Stroke is a leading cause of mortality. Over 30% of older adult patients with stroke die within a year of their stroke, of which over half of the deaths are after the hospitalization.1 Posthospitalization mortality is due to various etiologies (e.g., recurrent stroke, ischemic heart disease, and cancer).2 As a consequence, most stroke survivors have both a good reason and sufficient time to engage in advance care planning (ACP).
The goal of ACP is to ensure that people receive end-of-life care that is consistent with their values and preferences. Importantly, ACP increases concordance between the patient's end-of-life preferences and the care they receive and is associated with better quality of care at the end of life for the patient and improved quality of life among surviving caregivers.3,4 In this context, we sought to compare ACP engagement between stroke survivors and the general population of older adults. We hypothesize that due to the high risk of poststroke mortality, stroke survivors would have higher rates of ACP engagement than older adults who had not had a stroke.
Methods
We performed a retrospective cross-sectional analysis of community-dwelling older adults who participated in the 2018 US National Health and Aging Trends Study (NHATS). The NHATS is a nationally representative, longitudinal cohort study consisting of face-to-face interviews by trained study personnel of Medicare beneficiaries aged 65 years and older.
ACP engagement was defined as having (1) living will or advance directive; (2) durable power of attorney (DPOA); or 3) discussion of preferred medical treatment if were to become seriously ill. Stroke survivors were identified by self-report. Covariates, selected based on the prior theoretical and empirical evidence for predicting ACP engagement, were self-reported: age, sex, race, marital status (married/living with a partner vs other), nonstroke comorbidities, limitation in activities of daily living (ADLs; self-care and mobility limitations 0, 1–2, >3), and probable/possible dementia. Dementia was defined by a combination of self-report, proxy report, and assessments of memory, orientation, and executive functioning.5
We explored the association of stroke and ACP engagement (i.e., any of the 3 forms of ACP) and for each individual form, with adjusted logistic regression models including all covariates and applying survey weights. A post hoc secondary analysis included individual comorbidities.
Standard protocol approvals, registrations, and patient consents
Activities not regulated as human subjects research by the University of Michigan IRB.
Data availability
Data are freely available at nhats.org/researcher/nhats.
Results
The study population consisted of 4,820 older adults, representing 35,467,623 older Americans, including 658 (11%) stroke survivors. Compared with older adults, stroke survivors were older, less likely to be married/living with a partner (47% vs 55%, p < 0.01), more likely to have ADL limitations (45% vs 18%, p < 0.01) and had a greater number of comorbidities (mean [SD] 3.1[1.6] vs 2.4[1.3]).
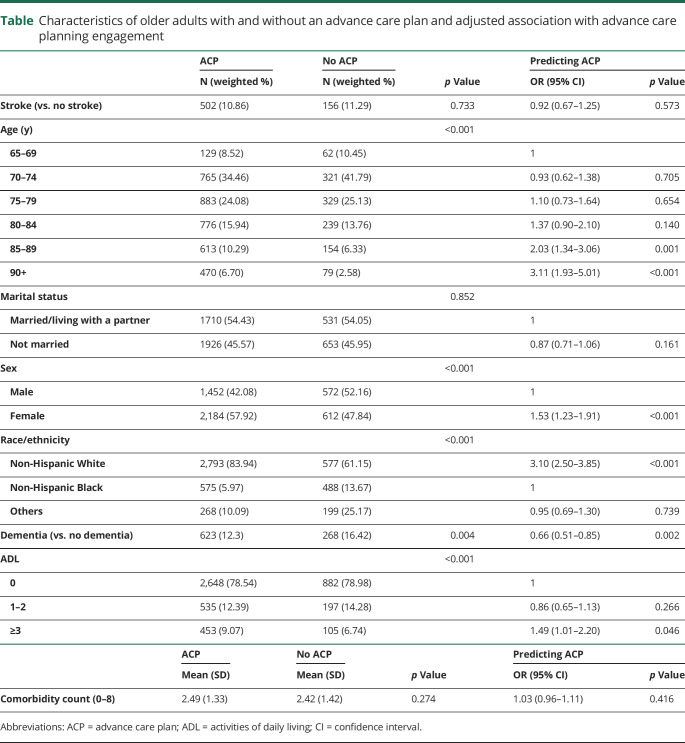
There was no difference between stroke survivors and older adults in ACP engagement (74% vs 75%, adjusted odds ratio 0.9, 95% confidence interval [CI] 0.7–1.3, p = 0.57, table), completion of living will/advance directive (55% vs 55%, aOR 1.0, 95% CI 0.8–1.3, p = 0.89), DPOA (53% vs 52%, aOR 1.0, 95% CI 0.8–1.2, p = 0.95), or discussion of end-of-life care (60% vs 62%, aOR 0.9, 95% CI 0.7–1.2, p = 0.43).
Table.
Characteristics of older adults with and without an advance care plan and adjusted association with advance care planning engagement
Those with dementia were less likely to engage in ACP (aOR 0.7, 95% CI 0.5–0.9, p < 0.01, table). The oldest old (85–89 years, aOR 2.0, 95% CI, 1.3–3.1, p < 0.01; and ≥90 years aOR 3.1, 95% CI 1.9–5, p < 0.01), women (aOR 1.5, 95% CI 1.2–1.9, p < 0.01), White people (aOR 3.1, 95% CI 2.5–3.9, p < 0.01, compared with Black people), and those with the greatest ADL limitations (aOR 1.5, 95% CI 1–2.2, p = 0.046) were more likely to engage in ACP. These associations were similar across models that explored the individual forms of ACP and that included individual comorbidities.
Discussion
In this nationally representative study of community-dwelling older adults, we found no difference in ACP engagement between stroke survivors and older adults. About 25% of US stroke survivors had not engaged in any form of ACP, results similar to a single-center stroke clinic.6 Older adults who were younger, Black, men, and have dementia were less likely than their counterparts to engage in ACP. Study limitations include that stroke, which has been shown to be reasonably reliable,7 comorbidities, and ACP were self-reported. Measures of stroke severity and time since stroke were not available. Our study population was limited to community-dwelling stroke survivors. In conclusion, despite their high poststroke mortality risk, stroke survivors are not more likely than older adults who have not had a stroke to engage in ACP. Hospital, clinic, and community strategies to introduce and encourage ACP among stroke survivors are needed.
Appendix. Authors
Study funding
This work is funded by NIH/NIA R01AG059733.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
References
- 1.Burke JF, Feng C, Skolarus LE. Divergent poststroke outcomes for black patients: lower mortality, but greater disability. Neurology 2019;93:e1664–e1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartmann A, Rundek T, Mast H, et al. Mortality and causes of death after first ischemic stroke the Northern Manhattan Stroke Study. Neurology 2001;57:2000–2005. [DOI] [PubMed] [Google Scholar]
- 3.Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Directors Assoc 2014;15:477–489. [DOI] [PubMed] [Google Scholar]
- 4.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental Health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kasper JD, Freedman VA, Spillman BC. Classification of persons by dementia status in the national Health and aging Trends study, technical paper #5. Baltimore: Johns Hopkins University School of Public Health. 2013. [Google Scholar]
- 6.Johnson PD, Ulrich A, Siv J, Taylor B, Tirschwell D, Creutzfeldt CJ. Planning after stroke survival: advance care planning in the stroke clinic. J Am Heart Assoc 2019;8:e011317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horner RD, Cohen HJ, Blazer DG. Accuracy of self-reported stroke among elderly veterans. Aging Ment Health 2001;5:275–281. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are freely available at nhats.org/researcher/nhats.