Abstract
Background:
Women experiencing recent sexual assault (SA) are at high risk for posttraumatic stress disorder (PTSD) and related conditions, with approximately half of women experiencing SA meeting criteria for PTSD. There are no guidelines for the prevention of common mental health disorders after SA. Thus, the purpose of this systematic review and meta-analysis is to synthesize research on secondary preventions for PTSD after SA, determine efficacy, whether any intervention is most promising, and when, how, and to whom interventions should be delivered.
Methods:
After searching electronic databases for secondary preventions for PTSD and related conditions among women experiencing recent SA, 17 studies were reviewed, quality was rated on the Clinical Trials Assessment Measure, and 10 were meta-analyzed (7 excluded due to not being RCTs or heterogeneity).
Results:
Results suggested a small to moderate effect of prevention on reducing PTSD and related symptoms. There was no moderating effect of medication vs. psychosocial interventions, timing, treatment modality, or targeted vs. universal prevention. Half of studies were high quality.
Conclusion:
Cognitive behavioral secondary preventions for PTSD appear to be safe and effective among women experiencing recent SA. Future research should identify best practices, mechanisms of treatment, and once identified, move towards implementation science.
Keywords: sexual assault, posttraumatic stress, secondary prevention, depression, anxiety, substance use
One in five women in the United States (US) report experiencing rape or other forms of sexual assault (SA; Smith et al., 2018), and many experience resulting posttraumatic stress disorder (PTSD) and other mental health disorders including depression, anxiety, and substance use disorder (Dworkin, Menon, Bystrynski, & Allen, 2017) that cause a great burden of personal suffering and economic cost (Peterson, DeGue, Florence, & Lokey, 2017). Despite 100,000 women annually presenting to SA emergency care who receive standard preventions for pregnancy and infectious disease (Smith et al., 2018), there is currently no standard intervention to prevent the more common sequelae of SA: PTSD and related conditions.
To synthesize research on existing secondary prevention programs (defined here as interventions delivered after sexual assault but before the development of stable PTSD symptoms), update prior reviews on the topic with new literature and use of meta-analysis (Dworkin & Schumacher, 2018), and investigate related questions, we conducted a systematic review consistent with PRISMA guidelines (Moher, Liberati, Tetzlaff, Altman, & Group, 2009) of secondary preventions for women experiencing recent SA to mitigate the development of PTSD and related mental health conditions. Particular attention to those experiencing SA (vs. other trauma; Guay, Beaulieu-Prévost, Sader, & Marchand, 2019) is important because women experiencing recent SA are at high risk for developing PTSD compared to those experiencing other trauma types (Smith, Summers, Dillon, & Cougle, 2016), often present to emergency care which is a unique opportunity for secondary prevention (Office on Violence Against Women, 2013), and have historically been underserved in terms of relative attention in research compared to the prevalence of SA (McMahon & Baker, 2011). We elected to focus on women only as they make up the vast majority of individuals experiencing SA (Smith et al., 2018) and have been the primary focus of most SA secondary prevention trials. To maximize the number of studies reviewed, secondary preventions were considered to be those that occurred within 90 days following SA (Kearns, Ressler, Zatzick, & Rothbaum, 2012). Specific aims were to evaluate: 1) are secondary prevention programs effective for mitigating the development of PTSD and related symptoms (e.g., depression, anxiety, substance use) among women experiencing recent SA; 2) is any intervention most promising; and 3) when, how, and to whom should interventions be delivered. Meta-analysis was used to overcome prior limitations of small samples and mixed results, and to quantitatively test whether treatment timing or modality, and sample selection affect outcomes, a valuable next step in the literature as there are currently no accepted guidelines for clinicians and researchers on these matters.
Method
Inclusion/Exclusion Criteria
Inclusion criteria for the review were studies that: were empirical or quantitative in nature; tested a secondary prevention for mental health; and recruited women experiencing recent SA. Exclusion criteria were testing a secondary prevention only focused on pregnancy, sexually transmitted infections, or subsequent SA. Only one study excluded participants with a pre-existing sexual assault history (Tarquinio, Brennstuhl, Reichenbach, Rydberg, & Tarquinio, 2012). Secondary preventions were considered to be those that occurred within 90 days following SA (Kearns et al., 2012).
Literature Search and Study Retrieval
Two databases were used to search for manuscripts: PubMed and PsycInfo. The following terms were paired to search for articles: SA; rape; prevent*; intervention; treatment in the title or abstract with posttraumatic stress disorder (PTSD), acute stress disorder (ASD) occurring anywhere in the text for the intervention and treatment searches. All articles were in English, could have been published at any time, and dissertations were not excluded. All were first screened for duplicates, then by title and abstract, and finally, by full text. We also reviewed citations, including of prior reviews, for any additional studies, and searched the PTSDpubs database. Searches were conducted in Summer 2019.
Data Extraction and Coding Procedures
Studies were coded by the first and second author using a form developed in concordance with previous recommendations (Supplementary Table 1; Guyatt et al., 2008; Haidich, 2010). For studies with multiple trauma types, only SA data was entered into analyses (e.g., for Zohar et al., 2018, the “intentional trauma” group was included). All studies were coded by first and second authors. Any disagreements were resolved through discussion and consultation with the third author.
Quality Assessment
For all randomized clinical trials, the Clinical Trials Assessment Measure (CTAM; Tarrier & Wykes, 2004) was used by the first and second authors to assess clinical trial quality. Scores range from 0 to 100, with scores <65 considered adequate quality. Any disagreements regarding coding were resolved through discussion and consultation with the third author.
Data Analytic Plan
Descriptive data for all studies (e.g., study characteristics) were entered into Excel spreadsheets. Meta-analysis was performed on all RCTs included in the current review as two groups were needed to analyze between-group effects. Statistical data, including means and standard deviations as well as effect sizes were entered into an Excel template, Meta-Essentials (Suurmond, van Rhee, & Hak, 2017), which calculates overall combined effects (Hedge’s g) using the Knapp-Hartung adjustment of the DerSimonian-Laird estimator (DerSimonian & Laird, 1986; IntHout, Ioannidis, & Borm, 2014). To measure heterogeneity of study effects, Cochrane’s Q, its significance level, and I2 measuring proportion of observed variance reflecting real differences in effect size were each computed. I2 values > 25% were considered large and worthy of further exploration (Borenstein, Hedges, Higgins, & Rothstein, 2009).
Meta-Essentials also provides the ability to analyze moderator effects and publication bias using a funnel plot depicting individual effect sizes and standard errors compared to their combined effect size. Publication bias is considered a possibility when there is evidence for asymmetry in the plot (Suurmond et al., 2017). Trim-and-fill procedures were used to account for any publication biases and provide more accurate adjusted effect size estimates (Duval & Tweedie, 2000). Egger regression was used to statistically test for asymmetry in the funnel plot and provide a quantitative assessment of bias vs. visual assessment (Egger, Smith, & Phillips, 1997). Finally, failsafe ns were computed to determine the number of “file drawer” studies without significant effects would be needed to nullify any current findings.
Considering many studies reported a variety of outcome measures, one single measure was selected for maintenance of the assumption of independence for meta-analyses. We selected measures of PTSD when possible, clinician-administered over self-report measures, then anxiety, depression, and substance use measures.
Results
Study Selection and Characteristics
17 studies were identified (see Figure 1; Supplementary Table 2). Most occurred within an emergency department or emergency care (n = 11), followed by outpatient treatment and/or research centers (n = 4), and rape crisis or SA centers (n = 2). Studies included a total of 2,182 women. Individual sample sizes ranged from 13 to 406 (M = 126.25). The mean age ranged from 23 to 39 (M = 29.56). The majority of studies recruited all women, with exception of three: (Gilmore et al., 2019a; 84.6% women; Rothbaum et al., 2012; 97.9%; Zohar et al., 2018; 100% women in SA sample). Regarding coding, there were several disagreements between coders that were resolved by consensus discussion and consultation with the third author. Further, interrater reliability was calculated prior to consensus discussion for a random 25% of the studies reviewed, indicating substantial agreement between coders (κ=.61, p<.001).
Figure 1.
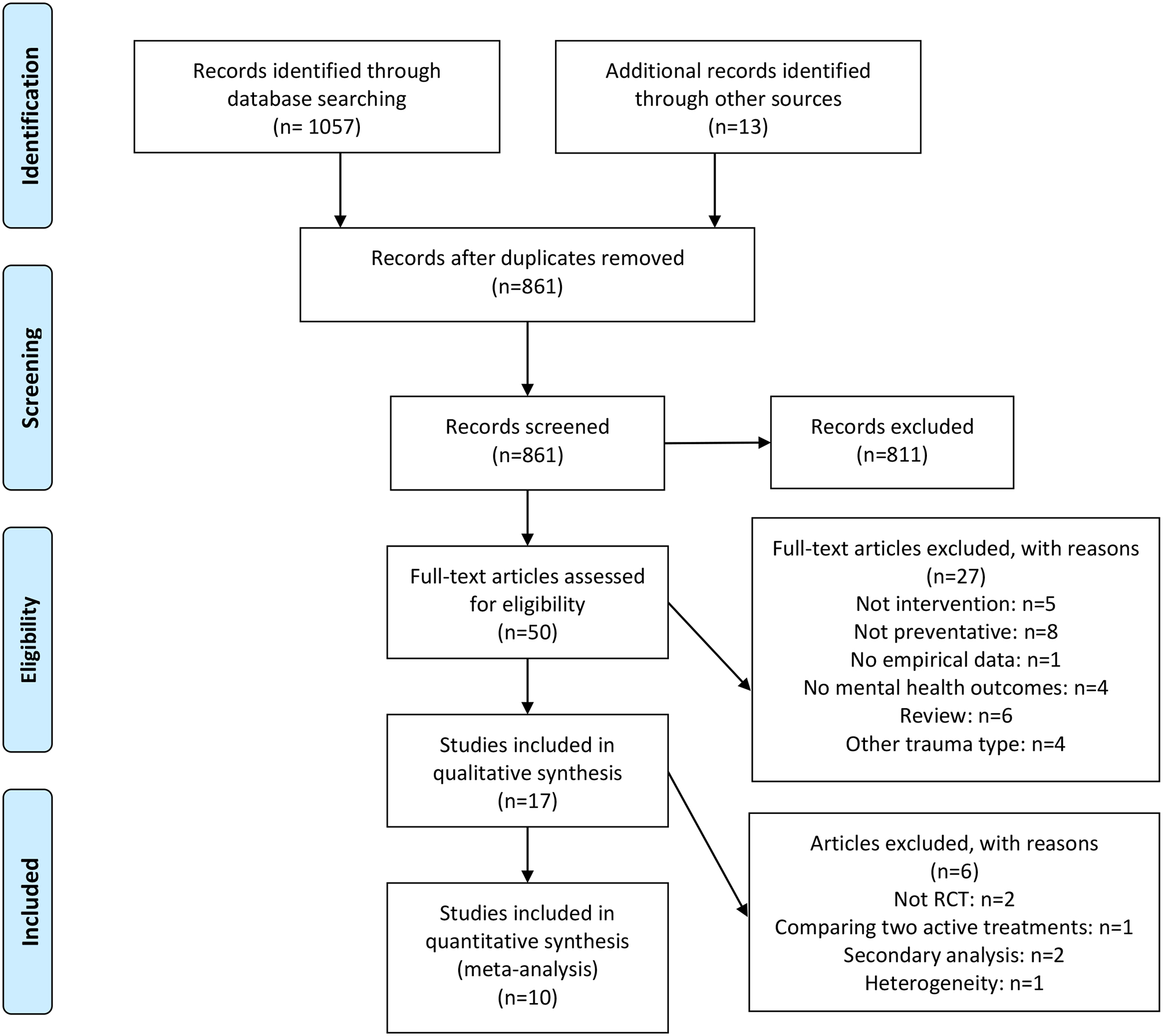
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) inclusion flow diagram
Participants
Inclusion Criteria.
The majority of studies included adult women aged 18 and older, but seven included adolescents (Acierno, Resnick, Flood, & Holmes, 2003; Foa, Hearst-Ikeda, & Perry, 1995; Gilmore et al., 2019b; Gilmore et al., in press; Resnick, Acierno, Kilpatrick, & Holmes, 2005; Resnick et al., 2007; Walsh et al., 2017). Seven studies recruited within 72 hours of exposure (Acierno et al., 2003; Miller, Cranston, Davis, Newman, & Resnick, 2015; Resnick, Acierno, Holmes, Kilpatrick, & Jager, 1999; Resnick et al., 2005; 2007; Rothbaum et al., 2012; Tarquinio et al., 2012), one within 120 hours (Gilmore et al., 2019a), three within 7 days (Gilmore et al., 2019b; Gilmore et al., in press; Walsh et al., 2017) one recent but unspecified (Hassija & Gray, 2011), two within a month (Frank et al., 1988; Nixon, Sterk, Pearce, & Weber, 2017; Zohar et al., 2018), and two within two months (Foa et al., 1995; Foa, Zoellner, & Feeny, 2006). A minority of studies recruited based on clinical characteristics or risk for PTSD (n = 4).
Exclusion Criteria.
Regarding comorbid psychopathology, seven studies excluded those with psychotic or bipolar spectrum disorders (Acierno et al., 2003; Foa et al., 1995; 2006; Nixon et al., 2017; Resnick et al., 1999; Rothbaum et al., 2012; Zohar et al., 2018). Individuals with current or history of substance use disorder were excluded in six studies (Foa et al., 1995; 2006; Nixon et al., 2017; Rothbaum et al., 2012; Tarquinio et al., 2012; Zohar et al., 2018). Those with ongoing risk for suicide were excluded from three studies (Nixon et al., 2017; Rothbaum et al., 2012; Zohar et al., 2018), and individuals with personality disorders were excluded from one study (Zohar et al., 2018). Further, four studies excluded women with serious physical injuries (Resnick et al., 1999; 2005; Rothbaum et al., 2012; Zohar et al., 2018). Five studies excluded individuals with intellectual disability or dementia (Acierno et al., 2003; Nixon et al., 2017; Resnick et al., 1999; 2005; Zohar et al., 2018). Two studies excluded individuals suffering from illness of “organic nature” (Foa et al., 1995; 2006), and one excluded individuals with “mental troubles” and contraindication for EMDR (Tarquinio et al., 2012).
Several studies excluded participants with acute peritraumatic difficulties such as acute intoxication (Acierno et al., 2003; Resnick et al., 1999; 2005; Rothbaum et al., 2012), severe agitation or distress (Acierno et al., 2003; Resnick et al., 1999; Rothbaum et al., 2012), exhaustion (Resnick et al., 1999), not alert or oriented or in severe pain (Rothbaum et al., 2012). A few studies included practical exclusion criteria, such as being unable to see or hear (Rothbaum et al., 2012), inability to provide consent (Miller et al., 2015; Resnick et al., 2007), and insufficient English (Nixon et al., 2017).
More rarely, participants were excluded if they were pregnant, lactating, or of childbearing age without using contraceptives (Zohar et al., 2018). Certain medical conditions were exclusion criteria (e.g., history of major physical illness) in one study (Zohar et al., 2018). Two studies excluded participants with ongoing relationships with the assailant (Foa et al., 1995; 2006). One excluded participants who lost consciousness for more than five minutes (Rothbaum et al., 2012). Finally, one study excluded participants taking psychiatric medications or participating in psychotherapy (Zohar et al., 2018).
Interventions
In terms of active interventions, several studies tested Resnick and colleagues’ seventeen minute video intervention that provided preparatory medical information for the medical and forensic examination, as well as psychoeducation regarding common responses to SA and cognitive-behavioral strategies to reduce avoidance and substance use (Acierno et al., 2003; Resnick et al., 1999; Resnick et al., 2005; Resnick et al., 2007). In some of these studies, both the seventeen-minute and a nine-minute video including psychoeducational component were included (Gilmore et al., 2019b; Miller et al., 2015; Walsh et al., 2017) and in one study only the nine-minute video was examined (Miller et al., 2015).
Several studies tested cognitive behavioral interventions. First, Frank and colleagues (1988) tested two CBT interventions: systematic desensitization (Wolpe, 1990), and CBT (Beck, 1972). Foa and colleagues (1995; 2006) tested a brief CBT intervention with four two-hour weekly group meetings involving psychoeducation, breathing and relaxation, imaginal and in vivo exposure, as well as cognitive restructuring. Gilmore and colleagues (2019a) utilized cognitive behavioral techniques in an mHealth application format targeting psychoeducation and coping skills. Some studies also used gold standard PTSD treatments. Hassija and Gray (2011) tested standard PE or CPT for an average of thirteen sessions via telehealth. Similarly, Nixon and colleagues (2016) used CPT for an average of six sessions. Rothbaum and colleagues (2012) tested a brief PE protocol lasting for three one-hour sessions.
One study tested a newly developed urgent eye movement desensitization and reprocessing (URG-EMDR) protocol of one session of EMDR involving recounting the SA along with lateral eye movements and brief processing, with the goal of reducing distress throughout the session (Tarquinio et al., 2012).
Finally, one study tested pharmacological interventions: Zohar and colleagues (2018) tested escitalopram titrated 10mg to 20mg per day up to 24 weeks.
Control Conditions
Control conditions varied, but many studies had no or weak control conditions (n=13): three were not randomized, thus had no control group (Gilmore et al., 2019a; Hassija & Gray, 2011; Tarquinio et al., 2012), and six compared the active condition to treatment as usual (Acierno et al., 2003; Miller et al., 2015; Nixon et al., 2016; Resnick et al., 1999; 2005; 2007). Three studies utilized assessment only as control (Foa et al., 1995; 2006; Rothbaum et al., 2012). Six had relatively stronger, active control conditions, including relaxation (Gilmore et al., 2019b; Walsh et al., 2017), supportive counseling (Foa et al., 2006, which was in addition to an assessment only group also counted above), two active treatments compared to a non-victimized control group (Frank et al., 1988), and placebo (Zohar et al., 2018).
Outcome Measures
Follow-Up Period.
Outcome assessments ranged from post-treatment (Frank et al., 1988; Gilmore et al., 2019a; Hassija & Gray, 2011; Resnick et al., 1999; Zohar et al., 2018), to six weeks (Acierno et al., 2003; Gilmore et al., 2019b; Resnick et al., 2005), two months (Miller et al., 2015), three months (Rothbaum et al., 2012), six months (Foa et al., 1995; Gilmore et al., 2019b; Resnick et al., 2007; Tarquinio et al., 2012; Walsh et al., 2017), twelve months (Foa et al., 2006; Nixon et al., 2016) following treatment. Studies administered a variety of measures at these time points.
PTSD.
In terms of clinical interview (used by five studies), two used the gold standard Clinician Administered PTSD Scale (Nixon et al., 2016; Weathers, Keane, & Davidson, 2001; Zohar et al., 2018). Three studies used the interview version of the PTSD Symptom Scale (PSS-I), which is also a widely-used semi-structured interview with excellent psychometric properties (Foa et al., 1995; Foa & Tolin, 2000; Foa et al., 2006; Rothbaum et al., 2012).
The self-report version of the PSS was used by six studies (Foa et al., 1995; Foa et al., 2006; Miller et al., 2015; Resnick et al., 1999; Resnick et al., 2005; Zohar et al., 2018). Two studies used the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997; Gilmore et al., 2019b; Rothbaum et al., 2012). Hassija and Gray (2011) used the PTSD Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993). Tarquinio et al. (2012) used the Impact of Event Scale (IES; Horowitz, Wilner, & Alvarez, 1979).
Depression.
Eight studies assessed depression as an outcome. Six studies used the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996; Foa et al., 1995; Foa et al., 2006; Frank et al., 1988; Nixon et al., 2016; Resnick et al., 2005; Rothbaum et al., 2012), one used the Center for Epidemiological Studies Depression Scale (CES-D; Hassija & Gray, 2011; Radloff, 1977), and another used the Montgomery–Asberg Depression Rating Scale (MADRAS) and a visual analogue scale (VAS) to assess depression (Benazzi, 1999; Zohar et al., 2018).
Anxiety.
Seven studies measured anxiety symptoms as an outcome. Two studies used the State Trait Anxiety Inventory (STAI; Frank et al., 1988; Miller et al., 2015; Spielberger, 2010), three used the Beck Anxiety Inventory (BAI; Beck & Steer, 1993; Foa et al., 2006; Resnick et al., 1999; Resnick et al., 2005), one used the Fear Survey Schedule (Frank et al., 1988; Veronen & Kilpatrick, 1980), and one used a VAS to measure anxiety (Zohar et al., 2018).
General Mental Health Disorders.
One study measured overall mental health functioning using the Clinical Global Impressions (CGI; Guy, 1976; Zohar et al., 2018).
Alcohol and Substance Use Disorders.
Four studies measured substance use as outcomes using the Timeline Followback (Acierno et al., 2003; Sobell & Sobell, 1992), clinical interview (Resnick et al., 2005), and self-report (Gilmore et al., 2019b; Walsh et al., 2017).
Quality
Using the CTAM, fourteen studies were scored for quality (the remaining two studies were not RCTs and thus not appropriate to be scored with the CTAM; Gilmore et al., 2019a; Hassija & Gray, 2011). Nine of fourteen (56.3%) met criteria for “high quality” according to receiving ≥65 on the CTAM. In terms of sample, three studies suffered from less than adequate sample sizes according to the CTAM, which suggests >27 participants per treatment arm or adequately described power analysis. Regarding allocation, two studies did not use true randomization and five did not adequately describe how randomization was completed. In terms of assessment, all studies used standardized measures to assess outcomes. For one, therapists were assessors and were not blind. For three others, blinding was not described. The majority used treatment as usual (TAU) instead of a credible control condition. The majority analyzed data appropriately. Four studies did not use PTSD symptoms as an outcome despite the PTSD focus of the treatments. Most (n=10) did not use intent-to-treat analyses or did not describe how missing data was handled, despite significant attrition. Regarding the active treatment, most studies used adequately described treatments with manualized protocols. Only one study described quality control (i.e., supervisors ensured adherence to treatment protocol).
We also reviewed proportions of participants who were approached and participated, excluded, and dropped from the study. The proportion of those approached who participated ranged from 1.4% to 94% (M=49%). The proportion of those excluded ranged from 8% to 70% (M=48%). Finally, the proportion of individuals who dropped or were lost to follow-up ranged from 0% to 56% (M=36%).
Are Secondary Preventions Effective?
There were 11 studies originally included in the meta-analysis (Table 1; Figure 1). Overall, active interventions displayed a medium combined effect on PTSD and related symptoms vs. control (Hedge’s g=.54, 95% CI [.04, 1.04]). However, significant heterogeneity was found (Q=103.83, p <.001, I2=90.37%), indicating combined effect sizes should not be interpreted. Upon further review, it was noted that one study greatly contributed to heterogeneity: Rothbaum et al. (2012). Potential reasons for this discrepancy will be discussed, but because there were no apparent unique characteristics of this study, subgroup analyses were deemed inappropriate. Therefore, this study was removed, and the final meta-analysis sample size was 10. Once this study was dropped, heterogeneity was within a moderate range and not significant (Q=12.68, p=.18, I2=29.00%). Final combined effect sizes were small to medium and statistically significant (g=.27, 95% CI [.08,.47]), favoring active secondary preventions over control conditions on reducing PTSD and related symptoms. There was no significant difference in outcomes regardless of whether medication or psychosocial interventions were used (β=.28, SE=.20, p=.150).
Table 1.
Effect sizes and weight for each study from the meta-analysis, as well as combined estimates.
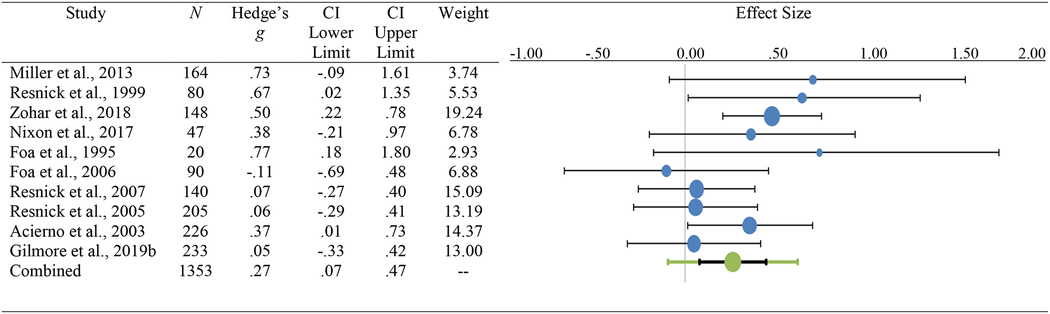
|
When, How, and To Whom Should Interventions be Delivered?
When.
First, we examined whether length of time since trauma (in days) moderated the effect of treatment outcome. Seven studies examined effects of a treatment delivered within hours of trauma exposure, while the other three studies ranged from 13 to 120 days. There was no significant impact of time of delivery on treatment outcomes (β=-.001, SE=.00, p=.718).
How.
Second, we examined whether method of delivery (i.e., 0=video vs. 1=in-person therapist) moderated treatment outcomes among psychosocial interventions (n=9). No effect of treatment modality on outcomes was detected (β=-.09, SE=.19, p=.626).
To Whom.
Finally, we examined whether selecting at-risk participants (targeted intervention) vs. all trauma-exposed participants (universal intervention) moderated treatment outcomes. Five studies used some form of risk for PTSD as inclusion criteria (e.g., displaying some or all initial symptoms of PTSD), while the remaining six recruited anyone who had experienced recent SA without any specific inclusion criteria. Again, no significant effects were found (β=.16, SE=.17, p=.350), suggesting participants benefited equally whether or not they demonstrated risk for PTSD.
Publication Bias
The funnel plot (Figure 2) displayed slight evidence of asymmetry, indicating publication bias. More studies to the right (higher end of the effect size) were found. Thus, a trim-and-fill procedure was used to adjust for potential publication bias (Figure 3; Duval & Tweedie, 2000). Adjusted combined effect size was smaller but remained significant in the small to medium range (Cohen’s d=.28, SE=.09, 95% CI [.08,.47]). Egger regression was not significant (B=1.52, SE=.1.12, 95% CI [-1.01, 4.05]). Rosenthal’s fail-safe n suggested 52 studies with no effect would be required to bring the overall combined effect size to a non-significant value, while Gleser and Olkin’s fail-safe n suggested only 13 studies would be needed.
Figure 2.
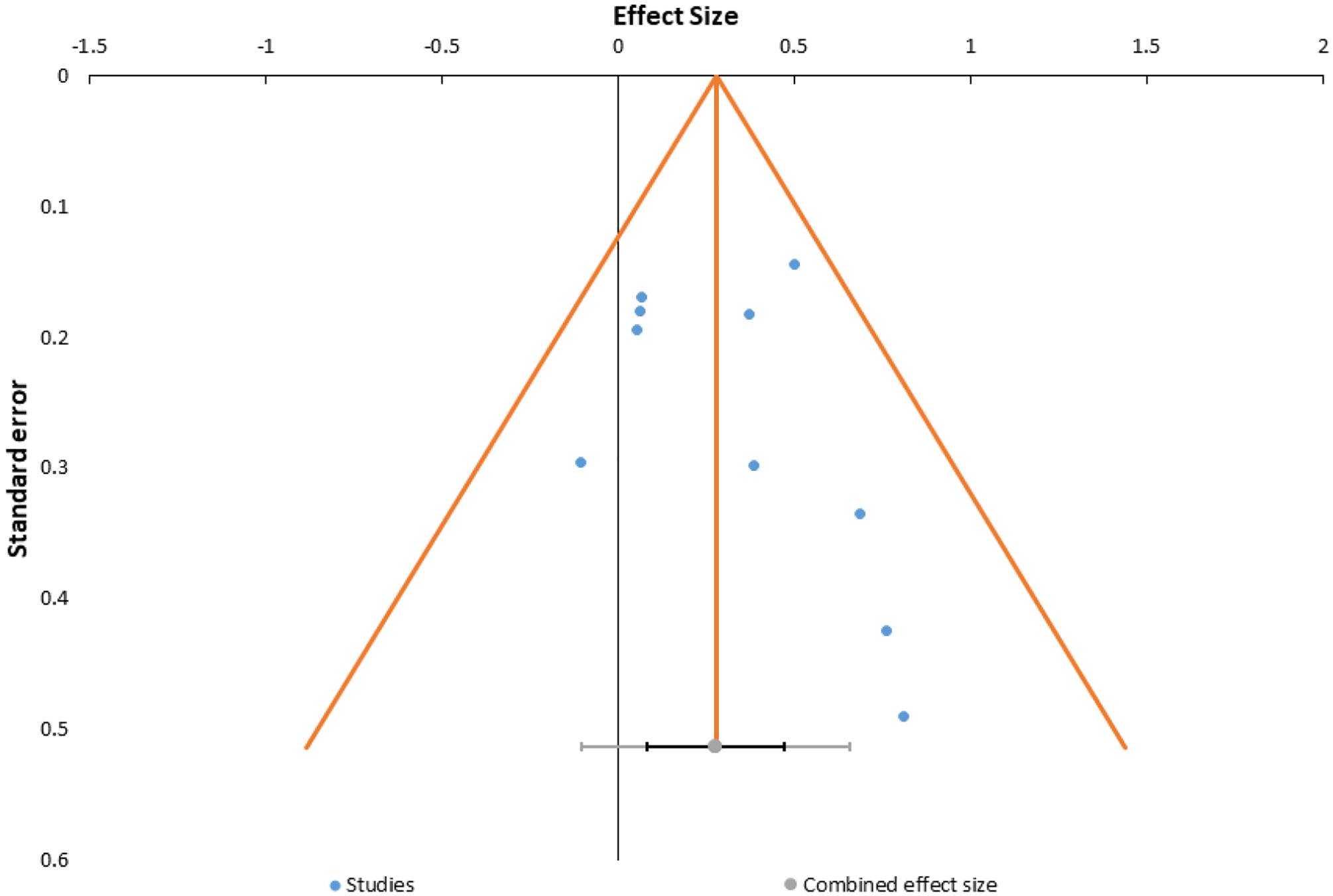
Funnel plot of effect sizes for secondary preventions among women experiencing recent SA
Figure 3.
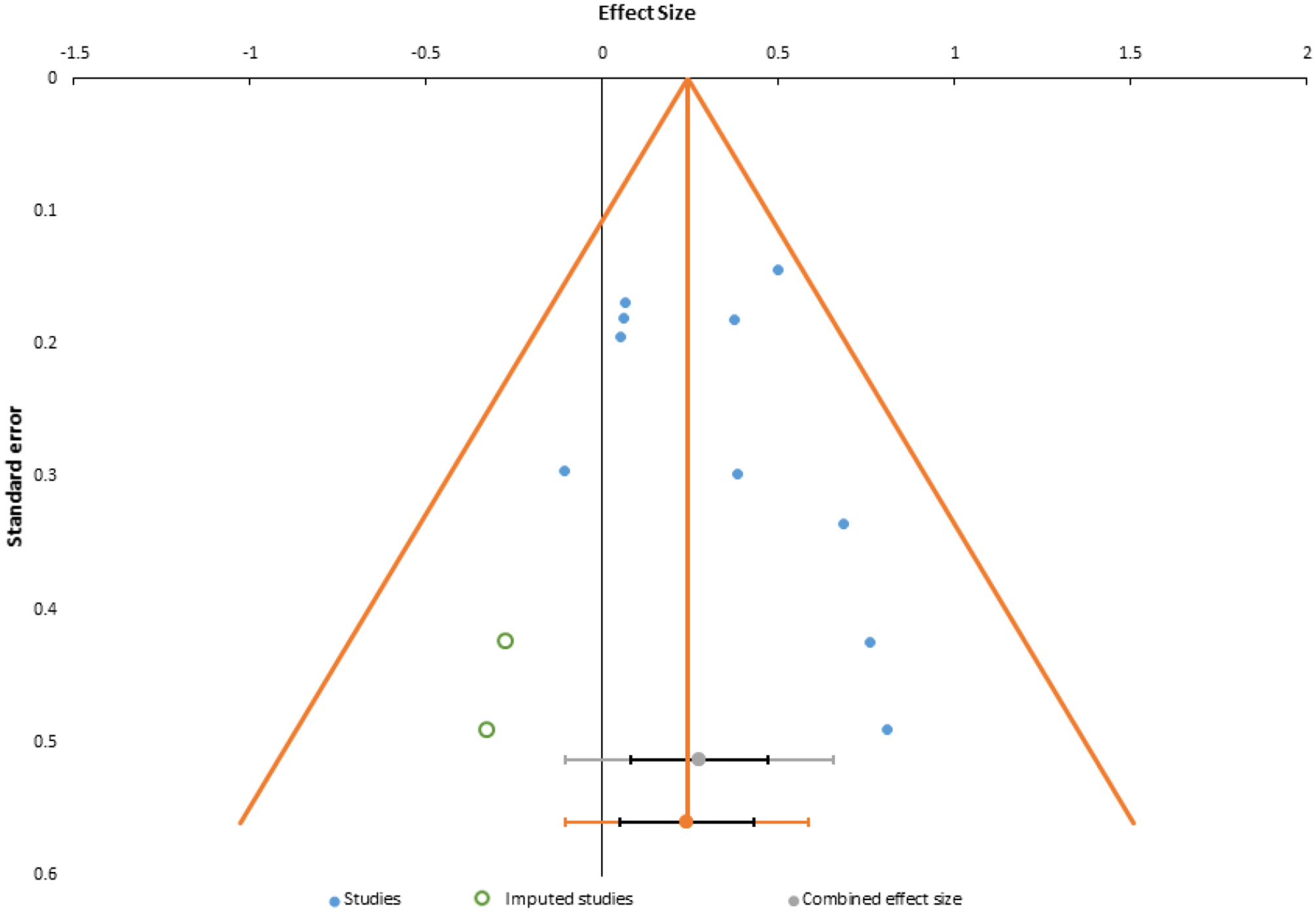
Funnel plot with imputed studies using trim-and-fill procedures.
Discussion
Results of the current systematic review of 17 studies and meta-analysis of 10 studies indicated that secondary preventions delivered within 90 days of SA were effective in reducing the development of PTSD and related symptoms, with a small to moderate effect size. Findings appear to be robust to publication bias. There was no statistically significant moderating impact of any of the following: pharmacological vs. psychological intervention, timing of intervention delivery, modality of treatment delivery, and universal vs. targeted approach.
Meta-Analytic Findings
After adjusting for publication bias, a small to moderate (Cohen’s d=.28) effect of secondary prevention on reducing PTSD and related symptoms was found. The sample size of studies included in the meta-analysis (n=10) was small, so results should be interpreted with some caution. Relatively small effects may be expected given the natural recovery process that occurs after trauma (Galatzer-Levy, Huang, & Bonanno, 2018). Overall, results are consistent with a prior review suggesting efficacy for early behavioral interventions for the prevention of PTSD symptoms among various trauma types (Agorastos, Marmar, & Otte, 2011), and a review of treatments for women experiencing recent SA with chronic PTSD, suggesting cognitive-behavioral interventions lead to reductions in PTSD symptoms (Vickerman & Margolin, 2009).
No moderators were associated with differential outcomes. First, pharmacological vs. psychological treatments had equivalent outcomes. This is consistent with research finding CBT is comparable to medication for PTSD (Rauch et al., 2019) but inconsistent with a meta-analysis finding that pharmacological secondary preventions are not effective (Amos, Stein, & Ipser, 2014). Only one medication trial was included, so more research is needed to form conclusions. Similarly, although not included in the meta-analysis, only one uncontrolled trial using EMDR has been conducted, so more research would be needed to demonstrate efficacy of EMDR as a preventative intervention following SA (Tarquinio et al., 2012). Second, time since trauma did not impact outcomes, in contrast with conceptualizations that intervening within the early hours after trauma could represent a “golden hour” for prevention (Zohar, Sonnino, Juven-Wetzler, & Cohen, 2009). However, all treatments were administered in the early days or weeks after trauma. Alternatively, more power may be needed to detect such an effect. Given these findings, it may be conceptually and practically preferable to deliver interventions as early as possible so the burden of PTSD can be mitigated (Dworkin et al., 2017). In sum, evidence suggests that intervening within hours to weeks after trauma exposure is equivalently effective. However, if individuals meet criteria for PTSD, first-line PTSD treatments are recommended (Ostacher & Cifu, 2019).
Next, there was no impact for modality of treatment intervention, with both video (e.g., Resnick and colleague’s video psychoeducation and cognitive-behavioral intervention [1999]) and in-person modalities demonstrating equivalent effect. We considered Resnick and colleague’s video intervention CBT-oriented, but it is brief and, in some studies included medical preparatory information related to medical examinations. Despite this, findings are consistent with a systematic review finding that computerized interventions for PTSD-related conditions produced similar effect sizes to in-person treatment (Amstadter, Broman-Fulks, Zinzow, Ruggiero, & Cercone, 2009). This is promising as video or computerized interventions may be an opportunity to intervene in the early hours or days following SA when it may be difficult to connect with a psychotherapist. Future research is necessary to determine the efficacy of such interventions as Resnick and colleague’s video intervention has produced mixed results on preventing PTSD, though more robust effects have been found on problematic substance use (Acierno et al., 2003; Gilmore et al., 2019b; Miller et al., 2015; Walsh et al., 2017). It is possible utilizing new technology could strengthen effects by providing more opportunity for psychoeducation and practice of techniques.
Our results also indicated that interventions provided similar effects when recruiting at-risk vs. all women, suggesting all participants can benefit from secondary prevention. This may not be surprising considering this population is particularly at risk for PTSD. However, for all moderating analyses, greater power is likely necessary to detect potential moderating effects of treatment outcomes (Brown et al., 2013). Thus, future research in this area could potentially elucidate when, how, and to whom secondary preventions would provide most benefit.
Finally, in regards to study inclusion for the meta-analysis, we found significant heterogeneity requiring us to remove Rothbaum and colleagues’ study due to the relatively large effect size (g = 2.56; Borenstein et al., 2009). We were unable to determine unique factors of this study that could be controlled for to maintain it in analyses. For example, the design included similar time points and measures to other studies, and an intervention focused on multi-session behavioral therapy with exposure, but other studies also included some components of behavioral therapy (though less explicitly focused on exposure) and/or included multiple sessions (e.g., Acierno et al., 2003; Foa et al., 1995; 2006; Miller et al., 2015; Nixon et al., 2017; Resnick et al., 1999; 2005; 2007). As such, it is unclear why this intervention performed better than others, and future research replicating findings may provide clarity on relative effectiveness.
Study Quality
Regarding study quality of all RCTs reviewed, over half met criteria for high quality according to the CTAM (n=9/14). The studies reviewed had notable strengths, including recruitment of locally representative samples, true randomization, and the use of standardized assessment measures, often with clinical interviews. Some common limitations were control conditions were often treatment-as-usual, thus trials were unable to rule out non-specific therapeutic factors that may have influenced results; many studies lacked details on assessor blinding. Further, some studies did not clearly justify the measures used to analyze results. For example, some included measures of PTSD that were not analyzed. In the future, studies should clearly justify measures used and test all a priori hypotheses. Fourth, most interventions did not include quality control, such as ensuring therapists were adherent to manuals. Fifth and finally, there were relatively low proportions of participants who enrolled vs. those approached, a high proportion excluded, and high drop-out rates across most studies. This highlights the inherent difficulty in recruiting and retaining this vulnerable population (Campbell & Adams, 2009), but constrains the generalizability of results. Future researchers should continue to strive to include the highest number of women possible and use countermeasures to ensure the highest possible levels of retention (Short et al., in press).
Clinical Implications
Secondary preventions appear to be effective in mitigating the development of PTSD and related conditions after SA. However, it is difficult to select a specific intervention to recommend. Most importantly, there certainly appears to be no harm in delivering early psychoeducational or cognitive-behavioral interventions to women experiencing recent SA. Thus far, research only indicates benefit to offering women the opportunity to participate in preventative psychoeducational or cognitive-behavioral interventions, as early as possible or desired. However, it is imperative to note that once women meet diagnostic criteria for PTSD, providers should deliver first-line treatments for PTSD which have a stronger evidence base (Vickerman & Margolin, 2009).
Limitations of Review and Meta-Analysis
The current review and meta-analysis provided the first systematic and quantitative evaluation of secondary preventions for PTSD and related symptoms among women experiencing recent SA and provides recommendations for future research and clinical practice. However, there are limitations and directions for future research. First, the sample size of studies is small (n=17), and smaller in the meta-analysis (n=10). More studies in the area are needed, particularly to make any conclusions regarding moderators. Second, the small number of studies was combined with heterogeneous methodology of included studies. Statistical heterogeneity was handled, but there were still key differences in study methods. Considering this, future research would solidify conclusions. Third, the scope of this review was limited to secondary preventions for women experiencing recent SA and cannot be generalized to those with chronic PTSD or other forms of trauma exposure. Further, results cannot be generalized to men or gender-nonconforming individuals who also experience sexual assault. However, this is an important population given the high prevalence of PTSD and promising opportunity for secondary prevention in the emergency care setting (Resnick et al., 2005). Fourth, authors were not blinded to authors and institutions when reviewing articles, which could reduce any potential bias in future research. Fifth, because there was a relatively small number of studies including strictly secondary prevention studies (e.g., before the development of PTSD or within one month following trauma exposure), we elected to include studies that recruited participants within 90 days of SA as this time frame allowed more studies to be included and also represents a time in which PTSD symptoms become fairly stable (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). However, only two studies included a small number of women who had experienced SA over a month ago (Foa et al., 1995; Foa et al., 2006). Sixth, it is impossible for this review to assess whether participants had prior trauma exposure and a pre-existing diagnosis of PTSD. Thus, some of the interventions may have served as a tertiary prevention for PTSD for women with premorbid PTSD. Seventh, the quality of studies other than RCTs was not formally assessed; however, this made up only 6/17 studies. Eighth, there were no systematic attempts to contact potential authors of “file drawer” studies, thus there remains the possibility of unpublished trials without significant effects. We attempted to overcome this limitation by calculating failsafe n statistics.
Future Research Directions
First, brief psychoeducation or cognitive-behavioral interventions are promising and studies should move forward to more stringent controls to ascertain the relative efficacy of these interventions (e.g., supportive counseling, relaxation and deep breathing interventions provided by Foa et al., 2006; Gilmore et al., 2019b; Walsh et al., 2017). There is a need for more representative inclusion of participants and retention of participant for studies, with recommendations outlined above. Critically, and in accordance with recent National Institute for Mental Health (NIMH) guidelines (National Institute for Mental Health, 2015), only one study evaluated potential treatment mechanisms (Gilmore et al., 2019b). Explicating mechanisms is crucial and may help find ways to strengthen the small effect sizes of effective interventions. Continuing to assess moderators of efficacy (e.g., prior trauma exposure; Miller et al., 2015) is also necessary to understand who benefits most from these interventions. Finally, as this research moves forward, researchers can begin implementing hybrid effectiveness-implementation designs to ensure that efficacious interventions can be disseminated into the communities where they are needed.
Conclusions
In summary, research on the secondary prevention of PTSD-related conditions among women experiencing recent SA has coalesced to suggest it is likely efficacious to use psychosocial, cognitive-behavioral, and potentially pharmacological, interventions to reduce the significant burden of PTSD in this population. Clinically, providers should consider delivery of psychoeducational or cognitive-behavioral secondary preventions in this population. Future research should continue to isolate the most promising interventions, compare these to more stringent controls, and learn how to best implement these interventions into appropriate settings, such as emergency care.
Supplementary Material
Acknowledgments:
This work was supported in part by funding from the National Institute on Drug Abuse (NIDA K23DA042935; PI: Gilmore). NIDA played no role in the development of this manuscript, data analysis, writing, or the decision to submit the manuscript for publication. The authors would like to thank Mariah Evans, who assisted in compiling references and formatting the manuscript.
Appendix 1.
Summary of studies included.
| Citation | Design | Participants | Setting & Location | Intervention | Control | Outcomes |
|---|---|---|---|---|---|---|
| Acierno et al., 2003 | RCT | 15+ years old within 72 hours of reporting rape (N = 226) | Emergency Department; United States | Video intervention (17 minutes) including medical prep and psychoeducation | Treatment as usual | 6-week: alcohol and marijuana use |
| Foa, et al., 1995 | Participants matched | 16+ years old with recent assault and PTSD diagnosis (N = 20) | Research and treatment center; Northeastern United States | Brief prevention program: 4 (2 hour) weekly meetings | Assessment only | 2 months and 5.5 months post-assault: PSS-I, PSS-SR, SAI, BDI |
| Foa et al., 2006 | RCT | Women with recent SA meeting DSM-IV symptom criteria for PTSD (not duration) (N = 90) | Research and treatment center; Northeastern United States | Brief cognitive behavioral intervention: 4 (2 hour) weekly meetings | Assessment only; Supportive counseling | Post-treatment, 2-, 3-, 6-, 9-, and 12- month: PSS-I, PSS-SR, BDI, BAI, ETO (Foa, Rothbaum, Riggs, & Murdock, 1991) |
| Frank et al., 1988 | RCT | Treatment seeking women experiencing recent SA (N = 84) | Research and treatment center; Northeastern United States | Systematic desensitization (14-session) or cognitive behavior therapy (14-session) | Non-victimized control group | Post-treatment: BDI, STAI, Fear Survey Schedule; Feelings of Inadequacy Scale (Church, Truss, & Velicer, 1980); SAS-II |
| Gilmore et al., 2019a | Usability and qualitative analysis | Adult women experiencing recent SA seeking SAMFE care (n = 13) and community providers (n = 25) | SAMFE centers; Southeastern United States | mHealth intervention focused on alcohol and substance use; suicide prevention; PTSD and depression; coping skills, physical health; referral to community resources | None | Post-assault PHQ-2 (Löwe, Kroenke, & Gräfe, 2005); PCL-5; AUDIT-C (Saunders, Aasland, Babor, De la Fuente, & Grant, 1993) |
| Gilmore et al., 2019b | RCT | Adolescent and adult women experiencing recent SA presenting for SAMFE care (N = 154) | SAMFE centers; Midwestern United Sites | Video intervention (9 or 18 minutes) including psychoeducation only (9 minute) or medical prep and psychoeducation (18 minutes); Video intervention (9 or 18 minutes) providing relaxation techniques only (e.g., diaphragm breathing) or medical prep and relaxation techniques (18 minutes) | Treatment as usual | 1.5-month: Prescription opioid misuse and non-medical use of prescription medication |
| Gilmore et al., in press | RCT | Women experiencing recent SA (age 15+) receiving SAMFE care (N = 233) | SAMFE centers; Midwestern United States | Video intervention (9 or 18 minutes) including psychoeducation only (9 minute) or medical prep and psychoeducation (18 minutes); Video intervention (9 or 18 minutes) providing relaxation techniques only (e.g., diaphragm breathing) or medical prep and relaxation techniques (18 minutes) | Treatment as usual | 1.5-, 3-, and 6-month: PDS, Perceived Control over Stressful Events Scale (Frazier et al., 2011) |
| Hassija & Gray, 2011 | Case series | Women referred from rape crisis center (N = 15) | Telehealth rural clinic; Western United States | Prolonged exposure or cognitive processing therapy (avg. 13 sessions) | None | Post-treatment: PCL, CES-D |
| Miller et al., 2015 | RCT | Adult women experiencing recent SA presenting for SAMFE care (N = 164) | SAMFE centers; United States | Video intervention (9 minutes) including psychoeducation only | Treatment as usual | 2-week & 2-month: PSS-SR, STAI-S, SUDs |
| Nixon et al., 2016 | RCT | Adult women experiencing past month SA with Acute Stress Disorder (N = 47) | Rape crisis center; United States | Cognitive processing therapy (6 sessions) | Treatment as usual (6 sessions) | 3-, 6-, and 12-month CAPS and BDI |
| Resnick et al., 1999 | Psuedo-randomized | Adult women experiencing recent SA presenting to emergency department within 72 hours post-assault (N = 48) | Emergency department; United States | Video intervention (17 minutes) including medical prep and psychoeducation | Treatment as usual | Post-treatment: SUDS, BAI 6-week: PSS-SR, BAI |
| Resnick et al., 2005 | RCT | 15+ years old girls and women experiencing recent SA presenting for SAMFE care (N = 205) | Emergency department; United States | Video intervention (17 minutes) including medical prep and psychoeducation | Treatment as usual | Post-treatment: SUDS, BAI 6-week: PSS-SR, BDI, PILL, BAI, assessment of alcohol and drug use |
| Resnick et al., 2007 | Randomized with dismantling conditions added half-way through trial | 14+ years old girls and women experiencing recent SA presenting for SAMFE care (N = 406) | Emergency department; Southeastern United States | Video interventions (17 mins) including medical prep and psychoeducation; medical prep only; psychoeducation only | Treatment as usual | Targeted follow-ups for 6 weeks and 6 months with considerable timing variability; Reported marijuana use outcomes |
| Rothbaum et al., 2012 | RCT | Individuals presenting to the Emergency Department meeting DSM-IV PTSD criterion A (N = 137) | Emergency department; Southeastern United States | Modified prolonged exposure: 3 (1hr) weekly sessions | Assessment only | 4-week: PSS-I, BDI, PDS 12-week: PSS-I |
| Tarquinio et al., 2012 | Uncontrolled trial | Women within 24–72 hours after first-time sexual assault (N = 17) | Research center; France | Newly developed eye movement desensitization and reprocessing (EMDR) urgent/emergency intervention (URG-EMDR) | None | 4-week and 6-month; IES (Horowitz, Wilner, & Alvarez, 1979); measures of sexuality; SUDS during treatment |
| Walsh et al., 2017 | RCT | Women experiencing recent SA (age 15+) receiving SAMFE care (N = 233) | SAMFE centers; Midwestern United States | Video intervention (9 or 18 minutes) including psychoeducation only (9 minute) or medical prep and psychoeducation (18 minutes); Video intervention (9 or 18 minutes) providing relaxation techniques only (e.g., diaphragm breathing) or medical prep and relaxation techniques (18 minutes) | Treatment as usual | Pre- and post-exam: PANAS-NA (Watson, Clark, & Tellegen, 1988); 1.5-, 3-, and 6-month: AUDIT, self-reported marijuana use, DAST (Skinner, 1982) |
| Zohar et al., 2018 | RCT | Adults with past-month trauma and reporting >2 DSM-IV criteria for acute stress disorder (N = 353) | Medical center and home-based treatment; Israel and South Africa | Escitalopram (titrated 10mg-20mg/day) up to 24 weeks | Placebo | Post-treatment: CAPS, PSS-SR, PSQI, MADRAS, VAS depression, VAS anxiety, CGI |
Note. BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; CAPS = Clinician-Administered-PTSD Scale; CES-D = Center for Epidemiological Studies-Depression Scale; CGI = Clinical Global Impression; DAST = Drug Abuse Screening Test; DSM-IV = Diagnostic and Statistical Manual – 4th Edition; ETO = Expectancy of Therapeutic Outcome; IES = Impact of Events Scale; MADRAS = Montgomery-Asberg Depression Rating Scale; PANAS-NA = Positive and Negative Affect Schedule – Negative Affect subscale; PCL = PTSD Checklist; PDS = Posttraumatic Diagnostic Scale; PILL = Pennebaker Inventory of Limbic Languidness; PSS-I = PTSD Symptom Scale-Interview; PSS-SR = PTSD Symptom Scale-Self Report; PSQI = Pittsburgh Sleep Quality Index; PTSD = Posttraumatic Stress Disorder; RCT = Randomized Controlled Trial; SAI = Standardized Assault Interview; SAS-II = Social Adjustment Scale II; SAMFE = Sexual assault medical and forensic exam; STAI = State Trait Anxiety Inventory; SUDS = Subjective Units of Discomfort Scales; VAS = Visual Analogue Scale. Note that measures not cited in-text are cited in their first occurrence in the table.
Footnotes
Declarations of interest: none.
Data Availability Statement: Data available upon reasonable request.
References
- Acierno R, Resnick HS, Flood A, & Holmes M (2003). An acute post-rape intervention to prevent substance use and abuse. Addictive behaviors, 28(9), 1701–1715. [DOI] [PubMed] [Google Scholar]
- Agorastos A, Marmar CR, & Otte C (2011). Immediate and early behavioral interventions for the prevention of acute and posttraumatic stress disorder. Current Opinions in Psychiatry, 24(6), 526–532. doi: 10.1097/YCO.0b013e32834cdde2 [DOI] [PubMed] [Google Scholar]
- Amos T, Stein DJ, & Ipser JC (2014). Pharmacological interventions for preventing post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Broman-Fulks J, Zinzow H, Ruggiero KJ, & Cercone J (2009). Internet-based interventions for traumatic stress-related mental health problems: a review and suggestion for future research. Clinical psychology review, 29(5), 410–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT (1972). Depression: Causes and Treatment. Philadelphia: University of Pennsylvania Press. [Google Scholar]
- Beck AT, & Steer RA (1993). Beck Anxiety Inventory Manual. San Antonio, TX: Harcourt Brace and Company. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. [Google Scholar]
- Benazzi F (1999). Severity gradation of the Montgomery Asberg Depression Rating Scale (MADRAS) in outpatients. Journal of Psychiatry and Neuroscience, 24(1), 51. [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein HR (2009). Introduction to Meta-Analysis. Chichester, West Sussex, UK: John Wiley & Sons, Ltd. [Google Scholar]
- Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, … Wang W (2013). Methods for synthesizing findings on moderation effects across multiple randomized trials. Prevention Science, 14(2), 144–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell R, & Adams AE (2009). Why do rape survivors volunteer for face-to-face interviews? A meta-study of victims’ reasons for and concerns about research participation. Journal of Interpersonal Violence, 24(3), 395–405. [DOI] [PubMed] [Google Scholar]
- Church MA, Truss CV, & Velicer WF (1980). Structure of the Janis-Field Feelings of Inadequacy Scale. Perceptual and Motor Skills. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, & Laird N (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7(3), 177–188. doi: 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and Fill: A Simple Funnel-Plot–Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics, 56(2), 455–463. doi: 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical psychology review, 56(65–81). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, & Schumacher JA (2018). Preventing posttraumatic stress related to sexual assault through early intervention: A systematic review. Trauma, Violence, & Abuse, 19(4), 459–472. doi: 10.1177/1524838016669518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, & Phillips AN (1997). Meta-analysis: principles and procedures. BMJ, 315(7121), 1533–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, & Perry K (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological assessment, 9(4), 445–451. [Google Scholar]
- Foa EB, Hearst-Ikeda D, & Perry KJ (1995). Evaluation of a brief cognitive-behavioral program for the prevention of chronic PTSD in recent assault victims. Journal of Consulting and Clinical Psychology, 63(6), 948. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, & Murdock TB (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59, 715–723. [DOI] [PubMed] [Google Scholar]
- Foa EB, & Tolin DF (2000). Comparison of the PTSD symptom scale–interview version and the clinician‐administered PTSD scale. Journal of Traumatic Stress, 13(2), 181–191. [DOI] [PubMed] [Google Scholar]
- Foa EB, Zoellner LA, & Feeny NC (2006). An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress, 19(1), 29–43. [DOI] [PubMed] [Google Scholar]
- Frank E, Anderson B, Stewart BD, Dancu C, Hughes C, & West D (1988). Efficacy of cognitive behavior therapy and systematic desensitization in the treatment of rape trauma. Behavior Therapy, 19(3), 403–420. [Google Scholar]
- Frazier P, Keenan N, Anders S, Perera S, Shallcross S, & Hintz S (2011). Perceived past, present, and future control and adjustment to stressful life events. Journal of Personality and Social Psychology, 100(4), 749. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical psychology review, 63, 41–55. doi: 10.1016/j.cpr.2018.05.008 [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Davidson TM, Leone RM, Wray LB, Oesterle DW, Hahn CK, … Acierno R (2019a). Usability Testing of a Mobile Health Intervention to Address Acute Care Needs after Sexual Assault. International Journal of Environmental Research and Public Health, 16(17), 3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Ledray L, Acierno R, Ruggiero KJ, … Resnick HS (2019b). Prescription Opioid Misuse After a Recent Sexual Assault: A Randomized Clinical Trial of a Video Intervention. The American Journal on Addictions, 28(5), 376–381. doi: 10.1111/ajad.12922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore AK, Walsh K, Frazier P, Meredith L, Ledray L, Davis J, … Resnick HS (in press). Post-sexual assault mental health: A randomized clinical trial of a video-based intervention. Journal of Interpersonal Violence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guay S, Beaulieu-Prévost D, Sader J, & Marchand A (2019). A Systematic Literature Review of Early Posttraumatic Interventions for Victims of Violent Crime. Aggression and Violent Behavior, 46, 15–24. doi: 10.1016/j.avb.2019.01.004 [DOI] [Google Scholar]
- Guy W (1976). ECDEU assessment manual for psychopharmacology. US Department of Health, and Welfare, 534–537. [Google Scholar]
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, & Schünemann HJ (2008). GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 336(7650), 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haidich A-B (2010). Meta-analysis in medical research. Hippokratia, 14(Suppl 1), 29. [PMC free article] [PubMed] [Google Scholar]
- Hassija C, & Gray MJ (2011). The effectiveness and feasibility of videoconferencing technology to provide evidence-based treatment to rural domestic violence and sexual assault populations. Telemedicine and e-Health, 17(4), 309–315. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, & Alvarez W (1979). Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. [DOI] [PubMed] [Google Scholar]
- IntHout J, Ioannidis JPA, & Borm GF (2014). The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Medical Research Methodology, 14(1), 25. doi: 10.1186/1471-2288-14-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearns MC, Ressler KJ, Zatzick D, & Rothbaum BO (2012). Early Interventions for PTSD: a Review. Depression and anxiety, 29(10), 833–842. doi: 10.1002/da.21997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, & Gräfe K (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research, 58(2), 163–171. [DOI] [PubMed] [Google Scholar]
- McMahon S, & Baker K (2011). Changing Perceptions of Sexual Violence Over Time. VAWnet, 1–16. doi:10.1.1.229.909 [Google Scholar]
- Miller KE, Cranston CC, Davis JL, Newman E, & Resnick H (2015). Psychological outcomes after a sexual assault video intervention: A randomized trial. Journal of Forensic Nursing, 11(3), 129–136. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group a. t. P. (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Annals of Internal Medicine, 151(4), 264–269. doi: 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- National Institute for Mental Health. (2015). Strategic Plan for Research. Retrieved from Bethesda, MD: https://www.nimh.nih.gov/about/strategic-planning-reports/index.shtml
- Nixon RD, Best T, Wilksch SR, Angelakis S, Beatty LJ, & Weber N (2016). Cognitive processing therapy for the treatment of acute stress disorder following sexual assault: a randomised effectiveness study. Behaviour Change, 33(4), 232–250. [Google Scholar]
- Nixon RDV, Sterk J, Pearce A, & Weber N (2017). A randomized trial of cognitive behavior therapy and cognitive therapy for children with posttraumatic stress disorder following single-incident trauma: Predictors and outcome at 1-year follow-up. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 471–478. doi: 10.1037/tra0000190 [DOI] [PubMed] [Google Scholar]
- Office on Violence Against Women. (2013). A National Protocol for Sexual Assault Medical Forensic Examinations. Retrieved from Washington DC: https://www.ncjrs.gov/pdffiles1/ovw/241903.pdf
- Ostacher MJ, & Cifu AS (2019). Management of Posttraumatic Stress Disorder. JAMA, 321(2), 200–201. doi: 10.1001/jama.2018.19290 [DOI] [PubMed] [Google Scholar]
- Peterson C, DeGue S, Florence C, & Lokey CN (2017). Lifetime economic burden of rape among US adults. American journal of preventive medicine, 52(6), 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Rauch SA, Kim HM, Powell C, Tuerk PW, Simon NM, Acierno R, & Stein MB (2019). Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: a randomized clinical trial. JAMA psychiatry, 76(2), 117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Holmes M, Kilpatrick DG, & Jager N (1999). Prevention of post-rape psychopathology: Preliminary findings of a controlled acute rape treatment study. Journal of Anxiety Disorders, 13(4), 359–370. [DOI] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Kilpatrick DG, & Holmes MM (2005). Description of an early intervention to prevent substance abuse and psychopathology in recent rape victims. Behavior Modification, 29(1), 156–188. [DOI] [PubMed] [Google Scholar]
- Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, … Kilpatrick D (2007). Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behaviour Research and Therapy, 45(10), 2432–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, & Walsh W (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5(3), 455–475. doi: 10.1002/jts.2490050309 [DOI] [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, … Houry D (2012). Early intervention may prevent the development of posttraumatic stress disorder: a randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry, 72(11), 957–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Short N, Sullivan J, Soward A, Bollen K, Liberzon I, Martin S, … McLean S (in press). Protocol for the first large-scale emergency care-based longitudinal cohort study of recovery after sexual assault: the Women’s Health Study. BMJ Open. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA (1982). Guide for using the drug abuse screening test (DAST). Toronto: Centre for Addiction and Mental Health. [Google Scholar]
- Smith HL, Summers BJ, Dillon KH, & Cougle JR (2016). Is worst-event trauma type related to PTSD symptom presentation and associated features? Journal of Anxiety Disorders, 38, 55–61. [DOI] [PubMed] [Google Scholar]
- Smith SG, Zhang X, Basile KC, Merrick MT, Wang J, Kresnow M, & Chen J (2018). The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief - Updated Release. Retrieved from Atlanta, GA: https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf [DOI] [PMC free article] [PubMed]
- Sobell LC, & Sobell MB (1992). Timeline follow-back Measuring alcohol consumption (pp. 41–72). Chicago, IL: Humana Press. [Google Scholar]
- Spielberger CD (2010). State-Trait anxiety inventory In Weiner IB & Craighead WE (Eds.), The Corsini encyclopedia of psychology. [Google Scholar]
- Suurmond R, van Rhee H, & Hak T (2017). Introduction, comparison, and validation of Meta-Essentials: A free and simple tool for meta-analysis. Research Synthesis Methods, 8(4), 537–553. doi: 10.1002/jrsm.1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarquinio C, Brennstuhl M, Reichenbach S, Rydberg J, & Tarquinio P (2012). Early treatment of rape victims: Presentation of an emergency EMDR protocol. Sexologies, 21(3), 113–121. [Google Scholar]
- Tarrier N, & Wykes T (2004). Is there evidence that cognitive behaviour therapy is an effective treatment for schizophrenia? A cautious or cautionary tale? Behaviour Research and Therapy, 42(12), 1377–1401. doi: 10.1016/j.brat.2004.06.020 [DOI] [PubMed] [Google Scholar]
- Veronen LJ, & Kilpatrick DG (1980). Self-reported fears of rape victims: A preliminary investigation. Behavior Modification, 4(3), 383–396. [Google Scholar]
- Vickerman KA, & Margolin GJ (2009). Rape treatment outcome research: empirical findings and state of the literature. Clinical psychology review, 29(5), 431–448. doi: 10.1016/j.cpr.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, Gilmore AK, Frazier P, Ledray L, Acierno R, Ruggiero KJ, … Resnick HS (2017). A randomized clinical trial examining the effect of video‐based prevention of alcohol and marijuana use among recent sexual assault victims. Alcoholism: clinical and experimental research, 41(12), 2163–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, & Keane T (1993). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician‐Administered PTSD Scale: A review of the first ten years of research. Depression and anxiety, 13(3), 132–156. [DOI] [PubMed] [Google Scholar]
- Wolpe J (1990). The practice of behavior therapy: Pergamon Press. [Google Scholar]
- Zohar J, Fostick L, Juven-Wetzler A, Kaplan Z, Shalev H, Schreiber G, … Seedat S (2018). Secondary Prevention of Chronic PTSD by Early and Short-Term Administration of Escitalopram: A Prospective Randomized, Placebo-Controlled, Double-Blind Trial. The Journal of clinical psychiatry, 79(2). [DOI] [PubMed] [Google Scholar]
- Zohar J, Sonnino R, Juven-Wetzler A, & Cohen H (2009). Can posttraumatic stress disorder be prevented. CNS Spectr, 14(1 Suppl 1), 44–51. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


