Abstract
Introduction
In breast cancer, local tumour control is thought to be optimised by administering higher local levels of cytotoxic chemotherapy, in particular doxorubicin. However, systemic administration of higher dosages of doxorubicin is hampered by its toxic side effects. In this study, we aim to increase doxorubicin deposition in the primary breast tumour without changing systemic doxorubicin concentration and thus without interfering with systemic efficacy and toxicity. This is to be achieved by combining Lyso-Thermosensitive Liposomal Doxorubicin (LTLD, ThermoDox, Celsion Corporation, Lawrenceville, NJ, USA) with mild local hyperthermia, induced by Magnetic Resonance guided High Intensity Focused Ultrasound (MR-HIFU). When heated above 39.5°C, LTLD releases a high concentration of doxorubicin intravascularly within seconds. In the absence of hyperthermia, LTLD leads to a similar biodistribution and antitumour efficacy compared with conventional doxorubicin.
Methods and analysis
This is a single-arm phase I study in 12 chemotherapy-naïve patients with de novo stage IV HER2-negative breast cancer. Previous endocrine treatment is allowed. Study treatment consists of up to six cycles of LTLD at 21-day intervals, administered during MR-HIFU-induced hyperthermia to the primary tumour. We will aim for 60 min of hyperthermia at 40°C–42°C using a dedicated MR-HIFU breast system (Profound Medical, Mississauga, Canada). Afterwards, intravenous cyclophosphamide will be administered. Primary endpoints are safety, tolerability and feasibility. The secondary endpoint is efficacy, assessed by radiological response.
This approach could lead to optimal loco-regional control with less extensive or even no surgery, in de novo stage IV patients and in stage II/III patients allocated to receive neoadjuvant chemotherapy.
Ethics and dissemination
This study has obtained ethical approval by the Medical Research Ethics Committee Utrecht (Protocol NL67422.041.18, METC number 18-702). Informed consent will be obtained from all patients before study participation. Results will be published in an academic peer-reviewed journal.
Trial registration numbers
NCT03749850, EudraCT 2015-005582-23.
Keywords: oncology, breast tumours, interventional radiology, magnetic resonance imaging, ultrasound, chemotherapy
Strengths and limitations of this study.
This first in human clinical trial investigates the combination of Lyso-Thermosensitive Liposomal Doxorubicin and Magnetic Resonance guided High Intensity Focused Ultrasound (MR-HIFU)-induced hyperthermia in breast cancer patients.
A dedicated MR-HIFU breast system with real-time MR temperature feedback will be used for safe non-invasive local hyperthermia treatment of breast tumours.
Because the study population consists of patients with de novo stage IV breast cancer, both local and systemic response to the treatment can be monitored.
A survival benefit of treating the primary tumour in patients with metastatic breast cancer has not been proven, therefore study participants will participate altruistically in the interest of future patients.
This approach could lead to improved local control during palliative chemotherapy in de novo stage IV breast cancer or neoadjuvant chemotherapy in stage II/III disease, with less extensive or even no surgery.
Introduction
Both neoadjuvant and adjuvant chemotherapy of breast cancer aim to improve survival by eradicating microscopic distant metastases. In addition, neoadjuvant treatment offers the opportunity to observe the biological behaviour of the primary tumour and increase the likelihood of less extensive radical (breast conserving) surgery. Given the fact that pathological complete response (pCR) is achieved at best in 68% of patients,1 efforts should be focused on improving primary tumour response. This may be achieved by increasing the dose of chemotherapy at the site of the tumour. In preclinical data, a higher concentration of chemotherapy in the tumour is correlated with increased tumour response, in particular for doxorubicin, one of the most frequently applied cytostatics in breast cancer treatment.2–4 Clinically, this was confirmed by studies using other chemotherapeutics, i.e. 5-fluorouracil and docetaxel. Higher tumour uptake of radio-active labelled 5-fluorouracil or docetaxel chemotherapy on positron emission tomography (PET) was shown to correlate, respectively, with longer survival in patients with liver metastasis of colorectal carcinoma5 and with better tumour response in lung cancer patients.6 In a study comparing different dose schedules of the adjuvant AC regimen, the highest dosages (60 mg/m2 doxorubicin and 600 mg/m2 cyclophosphamide) were most effective, and this is currently the standard of care.7 However, the administration of higher doses of doxorubicin is hampered by its systemic side effects. A randomised study evaluating even higher doxorubicin dosages (60 mg/m2 vs 75 mg/m2 and 90 mg/m2) did not find a difference in disease-free or overall survival. However, the higher dose levels did lead to significantly more dose reductions and delays, which could explain why the efficacy did not increase further.8 In the i-GO study, we aim to increase doxorubicin levels in the primary tumour, without interfering with systemic efficacy and toxicity, by combining Lyso-Thermosensitive Liposomal Doxorubicin (LTLD, ThermoDox; Celsion Corporation, Lawrenceville, NJ, USA) with mild local hyperthermia, induced by Magnetic Resonance guided High Intensity Focused Ultrasound (MR-HIFU). This will be followed by the intravenous administration of a second cytostatic agent, cyclophosphamide. The combined administration of doxorubicin and cyclophosphamide (AC) is a well-known regimen in the standard of care treatment in both the (neo)adjuvant setting as in the treatment of metastatic breast cancer.
The i-GO study will be a phase I feasibility study in stage IV breast cancer patients who present with distant metastases and a primary tumour in situ (de novo stage IV patients). Several studies have suggested that by obtaining loco-regional control in metastatic breast cancer, overall survival in advanced disease would be improved.9–11 However, randomised controlled trials have contradicted this.12 13 A recent presentation at ASCO 202014 confirmed that local treatment in addition to systemic therapy did not improve survival. As such, besides a personal preference of the patient and the possibility of preventing local morbidity, study participation will not have a benefit compared with the standard of care. However, based on pharmacokinetic studies (details outlined in online supplemental materials 1), we do expect at least an equally effective treatment. Study participants will participate altruistically in the interest of future patients in the neoadjuvant setting. In the future, the combination of LTLD, MR-HIFU hyperthermia and cyclophosphamide may lead to improved local control during neoadjuvant chemotherapy in stage II/III disease, with less extensive or even no surgery.
bmjopen-2020-040162supp001.pdf (1.6MB, pdf)
Lyso-thermosensitive liposomal doxorubicin
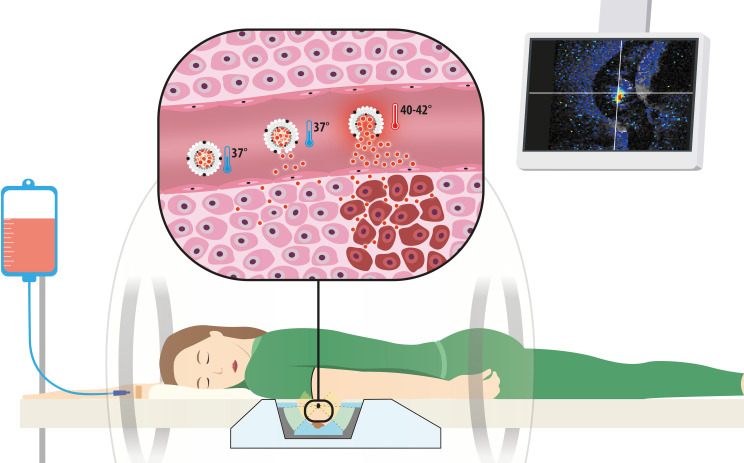
LTLD is a temperature-sensitive liposomal encapsulation of doxorubicin. Doxorubicin is a cytotoxic (chemotherapy) agent that is approved and frequently used for the treatment of a wide range of cancers, including breast cancer. When heated to 40°C–42°C, LTLD releases the encapsulated doxorubicin intravascularly within seconds15–17 (figure 1). In small animal tumour models, LTLD combined with hyperthermia results in a 3–25 fold higher tumour concentration than conventional doxorubicin2 18–22 and increased antitumour efficacy.2 16 18 In the absence of hyperthermia, doxorubicin leaks slowly from the liposome, and after 2 hours all of the doxorubicin is released.15 Furthermore, LTLD without hyperthermia leads to a similar biodistribution19 20 and antitumour efficacy16 18 compared with conventional doxorubicin.
Figure 1.
The concept of LTLD combined with MR-HIFU hyperthermia for local drug delivery in the primary breast tumour. The patient is lying in prone position on the dedicated MR-HIFU breast system under procedural sedation and analgesia, with the breast hanging in the water-filled cup. HIFU-induced hyperthermia is administered to the tumour for 60 min. Real-time MR thermometry (screen on the right) allows for precise control of the target temperature of 40°C–42°C in the tumour. After intravenous infusion, LTLD circulates through the vasculature and releases a small amount of doxorubicin at 37°C. However, when LTLD reaches the heated tumour, it releases a high amount of doxorubicin intravascularly within seconds. We hypothesise that the combination of LTLD and MR-HIFU hyperthermia will increase the tumour concentration of doxorubicin without interfering with systemic treatment efficacy and toxicity. LTLD, lyso-thermosensitive liposomal doxorubicin; MR-HIFU, magnetic resonance guided high intensity focused ultrasound.
Magnetic resonance-guided high intensity focused ultrasound
MR-HIFU is a truly non-invasive treatment modality that combines MRI and high intensity focused ultrasound to perform image-guided thermal tissue ablation (55°C–70°C)23–25 or mild local hyperthermia (40°C–43°C).26–28 Unlike other heating methods, using microwaves, radiofrequency or non-focused ultrasound, HIFU allows for non-invasive localised heating of deep-seated tumours.29 In addition to treatment planning based on anatomical MRI, MR-guidance can provide temperature feedback and control during hyperthermia treatment, through real-time MR thermometry. For this study, we will use a dedicated MR-HIFU breast system: the Sonalleve MR-HIFU breast tumour therapy system (hereafter referred to as ‘MR-HIFU breast system’, Profound Medical, Mississauga, Canada), integrated with a clinical 1.5 Tesla MR scanner (Achieva, Philips Healthcare, Best, The Netherlands). This system has a lateral sonication approach, which enables specific heating of the breast tumour, while reducing the risk of heating the skin or other organs to a minimum.30 A phase I study in our hospital with MR-HIFU ablation of breast tumours showed that the MR-HIFU breast system allows for safe, accurate and precise thermal ablation.31 32
Previous clinical studies
This will be the first-in-human study to evaluate LTLD with MR-HIFU hyperthermia in breast cancer patients. LTLD has been studied previously in combination with superficial hyperthermia in patients with chest wall recurrences of breast cancer.33 This phase I/II study showed that LTLD at 40 mg/m2 with superficial hyperthermia was safe and the 48% overall response (14/29, 95% CI 30% to 66%) was promising in this heavily pretreated population. A large randomised phase III study in 701 patients with hepatocellular carcinoma compared LTLD at 50 mg/m2 with radiofrequency ablation (RFA) to RFA alone (the HEAT study).34 35 In that study, the primary endpoint of 33% improvement in progression free survival was not met. However, a post hoc analysis in the subgroup of 285 patients with solitary lesions that were treated with ≥45 min of RFA showed a significant overall survival benefit for the combination treatment (HR for overall survival 0.63 (95% CI 0.41 to 0.96; p<0.05), in favour of RFA+LTLD with ≥45 min heating). Systemic adverse events increased in the RFA+LTLD arm (83% vs 35% with RFA alone) as expected, with a similar profile to that of conventional doxorubicin.35
Furthermore, the combination of LTLD and ultrasound guided HIFU hyperthermia has been evaluated in a phase I proof-of-concept study in 10 patients with incurable primary or metastatic liver tumours (the TARDOX study).36 37 Adverse events did not differ from those associated with doxorubicin alone and in the group of patients who underwent invasive thermometry, sufficient mean tumour temperatures were measured. In seven out of the 10 patients, the intratumoural doxorubicin concentration doubled after HIFU, although a within-patient comparison was not possible for all patients. We aim to take advantage of the same principle to treat the primary tumour in patients presenting with metastatic breast cancer. Monitoring the treatment by MR thermometry may further enhance safety, efficacy and feasibility. Using multiple cycles of LTLD+MR HIFU hyperthermia is expected to increase treatment efficacy and mimics the standard of care treatment.
Methods and analysis
This single-arm phase I feasibility study aims to determine the safety, tolerability and feasibility of the combination of LTLD, MR-HIFU-induced mild local hyperthermia and cyclophosphamide, for the enhanced local treatment of the primary tumour in patients presenting with metastatic breast cancer. All eligible participants will receive up to six cycles of LTLD at 21-day intervals, administered during MR-HIFU-induced hyperthermia to the primary tumour and cyclophosphamide administered afterwards.
Patient population
We will include six or 12 adult female patients with de novo stage IV (distant metastases at the time of diagnosis, with the primary tumour in situ) HER2-negative breast cancer, who have not received previous chemotherapy for their disease. Previous endocrine treatment in those with hormone-receptor positive disease is allowed. The small samples size was chosen because this is the first study evaluating the combination of MR-HIFU hyperthermia, LTLD and cyclophosphamide. No formal sample size calculation was performed. Potentially eligible patients will be referred to the department of Medical Oncology at the University Medical Center Utrecht, The Netherlands. In order to achieving adequate participant enrolment, medical oncologists in hospitals in the Netherlands will be asked to refer potentially eligible and interested patients.
Inclusion criteria
Patients must meet all of the following inclusion criteria:
Histologically confirmed adenocarcinoma of the breast and planned for palliative chemotherapy with doxorubicin and cyclophosphamide.
Biopsy-proven stage T1-2AnyNM1 at diagnosis of breast cancer.
Measurable disease according to either RECIST V.1.1 or PERCIST V.1.0 at baseline.
Non-pregnant, non-lactating female at least 18 years of age. If the patient is of childbearing age, she must have a negative serum pregnancy test prior to enrolment and must agree to practice an acceptable form of birth control while on study.
The tumour is located within the reach of the HIFU beam (based on pretreatment dynamic contrast-enhanced (DCE-)MRI findings).
The distance of the tumour from the skin, nipple and pectoral wall is at least 1.0 cm (based on pretreatment DCE-MRI findings).
The target breast is expected to fit in the cup of the MR-HIFU breast system (based on pretreatment MRI findings).
The patient is able to provide written informed consent and willing to comply with protocol requirements.
Exclusion criteria
Patients will be excluded if any of the following conditions are observed:
HER2-positive disease or classic invasive lobular carcinoma.
A treatment plan with curative intent is available.
Any prior chemotherapy treatment for invasive breast cancer (previous antihormonal therapy is allowed).
Any prior therapy with anthracyclines.
The patient weighs ≥90 kg (restriction of the HIFU table top).
Any concomitant malignancy or previous malignancy in the last 5 years, except basal cell or squamous cell cancer of the skin or in situ carcinoma of the cervix. Subjects with a prior contralateral breast malignancy more than 5 years ago can be included if they did not receive any chemotherapy.
Any previous malignancy in the unilateral breast (even if more than 5 years ago).
Prior sensitivity (including rash, dyspnoea, wheezing, urticarial or other symptoms) attributed to any liposomal-encapsulated drug.
-
Baseline laboratory values:
Absolute neutrophil count <1.5 x 10∧9/L.
Platelets <75 x 10∧9/L.
Haemoglobin <5.6 mmol/L (transfusion is allowed).
Total bilirubin >1.5 times upper limit of normal.
-
Alanine transaminase and aspartate transaminase
>2.5 times upper limit of normal.
>5 times upper limit of normal in case of liver metastases.
Estimated glomerular filtration rate <30 mL/min/1.73 m2.
WHO performance status >2.
Left ventricular Ejection fraction (LVEF)<50% (validated by baseline scan).
History of: acute coronary syndrome in the last year, cerebral vascular accident in the last year, abnormal cardiac stress testing within the last 6 months, symptomatic coronary artery disease, uncontrolled hypertension or cardiomyopathy, cardiac valvular surgery or open-heart surgery in the last year or known structural heart disease.
Any condition which may interfere with the hyperthermia portion of the trial such as: functioning cardiac pacemaker; metal plates, rods or prosthesis of the chest wall; breast prosthesis in the treated breast; severe numbness and/or tingling of the chest wall or breast; skin grafts and/or flaps on the breast or chest wall; scar tissue or surgical clips in the HIFU beam path.
Active infection.
Body temperature >38.0°C on the day of an MR-HIFU treatment.
Concurrent use of any of the following prohibited medications within a reasonable wash-out time: protease inhibitors, cyclosporine, carbamazepine, phenytoin, valproic acid, paclitaxel, trastuzumab and other liposomal drugs (Abelect, Ambisome, Nyotran) or lipid-complexed drugs. Caution will be exercised with medications, dietary components and herbal supplements that affect CYP2A4, CYP2D6 or P-gp or have been described to interact with doxorubicin in other ways.
Contraindications to MR imaging (e.g. pacemaker in situ, severe claustrophobia, metal implants incompatible with the MRI-scan, body size incompatible with MR bore).
Contraindications to gadolinium-based contrast agents and the tumour is not sufficiently visible on MRI without contrast (including prior allergic reaction to gadolinium-based contrast agent, and/or renal failure).
Contraindications to sedation and analgesia with propofol and remifentanil, including history of chronic obstructive pulmonary disease that results in the inability to perform a physical activity corresponding with a metabolic equivalent (MET(57)) of 4; dependence on artificial ventilation at home; sleep apnoea or an American Society of Anaesthesiologists classification ≥4.
Inability to lie in prone position.
A medical or psychiatric condition or other circumstances which would significantly decrease the chances of understanding the informed consent process, obtaining reliable data, achieving study objectives or completing the study treatment and/or examinations.
Endpoints
Primary endpoints are safety, tolerability and feasibility. These will be evaluated by the following assessments.
Safety and tolerability:
Incidence and severity of adverse events and severe adverse events.
Incidence of dose limiting toxicity (DLT, systemic and loco-regional).
Necessity for dose adjustments, delay and early cessation.
Incidence and severity of postprocedural pain.
Patient reported tolerability (questionnaires).
Cardiotoxicity: LVEF measurement and ECG abnormalities.
Feasibility:
The number of cycles in which hyperthermia treatment was sufficient: at least 30 min at the target temperature of 40°C–42°C.
The number of completed cycles with MR-HIFU-induced hyperthermia, LTLD and cyclophosphamide.
Quality of MR thermometry data acquired during the MR-HIFU treatment.
Spatiotemporal temperature distribution in the tumour.
Total duration of the study procedures on a treatment day.
Secondary endpoints consist of efficacy parameters:
Assessment of distant radiological objective response rates.
Assessment of local radiological objective response rates.
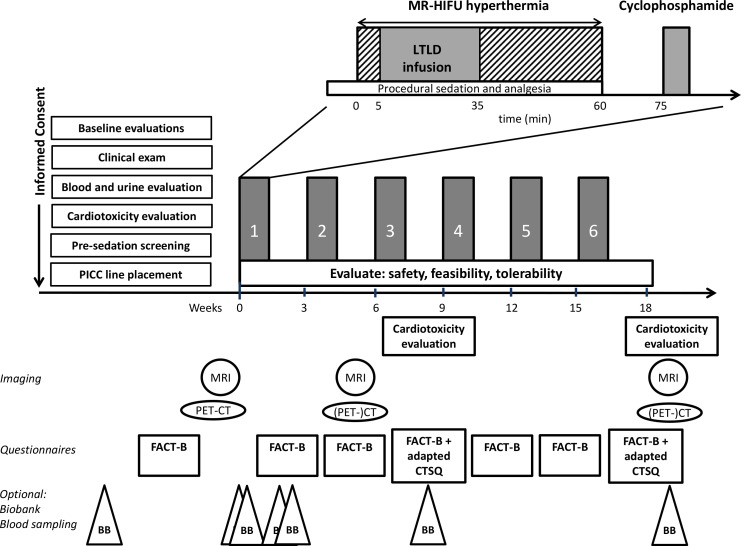
Study procedures
The study design (figure 2) was based on the AC regimen, a well-known chemotherapeutic regimen that consists of doxorubicin and cyclophosphamide. This regimen is used in the (neo)adjuvant setting as well as in the first-line chemotherapy treatment of metastatic breast cancer. Standard of care for our study population consists of six cycles at 21-day intervals. In this study, we will replace doxorubicin in this regimen with the combination of LTLD and MR-HIFU-induced hyperthermia.
Figure 2.
Study procedures. The standard of care palliative AC regimen consists of six cycles of doxorubicin and cyclophosphamide at 21-day intervals. In this study, we will replace doxorubicin with the combination of LTLD and MR-HIFU-induced hyperthermia, in up to six cycles. After informed consent, the baseline procedures will be performed as mentioned. During the cycles, the primary endpoints of safety (adverse events), feasibility and tolerability will be monitored, including cardiotoxicity evaluation and questionnaires on specified time points as indicated in the bottom of the figure. Imaging to determine local (MRI) and systemic ((PET/)CT) response will be performed at baseline, after cycles 2 and 6. Optionally, the patient can consent to additional blood sampling for future research, which will be stored in the Biobank. CTSQ, Cancer Therapy Satisfaction Questionnaire; FACT-B, Functional Assessment of Cancer Therapy-Breast; LTLD, lyso-thermosensitive liposomal doxorubicin; MR-HIFU, magnetic resonance guided high intensity focused ultrasound; PET, positron emission tomography; PICC, peripherally inserted central catheter.
All participants will receive procedural sedation and analgesia with propofol and remifentanil to limit patient movement during the treatment and to establish a regular breathing pattern that will facilitate respiratory gated MR thermometry.38 To prevent any hypersensitivity reactions to LTLD, the participants will also receive a premedication regimen of steroids, H1-histamine and H2-histamine antagonists. Antiemetics will be administered according to standard-of-care hospital guidelines for the AC regimen.
MR-HIFU hyperthermia will be performed on the MR-HIFU breast system, with the patient in prone position. We will aim for 60 min of hyperthermia at 40°C–42°C to the breast tumour, in four blocks of 15 min. After each block, the MR thermometry is restarted to minimise the possible influence of magnetic field drift or patient displacement. When MR thermometry indicates that the target temperature is reached, 50 mg/m2 of LTLD will be administered intravenously over 30 min, via a peripherally inserted central catheter (PICC), while the patient is on the MR-HIFU breast system. Temperature will be monitored by respiratory navigator-gated MR thermometry, using the proton resonance frequency shift method.39 40 In case the target temperature is not reached, conventional doxorubicin (60 mg/m2) will be administered instead of LTLD. Shortly after MR-HIFU, 600 mg/m2 of cyclophosphamide will be administered intravenously according to standard of care in the AC regimen.
Participants will receive up to six treatment cycles. Feasibility will be evaluated after each MR-HIFU treatment and during the course of the cycles. Safety and tolerability will be assessed 3 hours after MR-HIFU treatment, during telephone contact on day +1 and +7 and during a hospital visit on day +14 and +21 of each cycle, by monitoring of adverse events, laboratory measurements and evaluation of pain. Cardiotoxicity evaluations (LVEF and ECG) will be performed at baseline, after cycles 3 and 6. The participants will be asked to fill out the Dutch version of the Functional Assessment of Cancer Therapy-Breast (V.4, FACIT)41 at baseline and after each treatment cycle, combined with a selection of questions adapted from the Dutch version of the Cancer Therapy Satisfaction Questionnaire (Pfizer 2007, modified with permission from Pfizer)42 43 in cycles 3 and 6. Before starting the next cycle, any toxicities will be evaluated and if necessary, dose reductions will be made. DLT will be categorised in systemic or loco-regional toxicity (table 1). Thus, we aim to distinguish systemic chemotherapy effects from local effects of MR-HIFU hyperthermia and/or the high local doxorubicin concentration. Planned dose adjustments for these categories have been established (online supplemental materials 2). In case of a systemic DLT, the LTLD dosage will be decreased, while for loco-regional DLT, the duration of hyperthermia will be decreased. Cyclophosphamide dose will not be reduced. No dose increases will be performed. Depending on the severity and nature of the toxicity, study treatment can be delayed or even ceased. In case of solely loco-regional DLT, technical issues or other feasibility issues that restrict the use of MR-HIFU treatment, the participant will receive the standard of care AC regimen. If hyperthermia is insufficient (i.e. the target temperature of 40°C–42°C is not reached or was only maintained for less than 30 min) in two separate cycles, the treatment is not considered feasible for that patient and study participation will end.
Table 1.
Definitions of dose limiting toxicity
| Dose limiting systemic toxicity | |
| A | Hematologic DLT defined as grade 3 anaemia, grade 4 thrombocytopenia, febrile neutropenia or grade 4 neutropenia ≥7 days in duration. |
| B |
Non-hematologic DLT (non-loco-regional) defined as grade 3 or greater toxicity with the exceptions of alopecia, fatigue, nausea or vomiting and loco-regional effects. Including cardiotoxicity DLT, defined as follows:
|
| Dose limiting loco-regional toxicity | |
| C | Loco-regional DLT defined as postprocedural effects (e.g. pain or skin effects) on the treated breast warranting dose adjustment or delay. |
DLT, dose limiting toxicity; LVEF, left ventricular ejection fraction.
For the secondary endpoint of efficacy, MRI of the breast will be performed using a 3 Tesla MRI scanner with a dedicated breast coil, at baseline and after cycles 2 and 6 to determine local radiological objective response. In addition, MRI of the breast will be performed during each MR-HIFU treatment. However, the receiver coil in the MR-HIFU breast system is not suited for clinical imaging. In case a complete radiological response of the breast tumour is obtained after less than 6 cycles, the patient will continue with the conventional AC regimen. 18F -fluorodeoxyglucose positron emission tomography combined with CT (PET/CT) of the thorax and abdomen will be performed at baseline and CT or PET/CT after cycles 2 and 6 to determine the distant objective response according to RECIST V.1.144 or PERCIST V.1.0.45 PET/CT will be performed for response evaluation in patients with only PERCIST-measurable disease, such as patients with only bone metastases. If a patient shows distant progression of disease, study participation will end and the patient will be treated according to the standard of care. Additional specific reasons for study withdrawal are DLT that warrants a delay in treatment administration for longer than 14 days or a recurrence of DLT after dose reduction of LTLD (online supplemental materials 2).
The participants will be followed for adverse events from the time of signing informed consent until the end of study visit after six cycles of chemotherapy. Afterwards, patients will receive standard of care treatment.
If the patient consents to the biobank study, additional blood samples will be taken from the PICC line at seven time points (figure 2) when the patient is already at the hospital. These blood samples will be collected in the UMC Utrecht Biobank for future research. Moreover, in case tissue samples of the breast tumour and/or metastases were obtained in standard care before inclusion or following study participation, we will ask for consent to perform additional analyses on these samples.
Concomitant care and prohibited interventions
All supportive measures consistent with optimal medical care will be employed, including transfusion of blood and blood products, and treatment with antibiotics, antiemetics, antidiarrheals and analgesics, as appropriate.
Certain concomitant medications, a number of herbal supplements, food stuffs and nutritions are restricted during the study (online supplemental materials 3). Patients cannot use creams, ointments or lotions on the breast on the MR-HIFU treatment day, to avoid additional risks during the procedure. Patients cannot use methods or treatments that increase the body temperature or skin temperature during the study period (e.g. sauna, hot-water baths, warmth massages), because this could result in increased release of doxorubicin in the warmed areas, possibly causing extra adverse events.
Interim analysis
An interim analysis of safety and efficacy will determine whether accrual will continue after six participants (online supplemental materials 4). Safety will be evaluated once the first six patients complete two treatment cycles. If safety is sufficiently proven or is deemed inadequate, the trial will end after six participants. Otherwise accrual will continue until 12 patients have been treated, if necessary after dose adjustments. All patients who have signed informed consent will be evaluated for the primary endpoints of safety, feasibility and tolerability. Patients who have been withdrawn from the study because MR-HIFU-induced hyperthermia was insufficient in two separate treatment cycles and who did not experience a DLT will be replaced by another participant for in the interim safety evaluation. If this happens to four patients, the study will be terminated, because of insufficient feasibility.
Systemic efficacy will be evaluated once the first six patients have received the CT scan after cycle 2. If four or more of the first six participants show distant disease progression at that time, the trial will be stopped, as this suggests that efficacy against disease outside the heated treatment field is inadequate. This early stopping rule was based on a phase III trial with liposomal doxorubicin in metastatic breast cancer46 where 77.5% of the subjects were free of disease progression at 2 months postrandomisation (the 95% CI of 2/6 patients does not contain 0.775).
An independent, qualified monitor will monitor the study procedures. An external Data Safety Monitoring Board (DSMB) will review accumulating safety data at regular intervals throughout the study, perform the interim safety and efficacy analyses and monitor trial data integrity (DSMB charter in online supplemental materials 5).
Data analysis
Descriptive statistics will be used to describe the incidence and severity of adverse events (National Cancer Institute Common Terminology Criteria for Adverse Events V.5.0), the patient reported outcomes in the questionnaires and feasibility parameters including the number of completed study treatment cycles, duration of study procedures and spatiotemporal temperature distribution during MR-HIFU treatment. For the secondary endpoint of efficacy, distant and local radiological objective response rates (RECIST V.1.1) will be described.
Discussion
This is the first clinical trial that investigates the combination of LTLD and MR-HIFU-induced hyperthermia in breast cancer. In a small number of patients, we will focus primarily on safety, tolerability and feasibility of this procedure. We hypothesise that the combination of LTLD and MR-HIFU hyperthermia leads to improved treatment of the primary tumour, without changing the systemic doxorubicin concentration and thus without interfering with systemic efficacy and toxicity. A future randomised study with a control group receiving the standard of care AC regimen would be needed to prove this. Including patients with de novo stage IV breast cancer provides the unique possibility to monitor both local and systemic disease simultaneously. While in this setting a survival benefit of treating the primary tumour has not been proven, the study treatment (if proven safe and feasible) could in the future improve outcomes in the neoadjuvant setting.
We aim to replace doxorubicin by LTLD plus MR-HIFU hyperthermia in all six cycles of the AC regimen, because we expect this to maximise the local treatment effect. In each cycle, the feasibility to achieve tumour hyperthermia at 40°C–42°C for 30 min will be verified with MR thermometry. If hyperthermia treatment is repeatedly insufficient, or if (after any number of cycles) radiological complete response is already obtained, patients will continue on the standard-of-care AC regimen. The number of MR-HIFU hyperthermia plus LTLD cycles that our patients are willing and able to complete could be less than six, which would be an important feasibility finding.
Our goal is to maintain an equivalent systemic efficacy compared with the standard-of-care AC regimen using 60 mg/m2 conventional doxorubicin. Pharmacokinetic studies showed that the area under the curve (AUC0-∞) of free/unencapsulated doxorubicin in plasma of patients receiving LTLD 50 mg/m2 with local hyperthermia or RFA33 47 48 was higher than the AUC0-∞ of conventional doxorubicin 60 mg/m2.49–51 To be able to compare the AUCs, we converted the AUC0-∞ of the metabolite doxorubicinol that was measured in the LTLD studies to the AUC0-∞ of doxorubicin52–54 (additional explanation in online supplemental materials 1). The 50 mg/m2 LTLD dose was also recommended for and well tolerated in the phase III trial in combination with RFA.35 Due to local toxicity, the recommended dose for LTLD combined with local superficial hyperthermia for chest wall recurrences was decreased to 40 mg/m2.47 In our study, local (skin) toxicity is not expected because a margin of at least 1.0 cm is preserved from the tumour to the skin, therefore the LTLD dose of 50 mg/m2 was chosen. Real-time MR thermometry and the lateral configuration of the MR-HIFU breast system will help mitigate this risk. If however local DLT do occur, the duration of hyperthermia will be decreased while maintaining the LTLD dosage to avoid decreasing systemic efficacy. We will only decrease LTLD dosage in case of systemic DLT. If despite these measures, systemic efficacy seems inadequate, the trial will be halted prematurely based on the interim analysis for efficacy.
Because this is a small phase I feasibility study, the results will only provide a rough indication of local efficacy based on radiological response. To diminish the burden on participants, we will not perform tissue biopsies or breast surgery and therefore cannot describe the number of pathological complete responses or measure the concentration of doxorubicin in the tumour. Proof-of-concept that hyperthermia increases the tumour doxorubicin concentration has already been established in the TARDOX study, although doxorubicin concentrations were not compared between heated and unheated tumours.
With this phase I clinical trial, we aim to show that LTLD combined with MR-HIFU-induced hyperthermia on a dedicated MR-HIFU breast system can safely replace doxorubicin in the AC regimen. We hypothesise that this combination will result in improved response of the primary tumour without compromising the systemic efficacy on metastatic sites or increasing systemic toxicity. If feasibility and tolerability are adequate, this approach could in the future lead to optimal loco-regional control with less extensive or even no surgery, in stage II or III breast cancer patients allocated to receive neoadjuvant chemotherapy. Finally, it could also be suitable for other doxorubicin sensitive tumour types that benefit from enhanced local treatment, such as soft tissue sarcoma.
Ethics and dissemination
This study has obtained ethical approval by the Medical Research Ethics Committee of the UMC Utrecht (METC Utrecht) on 29 May 2019 (Protocol NL67422.041.18, METC number 18-702). This paper is based on protocol version 6, dated 28 August 2020. Substantial protocol amendments will also be evaluated by METC Utrecht and communicated to relevant parties by the investigators. Informed consent will be obtained from all patients by an authorised representative of the Principal Investigator before study participation (informed consent form in online supplemental materials 6). The results of this study will be disseminated by publication in an academic peer-reviewed journal.
Roles and responsibilities
This is an investigator-driven single-centre clinical trial, with the UMC Utrecht as sponsor and trial site. The UMC Utrecht is responsible for the study design, data collection, data management, analysis, interpretation of data, writing and submission of the report for publication. The Principal Investigator will rapport (serious) adverse (device) events to the METC Utrecht, to the Central Committee on Research Involving Human Subjects (CCMO) and to Celsion Corporation and Profound Medical according to national guidelines. UMC Utrecht has liability insurance which provides cover for damage to research subjects through injury or death caused by the study. Celsion Corporation (manufacturer of the investigational medicinal product) and Profound Medical (manufacturer of the investigational medical device) will provide technical support during the trial and have provided input on the study protocol. Both manufacturers will be allowed to review and comment on draft publications prior to submission. The investigators at the UMC Utrecht will have ultimate authority over the publication. An external DSMB (two clinicians and one statistician) has been established and an independent qualified monitor (Julius Clinical) has been appointed to perform intensive monitoring.
Data management
The handling of personal data will comply with the general data protection regulation (in Dutch known as AVG). After informed consent is signed, each patient receives a unique subject number. A subject identification code list will be used to link the data to the subject. The key to this pseudonymisation code will be available only to the investigators and employees of the research team.
Research data that are relevant for the study will be collected by the investigators on electronical Case Report Forms (eCRFs) in Research Online, in compliance with the good clinical practice guidelines for electronic data collection. An audit trail will be available. The completed eCRFs will be reviewed, signed and dated by the Principal Investigator or Coinvestigator. Scans, results and registrations of medical imaging will be collected on the Research Imaging Architecture (RIA), which is secured by password-protection and stores pseudonymised images. Data from the MR-HIFU device such as log files and MR images obtained during the MR-HIFU treatment that cannot be stored on the RIA will be stored in a secured UMC Utrecht bulk-storage folder. Celsion and Profound will not receive any patient’s identifiable (personal) information. UMC Utrecht shall provide pseudonymised data regarding the occurrence and severity of adverse device effects to Profound Medical and regarding the occurrence and severity of adverse events to Celsion Corporation. This cannot be refused by the patient and is obligatory for study participation. If the patient consents (optional), additional pseudonymised data on the study treatment will also be provided to Profound Medical and Celsion Corporation. Research data will be stored for 15 years after the end of study. Biomaterial is stored in the Central biobank (blood) or at the UMC Utrecht pathology department (tissue samples).
Patient and public involvement
Patient experiences have been the starting point for the grant proposal to the Dutch Cancer Foundation and patients were involved in the design of the study and the choice of outcome measures. Patients will not be actively involved in recruitment or dissemination of study results, however information regarding the study can be found by individual patients on the UMC Utrecht website and clinicaltrials.gov.
Trial status
Patient recruitment was initiated on 10 March 2020. On the submission date of this article, no patients had been enrolled yet. Due to the COVID-19 outbreak, the study has been temporarily discontinued. Recruitment has resumed as of 7 October 2020.
Supplementary Material
Acknowledgments
We thank Roelien Kronemeijer of the trial bureau medical oncology and Heleen Klein Wolterink-Blok, research nurse medical oncology, for their work leading up to the Medical Research Ethics Committee approval of the study and the start of patient recruitment. We thank Professor Gert Storm for his work in the preceding HIFU-CHEM project that has contributed to the current project. We thank Christiaan van Kesteren for his help with the design of figure 1. We thank Celsion Corporation for their support relating the use and safety of ThermoDox and their input during the design of the study. Finally, we thank Profound Medical for their support relating the use and safety of the MR-HIFU breast system in their role as legal manufacturer of this investigational medical device.
Footnotes
Contributors: JSdeM, BBMS, MNGJAB, SCL, CTWM, EvanderW and RD were all involved in the design of the study and in writing the manuscript. PJvanD, HHBV and AJW critically reviewed the design of the study providing additional comments and suggestions.
Funding: This work was supported by the Dutch Cancer Foundation (project no. UU 2015-7891), Center for Translational Molecular Medicine (CTMM) in the projects VOLTAVALO (project no. 09P-106) and HIFU-chem (project no. 03O-301) and by 'Friends of the UMC Utrecht'.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.van Ramshorst MS, van der Voort A, van Werkhoven ED, et al. Neoadjuvant chemotherapy with or without anthracyclines in the presence of dual HER2 blockade for HER2-positive breast cancer (TRAIN-2): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 2018;19:1630–40. 10.1016/S1470-2045(18)30570-9 [DOI] [PubMed] [Google Scholar]
- 2.Ponce AM, Viglianti BL, Yu D, et al. Magnetic resonance imaging of temperature-sensitive liposome release: drug dose painting and antitumor effects. J Natl Cancer Inst 2007;99:53–63. 10.1093/jnci/djk005 [DOI] [PubMed] [Google Scholar]
- 3.Koechli OR, Sevin B-U, Perras JP, et al. Comparative chemosensitivity profiles in three human breast cancer cell lines with the ATP-cell viability assay. Oncology 1994;51:552–8. 10.1159/000227402 [DOI] [PubMed] [Google Scholar]
- 4.Besse HC, Barten-van Rijbroek AD, van der Wurff-Jacobs KMG, et al. Tumor drug distribution after local drug delivery by hyperthermia, in vivo. Cancers 2019;11. 10.3390/cancers11101512. [Epub ahead of print: 09 10 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moehler M, Dimitrakopoulou-Strauss A, Gutzler F, et al. 18F-Labeled fluorouracil positron emission tomography and the prognoses of colorectal carcinoma patients with metastases to the liver treated with 5-fluorouracil. Cancer 1998;83:245–53. [DOI] [PubMed] [Google Scholar]
- 6.van der Veldt AAM, Lubberink M, Mathijssen RHJ, et al. Toward prediction of efficacy of chemotherapy: a proof of concept study in lung cancer patients using [¹¹C]docetaxel and positron emission tomography. Clin Cancer Res 2013;19:4163–73. 10.1158/1078-0432.CCR-12-3779 [DOI] [PubMed] [Google Scholar]
- 7.Budman DR, Berry DA, Cirrincione CT, et al. Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. The cancer and leukemia group B. J Natl Cancer Inst 1998;90:1205–11. 10.1093/jnci/90.16.1205 [DOI] [PubMed] [Google Scholar]
- 8.Henderson IC, Berry DA, Demetri GD, et al. Improved outcomes from adding sequential paclitaxel but not from escalating doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol 2003;21:976–83. 10.1200/JCO.2003.02.063 [DOI] [PubMed] [Google Scholar]
- 9.Khan SA. Surgical management of de novo stage IV breast cancer. Semin Radiat Oncol 2016;26:79–86. 10.1016/j.semradonc.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 10.Headon H, Wazir U, Kasem A, et al. Surgical treatment of the primary tumour improves the overall survival in patients with metastatic breast cancer: a systematic review and meta-analysis. Mol Clin Oncol 2016;4:863–7. 10.3892/mco.2016.778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soran A, Ozmen V, Ozbas S, et al. The importance of primary surgery in patients with de novo stage IV breast cancer; finalizing the protocol MF07-01 randomized clinical trial. Poster P1-20-01 at San Antonio Breast Cancer Symposium 2019 2019. [Google Scholar]
- 12.Badwe R, Hawaldar R, Nair N, et al. Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol 2015;16:1380–8. 10.1016/S1470-2045(15)00135-7 [DOI] [PubMed] [Google Scholar]
- 13.Tsukioki T, Shien T, Doihara H. Effect of local surgery on outcomes of stage IV breast cancer. Transl Cancer Res 2020;9:5102–7. 10.21037/tcr.2020.01.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan SA, Zhao F, Solin LJ, et al. A randomized phase III trial of systemic therapy plus early local therapy versus systemic therapy alone in women with de novo stage IV breast cancer: a trial of the ECOG-ACRIN Research Group (E2108). J Clin Oncol 2020;38:LBA2. 10.1200/JCO.2020.38.18_suppl.LBA2 [DOI] [Google Scholar]
- 15.Al-Jamal Wafa' T, Al-Ahmady ZS, Kostarelos K. Pharmacokinetics & tissue distribution of temperature-sensitive liposomal doxorubicin in tumor-bearing mice triggered with mild hyperthermia. Biomaterials 2012;33:4608–17. 10.1016/j.biomaterials.2012.03.018 [DOI] [PubMed] [Google Scholar]
- 16.Needham D, Anyarambhatla G, Kong G, et al. A new temperature-sensitive liposome for use with mild hyperthermia: characterization and testing in a human tumor xenograft model. Cancer Res 2000;60:1197–201. [PubMed] [Google Scholar]
- 17.Needham D, Dewhirst MW. The development and testing of a new temperature-sensitive drug delivery system for the treatment of solid tumors. Adv Drug Deliv Rev 2001;53:285–305. 10.1016/S0169-409X(01)00233-2 [DOI] [PubMed] [Google Scholar]
- 18.Kong G, Anyarambhatla G, Petros WP, et al. Efficacy of liposomes and hyperthermia in a human tumor xenograft model: importance of triggered drug release. Cancer Res 2000;60:6950–7. [PubMed] [Google Scholar]
- 19.Ranjan A, Jacobs GC, Woods DL, et al. Image-Guided drug delivery with magnetic resonance guided high intensity focused ultrasound and temperature sensitive liposomes in a rabbit VX2 tumor model. J Control Release 2012;158:487–94. 10.1016/j.jconrel.2011.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Staruch RM, Ganguly M, Tannock IF, et al. Enhanced drug delivery in rabbit VX2 tumours using thermosensitive liposomes and MRI-controlled focused ultrasound hyperthermia. Int J Hyperthermia 2012;28:776–87. 10.3109/02656736.2012.736670 [DOI] [PubMed] [Google Scholar]
- 21.de Smet M, Hijnen NM, Langereis S, et al. Magnetic resonance guided high-intensity focused ultrasound mediated hyperthermia improves the intratumoral distribution of temperature-sensitive liposomal doxorubicin. Invest Radiol 2013;48:395–405. 10.1097/RLI.0b013e3182806940 [DOI] [PubMed] [Google Scholar]
- 22.Li L, ten Hagen TLM, Hossann M, et al. Mild hyperthermia triggered doxorubicin release from optimized stealth thermosensitive liposomes improves intratumoral drug delivery and efficacy. J Control Release 2013;168:142–50. 10.1016/j.jconrel.2013.03.011 [DOI] [PubMed] [Google Scholar]
- 23.Kim Y-sun, Keserci B, Partanen A, et al. Volumetric MR-HIFU ablation of uterine fibroids: role of treatment cell size in the improvement of energy efficiency. Eur J Radiol 2012;81:3652–9. 10.1016/j.ejrad.2011.09.005 [DOI] [PubMed] [Google Scholar]
- 24.Hurwitz MD, Ghanouni P, Kanaev SV, et al. Magnetic resonance-guided focused ultrasound for patients with painful bone metastases: phase III trial results. J Natl Cancer Inst 2014;106. 10.1093/jnci/dju082. [Epub ahead of print: 23 Apr 2014]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsiao Y-H, Kuo S-J, Tsai H-D, et al. Clinical application of high-intensity focused ultrasound in cancer therapy. J Cancer 2016;7:225–31. 10.7150/jca.13906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chu W, Staruch RM, Pichardo S, et al. Magnetic resonance-guided high-intensity focused ultrasound hyperthermia for recurrent rectal cancer: Mr thermometry evaluation and preclinical validation. Int J Radiat Oncol Biol Phys 2016;95:1259–67. 10.1016/j.ijrobp.2016.03.019 [DOI] [PubMed] [Google Scholar]
- 27.Bing C, Patel P, Staruch RM, et al. Longer heating duration increases localized doxorubicin deposition and therapeutic index in VX2 tumors using MR-HIFU mild hyperthermia and thermosensitive liposomal doxorubicin. Int J Hyperthermia 2019;36:195–202. 10.1080/02656736.2018.1550815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu L, Partanen A, Talcott MR, et al. Feasibility and safety assessment of magnetic resonance-guided high-intensity focused ultrasound (MRgHIFU)-mediated mild hyperthermia in pelvic targets evaluated using an in vivo porcine model. Int J Hyperthermia 2019;36:1146–58. 10.1080/02656736.2019.1685684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deckers R, Rome C, Moonen CTW. The role of ultrasound and magnetic resonance in local drug delivery. J Magn Reson Imaging 2008;27:400–9. 10.1002/jmri.21272 [DOI] [PubMed] [Google Scholar]
- 30.Merckel LG, Bartels LW, Köhler MO, et al. MR-guided high-intensity focused ultrasound ablation of breast cancer with a dedicated breast platform. Cardiovasc Intervent Radiol 2013;36:292–301. 10.1007/s00270-012-0526-6 [DOI] [PubMed] [Google Scholar]
- 31.Deckers R, Merckel LG, Denis de Senneville B, et al. Performance analysis of a dedicated breast MR-HIFU system for tumor ablation in breast cancer patients. Phys Med Biol 2015;60:5527–42. 10.1088/0031-9155/60/14/5527 [DOI] [PubMed] [Google Scholar]
- 32.Merckel LG, Knuttel FM, Deckers R, et al. First clinical experience with a dedicated MRI-guided high-intensity focused ultrasound system for breast cancer ablation. Eur Radiol 2016;26:4037–46. 10.1007/s00330-016-4222-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zagar TM, Vujaskovic Z, Formenti S, et al. Two phase I dose-escalation/pharmacokinetics studies of low temperature liposomal doxorubicin (LTLD) and mild local hyperthermia in heavily pretreated patients with local regionally recurrent breast cancer. Int J Hyperthermia 2014;30:285–94. 10.3109/02656736.2014.936049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poon RT, Borys N. Lyso-thermosensitive liposomal doxorubicin: an adjuvant to increase the cure rate of radiofrequency ablation in liver cancer. Future Oncol 2011;7:937–45. 10.2217/fon.11.73 [DOI] [PubMed] [Google Scholar]
- 35.Tak WY, Lin S-M, Wang Y, et al. Phase III heat study adding Lyso-Thermosensitive liposomal doxorubicin to radiofrequency ablation in patients with unresectable hepatocellular carcinoma lesions. Clin Cancer Res 2018;24:73–83. 10.1158/1078-0432.CCR-16-2433 [DOI] [PubMed] [Google Scholar]
- 36.Lyon PC, Gray MD, Mannaris C, et al. Safety and feasibility of ultrasound-triggered targeted drug delivery of doxorubicin from thermosensitive liposomes in liver tumours (TARDOX): a single-centre, open-label, phase 1 trial. Lancet Oncol 2018;19:1027–39. 10.1016/S1470-2045(18)30332-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gray MD, Lyon PC, Mannaris C, et al. Focused ultrasound hyperthermia for targeted drug release from thermosensitive liposomes: results from a phase I trial. Radiology 2019;291:232–8. 10.1148/radiol.2018181445 [DOI] [PubMed] [Google Scholar]
- 38.van Breugel JMM, Wijlemans JW, Vaessen HHB, et al. Procedural sedation and analgesia for respiratory-gated MR-HIFU in the liver: a feasibility study. J Ther Ultrasound 2016;4:19. 10.1186/s40349-016-0063-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ishihara Y, Calderon A, Watanabe H, et al. A precise and fast temperature mapping using water proton chemical shift. Magn Reson Med 1995;34:814–23. 10.1002/mrm.1910340606 [DOI] [PubMed] [Google Scholar]
- 40.De Poorter J. Noninvasive MRI thermometry with the proton resonance frequency method: study of susceptibility effects. Magn Reson Med 1995;34:359–67. 10.1002/mrm.1910340313 [DOI] [PubMed] [Google Scholar]
- 41.Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the functional assessment of cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 1997;15:974–86. 10.1200/JCO.1997.15.3.974 [DOI] [PubMed] [Google Scholar]
- 42.Abetz L, Coombs JH, Keininger DL, et al. Development of the cancer therapy satisfaction questionnaire: item generation and content validity testing. Value Health 2005;8 Suppl 1:S41–53. 10.1111/j.1524-4733.2005.00073.x [DOI] [PubMed] [Google Scholar]
- 43.Cheung K, de Mol M, Visser S, et al. Reliability and validity of the cancer therapy satisfaction questionnaire in lung cancer. Qual Life Res 2016;25:71–80. 10.1007/s11136-015-1062-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 45.Wahl RL, Jacene H, Kasamon Y, et al. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 2009;50 Suppl 1:122S–50. 10.2967/jnumed.108.057307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan S, Davidson N, Juozaityte E, et al. Phase III trial of liposomal doxorubicin and cyclophosphamide compared with epirubicin and cyclophosphamide as first-line therapy for metastatic breast cancer. Ann Oncol 2004;15:1527–34. 10.1093/annonc/mdh393 [DOI] [PubMed] [Google Scholar]
- 47.Celsion Corporation . ThermoDox®, Lyso-Thermosensitive Liposomal Doxorubicin (LTLD), Investigator’s Brochure; 2019.
- 48.Wood BJ, Poon RT, Locklin JK, et al. Phase I study of heat-deployed liposomal doxorubicin during radiofrequency ablation for hepatic malignancies. J Vasc Interv Radiol 2012;23:248–55. 10.1016/j.jvir.2011.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gabizon A, Catane R, Uziely B, et al. Prolonged circulation time and enhanced accumulation in malignant exudates of doxorubicin encapsulated in polyethylene-glycol coated liposomes. Cancer Res 1994;54:987–92. [PubMed] [Google Scholar]
- 50.Swenson CE, Bolcsak LE, Batist G, et al. Pharmacokinetics of doxorubicin administered i.v. as Myocet (TLC D-99; liposome-encapsulated doxorubicin citrate) compared with conventional doxorubicin when given in combination with cyclophosphamide in patients with metastatic breast cancer. Anticancer Drugs 2003;14:239–46. 10.1097/00001813-200303000-00008 [DOI] [PubMed] [Google Scholar]
- 51.Joerger M, Huitema ADR, Richel DJ, et al. Population pharmacokinetics and pharmacodynamics of doxorubicin and cyclophosphamide in breast cancer patients: a study by the EORTC-PAMM-NDDG. Clin Pharmacokinet 2007;46:1051–68. 10.2165/00003088-200746120-00005 [DOI] [PubMed] [Google Scholar]
- 52.Jacquet JM, Bressolle F, Galtier M, et al. Doxorubicin and doxorubicinol: intra- and inter-individual variations of pharmacokinetic parameters. Cancer Chemother Pharmacol 1990;27:219–25. 10.1007/BF00685716 [DOI] [PubMed] [Google Scholar]
- 53.Callies S, de Alwis DP, Wright JG, et al. A population pharmacokinetic model for doxorubicin and doxorubicinol in the presence of a novel MDR modulator, zosuquidar trihydrochloride (LY335979). Cancer Chemother Pharmacol 2003;51:107–18. 10.1007/s00280-002-0542-3 [DOI] [PubMed] [Google Scholar]
- 54.Joerger M, Huitema ADR, Meenhorst PL, et al. Pharmacokinetics of low-dose doxorubicin and metabolites in patients with AIDS-related Kaposi sarcoma. Cancer Chemother Pharmacol 2005;55:488–96. 10.1007/s00280-004-0900-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-040162supp001.pdf (1.6MB, pdf)