Abstract
Background:
Aiming to tackle the rise of non-communicable diseases and an ageing population, Albania is engaged in boosting primary healthcare services and quality of care. The patients’ perspectives on their experience with public and private providers are, however, missing, although their viewpoints are critical while shaping the developing services. Consequently, we analyze perceptions of users of primary healthcare as it relates to non-clinical quality of care and the association to sociodemographic characteristics of patients and the type of provider.
Methods:
A facility-based survey was conducted in 2018 using the World Health Organization responsiveness questionnaire which is based on a 4-point scale along with 8 non-clinical domains of quality of care. The data of 954 patients were analyzed through descriptive statistics and linear mixed regression models.
Results:
Similar mean values were reported on total scale of the quality of care for private and public providers, also after sociodemographic adjustments. The highest mean score was reported for the domain “communication” (3.75) followed by “dignity” (3.65), while the lowest mean scores were given for “choice” (2.89) and “prompt attention” (3.00). Urban governmental PHC services were rated significantly better than private outpatient clinics in “coordination of care” (2.90 vs 2.12, P < .001). In contrast, private outpatient clinics were judged significantly better than urban PHC clinics in “confidentiality” (3.77 vs 3.38, P = .04) and “quality of basic amenities” (3.70 vs 3.02, P < .001). “Autonomy” was reported as least important attribute of quality.
Conclusion:
While the perception of non-clinical care quality was found to be high and similar for public and private providers, promptness and coordination of care require attention to meet patient’s expectations on good quality of care. There is a need to raise the awareness on autonomy and the involvement of patients’ aspects concerning their health.
Keywords: primary care, non-clinical quality, private provider, autonomy, communication, Albania
Introduction
The goal of primary healthcare (PHC) is to provide universally accessible first level services for individuals, families, and communities thereby ensuring their referral to hospital and other specialized services when needed. It is increasingly acknowledged that the quality of services matters to progress toward Universal Health Coverage (UHC).1,2 Patients’ viewpoints, perceptions and experiences, including non-therapeutic dimensions of care such as communication, attention, treatment or confidentiality, is a central aspect of quality of care.1-4
In Albania, a south-eastern European country with a health system in transition, most health care providers continue to be owned by the Government. They have a 3 tiers-level structure: primary, secondary, and tertiary healthcare services. After the fall of the communism system (1990), various reforms gained pace such as the permission of private service providers to operate, decentralization of primary care management, the complete privatization of the pharmaceutical sector and dentistry and the founding of the Health Insurance Institute.5 Private providers are today essentially concentrated in urban areas and major cities.
Albania has been engaged for several years in improving PHC services to better address health system challenges, such as the steady rise of non-communicable diseases (NCDs).6-8 Indeed, the most recent Demographic and Health Surveys (ADHS) conducted in 2009 respectively 2018, indicate for example marked increases in the prevalence rates of hypertension.9
In 2015, as part of its commitment to move toward UHC, the Ministry of Health and Social Protection (MoHSP) has introduced a free check-up program offered for all citizens aged 35 to 75 years—independent of their insurance coverage or health condition.6,10 In parallel, a mandatory health insurance scheme is in place, as part of the social protection system, covering medical examinations at the public and, more recently, at some private contracted health providers. Based on the results of ADHS 2018, around 37% of the population aged 15 to 59 years benefits from entitlements through the mandatory health insurance scheme.9 Based on the referral system and the drug reimbursement structure (ie, full or partial) the scheme is free or subsidized with co-payment.11 As the insurance system favors public providers, they absorb the bulk of service provision, leading to high utilization rates namely of the tertiary levels (university hospitals).12
Public PHC is currently being provided in Albania through a well-established network of 413 urban and rural health facilities and additional health posts. A package of basic medical services such as (i) emergency care; (ii) health services for children; (iii) women of reproductive age; (iv) adults and (v) elderly people; (vi) mental health care; and (vii) health promotion and education is offered mainly through health centers.11
In addition, there are private healthcare services. They may be for-profit or not-for profit providers. The for-profit outpatient clinics (providing PHC and specialty care services), which are sometimes located in private hospitals, have experienced substantial growth in the last decade, especially in urban areas. In 2019, 10 private hospitals, 229 specialized private diagnostics and laboratory clinics and 177 outpatients’ medical centers and cabinets were licensed.13 While adding a provider option for patients, they have proven challenging to the coordination of the national health system as, to some degree, they are duplicating both public PHC services and specialty services provided in polyclinics.14
Governmental PHC has often been challenged by ill-equipped facilities, bypass to secondary or tertiary care, lack of trust in PHC personnel and access barriers to services (eg, waiting times and distance to PHC centers).10,12,15 At a time of rapid change in health demands and growth in PHC providers it would seem important to understand what service users would value in terms of quality.
However, information on patient encounters’ with PHC both in public and private outpatient settings and their perspective as it relates to the non-clinical quality of care is missing in Albania.
Quality of Care and Patient Experience Across Settings
Quality of care is a broad concept which includes structural, technical, process, and outcomes aspects.16,17 Different instruments have been developed to measure and assess quality from different perspectives. A tool developed and validated for measuring and analyzing the non-clinical aspects of care is the “health system responsiveness tool.”18-20 In 2018 World Health Assembly proposed a set of indicators and a framework for measurements in patient centeredness areas to aid countries in embedding patient experience as an assessable and reportable component of quality.21
Both the public and private health organization are engaged in improving quality of care. The private sector is often viewed as more client-centered,22 better at patient education and interpersonal satisfaction,23 and patients seem to experience better timeliness and hospitality.24 Quality of care is comparatively well rated in public health services in some western European countries.25,26 Other studies find it difficult to draw clear deductions about the advantage of any particular type of settings, instead associating quality of care with the main features of health service provider such as the organization of and remuneration for services, number of skilled health specialists rather than the clear ownership of the health facilities.27,28 Recent systematic reviews led to contradictory conclusions in respect to quality of care differences between public and private providers due to different review methodologies and, above all, diverse settings and contexts where private providers played different roles within the health system.29
Several research studies have shown that rural populations are more reluctant to express discontent and are generally more satisfied with quality of care and health-care systems than their urban counterparts,30 though rural patients appear to mirror an undervaluing of primary care in favor of specialty care.31 Primary health care in many rural areas have the challenges of; staff recruitment, poor physical amenities; lack of accessibility to diagnostic health services which undermines quality and effective care when contrasted to urban settings.32,33
Additional evidence is required with regard to public and private users “experiences with quality of care and operating providers” characteristics,34 factors that drive quality variations and quality improvement approaches21 in order to guide PHC strengthening. To date, substantial published work is available in this field35-39 but none in Albania to the best of our knowledge.
With the ambition to provide information so improve UHC and access to PHC, this study analyses perceptions of the users of public and private PHC services pertaining to non-clinical quality of care and their associations with the sociodemographic characteristics of patients and the type of healthcare provider.
Methods
Study Setting
The data for this study were collected through a cross-sectional survey (including also exit interviews with patients) at health service level. The study was conducted within the frame of the “Health for All” (HAP) which covers 2 out of 12 regions in Albania. ‘HAP’ is funded by the Swiss Agency for Development and Cooperation. The overall goal of the project is that the Albanian population benefits from better health through improved primary health care services and health promotion activities. The regions covered by the survey were: (1) Fier which is located South-West of the capital, Tirana, with access to the seaside and (2) Diber a mountainous region, located in the Eastern part of the Country bordering North Macedonia. The census 2011 registered 447 263 persons living in the 2 regions (310 277 in Fier living in 87 605 households and 137 036 in Diber living in 33 204 households). The regions cover approximately 16% of the total population of Albania
Study Design and Sampling
A facility-based, cross-sectional survey was conducted including all governmental health centers (HC) in rural and urban areas in 2 regions. The study intended to include also all private health providers offering outpatient/ambulatory services in the regions covered. In one region (Diber), there were no private services and in the other one there were 8 clinics (Fier), all located in urban areas. From these 8 private clinics, 5 consented to participate. Therefore, 38 public healthcare facilities and 5 private healthcare facilities were included in the sampling.
The calculation of the sample size for patients from public facilities was tuned to being able to estimate parameters of patient satisfaction with sufficient precision. As all 38 public facilities of the 2 study districts could be recruited and the numbers of patients interviewed across the different facilities were chosen in proportion to facility size, the standard error associated with estimating a certain prevalence p in the underlying patient population was smaller than or equal to , where N denotes the total sample size.
Assuming that 20% of patients attending public health facilities in the 2 districts were unsatisfied with the respective health center, we wanted the respective estimation error to stay below 3% with a probability of 95%. This required a total sample size of 683 patients, that is, an average number of patients per facility of 18. Assuming a drop-out rate of 10%, this number had to be increased to 20. We further increased the number to 25 to gain statistical power for comparisons (eg, between urban and rural facilities). The same sampling strategy as in public facilities, was also employed for private clinics but with higher numbers of patient interviews because of the larger size of the facilities.
Questionnaire on Patient Perception
We assessed patients’ perceptions on 8 domains of responsiveness and service quality through the World Health Organization (WHO)’s Health System Responsiveness Questionnaire, a publicly and freely available tool40 which has been widely used in various settings.18,35,37,41 The tool is structured along 8 domains: (i) autonomy; (ii) choice of health care provider; (iii) clear communication; (iv) confidentiality; (v) dignity; (vi) prompt attention; (vii) quality of basic amenities; and (viii) access to social support networks. We excluded the domain of “access to social support networks” because our study focused on users of outpatient services. Based on our critique and as suggested by other researchers in this field, we added “coordination of care” as an additional domain, given the importance of patients with chronic conditions in the Albania setting.39
All individual items were scored on a scale from 1 to 4 (1 = bad; 2 = rather bad; 3 = good; 4 = very good). Patients were also asked to choose the domain they consider as “most important” when consulting a healthcare provider. Hence, in this study, we make a distinction between 2 categories of users’ measures of non-clinical quality of care: (i) patients’ most recent experience (the level of responsiveness as measured by the interactions that patients have with the healthcare provider) and (ii) patients’ expectations on attributes of quality (patients’ evaluations of what is considered important when receiving care in general, relative to their expectations).
The WHO questionnaire was translated from English to Albanian and then translated back to English prior to conducting the interviews. We changed the word “confidentiality” and translated as “privacy respected” and “autonomy” as “involvement in health decisions” in order to be easy comprehended and to be closer to laymen comprehension of the terms. Also, on “coordination of care,” we slightly changed the item “the physician knows if certain tests have to be conducted regularly” into “doctor knows your medical history (main developments on illness)” and “you were helped (feel assisted) to transit from one provider to the other”. Patients’ socio-demographic characteristics such as age, gender, employment status, education, status of health insurance coverage was also collected in addition to the patients’ health conditions including self-reported health status (poor/not poor) and the presence of chronic health condition (yes/no). In order to determine the internal consistency of the questionnaire, Cronbach’s alpha was calculated.
Data Collection
Data collection took place from July to August 2018. For study inclusion, participants had to be at least 18 years old, and they had to have had some form of outpatient care on the day of the interview.
Interviews were conducted by medical students that had completed at least a bachelor’s degree. Prior to data collection, interviewers were trained for 3 days and the questionnaires were pre-tested in a different population but in the same regions. Data collection was done electronically using tablets through Open Data Kit (ODK) platform. Participants’ responses were uploaded in a secured server at Swiss Tropical and Public Health Institute (Swiss TPH), Basel, Switzerland on the same day of the data collection and regular data quality check was conducted.
Data Analysis
In a first step, the characteristics of patients were compared across the 3 types of health facilities: (1) public urban PHC clinics, (2) private outpatient clinics, and (3) public rural PHC clinics. Mean scores of each domain, representing patients’ experience with quality were obtained using the margins syntax of Stata. Our primary analysis focused on the association between perceived non-clinical quality of care and type of facility. Factors associated with patient’s perceived quality of care were included as potential confounders of this association. They were: (i) age; (ii) gender; (iii) education; (iv) occupation; (v) insurance status (yes/no); (vi) self-rated health (poor/good); (vii) presence of 1 or more chronic condition(s); and (viii) utilization of clinics over the past 3 months. Linear mixed models, with random intercepts for districts and facilities nested in districts, were thus used to investigate the association between the utilization of the type of health facility and non-clinical quality of care domains adjusting for patients’ sociodemographic characteristics. The score of overall quality was determined as the mean of all available sub-scores requiring that at least 6 of the 8 sub-scores were present. Analyses were repeated in a subsample of patients who had no missing sub-scores and the respective results showed only minor differences. The statistical tests and P-values were obtained from the Wald tests of the respective parameter estimates, P < .05, and P < .1. Data was analyzed using Stata Statistical Software, version 15.
Ethical Considerations
The study protocol was approved by the ethics committee of north-western and central Switzerland (EKNZ- Ethikkommission Nordwest- und Zentralschweiz), No. 30715. The study also received clearance by the National Ethics Committee of Albania, nr.55, date 08.06.2018. All study patients had to provide written informed consent for participation.
Results
Patients’ Characteristics by Type of Healthcare Provider
Out of 1083 who were eligible study participants, 954 accepted to be interviewed corresponding to a response rate of 88%. The characteristics of the study participants are shown in Table 1. There was a slightly higher proportion of female visits compared to male visits (58% vs 42%). The mean age of participants was 37 ± 20.1. Most of the patients were in the age group 18 to 60 years (54%). About 33% of the participants were unemployed and 50% had basic education (primary and secondary school, 5 to 9 years of study).
Table 1.
Patients’ Characteristics by Socio-Demographic and Health Measures by Type of Healthcare Provider.
| Characteristics | Total N = 954 | Public urban clinics (2) N = 337 |
Private outpatient clinics (3) N = 178 |
Public rural clinics (4) N = 439 |
|---|---|---|---|---|
| 35% | 19% | 46% | ||
| Gender | ||||
| Male | 42% (401) | 37% (125) | 36% (64) | 48% (212) |
| Female | 58% (553) | 63% (212) | 64% (114) | 52% (227) |
| Age mean (year), SD (year) | 36 (20.8) | 36.5 (20.8) | 35 (20.7) | 35.9 (20.8) |
| 18 < 59 years old | 54% (478) | 52% (161) | 57% (95) | 54% (222) |
| ≥60 years old | 46% (406) | 48% (148) | 43% (71) | 46% (187) |
| Education | ||||
| University/college | 12% (90) | 18% (39) | 17% (28) | 6% (23) |
| High school* | 33% (251) | 37% (80) | 37% (62) | 30% (109) |
| Primary and secondary school* | 50% (379) | 43% (93) | 46% (78) | 57% (208) |
| Illiterate/other | 4% (31) | 2% (4) | 1% (1) | 7% (26) |
| Occupation | ||||
| Employed | 24% (199) | 24% (64) | 32% (53) | 20% (82) |
| Unemployed | 33% (280) | 30% (81) | 32% (55) | 36% (144) |
| Pensioner | 39% (329) | 42% (114) | 35% (58) | 39% (157) |
| Other | 4% (30) | 4% (10) | 1% (2) | 5% (18) |
| Self-rated health | ||||
| Poor | 20% (191) | 80% (270) | 6% (11) | 26% (113) |
| Good | 80% (763) | 20% (67) | 94% (167) | 74% (326) |
| Health insurance | ||||
| No | 19% (180) | 6% (20) | 33% (58) | 23% (102) |
| Yes | 81% (774) | 94% (317) | 67% (120) | 77% (337) |
| Benefit from social-economic support | ||||
| No | 79% (756) | 81% (274) | 94% (167) | 72% (315) |
| Yes | 21% (197) | 19% (63) | 6% (11) | 28% (123) |
| Chronic conditions | ||||
| 0 | 41% (395) | 39% (131) | 43% (76) | 43% (188) |
| 1 | 41% (388) | 42% (143) | 49% (87) | 36% (158) |
| 2 or more | 18% (170) | 19% (63) | 8% (15) | 21% (92) |
| Years suffered from the chronic illness(es)** | ||||
| ≤2 years | 21% (113) | 19% (38) | 31% (32) | 19% (43) |
| >2 years | 79% (426) | 81% (167) | 69 % (70) | 81% (189) |
| Number of times health facility was attended over the past 3 months | ||||
| ≤1 | 23% (222) | 19% (62) | 33% (58) | 23% (102) |
| ≥2 | 77% (732) | 81% (275) | 67% (120) | 77% (337) |
| Satisfaction with today’s consultation | ||||
| Unsatisfied | 5% (43) | 4% (12) | 0% | 7% (31) |
| Satisfied | 95% (911) | 96% (325) | 100% (178) | 93% (408) |
| Participated in promotion activities | ||||
| No | 96% (916) | 97.6% (329) | 100% (178) | 93% (409) |
| Yes | 4% (38) | 2.4% (8) | 0% | 7% (30) |
Primary and secondary school are up to 9 years of study (5-9). High school up to 12 years of study.
For certain sociodemographic categories such as “years suffered from the chronic illness(es)” we received lower responses.
Almost 60% of the all respondents stated that they suffered from at least 1 chronic health condition. The percentage of patients who reported suffering from 2 or more chronic conditions was higher in public rural PHC clinics (21%) and public urban PHC clinics (19%) compared to private clinics (8%). The proportion of patients recently diagnosed with a chronic condition (ie, less than 2 years ago) was higher in private clinics (31%) compared with the governmental PHC facilities (vs 19%), (Table 1).
A considerable proportion of patients utilizing urban public PHC clinics were pensioners (42%). Twenty-seven percent of patients utilizing rural PHC clinics perceived their health status as poor or rather poor, compared to 20% in urban PHC clinics. Nearly a third (28%) of patients attending a rural PHC service indicated that they are currently benefitting from some sort of economic or social aid scheme compared with 19% among those consulting a public urban PHC service.
Compared with public urban PHC clinics, private outpatient clinics in urban areas provided services to younger patients (57% of patients were <60 years) who perceived themselves as having good health (94%). Patients visiting governmental PHC clinics hold more frequently a health insurance card (public urban PHC 94% vs public PHC rural 77% vs private outpatient clinics 67%).
Rating of Non-Clinical Care Quality by Patients
For 6 of the 8 domains, Cronbach’s Alpha varied between 0.60 and 0.83, while the “confidentiality” and “choice” domains had values of 0.35 and 0.55, respectively. The values of the coefficient for the entire questionnaire was 0.65.
The mean responsiveness scores of patients’ experience along the quality of care domains by type of health care provider are shown in Table 2. The highest mean scores were reported for the communication domain (mean = 3.75; 95%-confidence interval = [3.70-3.80]) followed by dignity (3.65 [3.58-3.71]) and confidentiality (3.44 [3.31-3.64]). The lowest responses (lowest mean scores) were given for the domains of “choice” (2.89 [2.40-3.38]), “prompt attention” (3.00 [2.86-3.14]) and “coordination of care” (3.10 [2.83-3.37]). When averaging all scales, there was no significant difference between patients using the different types of providers. The overall mean score was however slightly higher among patients consulting rural PHC services as compared to urban governmental PHC-facilities (3.35 vs 3.21 P = .06).
Table 2.
Comparison of Patients’ Experience on Non-Clinical Quality of Care Domains by Facility Type Through Mean Scores† (and 95%-confidence interval).
| Domains/quality attributes | Total population | Public urban (2) | Private urban (3) | Public rural (4) | P value |
|---|---|---|---|---|---|
| Mean, [95% Conf. Interval] | |||||
| Dignity (n = 954) | 3.65 [3.58-3.71] | 3.70 [3.58-3.82] | 3.81 [3.64-3.98] | 3.59 [3.52-3.67] | 2 versus 3; P = .28 |
| 2 versus 4; P = .16 | |||||
| Communication (n = 933) | 3.75 [3.70-3.80] | 3.71 [3.61-3.81] | 3.7 [3.56-3.83] | 3.79 [3.72-3.85] | 2 versus 3; P = .88 |
| 2 versus 4; P = .19 | |||||
| Coordination of care (n = 854) | 3.10 [2.83-3.37] | 2.90 [2.71-3.08] | 2.12 [1.86-2.38] | 3.35 [3.23-3.47] | 2 versus 3; P < .01 |
| 2 versus 4; P < .01 | |||||
| Confidentiality (n = 940) | 3.47 [3.31-3.64] | 3.38 [3.15-3.60] | 3.77 [3.45-4.09] | 3.46 [3.31-3.61] | 2 versus 3; P = .04 |
| 2 versus 4; P = .5 | |||||
| Choice (n = 790) | 2.89 [2.40-3.38] | 2.69 [2.18-3.10] | 2.57 [2.00-3.14] | 3.06 [2.65-3.46] | 2 versus 3; P = .78 |
| 2 vsersu 4; P = .02 | |||||
| Autonomy (n = 772) | 3.19 [3.05-3.33] | 3.1 [2.84-3.37] | 3.42 [3.06-3.79] | 3.17 [3.00-3.34] | 2 versus 3; P = .16 |
| 2 versus 4; P = .66 | |||||
| Prompt attention (n = 622) | 3.00 [2.86-3.14] | 3.17 [2.97-3.36] | 2.94 [2.71-3.18] | 2.95 [2.78-3.11] | 2 versus 3; P = .07 |
| 2 versus 4; P = .01 | |||||
| Quality of basic amenities (n = 954) | 3.14 [2.98-3.31] | 3.02 [2.69-3.36] | 3.70 [3.23-4.17] | 3.10 [2.87-3.32] | 2 versus 3; P = .01 |
| 2 versus 4; P = .7 | |||||
| Total score (n = 890) | 3.30 [3.21-3.38] | 3.21 [3.07-3.33] | 3.26 [3.07-3.43] | 3.35 [3.26-3.42] | 2 versus 3; P = .65 |
| 2 versus 4; P = .06 |
Mean values were obtained from linear mixed models with random intercepts for districts and facilities nested in districts. Statistically significant, P < .05.
Urban governmental PHC services were rated significantly better than private outpatient clinics in “coordination of care” (2.90 vs 2.12, P < .001). In contrast, private outpatient clinics were judged significantly better than urban PHC clinics in “confidentiality” (3.77 vs 3.38, P = .04) and “quality of basic amenities” (3.70 vs 3.02, P < .001). For the other domains, no statistically significant differences were observed.
Differences were observed in the mean values between governmental urban and rural PHC services: patients consulting in rural PHC services provided higher average ratings for “coordination of care” (3.35 vs 2.90, P < .001) and the “ability to choose a doctor” (3.06 vs 2.64, P = .02), while the ratings for the domain of “prompt attention” was significantly lower compared with governmental urban PHC settings (2.95 vs 3.17, P = .016).
When ranking the importance of domains for consulting by type of provider, among all patients included in the survey by total, “communication” was rated highest, followed by “dignity” (Figure1). The domains seen as most important, communication and dignity, also received the highest mean quality ratings. The “prompt attention” domain was considered as an important domain by patients (ranked third); at the same time, it received low mean scores. “Autonomy” and “choice of provider” were least frequently reported as most important domain, also demonstrating lower mean ratings compared to other domains.
Figure 1.
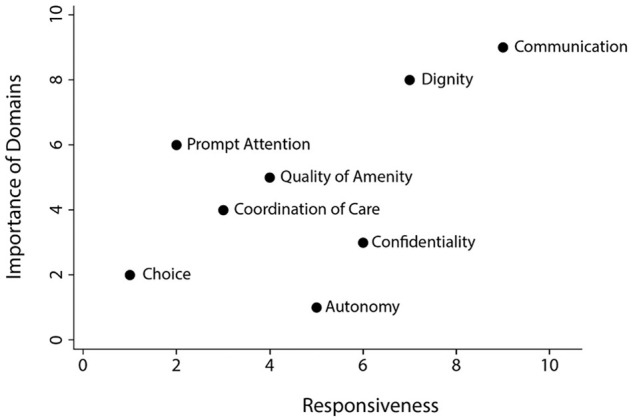
Importance and associated responsiveness of attributes of non-clinical quality of care†.
†Importance of the domains were calculated based on the patients’ individual ranking and were then crossed with the respective domains’ mean values (responsiveness).
Predictors of Non-Clinical Quality of Care
Table 3 presents the results of multivariable analyses of the 8 domains quality scores after adjustment for socioeconomic and health conditions of respondents. The mean total score showed no statistically significant difference between patients by type of health care provider (coefficient = 0.12, P = .27). However, the adjusted mean total score was significantly higher among rural patients compared to those consulting a public urban HC (coefficient = 0.2, P = .01).
Table 3.
(a) Differences in Domains and Overall Scores According to Provider Type, Adjusted for Patients’ Characteristics.†
| Dignity |
Communication |
Coordination of care |
Confidentiality |
Choice |
|
|---|---|---|---|---|---|
| Coef. CI | Coef. (CI) | Coef. (CI) | Coef. (CI) | Coef. (CI) | Coef. (CI) |
| Constant | 3.75* [3.56; 3.94] | 3.64* [3.48; 3.80] | 2.29* [2.04; 2.54] | 3.33* [3.02; 3.64] | 2.34* [1.85; 2.84] |
| Provider ref. urban PHC | |||||
| Private clinics | 0.09 [−0.15; 0.34] | −0.02 [−0.20; 0.16] | −0.62* [−0.94; −0.30] | 0.45* [0.03; 0.86] | 0.09 [−0.47; 0.66] |
| Rural PHC | −0.09 [−0.27; 0.09] | 0.07 [−0.06; 0.22] | 0.52* [0.29; 0.76] | 0.18 [−0.11; 0.47] | 0.55* [0.13; 0.97] |
| Gender ref. female | |||||
| Male | −0.006 [−0.06; 0.05] | −0.03 [−0.09; 0.02] | 0.07 [−0.01; 0.15] | 0.02 [−0.04; 0.07] | 0.02 [−0.06; 0.13] |
| Age ref. <60 years | |||||
| >60 years | 0.03 [−0.06; 0.13] | 0.04 [−0.05; 0.14] | −0.02 [−0.15; 0.09] | 0.007 [−0.09; 0.10] | 0.04 [−0.11; 0.21] |
| Education ref. university | |||||
| High school (12 years) | −0.01 [−0.11; 0.07] | 0 .08 [0.01; 0.18] | 0.03 [−0.09; 0.15] | −0.02 [−0.11; 0.07] | −0.01 [−0.16; 0.14] |
| Primary (9 years) | −0.05 [−0.14; 0.04] | 0.08 [−0.01; 0.18] | 0.05 [−0.07; 0.17] | −0.05 [−0.15; 0.04] | 0.03 [−0.11; 0.19] |
| Other | −0.08 [−0.24; 0.08] | 0.19* [0.03, 0.35] | 0.25 [0.03; 0.46] | 0.18 [0.01; 0.35] | 0.33 [0.05; 0.6] |
| Chronic conditions ref. no Ch. condition (0) | |||||
| 1 | 0.01 [−0.05; 0.08] | −0.03 [−0.09; 0.04] | 0.16* [0.06; 0.25] | −0.07 [−0.08; −0.06] | 0.04 [−0.08; 0.15] |
| ≥2 | −0.02 [−0.10; 0.07] | 0.01 [−0.07; 0.1] | 0.2* [0.07; 0.32] | 0.05 [−0.04; 0.14 | 0.04 [−0.1; 0.19] |
| Insurance ref. not insured | |||||
| Insured | −0.03 [−0.11; 0.03] | −0.01 [−0.09; 0.06] | 0.21* [0.09; 0.31] | −0.01 [−0.09; 0.07] | 0.08 [−0.05; 0.22] |
| Utilization of HC ref. (<=1) | |||||
| ≥2 | −0.001 [−0.07; 0.07] | 0.02 [−0.05; 0.09] | 0.12* [0.02; 0.21] | −0.012 [−0.08; 0.06] | 0.07 [−0.05; 0.2] |
| Benefiting SE.AID ref. no*** | 0 | ||||
| Yes | −0.08* [−0.16; 0.01] | −0.07** [−0.15; 0.01] | 0.03 [−0.07; 0.13] | −0.05 [−0.13; 0.03] | 0.11 [−0.02; 0.25] |
| Occupation ref. employed | |||||
| Unemployed | 0.06 [−0.01; 0.14] | 0.07** [−0.004; 0.14] | 0.09 [−0.008; 0.19] | 0.03 [−0.04; 0.11] | −0.11 [−0.24; 0.02] |
| Pensioner | −0.05 [−0.16; 0.05] | −0.04 [−0.01; 0.06] | 0.14* [−0.02; 0.28] | −0.06 [−0.17; 0.05] | −0.14 [−0.33; 0.04] |
| Health service ref. satisfied | |||||
| Unsatisfied | 0.09 [−0.11; 0.28] | −0.16 [−0.35; 0.03] | 0.18 [−0.06; 0.43] | 0.1 [−0.10; 0.31] | 0.29 [−0.07; 0.64] |
The analyses were conducted using linear mixed models with random intercepts for districts and facilities nested in districts. All variables were simultaneously included in the respective models. P-values were obtained from the Wald tests of the respective parameter estimates *P < .05. **P < .1. ***Benefit from social-economic support.
(b) Differences in Domains and Overall Scores According to Provider Type, Adjusted for Patients’ Characteristics.†
| Autonomy |
Prompt attention |
Qual. of Amenity |
Total mean score |
|
|---|---|---|---|---|
| Coef. CI | Coef. (CI) | Coef. (CI) | Coef. (CI) | Coef. (CI) |
| Constant | 2.80* [2.41; 3.19] | 3.44* [3.21; 3.68] | 2.94* [2.51; 3.38] | 3.05* [2.89; 3.21] |
| Provider ref. urban PHC | ||||
| Private clinics | 0.48* [−0.05; 1.02] | −0.24 * [−0.47; −0.01] | 0.8 * [0.29; 1.33] | 0.12 [−0.09; 0.34] |
| Rural PHC | 0.21 [−0.18; 0.61] | −0.13 [−0.31; 0.05] | 0.06 [−0.31; 0.43] | 0.2* [0.04; 0.36] |
| Gender ref. female | ||||
| Men | 0.04 [−0.07; 0.14] | −0.03 [−0.12; 0.05] | 0.004 [−0.08; 0.09] | 0.02 [−0.02; 0.05] |
| Age ref. <60 years | ||||
| >60 years | −0.04 [−0.21; 0.13] | 0.04 [−0.09; 0.18] | 0.11 [−0.03; 0.25] | 0.02 [−0.03; 0.09] |
| Education ref. university | ||||
| High school (12 years) | −0.08 [−0.23; 0.09] | −0.21* [−0.35; −0.08] | −0.02 [−0.15; 0.11] | −0.02 [−0.08; 0.03] |
| Primary (9 years) | 0.01 [−0.15; 0.16] | −0.27* [−0.41; −0.14] | 0.05 [−0.08; 0.18] | 0.015 [−0.07; 0.04] |
| Other | −0.01 [−0.33; 0.29] | −0.19 [−0.47; 0.08] | 0.18 [−0.05; 0.43] | 0.15 [0.04; 0.25] |
| Chronic conditions ref. no Ch. condition (0) | ||||
| 1 | 0.06 [−0.06; 0.19] | −0.16* [−0.27; −0.05] | 0.016 [−0.08; 0.11] | 0.002 [−0.04; 0.05] |
| ≥2 | 0.12 [−0.03; 0.27] | −0.16* [−0.29; −0.02] | −0.008 [−0.14; 0.12] | 0.02 [−0.03; 0.08] |
| Insurance ref. not insured | ||||
| Insured | 0.16* [0.13; 0.30] | 0.04 [−0.06; 0.16] | −0.02 [−0.13; 0.09] | 0.06* [0.01; 0.11] |
| Utilization of HC Ref. (<=1) | ||||
| ≥2 | 0.12**[−0.01; 0.25] | −0.04 [−0.14; 0.07] | 0.04 [−0.07; 0.14] | 0.03 [−0.02; 0.08] |
| Benefiting SE.AID *** ref. no | ||||
| Yes | 0.02 [−0.11; 0.16] | 0.01 [−0.11; 0.13] | 0.05 [−0.06; 0.16] | 0.005 [−0.05; 0.05] |
| Occupation ref. employed | ||||
| Unemployed | –0.10 [−0.23; 0.03] | −0.06 [−0.17; 0.05] | −0.02 [−0.13; 0.08] | 0.01 [−0.04; 0.06] |
| Pensioner | −0.14 [−0.33; 0.05] | −0.07 [−0.22; 0.08] | −0.09 [−0.25; 0.06] | −0.04 [−0.11; 0.03] |
| Health service ref. satisfied | ||||
| Unsatisfied | 0.09 [−0.31; 0.52] | 0.23 [−0.09; 0.55] | −0.14 [−0.43; 0.15] | 0.07 [−0.05; 0.21] |
The analyses were conducted using linear mixed models with random intercepts for districts and facilities nested in districts. All variables were simultaneously included in the respective models. Statistically significant, *P < .05. **P < .1. ***Benefit from social-economic support.
Patients consulting a rural PHC manifested a higher average rating on the domains of “coordination of care” (coefficient = 0.5, P < .01) and “choice” (coefficient = 0.5, P = .01) compared with patients from public urban PHC facilities.
The mixed model results showed that patients attending private providers reported lower scores on coordination of care (coefficient = −0.62, P < .01) and prompt attention (coefficient = −0.24, P = .03) in comparison to urban PHC clinics but reported a higher average scores of confidentiality (coefficient = 0.45, P = .03), quality of basic amenities (coefficient = 0.81, P = .002) and autonomy (coefficient = 0.48, P = .07).
Possession of a health insurance card was associated with a higher mean total score on quality of care (coefficient = 0.06, P = .02). Also, more frequent utilization of the facility was associated with higher mean values of the domains of “coordination of care” (coefficient = 0.12, P = .01) and—by trend—on autonomy (coefficient = 0.12, P = .07).
Patients with 1 or more chronic health conditions reported a lower average score on the “prompt attention” domain compared with those not suffering from any NCD (coefficient = −0.16, P = .03). However, they perceived experiencing better coordination of care when compared with healthy participants (coefficient = 0.16, P = .001; coefficient = 0.2, P = .001).
Discussion
This study has offered insight into the non-clinical quality of care attributes, simultaneously by measuring patients’ experience and expectations of quality among public and private PHC providers respectively, in 2 regions of Albania. The findings of this study are discussed based on the relevance of the main non-clinical quality attributes (domains) and their perceived responsiveness by healthcare provider type. Although the study instrument (questionnaire) showed overall good internal consistency, there were some outliers on confidentiality and choice domain, possibly related to lack of previous experiences with these terms by patients and diversity of items. Similar patterns of variability are however reported elsewhere in the literature.42
Quality of Care by Type of Health Care Provider
The study indicates that urban public PHC services and private outpatient clinics do perform similarly in respect to attributes of non-clinical quality of care. This is in contrast to, Bleich and colleagues who identified lower quality rates amongst private healthcare users compared to public counterparts, in a study conducted in 21 European Union countries.26 These results deviate from findings of other studies indicating that private health facilities appear to be of higher (interpersonal) process quality, including responsiveness and effort, and conceivably being more patient-orientated than public facilities.22-24
Our results do suggest that while the overall quality ratings were similar, private providers are rated better, on quality of basic amenities, confidentiality, and autonomy. Although confidentiality was well rated in terms of responsiveness (patients’ experience when receiving care, as assessed by the mean sores) (Table 2, Figure 1), this domain was considered by respondents as of comparatively low importance for consulting a PHC service (Figure 1). This aligns to other studies which identified confidentiality being a neglected aspect of care in less developed countries, partly due to lower importance given to this domain, mainly attributed to resource limitations and lack of awareness.43 One reason why confidentiality is better perceived in private sector in the present study could be linked to relatively good infrastructural conditions, appropriate space and waiting rooms. Indeed, the private providers in Albania have substantially invested in modern and updated technology and medical devices.14
At the same time, quality of basic amenities was perceived as an important attribute of quality of care (Figure 1) but were poorly rated by users of governmental services. Public health services in Albania over the last 2 decades are paradoxically perceived as a mix of poor quality in terms of infrastructure,6,14,44 yet, with highly satisfied patients45 yielding positive estimations on staff skills in terms of accurate diagnosis and staff readiness to respond on time in a kind and polite way.46
Similar perceptions do prevail when comparing urban and rural PHC experiences with the non -clinical quality of care: patients attending rural PHC were less critical and reported higher levels of agreement with the quality attributes compared to urban patients, reconfirming previous studies of rural patients being more positive about the care environment.30,47 One could argue that the reforms and efforts of the governments of Albania and their partners in improving rural PHC services by (i) refining physical infrastructure of the facilities, (ii) equipping facilities with appropriate medical devices, and (ii) fostering staff continuous education activities,45 might have positively impacted rural populations’ perception. It should be pointed out that efforts toward quality improvement initiatives and UHC have been the focus of the Albanian government. Additionally, since 2009 there has been compulsory accreditation of public and private health services providers (with an exception of laboratories), and the providers are expected to meet minimal standards of quality of care.15
The attitudes of the rural patients interviewed within the present study, may also mirror the past communism area positions of the society with strong community ties, where traditionally state-owned institutions, doctors included, were the ultimate and unquestionable authority.30,48 The findings may also reflect a lack of awareness of patients’ rights and weak, undeveloped patients’ centeredness concepts. Nevertheless, when compared with urban patients in public facilities, rural patients gave considerably lower mean values on prompt attention (Table 2), perceiving difficulties related to geographic proximity, means and costs of transport and waiting time. However, after adjustments for socioeconomic and health characteristics, these results did not yield a statistical significance when compared to urban public providers (Table 3). The pattern of differences in the mean scores between the different types of facilities did not change when analyzing the data only for Fier region, (the district that had both public and private clinics), see Supplemental Table 2. The magnitudes of differences were quite comparable with the exception of the mean value of “Choice” dimension among patients attending urban public facilities where the mean value decreased from 2.69 to 2.26 after excluding the district Diber (the district with no private clinics).
Patient-Provider Interaction: The Path Toward Informative and Participatory Decision-Making
Among the 8 non-clinical care attributes of quality, patients rated communication and dignity the highest. By contrast the choice of provider, prompt attention and coordination of care were scored lowest (Figure 1). These findings are consistent with previous research where both communication and dignity were highly rated in 5 central European countries.48 Some authors consider that this pattern can be elucidated by the historical, cultural, and social environment37 which formed populations’ expectations when encountering the health providers and health system. Also, in terms of importance of domains, as depicted from patients’ theoretical point of view, our study showed that patients, independent from using a public or private provider, agree that communication and dignity were the most important attributes of quality, followed by prompt attention. This is partly different from the outcomes of a previous study involving 41 countries who selected prompt attention as the most important domain, followed by dignity and communication.18
When averaging total scale (Table 3), patients receiving social or economic aid reported lower dignity and communication mean scores compared to those not receiving it. This aligns to previous research that has found that socio-economically disadvantaged groups are treated with less respect and inadequate communication by health workers.38
The autonomy domain incorporates the concept of patients’ empowerment and their right (including their caregivers’ rights) to medical information and their choice to refuse a medical treatment.22 However, autonomy did not appear to be among the important or even well-rated domains in our study. In fact, it was frequently rated as one of the least important domains (Figure 1). This shows that involvement of patients in treatment choices is still an evolving area, especially in the governmental sector. Some efforts are being invested by private outpatient clinics in giving patients more information about alternative types of treatments and tests; however, in our study there were not any noteworthy differences compared to the public sector. It has been argued that low attention to autonomy can be explained by persistent paternalistic behaviors of both provider and patients regarding their position with each other and within the health system.48 Patients’ voice in healthcare delivery process and community involvement on quality of care improvement initiatives are latent in Albania and have yet to be actively developed in the health system to support health policymaking.6
Prompt Attention, Choice, and Coordination of Care
When averaging ratings of responsiveness for the total population, domains of “ability to choose doctor,” “prompt attention,” and “coordination of care” were among the lowest rated, suggesting a poor performance. “Prompt attention” was ranked third by the level of importance and it was the second lowest rating by the level of responsiveness (Figure 1). This indicates that this domain is of high importance to patients but not experienced satisfactorily in the frame of their most recent PHC consultation, especially in rural settings.
Respondents receiving care from private outpatient clinics provided a low average score on the “prompt attention” domain. This may be related to 2 facts; first, private outpatient clinics operate during some hours of the day, by inviting several specialist doctors, sometimes from the capital city of Tirana or nearby countries such as doctors from Greece, Italy, or Turkey. Second, the patients attending private clinics frequently do not benefit from health insurance coverage. They may be living in close or distant villages, and they may have gone through different processes and obstacles within the public health care system prior to ending up at the private clinics. Moreover, doctors working at the same time at the public and private health sector (dual practices) and patient juggling are a concerning phenomenon, especially in low- and middle-income countries,49 making private PHC services not constantly available due to limited presences of doctors, hindering thus prompt attention, choice, and good coordination of care.14
The factors mentioned above might also explain the discontent of patients with their ability to choose the provider they want to consult about their medical condition even when choosing or transiting to the private health providers.
Sociodemographic Characteristics and Perceived Quality of Care
Our results showed that being in the possession of a health insurance card, having utilized the health service more recently and being a pensioner, were good predictors of positive quality ratings of the domains of “coordination of care” and “involvement in healing options” (autonomy). At the same, suffering from 1 or more chronic conditions were good predictors of lower quality ratings on the “prompt attention” domain and higher ratings for coordination of care. Thus, while shaping the new service delivery models, policy makers and public health researchers should emphasis the ways in which to deploy health workers and how to engage patients in treatment choices in order to deliver well-coordinated care
In the current study, people in good health were overall more critical of the quality of care, especially with the ability to choose a provider, while gender and age were no predictors of quality of care ratings. Previous studies have yielded mixed results between perceived quality and patients’ sociodemographic and health characteristics.26,35,37,47,48,50 Low perceived quality of care has been associated with users in poor health, uninsured people or users that have made fewer visits to providers.26 Other studies associate perceived good quality with older age and higher income,38 self-reported good health status and rural residency.30
Patients’ perceived quality differences may also be explained by variability of the quality instruments and the context on which the instruments have been implemented, factors related to individual characteristics, previous encounters with health care providers and the cultural, historical and geographical environment.
Study Limitations
This study has some limitations. The number of respondents who answered each item, varied from one domain to the other (selecting for example the “non applicable” answer option), reflecting variable understanding and sensitivity of respondents to 8 domains of WHO responsiveness tool. Therefore, when data was analyzed, a condition was set to have at least 75% of the all domains (6 out of 8) entirely answered. However, the mean values trend did not change even when we ran the analysis under different domains fulfilled rather than 6. The study was conducted applying a widely accepted and validated tool, however, entirely relying on self-reporting perceptions rather than measurements of an impartial observer; therefore, possible variations of the patients’ perceived non-clinical quality may be attributed to differences in patients’ characteristics, cultural aspects, previous experience and expectations rather than actual provider practice. Moreover, the questionnaire has not been validated previously in Albania. The response rate was quite high (88%), but certain categories of patients, for example younger patients did not give consent to participate. Therefore, a certain response bias cannot be excluded. Since the data collection took place during July and August, certain health conditions, typically for the other seasons (allergies or flu) might be less represented. Further, while all governmental providers in the 2 regions covered by the study participated, 3 out of 8 private out-patient provides did not consent to participate in the study. Private outpatient clinics were all located in urban areas of 1 of the 2 study regions. Consequently, the study is not in a position to analyze urban-rural differences in user perspectives on private services for both districts. This said, in Albania private services are nearly exclusively situated in urban settings so that the findings represent the general setting as prevailing in Albania. The 2 regions covered by the study make up around 16% of the territory of Albania and demographically represent around 15.7% of the population. One region (Diber) represents the mountains relatively poor part of the country while the second (Fier) is characteristic for the coastal, partially industrial settings in the country. Thus, the 2 regions reflect 2 patterns of Albania but cannot be considered as fully representing the socio-cultural and economic diversity of the country. Consequently, we cannot exclude the possibility that if applied to other regions, namely the urban context of the capital city Tirana, the results would differ. Last, given the inclusion criteria, participants had to benefit from some of outpatient care on the day of the interview; thus, people consulting PHC for other reasons such as for reimbursement of drug prescription, receiving a medical certificate or medical clearance for driving license were not included in the survey.
Conclusion
The overall perception and ratings of non-clinical quality of care by patients is similar across those consulting governmental and private services respectively in urban and rural areas. Respondents rated their experience with quality of care high, indicating that this dimension matters for consultation. Other dimensions of importance for patients independently of the type of service provider were communication and dignity. Opposite, users of public rural PHC services rated their experience with “prompt attention” considerably lower than those consulting public urban PHC services. Patients attending private outpatient clinics rated the dimension “coordination of care” as low.
Patients’ involvement in their care was not prioritized by patients and considered as a less important aspect of quality. This would suggest that relationship between health care provider and the patient should change from a “paternalistic” model to a “co-managing the illness” model, where both patients and caregivers meaningfully participate in decisions related to the healing process. Educating patients and doctors to make the most of their interactions would be an effective way to tackle the low awareness on autonomy.
Given the ageing population and concomitant rise of chronic health conditions, home care models, might be beneficial to reach out into communities and raise promptness of response of services. As Albania moves toward a better coordinated health service it will be of importance to build up an electronic medical record system so that different providers can share and exchange relevant patient information. In the absence of a consolidated health information system, lack of timely exchange of patients’ medical records, within and between public and private healthcare providers, members of the allied health workforce such as nurses could act as a point of continuity of care between patient, family and provider, improving thus coordination of care.
Supplemental Material
Supplemental material, sj-pdf-1-jpc-10.1177_2150132720970350 for Perspectives of Public and Private Primary Healthcare Users in Two Regions of Albania on Non-Clinical Quality of Care by Jonila Gabrani, Christian Schindler and Kaspar Wyss in Journal of Primary Care & Community Health
Acknowledgments
We would like to thank the team of the “Health for All Project” (Projekti HAP) for their support on the field-work. Special thanks to Besim Nuri and Susan Hamer for providing comments on the national and international context of the study. Additionally, we would like to thank Sabine Kiefer, Altina Peshkatari and Manuela Murthi, the regional coordinators of Fier and Diber region and data collectors for their outstanding contribution.
Footnotes
Author Contributions: Conceptualization, JG and KW; Data curation, JG, CS; Formal analysis, JG, CS; Methodology, JG, CS; Writing—original draft, JG; Review and editing, CS, and KW. KW made substantial contribution on critically revising the manuscript for important intellectual content. All authors contributed substantially to manuscript and agreed to the final version.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study has been conducted in the frame of the “Health for All Project” (Projekti HAP http://www.hap.org.al/) funded by the Swiss Agency for Development and Cooperation (SDC) and implemented by the Swiss Tropical and Public Health Institute. The funding agency had no role in the study design, data collection, analyses, and interpretation of the data, or preparation of the manuscript. The first author is supported by a Swiss Government Excellence Scholarship (2017.0655).
ORCID iD: Jonila Gabrani  https://orcid.org/0000-0002-8732-8193
https://orcid.org/0000-0002-8732-8193
Supplemental Material: Supplemental material for this article is available online.
References
- 1. The Lancet. Putting quality and people at the centre of health systems. Lancet. 2018;392:795. [DOI] [PubMed] [Google Scholar]
- 2. Kruk ME, Gage AD, Joseph NT, Danaei G, García-Saisó S, Salomon JA. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392:2203-2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bitton A, Ratcliffe HL, Veillard JH, et al. Primary health care as a foundation for strengthening health systems in low- and middle-income countries. J Gen Intern Med. 2017;32:566-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kringos DS, Boerma WGW, Hutchinson A, Saltman RB. Building primary care in a changing Europe. http://www.euro.who.int/en/about-us/partners/observatory/publications/studies/building-primary-care-in-a-changing-europe. 2015. [PubMed]
- 5. Maranaj Marku, Council of Europe, July 2010. Preliminary analysis on Albanian health system financing and corruption. https://rm.coe.int/16806ec8be. 2010.
- 6. Ministry of Health and Social Protection. Albanian national health strategy 2016-2020. https://shendetesia.gov.al/wp-content/uploads/2019/01/Health-Strategy-2020_eng.pdf. 2016.
- 7. Ministry of Health. National program on prevention and control of NCDs in Albania 2016-2020| ICCP Portal. https://www.iccp-portal.org/national-program-prevention-and-control-ncds-albania. 2016.
- 8. de Bruijn B, Filipi G, Nesturi M, Galanxhi E, Instituti i Statistikës. Population Ageing: Situation of Elderly People in Albania. Albania: INSTAT; 2015. [Google Scholar]
- 9. Institute of Statistics, Institute of Public Health and ICF. Albania demographic and health survey 2017-18. 2018. https://www.ishp.gov.al/wp-content/uploads/2015/04/ADHS-2017-18-Complete-PDF-FINAL-ilovepdf-compressed-1.pdf. 2018.
- 10. The Regional Office for Europe of the World Health Organization. Primary health care in Albania: rapid assessment (2018). 2018. https://www.euro.who.int/__data/assets/pdf_file/0011/373718/alb-phc-ra-eng.pdf.2018.
- 11. Compulsory Healthcare Insurance Fund. Annual Report 2013. https://www.fsdksh.com.al/images/stories/publikimet/botimet/ANNUAL%20REPORT_2013.pdf.2013.
- 12. Akshija I, Dibra A. Hospital doors under pressure; policies and trends in the major tertiary care hospital in Albania. Il G Chir. 2018;39:265-271. [PubMed] [Google Scholar]
- 13. Ministry of Health. Albania, health system overview. Presented at: Ministry of Health, Albania http://www.vhpb.org/files/html/Meetings_and_publications/Presentations/ALB92.pdf. 2016. [Google Scholar]
- 14. Uruçi E, Scalera F. Health market in Albania, problems and challenges. Interdiscip J Res Dev 2014;113:87-94. [Google Scholar]
- 15. Arqimandriti M, Ivkoviç M, Naskidashvili I, et al. Monitoring of the primary health care system in Albania. 2014. https://www.usaid.gov/sites/default/files/documents/1863/KZLN-FinalReport-%20EN%20-%20FINAL%20LES%20.pdf. 2014.
- 16. Hanefeld J, Powell-Jackson T, Balabanova D. Understanding and measuring quality of care: dealing with complexity. Bull World Health Organ. 2017;95:368-374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Boller C, Wyss K, Mtasiwa D, Tanner M. Quality and comparison of antenatal care in public and private providers in the United Republic of Tanzania. Bull World Health Organ. 2003;81:116-122. [PMC free article] [PubMed] [Google Scholar]
- 18. Valentine N, de Silva A, Kawabata K, Darby C. Health system responsiveness: concepts, domains and operationalization. In: Murray CJL, Evans DB, eds. Health Systems Performance Assessment: Debates, Methods and Empiricism. World Health Organization; 2003. [Google Scholar]
- 19. Schäfer W, Boerma WG, Kringos DS, et al. Measures of quality, costs and equity in primary health care instruments developed to analyse and compare primary care in 35 countries. Qual Prim Care. 2013;21:67-79. [PubMed] [Google Scholar]
- 20. Lévesque J-F, Haggerty J, Beninguissé G, et al. Mapping the coverage of attributes in validated instruments that evaluate primary healthcare from the patient perspective. BMC Fam Pract. 2012;13:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kruk ME, Kelley E, Syed SB, et al. Measuring quality of health-care services: what is known and where are the gaps? Bull World Health Organ. 2017;95:389-389A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berendes S, Heywood P, Oliver S, Garner P. Quality of private and public ambulatory health care in low and middle income countries: systematic review of comparative studies. PLoS Med. 2011;8:e1000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rannan-Eliya RP, Wijemanne N, Liyanage IK, et al. The quality of outpatient primary care in public and private sectors in Sri Lanka—how well do patient perceptions match reality and what are the implications? Health Policy Plan. 2015;30(suppl 1):i59-i74. [DOI] [PubMed] [Google Scholar]
- 24. Basu S, Andrews J, Kishore S, Panjabi R, Stuckler D. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. 2012;9:e1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murante AM, Seghieri C, Vainieri M, Schäfer WLA. Patient-perceived responsiveness of primary care systems across Europe and the relationship with the health expenditure and remuneration systems of primary care doctors. Soc Sci Med. 2017;186:139-147. [DOI] [PubMed] [Google Scholar]
- 26. Bleich SN, Özaltin E, Murray CJ. How does satisfaction with the health-care system relate to patient experience? Bull World Health Organ. 2009;87:271-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mayo-Bruinsma L, Hogg W, Taljaard M, Dahrouge S. Family-centred care delivery: comparing models of primary care service delivery in Ontario. Can Fam Physician. 2013;59:1202-1210. [PMC free article] [PubMed] [Google Scholar]
- 28. Tynkkynen L-K, Vrangbæk K. Comparing public and private providers: a scoping review of hospital services in Europe. BMC Health Serv Res. 2018;18:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Coarasa J, Das J, Gummerson E, Bitton A. A systematic tale of two differing reviews: evaluating the evidence on public and private sector quality of primary care in low and middle income countries. Glob Health. 2017;13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Footman K, Roberts B, Mills A, Richardson E, McKee M. Public satisfaction as a measure of health system performance: a study of nine countries in the former Soviet Union. Health Policy Amst Neth. 2013;112:62-69. [DOI] [PubMed] [Google Scholar]
- 31. Liu JJ, Bellamy G, Barnet B, Weng S. Bypass of local primary care in rural counties: effect of patient and community characteristics. Ann Fam Med. 2008;6:124-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jahan NK, Allotey P, Arunachalam D, et al. The rural bite in population pyramids: what are the implications for responsiveness of health systems in middle income countries? BMC Public Health. 2014;14(suppl 2):S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Papp R, Borbas I, Dobos E, et al. Perceptions of quality in primary health care: perspectives of patients and professionals based on focus group discussions. BMC Fam Pract. 2014;15:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Khan MS, Hashmani FN. Political and technical barriers to improving quality of health care. The Lancet. 2018;392:2146-2147. [DOI] [PubMed] [Google Scholar]
- 35. Robone S, Rice N, Smith PC. Health systems’ responsiveness and its characteristics: a cross-country comparative analysis. Health Serv Res. 2011;46:2079-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tille F, Röttger J, Gibis B, Busse R, Kuhlmey A, Schnitzer S. Patients’ perceptions of health system responsiveness in ambulatory care in Germany. Patient Educ Couns. 2019;102:162-171. [DOI] [PubMed] [Google Scholar]
- 37. Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Glob Health. 2017;2:e000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Valentine NB, Bonsel GJ, Murray CJL. Measuring quality of health care from the user’s perspective in 41 countries: psychometric properties of WHO’s questions on health systems responsiveness. Qual Life Res. 2007;16:1107-1125. [DOI] [PubMed] [Google Scholar]
- 39. Röttger J, Blümel M, Fuchs S, Busse R. Assessing the responsiveness of chronic disease care - Is the World Health Organization’s concept of health system responsiveness applicable? Soc Sci Med. 2014;113:87-94. [DOI] [PubMed] [Google Scholar]
- 40. WHO. The Health Systems Responsiveness Analytical Guidelines for Surveys in the MCSS. WHO; https://www.who.int/responsiveness/mcss/en/. 2005. [Google Scholar]
- 41. Valentine N, Darby C, Bonsel GJ. Which aspects of non-clinical quality of care are most important? Results from WHO’s general population surveys of “health systems responsiveness” in 41 countries. Soc Sci Med 1982. 2008;66:1939-1950. [DOI] [PubMed] [Google Scholar]
- 42. van der Kooy J, Valentine NB, Birnie E, et al. Validity of a questionnaire measuring the world health organization concept of health system responsiveness with respect to perinatal services in the dutch obstetric care system. BMC Health Serv Res. 2014;14:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang W, Maitland E, Nicholas S, et al. Comparison of patient perceived primary care quality in public clinics, public hospitals and private clinics in rural China. Int J Equity Health. 2017;16:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Peabody JW, DeMaria L, Smith O, Hoth A, Dragoti E, Luck J. Large-scale evaluation of quality of care in 6 countries of eastern Europe and Central Asia using clinical performance and value vignettes. Glob Health Sci Pract. 2017;5:412-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kiefer S, Kadesha B. Report on the assessment of quality of care in primary health care facilities in the two pilot regions. http://www.hap.org.al/wp-content/uploads/2017/03/Report-on-the-Assessment-of-Quality-of-Care-in-Primary-Health-Care-Facilities-in-the-two-Pilot-Regions.pdf. 2015.
- 46. Kalaja R, Myshketa R, Scalera F. Service quality assessment in health care sector: the case of durres public hospital. Procedia - Soc Behav Sci. 2016;235:557-565. [Google Scholar]
- 47. Ganguly E, Sharma PK. Client satisfaction with quality of health care in a rural area in Southern India. J Public Health Epidemiol. 2014;6:239-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Deckovic-Dukres V, Hrkal J, Németh R, Vitrai J, Zach H. Inequalities in health system responsiveness. Joint world health survey report based on data from selected central European Countries. 2007. [Google Scholar]
- 49. Slipicevic O, Malicbegovic A. Public and private sector in the health care system of the Federation bosnia and herzegovina: policy and strategy. Mater Socio-Medica. 2012;24:54-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Starfield B, Lemke KW, Herbert R, Pavlovich WD, Anderson G. Comorbidity and the use of primary care and specialist care in the elderly. Ann Fam Med. 2005;3:215-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jpc-10.1177_2150132720970350 for Perspectives of Public and Private Primary Healthcare Users in Two Regions of Albania on Non-Clinical Quality of Care by Jonila Gabrani, Christian Schindler and Kaspar Wyss in Journal of Primary Care & Community Health


