Abstract
This cross-sectional, descriptive study examined unmet social and economic needs and health information requests of low-income, expecting fathers who participated in the First 1000 Days program. The First 1000 Days is a systems-level intervention aiming to prevent obesity among low-income mothers and infants across 3 community health centers in Greater Boston, MA, USA. Fathers who attended their partner’s first prenatal care visit were invited to complete a program survey during early pregnancy. Among 131 fathers surveyed, 45% were white, 21% were Hispanic/Latino, 55% were foreign-born, and 69% reported an annual income under $50 000. Fathers reported elevated levels of food insecurity (18%) and 33% were unaware of someone that could provide a $50 loan; however, over 85% of fathers knew someone that could provide non-financial social support. Fathers requested information about pregnancy, birth preparation, and fatherhood. Findings support addressing fathers’ unmet needs during pregnancy and providing father-specific perinatal information.
Keywords: social determinants of health, fathers, pregnancy, health information needs, obesity
Introduction
Social and economic determinants of health—including economic stability, education, socio-contextual factors, health care access, and neighborhood/built environment factors—have been consistently linked to health behaviors and outcomes during pregnancy, birth, and early childhood.1-5 In the United States, certain social determinants of health (educational attainment, access to prenatal care, and race/ethnicity) are estimated to account for more than 10% of the variance in the average annual maternal mortality rate from 1997 to 2012.4 As policymakers and practitioners have implemented systems-level interventions to address these drivers of health inequality, a burgeoning area of research has emerged highlighting fathers’ roles in promoting healthy pregnancy, childbirth, and child-rearing outcomes,6-12 and general health disparities among men.13 The literature defines a “father” as the male(s) most engaged in the care of a child, regardless of biological relation, marital status, or living arrangement.12 However, little research has investigated how social determinants of health may be associated with health behaviors for new or expecting fathers and may affect fathers’ involvement (ie, caring, communicating, playing, visitation)12 in pregnancy and early childhood. This represents a gap in our understanding of familial factors influencing pregnancy, childbirth, and parenting outcomes.
Systematic reviews of father involvement during pregnancy and maternal health have found that male involvement is associated with reduced odds of maternal depression, higher likelihood of maternal access to health services, more preparedness around birth and birth complications, and better maternal nutrition.14-16 Additionally, having a father present during the first prenatal ultrasound is associated with higher likelihood of full-term pregnancy.6 During infancy, partner support is associated with higher likelihood and longer duration of breastfeeding17 and associations between father-child dietary intake exist as early as 20 months of age.18 During a child’s pre-school years, father involvement can increase children’s physical activity levels.19 In recognition of father’s profound influence on pregnancy and child outcomes, the American Academy of Pediatrics (AAP) advises health care professionals to communicate father’s unique role in modeling physical activity and safe behaviors (ie, seat belt use), ask expecting fathers what parenting skills they are lacking, provide resources to help fathers gain confidence, and promote the use of policies, such as the Family Medical Leave Act.12
Together, these findings suggest that interventions leveraging paternal availability, involvement, and engagement in health behaviors may promote better outcomes for mothers, fathers, and children. Yet, to our knowledge, no studies have described fathers’ unmet social or economic needs—such as housing/food insecurity, underemployment, and limited access to financial or social support—during pregnancy, as well as parenting information they most need during this early and sensitive period of familial transition. As a first step towards addressing these critical gaps in understanding, the current study has 2 exploratory aims. We first describe fathers’ unmet social and economic needs—corresponding to a social determinants of health framework20—during pregnancy in a diverse sample of low-income families. Second, we describe the information that fathers request learning around pregnancy, childbirth, parenting, and their own health behaviors.
Methods
Participants and Procedure
Data in the current study are derived from the First 1000 Days program, a large systems-level intervention aiming to prevent obesity and other chronic diseases among low-income mothers and their infants during pregnancy and the first 2 years of life.21 The intervention followed a Collective Impact approach (CI) through programming that addressed the individual, family, primary care, and community setting: universal screening of adverse health behaviors and social determinants, educational materials, connections to community resources, staff and provider training, and enhanced gestational weight gain and infant overweight tracking.21
A subset of fathers also participated in the program and served as a pilot to demonstrate fathers’ most pressing needs during pregnancy and gauge willingness to participate in future early life fatherhood interventions. Relevant to the current study, program components include surveys regarding fathers’ exposures to economic and social determinants of health and a text-messaging campaign designed to elicit fathers’ interests in learning about pregnancy, childbirth, and parenting. Fathers enrolled in the program by completing a survey when mothers initiated prenatal care at 1 of 3 community health centers in the Greater Boston Area. All 3 community health centers are affiliated with an academic medical center and serve low-income and racial/ethnic minorities. At the mother’s first prenatal care visit, fathers were approached in the waiting room and asked if interested in completing a First 1000 Days survey. Fathers, regardless of biological relation, martial, or residential status, were provided with a study fact sheet and if interested completed the survey on an iPad. Surveys were offered in English, Spanish, and Arabic. The current cross-sectional study is based on self-reports from fathers who completed surveys at study baseline, yielding an analytical sample of 131 mother-father dyads. Surveys were administered from August 2016 to September 2017.
Ethical Approval and Informed Consent
The First 1000 Days study protocol and method for obtaining fathers’ consent was reviewed and approved by the Partners Healthcare Institutional Review Board (2016P000801). At mothers’ initial prenatal care visit, fathers were provided with a study fact sheet/consent explaining that survey completion is voluntary, and that survey data would be used for program evaluation. Fathers completion of the survey served as consent for their data to be used for both clinical and research purposes as approved by the Partners Healthcare Institutional Review Board.
Measures
Unmet social and economic needs
Fathers’ unmet needs were assessed using a self-administered survey. Survey variables were categorized to address key exposures in the Healthy People 2020 social determinants of health framework.20 Unmet needs were grouped into 3 main areas: health care access, economic stability, social support, and health information. Health care access was assessed using a single-item question developed by the CDC’s Pregnancy Risk Assessment Monitory System (PRAMS)22 asking if the individual had visited a primary care provider in the 12 months prior to pregnancy.
Economic stability was measured using 2, 2-item screeners to assess housing and food insecurity, and single-item questions assessing employment, income, and enrollment in the Supplemental Nutrition Assistance Program (SNAP). The measure of housing insecurity was adopted from the National Survey of American Families,23 and asks fathers to report whether in the last 12 months, (1) there was a time when they were not able to pay the mortgage, bills, or rent and if, (2) there was a time when they or their children moved in with others because they could not pay mortgage, bills, or rent. If a father responded yes to either question, they were categorized as housing insecure. The food security screener was validated and adopted by the AAP for use in clinical settings.24 Two items asked fathers if, in the last 12 months, (1) they were worried about whether food would run out before they had money to buy more, and if, (2) the food they bought didn’t last and they didn’t have money to buy more. Fathers responding often true or sometimes true to either question were categorized as food insecure. In addition, a single-item question asked fathers if they currently received SNAP benefits. A single-item demographic question asked fathers to select if, within the past 12 months, they were mostly employed full-time (more than 35 hours/week), part-time (<35 hours/week), not employed (not looking for work), not employed (looking for work), or a student. Responses were categorized as employed full-time, employed part-time, or unemployed.
Social support was assessed with single-item questions measuring the following: perceived partner support, social isolation, emotional support, illness support, instrumental support, and marital status. Perceived partner support was measured using the Turner Support Scale,25 a single, Likert-scaled item asking fathers the degree to which they agreed with the statement: “I can count on my partner to be there when I need him/her.” Responses of strongly agree or agree indicated high perceived partner support, and responses of neutral, disagree, or strongly disagree indicated medium or low support. Social isolation was measured using the Berman-Syme Social Network Index, which has been used previously to construct measures of social isolation for participants in the National Health and Nutrition Examination Survey (NHANES III).26,27 Fathers were asked, “In a typical week, how many times do you talk on the telephone with or text your family, friends, or neighbors?” Response options included less than once per week, 1 to 2 times per week, 3 to 6 times per week, every day, or 2 or more times per day. Fathers indicating that they spoke with others less than 1 to 2 times per week were categorized as experiencing high levels of social isolation. Emotional support and illness support were each assessed with single-item, dichotomous yes/no response options. Emotional support was indexed by reporting they had someone to talk with about their problems, and illness support by having someone to help if they were sick and needed to be in bed. Instrumental support was assessed with 2 items in the same format, asking whether the participant had someone to take them to a clinic or doctor’s office if they need a ride, and whether they had someone who could loan them $50. These 4 dichotomous items measuring emotional, illness, and instrumental support were derived from the CDC’s PRAMS.22 In efforts to reduce survey length, the survey was adapted towards the end of data collection and resulted in the removal of these 4 questions.
Health information: Text messaging campaign and fathers’ requests for information
The Healthy People 2020 social determinants of health framework cites health literacy as an important social determinant under the health and health care domain20 and the AAP suggests fathers be asked about health information needs.12 In an effort to provide expecting fathers access to easy to understand health information and identify if fathers need parenting resources, the First 1000 Days program gave fathers the option to enroll in a text message campaign during their partner’s pregnancy and indicate health information needs via the survey.
The text messaging campaign (available in English and Spanish) provided fathers with 1 to 2 automated text messages per week with tips, encouragement and resources to engage in healthy behaviors, manage stress, prepare for the baby’s birth, and support early child development. Fathers’ enrollment in the campaign served as a proxy for whether this population of fathers demonstrate a need for more information on health behaviors, on how to support a healthy pregnancy, and if text messaging is a viable route for delivery of such information.
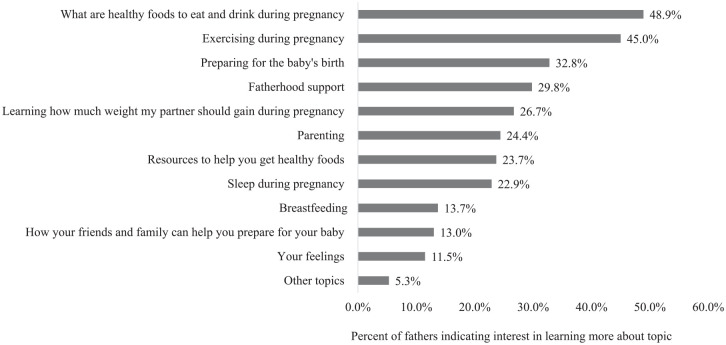
The final survey question asked fathers to indicate interest in learning more about the following topics: sleep, healthy foods to eat and drink, exercise, gestational weight gain, how friends and family can help prepare for the baby, resources to help get healthy foods, feelings, fatherhood support, breastfeeding, parenting, and preparing for the baby’s birth. Fathers were instructed to select as many topics as applied from the pre-determined list and provided with a resource sheet tailored to their health information requests. Each topic was treated as a single variable and the frequency of fathers that selected each individual topic was calculated.
Analysis Plan
Descriptive and summary statistics for all key model variables and demographics were assessed and described. Frequency statistics were calculated for fathers’ interests in learning more about different topics during pregnancy. Missingness is reported for all variables. All analyses were conducted using R Studio and SAS with statistical significance set at P ≤ .05.
Results
Unmet Social and Economic Needs
Over half of fathers were non-white (55%), born outside of the United States (55%), and 43% preferred to speak a language other than English at home (Table 1). Two thirds of fathers (63%) were married and cohabiting with their partners during the first trimester of pregnancy. The majority of fathers were employed full-time (74%), 11% were employed part-time and the remaining 15% were unemployed.
Table 1.
Participant Demographic Characteristics of Expectant Fathers in the First 1000 Days Program with Survey Data at Partner’s First Trimester (n = 131).
| Fathers | ||
|---|---|---|
| N | % | |
| Race/Ethnicity, n = 122 | ||
| Non-Hispanic White | 55 | 45.1 |
| Hispanic/Latino | 26 | 21.3 |
| Non-Hispanic Asian, American Indian or Alaskan Native | 23 | 18.8 |
| Non-Hispanic Black | 18 | 14.8 |
| Foreign-born, n = 126 | 69 | 54.8 |
| Preferred language spoken at home, n = 129 | ||
| English | 73 | 56.6 |
| Spanish | 24 | 18.6 |
| Arabic | 17 | 13.2 |
| Other | 15 | 11.6 |
| Employment status, n = 123 | ||
| Full-time | 91 | 74.0 |
| Part-time | 14 | 11.4 |
| Unemployed | 18 | 14.7 |
| Marital status, n = 126 | ||
| Married and cohabiting | 79 | 62.7 |
| Unmarried and cohabiting | 42 | 33.3 |
| Unmarried and not cohabiting | 6 | 4.8 |
| Mean | SD | |
| Household size, n = 119 | 3.32 | 1.42 |
About 40% of fathers reported not having seen a primary care provider in the last year (Table 2). Most fathers (69%) reported a total household income <$50 000 annually, or at least 19% less than the median household income in the Greater Boston Area in 2017 ($62 021).28 Based on reported gross annual income and household size, 54% of fathers met SNAP eligibility criteria in Massachusetts for the year 2019 (2017 criteria was not available).29 However, only 13% of fathers reported currently receiving SNAP benefits and 18% classified as food insecure. Almost 10% of fathers were housing insecure.
Table 2.
Expectant fathers’ health care, economic, and social support needs in the First 1000 Days program with survey data at partner’s first trimester (n = 131).
| Fathers | ||
|---|---|---|
| N | % | |
| Health care needs, n = 128 | ||
| Has seen a primary care provider within 12 months | ||
| Yes | 77 | 60.2 |
| No | 51 | 39.8 |
| Economic needs | ||
| Food insecure, n = 128 | ||
| Yes | 23 | 18.0 |
| No | 105 | 82.0 |
| Housing insecure, n = 129 | ||
| Yes | 12 | 9.3 |
| No | 117 | 90.7 |
| Receiving SNAP, n = 123a | ||
| Yes | 16 | 13.0 |
| No | 107 | 87.0 |
| Gross annual household income, n = 124 | ||
| <$10 000 | 16 | 12.9 |
| $10 000 to $20 000 | 17 | 13.7 |
| $20 000 to $50 000 | 52 | 41.9 |
| Greater than $50 000 | 39 | 31.5 |
| Social support needs | ||
| Partner support, n = 128 | ||
| High support | 119 | 93.0 |
| Medium or low support | 9 | 7.0 |
| Non-partner support: interactions with family, friends and neighbors, n = 131 | ||
| Low social isolation | 105 | 80.2 |
| High social isolation | 26 | 19.8 |
| Knows someone that could loan $50, n = 107b | 72 | 67.3 |
| Knows someone that could provide care if ill, n = 108b | 93 | 86.1 |
| Knows someone whom could talk with about problems, n = 106b | 93 | 87.7 |
| Knows someone that could provide ride to clinic, n = 106b | 91 | 85.8 |
Note. aSupplemental Nutrition Assistance Program.
Not all fathers answered this question as it was removed from the survey on 7/24/17.
Most fathers reported high levels of perceived partner support (93%). However, there was substantially more variance in report of non-partner support, as 20% of fathers reported not having contact with family, friends, or neighbors in a typical week and 33% reported not knowing someone who could provide a loan of $50. Approximately 14% of fathers reported not having support in case of illness, 14% reported not knowing someone who could take them to a clinic if they needed transportation, and 12% reported not having someone they could talk with about personal problems (Table 2). Post-hoc analyses (data not shown) exhibit that fathers with food or housing insecurity tended to report lower levels of partner and non-partner support overall and were significantly less likely to know someone that could loan $50 or someone that could provide a ride to clinic compared to fathers that were food or housing secure (P < .01 and P < .02, respectively).
Health Information: Text Messaging Campaign and Fathers’ Requests for Information
Ninety-seven fathers (74%) indicated wanting more information on at least 1 topic and 34 fathers (24%) did not select any topic. Out of all fathers, just under 50% reported wanting more information about healthy foods and beverages to consume during pregnancy, 45% were interested in exercise during pregnancy, and 33% of fathers reported wanting information about preparing for the baby’s birth (Figure 1). Approximately 23% wanted to know more about either sleep during pregnancy or resources to access healthy foods. Regarding parenting, almost a third (30%) wanted information about fatherhood support specifically, a quarter wanted to learn about general parenting (24%), and 14% wanted information about breastfeeding. Fathers were also interested in how family/friends can help prepare for their baby (13%) and learning more about their feelings (11.5%). For the text messaging campaign, an equal proportion of fathers opted to enroll as did not enroll (38%), with the remaining 25% indicating they would be interested “maybe in the future”, supporting some interest in this medium of health information delivery.
Figure 1.
Percent of expectant fathers interested in learning more about topics related to health behaviors, pregnancy, childbirth, and parenting in the First 1000 Days program (n = 131).
Note. A total of 34 fathers did not select a topic, though are included in frequency calculation. Percentages total past 100% as topics are not mutually exclusive (fathers could indicate interest in more than 1 topic).
Discussion
This exploratory, cross-sectional study aimed to identify the unmet needs of a diverse group of low-income expecting fathers, and gauge fathers’ interest in learning about health behaviors, pregnancy, childbirth, and parenting. Furthermore, this subset of fathers served as a pilot to inform future early life fatherhood interventions. In order to best support fathers of underserved populations during pregnancy, it is critical to understand the challenges and social determinants at play as future interventions will need to address these factors to achieve optimal father engagement, especially in low-income communities. Indeed, intervention recruitment and retention methods designed to address mothers’ concerns and interests may not be translatable for use with fathers.30,31 To the best of our knowledge, no study has reported fathers’ unmet social, health care, and economic needs during pregnancy and few studies have directly asked expecting fathers to voice pregnancy-related health information needs.
Overall, fathers in the First 1000 Days study population demonstrated that they have substantial unmet economic needs in relation to income, employment, food insecurity, housing insecurity, and SNAP access. Despite the fact that about 54% of fathers were eligible for SNAP in Massachusetts, only 13% reported accessing these services. A large percentage of fathers in the sample are foreign-born, which may make them reluctant to apply for SNAP benefits. Almost a fifth of fathers reported food insecurity in the current sample (18%); these rates are comparable to 2017 national food insecurity statistics for U.S. households with children (15.7%) and U.S. households headed by Hispanics (18.0%), but higher than those for men living alone (13.4%), for households in the state of Massachusetts (10.2%), and for households in the U.S. overall (11.8%).32 Though 18% of fathers were food insecure, a larger proportion (24%) indicated interest in resources to access “healthy foods”. Food security levels may not be reflective of diet quality, thus raising the importance of also asking about consistent access to nutritious foods. Most of the fathers in our sample were cohabiting with their partners (95%), suggesting that fathers’ unmet nutritional and housing needs may reflect the same issues for their families.
Just under 10% of fathers report having experienced unstable housing within the year. Research from the Fragile Families and Child Wellbeing Study suggests that 7-12% of expecting fathers reported housing insecurity, and 25% reported housing insecurity at least once over a nine-year period.33 Precarious housing conditions impede fathers’, especially nonresident fathers’, ability to consistently meet parenting responsibilities.33,34 Furthermore, the Children’s Health Watch study found that households behind on rent had increased odds of fair and/or poor caregiver and child health, child lifetime hospitalizations, and maternal depressive symptoms.34 A standardized instrument to screen for caregiver housing insecurity in the clinical setting is necessary and recommended by the AAP.34
Promisingly, levels of partner and non-partner support in the study suggested that fathers know of individuals they could reach out to for social support. Although a third of fathers reported not knowing an individual that could provide a $50 loan in times of need, over 85% reported having other tangible (ie, transportation) and intangible (ie, illness, emotional) forms of support. These non-financial forms of social support may be sources of resiliency as they can reduce stressful factors affecting low-income parents and facilitate a father’s ability to be involved.35 In past initiatives aimed at improving fathers’ employment outcomes, social networks were identified as particularly important for younger, nonresidential, and low-income fathers in fulfilling their parenting and financial responsibilities.35 Fathers’ social support needs should be assessed in early pregnancy and future interventions should incorporate social support building (ie, group discussions, peer mentorship) as well as other services (ie, GED preparation) solicited by fathers in past studies.31 Furthermore, interventions can employ fathers from the community to serve as “champions” by reaching out to fathers, validating the program’s legitimacy, and ultimately leveraging social ties to bridge the gap between community needs and the delivery of health services.30,36
Of the 40% of fathers who do not seek regular primary care, it is possible some are facing transportation barriers or avoiding seeking care. Around 14% of fathers reported they were unaware of an individual that could provide a ride to the clinic or doctor’s office. Transportation is an essential social determinant of health care access and it is estimated that annually at least 3.6 million people in the United States miss needed nonemergency medical care because of lack of transportation.37 Thus, this is a component to regular health care access that should be considered, especially in the context of racial/ethnic minorities who are more likely to face transportation barriers, in the management of chronic disease, such as obesity or diabetes, where frequent clinic visits are necessary,37 and in efforts to increase participation in fatherhood programs.30,31
Few other studies have directly asked fathers to express pregnancy-related or general parenting-related health information needs. In a small qualitative study, fathers most frequently mentioned needing more information on their role as a new father, practical newborn parenting tips, and relationship changes.38 These findings support our results as fatherhood and parenting were also among the more solicited topics. The most requested topics were related to fathers’ health behaviors (Figure 1), indicating that fathers may see pregnancy and the impending birth of a new child as motivation to seek information to improve their health behaviors.39 Additionally, many fathers indicated interest in learning about at least 1 topic related to pregnancy, childbirth, and parenting. Indeed, over a third of fathers signed up for the text messaging campaign, suggesting that fathers were both interested in and taking steps to actively increase their knowledge about health behaviors and pregnancy. In a study of text messages intended for fathers of infants, both mothers and fathers reported text messages were relevant to fatherhood and easy to understand.40 Though limited, these studies show fathers want parenting information specific to fathers and may find text messaging an acceptable and convenient medium for delivery.
It is critical health care providers and interventions ensure easy access to intelligible health information, especially among racial/ethnic minorities, individuals of lower socioeconomic status or whose first language is not English, as these groups face some of the lowest health literacy rates.41 Low parental health literacy has shown to impact parent behavior (ie, duration of breastfeeding)42 and child outcomes (ie, persistent asthma).43 Furthermore, fathers may be less prepared, at times excluded from their child’s health care visits,44,45 and may need more education and support to fulfill their role as a parent thus making additional resources valuable.30,12 In line with this evidence, the AAP recommends that child health care providers ask fathers about parenting skills and information they need and encourage fathers to attend pediatric office visits.12
Although this study provides information regarding fathers’ unmet social and economic needs and health information interests in early pregnancy, there are several limitations that bear noting. It is likely there is some level of selection bias and social desirability bias among this small sample of fathers due to the way the survey was administered. All data were based on self-reported and self-administered surveys completed on an iPad at the clinic, potentially next to their partner, leaving room for misinterpretation of questions or response bias. Only expecting fathers that attended their partner’s first prenatal visit could complete the survey and thus the sample of fathers may differ from those who did not attend the first prenatal visit, about whom data is not available. Moreover, fathers were only offered to participate at 1 of 3 health centers where mothers received the First 1000 Days intervention and fathers’ completion of the survey was not a pre-requisite for mothers’ exposure to the intervention, thus leading to a smaller sample size than that of the mothers. Recruiting fathers through mothers can result in a nonrepresentative sample as it is more likely the participant be married, have a higher education level and a more positive relationship with the mother, and leave out nonresidential biological fathers who may be active in their child’s life.30 Furthermore, due to limited survey questions and survey time constraints, we were unable to obtain data around additional social determinants (ie, neighborhood/built environment, education) incorporated in the Health People 2020 framework.20 Moreover, the request for information question did not include a “not interested” response option, which could explain why 34 fathers did not select a topic.
Despite these limitations, to the best of our knowledge, this is one of the first studies that has collected data on unmet needs among fathers during the sensitive antenatal period. Surveys were offered in the most common languages spoken at the health centers, allowing us to assess needs among a diverse group of low-income fathers. The current paucity of research on fathers’ unmet social needs during pregnancy, as well as fathers’ reports about information they want to receive during pregnancy, has limited researchers from identifying factors that may promote or inhibit father involvement during pregnancy or improve maternal-child outcomes, and creating innovative interventions to effectively recruit and retain fathers in prenatal intervention and prevention programs. The current study findings are novel and may inform future efforts to optimize the role of fathers during pregnancy and early infancy.
Implications for Research and Practice
Fathers in this low-income sample reported high levels of unmet economic needs, but higher levels of social support, and requested information about pregnancy, birth preparation, and fatherhood. Given that available social support is higher than economic support in this study of fathers and that the literature shows fathers’ social ties can serve as sources of resiliency in face of economic hardship, researchers should further examine if social networks can be leveraged to improve low-income father access to services and health information during pregnancy. Although family-based interventions typically only provide information to mothers, our study finds evidence to suggest that future interventions should consider providing fathers more support and information related to health behaviors, pregnancy, and parenting (ie, via text messaging). Findings also suggest that clinicians should encourage fathers to be present at antenatal visits and consider standardized screening for basic economic and social needs during the first trimester. These visits may serve as an opportunity to provide fathers tailored resources that can facilitate health behavior promotion, and thereby help fathers support a healthy pregnancy. Based on results from this study, future initiatives aimed at addressing low-income fathers’ unmet needs during pregnancy should screen for social determinants of health, consider utilizing text messaging campaigns, and provide father-specific information about health behaviors, pregnancy, and parenting.
Footnotes
Author Contributions: FNM: Contributed to conception and design; Contributed to acquisition, analysis, and interpretation; Drafted the manuscript; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
JAS: Contributed to conception and design; Contributed to interpretation; Drafted the manuscript; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MS: Contributed to conception and design; Contributed to acquisition, analysis, and interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
ML: Contributed to analysis and interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MEP: Contributed to conception and design; Contributed to acquisition and interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
BR: Contributed to acquisition and interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
TBL: Contributed to interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MK: Contributed to interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
AAB: Contributed to interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
KD: Contributed to interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
EMT: Contributed to conception and design; Contributed to acquisition, analysis, and interpretation; Critically reviewed the manuscript; Gave final approval; Agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by The Boston Foundation (G2015-0007), the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (K24DK105989), the Harvard Education Program in Cancer Prevention and Control (R25CA057711-25), and Massachusetts General Hospital.
ORCID iDs: Fernanda Neri Mini  https://orcid.org/0000-0003-0466-8676
https://orcid.org/0000-0003-0466-8676
Elsie M. Taveras  https://orcid.org/0000-0001-6158-2807
https://orcid.org/0000-0001-6158-2807
References
- 1. Amjad S, MacDonald I, Chambers T, et al. Social determinants of health and adverse maternal and birth outcomes in adolescent pregnancies: a systematic review and meta-analysis. Paediatr Perinat Epidemiol. 2019;33:88-99. [DOI] [PubMed] [Google Scholar]
- 2. Lu M. Reducing maternal mortality in the United States. JAMA. 2018;320:1237-1238. [DOI] [PubMed] [Google Scholar]
- 3. Maness SB, Buhi ER. Associations between social determinants of health and pregnancy among young people: a systematic review of research published during the past 25 years. Public Health Rep. 2016;131:86-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nelson DB, Moniz MH, Davis MM. Population-level factors associated with maternal mortality in the United States, 1997–2012. BMC Public Health. 2018;18:1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weightman AL, Morgan HE, Shepherd MA, Kitcher H, Roberts C, Dunstan FD. Social inequality and infant health in the UK: systematic review and meta-analyses. BMJ Open. 2012;2:e000964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee SH, Lazebnik R, Kuper-Sassé M, Lazebnik N. Is the presence of the father of the baby during first prenatal ultrasound study visit associated with improved pregnancy outcomes in adolescents and young adults? Int J Pediatr. 2016;2016:4632628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McBride N, Johnson S. Fathers’ role in alcohol-exposed pregnancies. Am J Prev Med. 2016;51:240-248. [DOI] [PubMed] [Google Scholar]
- 8. Κatsi V, Felekos I, Siristatidis C, et al. Preeclampsia: what does the father have to do with it? Curr Hypertens Rep. 2015;17:60. [DOI] [PubMed] [Google Scholar]
- 9. Lamb ME. ed. The Role of the Father in Child Development. 3rd ed. Wiley; 1997. [Google Scholar]
- 10. Sarkadi A, Kristiansson R, Oberklaid F, Bremberg S. Fathers’ involvement and children’s developmental outcomes: a systematic review of longitudinal studies. Acta Paediatrica. 2008;97:153-158. [DOI] [PubMed] [Google Scholar]
- 11. Allen S, Daly K. The Effects of Father Involvement: An Updated Research Summary of the Evidence Inventory. University of Guelph; 2007 [Google Scholar]
- 12. Yogman M, Garfield CF; Committee on Psychological Aspects of Child and Family Health, American Academy of Pediatrics. Fathers’ roles in the care and development of their children: the role of pediatricians. Pediatrics. 2016;138:e20161128. [DOI] [PubMed] [Google Scholar]
- 13. Bruce MA, Griffith DM, Thorpe RJ. Social determinants of men’s health disparities. Fam Community Health. 2015;38:281-283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PLoS One. 2018;13: e0191620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yargawa J, Leonardi-Bee J. Male involvement and maternal health outcomes: systematic review and meta-analysis. J Epidemiol Community Health. 2015;69:604-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheng ER, Rifas-Shiman SL, Perkins ME, et al. The influence of antenatal partner support on pregnancy outcomes. J Womens Health. 2016;25:672-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Abbass-Dick J, Dennis C-L. Breast-feeding coparenting framework: a new framework to improve breast-feeding duration and exclusivity. Fam Community Health. 2017; 40:28-31. [DOI] [PubMed] [Google Scholar]
- 18. Walsh AD, Cameron AJ, Hesketh KD, Crawford D, Campbell KJ. Associations between dietary intakes of first-time fathers and their 20-month-old children are moderated by fathers’ BMI, education and age. Br J Nutr. 2015;114:988-994. [DOI] [PubMed] [Google Scholar]
- 19. Morgan PJ, Collins CE, Plotnikoff RC, et al. The ‘Healthy Dads, Healthy Kids’ community randomized controlled trial: a community-based healthy lifestyle program for fathers and their children. Prev Med. 2014; 61:90-99. [DOI] [PubMed] [Google Scholar]
- 20. Healthy People. Social determinants of health. Office of Disease Prevention and Health Promotion. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. 2020. Updated February 5, 2019. Accessed February 5, 2019.
- 21. Blake-Lamb T, Boudreau AA, Matathia S, et al. Strengthening integration of clinical and public health systems to prevent maternal-child obesity in the First 1,000 Days: a Collective Impact approach. Contemp Clin Trials. 2018;65:46-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Pregnancy Risk Assessment Monitoring System (PRAMS): phase 8 standard questions. Centers for Disease Control. https://www.cdc.gov/prams/pdf/questionnaire/Phase-8-Standard-Core-Questions-508.pdf June 2016. Updated June 2016. Accessed May 8, 2019.
- 23. Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26-e32. [DOI] [PubMed] [Google Scholar]
- 25. Turner RJ, Grindstaff CF, Phillips N. Social support and outcome in teenage pregnancy. J Health Soc Behav. 1990;31:43-57. [PubMed] [Google Scholar]
- 26. Berkman L, Syme S. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186-204. [DOI] [PubMed] [Google Scholar]
- 27. Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103:2056-2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. U.S. Census Bureau. QuickFacts: Boston city, Massachusetts. https://www.census.gov/quickfacts/fact/table/bostoncitymassachusetts/INC110217#INC110217. 2018. Accessed May 3, 2019.
- 29. Department of Transitional Assistance program eligibility charts and tables. Mass.gov. https://www.mass.gov/lists/department-of-transitional-assistance-program-eligibility-charts-and-tables. 2019. Accessed June 26, 2019.
- 30. Vollmer RL, Adamsons K, Mobley AR. Recruitment, engagement, and retention of fathers in nutrition education and obesity research. J Nutr Educ Behav. 2019;51:1121-1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Stahlschmidt MJ, Threlfall J, Seay KD, Lewis EM, Kohl PL. Recruiting fathers to parenting programs: advice from dads and fatherhood program providers. Child Youth Serv Rev. 2013;35:1734-1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2017, ERR-256, U.S. Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/webdocs/publications/90023/err-256.pdf?v=0 Published September 2018. Accessed April 30, 2019.
- 33. Geller A, Curtis MA. A longitudinal examination of housing hardships among urban fathers. J Marriage Fam. 2018;80:1176-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sandel M, Sheward R, de Cuba SE, et al. Unstable housing and caregiver and child health in renter families. Pediatrics. 2018;141:e20172199. [DOI] [PubMed] [Google Scholar]
- 35. Castillo JT, Sarver CM. Nonresident fathers’ social networks: the relationship between social support and father involvement. Pers Relatsh. 2012;19:759-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25:815-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Thomas LV, Wedel KR, Christopher JE. Access to transportation and health care visits for medicaid enrollees with diabetes. J Rural Health. 2018;34:162-172. [DOI] [PubMed] [Google Scholar]
- 38. Deave T, Johnson D. The transition to parenthood: what does it mean for fathers? J Adv Nurs. 2008;63:626-633. [DOI] [PubMed] [Google Scholar]
- 39. Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol. 2003;58:5-14. [DOI] [PubMed] [Google Scholar]
- 40. Fletcher R, May C, Wroe J, et al. Development of a set of mobile phone text messages designed for new fathers. J Reprod Infant Psychol. 2016;34:525-534. [Google Scholar]
- 41. Kutner M, Greenburg E, Jin Y, Paulsen C. The health literacy of America’s adults: results from the 2003 national assessment of adult literacy. National Center for Education Statistics; 2006. Report No.: NCES 2006-483. [Google Scholar]
- 42. Kaufman H, Skipper B, Small L, Terry T, McGrew M. Effect of literacy on breast-feeding outcomes. South Med J. 2001;94:293-296. [PubMed] [Google Scholar]
- 43. DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7:25-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lowenstein LM, Perrin EM, Berry D, et al. Childhood obesity prevention: fathers’ reflections with healthcare providers. Childhood Obesity. 2013;9:137-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Allport BS, Solomon BS, Johnson SB. The other parent: an exploratory survey of providers’ engagement of fathers in pediatric primary care. Clin Pediatr (Phila). 2019;58: 555-563. [DOI] [PubMed] [Google Scholar]