Abstract
Environmental factors, and in particular diet, are known to play a key role in the development of Coronary Heart Disease. Many of these factors were unveiled by detailed nutritional epidemiology studies, focusing on the role of a single nutrient or food at a time. Here, we apply an Environment-Wide Association Study approach to Nurses’ Health Study data to explore comprehensively and agnostically the association of 257 nutrients and 117 foods with coronary heart disease risk (acute myocardial infarction and fatal coronary heart disease). After accounting for multiple testing, we identify 16 food items and 37 nutrients that show statistically significant association – while adjusting for potential confounding and control variables such as physical activity, smoking, calorie intake, and medication use – among which 38 associations were validated in Nurses’ Health Study II. Our implementation of Environment-Wide Association Study successfully reproduces prior knowledge of diet-coronary heart disease associations in the epidemiological literature, and helps us detect new associations that were only marginally studied, opening potential avenues for further extensive experimental validation. We also show that Environment-Wide Association Study allows us to identify a bipartite food-nutrient network, highlighting which foods drive the associations of specific nutrients with coronary heart disease risk.
Subject terms: Cardiovascular diseases, Epidemiology
Environmental and dietary factors are known to play a role in the development of coronary heart disease. Here the authors apply a genomic-inspired methodology to Nurses’ Health Study data to explore comprehensively and agnostically the association of 257 nutrients and 117 foods with coronary heart disease risk.
Introduction
The prevalence of heart disease, the leading cause of death throughout the world, is strongly influenced by diet and eating habits1–4. For example, a recent CDC (Centers for Disease Control and Prevention) report5, focusing on death rates caused by heart disease across the United States, documented substantial regional differences compatible with different eating patterns. Similarly, while among individuals of Japanese descent, coronary heart disease (CHD) incidence rates are only 1.6 per person-years in Japan, it increases to 3.0 in Hawaii, and 3.7 in San Francisco6, differences that cannot be explained by genetic factors, documenting the key role dietary and other environmental factors play in the development of the disease.
Much of our knowledge about the role of food on health comes from epidemiological association studies in which a single or limited number of exposure(s) is/are analyzed in relation to a phenotype, representing a hypothesis-driven path towards understanding diet–disease relationships. Yet, diet is not a simple sum of several nutrients, as each food product consists of a mixture of nutrients associated with multiple compounds of limited or unknown nutritional value7. Accordingly, the effect of each dietary compound on human health should not be investigated in isolation, but in the presence of other associated chemical compounds and relevant food sources. For example, Kolonel et al.8 initially reported that beta-carotene consumption was positively associated with the risk of prostate cancer. While this finding was worrisome, in a subsequent analysis of foods, intake of carrots, the largest source of beta-carotene, was not related to the risk of prostate cancer; the observed association was due to intake of papaya9. Thus, the analysis of foods provided evidence against the effect of beta-carotene and suggested that some factors specific to papaya might be responsible for the original finding10. An alternative approach is dietary pattern analysis that focuses on the effects of the overall diet11–13, rather than a single or a few nutrients. While dietary pattern analyses are ideal in the development of nutritional guidelines14, they are insufficient for the agnostic discovery of new signals for further experimental or mechanistic validation.
As an alternative to the traditional epidemiological studies, environment-wide association studies (or EWAS) were proposed to identify new environmental factors in disease and disease-related phenotypes in an unbiased manner. EWAS is inspired by the analytical procedures developed in genome-wide association studies (GWAS)15 in which a panel of “exposures” (genotype variants) is studied in relation to a phenotype of interest. For example, using the National Health and Nutrition Examination Survey dataset, an EWAS study explored the associations of 543 environmental attributes with type 2 diabetes, identifying five statistically significant associations validated across independent cohorts15. Wulaningsih et al.16 investigated 182 nutrition and lifestyle factors in relation to abdominal obesity, finding a statistically significant association of obesity with five factors in men and seven factors in women. Merritt et al.17 used European Prospective Investigation into Cancer and Nutrition (EPIC) data to evaluate endometrial cancer risk associations for the dietary intake of 84 foods and nutrients, concluding that only coffee intake had a statistically significant inverse relationship.
Despite the recent success of the EWAS methodology in unveiling multiple nutritional factors that together may contribute to our health, its widespread use is undermined by several factors and limitations18. Indeed, failing to achieve adequate statistical power in association detection, EWAS studies could not always recover known environment–disease associations confirmed by large, prospective cohort studies and randomized trials17,19,20. As we show below, these failures are not inherent in the EWAS methodology, but are mainly rooted in the limited size, limited variability, and lack of repeated measurements of the datasets to which EWAS has been applied thus far. While the statistical power of the EWAS study approach is a legitimate concern, the magnitude of the statistical power depends on multiple factors, including the nature and the size of the dataset, as well as the statistical tools/models used for the analysis. Indeed, as we show here, if we apply a wide-association study approach to an adequately sized longitudinal cohort dataset with sufficient variability, we consistently recover prior knowledge about diet–disease relationships.
The EWAS methodology may be particularly useful for diseases for which nutritional associations are unknown18. While the effect of dietary exposures on heart disease has been extensively studied and the causal effects of many of these associations confirmed, the diet–disease literature occasionally demonstrates conflicting findings2,21–23, limiting our understanding of the true effect of dietary exposures on diseases. We will show that the wide-association study approach can provide comparable insights in an efficient manner by applying an unbiased standardized set of analytical tools.
Here we implement an EWAS methodology, aiming to identify dietary factors associated with CHD systematically and comprehensively, focusing on both nutrient intake and food consumption. To overcome the limited statistical power of previous studies, we apply our methodology to the Nurses’ Health Study (NHS), a longitudinal prospective study designed to investigate the longitudinal effects of nutrition on health and disease development. While there are larger cohorts available for studying chronic diseases, such as the UK Biobank24 and the China Kadoorie Biobank25, both with around 500,000 participants, NHS is unique, owing to comprehensive longitudinal dietary data collection. Beginning in 1976, NHS gathered registered female nurses, ages 30–55 years, from across the United States, initially designed to investigate the use of oral contraception in relation with risk of breast cancer. Participants are asked to complete questionnaires every 2 years, and in 1980 a Food Frequency Questionnaire (FFQ) has been included, designed to capture dietary behaviors. Follow-up dietary questionnaires were administered in 1984, 1986, and every 4 years since then. Questionnaires used from 1984 and thereafter included about 130 foods plus detailed information about brands and types of margarine, breakfast cereals, multiple vitamins, and types of fat used for cooking and baking. As health professionals, nurses were chosen for their ability to complete the health-related questionnaires thoroughly and accurately26. To date, NHS has been expanded to NHS II and NHS III to cover a younger population of nurses27. These three cohorts resulted in an extensive published body of research on the relationships of environmental and genetic factors to various diseases28. The dietary drivers of CHD have been extensively studied within NHS data, most analyses primarily focusing on a single or limited number of exposures, while controlling for an appropriate set of adjusting variables. Some of these findings, as those for trans-fats, have inspired experimental studies and were confirmed to have a causal effect on developing heart diseases29–31.
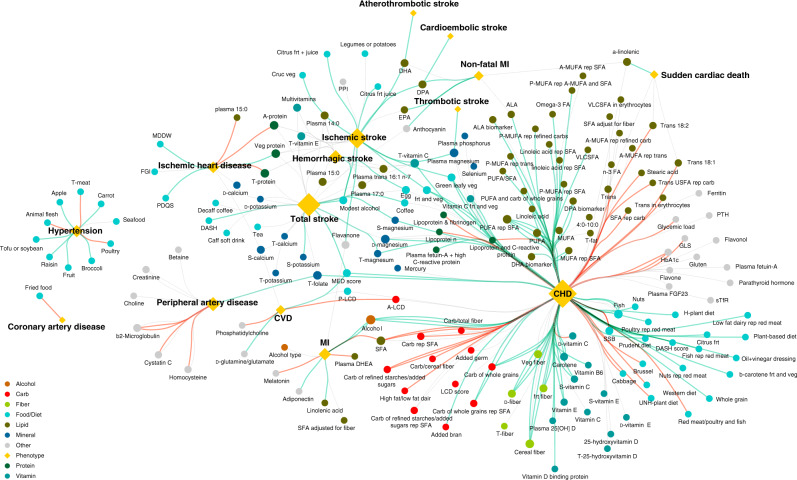
To have a broad picture of the existing knowledge about diet–disease associations in the NHS data, we mined the literature to identify all studies exploring the dietary determinants of heart-related diseases in original NHS and successive cohorts. The resulting knowledge graph (Fig. 1) shows that the most extensively studied cardiovascular phenotype using NHS data is CHD. Here, we use the term negative when a higher level of exposure is associated with a lower CHD risk. Similarly, we use positive term when a higher level of an exposure is associated with CHD risk. We made this choice for simplicity, and it should not be confused with a causal relationship.
Fig. 1. The Knowledge Graph of the Dietary Factors Associated with Cardiovascular Disease in the NHS Data.
The nodes of the graph are dietary exposures (circles) and cardiovascular diseases (diamonds) as two sets of nodes. Each studied association is shown by an edge whose color denotes the “direction” (i.e., positive or negative) of the association. Green and red links indicate negative and positive associations, respectively, between an exposure and a disease. Grey links denote associations that were studied but not found to be statistically significant. In the context of NHS, CHD refers to non-fatal MI and fatal coronary heart disease; also, coronary artery disease (CAD) refers to non-fatal MI and fatal coronary artery disease. Cardiovascular disease (CVD) is defined as a composite of coronary artery disease and non-fatal or fatal stroke. Source data are provided in Source Data - Figure 1.xlsx. The figure aims to illustrate the body of work derived from NHS data on cardiovascular diseases. A detailed comparison of the result of our analysis with previous NHS-related work and other findings in the literature is provided in the section “Comparison with the literature”.
Excluding studies of biomarkers and tissues, the neighborhood of CHD comprises nutrients, food items, and dietary scores. Cumulatively, 120 associations were studied, documenting 63 negative associations and 22 positive relations with CHD; in the remaining cases, there was no significant association between dietary exposure and CHD risk, as in the case of dietary magnesium32. The space of studied exposures is rather heterogeneous and is often driven by either the researcher’s interests or evidence from animal or mechanistic studies.
As illustrated in the knowledge graph, the single-association studies using NHS data have broadened our understanding of the dietary determinants of CHD. Some non-significant associations were found to be significant after the application of new statistical approaches in larger datasets. For example, while a study using the original NHS data found no association between fruit fiber intake and risk of CHD33, a pooled analysis of three NHS cohorts found that the higher consumption of dietary fiber from fruits was negatively associated with risk of CHD34.
Here, we show that a wide-association approach allows us to scan efficiently and systematically the dietary determinants of CHD, bypassing the problem with missing significant associations in epidemiological studies. By applying EWAS methodology to the NHS data, we find that a wide-association approach not only recovers the existing knowledge on diet–disease association, but also facilitates the discovery of novel associations, potentially inspiring future follow-up studies.
Results
Main findings
During the follow-up period, 2774 incident cases of non-fatal MI or fatal CHD were documented in NHS. The baseline average of total caloric intake and body mass index (BMI) among participants who later developed CHD were slightly higher than in those who did not develop CHD. In addition, prospective case subjects on average had lower physical activity compared with the non-case population (Supplementary Table 1). We examined the effect of 374 exposures on CHD risk, including 257 nutrients and 117 food items. The descriptive characteristics of these exposures are shown in Supplementary Table 2.
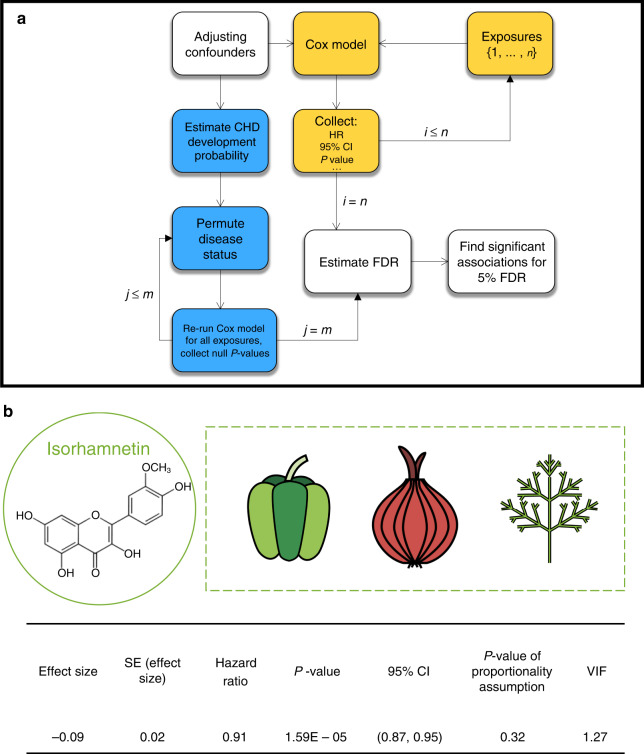
For the first phase of EWAS, using Cox regression models we collected the estimated effect size, the variance of effect size, hazard ratio (HR) for one standard deviation, P value, the 95% confidence interval (CI) for the HR, P value regarding the proportionality assumption, and the variance inflation factor (VIF). Consider, for example, the results of the long-term effect of isorhamnetin—an O-methylated flavon-ol from the class of flavonoids (Fig. 2b). The estimated HR (0.91, 95% CI: 0.87–0.95; P value 1.59 × 10−5) implies that one standard deviation higher consumption of Box–Cox-transformed isorhamnetin is associated with 91% lower CHD risk. The P value regarding the proportionality assumption indicates that the use of the Cox model is appropriate. The VIF equal to 1.27 suggests that there is no severe multicollinearity among the variables involved in the isorhamnetin test.
Fig. 2. Ewas Methodology Description and Output.
a For each exposure (i), we fit a Cox model to estimate CHD risk, while controlling for a set of adjusting variables (n exposures, in total). Through this process, we also collect the VIF and the P value regarding the proportionality assumption. After the fitting phase (yellow), we proceed with the multiple testing protocols (blue). We leverage confounding variables to estimate the likelihood of CHD development for each subject, and the disease status is then permuted accordingly, m times. For each exposure, the FDR is estimated, and associations with an FDR < 0.05 are considered statistically significant. b Isorhamnetin is an O-methylated flavonol from the class of flavonoids mainly found in green pepper, red onion, and dill. EWAS shows that isorhamnetin intake is negatively associated with CHD risk (HR: 0.91; 95% CI: 0.87–0.95; P value 1.59 × 10−5, from two-sided Wald test, with no adjustment for multiple comparisons). The P value regarding the proportionality assumption indicates the appropriateness of using the Cox model. The VIF of 1.27 is an indication of the absence of severe multicollinearity.
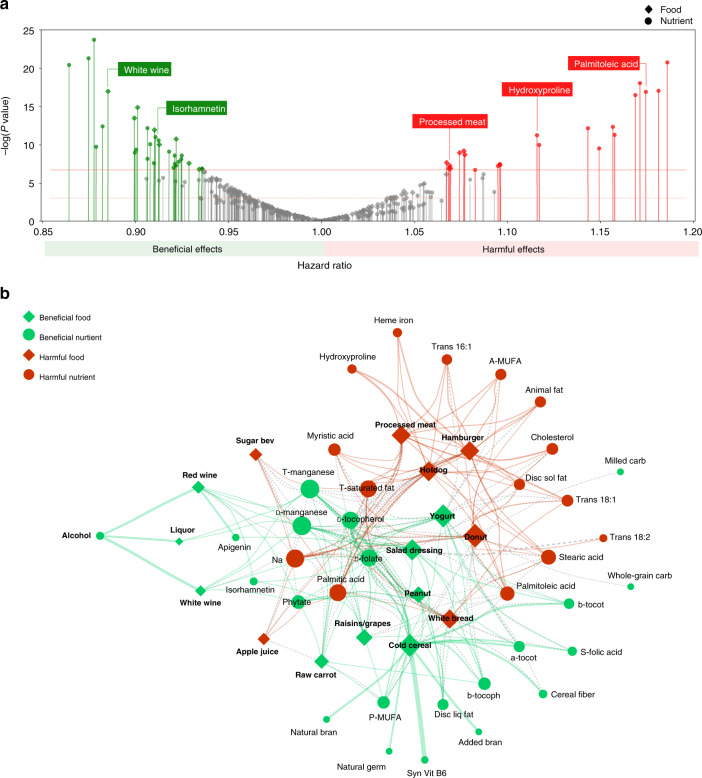
Figure 3a shows the distribution of Cox model P values for all investigated exposures. Exposures are ordered by the estimated HR, so that exposures with HR > 1.0 have harmful effects on CHD risk and exposures with HR < 1.0 are expected to be beneficial. Insignificant associations are mainly distributed around an HR of one, and exposures with smaller P values are scattered at the two ends of the distribution. Using the permutation procedure to account for multiple testing, we found 53 significant associations, including 16 food items and 37 nutrients. All significant associations had VIF < 5. For all significant associations, except for phytate, the P value regarding the proportionality assumption is >0.05. The minimum statistical power for detecting the smallest absolute effect size was 0.59, which is considered to be a moderate to a high level of power in clinical studies. A list of exposures that have a statistically significant association with CHD risk, together with their estimated HRs, is shown in Table 1. A list of both significant and non-significant associations is provided in Supplementary Table 3. We analyzed the correlations among the significant exposures, the result of which is shown in Supplementary Fig. 3. To help interpret our findings, we calculated the HR of each quintile of exposure intake compared with the first quintile, as a reference group (Supplementary Table 6).
Fig. 3. P value Distribution of Dietary Factors and the Bi-partite Food-Nutirent Network.
a P values are associated with two-sided Wald tests. The Y axis indicates the negative logarithm of the P value of each exposure. The dotted red horizontal line marks the level of 0.05 P value threshold and the solid red line demonstrates the level of 0.00117 P value threshold associated with the level of 0.05 FDR. Significant foods (diamonds) and nutrients (circles) with a negative association (HR < 1) are highlighted in green and exposures with a positive association (HR > 1) are shown in red. Source data are provided in Source Data - Figure 3-a.xlsx. b Bi-partite food-nutrient network, where negatively associated exposures are shown in green and positively associated exposures are shown in red. Different shapes are used to differentiate between foods (diamonds) and nutrients (circles). The node size is proportional to the absolute value of the estimated effect size. The link thickness is proportional to the amount of each nutrient’s composition in food. Source data are provided in Source Data - Figs. 3-b and 4-b.xlsx.
Table 1.
EWAS results.
| Type | Exposure | Effect size | SE (effect size) | Hazard ratio | 95% CI | P value of PH | VIF | P value | FDR |
|---|---|---|---|---|---|---|---|---|---|
| Nutrient | Alcohol | −0.13 | 0.02 | 0.88 | (0.84, 0.91) | 0.19 | 1.12 | 4.98E–11 | 0.000 |
| Nutrient | Added bran from wheat, rice, etc. | −0.13 | 0.02 | 0.87 | (0.84, 0.91) | 0.1 | 1.22 | 5.56E− 10 | 0.000 |
| Nutrient | Trans 16:1 | 0.17 | 0.03 | 1.19 | (1.12, 1.25) | 0.41 | 2.15 | 9.59E–10 | 0.000 |
| Nutrient | Discretionary liquid fat | −0.15 | 0.02 | 0.86 | (0.82, 0.91) | 0.84 | 1.48 | 1.33E–09 | 0.000 |
| Nutrient | Animal MUFA | 0.16 | 0.03 | 1.17 | (1.11, 1.24) | 0.78 | 2.09 | 1.42E–08 | 0.001 |
| Nutrient | Discretionary solid fat | 0.17 | 0.03 | 1.18 | (1.11, 1.25) | 0.71 | 2.51 | 3.82E–08 | 0.001 |
| Food | White wine | −0.12 | 0.02 | 0.89 | (0.85, 0.92) | 0.66 | 1.07 | 4.14E–08 | 0.001 |
| Nutrient | Palmitoleic acid | 0.16 | 0.03 | 1.17 | (1.11, 1.24) | 0.64 | 2.34 | 4.42E–08 | 0.001 |
| Nutrient | Animal fat | 0.16 | 0.03 | 1.17 | (1.10, 1.24) | 0.9 | 2.26 | 6.73E–08 | 0.001 |
| Food | Salad/oil and vinegar dressing | −0.1 | 0.02 | 0.9 | (0.87, 0.94) | 0.24 | 1.09 | 3.41E–07 | 0.001 |
| Food | Yogurt | −0.11 | 0.02 | 0.9 | (0.86, 0.94) | 0.09 | 1.07 | 1.37E–06 | 0.003 |
| Nutrient | Phytate | −0.13 | 0.03 | 0.88 | (0.84, 0.93) | 0.02 | 1.96 | 4.01E–06 | 0.005 |
| Nutrient | Stearic acid | 0.15 | 0.03 | 1.16 | (1.09, 1.23) | 0.82 | 2.76 | 4.25E–06 | 0.005 |
| Nutrient | Carbohydrate from milled wholegrain | −0.1 | 0.02 | 0.91 | (0.87, 0.95) | 0.29 | 1.29 | 5.03E–06 | 0.005 |
| Nutrient | Sodium | 0.13 | 0.03 | 1.14 | (1.08, 1.21) | 0.13 | 2.28 | 5.11E–06 | 0.005 |
| Food | Raw carrots | −0.09 | 0.02 | 0.91 | (0.87, 0.95) | 0.06 | 1.1 | 6.33E–06 | 0.005 |
| Nutrient | Total saturated fat | 0.15 | 0.03 | 1.16 | (1.08, 1.24) | 0.78 | 3.14 | 1.20E–05 | 0.007 |
| Nutrient | Hydroxyproline | 0.11 | 0.03 | 1.12 | (1.06, 1.17) | 0.25 | 1.64 | 1.26E–05 | 0.007 |
| Nutrient | Isorhamnetin | −0.09 | 0.02 | 0.91 | (0.87, 0.95) | 0.32 | 1.27 | 1.59E–05 | 0.007 |
| Food | Liquor | −0.08 | 0.02 | 0.92 | (0.89, 0.96) | 0.12 | 1.06 | 2.06E–05 | 0.009 |
| Nutrient | Carbohydrate from wholegrain | −0.09 | 0.02 | 0.91 | (0.87, 0.95) | 0.22 | 1.28 | 2.46E–05 | 0.010 |
| Nutrient | Cereal fiber | −0.1 | 0.02 | 0.91 | (0.87, 0.95) | 0.2 | 1.49 | 4.04E–05 | 0.012 |
| Food | Red wine | −0.09 | 0.02 | 0.91 | (0.87, 0.95) | 0.63 | 1.04 | 4.28E–05 | 0.012 |
| Nutrient | Trans 18:2 | 0.11 | 0.03 | 1.12 | (1.06, 1.18) | 0.19 | 1.83 | 4.48E–05 | 0.012 |
| Nutrient | Dietary tocopherols | −0.13 | 0.03 | 0.88 | (0.83, 0.94) | 0.75 | 2.78 | 5.71E–05 | 0.013 |
| Nutrient | Palmitic acid | 0.14 | 0.03 | 1.15 | (1.07, 1.23) | 0.93 | 3.37 | 7.01E–05 | 0.015 |
| Nutrient | Dietary folate | −0.11 | 0.03 | 0.9 | (0.85, 0.95) | 0.49 | 1.91 | 8.33E–05 | 0.016 |
| Food | Doughnuts | 0.07 | 0.02 | 1.08 | (1.04, 1.12) | 0.1 | 1.1 | 9.84E–05 | 0.017 |
| Nutrient | Beta-tocotrienol | −0.09 | 0.02 | 0.92 | (0.88, 0.96) | 0.43 | 1.31 | 1.07E–04 | 0.018 |
| Nutrient | Plant MUFA | −0.11 | 0.03 | 0.9 | (0.85, 0.95) | 0.8 | 2.05 | 1.22E–04 | 0.019 |
| Food | Hotdog | 0.07 | 0.02 | 1.07 | (1.04, 1.11) | 0.05 | 1.09 | 1.26E–04 | 0.019 |
| Food | White bread | 0.07 | 0.02 | 1.08 | (1.04, 1.12) | 0.08 | 1.12 | 1.61E–04 | 0.022 |
| Nutrient | Natural germ | −0.08 | 0.02 | 0.92 | (0.88, 0.96) | 0.39 | 1.24 | 1.78E–04 | 0.022 |
| Nutrient | Apigenin | −0.08 | 0.02 | 0.92 | (0.89, 0.96) | 0.81 | 1.15 | 1.79E–04 | 0.022 |
| Nutrient | Beta-tocopherol | −0.1 | 0.03 | 0.91 | (0.86, 0.96) | 0.55 | 1.87 | 2.73E–04 | 0.028 |
| Nutrient | Natural bran | −0.08 | 0.02 | 0.92 | (0.89, 0.96) | 0.45 | 1.26 | 2.90E–04 | 0.028 |
| Nutrient | Supplemental selenium | −0.08 | 0.02 | 0.92 | (0.88, 0.96) | 0.89 | 1.38 | 4.01E–04 | 0.034 |
| Food | Apple juice or cider | 0.07 | 0.02 | 1.07 | (1.03, 1.11) | 0.95 | 1.07 | 4.49E–04 | 0.036 |
| Nutrient | Dietary manganese | −0.09 | 0.03 | 0.91 | (0.86, 0.96) | 0.08 | 2 | 4.82E–04 | 0.037 |
| Food | Peanuts | −0.07 | 0.02 | 0.93 | (0.89, 0.97) | 0.09 | 1.08 | 4.92E–04 | 0.037 |
| Nutrient | Alpha-tocotrienol | −0.08 | 0.02 | 0.92 | (0.88, 0.96) | 0.43 | 1.51 | 5.37E–04 | 0.037 |
| Nutrient | Myristic acid | 0.09 | 0.03 | 1.1 | (1.04, 1.15) | 0.59 | 1.99 | 5.44E–04 | 0.037 |
| Nutrient | Cholesterol | 0.09 | 0.03 | 1.1 | (1.04, 1.16) | 0.43 | 2 | 6.09E–04 | 0.039 |
| Nutrient | Supplemental or fortified folic acid | −0.08 | 0.02 | 0.92 | (0.88, 0.97) | 0.53 | 1.55 | 6.63E–04 | 0.040 |
| Food | All processed meats | 0.07 | 0.02 | 1.07 | (1.03, 1.11) | 0.23 | 1.14 | 6.73E–04 | 0.040 |
| Nutrient | Trans 18:1 | 0.09 | 0.03 | 1.09 | (1.04, 1.15) | 0.62 | 1.93 | 6.94E–04 | 0.040 |
| Nutrient | Total manganese | −0.08 | 0.02 | 0.92 | (0.88, 0.97) | 0.99 | 1.59 | 8.72E–04 | 0.046 |
| Food | Hamburger | 0.07 | 0.02 | 1.07 | (1.03, 1.11) | 0.09 | 1.18 | 9.53E–04 | 0.047 |
| Food | Beverages with sugar | 0.07 | 0.02 | 1.07 | (1.03, 1.11) | 0.86 | 1.13 | 9.70E–04 | 0.047 |
| Nutrient | Synthetic vitamin B6 | −0.07 | 0.02 | 0.94 | (0.90, 0.97) | 0.66 | 1.07 | 1.02E–03 | 0.047 |
| Food | Cold breakfast cereal | −0.07 | 0.02 | 0.94 | (0.90, 0.97) | 0.13 | 1.1 | 1.02E–03 | 0.047 |
| Food | Raisins or grapes | −0.07 | 0.02 | 0.93 | (0.90, 0.97) | 0.91 | 1.11 | 1.09E–03 | 0.048 |
| Nutrient | Heme iron | 0.08 | 0.02 | 1.08 | (1.03, 1.14) | 0.51 | 1.55 | 1.17E–03 | 0.050 |
The exposures that are statistically significant in association with CHD risk are listed. P values are associated with two-sided Wald tests.
Traditional epidemiological studies are limited to the detection of a single exposure (food or nutrient) in relation to CHD; however, the developed EWAS methodology allows us to explore the space of food/nutrient associations related to the disease. That is, in addition to unveiling which nutrient shows significant association with CHD, EWAS also helps us understand which nutrient in connection with which food is responsible for the effect. To demonstrate this principle, we use the food composition table of NHS to extract the contribution of each significant food to the total amount of a significant nutrient in the food supply (Fig. 3a). Using a force-directed layout algorithm, we represent this information as a bipartite network, allowing us to explore the significant inter-dependencies among nutrients and food items. In Fig. 3b, negatively associated nutrients and foods are color coded as green and positively associated nutrients and foods are shown in red. We retrieve two clearly distinct clusters, negatively associated nutrients and foods on one hand, and positively associated nutrients and foods on the other. We also find that several food items, such as white bread and yogurt are connected to both negatively and positively associated nutrients. As expected, foods high in negatively associated nutrients are also related to lower CHD risk and foods containing positively associated nutrients are related to higher CHD risk.
In the network shown in Fig. 3b, each node has its own estimated HR. For each nutrient, we compare the estimated HR with the expected geometric hazard ratio , determined by Eq. (1),
| 1 |
where is the normalized weight of the link connecting nutrient i to food k, is the estimated effect size of food k, is the estimated hazard ratio of food k, and (Fig. 4a).
Fig. 4. Comparison between Actual Nutirent HR and Weighted Food HR.
a The structure of the food composition table is shown on the left. A network is built based on a subset of the composition table where significant nutrients and significant food items are extracted. In the network on the right, the weight of a link between a nutrient and a food is proportional to the amount of a nutrient in each specific food item compared with all other food items. b Points in the top right corner and in the bottom left corner correspond to the nutrients whose actual HR is in the same direction as their weighted food HR. For whole-grain carbohydrates, milled whole-grain carbohydrates, total saturated fat, trans-fatty acid 18:2, sodium, and myristic acid, the actual HR has an opposite direction compared with the weighted food HR. Source data are provided in Source Data Figure 3-b and 4-b.xlsx.
As we show in Fig. 4b, for the majority of nutrients, the actual nutrient HR has the same directionality as the weighed food HR, indicating that EWAS captures both important nutrients and their main drivers in the food system. Whole-grain carbohydrate and milled whole-grain carbohydrate were found to be negatively associated with CHD risk; however, among food items high in these two exposures, we only found doughnuts to relate with higher CHD risk statistically significantly. Consequently, the weighted food HR for these exposures has an opposite directional effect. Yet, the correlation analysis (Supplementary Fig. 3) shows that these two exposures have negative correlations with positively associated foods, such as white bread and processed meats, and positive correlations with negatively associated foods, such as cold breakfast cereal and raw carrots. Moreover, myristic acid, trans-18:2, sodium, and total saturated fat were found to be positively associated with higher CHD risk themselves, but the weighted food HR for them indicates an opposite direction. These nutrients are not only distributed among positively associated foods, but also negatively associated foods. Myristic acid is in both processed meats and yogurt, trans-fatty acid 18:2 is present in salad/oil, vinegar dressing, and doughnuts, sodium is spread among salad/oil and vinegar dressing and processed meats, and total saturated fat is found in yogurt and processed meat. However, the consumption of these exposures is positively correlated with positively associated foods (Supplementary Fig. 3). The observed disparity indicates that for most of the nutrients, the structure of the food system determines the amount of nutrients in the diet, while for some other nutrients individual choices drive the nutrient amount in the diet. The signal determined by significant foods is a strong driver, but not always sufficient to capture exhaustively the nutrient associations with CHD. Even though some of the nutrients are not well captured by the food approximation (yellow points), with this approach we tend to correctly estimate the sign of the association, while underestimating the effect size. This observation indicates that solely looking at food items, one would underestimate the effect of those nutrients whose consumption is strongly determined by the behavioral aspect and not mainly by their average amount in food. Additionally, this observation can be partially explained by the higher resolution in the calculation of nutrient intake for breakfast cereals, margarine, and types of fats used for cooking and baking, for which we asked separate questions about their type and brand that linked with extensive databases for detailed composition values.
Comparison with the literature
Applying the EWAS methodology to NHS data allowed us to identify 53 dietary exposures that show statistically significant association with CHD risk. Next, we discuss our results in the context of the previous literature, offering a direct validation of our findings, also helping detect novel knowledge, and to generate new hypotheses. We found that in most cases, EWAS strengthens the existing knowledge about the effect of diet on CHD, and in some cases, it sheds a light on exposures that have not been thoroughly studied in the literature.
Most of our statistically significant findings were in agreement with the previous literature, strengthening the prior findings and supporting the robustness of the EWAS platform. Among food items, we found that white wine, red wine, and liquor, but not beer, have a negative association with higher CHD risk, aligned with previous findings35,36. Despite recovering an inverse association between alcohol intake and CHD risk (HR 0.88; 95% CI: 0.84–0.91; P value < 5 × 10−11), it is worth noting that the overall level of alcohol consumption is not very high in this population study, and such inverse association has not been replicated in other quasi-experimental Mendelian randomization studies37,38.
Moreover, we found salad/oil and vinegar dressing, yogurt, cold breakfast cereal, raw carrots, raisins or grapes, and peanuts have a negative association with higher CHD risk, in line with previous studies39–44. Moreover, we found that total processed meat consumption, hot dogs, apple juice or cider, beverages with sugar, and white bread have positive association with higher CHD risk, as previously shown by other studies45–48.
Many compounds from lipid and fatty acid groups have been studied previously in relation to CHD risk. In line with previous studies49–55, we found that higher consumption of cholesterol, trans-fatty acid 16:1, trans-fatty acid 18:1, trans- fatty acid 18:2, total saturated fat, animal monounsaturated fatty acids (MUFA), myristic acid, palmitoleic acid, palmitic acid, and stearic acid are associated with a higher risk of developing CHD (P value < 1 ×10−3). These dietary factors are mainly distributed among animal-based foods. By contrast, we found that plant MUFA can be protective against CHD development (HR 0.90; 95% CI: 0.85–0.95; P value < 2 × 10−4), which has also been shown by Zong et al.53. Plant MUFAs are abundant in salad/oil and vinegar dressing and peanuts, food items that we also found to be statistically significantly associated with lower CHD risk (salad/oil and vinegar dressing: HR 0.90; 95% CI: 0.87–0.94; P value < 4 × 10−7; peanuts: HR 0.93; 95% CI: 0.89–0.97; P value < 5 × 10−4).
Whole grains are composed of endosperm, germ, and bran, in contrast with milled whole grains in which only endosperm is retained. We found that higher consumption of carbohydrate from whole grains is associated with lower CHD risk, similar to the findings in ref. 56. While the milling process removes several valuable compounds in whole grains, we interestingly detected a similar protective effect for carbohydrate from milled whole grains. In addition, we showed that both natural bran and added bran are negatively associated with CHD risk, consistent with previous studies57,58. We also documented a negative association for cereal fiber with CHD (HR 0.91; 95% CI: 0.87–0.95; P value < 5 × 10−5), in agreement with ref. 59. One of the food groups that can be rich in natural bran and germ, added bran, and cereal fiber is cold breakfast cereal, which we also found to be negatively related to CHD (HR 0.94; 95% CI: 0.90–0.97; P value < 2 × 10−3).
While we rediscovered the negative association of manganese consumption with CHD risk (HR 0.92; 95% CI: 0.88–0.97; P value < 1 × 10−3)60, we also found that higher supplemental selenium is associated with lower CHD risk (HR 0.92; 95% CI: 0.88–0.96; P value < 5 × 10−4). A specific cardiomyopathy responsive to selenium supplementation has been observed in domestic animals61 and among Chinese persons with Keshan disease62. However, more recent studies found no association between selenium supplementation and primary prevention of cardiovascular disease (CVD), for which reason it is not recommended for CVD prevention63,64. Moreover, our observed positive association of sodium (HR 1.14; 95% CI: 1.08–1.21; P value < 6 × 10−6) is also consistent with prior studies65.
Our findings indicate that higher consumption of dietary folate (HR 0.90; 95% CI: 0.85–0.95; P value < 9 × 10−5) and folic acid (HR 0.92; 95% CI: 0.88–0.97; P value < 7 × 10−4) are related to lower CHD risk, again aligned with previous findings66,67. While the beneficial effect of natural vitamin B6 was previously documented66, we interestingly found that increased synthetic vitamin B6 consumption is related to lower CHD risk (HR 0.94; 95% CI: 0.90–0.97; P value < 2 × 10−3). Moreover, our results reveal that beta-tocopherol, total dietary tocopherol intake, alpha-tocotrienol, and beta-tocotrienol are negatively associated with CHD risk (HR < 0.92; P value < 6 × 10−4). Earlier studies reported similar effects regarding alpha-tocopherol, total tocopherol intake, and alpha-tocotrienol68,69. While the antioxidant and anti-inflammatory effects of some of the vitamin E isomers have been documented, little is known about the effect of beta-tocopherol and beta-tocotrienol on cardiovascular health. These two compounds are mainly found in whole-grain products and nuts. In the liver, beta-tocopherol undergoes omega-hydroxylation, oxidation, and beta-oxidation to generate 13′-hydroxychromanols/carboxychromanols, which have potential antioxidant properties70,71. This fact strengths our findings regarding the protective effect of beta-tocopherol against CHD. Moreover, beta-tocotrienol, in particular, was shown to be inversely related to the risk of type 2 diabetes mellitus72, but has not been well-studied regarding its effects on the cardiovascular system. However, among different forms of tocotrienols, beta-tocotrienol has the highest antioxidant activity73, in support of the protective effect against CHD that we observed in EWAS.
We found that heme iron (HR 1.08; 95% CI: 1.03–1.14; P value < 2 × 10−3) is statistically significantly associated with higher CHD risk. Similar effects were detected in ref. 74. We also found isorhamnetin and apigenin (HR < 0.92; P value < 2 × 10−4) to be inversely associated with CHD risk, in line with refs. 75,76 (Supplementary Table 7). Moreover, in EWAS, we found that higher dietary hydroxyproline intake is associated with higher CHD risk (HR 1.12; 95% CI: 1.06-1.17; P value < 2 × 10−5). Hydroxyproline is a nonessential amino acid derivative and a major component of the protein collagen mainly found in animal-based food products, such as beef, chicken, and pork. Increased hydroxyproline levels in the urine and/or serum are normally associated with degradation of connective tissue and Marfan syndrome77, and were also found to be related to Paget disease78. The decrease in various hydroxyproline fractions in aortic tissue of rabbits has been shown to be a risk factor for the progression of atherosclerosis79. Nonetheless, serum hydroxyproline is mainly associated with peptides released from the breakdown of collagen, and dietary hydroxyproline intake does not considerably affect serum hydroxyproline levels unless consumed in the form of gelatin80. While non-prescription hydroxyproline supplements are available as l-hydroxyproline and N-acetyl-l-hydroxyproline, there seems to be no evidence for the effectiveness of oral hydroxyproline supplements in the prevention or treatment of osteoarthritis, osteoporosis, rheumatoid arthritis, skin ulcers, sports injuries, and wrinkled skin, or in promoting muscle growth or weight loss81. The lack of effectiveness of dietary hydroxyproline is probably a consequence of its failure to be incorporated into collagen: only proline is bioavailable for this purpose. Proline only becomes hydroxylated during a later stage of collagen formation in order to facilitate the strengthening of the collagen helix. Once a collagen helix forms, it does so irreversibly in mammals82. The ambiguous role of dietary hydroxyproline, along with the positive association with higher CHD risk that we observed in EWAS, emphasizes the need for exploring the metabolic role that this amino acid plays in health and disease. A potential mechanism that can explain the positive association between hydroxyproline consumption and CHD risk is its metabolic reaction with succinate and CO2, producing 2-oxoglutarate. Chen et al.83 showed that increased serum 2-oxoglutarate is associated with high myocardial energy expenditure and poor prognosis in chronic heart failure patients.
Validation in NHS II
In the second phase of our study, we used NHS II in order to validate statistically significant associations that we found in the original NHS. During 20 years of follow-up in NHS II, 90,861 participants were followed and 604 CHD incidents were documented (Supplementary Methods 3.1). We examined the relationship between 53 exposures found in NHS with CHD risk and deemed an exposure tentatively validated if it had achieved a false discovery rate (FDR) <0.05 significance in NHS and achieved nominal statistical significance in NHS II (P value < 0.05). Tentatively validated exposures in NHS II had the same directional association with CHD risk as in the original NHS (Table 2). A list of validated and non-validated associations is provided in Supplementary Table 5.
Table 2.
Validation in NHS II.
| Type | Exposure | Effect size | SE (effect size) | Hazard ratio | 95% CI | P value of PH | VIF | P value |
|---|---|---|---|---|---|---|---|---|
| Nutrient | Cereal fiber | −0.28 | 0.06 | 0.75 | (0.68, 0.84) | 0.7 | 1.62 | 2.70E–07 |
| Nutrient | Total manganese | −0.28 | 0.06 | 0.76 | (0.68, 0.85) | 0.32 | 1.68 | 5.82E–07 |
| Nutrient | Alcohol | −0.21 | 0.04 | 0.81 | (0.74, 0.88) | 0.3 | 1.12 | 1.06E–06 |
| Nutrient | Beta-tocotrienol | −0.25 | 0.05 | 0.78 | (0.70, 0.86) | 0.56 | 1.39 | 1.92E–06 |
| Nutrient | Alpha-tocotrienol | −0.25 | 0.05 | 0.78 | (0.70, 0.87) | 0.84 | 1.52 | 3.64E–06 |
| Nutrient | Dietary manganese | −0.28 | 0.06 | 0.76 | (0.68, 0.85) | 0.74 | 1.96 | 3.72E–06 |
| Nutrient | Added bran from wheat, rice, etc. | −0.21 | 0.05 | 0.81 | (0.74, 0.89) | 0.79 | 1.13 | 5.86E–06 |
| Food | Cold breakfast cereal | −0.2 | 0.05 | 0.82 | (0.74, 0.89) | 0.16 | 1.11 | 1.18E–05 |
| Nutrient | Dietary folate | −0.25 | 0.06 | 0.78 | (0.69, 0.88) | 0.08 | 2.03 | 3.50E–05 |
| Nutrient | Natural bran | −0.2 | 0.05 | 0.82 | (0.75, 0.90) | 0.73 | 1.25 | 3.62E–05 |
| Nutrient | Carb from milled wholegrain | −0.2 | 0.05 | 0.82 | (0.75, 0.90) | 0.69 | 1.26 | 3.90E–05 |
| Nutrient | Stearic acid | 0.28 | 0.07 | 1.32 | (1.15, 1.51) | 0.45 | 2.64 | 6.26E–05 |
| Nutrient | Carb from wholegrain | −0.19 | 0.05 | 0.83 | (0.75, 0.91) | 1 | 1.28 | 6.47E–05 |
| Food | Salad/oil and vinegar dressing | −0.16 | 0.05 | 0.85 | (0.78, 0.93) | 0.15 | 1.17 | 3.41E–04 |
| Food | Raw carrots | −0.17 | 0.05 | 0.84 | (0.77, 0.93) | 0.93 | 1.14 | 4.02E–04 |
| Food | Red wine | −0.18 | 0.05 | 0.84 | (0.76, 0.93) | 0.72 | 1.07 | 7.00E–04 |
| Nutrient | Phytate | −0.21 | 0.06 | 0.81 | (0.71, 0.92) | 0.34 | 2.18 | 9.66E–04 |
| Nutrient | Beta-tocopherol | −0.21 | 0.06 | 0.81 | (0.71, 0.92) | 0.9 | 2.08 | 1.01E–03 |
| Nutrient | Apigenin | −0.15 | 0.04 | 0.86 | (0.79, 0.94) | 0.86 | 1.2 | 1.07E–03 |
| Nutrient | Supplemental or fortified folic acid | −0.17 | 0.05 | 0.85 | (0.77, 0.94) | 0.03 | 1.41 | 1.38E–03 |
| Nutrient | Discretionary solid fat | 0.21 | 0.07 | 1.23 | (1.08, 1.41) | 0.72 | 2.46 | 1.49E–03 |
| Nutrient | Natural germ | −0.14 | 0.05 | 0.87 | (0.79, 0.95) | 0.18 | 1.27 | 2.42E–03 |
| Nutrient | Total saturated fat | 0.22 | 0.07 | 1.25 | (1.08, 1.44) | 0.65 | 3.04 | 2.88E–03 |
| Nutrient | Trans 16:1 | 0.17 | 0.06 | 1.19 | (1.06, 1.33) | 0.47 | 2.06 | 3.27E–03 |
| Nutrient | Palmitic acid | 0.23 | 0.08 | 1.25 | (1.08, 1.46) | 0.94 | 3.31 | 3.47E–03 |
| Food | Beverages with sugar | 0.12 | 0.04 | 1.12 | (1.04, 1.22) | 0.29 | 1.11 | 4.38E–03 |
| Food | White wine | −0.14 | 0.05 | 0.87 | (0.79, 0.96) | 0.83 | 1.07 | 4.40E–03 |
| Nutrient | Synthetic vitamin B6 | −0.13 | 0.05 | 0.88 | (0.80, 0.96) | 0.16 | 1.08 | 4.92E–03 |
| Nutrient | Trans 18:1 | 0.15 | 0.06 | 1.16 | (1.04, 1.29) | 0.17 | 1.71 | 7.17E–03 |
| Nutrient | Supplemental selenium | −0.12 | 0.05 | 0.89 | (0.81, 0.97) | 0.09 | 1.28 | 7.41E–03 |
| Nutrient | Palmitoleic acid | 0.16 | 0.06 | 1.18 | (1.04, 1.33) | 0.77 | 2.19 | 9.24E–03 |
| Nutrient | Animal fat | 0.16 | 0.06 | 1.18 | (1.04, 1.33) | 0.97 | 2.23 | 1.03E–02 |
| Nutrient | Animal MUFA | 0.15 | 0.06 | 1.16 | (1.03, 1.31) | 0.67 | 2.03 | 1.18E–02 |
| Food | Hotdog | 0.12 | 0.05 | 1.12 | (1.03, 1.23) | 0.75 | 1.1 | 1.18E–02 |
| Food | Raisins or grapes | −0.12 | 0.05 | 0.89 | (0.80, 0.98) | 0.28 | 1.08 | 1.90E–02 |
| Nutrient | Hydroxyproline | 0.12 | 0.05 | 1.12 | (1.01, 1.25) | 0.15 | 1.55 | 3.22E–02 |
| Food | Yogurt | −0.09 | 0.05 | 0.91 | (0.83, 1.00) | 0.14 | 1.1 | 3.95E–02 |
From 53 statistically significant exposures found in NHS, 37 were validated in NHS II. P values are associated with two-sided Wald tests.
Discussion
Our analysis of the dietary determinants of CHD has several limitations based on the nature of the data we used in our analysis. First, the study subjects are only women with a specific occupation (nurses), which restricts the generalizability of the findings to populations comprising males, as well as to more heterogeneous occupational groups and socio-economic backgrounds (Supplementary Figs. 4 and 5). Second, the present study only focused on the effect of dietary factors on CHD risk. Even though diet is an important part of an individual’s environmental exposure, it does not cover the entire exposome84. The environment also includes persistent organic pollutants, plastic-associated chemicals, bacterial and viral infections, air quality, stress, and social network effects85, as well as the endogenous microbiome. Moreover, our diet is not limited to nutrient content; it also carries food additives and other chemicals added during the packaging process, which are absent in the food composition databases, and hence are not included in this analysis. Including these chemicals is necessary for a more comprehensive picture of the effect of the diet on health86,87. The only way to overcome these limitations is to include more environmental factors, offering a more comprehensive understanding of the global environment’s effects on health and disease. Moreover, the FFQ used in NHS covers a number of food items that includes the large majority of those consumed by Americans, but the diet of some participants may not be completely represented. Third, while we included the confounding variables that were previously used in other studies on CHD relying on NHS data, our study remains limited to the common confounding variables usually considered when exploring diet–CHD associations. Hence, residual confounding by unmeasured variables cannot be excluded. The obtained results do not unveil causal effects, but, rather, help us generate new hypotheses, which need to be examined in more detail in these and other prospective cohorts and experimental studies. We must also investigate carefully and mechanistically the influence of these dietary factors on human metabolism, exposures that require detailed measurements in terms of dietary bioavailability, hence they can serve as targets for further investigation for mechanism-based analysis.
Our overall goal was to apply GWAS-like analytical approaches to study the dietary determinants of CHD. The methodology allowed us to explore both food items and nutrients, offering a more comprehensive picture of the effect of diet on CHD and helping us visualize the obtained relationships using network tools. Our study not only reproduced the prior knowledge in the diet–CHD domains, but also led to novel associations. While some of the previous EWAS studies failed to achieve adequate statistical power in association detection19,20, our positive results suggest that these failures were often related to the cohort size and the absence of repeated longitudinal dietary assessments. Indeed, our use of a large longitudinal dataset with a long follow-up period and a sufficient number of subjects helped us achieve sufficient statistical power to detect even relatively small effect sizes. However, enabling a wide-association study to investigate environmental factors requires careful consideration in designing cohort studies, and detailed, comprehensive exposure assessment methods to ensure that the effect of the environment is fully captured. While selectively testing and reporting one or a few associations has been argued to be a source of biased results and false positives88,89, there is clearly a role for testing specific etiologic hypotheses as this allows greater statistical power and a more detailed examination of an exposure–outcome relationship. An environment-wide association study is a complementary approach that allows us to rank the associations and report transparently both significant and non-significant associations. It also allowed us to generate new hypotheses that can be further investigated in single-association studies and mechanism-based studies. It is worth mentioning that until recently NIH was unlikely to fund research proposals without well-developed hypotheses, restricting the possibility of conducting wide-association studies and this analysis was only possible because of the accrual of over 30 years of follow-up in this large cohort.
In the present study, we explored the effect of only 374 dietary exposures. Yet, when it comes to the chemical composition of the food we consume, these nutritional components represent only a tiny fraction of the thousands of distinct definable biochemicals that have been identified in foods90. While many of these chemicals have well-documented or potential implications for health, they remain largely unquantified in any systematic fashion across different individual foods. Their invisibility to experimental, clinical, epidemiological, and demographic studies—turning them into the virtual dark matter of nutrition research—represents a roadblock toward a better, more consistent, more reproducible understanding of how diet affects health91,92. In the high-resolution diet description space, the conventional single-association approach is even more impractical and lacks scalability. The EWAS methodology, however, would be able to test higher order of magnitude of dietary compounds, to identify significant associations with a disease of interest or with a prescription for health.
Methods
Knowledge graph
To create the knowledge graph, we firstly identified in PubMed all papers that have NHS or Health Professionals Follow-up Study in the title or abstract, along with papers co-authored by the main PIs of the NHS. We manually filtered papers that studied the association between dietary exposures and cardiovascular complications, such as coronary heart disease, stroke, and hypertension. Since not all papers are indexed on PubMed, we searched the web using the same criteria to find the remaining papers. Next, we manually examined the abstracts of the obtained papers and extracted the exposure–phenotype relations, the associations found, the effect size, and other related information (Table 3). More than one association might be studied in a paper. Overall, we found 292 studied associations documented in 91 papers, altogether 124 negative and 45 positive associations were documented in relation to cardiovascular complications. In the remaining cases, there was no significant association between an exposure and a phenotype of study. The obtained data are shown in a knowledge graph (Fig. 1) where each link represents an association. The space of studied exposures is rather heterogeneous and is often driven by the researcher’s interests and experience. For example, the effects of some nutrients were studied with respect to replacement with other nutrients, such as the effect of replacing trans-fat with MUFAs. In some cases, the intake ratio of two nutrients, for example, the ratio of polyunsaturated fat to trans-fat, or of two food items was examined. Moreover, according to the exposure of interest, the set of adjusting variables used to account for confounding effects varied from one study to another. The raw data and code used for constructing the knowledge graph are available at ref. 93.
Table 3.
Knowledge graph data preparation.
| PubMed ID | Year | Title | Abstract | Exposure | Phenotype | Gender | Association | Model | Effect size |
|---|---|---|---|---|---|---|---|---|---|
| 29529162 | 2018 | Carbohydrate quality and quantity and risk of coronary heart disease among us women and men | ... We aimed to assess the relation between various measures of carbohydrate quality and incident CHD. Data on diet and lifestyle behaviors were prospectively collected on 75,020 women and 42,865 men participating in the Nurses’ Health Study (NHS) and the Health Professionals Follow-Up Study (HPFS) starting in 1984 and 1986, respectively, and every 2–4 years thereafter until 2012 ... In models adjusted for age, lifestyle behaviors, and dietary variables, the highest quintile of carbohydrate intake was not associated with incident CHD (pooled RR = 1.04; 95% CI: 0.96, 1.14; P trend = 0.31). Total fiber intake was not associated with risk of CHD (pooled RR = 0.94; 95% CI: 0.85, 1.03; P trend = 0.72), while cereal fiber was associated with a lower risk for incident CHD (pooled RR = 0.80; 95% CI: 0.74, 0.87; P trend <0.0001). In fully adjusted models, the carbohydrate-to-total fiber ratio was not associated with incident CHD (pooled RR = 1.04; 95% CI: 0.96, 1.13; P trend = 0.46). However, the carbohydrate-to-cereal fiber ratio and the starch-to-cereal fiber ratio were associated with an increased risk for incident CHD (pooled RR = 1.20; 95% CI: 1.11, 1.29; P trend <0.0001, and pooled RR = 1.17; 95% CI: 1.09, 1.27; P trend <0.0001)...59 | Total fiber | CHD | Both | No association | Cox | – |
| Cereal fiber | CHD | Both | Negative | Cox | 0.8 | ||||
| Ratio of carb to total fiber | CHD | Both | No association | Cox | – | ||||
| Ratio of carb to cereal fiber | CHD | Both | Positive | Cox | 1.2 |
Population
Using the year 1986 as the baseline because the dietary questionnaires have been unchanged since, we followed women who were healthy and free of chronic diseases up to 2014. In the baseline year, participants with a history of CVD, diabetes mellitus, and cancer were excluded. We also excluded women whose demographic data were missing, whose reported average energy intake was <600 or >3500 kcal/day, or left >70 questions in the FFQ unanswered10,94–97. Participants received one questionnaire every 2 years to report their medical data and one questionnaire every 4 years to document their dietary data. At any point within the follow-up period, if a participant reported development of non-fatal myocardial infarction (MI) or fatal CHD98–100, she will be classified as a case, with no further update of her dietary records. If she developed other diseases, such as diabetes mellitus or cancer, she would still be classified as a non-case, with no further update of her dietary records (Supplementary Methods 3.1 and Supplementary Fig. 1). These exclusion criteria were chosen by virtue of minimizing reverse causation bias and reducing the impact of measurement errors and missing data. In total, we included 62,811 subjects in the analysis, representing 2774 cases (4%) and 60,037 controls (96%).
Ascertainment of diet
NHS uses an internally designed FFQ, with documented reproducibility and validity10,101,102. The FFQ has been regularly updated to adapt to changes in the food market and to capture additional food items103. For each food item, the FFQ specified a commonly used unit or portion size, asking each subject how often, on average, she had consumed that quantity during the past year104. Nine responses were possible, ranging from “almost never” to “six or more times per day.” We converted the frequency responses to the number of servings per day for each food item. We calculated daily intake of nutrients by multiplying the frequency of consumption of each item by its nutrient content and summing the nutrient contributions of all foods on the basis of Harvard University Food Composition Database derived from US Department of Agriculture sources105 and other resources, including published reports, data from manufacturers, and in-house analyses of fatty acid composition106. We looked into several food items more closely. For example, we used an algorithm designed by Jacobs et al.107 to classify breakfast cereals into wholegrain and refined grain. We also collected detailed information on the type of fat or oil used in food preparation and brand or type of margarines to calculate the fatty acid consumption.
Ascertainment of CHD
We ascertained incident cases of CHD (non-fatal MI or fatal CHD) that occurred after the return of the 1986 questionnaire but before June 1, 2014. Physicians, unaware of the self-reported risk factor status, systematically reviewed the medical records of those who reported having an MI on each biennial questionnaire. MI was classified as confirmed if the World Health Organization criteria, that is, symptoms, electrocardiographic changes, or elevated cardiac enzyme concentrations, were met108. Fatal CHD was confirmed by either hospital records or through an autopsy if CHD was listed as the cause of death on the death certificate, if it was listed as an underlying and most plausible cause of death, or if evidence of previous CHD was available. Deaths were identified from state vital statistics records and the National Death Index, or were reported by the families and the postal system47.
Statistical analysis
Figure 2a shows a brief snapshot of the statistical approaches used in this paper. We used the extended Cox model for time-dependent variables to associate each exposure with the time to occurrence of CHD. The underlying time for the Cox model is the time on study for each participant. We used the cumulative average (Supplementary Methods 3.2) of the food intakes from baseline to the start of each 2-year follow-up interval, which represents the long-term habitual intake and reduces random within-person variation10,109–116 (for analyses in which the time-dose effects are taken into account see Supplementary Table 4 and Supplementary Fig. 6). We adjusted the analyses for potential risk factors and confounders, including age (Supplementary Fig. 2), BMI, physical activity, and total caloric intake as continuous covariates; and ethnicity, smoking status, multivitamin use, vitamin E supplement use, post-menopausal hormone use, aspirin use, high blood pressure117, elevated cholesterol118, and family history of MI and high blood pressure as categorical variables. We selected the set of confounding variables based on their potential effects on both exposures and the outcome. Dietary exposures entered the analysis as continuous variables. We used Box–Cox transformation to stabilize the variance and improve the validity of measures of association. Later, the exposures were z-transformed in order to compare the effect sizes from many regressions.
To examine the validity of the EWAS results, we assessed the proportionality assumption for each test. We also tested whether there was severe multicollinearity among the variables in each test by calculating the VIF, which can potentially make effect size estimates unstable, reduce or eliminate statistical power, and cause the coefficients to switch signs119. Ultimately, to control for type I error due to multiple hypotheses testing, we calculated the FDR, the estimated proportion of false discoveries made versus the number of real discoveries at a given significance level120 (Supplementary Methods 3.3). To estimate the number of false discoveries, we created a null distribution of Cox model P values by randomly shuffling the CHD status 1000 times and recomputing the P values. Accordingly, we estimated the FDR to be the ratio of the proportion of results that were called significant at a given level α in the null distribution and the proportion of results called significant from real tests. Since in the FDR estimation, we utilize the data themselves, we naturally consider the correlated structure of the data, given the intrinsic dependencies among dietary factors121. Since the confounding effect of the adjusting covariates on CHD risk exists, certain subjects have greater odds of developing CHD. Therefore, we maintained the confounding role of the adjusting covariates in each permuted dataset while the association between the exposure and CHD has been eliminated122. We used Cox regression to estimate the odds of developing CHD as a function of adjusting covariates. Next, we permuted the CHD cases among the subjects as taking a random sample from a biased pool. Furthermore, we re-ran the analyses and calculated the null P values. Repeating this procedure 1000 times, we measured the FDR as the ratio of the proportion of results that were called significant at a given level α in the null distribution to a proportion of results called significant from our real tests.
Study protocol
The study protocol was approved by the institutional review board (IRB) of the Brigham and Women’s Hospital, and the IRB allowed participants’ completion of questionnaires to be considered as implied consent. Written informed consent was obtained from participants to release medical records documenting the incidence of coronary heart disease.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Acknowledgements
We were supported by grants from NIH (grants P01 HL132825, UM1 CA186107, P01 CA87969, R01 CA49449, R01 HL034594, R01 HL088521, UM1 CA176726, R01 CA67262, U54 HL119145, U01 HG007690, and P50 GM107618) and AHA (grants 151708, 414110-68953, and D700382). A.-L.B. was supported by NIH 1P01HL132825, Rockefeller Foundation 2109 FOD 026, and the European Union’s Horizon 2020 research and innovation programme under grant agreement No 810115 - DYNASNET.
Source data
Author contributions
S.M. performed data query and integration, statistical modeling, network analysis, and programming and contributed to writing the manuscript. G.M. contributed to network analysis, statistical modeling, programming, and writing the manuscript. Y.L. contributed to data query and programming. J.L. contributed to interpreting the results and writing the manuscript. W.C.W. contributed to data collection, analyzing the results, and writing the manuscript. A.-L.B. contributed to the conceptual design of the study and writing the manuscript.
Data availability
The authors declare that all data supporting the findings of this study are available upon request to Nurses’ Health Study (NHS) and when the request for data access is approved. Access is restricted due to participant confidentiality and privacy concerns. Individuals who want to request access to NHS data must first submit an online request form. If the project is approved, completion of a data use agreement, completion of CITI training demonstrating ethical training in using human subjects’ data, and a small provision of funds to support the computing system will also be required. Further information including the procedures to obtain and access data from the NHS is described in ref. 123 (contact email: nhsaccess@channing.harvard.edu). The Food Frequency Questionnaires used in NHS are available in ref. 104. Harvard University Food Composition Database can be accessed in ref. 106. Source data are provided with this paper.
Code availability
The programming materials are available on GitHub and Zenodo platforms93. R version 3.4.0 was used for data analysis and Python version 2.7.16 and MATLAB 2019a were used for data visualizations.
Competing interests
A.-L.B. is founder of Nomix and Foodome, and J.L. and A.-L.B. are founders of Scipher Medicine, companies that explore the use of network-based tools in health. The remaining authors declare no competing interests.
Footnotes
Peer review information Nature Communications thanks Ramon Estruch, Paolo Vineis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Soodabeh Milanlouei, Giulia Menichetti.
Supplementary information
Supplementary information is available for this paper at 10.1038/s41467-020-19888-2.
References
- 1.Siscovick DS, et al. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA. 1995;274:1363–1367. doi: 10.1001/jama.1995.03530170043030. [DOI] [PubMed] [Google Scholar]
- 2.Estruch R, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 3.Li S, et al. Better diet quality and decreased mortality among myocardial infarction survivors. JAMA Intern. Med. 2013;173:1808–1819. doi: 10.1001/jamainternmed.2013.9768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Archiv. Intern. Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 5.Division for Heart Disease and Stroke Prevention. Heart Disease and Stroke Mapswww.cdc.gov/dhdsp/maps (2016).
- 6.Robertson TL, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: coronary heart disease risk factors in Japan and Hawaii. Am. J. Cardiol. 1977;39:244–249. doi: 10.1016/S0002-9149(77)80198-7. [DOI] [PubMed] [Google Scholar]
- 7.Capuano, E., Oliviero, T. & van Boekel, M. A. Modeling food matrix effects on chemical reactivity: challenges and perspectives. Crit. Rev. Food Sci. Nutr.58, 1–15 (2017). [DOI] [PubMed]
- 8.Kolonel LN, Yoshizawa CN, Hankin JH. Diet and prostatic cancer: a case-control study in Hawaii. Am. J. Epidemiol. 1988;127:999–1012. doi: 10.1093/oxfordjournals.aje.a114903. [DOI] [PubMed] [Google Scholar]
- 9.Marchand LL, Hankin JH, Kolonel LN, Wilkens LR. Vegetable and fruit consumption in relation to prostate cancer risk in Hawaii: a reevaluation of the effect of dietary beta-carotene. Am. J. Epidemiol. 1991;133:215–219. doi: 10.1093/oxfordjournals.aje.a115865. [DOI] [PubMed] [Google Scholar]
- 10.Willett, W. Nutritional Epidemiology (Oxford Univ. Press, 2012).
- 11.Cespedes EM, Hu FB. Dietary patterns: from nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015;101:899–900. doi: 10.3945/ajcn.115.110213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Shimazu T, et al. Dietary patterns and cardiovascular disease mortality in Japan: a prospective cohort study. Int. J. Epidemiol. 2007;36:600–609. doi: 10.1093/ije/dym005. [DOI] [PubMed] [Google Scholar]
- 14.Tapsell LC, Neale EP, Satija A, Hu FB. Foods, nutrients, and dietary patterns: interconnections and implications for dietary guidelines. Adv. Nutr. 2016;7:445–454. doi: 10.3945/an.115.011718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel CJ, Bhattacharya J, Butte AJ. An environment-wide association study (EWAS) on type 2 diabetes mellitus. PLoS ONE. 2010;5:e10746. doi: 10.1371/journal.pone.0010746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wulaningsih W, et al. Investigating nutrition and lifestyle factors as determinants of abdominal obesity: an environment-wide study. Int. J. Obes. 2017;41:340. doi: 10.1038/ijo.2016.203. [DOI] [PubMed] [Google Scholar]
- 17.Merritt MA, et al. Investigation of dietary factors and endometrial cancer risk using a nutrient-wide association study approach in the EPIC and Nurses’ Health Study (NHS) and NHS II. Cancer Epidemiol. Prev. Biomarkers. 2015;24:466–471. doi: 10.1158/1055-9965.EPI-14-0970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forman, J. P. & Willett, W. C. Nutrient-wide association studies: another road to the same destination. Circulation126, 2447–2448 (2012). [DOI] [PubMed]
- 19.Tzoulaki I, et al. A nutrient-wide association study on blood pressure. Circulation. 2012;126:2456–2464. doi: 10.1161/CIRCULATIONAHA.112.114058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGinnis DP, Brownstein JS, Patel CJ. Environment-wide association study of blood pressure in the national health and nutrition examination survey (1999–2012) Scientific Rep. 2016;6:30373. doi: 10.1038/srep30373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mubarak A, Hodgson JM, Considine MJ, Croft KD, Matthews VB. Supplementation of a high-fat diet with chlorogenic acid is associated with insulin resistance and hepatic lipid accumulation in mice. J. Agric. Food Chem. 2013;61:4371–4378. doi: 10.1021/jf400920x. [DOI] [PubMed] [Google Scholar]
- 22.Onakpoya, I., Terry, R. & Ernst, E. The use of green coffee extract as a weight loss supplement: a systematic review and meta-analysis of randomised clinical trials. Gastroenterol. Res. Pract. 2011, 382852 (2011). [DOI] [PMC free article] [PubMed]
- 23.Vogel RA, Corretti MC, Plotnick GD. The postprandial effect of components of the Mediterranean diet on endothelial function. J. Am. College Cardiol. 2000;36:1455–1460. doi: 10.1016/S0735-1097(00)00896-2. [DOI] [PubMed] [Google Scholar]
- 24.Sudlow C, et al. Uk biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779. doi: 10.1371/journal.pmed.1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen Z, et al. China kadoorie biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 2011;40:1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colditz GA. The Nurses’ Health Study: a cohort of us women followed since 1976. J. Am. Med. Women’s Assoc. 1995;50:40. [PubMed] [Google Scholar]
- 27.Colditz GA, Manson JE, Hankinson SE. The Nurses’ Health Study: 20-year contribution to the understanding of health among women. J. Women’s Health. 1997;6:49–62. doi: 10.1089/jwh.1997.6.49. [DOI] [PubMed] [Google Scholar]
- 28.Colditz GA, Hankinson SE. The Nurses’ Health Study: lifestyle and health among women. Nat. Rev. Cancer. 2005;5:388. doi: 10.1038/nrc1608. [DOI] [PubMed] [Google Scholar]
- 29.Willett WC, et al. Intake of trans fatty acids and risk of coronary heart disease among women. Lancet. 1993;341:581–585. doi: 10.1016/0140-6736(93)90350-P. [DOI] [PubMed] [Google Scholar]
- 30.Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am. J. Clin. Nutr. 2003;77:1146–1155. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 31.Mozaffarian D, Clarke R. Quantitative effects on cardiovascular risk factors and coronary heart disease risk of replacing partially hydrogenated vegetable oils with other fats and oils. Eur. J. Clin. Nutr. 2009;63:S22. doi: 10.1038/sj.ejcn.1602976. [DOI] [PubMed] [Google Scholar]
- 32.Chiuve SE, et al. Dietary and plasma magnesium and risk of coronary heart disease among women. J. Am. Heart Assoc. 2013;2:e000114. doi: 10.1161/JAHA.113.000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wolk A, et al. Long-term intake of dietary fiber and decreased risk of coronary heart disease among women. JAMA. 1999;281:1998–2004. doi: 10.1001/jama.281.21.1998. [DOI] [PubMed] [Google Scholar]
- 34.Pereira MA, et al. Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch. Intern. Med. 2004;164:370–376. doi: 10.1001/archinte.164.4.370. [DOI] [PubMed] [Google Scholar]
- 35.Mukamal KJ, et al. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N. Engl. J. Med. 2003;348:109–118. doi: 10.1056/NEJMoa022095. [DOI] [PubMed] [Google Scholar]
- 36.Estruch R, et al. Moderate consumption of red wine, but not gin, decreases erythrocyte superoxide dismutase activity: a randomised cross-over trial. Nutr. Metab. Cardiovasc. Dis. 2011;21:46–53. doi: 10.1016/j.numecd.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Millwood IY, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in china. Lancet. 2019;393:1831–1842. doi: 10.1016/S0140-6736(18)31772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holmes MV, et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2014;349:g4164. doi: 10.1136/bmj.g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu FB, et al. Dietary intake of α-linolenic acid and risk of fatal ischemic heart disease among women. Am. J. Clin. Nutr. 1999;69:890–897. doi: 10.1093/ajcn/69.5.890. [DOI] [PubMed] [Google Scholar]
- 40.Rice BH. Dairy and cardiovascular disease: a review of recent observational research. Curr. Nutr. Rep. 2014;3:130–138. doi: 10.1007/s13668-014-0076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Djoussé L, Gaziano JM. Breakfast cereals and risk of heart failure in the physicians’ health study I. Arch. Intern. Med. 2007;167:2080–2085. doi: 10.1001/archinte.167.19.2080. [DOI] [PubMed] [Google Scholar]
- 42.Gaziano JM, et al. A prospective study of consumption of carotenoids in fruits and vegetables and decreased cardiovascular mortality in the elderly. Ann. Epidemiol. 1995;5:255–260. doi: 10.1016/1047-2797(94)00090-G. [DOI] [PubMed] [Google Scholar]
- 43.Puglisi MJ, et al. Raisins and additional walking have distinct effects on plasma lipids and inflammatory cytokines. Lipids Health Dis. 2008;7:14. doi: 10.1186/1476-511X-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hu FB, et al. Frequent nut consumption and risk of coronary heart disease in women: prospective cohort study. BMJ. 1998;317:1341–1345. doi: 10.1136/bmj.317.7169.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Micha R, Michas G, Mozaffarian D. Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—an updated review of the evidence. Curr. Atheroscler. Rep. 2012;14:515–524. doi: 10.1007/s11883-012-0282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pase MP, Grima N, Cockerell R, Pipingas A. Habitual intake of fruit juice predicts central blood pressure. Appetite. 2015;84:68–72. doi: 10.1016/j.appet.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 47.Fung TT, et al. Sweetened beverage consumption and risk of coronary heart disease in women. Am. J. Clin. Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sieri S, et al. Dietary glycemic load and index and risk of coronary heart disease in a large italian cohort: the epicor study. Arch. Intern. Med. 2010;170:640–647. doi: 10.1001/archinternmed.2010.15. [DOI] [PubMed] [Google Scholar]
- 49.Connor WE, Connor SL. Dietary cholesterol and coronary heart disease. Curr. Atherosclerosis Rep. 2002;4:425–432. doi: 10.1007/s11883-002-0046-y. [DOI] [PubMed] [Google Scholar]
- 50.Mozaffarian D, Aro A, Willett WC. Health effects of trans-fatty acids: experimental and observational evidence. Eur. J. Clin. Nutr. 2009;63:S5. doi: 10.1038/sj.ejcn.1602973. [DOI] [PubMed] [Google Scholar]
- 51.Sun Q, et al. A prospective study of trans fatty acids in erythrocytes and risk of coronary heart disease. Circulation. 2007;115:1858–1865. doi: 10.1161/CIRCULATIONAHA.106.679985. [DOI] [PubMed] [Google Scholar]
- 52.Zong G, et al. Intake of individual saturated fatty acids and risk of coronary heart disease in us men and women: two prospective longitudinal cohort studies. BMJ. 2016;355:i5796. doi: 10.1136/bmj.i5796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zong G, et al. Monounsaturated fats from plant and animal sources in relation to risk of coronary heart disease among us men and women. Am. J. Clin. Nutr. 2018;107:445–453. doi: 10.1093/ajcn/nqx004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Djoussé L, Weir NL, Hanson NQ, Tsai MY, Gaziano JM. Plasma phospholipid concentration of cis-palmitoleic acid and risk of heart failureclinical perspective. Circ. Heart Fail. 2012;5:703–709. doi: 10.1161/CIRCHEARTFAILURE.112.967802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hu FB, Manson JE, Willett WC. Types of dietary fat and risk of coronary heart disease: a critical review. J. Am. Coll. Nutr. 2001;20:5–19. doi: 10.1080/07315724.2001.10719008. [DOI] [PubMed] [Google Scholar]
- 56.Li Y, et al. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J. Am. Coll. Cardiol. 2015;66:1538–1548. doi: 10.1016/j.jacc.2015.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wu H, et al. Association between dietary whole grain intake and risk of mortality: two large prospective studies in US men and women. JAMA Intern. Med. 2015;175:373–384. doi: 10.1001/jamainternmed.2014.6283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jensen MK, et al. Intakes of whole grains, bran, and germ and the risk of coronary heart disease in men. Am. J. Clin. Nutr. 2004;80:1492–1499. doi: 10.1093/ajcn/80.6.1492. [DOI] [PubMed] [Google Scholar]
- 59.AlEssa HB, et al. Carbohydrate quality and quantity and risk of coronary heart disease among us women and men. Am. J. Clin. Nutr. 2018;107:257–267. doi: 10.1093/ajcn/nqx060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosique-Esteban N, Guasch-Ferré M, Hernández-Alonso P, Salas-Salvadó J. Dietary magnesium and cardiovascular disease: a review with emphasis in epidemiological studies. Nutrients. 2018;10:168. doi: 10.3390/nu10020168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burk, R. F. in Human and Veterinary Nutrition, Biochemical Aspects of Nutrients, Vol. 30, 88–106 (Karger Publishers, 1978).
- 62.Chen X, et al. Studies on the relations of selenium and keshan disease. Biol. Trace Element Res. 1980;2:91–107. doi: 10.1007/BF02798589. [DOI] [PubMed] [Google Scholar]
- 63.Stranges S, et al. Effects of selenium supplementation on cardiovascular disease incidence and mortality: secondary analyses in a randomized clinical trial. Am. J. Epidemiol. 2006;163:694–699. doi: 10.1093/aje/kwj097. [DOI] [PubMed] [Google Scholar]
- 64.Flores-Mateo G, Navas-Acien A, Pastor-Barriuso R, Guallar E. Selenium and coronary heart disease: a meta-analysis. Am. J. Clin. Nutr. 2006;84:762–773. doi: 10.1093/ajcn/84.4.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aburto NJ, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rimm EB, et al. Folate and vitamin b6 from diet and supplements in relation to risk of coronary heart disease among women. JAMA. 1998;279:359–364. doi: 10.1001/jama.279.5.359. [DOI] [PubMed] [Google Scholar]
- 67.Malinow MR, et al. Reduction of plasma homocyst(e)ine levels by breakfast cereal fortified with folic acid in patients with coronary heart disease. N. Engl. J. Med. 1998;338:1009–1015. doi: 10.1056/NEJM199804093381501. [DOI] [PubMed] [Google Scholar]
- 68.Li G, et al. Circulating tocopherols and risk of coronary artery disease: a systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2016;23:748–757. doi: 10.1177/2047487315595313. [DOI] [PubMed] [Google Scholar]
- 69.Prasad K. Tocotrienols and cardiovascular health. Curr. Pharm. Des. 2011;17:2147–2154. doi: 10.2174/138161211796957418. [DOI] [PubMed] [Google Scholar]
- 70.Jiang Q. Natural forms of vitamin E: metabolism, antioxidant, and anti-inflammatory activities and their role in disease prevention and therapy. Free Radic. Biol. Med. 2014;72:76–90. doi: 10.1016/j.freeradbiomed.2014.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mathur P, Ding Z, Saldeen T, Mehta JL. Tocopherols in the prevention and treatment of atherosclerosis and related cardiovascular disease. Clin. Cardiol. 2015;38:570–576. doi: 10.1002/clc.22422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Montonen J, Knekt P, Järvinen R, Reunanen A. Dietary antioxidant intake and risk of type 2 diabetes. Diabetes Care. 2004;27:362–366. doi: 10.2337/diacare.27.2.362. [DOI] [PubMed] [Google Scholar]
- 73.Shahidi F. Antioxidants in food and food antioxidants. Food/Nahrung. 2000;44:158–163. doi: 10.1002/1521-3803(20000501)44:3<158::AID-FOOD158>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 74.Yang W, et al. Is heme iron intake associated with risk of coronary heart disease? A meta-analysis of prospective studies. Eur. J. Nutr. 2014;53:395–400. doi: 10.1007/s00394-013-0535-5. [DOI] [PubMed] [Google Scholar]
- 75.Gao L, et al. Isorhamnetin protects against cardiac hypertrophy through blocking PI3K–AKT pathway. Mol. Cell. Biochem. 2017;429:167–177. doi: 10.1007/s11010-017-2944-x. [DOI] [PubMed] [Google Scholar]
- 76.Zhang K, Song W, Li D, Jin X. Apigenin in the regulation of cholesterol metabolism and protection of blood vessels. Exp. Ther. Med. 2017;13:1719–1724. doi: 10.3892/etm.2017.4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Laitinen O, Nikkilä E, Kivirikko K. Hydroxyproline in the serum and urine normal values and clinical significance. Acta Med. Scand. 1966;179:275–284. doi: 10.1111/j.0954-6820.1966.tb05459.x. [DOI] [PubMed] [Google Scholar]
- 78.Wheeless, C. R. Wheeless’ Textbook of Orthopaedics (C.R. Wheeless, M.D., 1996).
- 79.Abdelhalim MAK, Siddiqi N, Alhomida A, Al-Ayed MS. The changes in various hydroxyproline fractions in aortic tissue of rabbits are closely related to the progression of atherosclerosis. Lipids Health Dis. 2010;9:26. doi: 10.1186/1476-511X-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Prockop DJ, Sjoerdsma A. Significance of urinary hydroxyproline in man. J. Clin. Invest. 1961;40:843–849. doi: 10.1172/JCI104318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.US Food and Drug Administration. New Dietary Ingredient Notification for N-Acetyl-l-Hydroxyproline (US Food and Drug Administration, 2001).
- 82.Barbul A. Proline precursors to sustain mammalian collagen synthesis. J. Nutr. 2008;138:2021S–2024S. doi: 10.1093/jn/138.10.2021S. [DOI] [PubMed] [Google Scholar]
- 83.Chen P, et al. Increased serum 2-oxoglutarate associated with high myocardial energy expenditure and poor prognosis in chronic heart failure patients. Biochim. Biophys. Acta. 2014;1842:2120–2125. doi: 10.1016/j.bbadis.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 84.Rappaport SM, Smith MT. Environment and disease risks. Science. 2010;330:460–461. doi: 10.1126/science.1192603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N. Engl. J. Med. 2007;357:370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 86.Bouvard V, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16:1599. doi: 10.1016/S1470-2045(15)00444-1. [DOI] [PubMed] [Google Scholar]
- 87.Tonacchera M, et al. Relative potencies and additivity of perchlorate, thiocyanate, nitrate, and iodide on the inhibition of radioactive iodide uptake by the human sodium iodide symporter. Thyroid. 2004;14:1012–1019. doi: 10.1089/thy.2004.14.1012. [DOI] [PubMed] [Google Scholar]
- 88.Ioannidis JP, Loy EY, Poulton R, Chia KS. Researching genetic versus nongenetic determinants of disease: a comparison and proposed unification. Sci. Transl. Med. 2009;1:7ps8–7ps8. doi: 10.1126/scitranslmed.3000247. [DOI] [PubMed] [Google Scholar]
- 89.Boffetta P, et al. False-positive results in cancer epidemiology: a plea for epistemological modesty. J. Natl Cancer Inst. 2008;100:988–995. doi: 10.1093/jnci/djn191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.The Metabolomics Innovation Centre (TMIC). FooDBhttp://foodb.ca (2018).
- 91.Barabási A-L, Menichetti G, Loscalzo J. The Nutritional Dark Matter: the unmapped chemical complexity of our diet. Nat. Food. 2019;1:33–37. doi: 10.1038/s43016-019-0005-1. [DOI] [Google Scholar]
- 92.Hooton, F., Menichetti, G. & Barabási, A.-L. Exploring food contents in scientific literature with FoodMine. Scientific Reports10, (2020) [DOI] [PMC free article] [PubMed]
- 93.Milanlouei, S. & Menichetti, G. soodimilanlouei/EWAS-NHS: v1.0.1 (Version v1.0.1). Zenodo. 10.5281/zenodo.4038928 (2020).
- 94.Michels KB, Willett WC. Self-administered semiquantitative food frequency questionnaires: patterns, predictors, and interpretation of omitted items. Epidemiology. 2009;20:295. doi: 10.1097/EDE.0b013e3181931515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gates MA, et al. A prospective study of dietary flavonoid intake and incidence of epithelial ovarian cancer. Int. J. Cancer. 2007;121:2225–2232. doi: 10.1002/ijc.22790. [DOI] [PubMed] [Google Scholar]
- 96.Conen D, et al. Caffeine consumption and incident atrial fibrillation in women. Am. J. Clin. Nutr. 2010;92:509–514. doi: 10.3945/ajcn.2010.29627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guasch-Ferré M, et al. Nut consumption and risk of cardiovascular disease. J. Am. Coll. Cardiol. 2017;70:2519–2532. doi: 10.1016/j.jacc.2017.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hu FB, et al. Dietary fat intake and the risk of coronary heart disease in women. N. Engl. J. Med. 1997;337:1491–1499. doi: 10.1056/NEJM199711203372102. [DOI] [PubMed] [Google Scholar]
- 99.Hu FB, et al. Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA. 2002;287:1815–1821. doi: 10.1001/jama.287.14.1815. [DOI] [PubMed] [Google Scholar]
- 100.Liu S, et al. Whole-grain consumption and risk of coronary heart disease: results from the Nurses’ Health Study. Am. J. Clin. Nutr. 1999;70:412–419. doi: 10.1093/ajcn/70.3.412. [DOI] [PubMed] [Google Scholar]
- 101.Yuan C, et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am. J. Epidemiol. 2017;187:1051–1063. doi: 10.1093/aje/kwx328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yuan C, et al. Validity of a dietary questionnaire assessed by comparison with multiple weighed dietary records or 24-hour recalls. Am. J. Epidemiol. 2017;185:570–584. doi: 10.1093/aje/kww104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Oh K, Hu FB, Manson JE, Stampfer MJ, Willett WC. Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the Nurses’ Health Study. Am. J. Epidemiol. 2005;161:672–679. doi: 10.1093/aje/kwi085. [DOI] [PubMed] [Google Scholar]
- 104.Harvard, T. H. Chan School of Public Health Nutrition Department. Nurses’ Health Study: Food Frequency Questionnaires. https://www.nurseshealthstudy.org/participants/questionnaires (2020).
- 105.US Department of Agriculture. Composition of Foods, 1976 to 1992. Agricultural Handbook No. 8 Series (Department of Agriculture, Washington, 1989).
- 106.Harvard T.H. Chan School of Public Health Nutrition Department. Harvard University Food Composition Databasehttps://regepi.bwh.harvard.edu/health/nutrition.html (2020).
- 107.Jacobs, D. R., Meyer, K. A., Kushi, L. H. & Folsom, A. R. Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: the Iowa Women’s Health Study. Am. J. Clin. Nutr.68, 248–257 (1998). [DOI] [PubMed]
- 108.Rose, G. A. et al. Cardiovascular Survey Methods, Vol. 56 (WHO, Geneva, 1982).
- 109.Kahn HA, Dawber TR. The development of coronary heart disease in relation to sequential biennial measures of cholesterol in the Framingham study. J. Clin. Epidemiol. 1966;19:611–620. doi: 10.1016/0021-9681(66)90098-1. [DOI] [PubMed] [Google Scholar]
- 110.Larsson SC, Giovannucci E, Wolk A. Coffee consumption and stomach cancer risk in a cohort of Swedish women. Int. J. Cancer. 2006;119:2186–2189. doi: 10.1002/ijc.22105. [DOI] [PubMed] [Google Scholar]
- 111.Kim EH, et al. Dietary fat and risk of postmenopausal breast cancer in a 20-year follow-up. Am. J. Epidemiol. 2006;164:990–997. doi: 10.1093/aje/kwj309. [DOI] [PubMed] [Google Scholar]
- 112.Haring, B. et al. Dietary protein intake and coronary heart disease in a large community based cohort: results from the Atherosclerosis Risk in Communities (ARIC) Study. PLoS ONE9, e109552 (2014). [DOI] [PMC free article] [PubMed]
- 113.Halton TL, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N. Engl. J. Med. 2006;355:1991–2002. doi: 10.1056/NEJMoa055317. [DOI] [PubMed] [Google Scholar]
- 114.Streppel MT, Ocké MC, Boshuizen HC, Kok FJ, Kromhout D. Dietary fiber intake in relation to coronary heart disease and all-cause mortality over 40 y: the Zutphen Study. Am. J. Clin. Nutr. 2008;88:1119–1125. doi: 10.1093/ajcn/88.4.1119. [DOI] [PubMed] [Google Scholar]
- 115.Eshak ES, et al. Soft drink intake in relation to incident ischemic heart disease, stroke, and stroke subtypes in Japanese men and women: the Japan Public Health Centre–based study cohort I. Am. J. Clin. Nutr. 2012;96:1390–1397. doi: 10.3945/ajcn.112.037903. [DOI] [PubMed] [Google Scholar]
- 116.Hu FB, et al. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am. J. Epidemiol. 1999;149:531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 117.Lawes, C. M., Bennett, D. A., Lewington, S. & Rodgers, A. in Seminars in Vascular Medicine, Vol. 2, 355–368 (Thieme Medical Publishers, Inc., New York, 2002). [DOI] [PubMed]
- 118.Huxley, R., Lewington, S. & Clarke, R. in Seminars in Vascular Medicine, Vol. 2, 315–324 (Thieme Medical Publishers Inc., New York, 2002). [DOI] [PubMed]
- 119.Belsley, D. A. in Encyclopedia of Statistical Sciences, Vol. 2 (Wiley, 2004).
- 120.Storey JD, Tibshirani R. Statistical significance for genomewide studies. Proc. Natl Acad. Sci. USA. 2003;100:9440–9445. doi: 10.1073/pnas.1530509100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Noble WS. How does multiple testing correction work? Nat. Biotechnol. 2009;27:1135. doi: 10.1038/nbt1209-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Epstein MP, et al. A permutation procedure to correct for confounders in case-control studies, including tests of rare variation. Am. J. Hum. Genet. 2012;91:215–223. doi: 10.1016/j.ajhg.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Harvard T.H. Chan School of Public Health Nutrition Department. External Collaboration Requesthttps://www.nurseshealthstudy.org/researchers (2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors declare that all data supporting the findings of this study are available upon request to Nurses’ Health Study (NHS) and when the request for data access is approved. Access is restricted due to participant confidentiality and privacy concerns. Individuals who want to request access to NHS data must first submit an online request form. If the project is approved, completion of a data use agreement, completion of CITI training demonstrating ethical training in using human subjects’ data, and a small provision of funds to support the computing system will also be required. Further information including the procedures to obtain and access data from the NHS is described in ref. 123 (contact email: nhsaccess@channing.harvard.edu). The Food Frequency Questionnaires used in NHS are available in ref. 104. Harvard University Food Composition Database can be accessed in ref. 106. Source data are provided with this paper.
The programming materials are available on GitHub and Zenodo platforms93. R version 3.4.0 was used for data analysis and Python version 2.7.16 and MATLAB 2019a were used for data visualizations.