Abstract
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has seen many cardiopulmonary rehabilitation services delivering programmes remotely. One area of concern is how to assess exercise capacity when a supervised exercise test is not possible. The aim of this review was to examine the relationship between functional exercise tests and recommended exercise tests for cardiopulmonary rehabilitation.
Methods
A rapid narrative review was carried out. Searches were conducted by two of the study authors. The study had the following features. Participants: adults, all with long-term conditions; intervention: any/none; outcome: Duke activity status index (DASI), sit to stand (STS, 30 s, 1 min and 5 repetitions), short physical performance battery (SPPB), 4-metre gait speed (4MGS) or step test (Chester/others) AND directly compared to one of the recommended exercise tests for cardiopulmonary rehabilitation: 6-min walk test (6MWT), incremental shuttle walk test (ISWT) or cardiopulmonary exercise test (CPET) in terms of reporting agreement/correlation; Study design: primary research only, controlled trials or observational studies.
Results
Sixteen articles out of 249 screened were included (n=2271 patients). Overall, there were weak–strong correlations for the included tests with a recommended exercise test (r=0.38–0.85). There were few reported issues with feasibility or safety of the tests. However, all tests were supervised in a clinical setting. The test that had the highest correlation with the field walking test was the 4MGS with the ISWT (r=0.78) and with the 6MWT (r=0.85).
Discussion
The 4MGS has the highest correlation with routine measures of exercise tolerance. However, it may be difficult to standardise in a remote assessment or to prescribe exercise from. Clinicians should strive for face-to-face standardised exercise tests where possible to be able to guide exercise prescription.
Short abstract
Clinicians should strive for face-to-face standardised exercise tests where possible to be able to guide exercise prescription https://bit.ly/34saiQR
Introduction
Patients with chronic respiratory and cardiac disease benefit from centre-based rehabilitation in the form of exercise and disease management education. The benefits of this intervention have been proven in a range of outcome measures including exercise tolerance, quality of life, mood and mortality [1, 2]. Despite the known benefits, uptake to rehabilitation is poor [3, 4], and this problem is not unique to the United Kingdom [5]. To this end, recently we have seen the emergence of new programme formats that aim to improve access and uptake, including tele-rehabilitation and other home-based models. However, the evidence base for remotely delivered rehabilitation is not secure particularly in older patients with COPD [6]. Patient experience with remotely delivered healthcare is variable and will only be relevant for those who can access and engage with the technology [7, 8]. Evidence for tele-rehabilitation in the cardiac rehabilitation population is more convincing [9], perhaps due to patient demographics. All international guidelines state that an exercise programme should be individually prescribed and progressed, predicated on a measure of exercise capacity. Otherwise the programme is not recognised as pulmonary/cardiac rehabilitation (PR/CR) [10, 11]. The recent coronavirus disease 2019 (COVID-19) pandemic and ongoing social distancing measures have had a profound effect on how rehabilitation services are delivered around the world [12]. Many centres have temporarily suspended face-to-face activity and assessments have largely ceased; this has posed a challenge to rehabilitation providers, who have been unable to individually assess and prescribe the essential exercise component of the programme. Added to this, rehabilitation staff may have been redeployed to acute areas, COVID research teams or to work from home due to shielding.
Centres have risen to this challenge and turned to providing remote programmes in the form of home-based manuals, phone calls and virtual classes (tele-rehabilitation) [13]. However, there is a worry from the rehabilitation community that the effectiveness of rehabilitation may be diluted [12], particularly if no measure of exercise tolerance is completed at baseline.
Many functional exercise tests lend themselves to being conducted virtually in the home with minimal equipment (e.g. various sit to stand (STS) tests: e.g. 1-min STS [14], 4 metre gate speed (4MGS) [15], short physical performance battery (SPPB) [16] and various step tests, e.g. Chester Step test [17]). Furthermore, the Duke Activity Status Index (DASI) questionnaire has been suggested as a proxy for maximal exercise tolerance and yields a metabolic equivalents (METS) value [18] that can be converted to heart rate training zones. There is no specific national/international guidance on how to conduct virtual assessments (including exercise testing) in patients with cardiopulmonary disease, though locally developed protocols have been implemented. This is despite anxieties around safety; in particular, cardiovascular stability and oxygen desaturation when the assessment is not conducted in person. Greenhalgh and colleagues [19] have recently completed a rapid review of remote exercise testing for oxygen desaturation in COVID patients. They concluded that the 1-min sit to stand (1MSTS) and the 40-step test, validated in other lung diseases, could be considered, and a 3% decrease in pulse oximetry would be cause for concern. Furthermore, they argue that the test should not be used outside of a supervised healthcare visit if saturation was <96%. However, what has not been explored in a systematic way is the correlation between recommended measures of exercise tolerance in cardiopulmonary disease (e.g. cardiopulmonary exercise test (CPET), the 6-min walk test (6MWT) [20] or incremental shuttle walk test (ISWT) [21]) and these functional alternatives. Future research in the wake of COVID is likely to examine how reliable, practical and safe these functional measures are for virtual use and how responsive the measures to interventions such as rehabilitation. Prior to this we need to scope the literature for how valid these alternatives are for exercise prescription (i.e. how do they relate to a recommended exercise test?).
The aim of this rapid narrative review was to examine the relationship between functional exercise tests (in terms of correlation and/ or agreement) and measures of exercise tolerance, in patients with long-term conditions. Although our population of interest is those with cardiorespiratory disease, there may be useful data from other long-term conditions which could influence the review findings.
Methods
The review took place in May 2020. Searches were conducted by lead authors LHW and ED, with a third reviewer (SS) to resolve any discrepancies. The review was developed and reported using PRISMA methodology [22].
Inclusion criteria were as follows:
Participants: Adults (>18 years), all with long-term conditions.
Intervention: Any/none.
Outcome – functional tests that can be performed in the home: DASI, STS (30 s, 1 min and 5 repetitions), SPPB, 4MGS, step test (Chester/others) AND directly compared to one of the recommended standardised tests for exercise prescription: 6MWT, ISWT or CPET in terms of reporting agreement or correlation [10–11]. See previous references [20, 21] for description of the test procedures. Secondary outcomes of interest were: feasibility, safety, equipment, reliability/repeatability and sensitivity.
Study design: Primary research only, controlled trials or observational studies.
Exclusion criteria were as follows:
Participants: Paediatrics, not long-term conditions (e.g. surgical procedures).
Outcome – functional tests of interest: One of the five tests of interest not reported OR one of the five tests reported but not directly compared with a recommended exercise test for agreement/correlation. Tests that require additional equipment not routinely found in the patients’ home were excluded.
Study design: Reviews, single case studies, abstracts.
Search terms for rapid review
This was not a systematic review and as such, search terms were limited to:
SPPB Or “Short physical performance Battery” OR 4MGS OR “Four meter gait speed” OR STS OR “sit to stand” OR “step test” OR DASI OR “Duke Activity Status Index”
We then searched through the hits to apply our inclusion and exclusion criteria. Databases searched were Medline and the Allied and Complimentary Medicine Database (AMED). There were no limits set on the language or time period of publication.
Data extraction and risk of bias assessment
Data extraction was performed by all authors manually and transcribed to an Excel spreadsheet. A brief risk of bias assessment was conducted at the same time using the COSMIN taxonomy (Measurement Properties of Outcome Measurement Instruments) [23]. This is specifically designed for clinician-reported and performance-based outcome measures. For eight categories the scale is poor, fair, good or excellent. We have converted this to an average rating low/moderate or high risk of bias.
Results
Figure 1 shows the PRISMA flow diagram of screened articles. Duplicates (n=33) were removed. Reasons for exclusion were as follows: not one of the five tests of interest (n=31), no validity outcome (i.e. correlation/agreement with routine exercise tests) (n=73), not a long-term condition (n=82), paediatrics (n=4) and wrong study design/publication type (n=10).
FIGURE 1.
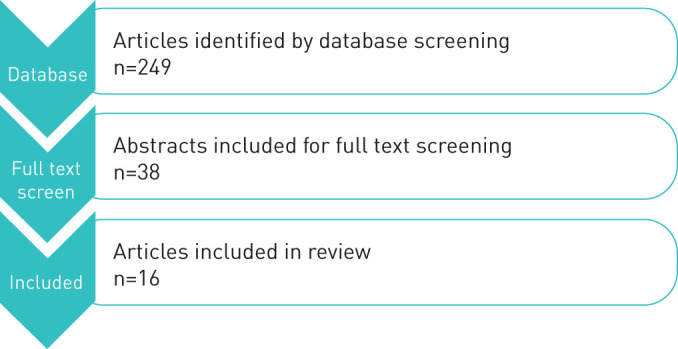
PRISMA flow diagram of screened articles.
Primary outcome
Table 1 shows details of the included articles and average risk of bias score.
TABLE 1.
Included article details and average risk of bias score
| First author year [ref.] | Outcome measure | n | Disease | Agreement/correlation to gold standard | Risk of bias |
| Briand 2018 [24] | 1-min STS | 107 | ILD | 1-min STS and 6MWT r=0.5 | Moderate |
| Carter 2002 [25] | DASI | 119 | COPD | DASI and 6MWT r=0.53 | High |
| Coute 2017 [26] | DASI | 100 | CV | Predicted METS from DASI and maximum exercise METS r=0.38 | High |
| Crook 2017 [27] | 1-min STS | 255 (2 studies combined) | COPD | 1-min STS and r=0.59 study 1 at baseline and r=0.67 at follow-up; r=0.64 study 2 at baseline and r=0.68 at follow-up | Moderate |
| Di Thommazo-Luporini 2015 [28] | Step test (6-min) | 56 | Obesity | CPET (treadmill test V′O2max) r=0.56 | High |
| Jones 2013 [29] | 5STS | 475 | COPD | ICC with ISWT −0.59 | Low |
| Kon 2013 [30] | 4MGS | 586 | COPD | 4MGS and ISWT r=0.78, 4MGS and ISWT % pred 0.72 | Moderate |
| Matkovic 2017 [31] | 4MGS | 111 | COPD | 4MGS and 6MWT r=0.85 | Moderate |
| Mori 2019 [32] | SPPB | 53 | Charcot–Marie–Tooth | ICC with 6MWT 0.35 | High |
| Meriem 2015 [33] | 1-min STS | 49 | COPD | 1-min STS and 6 MWT r=0.47 | Moderate |
| Nolan 2018 [34] | 4MGS | 46 | IPF | 4MGS and 6MWT r=0.76 | Low |
| Ozalevli 2007 [35] | 1-min STS | 53 | COPD | 1-min STS and 6MWT r=0.75 | Moderate |
| Reed 2020 [36] | DASI and Chester Step test | 50 | CV | Step test and CPET (treadmill test V′O2max) r=0.69, DASI and CPET r=0.38 | Moderate |
| Reyschler 2018 [37] | 1-min STS | 42 | COPD | 1 min STS and 6 MWT r=0.72 | Moderate |
| Wilkinson 2018 [38] | 1 min STS and 5STS | 41 | CKD | 5STS and ISWT r=0.55 time point 1 and r=0.74 at 6 weeks; 1 min STS r not reported | Moderate |
| Zhang 2018 [39] | 5STS and 30 s STS | 128 | COPD | 5STS and 6 MWT r=−0.51, 30 s STS and 6 MWT r=0.53 | Moderate |
STS: sit to stand; ILD: interstitial lung disease; 6MWT: 6-min walk test; DASI: Duke Activity Status Index; CV: cardiovascular; METS: metabolic equivalents; CPET: cardiopulmonary exercise test; V′O2max: peak oxygen uptake; ICC: intraclass correlation coefficient; ISWT: incremental shuttle walk test; 4MGS: 4-metre gait speed; SPPB: short physical performance battery; r: correlation coefficient; IPF: idiopathic pulmonary fibrosis; CKD: chronic kidney disease.
Secondary outcomes (where reported)
Feasibility
There were 12 studies that explored feasibility of outcome measures [24–26, 28–31, 34, 36–39]. These studies included the DASI, step tests, 5STS and 4MGS. Reported completion of the tests ranged from 85 to 100%. The DASI was reported to be completed by 100% of participants in the studies. One study reported that 7% of patients failed to complete the 30STS [39]. All studies explored the test in a hospital or outpatient setting under supervision, and therefore it may not be feasible to perform these in a home-based environment.
Safety/equipment
The equipment used in the listed tests include a step, chair, stopwatch, 4-metre track and in some instances a heart rate/oxygen saturation monitor. The step and chair heights, where described, would be a standardised height between patients and between testing time points (e.g. pre- and post-intervention). Two studies stated that the haemodynamic stress was lower for STS tests when compared to a 6MWT [33, 35]. None of the included studies reported any serious adverse events when performing the tests. However the tests were performed in clinical settings under supervision.
Reliability/repeatability
Seven studies assessed the reliability and repeatability of the tests [27, 29–30, 34, 37–39]. Inter-rater reliability was the most commonly reported measure using intraclass correlation coefficient (ICC). These were all moderate, good or excellent, range 0.68 (5STS [38]) and 0.99 (4MGS [30, 34], STS [27, 29]). Test re-test ICCs were good where reported (0.93–0.97) [27, 29–30, 34]. Two studies reported limits of agreement between two testing sessions for the 4MGS: these were 0.09 to −0.09 [34] and 0.135 to −0.125 [30]. One study examined the limits of agreement for the peak oxygen uptake (V′O2) predicated from the DASI questionnaire and Chester Step test with the CPET [36]. Both tests overestimated V′O2 when compared to the CPET: DASI by 3.6 mL·kg·min−1 and the step test by 4.1 mL·kg·min−1. One study compared nadir oxygen saturation measured by pulse oximetry (SpO2) in the 1-min STS test to the 6MWT: the agreement ICC was 0.77 [24].
Sensitivity
Many of the studies were single time point/not testing response to an intervention. However, the sensitivity of the tests was explored in six studies, generally following exercise-based rehabilitation [27, 29, 34, 36, 38–39]. One study suggested a minimal important difference (MID) for the 5STS in patients with COPD of 1.3–1.7 s [29] and the MID for this outcome was reported as 7.5 s in patients with chronic kidney disease (CKD) [38]. For the 1-min STS, one study found an MID of 3 reps in COPD [27] and 4 reps in CKD [38]. Zhang et al. [39] reported receiver operating characteristic (ROC) curves and showed that the area under the curve (AUC) of the 5STS score in predicting poor 6-min walk distance (6MWD of <350 m) was 0.731, whereas the AUC of the 30STS score was 0.724, indicating that both tests are useful tools in predicting 6MWT performance. The 4MGS improved significantly following pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis (IPF) (mean (95% CI) change: 0.16 (0.12–0.20) m·s−1), effect size 0.65 [34]). In the cardiovascular study comparing DASI and the Chester Step test to the CPET, the change in DASI was 2.3±5 and for the Chester Step test the change was 1.9±5 mL·kg·min−1 [36].
Discussion
This rapid review included 16 studies (2271 patients) with the aim of comparing functional exercise tests with recommended exercise tests in order to guide exercise prescription in patients with long-term conditions. Thirteen out of 16 studies were conducted in our population of interest (cardiopulmonary). This review was intended as a rapid review to guide practice in terms of exercise prescription. Searches were performed systematically and inclusion was assessed independently by two authors (ED/LHW). However, search terms were limited, and there were a large number of texts that were not included as they did not compare the agreement/correlation between the test of interest to a standard test, despite conducting a standard test in their study. Given the time scale of the rapid review, authors were not contacted for additional data. This may affect the review conclusions. Since this review was conducted, one study has assessed the 1-min STS with the 6MWT (r=0.82) and CPET (r=0.71); however, this was in a small sample (n=15) of interstitial lung disease patients with a high risk of bias [40]. Therefore, this would not change the conclusion of this review. Furthermore, a rapid risk of bias assessment was performed by the authors; most studies (10 out of 16) were at moderate risk of bias, which again may affect our findings.
It is imperative that cardiopulmonary rehabilitation is reinstated to a high standard as quickly as possible due to the importance of the intervention and the effects that shielding and isolation have on deconditioning [41]. Overall there was weak to strong correlations for the included tests (STS tests, step tests, DASI, 4MGS, SPPB) with recommended exercise tests (CPET, ISWT, 6MWT) (r=0.38–0.85). The tests generally had good to excellent reliability and repeatability. The test that correlated most highly with exercise tests was the 4MGS with the ISWT (r=0.78 [30]) and with the 6 MWT (r=0.85 [31]). This test was also shown to be sensitive to change following exercise rehabilitation in IPF (medium effect size of 0.65 [34]). The study by Kon et al. [30] reported 90% feasibility to perform the 4MGS in a home environment, though this was taken from a previous study [42] and not their own, which was performed in a hospital clinic. There were few reported issues with feasibility or safety in the included tests; only one study [39] reported that 7% of patients failed to complete the 30STS presumably due to fatigue. However, all tests included in this review were conducted in a supervised setting. Therefore the feasibility and safety of these measures in the home warrant further consideration.
Risk assessment should be performed prior to virtual assessment via a subjective assessment, medical notes screening and/or a risk assessment proforma to identify patients who are safe to perform these tasks at home [43, 44], and the usual contraindications to exercise testing will remain [10, 45] alongside local Standard Operating Procedures. Consideration should be given to patients that have cardiovascular instability and exercise-induced desaturation. Ideally a patient's heart rate response and oxygen saturation would be measured during exercise testing and in the recovery period, which has implications for equipment provision if intended to be performed in the home. Monitoring of symptoms (i.e. Borg breathlessness and perceived exertion scales) may help to guide exercise prescription, alongside the rise in wearable technology which would facilitate increased monitoring at home. Other equipment required is an important consideration. If performing tests at home, it will be difficult to standardise the test due to chair or step height discrepancies, course length, etc., though within-individual comparisons would be possible if the same height of chair/step and course length was used pre- and post-intervention. Safety in terms of avoiding trips and falls is of particular concern with steps.
Virtual assessment also relies on technology provision and digital literacy, which is known to be poor among patients with respiratory disease [8], and therefore non-technology-based alternatives are important. Provision of devices and training may be required for patients prior to assessment. All participants included in this review performed the test in a hospital environment, and therefore we do not know the implications of performing these tests at home. Furthermore, there will be local decisions that need to be made about the best virtual platform depending on what is considered safe in terms of data security and confidentiality.
This review excluded studies that required additional equipment; however, there is evidence for use of the 6-min stepper test in respiratory disease. These studies explore feasibility, comparison to 6MWT and sensitivity to PR [46]. We excluded two studies on cystic fibrosis [47–48]. Though these studies compared the 1-min STS to a standard (CPET), they looked at the relationship between cardiorespiratory variables and not the actual test results (e.g. Watts versus STS strokes). Of note the agreement in V′O2max in these studies derived from STS and CPET ranged between r=0.59 and 0.98. This review included studies that explored long-term conditions, and as a result, a number of studies exploring the DASI in pre/post-surgical patients were excluded. The DASI has previously been used in cardiac rehabilitation to prescribe target heart rate for exercise training and has been found to provide broadly equivalent MET levels to a CPET. This may be of value given that it is a functional questionnaire and carries minimal safety and feasibility implications. Though the 4MGS performed the best when compared to recommended exercise tests, this does raise issues in how to prescribe exercise from this test as you can from the ISWT and 6MWT [49]. Rehabilitation should include prescribed exercise, and if it is not possible to derive exercise prescription, standard rehabilitation has not been delivered. This will have clinical implications for the patients, for service provision and for national audit reporting.
Based on the results of this review, the 4MGS had the best correlation with exercise tests; however, it may be difficult to standardise in a home environment/during a virtual assessment. These findings are surprising given that the 4MGS is not a maximal test, and patients can walk at their own speed. There is scope to perform the subjective assessment at home and an exercise test in a clinical or community setting. Practical considerations for infection prevention and how this might impact on a walking test, such as wearing a mask, may impact validity, although some evidence indicates that there is minimal alteration in peak ventilation when a mask is worn [50–51]. With a potential second wave predicted for autumn/winter 2020 it is important that we futureproof rehabilitation to enable assessments and programmes without delay. Clinicians should strive for face-to-face services with standardised exercise tests where possible to be able to guide exercise prescription. However, the current situation provides an opportunity for services to evaluate the efficacy of providing interventions delivered in the home/virtually. Future research should examine how feasible, reliable and safe these functional tests are for virtual use and how responsive they are to rehabilitation delivered virtually.
Footnotes
Conflict of interest: L. Houchen-Wolloff has nothing to disclose.
Conflict of interest: E. Daynes has nothing to disclose.
Conflict of interest: A. Watt has nothing to disclose.
Conflict of interest: E. Chaplin has nothing to disclose.
Conflict of interest: N. Gardiner has nothing to disclose.
Conflict of interest: S. Singh has nothing to disclose.
References
- 1.Anderson L, Thompson DR, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016; 2016: CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2: CD003793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.British Heart Foundation National Audit of Cardiac Rehabilitation (NACR) Quality and Outcomes Report 2018 https://www.bhf.org.uk/informationsupport/publications/statistics/national-audit-of-cardiac-rehabilitation-quality-and-outcomes-report-20184 Date last accessed: 9 September 2020.
- 4.Royal College of Physicians, British Thoracic Society Pulmonary Rehabilitation: Steps to breathe better. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: Clinical audit of Pulmonary Rehabilitation services in England and Wales. 2015 https://www.rcplondon.ac.uk/projects/outputs/pulmonary-rehabilitation-steps-breathe-better Date last accessed: 9 September 2020.
- 5.Spitzer KA, Stefan MS, Priya A, et al. Participation in pulmonary rehabilitation after hospitalization for chronic obstructive pulmonary disease among Medicare beneficiaries. Ann Am Thorac Soc 2019; 16: 99–106. doi: 10.1513/AnnalsATS.201805-332OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaw G, Whelan ME, Armitage LC, et al. Are COPD self-management mobile applications effective? A systematic review and meta-analysis. NPJ Prim Care Respir Med 2020; 30: 11. doi: 10.1038/s41533-020-0167-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dinesen B, Huniche L, Toft E. Attitudes of COPD patients towards tele-rehabilitation: a cross-sector case study. Int J Environ Res Public Health 2013; 10: 6184–6198. doi: 10.3390/ijerph10116184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polgar O, Aljishi M, Barker RE, et al. Digital habits of PR service-users: implications for home-based interventions during the COVID-19 pandemic. Chron Respir Dis 2020; 17: 1479973120936685. doi: 10.1177/1479973120936685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rawstorn JC, Gant N, Rolleston A, et al. End users want alternative intervention delivery models: usability and acceptability of the REMOTE-CR Exercise-Based Cardiac Telerehabilitation Program. Arch Phys Med Rehabil 2018; 99: 2373–2377. doi: 10.1016/j.apmr.2018.06.027 [DOI] [PubMed] [Google Scholar]
- 10.British Association for Cardiovascular Prevention and Rehabilitation The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation. 2017 http://www.bacpr.com/resources/6A7_BACR_Standards_and_Core_Components_2017.pdf Date last accessed: 9 September 2020.
- 11.Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013; 68: Suppl 2, ii1–i30. doi: 10.1136/thoraxjnl-2013-203808 [DOI] [PubMed] [Google Scholar]
- 12.Houchen-Wolloff L, Steiner MC. Pulmonary rehabilitation at a time of social distancing: prime time for tele-rehabilitation? Thorax 2020; 75: 446–447. doi: 10.1136/thoraxjnl-2020-214788 [DOI] [PubMed] [Google Scholar]
- 13.Babu AS, Arena R, Ozemek C, et al. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol 2020; 36: 792–794. doi: 10.1016/j.cjca.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills 1995; 80: 163–166. doi: 10.2466/pms.1995.80.1.163 [DOI] [PubMed] [Google Scholar]
- 15.Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc 2003; 51: 314–322. doi: 10.1046/j.1532-5415.2003.51104.x [DOI] [PubMed] [Google Scholar]
- 16.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000; 55: M221–M231. doi: 10.1093/gerona/55.4.M221 [DOI] [PubMed] [Google Scholar]
- 17.Buckley JP, Sim J, Eston RG, et al. Reliability and validity of measures taken during the Chester step test to predict aerobic power and to prescribe aerobic exercise. Br J Sports Med 2004; 38: 197–205. doi: 10.1136/bjsm.2003.005389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 1989; 64: 651–654. doi: 10.1016/0002-9149(89)90496-7 [DOI] [PubMed] [Google Scholar]
- 19.Greenhalgh T, Javid B, Knight M, et al. What Is the Efficacy and Safety of Rapid Exercise Tests for Exertional Desaturation in Covid-19? CEBM, 2020. https://www.cebm.net/covid-19/what-is-theefficacy-and-safety-of-rapid-exercise-tests-for-exertional-desaturation-in-covid-19/ Date last accessed: 9th September 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982; 284: 1607–1608. doi: 10.1136/bmj.284.6329.1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh SJ, Morgan MD, Scott S, et al. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992; 47: 1019–1024. doi: 10.1136/thx.47.12.1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mokkink LB, de Vet HCW, Prinsen CAC, et al. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual Life Res 2018; 27: 1171–1179. doi: 10.1007/s11136-017-1765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briand J, Behal H, Chenivesse C, et al. The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease. Ther Adv Respir Dis 2018; 12: 1753466618793028. doi: 10.1177/1753466618793028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carter R, Holiday DB, Grothues C, et al. Criterion validity of the Duke Activity Status Index for assessing functional capacity in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2002; 22: 298–308. doi: 10.1097/00008483-200207000-00014 [DOI] [PubMed] [Google Scholar]
- 26.Coute RA, Ehrenfeld JM, Gupta DK, et al. Electronically self-assessed functional capacity and exercise testing: a comparison of the Duke Activity Status Index and Patient-Reported Outcomes Measurement Information System tools. Am Heart J 2017; 188: 82–86. doi: 10.1016/j.ahj.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 27.Crook S, Busching G, Schultz K, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur Respir J 2017; 49: 1601871. doi: 10.1183/13993003.01871-2016 [DOI] [PubMed] [Google Scholar]
- 28.Di Thommazo-Luporini L, Pinheiro CL, Luporini R, et al. The six-minute step test as a predictor of cardiorespiratory fitness in obese women. Eur J Phys Rehabil Med 2015; 51: 793–802. [PubMed] [Google Scholar]
- 29.Jones SE, Kon SS, Canavan JL, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax 2013; 68: 1015–1020. doi: 10.1136/thoraxjnl-2013-203576 [DOI] [PubMed] [Google Scholar]
- 30.Kon SS, Patel MS, Canavan JL, et al. Reliability and validity of 4-metre gait speed in COPD. Eur Respir J 2013; 42: 333–340. doi: 10.1183/09031936.00162712 [DOI] [PubMed] [Google Scholar]
- 31.Matkovic Z, Cvetko D, Rahelic D, et al. Nutritional status of patients with chronic obstructive pulmonary disease in relation to their physical performance. COPD 2017; 14: 626–634. doi: 10.1080/15412555.2017.1386643 [DOI] [PubMed] [Google Scholar]
- 32.Mori L, Prada V, Signori A, et al. Outcome measures in the clinical evaluation of ambulatory Charcot-Marie-Tooth 1A subjects. Eur J Phys Rehabil Med 2019; 55: 47–55. doi: 10.23736/S1973-9087.18.05111-0 [DOI] [PubMed] [Google Scholar]
- 33.Meriem M, Cherif J, Toujani S, et al. Sit-to-stand test and 6-min walking test correlation in patients with chronic obstructive pulmonary disease. Ann Thorac Med 2015; 10: 269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nolan CM, Maddocks M, Maher TM, et al. Phenotypic characteristics associated with slow gait speed in idiopathic pulmonary fibrosis. Respirology 2018; 23: 498–506. doi: 10.1111/resp.13213 [DOI] [PubMed] [Google Scholar]
- 35.Ozalevli S, Ozden A, Itil O, et al. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir Med 2007; 101: 286–293. doi: 10.1016/j.rmed.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 36.Reed JL, Cotie LM, Cole CA, et al. Submaximal Exercise Testing in Cardiovascular Rehabilitation Settings (BEST Study). Front Physiol 2019; 10: 1517. doi: 10.3389/fphys.2019.01517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reyschler G, Boucard E, Peran L, et al. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin Resp J 2017; 12: 1247–1256. doi: 10.1111/crj.12658 [DOI] [PubMed] [Google Scholar]
- 38.Wilkinson TJ, Xenophontos S, Gould DW, et al. Test–retest reliability, validation, and ‘minimal detectable change’ scores for frequently reported tests of objective physical function in patients with non-dialysis chronic kidney disease. Physiother Theory Pract 2019; 35: 565–576. doi: 10.1080/09593985.2018.1455249 [DOI] [PubMed] [Google Scholar]
- 39.Zhang Q, Li YX, Li XL, et al. A comparative study of the five-repetition sit-to-stand test and the 30-second sit-to-stand test to assess exercise tolerance in COPD patients. Int J Chron Obstruct Pulmon Dis 2018; 13: 2833–2839. doi: 10.2147/COPD.S173509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Labrecque PT, Harvey J, Nadreau É, et al. Validation and cardiorespiratory response of the 1-min sit-to-stand test in interstitial lung disease. Med Sci Sports Exerc 2020; 10: 1249. [DOI] [PubMed] [Google Scholar]
- 41.Middleton A, Simpson KN, Bettger JP, et al. COVID-19 pandemic and beyond: considerations and costs of telehealth exercise programs for older adults with functional impairments living at home – lessons learned from a pilot case study. Phys Ther 2020; 100: 1278–1288. doi: 10.1093/ptj/pzaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Simonsick EM, Maffeo CE, Rogers SK, et al. Methodology and feasibility of a home-based examination in disabled older women: the Women's Health and Aging Study. J Gerontol A Biol Sci Med Sci 1997; 52: M264–M274. doi: 10.1093/gerona/52A.5.M264 [DOI] [PubMed] [Google Scholar]
- 43.Brough C, Boyce S, Houchen-Wolloff L, et al. Evaluating the interactive web-based program, activate your heart, for cardiac rehabilitation patients: a pilot study. J Med Internet Res 2014; 16: e242. doi: 10.2196/jmir.3027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chodzko-Zajko WJ, Resnick B, Ory MG. Beyond screening: tailoring physical activity options with the EASY tool. Transl Behav Med 2012; 2: 244–248. doi: 10.1007/s13142-012-0134-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014; 44: 1428–1446. doi: 10.1183/09031936.00150314 [DOI] [PubMed] [Google Scholar]
- 46.Grosbois JM, Riquier C, Chehere C, et al. Six-minute stepper test: a valid clinical exercise tolerance test for COPD patients. Int J Chron Obstruct Pulmon Dis 2016; 11: 657–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gruet N, Peyre-Tartaruga L, Mely L, et al. The 1-minute sit-to-stand test in adults with cystic fibrosis: correlations with cardiopulmonary exercise test, 6-minute walk test, and quadriceps strength. Resp Care 2016; 61: 1620–1628. doi: 10.4187/respcare.04821 [DOI] [PubMed] [Google Scholar]
- 48.Radtke T, Hebestreit H, Puhan M, et al. The 1-min sit-to-stand test in cystic fibrosis – insights into cardiorespiratory responses. J Cyst Fibros 2017; 16: 744–751. doi: 10.1016/j.jcf.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 49.Dunagan J, Adams J, Cheng D, et al. Development and evaluation of a treadmill-based exercise tolerance test in cardiac rehabilitation. Proc (Bayl Univ Med Cent) 2013; 26: 247–251. doi: 10.1080/08998280.2013.11928972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johns DP, Ingram C, Booth H, et al. Effect of a microaerosol barrier filter on the measurement of lung function. Chest 1995; 107: 1045–1048. doi: 10.1378/chest.107.4.1045 [DOI] [PubMed] [Google Scholar]
- 51.Roberge RJ, Coca A, Williams WJ, et al. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care 2010; 55: 569–577. [PubMed] [Google Scholar]


