Abstract
Background
Immunotherapy has afforded new treatment options for extensive small cell lung cancer (ES‐SCLC). However, reports on the effectiveness of immune checkpoint inhibitors (ICIs) combined with chemotherapy on survival in ES‐SCLC patients are inconsistent. Therefore, we conducted a meta‐analysis on the efficacy and safety of ICI combined with chemotherapy for ES‐SCLC.
Methods
We searched for randomized controlled clinical trials related to first‐line treatment of ES‐SCLC with ICI combined with chemotherapy in PUBMED, ESMO, ASCO, and WCLC since 2018. The primary outcome was overall survival (OS).
Results
Four studies were included. Compared to chemotherapy alone, ICI in combination with chemotherapy as first‐line treatment reduced the risk of death (hazard ratio [HR]: 0.76; 95% CI: 0.68–0.86; P < 0.00001) and disease progression (HR: 0.76; 95% CI: 0.68–0.84; P < 0.00001). The objective response rate (ORR) with ICI plus chemotherapy was significantly higher than that with chemotherapy alone (HR: 1.10; 95% CI: 1.02–1.19, P = 0.01). The duration of response (DoR) rate at one year was also better with ICI plus chemotherapy (HR: 3.46; 95% CI: 2.24–5.33; P < 0.00001). Security analysis revealed that the incidence of immune‐mediated adverse events (imAEs) (HR: 3.77; 95% CI: 1.99–7.15, P < 0.0001) and grade 3/4 imAEs (HR: 7.01; 95% CI: 2.48–19.81; P = 0.0002) increased significantly with ICI plus chemotherapy.
Conclusions
ICI combined with chemotherapy as first‐line treatment can significantly improve the OS and progression‐free survival (PFS) of ES‐SCLC patients, but the toxicity caused by immunotherapy should be carefully considered.
Key points
Significant findings of the studyOur meta‐analysis shows that PD‐L1/PD‐1 plus chemotherapy can significantly improve the OS and PFS of ES‐SCLC patients when used as first‐line therapy.
What this study adds
This study fills gaps regarding the efficacy of immunotherapy combined with chemotherapy as first‐line treatment for ES‐SCLC, and provides better evidence for the use of PD‐L1/PD‐1 immunotherapy plus chemotherapy for patients with ES‐SCLC.
Keywords: First‐line treatment, immune checkpoint inhibitor, meta‐analysis, PD‐1/PD‐L1 inhibitor, small cell lung cancer

This is a meta‐analysis evaluated the efficacy and safety of PD‐L1/PD‐1 immunotherapy combined with first‐line chemotherapy for extensive small cell lung cancer. A total of 1538 patients from four trials were included in our meta‐analysis. Our study proved that PD‐L1/PD‐1 immunotherapy combined with chemotherapy can significantly improve the OS and PFS of first‐line ES‐ SCLC.
Introduction
Small cell lung cancer (SCLC) is a high‐grade lung neuroendocrine carcinoma characterized by short tumor doubling time and rapid progression. 1 , 2 Approximately 60%–65% of SCLC patients present with metastases at the time of diagnosis. 3 Moreover, although initially sensitive to chemoradiotherapy, SCLC usually recurs and progresses within six months, and current treatments are ineffective after progression. 4 Therefore, the first‐line treatment regimen for SCLC is crucial. To address the need for more effective treatments, the search for drugs that can improve survival in SCLC is ongoing. Indeed, more than 40 phase III studies have been conducted over the past 30 years. Currently, etoposide combination with platinum is the standard first‐line treatment for extensive‐stage SCLC (ES‐SCLC). However, survival has not improved substantially over the past 30 years, and the five‐year survival rate remains around 7%. 5 It can be concluded that new treatment options are urgently required for this recalcitrant cancer. 6
The genome of SCLC is complex and druggable targets are limited. 7 , 8 , 9 Although several molecular targeted agents have been tested as first‐line treatment for SCLC, none of these treatments have improved overall survival. 10 SCLC is closely associated with smoking and it has a relatively high tumor mutation burden (TMB). 11 Theoretically, SCLC is a tumor type that should benefit from immunotherapy. Immune checkpoint drugs targeting programmed death 1 (PD‐1) and programmed cell death ligand 1 (PD‐L1), two important immune checkpoints, have already been approved for use against a variety of solid tumors. Hence, immune checkpoint inhibitors (ICIs) that may improve survival have also being tested against SCLC.
The ICI nivolumab is a monoclonal antibody against PD‐1. Checkmate‐032, a multicenter, open‐label, phase I/ II trial, 12 evaluated the efficacy and safety of nivolumab monotherapy and a combination of nivolumab plus ipilimumab in patients with limit‐stage SCLC (LS‐SCLC) or ES‐SCLC after at least one platinum‐based chemotherapy regimen. The objective response rate (ORR) was 11.9% in patients receiving nivolumab monotherapy as third‐ or later‐line (3L+) treatment. The median duration of response (DoR) was 17.9 months. 13 These results suggest that nivolumab provided durable responses in patients with SCLC that had progressed even with multiple lines of treatment. The US Food and Drug Administration (FDA) subsequently approved nivolumab monotherapy for patients with metastatic SCLC with progression after platinum‐based chemotherapy and at least one other line of therapy. 13 Thus, nivolumab became the first recommended third‐line treatment option for SCLC.
Because immunotherapy elicited a sustained response in previously treated SCLC, immunotherapy was also explored as a first‐line treatment for ES‐SCLC. The first trial on PD‐1/PD‐L1 inhibitors as the first‐line treatment in patients with ES‐SCLC was IMpower133. 14 In that study, the efficacy and safety of atezolizumab plus carboplatin and etoposide was compared with those of placebo plus carboplatin and etoposide. The median overall survival (OS) increased by two months after atezolizumab plus chemotherapy, and the risk of death was reduced by 30%. The IMpower133 study was the first phase III study to show an improvement in OS following first‐line systemic treatment of ES‐SCLC for more than 30 years. In March 2019, the FDA approved atezolizumab in combination with cisplatin and etoposide for patients with ES‐SCLC as a first‐line treatment option. 15 These findings changed the standard first‐line therapy for patients with ES‐SCLC. 16
The phase III CASPIAN study was another first‐line immunotherapy trial on patients with ES‐SCLC. 17 When the results were initially published, the OS was 62.6%, and the median OS was 13.0 months in the durvalumab plus chemotherapy group, which was significantly better than that in the chemotherapy alone group (10.3 months). Recently, the results of this study were updated. 18 The OS rate increased to 82%, and the median OS rate was 12.9 months in the durvalumab plus chemotherapy group compared to 10.5 months in the chemotherapy alone group. Moreover, durvalumab plus chemotherapy reduced the risk of death by 25%. However, the durvalumab and tremelimumab plus chemotherapy groups in the CASPIAN study did not show any improvement in OS and progression‐free survival (PFS) compared to the chemotherapy group.
The KEYNOTE‐604 study was a randomized, double‐blind phase III trial comparing pembrolizumab (a PD‐1 inhibitor) plus standard‐of‐chemotherapy with standard chemotherapy in patients with previously untreated ES‐SCLC. The primary endpoints were PFS and OS. In the interim analysis, pembrolizumab plus chemotherapy was associated with improved PFS compared with chemotherapy. However, in the final analysis, although patients still benefited from prolonged PFS when using pembrolizumab plus chemotherapy, no significant improvement in OS was observed. 19 The same was true for the combination of nivolumab and chemotherapy in a separate phase II study. The median PFS of nivolumab combined with chemotherapy and chemotherapy alone were 5.5 and 4.7 months, respectively, demonstrating a significant statistical difference. 20 However, statistically significant differences in OS at the secondary end point were not observed.
From the above studies, we conclude that PD‐1/PD‐L1 inhibitors combined with chemotherapy did not achieve consistent results in terms of improved OS in patients with ES‐SCLC. A similar conclusion was reached with respect to PFS and ORR. Therefore, we conducted a meta‐analysis of data from published randomized controlled studies to further analyze the efficacy and safety of PD‐1/PD‐L1 inhibitors combined with standard chemotherapy as first‐line treatment in patients with ES‐SCLC.
Methods
Search method
A literature search was performed using PubMed for studies published up to July, 2020. Recent abstracts (since 2018) from the European Society for Medical Oncology (ESMO), American Society of Clinical Oncology (ASCO), and World Conference on Lung Cancer (WCLC) were also searched. The main search terminologies used were “small cell lung cancer OR SCLC”, “extensive disease”, “PD‐1/ PD‐L1”, “pembrolizumab”, “nivolumab”, “atezolizumab”, “durvalumab”, “avelumab”, and “chemotherapy.” Relevant references of eligible clinical trials were also manually searched.
Inclusion criteria
The suitability of the selected studies for further analysis was assessed using the following inclusion criteria: (i) prospective studies designed as randomized control trials (RCTs); (ii) trials focused on comparing PD‐1/PD‐L1 inhibitors plus chemotherapy versus chemotherapy alone in patients with untreated ES‐SCLC; (iii) SCLC confirmed by histopathology and/or cytology; (iv) studies that reported HR with 95% confidence interval (95% CI) of PFS and/or OS; (v) Abstracts that met the standards of the European Society for Medical Oncology (ESMO), America Society of Clinical Oncology (ASCO), and World Conference on Lung Cancer (WCLC) with adequate data; and (vi) higher quality study among duplicate studies.
Data extraction
General information extracted from the literature included the following: name of the study, year of publication, study phase, therapy, sample size, PFS, OS, and adverse events (AEs). Two authors (Zhang S and Li S) independently collected data in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐analyses statement 21 by carefully reading the full text of the included literature. Discrepancies in the extracted data were resolved by a third reviewer. The risk of bias of the trials was assessed using the risk of bias tool of the Cochrane Collaboration.
Statistical analysis
The meta‐analysis was performed using Review Manager version 5.3 software (RevMan; The Cochrane collaboration Oxford, United Kingdom). A Q test and I 2 were used to assess heterogeneity among the studies. A random‐effects model was used when significant heterogeneity was indicated (I 2˃50% and P < 0.10), otherwise, a fixed‐effects model was used. HR and 95% CI were collected to estimate the pooled estimates for PFS and OS. If the HR was <1.0, the treatment effect size for patients treated with PD‐1/PD‐L1 inhibitor combined with chemotherapy was considered to be greater than that for patients treated with chemotherapy alone. The odds ratio (OR) and 95% CI were used to estimate the effect of ORR, one‐year survival rate, two‐year survival rate, one‐year DoR rate, one‐year PFS rate, and toxicity. Publication bias was estimated using Begg's test and Egger's test. A two‐sided P‐value of <0.05 was used to determine statistical significance.
Results
Data characteristics and quality assessment
A total of 317 studies were identified using the initial search strategy. After excluding reviews, single‐arm design studies, and irrelevant studies, four high‐quality trials 18 , 20 , 22 , 23 were included in this meta‐analysis. The complete screening process is depicted in a flow chart in Figure 1. A total of 1538 patients were included in our meta‐analysis, including 772 patients in the PD‐1/PD‐L1 inhibitor plus chemotherapy group and 766 patients in the placebo plus chemotherapy or chemotherapy group. All four studies were prospective randomized controlled studies: three were phase III trials and one was a phase II trial. Three of the four studies were international multicenter studies, and one had been conducted in the United States. The baseline characteristics of all four trials are summarized in Table 1.
Figure 1.
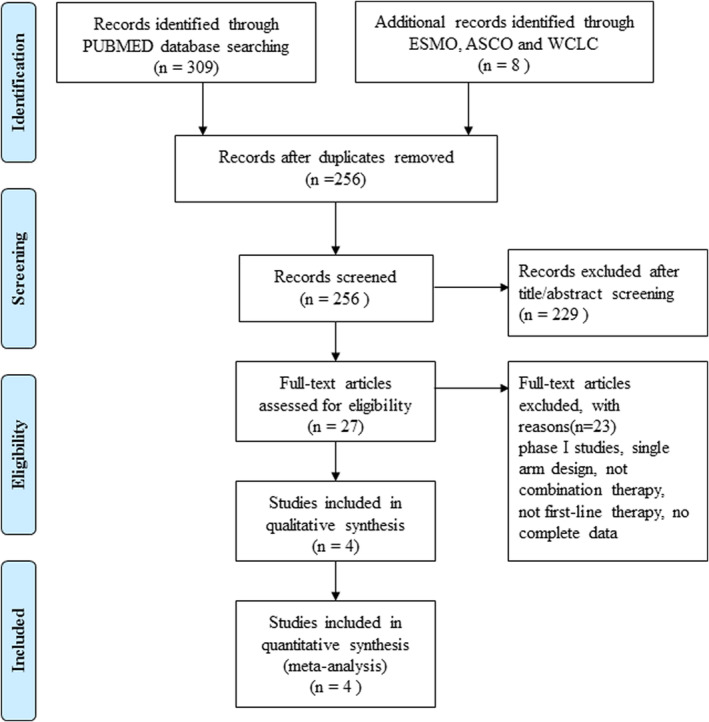
Flow chart of trial selection process.
Table 1.
Characteristics of the randomized trials included in the meta‐analysis
| Study | Latest data | Phase | Regimens (per arm) | Patients enrolled | Age<65/≥65 | Male/ female | ECOG PS(0/1) | Brain metastases |
|---|---|---|---|---|---|---|---|---|
| KEYNOTE‐604 | Rudin et al 22 | III |
Pembrolizumab + EP/EC Placebo + EP/EC |
228 225 |
115/113 101/124 |
152/76 142/83 |
60/168 56/169 |
33/195 22/203 |
| IMpower133 14 | Horn et al 14 and Reck et al 23 | III |
Atezolizumab + EC Placebo + EC |
201 202 |
111/90 106/96 |
129/72 132/70 |
73/128 67/135 |
17/184 18/184 |
| EA5161 20 | Ticiana et al 20 | II |
Nivolumab + EP/EC EP/EC |
75 70 |
NR |
35/45 36/44 |
23/57 24/56 |
NR |
| CASPIAN 17 | Paz‐Are et al 17 and Luis et al 18 | III |
Durvalumab + EP/EC EP/EC |
268 269 |
167/101 157/112 |
190/78 184/85 |
99/169 90/179 |
28/240 27/242 |
Although IMpower133 and CASPIAN were studies on PD‐L1 inhibitors combined with chemotherapy, KEYNOTE‐604 and EA5161 were studies on PD‐1 inhibitors combined with chemotherapy. Only the IMpower133 study included carboplatin plus etoposide as the chemotherapy regimen. The other three studies used either carboplatin or cisplatin. The KEYNOTE‐604 and IMpower133 studies were randomized, double‐blind, placebo‐controlled studies, with OS and PFS as the coprimary endpoints. The CASPIAN study design included three study cohorts: durvalumab combined with chemotherapy; durvalumab plus tremelimumab plus chemotherapy; and chemotherapy alone groups. The CASPIAN study reported OS as the primary endpoint. The primary endpoint of the EA5161 study was PFS. The risk of bias assessment is shown in Figure 2.
Figure 2.

Risk of bias summary.
Overall survival
OS data from the four trials were directly available, without significant heterogeneity (I 2 = 0%, P = 0.97). The pooled results show that PD‐1/PD‐L1 inhibitor plus chemotherapy significantly improved the OS of ES‐SCLC patients compared with chemotherapy alone (HR: 0.76; 95% CI: 0.68–0.86; P < 0.00001) (Fig 3a).
Figure 3.

Forest plot of meta‐analysis for (a) overall survival; (b) one‐year overall survival rate; and (c) two‐year overall survival rate.
The KEYNOTE‐604, IMpower133, and CASPIAN studies provided data for OS subgroup analysis. A combination of PD‐1/PD‐L1 inhibitor and chemotherapy significantly improved OS compared with chemotherapy only, irrespective of patient sex, male (HR: 0.79; 95% CI: 0.68–0.91; P = 0.001) versus female (HR: 0.72; 95% CI: 0.58–0.89; P = 0.003); patient Cooperative Oncology Group performance‐status (ECOG PS), ECOG PS0 (HR: 0.74; 95% CI: 0.59–0.92; P = 0.006) versus ECOG PS1 (HR: 0.80; 95% CI: 0.69–0.92; P = 0.002); patient age, ≥65 years (HR: 0.74; 95% CI: 0.62–0.89; P = 0.001) versus age < 65 years (HR: 0.80; 95% CI: 0.68–0.94; P = 0.007); or the presence/absence of baseline hepatic metastases, with baseline hepatic metastases (HR: 0.80, 95% CI: 0.67–0.96, P = 0.010) versus without baseline hepatic metastases (HR: 0.75; 95% CI: 0.64–0.87; P = 0.0002). The aggregated results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy prolonged OS in patients without brain metastases (HR: 0.75; 95% CI: 0.66–0.85; P < 0.0001), although this effect was not observed in patients with brain metastases (HR: 1.00; 95% CI: 0.69–1.44; P = 1.000) (Fig S1–S10).
Data on the one‐year survival rate and two‐year survival rate were available from three trials and two trials, respectively. The pooled results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy was more advantageous with respect to both the one‐year OS rate (HR: 1.27; 95% CI: 1.13–1.43; P < 0.0001) and the two‐year OS rate than chemotherapy alone (HR: 1.71; 95% CI: 1.29–2.27; P = 0.0002) (Fig 3b,c).
Progression‐free survival
All four trials reported PFS. No heterogeneity was identified (I 2 = 0%, P = 0.86). The pooled results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy could significantly improve PFS in patients with ES‐SCLC (HR: 0.76; 95% CI: 0.68–0.84; P < 0.00001) (Fig 4a).
Figure 4.

Forest plot of meta‐analysis for (a) progression‐free survival; and (b) and one‐year progression‐free survival rate.
Three trials reported a one‐y PFS rate. No significant heterogeneity was identified among these trials (I 2 = 0%, P = 0.64). Compared with chemotherapy alone, PD‐1/PD‐L1 inhibitor plus chemotherapy significantly improved the one‐year PFS rate (HR: 3.02; 95% CI: 2.11–4.34; P < 0.00001) (Fig 4b).
In addition, a subgroup analysis was performed based on two trials. The aggregated results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy significantly improved PFS compared with chemotherapy alone irrespective of patient sex, male (HR: 0.75; 95% CI: 0.58–0.99 P = 0.040) versus female (HR: 0.67; 95% CI: 0.53–0.87; P = 0.002); ECOG PS status, ECOG PS0 (HR: 0.74; 95% CI: 0.57–0.97; P = 0.030) versus ECOG PS1 (HR: 0.74; 95% CI: 0.62–0.88; P = 0.0005); or patient age, ≥65 years (HR: 0.74; 95% CI: 0.60–0.90; P = 0.003) versus <65 years (HR: 0.73; 95% CI: 0.60–0.89; P = 0.002). Moreover, the pooled results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy prolonged PFS in patients without brain metastases (HR: 0.71; 95% CI: 0.61–0.83; P < 0.0001) and in patients without hepatic metastases (HR: 0.67; 95% CI: 0.55–0.80; P < 0.0001). However, this effect was not observed in patients with brain metastases (HR: 1.03; 95% CI: 0.66–1.60; P = 0.900) or in patients with hepatic metastases (HR: 0.84; 95% CI: 0.67–1.06; P = 0.140) (Fig S11–S20).
Overall response rate
All four trials reported ORR. Compared to chemotherapy alone, PD‐1/PD‐L1 inhibitor plus chemotherapy significantly improved the ORR (HR: 1.10; 95% CI: 1.02–1.19; P = 0.010) (Fig 5a). No apparent heterogeneity was observed among the studies (I 2 = 23%, P = 0.27).
Figure 5.

Forest plot of meta‐analysis for (a) objective response rate; and (b) one‐year duration of response rate.
One‐year duration of response rate
Only IMpower133 reported the HR of the median DoR, although three studies reported the one‐year DoR rate data. Therefore, the one‐year DoR rate was pooled. Unlike chemotherapy only, the PD‐1/ PD‐L1 inhibitor plus chemotherapy significantly improved the one‐year DoR rate (HR: 3.46; 95% CI: 2.24–5.33; P < 0.00001). No apparent heterogeneity was observed among the studies (I 2 = 0%, P = 0.43) (Fig 5b).
Toxicity
We assessed the toxicities of immune‐mediated adverse events (imAEs) at all grades based on three trials of PD‐1/ PD‐L1 inhibitor plus chemotherapy versus chemotherapy alone, and imAEs at grade 3 or above based on two trials. The pooled estimates suggest that the PD‐1/PD‐L1 inhibitor plus chemotherapy regimen induced a significantly higher rate of both all‐grade imAEs (HR: 3.77; 95% CI: 1.99–7.15, P < 0.0001) and grade 3 or above imAEs (HR: 7.01; 95% CI: 2.48–19.81; P = 0.0002) (Fig 6a,b).
Figure 6.

Forest plot of meta‐analysis for (a) all grade immune‐mediated adverse events; and (b) grade 3 or above immune‐mediated adverse events.
Publication bias
To avoid publication bias as much as possible, trials were selected strictly according to the inclusion criteria. However, as only four studies were included, it was not possible to derive Begg's funnel plot to evaluate publication bias. A plot was, however, included only for reference. No publication bias for OS and PFS was observed from this plot (P = 1.000 and P = 0.174). To prove the robustness of our results, a sensitivity analysis was conducted. According to this analysis, the results were not affected by the exclusion of each trial, indicating that the conclusion was robust.
Discussion
Prior to the application of immunotherapy, the median OS of patients with ES‐SCLC was approximately 10 months. According to the IMpower133 study, 14 an increase in OS by almost two months could be achieved by using atezolizumab plus etoposide/carboplatin. Subsequently, the CASPIAN study confirmed that durvalumab plus chemotherapy could improve OS in ES‐SCLC. 17 Both studies established a new optimal criterion for first‐line treatment of ES‐SCLC. A series of validation studies have also been initiated using other PD‐1/PD‐L1 inhibitors. The results of several additional studies on the application of PD‐1/ PD‐L1 inhibitors in combination with chemotherapy as a first‐line treatment for ES‐SCLC have since been published.
In the present study, we conducted a meta‐analysis of published prospective studies reporting the results of first‐line treatment of ES‐SCLC with PD‐1/PD‐L1 inhibitor plus chemotherapy. In total, four prospective randomized controlled studies matched the inclusion criteria and were selected for meta‐analysis. Our results showed that PD‐1/PD‐L1 inhibitor plus chemotherapy achieved a clinically significant improvement in OS compared with standard chemotherapy alone. In addition, PFS was significantly prolonged during first‐line treatment of ES‐SCLC. However, no advantages related to ORR were noted, and immunotherapy‐related toxicity was significantly increased. This latter observation demands further careful consideration.
Although cotreatment with chemotherapy and one of the two PD‐L1 inhibitors—atezolizumab or durvalumab—prolonged the OS in patients with ES‐SCLC, cotreatment with chemotherapy and one of the two PD‐1 inhibitors—pembrolizumab or nivolumab—showed only a tendency to prolong OS (the differences in OS were not statistically significant). In addition, while the OS rate at 12 and 24 months was consistent in several studies, PD‐1/ PD‐L1 inhibitor combination chemotherapy significantly improved the OS rate at 12 and 24 months. Thus, our meta‐analysis confirmed that immunotherapy combined with chemotherapy could improve median OS, and was associated with an increase in OS at 12 and 24 months. Because immunotherapy is characterized by sustained efficacy and delayed benefit, it may not be possible to accurately evaluate the efficacy of immunotherapy using median PFS or OS as the endpoint. 24 A previous meta‐analysis of 25 non‐small cell lung cancer (NSCLC) studies found that the strongest correlation involving OS was with the OS rate at 12 months. 25 Thus, the optimal endpoint of immunotherapy may be different from that of chemotherapy and should be explored in future studies.
Brain metastasis is associated with a poor SCLC prognosis. Approximately 10%–25.8% of patients with SCLC at diagnosis had symptomatic or asymptomatic brain metastases. 26 , 27 , 28 , 29 , 30 The effects of chemotherapy in patients with brain metastasis are limited, and whole brain radiotherapy is the current therapeutic model for SCLC with brain metastasis. Recently, a Phase II study reported the preliminary efficacy of pembrolizumab for patients with NSCLC with untreated brain metastases. 31 Thus, immunotherapy may be effective for treating intracranial lesions. First‐line immunotherapy studies that enrolled ES‐SCLC patients with asymptomatic or stable brain metastases for treatment included the IMpower133, CASPIAN, and KEYNOTE‐604 trials. Nonetheless, only in the CASPIAN study (durvalumab plus chemotherapy) was the OS of all patients improved (with or without brain metastasis at baseline) compared to chemotherapy alone. 17
In the KEYNOTE‐604 study, 19 brain metastases occurred in 14.5% of patients in the pembrolizumab treatment group and 9.8% of patients in the control group. A higher proportion of patients with brain metastases were observed in the pembrolizumab in combination with chemotherapy group (in the KEYNOTE‐604 study) compared with the durvalumab in combination with chemotherapy group (10%) in the CASPIAN study or the atezolizumab plus chemotherapy group (8.5%) in the IMpower133 study. 14 , 17 The higher proportion of patients with brain metastases in the pembrolizumab treatment group could be one of the reasons why the KEYNOTE‐604 study did not achieve positive results. Overall, a total of 145 patients with brain metastasis were included in these studies, including 78 patients in the immunotherapy combined with chemotherapy group and 67 patients in the chemotherapy alone group. Therefore, the sample size was very limited. It should also be noted that the criteria for inclusion of patients with brain metastases varied among the three studies. We conclude that the question of whether immunotherapy combined with chemotherapy could be a viable therapeutic option for SCLC with brain metastasis needs further exploration.
Another factor affecting the prognosis of SCLC is liver metastasis. In total, 20.3%–44.8% of SCLC patients presented with liver metastases at the time of diagnosis. 30 , 32 , 33 It has previously been reported that the one‐year survival rate of SCLC patients with liver metastasis is less than 20%. 33 In the KEYNOTE‐189 study (2019 AACR), pembrolizumab plus chemotherapy improved PFS and OS in nonsquamous NSCLC patients with liver metastases unlike chemotherapy alone. Thus, immunotherapy may benefit patients with liver metastasis. Although patients with liver metastases were included in all three phase III studies of first‐line immunotherapy for ES‐SCLC, specific research on immunotherapy for SCLC patients with liver metastasis is lacking. In our meta‐analysis, we analyzed data from a subgroup of patients with liver metastasis. Compared with chemotherapy alone, immunotherapy in combination with chemotherapy could improve the OS in patients with liver metastasis, suggesting that immunotherapy plus chemotherapy may be a more effective treatment model for SCLC patients with liver metastasis than chemotherapy alone.
PFS is an important index of efficacy, and was used as the primary endpoint in three of the four included studies. Compared with chemotherapy alone, PD‐1/ PD‐L1 inhibitor in combination with chemotherapy showed a statistically significant improvement in PFS. However, PFS was only the secondary endpoint in the CASPIAN study, and no statistically significant difference in PFS was observed between the chemotherapy alone group and the durvalumab in combination with chemotherapy group. Over all four studies, the median PFS in the immunotherapy plus chemotherapy group was 4.8–5.5 months, while the median PFS in the chemotherapy alone group was 4.3–5.4 months. Although it was confirmed in our meta‐analysis that immunotherapy combined with chemotherapy was able to bring about a statistical improvement in PFS, the clinical significance was limited. Similarly, although the meta‐analysis suggested that ORR was statistically improved in the immunotherapy in combination with chemotherapy group, there were no breakthroughs for ORR compared with the historical data. We suggest that enrichment of the benefit population is a possible strategy to improve the effect of ES‐SCLC.
Biomarkers are key to improving the efficacy of first‐line immunotherapy for SCLC. However, studies indicate that neither the expression of PD‐L1 nor TMB could predict the efficacy of first‐line immunotherapy for ES‐SCLC. 14 , 17 , 19 Recently, studies on the molecular types of SCLC have found that SCLC with the Y subtype showed high expression of immune response‐related genes, significant T cell receptor rearrangement, and significantly high expression of HLA, suggesting that SCLC subtype Y may benefit from immunotherapy. 34 , 35 In addition, SCLC with low neuroendocrine phenotype was found to show increased levels of immune cell infiltration and higher expression of poliovirus receptor (PVR), indoleamine 2,3‐dioxygenase (IDO), major histocompatibility complex II (MHCII), and T cell immunoglobulin and mucin‐domain containing‐3 (TIM3) proteins than the high neuroendocrine phenotype. The results of these studies suggest that therapeutic strategies involving PVR, IDO, and TIM3 combined with PD‐1/ PD‐L1 inhibitors may complement each other synergistically, and that this is a potential strategy to improve the efficacy of first‐line immunotherapy for SCLC. 36
Our study has several limitations. As only four studies have been published thus far, and numerous studies on first‐line treatment of ES‐SCLC with PD‐1/PD‐L1 inhibitors in combination with chemotherapy are ongoing, the conclusions obtained from the current meta‐analysis will need to be updated and confirmed. Second, our meta‐analysis did not stratify the analysis of PD‐1 and PD‐L1 inhibitors. With accumulation of more data on PD‐1 or PD‐L1 inhibitors combined with chemotherapy, a supplementary analysis will be conducted to determine whether there is a difference in efficacy between PD‐1 inhibitor plus chemotherapy and PD‐L1 inhibitor plus chemotherapy as first‐line treatment in patients with ES‐SCLC. Finally, treatment of SCLC with CTLA‐4 (cytotoxic T lymphocyte antigen‐4) inhibitors did not provide additional benefits. Neither ipilimumab plus chemotherapy nor tremelimumab plus durvalumab and chemotherapy improved OS in patients with ES‐SCLC. Therefore, studies containing CTLA‐4 inhibitors were not included in our study. At present, new treatment modes such as PD‐1/ PD‐L1 inhibitor and chemotherapy combination plus antiangiogenic tyrosine kinase inhibitors or T cell immunoglobulin and ITIM domain (TIGIT) inhibitors are being explored for ES‐SCLC. These new regimens will hopefully show additional clinical benefits in the treatment of ES‐SCLC.
In conclusion, our meta‐analysis provides further evidence regarding first‐line treatment of ES‐SCLC with PD‐1/PD‐L1 inhibitors combined with chemotherapy. However, the combination treatment increases immune‐related toxicity, and this needs to be addressed. Future strategies to improve the effects of this first‐line treatment in patients should include analysis of biomarkers and exploration of new combined immunotherapy strategies.
Disclosure
The authors declare there are no conflicts of interest.
Supporting information
Appendix S1. Supporting Information.
References
- 1. Kojima H, Watanabe R, Isaka M et al High‐grade neuroendocrine carcinoma with bronchial intraepithelial tumor spread: Possibly a new histologic feature of large‐cell neuroendocrine carcinoma. J Thorac Oncol 2015; 10: 1337–40. [DOI] [PubMed] [Google Scholar]
- 2. Carney DN, Gazdar AF, Bepler G et al Establishment and identification of small cell lung cancer cell lines having classic and variant features. Cancer Res 1985; 45: 2913–23. [PubMed] [Google Scholar]
- 3. Bernhardt EB, Jalal SI. Small cell lung cancer. Cancer Treat Res 2016; 170: 301–22. [DOI] [PubMed] [Google Scholar]
- 4. Owonikoko TK, Behera M, Chen Z et al A systematic analysis of efficacy of second‐line chemotherapy in sensitive and refractory small‐cell lung cancer. J Thorac Oncol 2012; 7: 866–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Byers LA, Rudin CM. Small cell lung cancer: Where do we go from here? Cancer 2015; 121: 664–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. A plan of attack for deadly cancers. Cancer Discov 2014; 4: 980. American Association for Cancer Research. [DOI] [PubMed] [Google Scholar]
- 7. George J, Lim JS, Jang SJ et al Comprehensive genomic profiles of small cell lung cancer. Nature 2015; 524: 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peifer M, Fernández‐Cuesta L, Sos ML et al Integrative genome analyses identify key somatic driver mutations of small‐cell lung cancer. Nat Genet 2012; 44: 1104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rudin CM, Durinck S, Stawiski EW et al Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small‐cell lung cancer. Nat Genet 2012; 44: 1111–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Waqar SN, Morgensztern D. Treatment advances in small cell lung cancer (SCLC). Pharmacol Ther 2017; 180: 16–23. [DOI] [PubMed] [Google Scholar]
- 11. Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA, Kinzler KW. Cancer genome landscapes. Science 2013; 339: 1546–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Antonia SJ, López‐Martin JA, Bendell J et al Nivolumab alone and nivolumab plus ipilimumab in recurrent small‐cell lung cancer (CheckMate 032): A multicentre, open‐label, phase 1/2 trial. Lancet Oncol 2016; 17: 883–95. [DOI] [PubMed] [Google Scholar]
- 13. Ready NE, Ott PA, Hellmann MD et al Nivolumab monotherapy and nivolumab plus ipilimumab in recurrent small cell lung cancer: Results from the CheckMate 032 randomized cohort. J Thorac Oncol 2020; 15: 426–35. [DOI] [PubMed] [Google Scholar]
- 14. Horn L, Mansfield AS, Szczęsna A et al First‐line atezolizumab plus chemotherapy in extensive‐stage small‐cell lung cancer. N Engl J Med 2018; 379: 2220–9. [DOI] [PubMed] [Google Scholar]
- 15. First‐Line Atezolizumab OK'd for SCLC. Cancer Discov 2019; 9: 568–9. [DOI] [PubMed] [Google Scholar]
- 16. Pacheco J, Bunn PA. Advancements in small‐cell lung cancer: The changing landscape following IMpower‐133. Clin Lung Cancer 2019; 20: 148–160.e2. [DOI] [PubMed] [Google Scholar]
- 17. Paz‐Ares L, Dvorkin M, Chen Y et al Durvalumab plus platinum‐etoposide versus platinum‐etoposide in first‐line treatment of extensive‐stage small‐cell lung cancer (CASPIAN): A randomised, controlled, open‐label, phase 3 trial. Lancet 2019; 394: 1929–39. [DOI] [PubMed] [Google Scholar]
- 18. Paz‐Ares LG, Dvorkin M, Chen Y et al Durvalumab ± tremelimumab ± platinum‐etoposide in first‐line extensive stage SCLC (ES‐SCLC): Updated results from the phase III CASPIAN study. J Clin Oncol 2020; 38 (Suppl. 15): 9002. [Google Scholar]
- 19. Rudin CM, Awad MM, Navarro A et al Pembrolizumab or placebo plus etoposide and platinum as first‐line therapy for extensive‐stage small‐cell lung cancer: Randomized, double‐blind, phase III KEYNOTE‐604 study. J Clin Oncol 2020; 38: 2369–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leal T, Wang Y, Dowlati A et al Randomized phase II clinical trial of cisplatin/carboplatin and etoposide (EC) alone or in combination with nivolumab as frontline therapy for extensive‐stage small cell lung cancer (ES‐SCLC): ECOG‐ACRIN EA5161. J Clin Oncol 2020; 38 (Suppl. 15): 9000. [Google Scholar]
- 21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. Int J Surg 2010; 8: 336–41. [DOI] [PubMed] [Google Scholar]
- 22. Rudin CM, Awad MM, Navarro A et al Pembrolizumab (pembro) or placebo plus etoposide and platinum (EP) as first‐line therapy for extensive‐stage (ES) small‐cell lung cancer (SCLC). J Clin Oncol 2020; 38 (21): 2369–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reck M, Liu S, Mansfield A et al IMpower133: Updated overall survival (OS) analysis of first‐line (1L) atezolizumab (atezo) + carboplatin + etoposide in extensive‐stage SCLC (ES‐SCLC). Ann Oncol 2019; 30 (5): v710–1. [Google Scholar]
- 24. Anagnostou V, Yarchoan M, Hansen AR et al Immuno‐oncology trial endpoints: Capturing clinically meaningful activity. Clin Cancer Res 2017; 23: 4959–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Blumenthal GM, Zhang L, Zhang H et al Milestone analyses of immune checkpoint inhibitors, targeted therapy, and conventional therapy in metastatic non‐small cell lung cancer trials: A meta‐analysis. JAMA Oncol 2017; 3: e171029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Seute T, Leffers P, ten Velde GPM, Twijnstra A. Neurologic disorders in 432 consecutive patients with small cell lung carcinoma. Cancer 2004; 100: 801–6. [DOI] [PubMed] [Google Scholar]
- 27. Hirsch FR, Paulson OB, Hansen HHVJJ. Intracranial metastases in small cell carcinoma of the lung: Correlation of clinical and autopsy findings. Cancer 1982; 50: 2433–7. [DOI] [PubMed] [Google Scholar]
- 28. Seute T, Leffers P, ten Velde GP, Twijnstra A. Detection of brain metastases from small cell lung cancer: Consequences of changing imaging techniques (CT versus MRI). Cancer 2008; 112: 1827–34. [DOI] [PubMed] [Google Scholar]
- 29. Seute T, Leffers P, Wilmink JT, ten Velde GPM, Twijnstra A. Response of asymptomatic brain metastases from small‐cell lung cancer to systemic first‐line chemotherapy. J Clin Oncol 2006; 24: 2079–83. [DOI] [PubMed] [Google Scholar]
- 30. Li J, Liu F, Yu H, Zhao C, Li Z, Wang H. Different distant metastasis patterns based on tumor size could be found in extensive‐stage small cell lung cancer patients: A large, population‐based SEER study. PeerJ 2019; 7: e8163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goldberg SB, Schalper KA, Gettinger SN et al Pembrolizumab for management of patients with NSCLC and brain metastases: Long‐term results and biomarker analysis from a non‐randomised, open‐label, phase 2 trial. Lancet Oncol 2020; 21: 655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ren Y, Dai C, Zheng H et al Prognostic effect of liver metastasis in lung cancer patients with distant metastasis. Oncotarget 2016; 7: 53245–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nakazawa K, Kurishima K, Tamura T et al Specific organ metastases and survival in small cell lung cancer. Oncol Lett 2012; 4: 617–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Singh J, Luqman S, Meena A. Emerging role of phytochemicals in targeting predictive, prognostic, and diagnostic biomarkers of lung cancer. Food Chem Toxicol 2020; 144: 111592. [DOI] [PubMed] [Google Scholar]
- 35. Gay C, Diao L, Stewart C et al OA03.06 ASCL1, NEUROD1, and POU2F3 drive distinct subtypes of small cell lung cancer with unique therapeutic vulnerabilities. J Thorac Oncol 2019; 14 (10): S213. [Google Scholar]
- 36. Owonikoko TK, Dwivedi B, Chen Z et al YAP1 positive small‐cell lung cancer subtype is associated with the T‐cell inflamed gene expression profile and confers good prognosis and long term survival. J Clin Oncol 2020; 38 (suppl 15): 9019–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information.


