities at different administrative divisions ensured that the virus would not spread beyond the more than 2000 new counts per day at its peak.
FIGURE 6.
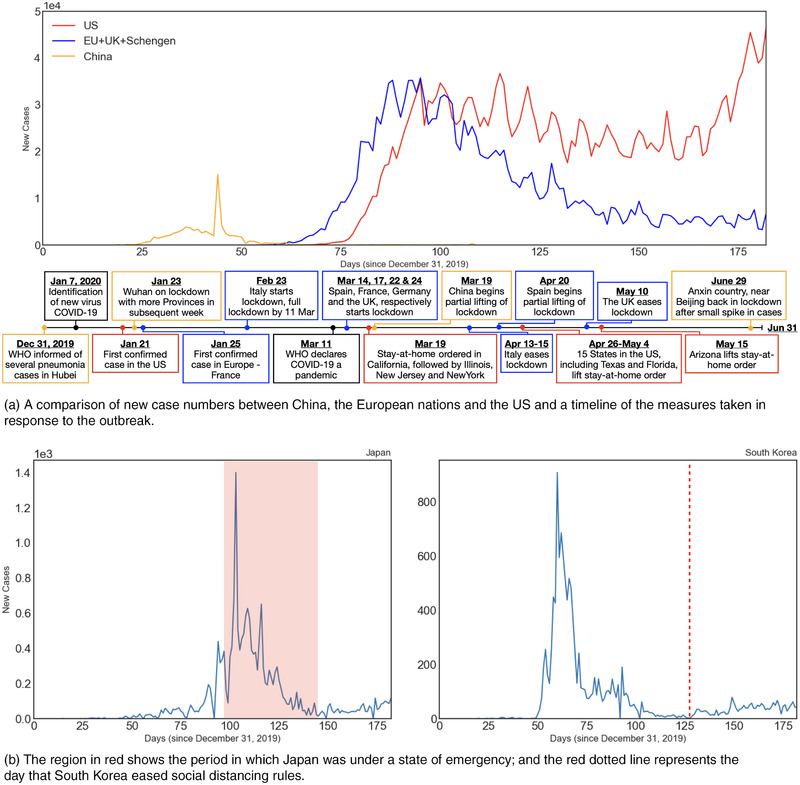
A timeline showing the trajectory of the number of new cases per day in (A) the US, European nations and China; and (B) Japan and Korea.
An analysis of China's timeline also shows a deliberate attempt to gradually lift the lockdown only when they were confident that the spread can be contained. Despite the successful attempts to arrest the spread of the virus through a lockdown, the WHO clarified that the move is not a recommendation given by them and the authorities have to ascertain the effectiveness of such a containment strategy.[ 52 , 53 ] This strategy was also adopted in the early stages by Italy. The lockdown measures implemented by Italy was considered the most radical measure implemented against the outbreak outside China.[ 54 ]
Turning our attention to Japan and South Korea, these two countries have commonly been cited as successful case studies with regards to the management of COVID‐19 outbreak. Both countries adopted different strategies, as seen in Section 2. Japan chose to implement a containment policy by identifying clusters, while South Korea adopted the strategy of mass testing for both suspected individuals and general public through drive‐through testing facilities in the early stages of the spread. Despite not being at the top of the list when it comes to testing per capita, the initial response by conducting mass testing early with the aim of identifying asymptomatic individuals and quarantining them has proven to be helpful. Figure 6B shows the number of new cases in Japan and South Korea. It is worth noting that the number of daily new cases is on the increase after a week Japan emerged from their state‐of‐emergency on May 25, with the same trend being observed in South Korea, after easing of social distancing rules on May 6. Experts have advised that this is not a second wave because of the coordinated efforts employed by both countries to monitor and contain new cases.
Based on a data‐driven approach, we have identified three key strategies in curbing the spread of COVID‐19. They are:
One: Controlled movement by implementing some form of coordinated social distancing, stay‐at‐home order or extreme lockdown.
Two: Early and sustained implementation of containment through internal and external border controls.
Three: Efficient and early testing to identify symptomatic and asymptomatic transmitters.
These important lessons are drawn from the actions taken by highly connected countries, like Japan and South Korea, and regions with porous borders like the inter provincial borders in China and the European nations.
Warning for the US
We acknowledge that the fight against COVID‐19 is far from over. The rising cases in the US at the end of June entering in July, show that the country is facing a health care crisis as the set of second waves in some states are coinciding with the increasing number of new cases in states with late first waves. This causes the infected cases to increase exponentially. The US is in a unique position, as the virus was brought in through the cities with large international airports first. The virus then spread within its borders through internal travel. This is the contributing factor that caused the successive wave phenomenon. With no internal travel ban, cities that have brought the virus under control, and are opening up, are facing a new wave, which then coincides with the first waves of the inland states. As the stay‐at‐home orders were lifted before a clear indication of the virus being under control, such move has resulted in the explosion of cases. Yet, for such protean virus like SARS‐2‐CoV, the execution of strategic measures cannot be ignored. COVID‐19 has been sweeping through the nation like waves on the beach, and it can only be stopped when it comes crashing into an obstacle. Otherwise, it will constructively interfere with other wavelets to give a sustained wave of COVID‐19 cases, as observed in the US.
In terms of the current emergency, states that have lifted their state of emergency may have to re‐impose controlled movement through mandatory social distancing and/or stay‐at‐home orders. In certain states where case counts are increasing exponentially, a potential lockdown may have to be implemented. These are measures that are in line with key strategy One and have been tried and tested; not just in countries mentioned in the current paper, but many other nations[ 55 ] as well. In alignment with key strategy Two, a collective effort between the federal and state government is necessary to implement internal border controls, like those seen in the Schengen area and East Asian nations. Border controls help to contain the virus in a locality, thereby preventing it from infecting more individuals, in waves, as a means of reproduction and mutation.
In a system of governance like the US (where the coordinating authority of healthcare is delegated to the state governors), the federal government must assume authority and responsibility to ensure that governors adhere to the guidelines issued by the CDC. The majority of the world's governments have shown that the fight against COVID‐19 requires unity and coordination amongst the different levels of governing authorities, infectious disease division and scientific community. The handling of the COVID‐19 is a public health crisis and should not be used as a partisan issue.[ 56 , 57 ]
Lastly, we will touch on the key strategy Three—testing. Clearly, the style of governance in the US differs wildly from China's. Strict lockdowns do not embody the spirit of liberty for which the union hinges upon, at the same time, countries like South Korea has shown that with social distancing, isolation and testing, it is also possible to control the spread of the virus. The US has capabilities far greater than South Korea to administer large‐scale coordinated testing, yet it did not implement them in the early stages of the COVID‐19 pandemic. This is coupled with mixed indications on a potential second wave the magnitude of testing and conflicting intentions by the President of the US to scale back testing.[ 58 , 59 , 60 ] Crucially, the US has not reached the scale of testing (suggested by health experts) required to contain the virus. Slow testing means that asymptomatic transmitters continue to spread the virus in the community, making the immediate future of its battle against COVID‐19 look painfully and regrettably bleak.
Yet, we should not ignore the states that have appeared to keep the virus under control—these states are not exactly out of the rough patch, just yet. A small slip or oversight may result in a new wave of infections, like the one seen in South Korea and to a greater extent, Singapore.[ 61 ] As the cases decrease week on week, the attention should now be diverted to its internal borders with other states. The threat of another wave now comes from a slip‐up in across‐state‐boundary imported cases. Thus, for these local governments, attention should not just be placed on how to effectively implement key strategy Two but on a more holisitic approach.
The three key strategies mentioned above must be implemented in certain manner at the state level and mandated at the federal level. Otherwise, the prospect of seeing a superposition of first waves, second waves from further lifting of stay‐at‐home orders and/or even a third wave from states when borders start to open, may bring the health care infrastructure of this superpower to its knees, if COVID‐19 has not already done so. As of now, it does appear that the strategy adopted by the US is, by all empirical data, failing.
Warning for the future
As of writing of this paper, the world is certainly not out of this crisis yet. The increasing trend in infected cases in major countries like Brazil and Russia continues to be of concern to the WHO. However, with many countries already out of their first wave and bracing themselves for a potential second wave, these three key strategies have proven to work and many countries have adopted them to varying degrees of implementation. Labelled as the worst pandemic in this century, it may also not be the last for mankind, especially with globalization, hyperconnectivity, and the extreme centralization and increasing fragility of supply chains.[ 62 ] The lessons learnt from the first wave must be put into good use in containing, or better yet, in preventing a second wave of infections.
Although the situation is changing rapidly in the meantime, the number of new cases recorded beyond June 30, 2020 is trending in the direction that affirms the guidance provided by this paper. As part of the collective scientific response to tackling the COVID‐19 pandemic, this paper made use of 6 months worth of case count data and the strategies employed by multiple countries to present three key strategies. Therefore, these three key strategies cannot be ignored, not even after the current pandemic. The conclusions may seem straightforward, but this is backed up by concrete data that the international community has been waiting to analyse. Now that we have the data and the appropriate course of action, the warnings offered here cannot and should not be ignored anymore.
While we have highlighted the importance of the three key strategies, the extent of implementation needs to be evaluated in accordance to the socio‐economic needs of each country. Be that as it may, our data‐driven approach has shown these three key strategies are guaranteed to reduce the number of new cases significantly. Therefore, these three key strategies should be applied to the context suitable for each country to minimize loss in population and economy.
Finally, hindsight is always 20/20, but we do not need to be deep in a crisis only to acknowledge that certain measures should have been executed earlier. The precautionary principle brings with it debates of being unscientific and an obstacle to progress. Yet, we are brought into this complicated and uncharted terrain because of the rejection by international bodies like the WHO to definitively recommend strict guidelines in the early days of the virus. Be that as it may, it is still the task of the government of individual countries to adopt these strict guidelines. This time, with hindsight, precaution was indeed better than the cure. It is useful to examine the methodologies of science and to consider ways, without compromising integrity and objectivity, that research can be helpful to those who will act with precaution. This paper is important as a warning for future pandemics, that we do not need to have data numbers that read '10 million infected individuals and half a million deaths' before we definitively conclude that early adoption of the three key strategies was not throwing caution to the wind.
CONCLUSION
The successes and failures of COVID‐19 management thus far have set a precedent for how countries should approach future pandemics of this magnitude. The observations and warnings from this paper focus on the approach taken by the US, the group of European nations, China, Japan and South Korea in combating COVID‐19. Despite the WHO being unsure in the beginning stages of COVID‐19, we have now definitively confirmed that the three key strategies are effective in containing the virus and bringing the number of new cases down. In particular, we have taken a data‐driven approach to conclude that (i) decisive form of movement control should be implemented, (ii) strategic coordinated partnership with neighbouring countries or territories is a viable strategy of containment, and (iii) early testing must be conducted to identify symptomatic and asymptomatic transmitters. These strategies are possible considerations and should be implemented in combination to avoid the repeated wave phenomenon seen in the US. A main contribution from this paper is that we have taken a data‐driven approach to analyse the effects of these key strategies that was effective in containing and reducing the number of new cases. As the world moves forward and prepares itself for a potential pandemic of such scale, the lessons learnt from COVID‐19, and in particular the above‐mentioned key strategies should be part of every country's pandemic response. When another virus of such protean nature hits us again, we will not be caught off‐guard by successive wavelets constructively interfering to give a sustained wave. Importantly, we must not allow future pandemics to develop into a full‐blown wave, as COVID‐19 has. Such a data‐driven approach will also be useful to establish new benchmarks in response to future crises of this nature, especially in highly connected territories and regions across the world.
CONFLICT OF INTEREST
The authors declare no competing interests.
ACKNOWLEDGMENT
This project was supported by the Singapore University of Technology and Design Grant No. SRG SCI 2019 142 and SGPCTRS1804.
Lai, J. W. , & Cheong, K. H. (2020). Superposition of COVID‐19 waves, anticipating a sustained wave, and lessons for the future. BioEssays, 42, e2000178. 10.1002/bies.202000178
Footnotes
As there is no clear definition for “second wave”, we interpret a “second wave” as a considerable increase in new cases after a clearly observed drop or stagnation in the number of new cases following the initial increase in infections.
REFERENCES
- 1. World Health Organisation . (2020). Coronavirus disease (COVID‐2019) situation reports, Online, Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
- 2. Cherry, J. D. (2004). The chronology of the 2002‐2003 SARS mini pandemic. Paediatr. Respir. Rev. 5(4), 262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chew, S. K. (2007). SARS: How a global epidemic was stopped. Bull. World Health Organ. 85(4), 324. [Google Scholar]
- 4. Chan‐Yeung, M. , & Xu, R.‐H. (2003). SARS: Epidemiology. Respirology, 8(Suppl. 1), S9–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zumla, A. , Hui, D. S. , & Perlman, S. (2015). Middle East respiratory syndrome. Lancet, 386(9997), 995–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organisation . (2020). Coronavirus disease (COVID‐19) pandemic, Online, Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 7. Liu, Y. , Gayle, A. A. , Wilder‐Smith, A. , & Rocklöv, J. (2020). The reproductive number of COVID‐19 is higher compared to SARS coronavirus. J. Travel Med., 27 (2), taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhao, S. , Lin, Q. , Ran, J. , Musa, S. S. , Yang, G. , Wang, W. , … Wang, M. H. (2020). Preliminary estimation of the basic reproduction number of novel coronavirus (2019‐nCoV) in China, from 2019 to 2020: A data‐driven analysis in the early phase of the outbreak. Int. J. Infect. Dis., 92, 214–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. D'Arienzo, M. , & Coniglio, A. (2020). Assessment of the SARS‐CoV‐2 basic reproduction number, R0, based on the early phase of COVID‐19 outbreak in Italy. Biosafety Health, 2(2), 57–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boccia, S. , Ricciardi, W. , & Ioannidis, J. P. A. (2020). What other countries can learn from Italy during the COVID‐19 pandemic, JAMA Intern. Med., 180(7), 927. [DOI] [PubMed] [Google Scholar]
- 11. Forman, R. , Atun, R. , McKee, M. , & Mossialos, E. (2020). 12 Lessons learned from the management of the coronavirus pandemic. Health Policy, 124(6), 577–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mackenzie, J. S. , & Smith, D. W. (2020). COVID‐19: A novel zoonotic disease caused by a coronavirus from China: What we know and what we don't. Microbiol. Australia, 41(1), 45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organisation . (2020). Timeline of WHO's response to COVID‐19, Online, Retrieved from https://www.who.int/news-room/detail/29-06-2020-covidtimeline
- 14. Ghinai, I. , McPherson, T. D. , Hunter, J. C. , Kirking, H. L. , Christiansen, D. , Joshi, K. , … Uyeki, T. M. (2020). First known person‐to‐person transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) in the USA. Lancet, 395(10230), 1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Penney, J. (2020). U.S. got more confirmed “index cases” of coronavirus from Europe than from China, Online, Retrieved from https://theintercept.com/2020/04/12/u-s-got-more-confirmed-index-cases-of-coronavirus-from-europe-than-from-china/,
- 16. Stokes, E. K. , Zambrano, L. D. , Anderson, K. N. , Marder, E. P. , Raz, K. M. , Felix, S. E. B. , … Fullerton, K. E. (2020). MMWR Morb. Mortal. Wkly. Rep., 69(24), 759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. European Commission . (2020). Overview of the Commission's response, Online, Retrieved from https://ec.europa.eu/info/live-work-travel-eu/health/coronavirus-response/overview-commissions-response_en
- 18. European Council . (2020). COVID‐19 coronavirus pandemic, Online, Retrieved from https://www.consilium.europa.eu/en/policies/coronavirus/
- 19. European Parliament . (2020). Border controls in schengen due to coronavirus: what can the eu do?, Online, Retrieved from https://www.europarl.europa.eu/news/en/headlines/priorities/eu-response-to-coronavirus/20200506STO78514/reopening-schengen-borders-after-covid-19-what-can-eu-do
- 20. The Guardian . (2020). Germany and France reopen borders as Europe emerges from lockdown, Online, Retrieved from https://www.theguardian.com/world/2020/jun/15/germany-and-france-reopen-borders-as-europe-emerges-from-lockdown
- 21. Politico . (2020). Europe's country‐by‐country travel restrictions explained, Online, Retrieved from https://www.politico.eu/article/coronavirus-travel-europe-country-by-country-travel-restrictions-explained-summer-2020/,
- 22. The Guardian . (2020). China to lift travel restrictions in Hubei after months of coronavirus lockdown, Online, Retrieved from https://www.theguardian.com/world/2020/mar/24/china-to-lift-travel-restrictions-in-hubei-after-months-of-coronavirus-lockdown,
- 23. Bloomberg . (2020). China to lift lockdown over virus epicenter Wuhan on april 8, Online, Retrieved from https://www.bloomberg.com/news/articles/2020-03-24/china-to-lift-lockdown-over-virus-epicenter-wuhan-on-april-8,
- 24. Channel News Asia . (2020). China sees uptick in new covid‐19 cases, including 17 in Beijing, Online, Retrieved from https://www.channelnewsasia.com/news/asia/china-sees-uptick-in-new-covid-19-cases--including-17-in-beijing-12875704.
- 25. BBC . (2020). Coronavirus in Suifenhe: Remote border town locks down as China opens up, Online, Retrieved from https://www.bbc.com/news/world-asia-china-52225475, Accessed on 27 June 2020.
- 26. BBC . (2020). Hebei: China locks down 400,000 people after virus spike near Beijing, Online, Retrieved from https://www.bbc.com/news/world-asia-53216047
- 27. Cabinet Public Relations Office of Japan . (2020). Fourth meeting of the novel coronavirus response headquarters, Online, Retrieved from https://japan.kantei.go.jp/98_abe/actions/202002/_00001.html
- 28. Cabinet Public Relations Office of Japan . (2020). Fifth meeting of the novel coronavirus response headquarters, Online, Retrieved from https://japan.kantei.go.jp/98_abe/actions/202002/_00006.html
- 29. Kyodo News . (2020). Abe declares coronavirus emergency over in Japan, Online, https://english.kyodonews.net/news/2020/05/a1f00cf165ae-japan-poised-to-end-state-of-emergency-over-coronavirus-crisis.html
- 30. The Straits Times . (2020). Japan faces second wave of infections in Tokyo and Fukuoka, Online, Retrieved from https://www.straitstimes.com/asia/east-asia/japan-faces-second-wave-of-infections-in-tokyo-and-fukuoka
- 31. Nikkei Asian Review . (2020). Tokyo spike is not a second wave, election‐bound Koike says, Online, Retrieved from https://asia.nikkei.com/Spotlight/Coronavirus/Tokyo-spike-is-not-a-second-wave-election-bound-Koike-says
- 32. Du, L. , & Huang, G. (2020). Did Japan just beat the virus without lockdowns or mass testing?, Online, Retrieved from https://www.bloomberg.com/news/articles/2020-05-22/did-japan-just-beat-the-virus-without-lockdowns-or-mass-testing
- 33. Kim, H. (2020). South Korea learned its successful COVID‐19 strategy from a previous coronavirus outbreak: MERS, Online, Retrieved from https://thebulletin.org/2020/03/south-korea-learned-its-successful-covid-19-strategy-from-a-previous-coronavirus-outbreak-mers/,
- 34. Normile, D. (2020). Coronavirus cases have dropped sharply in South Korea. What's the secret to its success? Science, 10.1126/science.abb7566 [DOI] [Google Scholar]
- 35. Zastrow, M. (2020). How South Korea prevented a coronavirus disaster—and why the battle isn't over, Online, Retrieved from https://www.nationalgeographic.com/science/2020/05/how-south-korea-prevented-coronavirus-disaster-why-battle-is-not-over/
- 36. CoronaBoard . (2020). COVID‐19 dashboard South Korea, Online, Retrieved from https://coronaboard.kr/en/
- 37. Hadden, J. (2020). Photos show South Korea gradually reopening after the rate of new confirmed cases of coronavirus slowed down dramatically in recent weeks to less than ten a day, Online, Retrieved from https://www.businessinsider.com/photos-of-life-resuming-in-south-korea-after-coronavirus-pandemic-2020-5
- 38. BBC . (2020). Coronavirus: South Korea confirms second wave of infections, Online, Retrieved from https://www.bbc.com/news/world-asia-53135626
- 39. Bai, Y. , Yao, L. , Wei, T. , Tian, F. , Jin, D.‐Y. , Chen, L. , & Wang, M. (2020). Presumed asymptomatic carrier transmission of COVID‐19. JAMA, 323(14), 1406–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hu, Z. , Song, C. , Xu, C. , Jin, G. , Chen, Y. , Xu, X. , … Shen, H. (2020). Clinical characteristics of 24 asymptomatic infections with COVID‐19 screened among close contacts in Nanjing, China. Sci. China Life Sci., 63(5), 706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lu, S. , Lin, J. , Zhang, Z. , Xiao, L. , Jiang, Z. , Chen, J. , … Luo, S. (2020). Alert for non‐respiratory symptoms of coronavirus disease 2019 patients in epidemic period: A case report of familial cluster with three asymptomatic COVID‐19 patients. J. Med. Virol., 10.1002/jmv.25776 [DOI] [PubMed] [Google Scholar]
- 42. Nishiura, H. , Kobayashi, T. , Miyama, T. , Suzuki, A. , mok Jung, S. , Hayashi, K. , … Linton, N. M. (2020). Estimation of the asymptomatic ratio of novel coronavirus infections (COVID‐19). Int. J. Infect. Dis, 94, 154–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wu, F. , Wang, A. , Liu, M. , Wang, Q. , Chen, J. , … Huang, J. (2020). Neutralizing antibody responses to SARS‐CoV‐2 in a COVID‐19 recovered patient cohort and their implications. SSRN Electron. J., 10.2139/ssrn.3566211 [DOI] [Google Scholar]
- 44. Xiang, F. , Wang, X. , He, X. , Peng, Z. , Yang, B. , Zhang, J. , … Ma, W.‐L. (2020). Antibody detection and dynamic characteristics in patients with coronavirus disease 2019. Clin. Infect. Dis., 10.1093/cid/ciaa461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shi, Y. , Wang, Y. , an Jianan Huang, C. S. , Gan, J. , Huang, X. , Bucci, E. , … Melino, G. (2020). COVID‐19 infection: The perspectives on immune responses. Cell Death Differentiation, 27, 1451–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Li, X. , Geng, M. , Peng, Y. , Meng, L. , & Lu, S. (2020). Molecular immune pathogenesis and diagnosis of COVID‐19. J. Pharm. Anal., 10, 102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tay, M. Z. , Poh, C. M. , Rínia, L. , MacAry, P. A. , & Ng, L. F. P. (2020). The trinity of COVID‐19: Immunity, inflammation and intervention. Nat. Rev. Immunol., 20(6), 363–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Thevarajan, I. , Nguyen, T. H. O. , Koutsakos, M. , Druce, J. , Caly, L. , van de Sandt, C. E. , … Kedzierska, K. (2020). Breadth of concomitant immune responses prior to patient recovery: A case report of non‐severe COVID‐19. Nat. Med., 26(4), 453–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Max Roser, E. O.‐O. , Ritchie, H. , & Hasell, J. (2020). Our World in Data, Accessed on 01 July 2020. [Google Scholar]
- 50. BBC . (2020). Coronavirus: Fauci warns of 100,000 us cases per day, Online, Retrieved from https://www.bbc.com/news/world-us-canada-53237824
- 51. Gunia, A. , & Zennie, M. (2020). China reported a huge increase in new COVID‐19 cases. Here's why it's actually a step in the right direction, Online, Retrieved from https://time.com/5783401/covid19-hubei-cases-classification/
- 52. Reuters . (2020). Wuhan lockdown ‘unprecedented’, shows commitment to contain virus: WHO representative in China, Online, Retrieved from https://www.reuters.com/article/us-china-health-who-idUSKBN1ZM1G9
- 53. BBC . (2020). Coronavirus: How is the Chinese city at the centre of the outbreak coping?, Online, Retrieved from https://www.bbc.com/news/world-asia-51224504
- 54. BBC . (2020). Coronavirus: Northern Italy quarantines 16 million people, Online, Retrieved from https://www.bbc.com/news/world-middle-east-51787238
- 55. Kaplan, J. , Frias, L. , & McFall‐Johnsen, M. (2020). Our ongoing list of how countries are reopening, and which ones remain under lockdown, Online, Retrieved from https://www.businessinsider.com/countries-on-lockdown-coronavirus-italy-2020-3#new-zealand-now-has-nine-cases-of-coronavirus-after-24-days-with-no-cases-1,
- 56. Aljazeera . (2020). US gov't under fire over COVID‐19 response, Online, Retrieved from https://www.aljazeera.com/news/2020/05/govt-fire-covid-19-response-200510141701694.html
- 57. Fletcher, E. R. , & Ren, G. (2020). Leave politics out of pandemic: WHO rebuts United States criticism over COVID‐19 early warnings, Online, Retrieved from https://healthpolicy-watch.news/who-director-general-rebuts-united-states-criticism-regarding-who-role-in-pandemic/,
- 58. The Guardian . (2020). Global report: Trump says he ordered coronavirus testing to ‘slow down’, Online, Retrieved from Global report: Trump says he ordered coronavirus testing to 'slow down'
- 59. Facher, L. (2020). Top U.S. health officials say they were never told to slow down COVID‐19 testing, contradicting Trump, Online, Retrieved from https://www.statnews.com/2020/06/23/fauci-never-ordered-to-slow-down-testing/
- 60. Sarkis, S. (2020). Trump: Did he order COVID‐19 testing slowed or not?, Online, Retrieved from https://www.forbes.com/sites/stephaniesarkis/2020/06/23/trump-did-he-order-covid-19-testing-slowed-or-not/
- 61. Leung, H. (2020). Singapore was a coronavirus success story—until an outbreak showed how vulnerable workers can fall through the cracks, Online, Retrieved from https://time.com/5825261/singapore-coronavirus-migrant-workers-inequality/
- 62. Cheong, K. H. , & Jones, M. C. (2020). Introducing the 21st Century's new four horsemen of the coronapocalypse. BioEssays, 42(7), 2000063. [DOI] [PubMed] [Google Scholar]


