Abstract
Introduction
On the world stage unlimited internet access by smartphones have made in social, cultural and economic relations, has transformed the world to be faster and more efficient. In this context, health care requires more attention. Health professionals must be concerned about the majority of the patient’s care on the use of smartphone’s in this process. Smartphones can be cause distractions and cause poor patient care. Behavioral and psychological changes related to abusive and uncontrolled use in this population may create severe impacts not only on the user’s life but also on the community health care.
Method
A careful research was performed through PubMed, Web of Science and Psycho Info databases using the terms: “Smartphone addiction”, “Smartphone dependence”, “Smartphone abuse”, “physicians”, “nurses” and ‘‘health professionals”. The search covered the past 5 years up to August 2019. Articles that examine abusive use on smartphones in health professionals were included. We analyzed how this concept evolved over the last five years and hope to contribute to the better understanding of the issue and its impacts on this population and on the health care.
Results
There is a lack of specific trial instruments on screening of smartphone addiction or abusive use, tending to adopt different diagnostic criteria by the reports included. There are also a lack of studies discussing etiology of this compulsive behavior. Although known risks, published reports show there is no consciousness of abusive use and possible damages in healthcare by some health professionals. Instead, there are others that can affirm there are unpredictable risks in patient care and tend to stimulate conscience use politics in health settings. Most of them point out smartphone’s app benefits.
Conclusion
Smartphones and its functionalities became part of everyone's life by the various benefits guaranteed. However, an addictive behavior can cause damage, principally in the Health Care setting and health professional’s abusive use must be monitored. Further investigation is needed to determine the motivations of this addictive behavior and if abusive smartphone usage is a new psychiatric classification or merely the substrate of other disorders.
Keywords: Smartphone addiction, smartphone dependence, smartphone abuse, physicians, nurses, health professionals
Introduction
The facilities generated by technology and free and unlimited internet access by smartphones or other personal electronic devices have made social, cultural and economic relations fast and efficient. In our days, greater caution is indispensable in the use of technology because the overuse can cause damage to users, despite the benefits that these technologies offer.1
According to official data from the United Nations specialized agency for information and communication technologies,2 the emergence of individual users of internet and mobile occurred in 1994. From 2002, there was an increase in the use of both worldwide, reaching in 2012 almost 40% of internet users in the world population and more than 90 mobile phone subscriptions per 100 inhabitants.
Current overview
In the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-4),3 there was no recognition of any technology dependence as a distinct diagnosis, being allowed only inclusion of internet addiction in the diagnostic section of “Impulse Control, No Other Specification”, without criteria for its definition and formal diagnosis. However, in the fifth edition (DSM-5),4 more precisely in section III of the chapter “Conditions for Further Study” proposed criteria are described for what the manual calls “Internet Gaming Disorder”. It demonstrates the need observed by the American Psychiatric Association (APA) for the improvement of studies and technical-scientific investments in the area of digital dependency.
The understanding of the parameters of behaviors, risks and consequences of the use and abuse before them will enable the development of healthy habits, better use of the benefits provided and less impairment in socio-occupational, personal and environmental life. It is important to differentiate between the usual and necessary use of technologies - people who say they are dependent on having work needs for research or other work issues or for the convenience of quick contact with family and co-workers throughout the day; and harmful use - when there are significant socio-occupational losses and undesirable consequences.
There is a need to evaluate the use of these technologies in certain sectors of society. The use of the smartphone with internet access and digital devices are considered indispensable tools in academic training, which has been fostered by research practices since the beginning and requires more technology to improve techniques and dynamism in learning. Talking about a population that works directly and indirectly with the use of technology in daily practice: would it be more predisposed to harmful use inside and outside the workplace? Literature has been working to study digital dependency in patients, aiming to better understand the subject and to discuss interventionist practices. What if it is the time to discuss this worrying subject between health professionals?
Impact of smartphone usage in healthcare
It is important to note that with the explosion of smartphone applications, there was a greater possibility of rapid communication among health professionals and quick access to useful information that facilitates and improves the practice of patient care. However, smartphone use in healthcare settings may be dangerous and cause infractions to the code of health professional’s ethics (such as negligence or imprudence), consequently and more important, cause damage to patient health.5
Health professionals in patient care need to be attentive to the performance of their activities. Ssmartphones are elements of distraction, their use in service can cause inattention and errors in their procedures causing harm to their patients.6
Smartphone addiction and social media apps
In the face of smartphone social media apps, statistics from Facebook7 on 30 June 2017 reveal that the daily average is 1.32 billion active people (1.15 billion people in mobile devices), reaching monthly numbers of 2.01 billion active users. Compared to other social media platforms, more than 1 billion people in more than 180 countries used WhatsApp.8 Instagram now has more than 600 million users worldwide who capture and share more than 95 million moments daily.9 Twitter10 has 328 million users monthly active worldwide; and Snapchat now has access to more than 173 million daily users (more than 300 million active users monthly), who view about 10 billion videos per day.11 This represents an increase of more than 350% only in the last year. This data shows how much communication has changed between people in the present century and how much people resort and may be dependent on electronic devices.
In the streets, in restaurants or in any public environment we can see how much general people are holding a smartphone or other electronic device. What about in hospitals or other care scenarios? How dangerous can it be? The purpose of this review article is to discuss the studies found in the literature that aim to characterize the dependence of smartphones with health professionals, as well as any information that helps in the understanding and elaboration of diagnostic criteria, screening and the formulation of a specific theory about the subject matter.
Methods
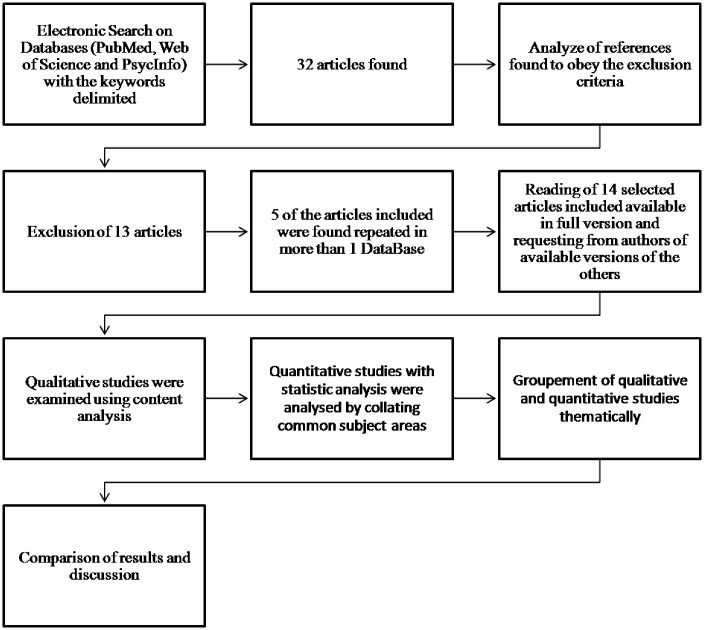
An electronic search was performed ending August 2019. It was used of electronic databases (PubMed, Web of Science and PychoInfo) was employed using the Boolean operator ‘AND’ to combine keyword “Smartphone addiction’’ or “Smartphone dependence” or “Smartphone abuse” with the following terms: ‘‘physicians’’, “nurses” and ‘‘health professionals”. Were found 32 articles (13 articles in PubMed, 16 articles in Web of Science, 3 articles in Psycho Info) and 13 articles were excluded from this review. The reference lists of these selected articles were also included in the search. Between the 19 articles included there were 5 repeated. Only articles in English and focused on smartphone usage by health professionals were included. The figure 1 above shows this process.
Figure 1.
Preferred Reporting Itmes for Systematic Reviews and Meta-Analysis – PRISMA
Results
Healthcare scenario and smartphone use: Benefits versus ill effects
In 2014, Peter J Papadakos12 in his article “Electronic distractions of the respiratory therapist and their impact on patient safety” described that, in the last decade, the explosion of personal electronic devices (PED) and social networking applications changed the way people communicate. The article was characterized as a watershed for concerns about the abusive use of technologies in healthcare environments. A 2011 New York Times article called “Distracted Physician” by Matt Richtel drew attention to the fact that several health organizations should be concerned about this problem, mainly because it affects the health of patients, and thus mobilized them to create protocols and guidelines to encourage the conscious use of technologies in the health environment during professional practice. Distractions from smartphones and mobile devices were among the top 10 items for caregivers in the United States in 2013, according to the annual list of technology risks from the Emergency Care Research Institute (ECRI). The author cites that in The Critical Care Medicine of The University of Rochester (New York) they use the process of self awareness to electronic addiction to health care professionals and public - one of the tools they uses The University of Rochester’s modified CAGE questionnaire.12 The questionnaire has been useful and highly validated screening for alcohol abuse. It has a great acceptance and comprehensiveness. The questionnaire enables each one to review their own habits in order to regulate the abusive use of PED in the professional environment and motivates a discussion on the subject. The author considers that an electronic etiquette and an education on electronic distraction is needed to minimize problems between healthcare personnel and patients’ families. The preservation of human observational skills that are being changed by electronic tools and facilities is considered paramount by the author.12
In 2015, Sumi Cho and Eunjoo Lee13 published a development of a brief instrument to measure smartphone addiction among nursing students. This instrument covers 4 factors: withdrawal, tolerance, interference with daily routines and positive expectations. This scale is about 18 items (19 previously) with demonstrated reliability and validity. This study demonstrated that nursing students who had more answers, which suggests smartphone addiction tended to be distracted at work and also to disagree with establishing smartphones education policies in healthcare scenario.13 One year later, the same Authors14 published an assessment of 312 third-year nursing students' smartphone use by a self-report questionnaire. Almost half of the students confirmed they used smartphones a couple of times and about a quarter were sometimes distracted by the usage. Additionally, the majority of them had already experienced nurses with this behavior during their work.
In 2016, JP Attri et al.15 published a review article with guidelines regarding use of smartphones in operating room and critical care scenario. In one hand, this review demonstrated various smartphones’ apps benefits in healthcare practices. The fast access to treatment guidelines and searches, as well as the fast access to procedures or laboratory results, minimizes the need for tools in medical practice, permitting intercommunication between health professionals. It can possibly lead to improvement on health care and help patients cope with diseases. In other hand, the article pointed out disadvantage of the use of these devices and established some recommendations about the safe use of them. The authors stand out only about 2-3% of people can actually multitask and devices can hurt cognitive performance as well as interfere with the medical equipment.15
Some of the studies excluded16–19 on this review showed different measurement for Smartphone addiction/dependence. However, these referred articles do not explored this addictive behavior on health professionals and for that reason were not included on this present review.
Mobile health (mHealth) apps
In 2013, Corazza, O. et al.20 published an article about The Recreational Drugs European Network Project (ReDNet project), that shows efficacy of technology-based forms of intervention on novel psychoactive substances (NPS) by recognizing products online (at its end identified 650 NPS and combinations) and publishing relevant information through some technological appliances to young people, professionals and European Union/International agencies. They contributed to national policy makers, advices to general people and health care professionals. It also concluded that web-monitoring activities are fundamental in this subject and technological tools can be successfully incorporated in specific prevention schemas.20
One year later, in 2014, Deborah S Hasin, Efrat Aharonovich, and Eliana Greenstein21 affirmed mobile technologies are a great ally in patients care and can make clinical practice faster and keep its efficiency. The authors analyzed the feasibility and acceptability of HealthCall for the smartphone (HealthCall-S) instead of Interactive voice response (HealthCall-IVR) – these technologies were proposed after brief interventions in HIV alcohol dependent patients. They highlighted that in the future, technologies may emerge offering features even more advantageous than the smartphone. HealthCall-S was very acceptable and there was a better patient engagement in the study's comparison. The authors suggested this technology could strengthen self-awareness, motivation and self-efficacy.21
In 2015, Carpenter, V. L. et al.,22 published an article about smoking cessation treatment to homeless people by a smartphone app intervention. He concluded it can be a feasible tool in clinical practice instead of psychiatric comorbidities shown on this population’s study. The app demonstrated great adherence and was considered an useful intervention. In the same year, Rosa, C. et al.,23 provides a general overview of the use of e-technologies in clinical trials research for recruitment, retention and data collection, dissemination of study results and for interventions such as prevention and treatment; and its advantages, challenges and limitations – as ethical standards and patient privacy. This article demonstrated how clinical trials have been slow in using these technologies and ensure great possibilities of improvement on clinical trials while reducing costs.23
In 2015, Pereira-Azevedo N et al.,24 published an article analyzing the participation of health professionals and Urology associations in development of Urology Mobile Health (mHealth) apps. He concluded there is a lack of specialist’s participation (principally on those targeted to patients) and lack of regulation. More than a half was free and targeted to health professionals. The authors cited mHealth can represent an essential tool in the future and can be an opportunity to improve patient’s care. The mHealth systems were also analyzed by Zapata, B.C. et al.,25 in the same year, on a Systematic Literature Review in terms of usability. They concluded there is a need of adapting Healtlh apps to users need and usability could be upgraded by the introduction of automated mechanisms.
In the same year, Mahajan, A., Bal, S. & Hahn, H.26 analized a free smartphone app for physicians to evaluate proper use criteria for Myocardial perfusion imaging and its feasibility in clinical practice. The authors found relevance on using this app in reducing healthcare costs and inappropriate radiation burden to patients. In 2015, Parker C.27 published an article that emphasizes how smartphones and websites can be used in the conduct of treatment or procedures used in obstetrics. The author mentioned efforts were made with the help of electronic devices to avoid new trauma in a patient with posttraumatic stress disorder by Rape trauma syndrome.
In 2016, Davis, T. L., DiClemente, R., & Prietula, M.,28 focused on Health’s core characteristics (penetration into populations; availability of apps; wireless broadband access to the Internet; and tethered to individuals). The authors emphasized smartphones are becoming more accessible, but there are still differences between regions around the world and between people - cultural and economic pattern. They also point out differences between mobile phones functionalities, supposed to be unlimited in the future. They ensure that if mHealth is correctly used, well adapted to individual’s behavior and life, health goals can be reached. However, health professionals need to be ready for this type of smartphone application, which is evolving from moment to moment and improving health care.28
In 2016, Mares, M.L. et al.29 published an article focused on implementation of an mHealth system, named Seva, for substance use disorders in primary care. The authors examined the initial perspectives of 53 physicians in the first year of implementation of Seva, a smartphone application that provides information on tracking and relapsing patients' health through a web portal called the Clinical Report, which at the same time, helps patients with online support, discussion, health tracking and tools to deal with patients' wishes. They concluded that patients tend to use it and receive valuable information by the app. However physicians are less leaning to monitor patients by their workload. There were concerns about efficiently monitoring patients’ interactions online in face of physician’s reluctance to engage with such a system that was used by behavioral health care providers and the addiction-focused Health Promotions team which perceived substantial benefits.29
The other studies excluded30–35 on this review were not about Smartphone use/addiction by health professionals.
Discussion
The concern about the harmful use of smartphones by health professionals is still not a topic of great scientific interest, considering the few articles12–15 found in the review that deal with this subject, despite the relevance of the topic highlighted by the few that approach it. These articles showed the lack of specific trial instruments on the screening of smartphone addiction or abusive use, tending to adoption of different diagnostic criteria by the reports included. As the subject is still new in the scientific environment, and still not well investigated or understood, there are also a lack of studies discussing etiology of this compulsive behavior (none of the articles included). Few studies are about the need to create guidelines for prevention, diagnosis and treatment of health professionals with this behavior. Published reports included show there is no consciousness of abusive use and possible damages in health care by some health professionals.13,14 The concepts of abusive use and dependence comes from the studies of chemical dependence, which is why they are still described today only in the definitions of related disorders. Can any compulsive behavior be understood as an addiction?
Of course it is essential to adopt a more sensible, evidence based policy towards mobile phone usage in our clinical practice with great caution, owing to clearly known benefits.15 Politics and education on smartphone usage should be taken in college, before becoming health professionals, aiming to enhance the quality of Health Care and patient safety.13 An awareness about the risks of smartphone use is necessary in academic and hospital settings to improve health care and prevent infractions to the code of health professional ethics (such as negligence or imprudence). In addition to the need of developing policies that encourage smart and safe use of smartphones during clinical practice,12,14 associated with the development of privacy policies on smartphone apps.23,28,29
Most of the studies20–29 today still focus on highlighting the benefits guaranteed by smartphone technology in clinical practice, focusing on health applications for smartphones and its benefits in patient care and in clinical decision or treatment. They also highlight the importance of improving the applications for patients needs and adherence. Can it represent a possible motivation for a future addiction behavior? Difficult to answer, but consists of a doubt that possibly only future researchers can figure out.
Further research is needed in the area to develop a guideline for screening and treating dependence on smartphones, with well-established criteria and universal validation.
Article limitations
Our present review was made on three databases. Although the articles unavailable were requested from the authors, we did not have access to all of them and were not able to collect as much data as intended from all studies included.14,20,27 The subject of the article is of little scientific knowledge that needs to be filled, and the lack of available data possibly narrows our results and discussion. Further research is essential to solve our challenges and point out if smartphone addiction/dependence represents a mental health problem between health professionals worldwide.
Conclusion
Smartphones and its functionalities have become part of everyone's life by the various benefits guaranteed. However, an addictive behavior can cause unpredictable damages, principally in the heath care setting and health professional’s abusive use must be monitored.
It’s imperative an education on electronic distraction and etiquette must be taught for these mentioned workers. Even in college, when the facilities generated by smartphones tools can evolve and implant the practice of excessive usage as natural, contributing to the disturbance of necessary observational skills.
Further research and investigations are needed to determine the motivations of this addictive behavior and signal if smartphone addiction/dependence is a new psychiatric classification or merely the substrate of other disorders. Finally, it should be required to develop a universal guideline for the screening and treatment to guide specialists and searches.
Acknowledgments
None.
Peer review: This manuscript was reviewed by reviewers who have chosen to remain anonymous.
Contributorship: King ALS developed the project and wrote the article; Padua MK wrote the article and discussed the data, Gonçalves LL wrote the article and discussed the data, Santana AS wrote the article and discussed the data; Nardi AE contributed to the work orientation and discussed the data.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Not applicable.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: Not applicable.
ORCID iD: Lucio Lage Gonçalves https://orcid.org/0000-0001-5189-2924
References
- 1.King AL, Nardi AE. Novas tecnologias: uso e abuso In: Associação Brasileira de Psiquiatria; Nardi AE, Silva AG, Quevedo JL, organizadores. PROPSIQ Programa de Atualização em Psiquiatria: Ciclo 3. Porto Alegre: Artmed/Panamericana, 2013, pp.9–27 (Sistema de Educação Médica Continuada a Distância, v. 2). [Google Scholar]
- 2.ITU international telecommunication union and ICTs United Nations specialized agency for information and communication technologies, www.itu.int/net4/itu-d/ icteye/FocusAreas.aspx?paramWorkArea=WTI (accessed 5 January 2020).
- 3.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: Author, American Psychiatric Association, 2000. [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing, 2013. [Google Scholar]
- 5.King ALS, Nardi AE, Cardoso A. (Organizadores). Nomofobia-Dependência do computador, internet, redes sociais? dependência do telefone celular? O impacto das novas tecnologias interferindo no comportamento humano. Editora Atheneu, RJ, 2014.
- 6.King AL, Nardi AE. Novas tecnologias: uso e abuso In: Associação Brasileira de Psiquiatria; Nardi AE, Silva AG, Quevedo JL, organizadores. PROPSIQ Programa de Atualização em Psiquiatria: Ciclo 3. Porto Alegre: Artmed/Panamericana, 2013, pp. 27. (Sistema de Educação Médica Continuada a Distância, v. 2). [Google Scholar]
- 7.Facebook. Disponível em, http://br.newsroom.fb.com/company-info/ (2017, accessed 7 October 2020).
- 8.WhatsApp. Disponível em, www.whatsapp.com/about/ (2018, accessed 7 October 2020).
- 9.Instagram. Disponível em, www.instagram.com/about/us/ (2018, accessed 7 October 2020).
- 10.Semiocast Company. Disponível em, http://semiocast.com/publications/2012_01_31_Brazil_becomes_2nd_country_on_Twitter_superseds_Japan (accessed 7 October 2020).
- 11.Snapchat Internal Data. Disponível em, www.snapchat.com/l/pt-br/ads (accessed 7 October 2020).
- 12.Papadakos PJ. Electronic distractions of the respiratory therapist and their impact on patient safety. Respir Care 2014; 59: 1306–1309. [DOI] [PubMed] [Google Scholar]
- 13.Cho S, Lee E. Development of a brief instrument to measure smartphone addiction among nursing students. Comput Inform Nurs 2015; 33: 216–224. [DOI] [PubMed] [Google Scholar]
- 14.Cho S, Lee E. Distraction by smartphone use during clinical practice and opinions about smartphone restriction policies: a cross-sectional descriptive study of nursing students. Nurse Educ Today 2016; 40: 128–133. [DOI] [PubMed] [Google Scholar]
- 15.Attri J, Khetarpal R, Chatrath V, et al. Concerns about usage of smartphones in operating room and critical care scenario. Saudi J Anaesth 2016; 10: 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee H, Ahn H, Choi S, et al. The SAMS: Smartphone addiction management system and verification. J Med Syst 2014; 38: 1. [DOI] [PubMed] [Google Scholar]
- 17.Kwon M, Kim D-J, Cho H, et al. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One 2013; 8: e83558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C-H, Lin S-H, Pan Y-C, et al. Smartphone gaming and frequent use pattern associated with smartphone addiction. Medicine (Baltimore) 2016; 95: e4068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alosaimi FD, Alyahya H, Alshahwan H, et al. Smartphone addiction among university students in Riyadh, Saudi Arabia. Saudi Med J 2016; 37: 675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Corazza O, Assi S, Simonato P, et al. Promoting innovation and excellence to face the rapid diffusion of novel psychoactive substances in the EU: the outcomes of the ReDNet project. Hum Psychopharmacol 2013; 28: 317–323. [DOI] [PubMed] [Google Scholar]
- 21.Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Addict Sci Clin Pract 2014; 9: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carpenter VL, Hertzberg JS, Kirby AC, et al. Multicomponent smoking cessation treatment including mobile contingency management in homeless veterans. J Clin Psychiatry 2015; 76: 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosa C, Campbell ANC, Miele GM, et al. Using e-technologies in clinical trials. Contemp Clin Trials 2015; 45: 41–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pereira-Azevedo N, Carrasquinho E, Cardoso de Oliveira E, et al. mHealth in urology: a review of experts’ involvement in app development. PLoS One 2015; 10: e0125547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zapata BC, Fernández-Alemán JL, Idri A, et al. Empirical studies on usability of mHealth apps: a systematic literature review. J Med Syst 2015; 39: 1. [DOI] [PubMed] [Google Scholar]
- 26.Mahajan A, Bal S, Hahn H. Myocardial perfusion imaging determination using an appropriate use smartphone application. J Nucl Cardiol 2015; 22: 66–71. [DOI] [PubMed] [Google Scholar]
- 27.Parker C. An innovative nursing approach to caring for an obstetric patient with rape trauma syndrome. J Obstet Gynecol Neonatal Nurs 2015; 44: 397–404. [DOI] [PubMed] [Google Scholar]
- 28.Davis TL, DiClemente R, Prietula M. Taking mHealth forward: examining the core characteristics. JMIR mHealth Uhealth 2016; 4: e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mares M-L, Gustafson DH, Glass JE, et al. Implementing an mHealth system for substance use disorders in primary care: a mixed methods study of clinicians’ initial expectations and first year experiences. BMC Med Inform Decis Mak 2016; 16: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tang W, Mao J, Tang S, et al. Disclosure of sexual orientation to health professionals in China: results from an online cross-sectional study. J Int AIDS Soc 2017; 20: 21416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim S-J, Cho H, Baek S-S. Effects of healthy life practice education on reported health behaviors among fourth-grade elementary school students in South Korea. J Sch Nurs 2016; 32: 397–406. [DOI] [PubMed] [Google Scholar]
- 32.Morling JR, Mackie P, Sim F, et al. Let's talk. Public Health 2017; 145: A1–A2. [DOI] [PubMed] [Google Scholar]
- 33.Kim K, Lee H, Hong JP, et al. Poor sleep quality and suicide attempt among adults with internet addiction: a nationwide community sample of Korea. PLoS One 2017; 12: e0174619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eysenbach G, Bull S, Legrand S, et al. Taking mHealth forward: examining the core characteristics. JMIR mHealth uHealth 2016; 4: e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schneider JP, Weiss R, Samenow C. Is it really cheating? Understanding the emotional reactions and clinical treatment of spouses and partners affected by cybersex infidelity. Sex Addict Compulsivity 2012; 19: 123–139. [Google Scholar]