Abstract
Background
Unaffordability of medications is a barrier to effective treatment. Cost-related nonadherence (CRN) is a crucial, widely used measure of medications access.
Objectives
Our study examines the current national prevalence of and risk factors for CRN (e.g., not filling, skipping or reducing doses) and companion measures in the US Medicare population.
Research Design
Survey-weighted analyses included logistic regression and trends 2006–2016.
Subjects
Main analyses used the 2016 Medicare Current Beneficiary Survey. Our study sample of 12,625 represented 56 million community-dwelling beneficiaries.
Measures
Additional outcome measures were spending less on other necessities in order to pay for medicines and use of drug cost reduction strategies such as requesting generics.
Results
In 2016, 34.5% of enrollees under 65 years with disability and 14.4% of those 65 years and older did not take their medications as prescribed due to high costs; 19.4% and 4.7%, respectively, experienced going without other essentials to pay for medicines. Near-poor older beneficiaries with incomes $15–25K had 50% higher odds of CRN (vs >$50K), but beneficiaries with incomes <$15K, more likely to be eligible for the Part D Low-Income Subsidy, did not have significantly higher risk. Three indicators of worse health (general health status, functional limits, and count of conditions) were all independently associated with higher risk of CRN.
Conclusions
Changes in the risk profile for CRN since Part D reflect the effectiveness of targeted policies. The persistent prevalence of CRN and associated risks for sicker people in Medicare demonstrate the consequences of high cost-sharing for prescription fills.
Introduction
High out-of-pocket drug costs are a primary barrier to medication use.1,2 Longitudinal studies among older Americans have found that failure to adhere to medication regimens due to costs is associated with subsequent poorer health outcomes and increased use of acute services.3–5 Medicare enrollees are either over 65 years old or under 65 with long-term disabilities. Their large burden of chronic illness, substantial medication needs, and relatively modest financial resources make them particularly vulnerable to cost-related medication nonadherence.
The Centers for Medicare and Medicaid Services began tracking enrollees’ self-reports of cost-related nonadherence (CRN) through their principal annual survey, the Medicare Current Beneficiary Survey (MCBS), in 2004. Members of our study team led the development and testing of the questionnaire items used to measure CRN.6,7 Later, we used repeated annual CRN measurements to evaluate the impact of the implementation of the subsidized Medicare Part D drug benefit in 2006. The sudden availability of Part D coverage led to a 15% decrease in the rate of CRN among Medicare enrollees overall.8 We determined that sicker enrollees were slower to experience improvements in their ability to afford medications after Part D9 and experienced greater erosion of those improvements in later years.10,11
We have documented greater likelihood of CRN among enrollees who have depression12 or rheumatoid arthritis.13 Studies have used these survey data to examine CRN among enrollees who have glaucoma,14 diabetes,15 and cancer.16 Other investigators have demonstrated the potential for using year-to-year changes in CRN for individuals to evaluate Part D17 and applied factor analyses to characterize the underlying structure of CRN and its relationship to companion measures.18 In the MCBS, cost-related nonadherence encompasses the following behaviors: not filling prescriptions, delaying fills, and skipping or reducing doses due to costs. Related questions ask whether beneficiaries ever forgo other basic needs in order to pay for medications and about personal strategies used to reduce drug costs.
The landscape of Medicare prescription drugs has changed since our initial detailed descriptions of the CRN measures. The Part D program was launched and has matured. More than 7 in 10 beneficiaries currently have coverage through a Part D plan,19 while about 12% have no creditable drug coverage,19 down from estimates of about 25%20 prior to 2006. The “donut hole” coverage gap, a prominent and widely criticized original feature of Part D that led to reduced adherence among beneficiaries with chronic conditions,21,22 was slowly eliminated under a provision of the Affordable Care Act. Few Part D plans resemble the standard defined Part D benefit structure.19 Many have no deductible,23 and most use a copayment tier structure that strongly incentivizes beneficiaries toward inexpensive generic medications. However, for specialty drugs and biologics, including insulin, fast-rising prices and burdensome Part D cost-sharing requirements have gained increased attention from consumer advocates and policymakers.24–27 The Medicare Current Beneficiary Survey has also evolved during this period, adding more questions, improving measurement of beneficiary demographics, and enhancing data collection techniques.
With the utility of the CRN measure now clear and an evolved policy context, we have updated our previous national study of difficulties affording medication. This paper presents current data on the prevalence of and risk factors for CRN in Medicare, and compares risk factors in 2016 with those identified in 2004. In addition, we provide the first corresponding examination of key companion measures to CRN: spending less on other basic needs to afford medications and strategizing to reduce drug costs.
METHODS
Data source and population
The Medicare Current Beneficiary Survey (MCBS) by the US Centers for Medicare and Medicare Services samples beneficiaries from national Medicare enrollment files in rotating panels for up to 4 years. It combines data from thrice-annual, 1-hour, in-person interviews and administrative sources to provide comprehensive information on enrollee demographics, health status, health behaviors, and health care utilization. Between 2012 and 2015, MCBS overhauled its operations;28 recent improvements include finer geographic sampling units, more diverse Hispanic representation, more complete income information, enhanced computer support during interviews, audiorecorded audits, and additional quality controls during data processing. Data used in this paper are from the 2016 MCBS.
For our main analyses, we required that respondents have at least 1 response within the interview module that includes our key questions of interest and continuous 2016 enrollment so that these questions, which appeared in the Fall round, would typically refer to time spent as beneficiaries. We excluded individuals residing in long-term care facilities as they are not interviewed. Our sample (n=12,625) included those enrolled in both traditional Medicare and Medicare Advantage (private managed care plans). Secondary analyses of trends over time are based on MCBS years 2006 to 2015, excluding 2014, for which data were not released because of the MCBS operational transition.
Measures
Our measure of cost-related medication nonadherence (CRN) is a composite of 5 questions indicating that the respondent reported ever, in the previous 12 months: not filling a prescription or delaying a fill because it cost too much; or, skipping a dose or taking a smaller dose than prescribed to make a medicine last longer. To measure not filling due to costs, we included responses from both a direct question and a separate two-step question which first asks whether the respondent ever did not get a prescribed medicine for any reason and then asks why, showing a picklist that includes “cost” as a possible reason. A single question asking whether the respondent had ever, in the past 12 months, “spent less money on food, heat, or other basic needs to have money for medicine” suggests a high burden of drug costs leading to extreme compensatory behavior. The CRN composite and this “spent less” question have been extensively validated in both methodology- and policy-focused studies, by our team and others.5–18,29 Fielding errors resulting in incomplete data capture of CRN in 2004 and 2005 were corrected by 2006.8–11
Our primary measures also include strategies to reduce drug cost burden. Of 8 MCBS questions about how beneficiaries obtain medications, we selected three that unambiguously reflected beneficiaries’ efforts to reduce drug costs.18 These were self-reports of ever, in the past 12 months, (1) asking for generics instead of brand name drugs, (2) comparing drug prices or shopping around for the best price, and (3) talking with one’s doctor about stopping a medicine to save money or substituting a medicine with another that is less expensive. We created a composite indicating use of any of these three behaviors.
We used key covariate measures from prior research6,8–11,29 to describe the community-dwelling Medicare population and conduct updated tests of potential predictors of CRN and the companion measures. Age and sex derive from enrollment data. Income, educational attainment, race, ethnicity, general health status, chronic condition diagnoses, and functional limitations were self-reported. We created categories of drug coverage type (Table 1) by combining data from both survey and administrative sources in the MCBS.
Table 1 –
(a) Characteristics of community-dwelling Medicare beneficiaries in 2016, and (b) Overall prevalence of cost-related nonadherence and companion outcomes
| Table 1 (a) - Characteristics of community-dwelling Medicare beneficiaries in 2016 | ||||||
|---|---|---|---|---|---|---|
| Enrollees under 65 y | Enrollees 65 y and over | |||||
| Characteristic | N | Weighted % (95% CI) |
N | Weighted % (95% CI) |
||
| Age, y | ||||||
| ≤54 | 1491 | 44.6 | (41.8–47.3) | |||
| 55–64 | 664 | 55.4 | (52.7–58.2) | |||
| 65–74 | 3971 | 57.1 | (55.9–58.3) | |||
| 75–84 | 4244 | 30.8 | (29.8–31.8) | |||
| ≥85 | 2255 | 12.1 | (11.4–12.8) | |||
| Sex | ||||||
| Male | 1105 | 50.0 | (46.8–53.1) | 4585 | 44.7 | (43.5–45.9) |
| Female | 1050 | 50.0 | (46.9–53.2) | 5885 | 55.3 | (54.1–56.5) |
| Household income, $ | ||||||
| < $15K | 1191 | 45.9 | (43.3–48.5) | 1974 | 16.6 | (15.2–17.9) |
| $15k to $25k | 456 | 22.9 | (20.6–25.2) | 2002 | 17.4 | (16.4–18.3) |
| $25k to $50k | 287 | 16.8 | (14.3–19.3) | 2919 | 27.7 | (26.3–29.1) |
| > $50K | 221 | 14.4 | (12.2–16.5) | 3575 | 38.4 | (36.7–40.1) |
| Education | ||||||
| No high school diploma | 456 | 21.0 | (18.2–23.8) | 1981 | 16.4 | (15.0–17.8) |
| High school diploma | 840 | 35.0 | (32.3–37.8) | 2853 | 25.6 | (24.1–27.2) |
| Some college | 681 | 33.3 | (30.0–36.5) | 2892 | 28.6 | (27.2–30.1) |
| Bachelors and above | 164 | 10.1 | (8.1–12.2) | 2702 | 28.9 | (26.9–31.0) |
| Race | ||||||
| White | 1470 | 70.2 | (66.4–74.1) | 8797 | 82.7 | (80.5–84.8) |
| African American | 448 | 18.1 | (14.2–22.0) | 880 | 8.9 | (7.2–10.6) |
| All Other | 192 | 9.1 | (7.3–10.9) | 631 | 6.9 | (5.7–8.1) |
| Hispanic ethnicity | ||||||
| Not Hispanic | 1894 | 87.8 | (84.9–90.7) | 9457 | 91.5 | (89.6–93.4) |
| Hispanic | 247 | 11.6 | (8.7–14.6) | 961 | 8.0 | (6.1–10.0) |
| General health status | ||||||
| Excellent, very good, or good | 1007 | 42.8 | (39.9–45.8) | 8503 | 82.0 | (80.9–83.1) |
| Fair or poor | 1135 | 56.5 | (53.5–59.5) | 1919 | 17.6 | (16.4–18.7) |
| No. of limitations in ADLs(1) | ||||||
| Zero | 1143 | 47.3 | (44.3–50.3) | 7306 | 73.9 | (72.6–75.2) |
| 1 to 2 | 576 | 29.5 | (26.7–32.3) | 2117 | 17.9 | (17.0–18.8) |
| 3 to 6 | 436 | 23.2 | (20.9–25.4) | 1046 | 8.2 | (7.5–8.9) |
| No. of chronic conditions(2) | ||||||
| Zero or 1 | 574 | 19.0 | (17.0–21.0) | 2467 | 27.1 | (25.9–28.4) |
| 2 to 3 | 878 | 40.1 | (37.1–43.1) | 4899 | 46.2 | (45.0–47.3) |
| 4 to 10 | 703 | 40.9 | (37.9–43.9) | 3103 | 26.7 | (25.5–27.8) |
| Drug Coverage(3) | ||||||
| Part D with Low Income Subsidy | 1475 | 58.0 | (54.8–61.1) | 1634 | 14.5 | (12.8–16.3) |
| Medicare Advantage with Part D | 191 | 12.5 | (10.1–14.9) | 2909 | 29.0 | (27.0–31.0) |
| Traditional Medicare with Part D | 167 | 10.0 | (8.2–11.7) | 3427 | 31.6 | (29.8–33.3) |
| Other drug supplement plan | 193 | 12.8 | (10.8–14.8) | 1783 | 18.0 | (16.4–19.6) |
| No drug coverage | 129 | 6.8 | (5.3–8.3) | 717 | 6.8 | (6.0–7.7) |
| Table 1 (b) - Prevalence of cost-related nonadherence and companion outcomes(13.4–15.3) | ||||||
| Any cost-related nonadherence (CRN composite) | 2150 | 34.5 | (31.0–37.0) | 10457 | 14.4 | (13.4–15.3) |
| “Skipped doses to make the medicine last longer” | 2141 | 15.2 | (13.3–17.1) | 10438 | 4.3 | (3.8–4.7) |
| “Took smaller doses than prescribed to make the medicine last longer” | 2140 | 16.2 | (14.1–18.4) | 10438 | 5.1 | (4.5–5.7) |
| “Decided not to fill a prescription because it cost too much” | 2139 | 22.0 | (19.6–24.4) | 10436 | 8.7 | (8.0–9.5) |
| “Delayed getting a prescription filled because it cost too much” | 2140 | 20.6 | (18.4–22.8) | 10439 | 6.5 | (5.9–7.1) |
| “Did not get a prescribed medicine”, and “reason” was “cost” | 2135 | 8.0 | (6.3–9.7) | 10423 | 2.9 | (2.4–3.3) |
| “Spent less money on food, heat, or other basic needs to have money for medicine” | 2141 | 19.4 | (17.0–21.7) | 10438 | 4.7 | (4.1–5.2) |
| Any drug cost reduction strategy (composite)(4) | 2144 | 47.6 | (44.4–50.9) | 10443 | 44.0 | (42.2–45.8) |
| “Asked for generics instead of brand name drugs” | 2127 | 36.8 | (33.4–40.1) | 10389 | 36.9 | (35.0–38.6) |
| “Compared prices or shopped around for the best price” | 2137 | 21.4 | (19.1–23.6) | 10434 | 14.3 | (13.3–15.3) |
| “Talked with doctor about stopping a medicine to save money or substituting a medicine with one that is less expensive” | 2132 | 19.8 | (17.5–22.0) | 10430 | 13.9 | (13.0–14.9) |
Notes:
Limitations in ADL (activities of daily living) is a measure of functioning.32
Count of self-reported chronic conditions included diagnoses of cardiac disease, hypertension, diabetes, cancer, stroke, arthritis, dementia, psychiatric disorder (including depression), neurological disorder (excluding stroke), and pulmonary illness (including asthma and chronic obstructive pulmonary disease).
Drug coverage types are mutually exclusive and were defined and assigned hierarchically as follows: any enrollment in Part D with Low-Income Subsidy (LIS) during 2016 (either with traditional Medicare coverage or with a Medicare Advantage plan); any Medicare Advantage with Part D but no LIS; any traditional Medicare coverage with Part D but no LIS; any other non-Part D drug coverage including employer-sponsored and US Veterans Affairs; no drug coverage.
Additional MCBS questions about use of mail order, internet, free samples, credit cards, or retailer discounts were not included because, given the question wording and/or common current practices, positive responses may or may not reflect beneficiaries’ own efforts to reduce costs.18
Analyses
We conducted separate analyses for the population aged under 65 years, who qualify for Medicare based on long-term disability, and those 65 years and above, who qualify based on age. We used MCBS survey weights to create estimates for the national population of approximately 56 million community-dwelling beneficiaries.28,30
We estimated the proportions of the 2 study groups falling in each covariate stratum in 2016 with 95% confidence intervals. Next, we calculated positive response rates for all item-specific and composite measures of interest to estimate the prevalence of CRN, spending less on other needs to pay for medicines, and use of cost reduction strategies, overall and within covariate strata. Multivariate logistic regression models determined whether the covariate measures independently predicted each primary outcome. We contrasted these model results with sensitivity analyses that omitted the drug coverage variable because it is endogenous. Additional sensitivity analyses explored potential differences by US region and included chronic conditions individually instead of as a count. Finally, we estimated the overall annual prevalence of our primary study outcomes from 2006 to 2016, exclusive of 2014.
Analyses were conducted using the statistical software SAS 9.3 (SAS Institute, Cary NC). This study was approved by the Harvard Pilgrim Health Care Institutional Review Board.
RESULTS
Characteristics of community-dwelling enrollees in 2016 are shown in Table 1a. Enrollees under age 65, who have long-term disability, represent 16.1% of community-dwelling enrollees and are more likely than those age 65 years and over to have indicators of social or clinical vulnerability. For example, 45.9% of enrollees under age 65 and 17.4% of enrollees age 65 or older were in our lowest income category (<$15K per year). The under-65 population also had lower educational attainment and higher counts of functional limitations and chronic conditions. Multimorbidity was common in both groups: 81.0% of enrollees under 65 and 72.9% of those 65 and older had at least two chronic conditions.
Unadjusted prevalence results
The prevalence of cost-related nonadherence is presented in Table 1b with the companion outcomes. Among older enrollees, 14.4% experienced CRN. CRN was more than twice as prevalent among those under age 65, 34.5%. Item-specific rates indicated that not filling a prescription due to high cost was the most frequent CRN behavior in both groups. (Direct questioning was more likely to ascertain this information than a two-step approach.)
About 1 in 5 of those under age 65 (19.4%) and 4.7% of older beneficiaries experienced the more severe outcome, spending less on other basic needs to have money for medicines. Strategizing to reduce drug costs was common in both groups; we estimated that 47.6% of the younger enrollees and 44.0% of older enrollees used at least one of the three cost-reduction strategies. Nearly identical proportions in both groups (36.8% and 36.9%, respectively) had asked for generics over brands, while shopping around for the best price and talking to one’s doctor about stopping or substituting medications were more common among those under age 65 (19.8%, vs 13.9%).
Detailed prevalence results by population strata are presented in Table 2, with highlights in Figure 1. Differences by income were relatively modest. For CRN among those under 65, point estimates across the 4 income strata ranged from 30.6 to 38.6; overlapping confidence intervals indicated no statistically significant differences. Among those 65 and older, all 4 point estimates were between 11.6% and 17.7%, with several confidence intervals overlapping. Examining results for 5 drug coverage types, we observed in both groups that the highest point estimates were for enrollees in traditional fee-for-service Medicare with a stand-alone Part D plan, and the lowest was for those with other, non-Part D drug coverage including employer-sponsored coverage. Again, confidence intervals were overlapping with few significant differences.
Table 2 –
Prevalence of CRN, spending less on other basic needs to afford medicine, and cost reduction strategies, by demographic and health characteristics, 2016
| Any cost-related nonadherence | Spent less on other basic needs | Any cost reduction strategy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 65 y | 65 y and over | Under 65 y | 65 y and over | Under 65 y | 65 y and over | |||||||
| Characteristic | Weighted % (95% CI) |
Weighted % (95% CI) |
Weighted % (95% CI) |
Weighted % (95% CI) |
Weighted % (95% CI) |
Weighted % (95% CI) |
||||||
| Age, y | ||||||||||||
| ≤54 | 35.0 | (31.5–38.5) | 18.8 | (15.5–22.1) | 42.7 | (39.0–46.3) | ||||||
| 55–64 | 34.1 | (30.4–37.8) | 19.8 | (16.8–22.8) | 51.7 | (47.0–56.4) | ||||||
| 65–74 | 17.0 | (15.5–18.4) | 5.4 | (4.5–6.3) | 46.8 | (44.5–49.2) | ||||||
| 75–84 | 12.0 | (10.8–13.1) | 4.3 | (3.8–4.8) | 42.8 | (40.7–44.9) | ||||||
| ≥85 | 8.5 | (7.1–9.9) | 2.2 | (1.6–2.8) | 33.9 | (31.6–36.2) | ||||||
| Sex | ||||||||||||
| Male | 28.5 | (25.2–31.9) | 12.8 | (11.4–14.1) | 15.3 | (12.2–18.4) | 3.5 | (2.8–4.1) | 43.0 | (39.2–46.9) | 43.7 | (41.5–45.8) |
| Female | 40.5 | (36.7–44.3) | 15.7 | (14.6–16.8) | 23.4 | (19.6–27.2) | 5.6 | (4.9–6.4) | 52.3 | (47.4–57.1) | 44.3 | (42.2–46.3) |
| Household income, $ | ||||||||||||
| < $15K | 30.6 | (27.2–33.9) | 14.3 | (12.3–16.3) | 17.7 | (14.3–21.1) | 7.8 | (6.2–9.4) | 39.8 | (35.5–44.1) | 35.2 | (31.6–38.7) |
| $15k to $25k | 38.5 | (33.2–43.8) | 17.7 | (15.5–19.8) | 22.4 | (17.1–27.7) | 7.9 | (6.5–9.2) | 53.4 | (47.3–59.6) | 42.8 | (40.1–45.4) |
| $25k to $50k | 36.3 | (29.6–43.0) | 16.3 | (14.7–17.8) | 21.4 | (15.8–26.9) | 4.7 | (3.7–5.7) | 51.1 | (43.7–58.5) | 46.8 | (44.3–49.4) |
| > $50K | 38.5 | (30.3–46.8) | 11.6 | (10.5–12.7) | 17.5 | (11.4–23.5) | 1.9 | (1.3–2.4) | 59.5 | (51.3–67.8) | 46.4 | (44.1–48.6) |
| Education | ||||||||||||
| No high school diploma | 35.8 | (29.5–42.1) | 16.3 | (14.4–18.3) | 17.4 | (13.2–21.6) | 7.7 | (6.2–9.3) | 39.0 | (31.5–46.6) | 36.0 | (33.0–39.0) |
| High school diploma | 29.6 | (26.0–33.2) | 13.8 | (11.8–15.7) | 17.4 | (14.0–20.7) | 5.6 | (4.4–6.9) | 44.9 | (40.1–49.8) | 43.5 | (40.8–46.3) |
| Some college | 38.0 | (33.7–42.3) | 15.5 | (13.6–17.4) | 21.5 | (17.1–26.0) | 4.5 | (3.5–5.4) | 52.8 | (48.1–57.5) | 46.2 | (43.3–49.2) |
| Bachelors and above | 36.4 | (26.5–46.2) | 12.7 | (11.2–14.2) | 22.1 | (13.4–30.7) | 2.2 | (1.7–2.8) | 59.6 | (50.5–68.6) | 46.9 | (44.4–49.4) |
| Race | ||||||||||||
| White | 33.6 | (30.7–36.5) | 13.9 | (12.9–15.0) | 16.9 | (14.5–19.3) | 3.8 | (3.4–4.3) | 50.5 | (46.5–54.5) | 45.9 | (44.1–47.8) |
| African American | 36.1 | (28.9–43.2) | 18.9 | (15.4–22.5) | 24.3 | (18.2–30.5) | 9.9 | (7.5–12.2) | 38.9 | (31.8–46.0) | 34.4 | (30.0–38.8) |
| All Other | 38.5 | (28.7–48.3) | 14.1 | (10.7–17.6) | 25.0 | (16.0–34.0) | 7.6 | (5.2–10.1) | 45.2 | (36.7–53.7) | 35.1 | (29.7–40.5) |
| Hispanic ethnicity | ||||||||||||
| Not Hispanic | 35.7 | (33.1–38.2) | 14.4 | (13.4–15.5) | 19.5 | (17.0–22.0) | 4.6 | (4.0–5.1) | 49.5 | (46.4–52.6) | 45.1 | (43.3–46.8) |
| Hispanic | 26.2 | (19.6–32.8) | 13.6 | (10.9–16.2) | 18.4 | (12.4–24.3) | 6.1 | (4.1–8.1) | 34.5 | (25.7–43.3) | 32.2 | (27.7–36.7) |
| General health status | ||||||||||||
| Excellent, very good, or good | 26.8 | (23.2–30.4) | 12.3 | (11.4–13.2) | 12.4 | (9.4–15.4) | 3.2 | (2.7–3.6) | 43.4 | (39.6–47.2) | 43.5 | (41.5–45.4) |
| Fair or poor | 40.3 | (36.9–43.8) | 24.2 | (21.8–26.7) | 24.6 | (21.3–27.9) | 11.5 | (9.6–13.5) | 50.6 | (46.0–55.2) | 46.9 | (44.0–49.9) |
| No. of limitations in ADLs | ||||||||||||
| Zero | 28.8 | (25.2–32.5) | 11.8 | (10.8–12.8) | 13.5 | (11.2–15.8) | 2.8 | (2.3–3.3) | 43.9 | (40.2–47.6) | 42.6 | (40.6–44.7) |
| 1 to 2 | 37.0 | (31.8–42.2) | 20.1 | (18.2–22.0) | 19.8 | (15.7–23.9) | 8.9 | (7.3–10.4) | 48.7 | (43.0–54.4) | 47.3 | (45.0–49.6) |
| 3 to 6 | 43.1 | (37.3–48.9) | 25.3 | (21.7–28.9) | 30.8 | (24.9–36.7) | 12.5 | (9.7–15.4) | 54.0 | (47.5–60.5) | 49.4 | (45.3–53.6) |
| No. of chronic conditions | ||||||||||||
| Zero or 1 | 21.7 | (17.7–25.7) | 8.6 | (7.3–9.9) | 11.8 | (7.7–16.0) | 1.8 | (1.1–2.5) | 35.3 | (29.8–40.8) | 34.8 | (32.4–37.2) |
| 2 to 3 | 35.5 | (31.3–39.7) | 14.3 | (13.0–15.6) | 18.2 | (14.8–21.5) | 4.1 | (3.5–4.8) | 45.6 | (40.4–50.8) | 45.3 | (43.0–47.7) |
| 4 to 10 | 39.4 | (35.7–43.1) | 20.5 | (18.6–22.3) | 24.0 | (20.1–27.9) | 8.5 | (7.2–9.9) | 55.4 | (50.4–60.5) | 51.1 | (48.7–53.5) |
| Drug Coverage | ||||||||||||
| Part D with Low Income Subsidy | 30.6 | (27.4–33.9) | 16.4 | (13.8–19.1) | 16.8 | (13.7–19.9) | 10.8 | (8.8–12.9) | 39.9 | (35.8–44.0) | 40.9 | (37.8–44.1) |
| Medicare Advantage with Part D | 45.8 | (38.2–53.5) | 13.8 | (12.2–15.5) | 24.8 | (17.9–31.7) | 4.4 | (3.5–5.2) | 68.4 | (61.2–75.7) | 52.7 | (50.8–54.6) |
| Traditional Medicare with Part D | 52.0 | (42.2–61.8) | 17.2 | (15.4–18.9) | 29.3 | (19.9–38.7) | 3.8 | (2.9–4.6) | 72.3 | (64.0–80.7) | 37.1 | (32.4–41.7) |
| Other drug supplement plan | 24.8 | (18.1–31.6) | 9.3 | (7.5–11.1) | 14.2 | (8.6–19.7) | 2.3 | (1.4–3.1) | 43.8 | (34.3–53.3) | 44.0 | (40.7–47.2) |
| No drug coverage | 38.9 | (28.4–49.4) | 13.2 | (10.1–16.3) | 26.4 | (16.4–36.4) | 3.3 | (1.8–4.8) | 46.7 | (34.6–58.9) | 32.4 | (28.9–35.9) |
Figure 1 –
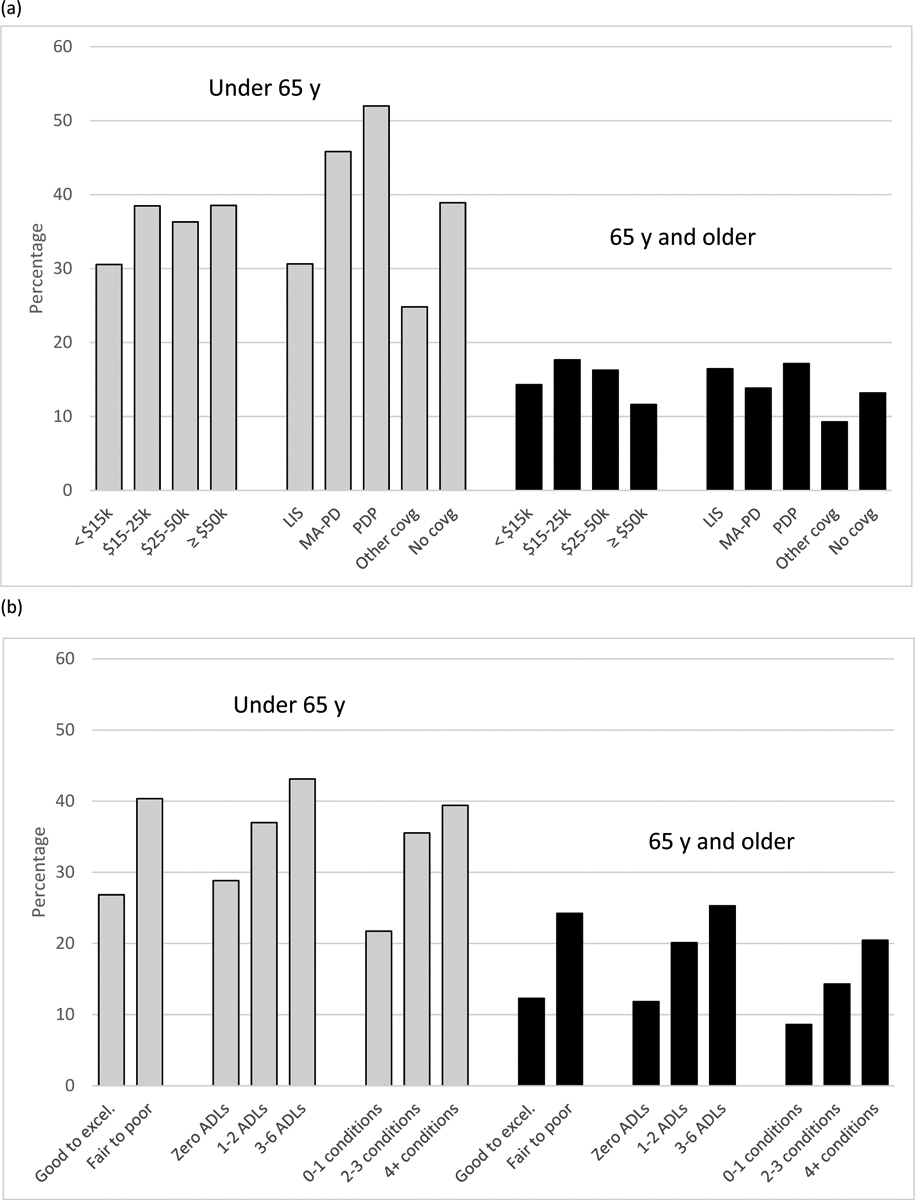
Unadjusted prevalence of cost-related nonadherence in selected population strata: (a) by household income and drug coverage type, and (b) by general health status and number of chronic conditions
By contrast, we observed stronger associations of CRN with health status. For example, CRN was about 50% higher, relatively, among those under 65 in fair-to-poor general health, versus their healthier peers (40.3% vs 26.8%). Among those 65 and over, sicker beneficiaries had nearly twice the level of CRN as healthier peers (24.2% vs. 12.3%). We observed similar strong associations of CRN with level of functional impairment and number of chronic conditions (Figure 1). Sicker people aged 65 years and older were also more likely to experience “spending less on other basic needs to afford medications,” based on any of our health measures (general health status, functional impairments, and number of chronic conditions).
In the smaller under-65 group, the relationships between both CRN and “spending less” and poorer health were similar. However, differences between health strata were not always statistically significant.
Adjusted odds ratios
In multivariate analyses of the population over age 65, the adjusted odds of any CRN were 50% higher for enrollees in fair-to-poor general health vs healthier peers, and about twice as high for beneficiaries with the most functional limitations (OR=2.0) or chronic conditions (OR=2.1), versus the fewest (Table 3). The second-to-lowest income group had odds of CRN 1.5 times higher than the wealthiest group; however, the lowest income group did not have significantly higher odds.
Table 3 –
Adjusted odds ratio estimates of CRN, spending less on other basic needs to afford medicine, and cost reduction strategies
| Any cost-related nonadherence | Spent less on other basic needs | Any cost reduction strategy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 65 y | 65 y and over | Under 65 y | 65 y and over | Under 65 y | 65 y and over | |||||||
| Characteristic | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||||||
| Age, y | ||||||||||||
| ≤54 | 1.00 | 1.00 | 1.00 | |||||||||
| 55–64 | 0.73 | (0.57–0.93) | 0.91 | (0.67–1.24) | 1.07 | (0.83–1.38) | ||||||
| 65–74 | 1.00 | 1.00 | 1.00 | |||||||||
| 75–84 | 0.57 | (0.49–0.67) | 0.60 | (0.48–0.76) | 0.76 | (0.68–0.84) | ||||||
| ≥85 | 0.33 | (0.26–0.41) | 0.24 | (0.17–0.34) | 0.49 | (0.43–0.56) | ||||||
| Sex | ||||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Female | 1.66 | (1.31–2.10) | 1.21 | (1.04–1.41) | 1.56 | (1.10–2.23) | 1.30 | (1.02–1.64) | 1.42 | (1.12–1.79) | 1.04 | (0.94–1.14) |
| Household income, $ | ||||||||||||
| < $15K | 0.76 | (0.43–1.34) | 1.08 | (0.83–1.39) | 1.37 | (0.73–2.56) | 1.82 | (1.12–2.98) | 0.71 | (0.43–1.17) | 0.94 | (0.79–1.13) |
| $15k to $25k | 0.94 | (0.56–1.60) | 1.47 | (1.23–1.77) | 1.52 | (0.79–2.92) | 2.73 | (1.87–3.97) | 0.99 | (0.60–1.65) | 1.03 | (0.89–1.18) |
| $25k to $50k | 0.85 | (0.47–1.54) | 1.40 | (1.21–1.63) | 1.29 | (0.72–2.31) | 1.87 | (1.24–2.82) | 0.70 | (0.41–1.19) | 1.08 | (0.95–1.23) |
| > $50K | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Education | ||||||||||||
| No high school diploma | 1.40 | (0.73–2.68) | 1.03 | (0.84–1.26) | 0.81 | (0.42–1.54) | 1.51 | (0.96–2.39) | 0.73 | (0.44–1.22) | 0.83 | (0.70–0.98) |
| High school diploma | 0.98 | (0.60–1.62) | 0.88 | (0.72–1.07) | 0.88 | (0.50–1.57) | 1.50 | (0.99–2.28) | 0.78 | (0.49–1.24) | 0.91 | (0.78–1.06) |
| Some college | 1.14 | (0.66–1.98) | 1.05 | (0.87–1.27) | 0.91 | (0.48–1.70) | 1.27 | (0.86–1.87) | 0.88 | (0.57–1.38) | 0.96 | (0.82–1.12) |
| Bachelors and above | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Race | ||||||||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| African American | 1.19 | (0.81–1.74) | 1.28 | (0.98–1.68) | 1.69 | (1.11–2.59) | 1.72 | (1.26–2.35) | 0.66 | (0.46–0.93) | 0.67 | (0.54–0.83) |
| All Other | 1.30 | (0.83–2.03) | 0.96 | (0.71–1.31) | 1.70 | (1.02–2.83) | 1.62 | (1.09–2.43) | 0.90 | (0.58–1.39) | 0.74 | (0.58–0.95) |
| Hispanic ethnicity | ||||||||||||
| Not Hispanic | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Hispanic | 0.45 | (0.31–0.66) | 0.86 | (0.66–1.12) | 0.65 | (0.39–1.10) | 0.76 | (0.47–1.24) | 0.43 | (0.29–0.63) | 0.65 | (0.51–0.82) |
| General health status | ||||||||||||
| Excellent, very good, or good | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Fair or poor | 1.38 | (1.04–1.84) | 1.49 | (1.25–1.78) | 1.61 | (1.13–2.31) | 1.70 | (1.27–2.27) | 1.04 | (0.83–1.30) | 1.02 | (0.90–1.16) |
| No. of limitations in ADLs | ||||||||||||
| Zero | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 1 to 2 | 1.20 | (0.87–1.67) | 1.58 | (1.33–1.88) | 1.29 | (0.93–1.79) | 2.27 | (1.63–3.17) | 1.08 | (0.84–1.39) | 1.20 | (1.05–1.38) |
| 3 to 6 | 1.45 | (1.02–2.05) | 1.99 | (1.62–2.45) | 2.20 | (1.49–3.23) | 2.79 | (1.82–4.26) | 1.31 | (0.94–1.82) | 1.49 | (1.25–1.76) |
| No. of chronic conditions | ||||||||||||
| Zero or 1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 2 to 3 | 1.65 | (1.21–2.26) | 1.67 | (1.38–2.03) | 1.27 | (0.80–2.01) | 1.85 | (1.20–2.85) | 1.19 | (0.85–1.68) | 1.63 | (1.44–1.84) |
| 4 to 10 | 1.94 | (1.44–2.59) | 2.12 | (1.68–2.68) | 1.71 | (1.08–2.71) | 2.41 | (1.50–3.90) | 1.79 | (1.29–2.47) | 2.14 | (1.89–2.42) |
| Drug Coverage | ||||||||||||
| Part D with Low Income Subsidy | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Medicare Advantage with Part D | 2.01 | (1.34–3.02) | 1.13 | (0.86–1.49) | 1.78 | (1.09–2.90) | 0.86 | (0.59–1.25) | 2.84 | (1.83–4.39) | 1.55 | (1.26–1.90) |
| Traditional Medicare with Part D | 2.49 | (1.51–4.09) | 1.50 | (1.14–1.97) | 2.48 | (1.39–4.43) | 0.77 | (0.50–1.17) | 3.39 | (1.89–6.08) | 2.09 | (1.73–2.52) |
| Other drug supplement plan | 0.69 | (0.40–1.20) | 0.75 | (0.53–1.06) | 0.92 | (0.49–1.73) | 0.53 | (0.31–0.92) | 0.93 | (0.53–1.64) | 1.34 | (1.07–1.66) |
| No drug coverage | 1.71 | (1.01–2.87) | 1.09 | (0.74–1.62) | 2.10 | (1.06–4.13) | 0.60 | (0.33–1.08) | 1.19 | (0.66–2.14) | 1.22 | (0.94–1.59) |
Notes:
Bolded text indicates odds ratio estimates were statistically significant at P<0.05.
We observed that the odds of forgoing basic needs were consistently higher for sicker enrollees, regardless of which of the three health measures was used, even when controlling for the other 2 measures. However, when assessing income effects, we observed that it was again the second-to-lowest income group that was at highest risk compared to the wealthiest (OR 2.7, CI 1.9–4.0).
Among older beneficiaries, comparing the odds for different drug coverage types versus Part D coverage with Low-Income Subsidy, we found that having traditional Medicare with a stand-alone Part D plan was associated with elevated odds of CRN (OR 1.5, CI 1.1–2.0), and non-Part D coverage was associated with lower odds of spending less on other basic needs (OR 0.5, CI 0.3–0.9). Alternative versions of our main models without the endogenous drug coverage variables gave very similar results for health status and income (see Supplemental Digital Content 1). Additional sensitivity models (see Supplemental Digital Content 2) showed that arthritis, psychiatric diagnoses, and pulmonary illnesses, specifically, were associated with drug unaffordability in both age groups, as were diabetes and hypertension in the older group. These models also suggested elevated risk in the South and Midwest regions, though not in the West, as compared to the Northeast.
Use of any of 3 cost reduction strategies was associated with higher counts of chronic conditions among older beneficiaries, but was not independently associated with general health or income status (Table 3). Using strategies to reduce drug costs was higher among women, who were at consistently higher risk for hardship (i.e., both CRN and “spending less”). The 65–74 years age group was similar in this regard, compared to all beneficiaries age 75 years and older. On the other hand, non-white beneficiaries (both over and under 65 years, vs whites) were at higher risk of spending less on essentials to pay for medicines, yet were less likely to use cost reduction strategies (Table 3).
Annual trends
Figure 2 shows annual rates of any CRN and spending less on other basic needs to afford medicines from 2006 to 2016. The highest point estimate for CRN prevalence among older beneficiaries was in the most recent year, 2016 (14.4%). The “spent less” measure has been relatively stable over time. Use of cost-reduction strategies declined from 61.9% in 2011 to 47.6% in 2016 among older beneficiaries, and from 55.5% to 44.0% among those under age 65; these decreases appear to be primarily driven by reductions in asking for generics. Full longitudinal results are available in Supplemental Digital Content 3.
Figure 2 – Annual prevalence of cost-related nonadherence and spending less on other basic needs to pay for medicines, 2006 to 2016.
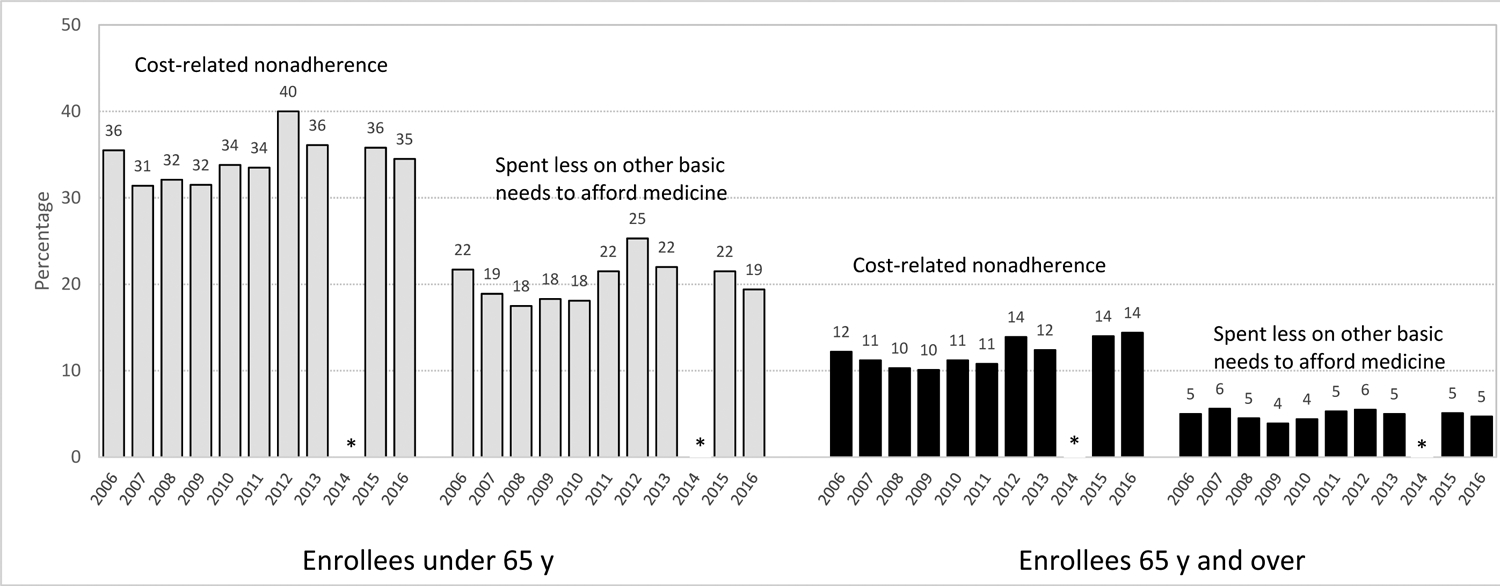
Notes:
* Survey year 2014 was not released by MCBS due to a comprehensive overhaul of operations.
Survey years 2004 and 2005 were omitted because of MCBS fielding errors leading to incomplete measurement of CRN. Previous longitudinal studies adjusting for changes in measurement between 2005 and 2006 are available.8–11 Higher estimates in 2012 may be due to initiation of audiorecorded auditing that year.
DISCUSSION
Our results demonstrate that cost-related nonadherence (CRN) is a persistent problem hindering the ability of many Medicare beneficiaries to access pharmacologic treatments. In 2016, about 1 in 7 enrollees age 65 years and older experienced CRN within the previous year. The rate of CRN was much higher, more than 1 in 3, among enrollees under age 65 with long-term disability. We found that worse health was consistently associated with CRN in both groups. In fact, the three measures of worse health that we included in our statistical models -- general health status, lower functioning, and a count of chronic conditions – independently predicted CRN.
This updated exploration of the prevalence and predictors of CRN in Medicare is needed because of changes in both policy and measurement since our earlier studies.6 In the intervening years, Medicare Part D became available as a voluntary, subsidized prescription drug benefit and is now a well-established program. Using similar models, our results are generally similar to earlier reports, with notable exceptions. In the 2004 MCBS, seniors in the lowest stratum of income had adjusted odds of CRN 50% higher than seniors in the highest income stratum. In 2016, by contrast, those in the lowest stratum, who correspond roughly to people at or below the federal poverty level,31 were no longer at significantly higher risk; however, seniors with incomes roughly 2–3 times the poverty level bore elevated risk. (Among beneficiaries under 65, a smaller and broadly disadvantaged group, we detected no significant differences in CRN risk among income strata.)
This evolution in the income-associated risk of CRN is consistent with the design of the Medicare Part D benefit. Individuals near the poverty level and below were targeted for generous additional financial assistance under Part D’s Low-Income Subsidy program (LIS). Individuals just above this stratum, but not financially well-off, are not eligible for LIS, so would be expected to remain at continued risk, as we observed. Part D plans feature substantial patient cost-sharing (e.g., deductibles, tiered copayments, and co-insurance) when prescriptions are filled. Total cost-sharing is higher for people with multiple illnesses who require multiple drug treatments. We were therefore not surprised to see more affordability problems among sicker enrollees. Following Part D, drug coverage has been more universal and more consistent in its generosity, such that drug coverage type is no longer a strong predictor of CRN among older Medicare beneficiaries.
A 2019 report32 using the 2015 MCBS also addressed risk factors for CRN and reached a different conclusion: that drug coverage was “the most influential factor in explaining CRN”. In contrast to their approach, our study included more types of beneficiaries and variable definitions more likely to tease out the effects of income and Part D subsidies. Like Gu et al.,32 we observed associations between drug coverage type and CRN. However, these associations are difficult to interpret because of the inherent self-selection in drug coverage type, based on factors such as past employment, socioeconomic status, and health status. Simultaneity is also a potential concern when out-of-pocket drug costs and drug utilization are included in models with drug coverage. We sought to minimize bias by emphasizing a limited number of variables less subject to self-selection.
In this report, we explored for the first time the predictors of spending less on other basic needs to pay for medicines, which is a less frequent and more extreme measure of hardship around drug costs. This outcome was associated not only with worse health among older beneficiaries but also multiple indicators of socioeconomic vulnerability, including all 3 lower income strata, lower educational attainment (borderline significance), and non-white race.
We present data on general trends in these two outcomes since Part D implementation. Apparent increases in CRN in the past decade require an important caveat that improvements were also made to the survey in this period. Given recent reports of very high prices for insulin and specialty drugs,24–27 more focused research on patient cost burden and affordability are merited, including studies of specific conditions and their treatment costs. In 2019, the Part D “donut hole” was entirely eliminated, but in 2020 the Part D threshold for catastrophic coverage increased substantially;33 both policy changes have potential to affect drug affordability among the sickest beneficiaries and multiple proposals for further adjustments to Part D are in discussion annually.
A more than 10 percentage-point reduction in the use of cost-reduction strategies (2011–2016) appears attributable to less frequent requesting of generics. It may be that more routine use of generics, when a generic version is available, has made the strategy of requesting them less common.34 Controlling for other factors, and despite signs of greater hardship, certain disadvantaged groups (especially, non-white beneficiaries and older people without a high school diploma) were less likely to use drug cost reduction strategies, pointing to opportunities within health systems to screen for drug affordability problems and offer more explicit guidance to high-risk patients.25
Our study has several limitations. We opted for parsimonious models and it is possible that omitted factors could further explain variation in these outcomes. Also, CRN and the companion measures rely on respondents’ self-reports. As such, they are subject to recall biases, especially given the lengthy 12-month reference period, and possible stigma and social desirability bias around having insufficient financial resources for medication or not adhering to physician-recommended treatment. Nevertheless, CRN has been shown repeatedly to be sensitive and capable of detecting small differences. Its construct validity is well documented. More than a decade of research on CRN in Medicare supports the utility of this composite measure for evaluating policy changes and understanding disparities among key segments of the enrollee population. The CRN composite provides a foundation for research on Medicare drug affordability. Following the recent enhancements to the MCBS, longitudinal analyses will be useful for assessing future changes in the Medicare program or the well-being of its population.
Cost-related nonadherence persists as a behavior threatening treatment effectiveness and better health outcomes for Medicare beneficiaries, especially sicker individuals and people under age 65 years with disability. Clinicians must be alert to barriers that patients may face when filling their prescriptions and work with patients to identify affordable regimens. Policymakers should consider more nuanced drug benefit designs that ensure the affordability of essential treatments and other ways to relieve high drug cost burden among vulnerable beneficiaries.
Supplementary Material
Supplemental Digital Content 1 – Sensitivity analysis showing adjusted odds ratio estimates of CRN, spending less on other basic needs to afford medicine, and cost reduction strategies with drug coverage variables omitted
Supplemental Digital Content 2 – Sensitivity analyses examining US region and specific chronic conditions as potential risk factors
Supplemental Digital Content 3 – Longitudinal analyses, 2006–2016
Acknowledgements
We are grateful for supportive data analyses by Prathwish Shetty, MSc (Northeastern University), and Xin Xu, MS (HPHC/HMS). We also thank CMS staff, in particular MCBS Director Debra Reed-Gillette, MS, for insights into MCBS data and operations. This study was supported by the National Institute on Aging (grant nos. R01AG028745 and R01AG022362, PI Soumerai, and R21AG060401, PI Madden) and Northeastern University.
Disclosure: Funding from the National Institutes of Health (NIH)
Footnotes
The authors have no potential conflicts of interest to disclose.
REFERENCES
- 1.Kennedy J, Tuleu I, Mackay K. Unfilled prescriptions of medicare beneficiaries: prevalence, reasons, and types of medicines prescribed. J Manag Care Pharm 2008;14:553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gellad WF, Grenard J, McGlynn EA. A Review of Barriers to Medication Adherence: A Framework for Driving Policy Options: The RAND Corporation; 2009. [Google Scholar]
- 3.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care 2004;42:626–34. [DOI] [PubMed] [Google Scholar]
- 4.Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care 2010;48:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanchard J, Madden JM, Ross-Degnan D, Gresenz CR, Soumerai SB. The relationship between emergency department use and cost-related medication nonadherence among Medicare beneficiaries. Ann Emerg Med 2013;62:475–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med 2006;166:1829–35. [DOI] [PubMed] [Google Scholar]
- 7.Pierre-Jacques M, Safran DG, Zhang F, et al. Reliability of new measures of cost-related medication nonadherence. Med Care 2008;46:444–8. [DOI] [PubMed] [Google Scholar]
- 8.Madden JM, Graves AJ, Zhang F, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA 2008;299:1922–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madden JM, Graves AJ, Ross-Degnan D, Briesacher BA, Soumerai SB. Cost-related medication nonadherence after implementation of Medicare Part D, 2006–2007. JAMA 2009;302:1755–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naci H, Soumerai SB, Ross-Degnan D, et al. Medication affordability gains following Medicare Part D are eroding among elderly with multiple chronic conditions. Health Aff (Millwood) 2014;33:1435–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naci H, Soumerai SB, Ross-Degnan D, et al. Persistent medication affordability problems among disabled Medicare beneficiaries after Part D, 2006–2011. Med Care 2014;52:951–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bambauer KZ, Safran DG, Ross-Degnan D, et al. Depression and cost-related medication nonadherence in Medicare beneficiaries. Arch Gen Psychiatry 2007;64:602–8. [DOI] [PubMed] [Google Scholar]
- 13.Harrold LR, Briesacher BA, Peterson D, et al. Cost-related medication nonadherence in older patients with rheumatoid arthritis. J Rheumatol 2013;40:137–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blumberg DM, Prager AJ, Liebmann JM, Cioffi GA, De Moraes CG. Cost-Related Medication Nonadherence and Cost-Saving Behaviors Among Patients With Glaucoma Before and After the Implementation of Medicare Part D. JAMA Ophthalmol 2015;133:985–96. [DOI] [PubMed] [Google Scholar]
- 15.Zhang JX, Meltzer DO. The High Cost-related Medication Non-adherence Rate Among Medicare-Medicaid Dual-Eligible Diabetes Patients. J Health Med Econ 2016;2. [PMC free article] [PubMed] [Google Scholar]
- 16.Nekhlyudov L, Madden J, Graves AJ, Zhang F, Soumerai SB, Ross-Degnan D. Cost-related medication nonadherence and cost-saving strategies used by elderly Medicare cancer survivors. J Cancer Surviv 2011;5:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kennedy JJ, Maciejewski M, Liu D, Blodgett E. Cost-related nonadherence in the Medicare program: the impact of Part D. Med Care 2011;49:522–6. [DOI] [PubMed] [Google Scholar]
- 18.Burcu M, Alexander GC, Ng X, Harrington D. Construct validity and factor structure of survey-based assessment of cost-related medication burden. Med Care 2015;53:199–206. [DOI] [PubMed] [Google Scholar]
- 19.An Overview of the Medicare Part D Prescription Drug Benefit. The Henry J. Kaiser Family Foundation, 2019. (Accessed February 7, 2020, at https://www.kff.org/medicare/fact-sheet/an-overview-of-the-medicare-part-d-prescription-drug-benefit/.) [Google Scholar]
- 20.Hoadley J Medicare’s New Adventure: The Part D Drug Benefit: The Commonweath Fund; 2006. [Google Scholar]
- 21.Gu Q, Zeng F, Patel BV, Tripoli LC. Part D coverage gap and adherence to diabetes medications. Am J Manag Care 2010;16:911–8. [PubMed] [Google Scholar]
- 22.Li P, McElligott S, Bergquist H, Schwartz JS, Doshi JA. Effect of the Medicare Part D coverage gap on medication use among patients with hypertension and hyperlipidemia. Ann Intern Med 2012;156:776–84, W-263, W-4, W-5, W-6, W-7, W-8, W-9. [DOI] [PubMed] [Google Scholar]
- 23.Medicare Part D in 2018: The Latest on Enrollment, Premiums, and Cost Sharing. The Henry J. Kaiser Family Foundation, 2018. (Accessed February 7, 2020, at https://www.kff.org/medicare/issue-brief/medicare-part-d-in-2018-the-latest-on-enrollment-premiums-and-cost-sharing/.) [Google Scholar]
- 24.Doshi JA, Li P, Pettit AR, Dougherty JS, Flint A, Ladage VP. Reducing out-of-pocket cost barriers to specialty drug use under Medicare Part D: addressing the problem of “too much too soon”. Am J Manag Care 2017;23:S39–S45. [PubMed] [Google Scholar]
- 25.Herkert D, Vijayakumar P, Luo J, et al. Cost-Related Insulin Underuse Among Patients With Diabetes. JAMA Intern Med 2019;179:112–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schondelmeyer SW, Purvis L. Trends in Retail Prices of Specialty Prescription Drugs Widely Used by Older Americans: 2017 Year-End Update. Washington, DC: AARP Public Policy Institute; 2019. [Google Scholar]
- 27.Pear R Lawmakers in Both Parties Vow to Rein In Insulin Costs. New York Times; April 10, 2019 [Google Scholar]
- 28.Services CfMM. MCBS 2015 Data User’s Guide: General Information. Baltimore: CMS Office of Enterprise Data and Analytics; 2017. [Google Scholar]
- 29.Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med 2007;22:864–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Total Medicare Enrollment 2011–2016. CMS Program Statistics; (Accessed on Feb 7, 2020 at https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/2016/Downloads/MDCR_ENROLL_AB/2016_CPS_MDCR_ENROLL_AB_1.pdf). [Google Scholar]
- 31.U.S. Federal Poverty Guidelines Used to Determine Financial Eligibility for Certain Federal Programs. DHHS Office of The Assistant Secretary for Planning and Evaluation; (Accessed on Feb 7, 2020 at https://aspe.hhs.gov/poverty-guidelines). [Google Scholar]
- 32.Gu D, Shen C. Assessing the Importance of Factors Associated with Cost-Related Nonadherence to Medication for Older US Medicare Beneficiaries. Drugs Aging 2019;36:1111–21. [DOI] [PubMed] [Google Scholar]
- 33.How Will The Medicare Part D Benefit Change Under Current Law and Leading Proposals? The Henry J. Kaiser Family Foundation, 2019. (Accessed July 22, 2020, at https://www.kff.org/medicare/issue-brief/how-will-the-medicare-part-d-benefit-change-under-current-law-and-leading-proposals/.) [Google Scholar]
- 34.Tang Y, Gellad WF, Men A, Donohue JM. Impact of medicare part D plan features on use of generic drugs. Med Care 2014;52:541–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katz S Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc 1983;31:721–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1 – Sensitivity analysis showing adjusted odds ratio estimates of CRN, spending less on other basic needs to afford medicine, and cost reduction strategies with drug coverage variables omitted
Supplemental Digital Content 2 – Sensitivity analyses examining US region and specific chronic conditions as potential risk factors
Supplemental Digital Content 3 – Longitudinal analyses, 2006–2016


