Abstract
Objectives
To determine for each basic, instrumental, and mobility activity after hospitalization for acute medical illness: (1) disability prevalence immediately before and monthly for 6 months after hospitalization; (2) disability incidence 1 month after hospitalization; and (3) recovery time from incident disability during months 2 to 6 after hospitalization.
Design
Prospective cohort study.
Setting
New Haven, Connecticut.
Participants
A total of 515 community-living persons, mean age 82.7 years, hospitalized for acute noncritical medical illness and alive within 1 month of hospital discharge.
Measurements
Disability was defined monthly for each basic (bathing, dressing, walking, transferring), instrumental (shopping, housework, meal preparation, taking medications, managing finances), and mobility activity (walking a quarter mile, climbing flight of stairs, lifting/carrying 10 pounds, driving) if help was needed to perform the activity or if a car was not driven in the prior month.
Results
Disability was common 1 and 6 months after hospitalization for activities frequently involved in leaving the home to access care including walking a quarter mile (prevalence 65% and 53%, respectively) and driving (65% and 61%). Disability was also common for activities involved in self-managing chronic health conditions including meal preparation (53% and 41%) and taking medications (41% and 31%). New disability was common and often prolonged. For example, 43% had new disability walking a quarter mile, and 30% had new disability taking medications, with mean recovery time of 1.9 months and 1.7 months, respectively. Findings were similar for the subgroup of persons residing at home (ie, not in a nursing home) at the first monthly follow-up interview after hospitalization.
Conclusion
Disability in specific functional activities important to leaving home to access care and self-managing health conditions is common, often new, and present for prolonged time periods after hospitalization for acute medical illness. Post-discharge care should support patients through extended periods of vulnerability beyond the immediate transitional period.
Keywords: geriatrics, disability, function, hospital care, transitional care
Among older persons, new disabilities are common after hospitalization for acute medical illness. These disabilities span multiple domains including basic self-care activities such as bathing and dressing,[1–6] instrumental activities such as shopping and preparing meals,[1] and mobility within and outside of the home.[2, 6, 7] New disabilities are associated with multiple adverse outcomes[8] including rehospitalization,[9, 10] nursing home placement, and death.[3, 10] Persistent disability is associated with an especially poor prognosis.[3]
Disability prevalence, incidence, and recovery after hospitalization have not been previously described at the individual task level across basic, instrumental, and mobility activities concurrently and monthly in the post-hospital period. Such granular descriptions of disability and recovery in individual functional tasks have been largely restricted to persons undergoing elective surgical procedures[11–16] or having experienced injurious falls including hip fractures.[17–20] Studies of medical hospitalizations have almost exclusively focused on basic activities[3, 21–23] but without pre-hospital assessments or serial monthly assessments after discharge to delineate disability incidence and recovery more clearly across the full range of individual functional tasks. These data are critical to understanding the specific functional needs experienced by older persons after medical illness, how often these needs are new, and their expected time course, as well as to design both transitional- and post-acute care services rationally to best support older adults after hospitalization, many of whom may have new difficulties with leaving their home to access care and with self-managing their chronic health conditions.
To examine this topic, we studied medical hospitalizations from the Precipitating Events Project (PEP), an ongoing longitudinal study of 754 community-living persons, aged 70 years or older, who were initially nondisabled in their basic activities.[24] We focused on community-living persons because new disability is of greater significance in this context rather than among persons who are already institutionalized. We calculated the (1) prevalence of disability for each basic, instrumental, and mobility activity immediately before and monthly for 6 months after hospitalization; (2) incidence of disability for each activity 1 month after hospitalization; and (3) time to recovery from incident disability for each activity during months 2 to 6 after hospitalization.
METHODS
Study Population
Study participants are a subset of members of the PEP, a longitudinal study of 754 community-living persons, aged 70 years or older, who required no assistance at the time of the initial PEP study enrollment in four basic activities: bathing, dressing, walking inside the house, and transferring from a chair.[24] Participants were drawn from a computerized list of 3157 age-eligible members of a large health plan in greater New Haven. They were excluded if they had significant cognitive impairment and no available proxy, if they did not speak English, if they had a limited life expectancy of less than 12 months based on the presence of a terminal diagnosis, or if they planned to move away from New Haven in the 12 months after enrollment. Eligibility was determined during a screening telephone interview and confirmed by a research nurse during an in-home assessment.[25] Of the 2753 potential participants who were age eligible, alive, and could be contacted by telephone, only 4.6% declined to complete the screening interview. Ultimately 75.2% of potentially eligible participants agreed to study enrollment. The Yale Human Investigation Committee approved the study protocol, and all study participants provided verbal informed consent.
Comprehensive home-based assessments were completed at baseline and subsequently at 18-month intervals for 216 months (with the exception of 126 mo), and telephone interviews were completed monthly through June 30, 2016. For participants who had significant cognitive impairment or were otherwise unavailable, a proxy was interviewed using a rigorous protocol, with demonstrated reliability and validity.[26] A total of 516 (89.6%) participants died after a median of 110 months; 20 (2.6%) dropped out of the study after a median of 56 months. Data were otherwise available for 99.5% of 6486 monthly interviews.
Analytic Samples
Assembly of the primary analytic sample is summarized in Supplementary Figure S1. From the cohort of 754 PEP participants, we included the first hospitalization and drew baseline characteristics from the last face-to-face interview before the hospitalization. Because our aim was to evaluate disability and recovery after hospitalization for medical illness, we did not include hospitalizations for surgical procedures[27] or with in-hospital death. We also did not include hospitalizations involving stays in an intensive care unit because persons with critical illness are a distinct population with frequent disability and prolonged recovery as previously described.[28–30]
Included hospitalizations originated from the emergency department because these are less likely to be elective. We excluded hospitalizations among participants residing in a nursing home in the month before hospitalization as well as among participants discharged on hospice because many of these people have significant preexisting disabilities and advanced illness and would therefore not be expected to recover from incident disability in a new activity after hospitalization. We also excluded hospitalizations resulting in death after discharge but before the first follow-up interview. We ultimately retained only the first hospitalization per participant to eliminate bias from participants contributing more than one hospitalization to the analytic sample.
We additionally examined disability among the subgroup of participants residing at home at the first monthly follow-up interview after hospital discharge. Disabilities in this secondary analytic sample may be particularly challenging to manage in the absence of the around-the-clock supports for basic, instrumental, and mobility activities.
Data Collection
The baseline characteristics of hospitalized participants were drawn from the last comprehensive homebased assessment performed before hospitalization. In addition to demographic factors describing age, sex, ethnicity, educational attainment, and living situation (alone or not), we also examined factors from four domains related to disability[31]: health status, psychosocial, behavioral, and physical capacity. Health status factors included nine self-reported chronic conditions, cognitive impairment (Mini-Mental Status Examination score <24),[32] corrected near vision,[33] hearing,[34] self-report of 4.5 kg of weight loss in the past year,[35] and body mass index (BMI).
Psychosocial factors included depressive symptoms[36] and social support.[37] Behavioral factors included smoking status and physical activity levels.[38] Physical capacity factors included a modified version of the Short Physical Performance Battery (score range = 0–12)[39] that included the standard balance maneuvers but substituted three timed chair stands (instead of five) and a timed rapid gait test instead of a timed usual gait test,[40] as well as dominant hand grip strength adjusted for sex and BMI.[35]
Trained research staff collected data on disability during the monthly telephone interviews based on participant self-report. Disability was defined for each basic (bathing, dressing, walking across a room, transferring from a chair), instrumental (shopping, housework, meal preparation, taking medications, managing finances), and mobility activity (walking a quarter mile, climbing a flight of stairs, lifting or carrying 10 pounds) if help was needed from another person to perform the activity. For driving, disability was defined as not driving a car in the prior month as previously described.[31] Reliability of these assessments was substantial when 126 participants were interviewed twice within 3 days by different interviewers,[24] and it was moderate or better for 11 of the 13 activities.[41]
Study Outcomes
For each basic, instrumental, and mobility activity, outcomes included (1) disability prevalence in the month before hospitalization and each of the 6 months after hospitalization; (2) disability incidence at the first monthly follow-up interview after hospitalization among persons without disability in the month before hospitalization; and (3) recovery from incident disability during months 2 to 6 after hospitalization. For all activities other than driving, recovery was defined as the ability to once again perform the activity without help from another person. For driving, recovery was defined as the performance of this activity once again.
Statistical Analysis
We reported characteristics of all hospitalized patients before the included hospitalizations using counts (percentages) or means with standard deviations. We also separately reported preadmission characteristics for hospitalized patients with incident disability in each basic, instrumental, and mobility activity in the month after hospitalization.
We calculated the prevalence of disability in each basic, instrumental, and mobility activity in the month before hospitalization and each of the 6 months after hospitalization. We then calculated the proportion of participants with new disability (ie, incident) in each basic, instrumental, and mobility activity comparing the month after hospitalization with the month before hospitalization. We next used Kaplan-Meyer survival curves to evaluate time to recovery for each activity among incident cases only, with follow-up starting from month 2 after hospitalization. The cumulative probability of recovery for each activity was estimated after accounting for censoring due to mortality and loss to follow-up. We finally calculated the proportion of participants with incident disability in each basic, instrumental, and mobility activity who were nondisabled in the specific activity 6 months after hospitalization. We repeated all analyses for the subset of study participants who were at home, rather than in a nursing facility, at the first monthly follow-up interview after hospital discharge.
All analyses were performed using SAS v.9.4); a two-tailed P < .05 was considered statistically significant.
RESULTS
Table 1 shows the characteristics of the 515 study participants before the first index hospitalization. The mean age was 82.7 years. Geriatric conditions, living alone, and low social support were common. Table 2 shows a subset of characteristics before the first index hospitalization among the 402 study participants reporting incident disability in specific activities after hospitalization. Supplementary Tables S1 and S2 show the characteristics of the 368 study participants residing at home during the first monthly follow-up interview after hospital discharge and the subgroup of 238 reporting incident disability in specific activities at this interview, respectively.
Table 1.
Characteristics of Hospitalized Participants at Last Face-to-Face Interview Before Hospitalization for Acute Medical Illness (N = 515)
| Characteristic | Measurement details | N (%) or mean (SD) |
|---|---|---|
| Demographics | ||
| Mean (SD) age, y | 82.7 (5.6) | |
| Female sex | 338 (65.6) | |
| Non-Hispanic white ethnicity | 458 (88.9) | |
| Living alone | 240 (46.6) | |
| Did not complete high school | 185 (35.9) | |
| Health related | ||
| Mean (SD) chronic conditions, n | Nine self-reported physician-diagnosed conditions | 2.2 (1.3) |
| Cognitive impairment | MMSE score <24 | 92 (17.9) |
| Moderate or severe visual impairment | Jaeger card score >696 | 130 (25.2) |
| Moderate or severe hearing impairment | Two or more tones missed on hearing test | 168 (32.6) |
| Depressive symptoms | CES-D score ≥20 | 100 (19.4) |
| Weight loss | ≥4.5 kg in past year | 129 (25.1) |
| Overweight or obese | BMI ≥25 mg/m2 | 283 (54.9) |
| Psychosocial | ||
| Low social support | MOS score ≤18 | 138 (26.8) |
| Behavioral | ||
| Current smoker | 35 (6.8) | |
| Low physical activity | PASE score <52 (women) or <64 (men) | 258 (50.1) |
| Physical capacity | ||
| Mean (SD) SPPB score | Score range = 0–12 | 5.6 (2.8) |
| Hand grip less than sex-specific and BMI-specific cut points | 352 (68.4) |
Abbreviations: BMI, body mass index; CES-D, Center of Epidemiologic Studies Depression Scale; MMSE, Mini-Mental State Examination; MOS, medical outcomes study; PASE, physical activity scale for the elde rly; SD, standard deviation; SPPB, short physical performance battery.
Note: Study participants are a subset of members of the Precipitating Events Project, as described in the Methods section of the text.
Table 2.
Characteristics of Hospitalized Participants with New Disability in Specific Activities After Hospitalization for Acute Medical Illness
| Functional domain (n = newly disabled in domain) | Mean (SD) age, y | Female sex, n (%) | Non-Hispanic white ethnicity, n (%) | Did not complete high school, n (%) | Mean (SD) chronic conditions |
|---|---|---|---|---|---|
| Basic activities | |||||
| Bathing (n = 136) | 84.2 (5.1) | 103 (75.7) | 126 (92.7) | 48 (35.3) | 2.3 (1.3) |
| Dressing (n = 100) | 84.4 (5.2) | 70 (70.0) | 91 (91.0) | 37 (37.0) | 2.4 (1.3) |
| Walking across a room (n = 96) | 84.8 (5.5) | 73 (76.0) | 89 (92.7) | 33 (34.4) | 2.4 (1.4) |
| Transferring from a chair (n = 79) | 845 (5.4) | 61 (77.2) | 68 (86.1) | 25 (31.7) | 2.4 (1.4) |
| Instrumental activities | |||||
| Shopping (n = 127) | 82.7(5.1) | 87 (68.5) | 116 (91.3) | 39 (30.7) | 2.4 (1.3) |
| Housework (n = 95) | 82.1 (4.8) | 64 (67.4) | 83 (87.4) | 36 (37.9) | 2.3 (1.3) |
| Meal preparation (n = 153) | 83.0 (4.8) | 113 (73.9) | 138 (90.2) | 48 (31.4) | 2.3 (1.4) |
| Taking medications (n = 128) | 83.8 (4.7) | 90 (70.3) | 114 (89.1) | 41 (32.0) | 2.3 (1.3) |
| Managing finances (n = 101) | 83.8 (5.4) | 67 (68.4) | 92 (93.9) | 28 (28.6) | 2.1 (1.3) |
| Mobility activities | |||||
| Walking quarter mile (n = 113) | 83.0 (5.2) | 70 (62.0) | 103 (91.2) | 36 (31.9) | 2.2 (1.3) |
| Climbing a flight of stairs (n = 146) | 840 (5.3) | 100 (68.5) | 129 (88.4) | 49 (33.6) | 2.2 (1.2) |
| Lifting or carrying 10 pounds (n = 133) | 82.8 (5.3) | 97 (72.9) | 118 (88.7) | 46 (34.6) | 2.1 (l.2) |
| Driving (n = 62) | 82.2 (4.9) | 41 (66.1) | 54 (87.1) | 19 (30.7) | 2.2 (1.3) |
Abbreviation: SD, standard deviation.
Note: Total N = 402 participants with incident disability in one or more of the 13 functional activities.
Figure 1 shows the prevalence of disability for each basic, instrumental, and mobility activity in panels A, B, and C, respectively. At months 1 and 6 after hospitalization, disability was common for activities frequently involved in leaving the home to access care including dressing (25% and 18%), walking across a room (19% and 9%), transferring from a chair (prevalence 18% and 10%, respectively), walking a quarter mile (65% and 53%), climbing a flight of stairs (45% and 31%), and driving (65% and 61%). Disability at months 1 and 6 after hospitalization was also common for activities involved in health promotion and self-management including meal preparation (prevalence 53% and 41%, respectively) and taking medications (41% and 31%). Supplementary Figure S2 shows the prevalence of disability among study participants residing at home during the first follow-up interview. Although disability was less common among participants at home, it was still often present.
Figure 1.
Prevalence of disability before and after hospitalization for acute medical illness for each basic, instrumental, and mobility activity. Data on disability were collected during monthly telephone interviews. Disability was defined for each basic (bathing, dressing, walking across a room, transferring from a chair), instrumental (shopping, housework, meal preparation, taking medications, managing finances), and mobility activity (walking a quarter mile, climbing a flight of stairs, lifting or carrying 10 pounds) if help was needed from another person to perform the activity. Disability was defined for driving if the participant did not drive a car in the month preceding the interview. The number of participants contributing data was 515 in the month before hospitalization and 515, 499, 489, 481, 478, and 472 during months 1 through 6 after hospital discharge, respectively. Data for basic activities are shown in panel A, instrumental activities in panel B, and mobility activities in panel C.
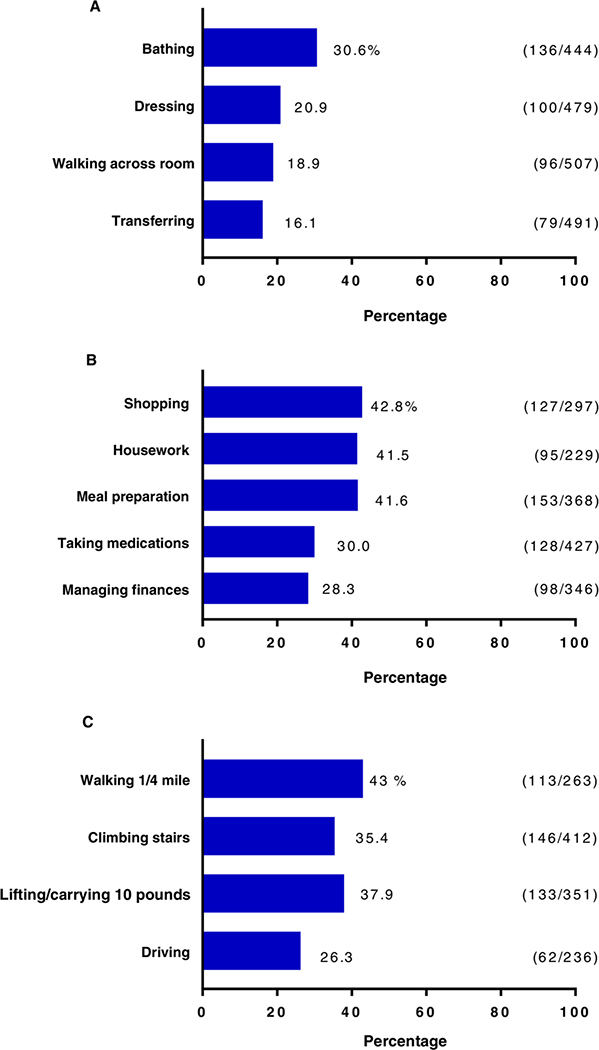
Figure 2 shows the incidence of disability at the first monthly follow-up interview after hospitalization for each basic, instrumental, and mobility activity in panels A, B, and C, respectively. New disability was common after hospitalization. For example, 30.6% of participants had new disability in bathing, 41.5% had new disability with housework, 30.0% had new disability taking medications, and 43.0% had new disability walking a quarter mile. Supplementary Figure S3 shows the incidence of disability at the first monthly follow-up interview after hospitalization among study participants residing at home during the first follow-up interview. Incident disability was again common.
Figure 2.
Proportion newly disabled at 1 month after hospitalization for acute medical illness for each basic, instrumental, and mobility activity. We calculated the incidence proportion of disability in each basic, instrumental, and mobility activity comparing the month after hospitalization with the month before hospitalization in panels A, B, and C, respectively.
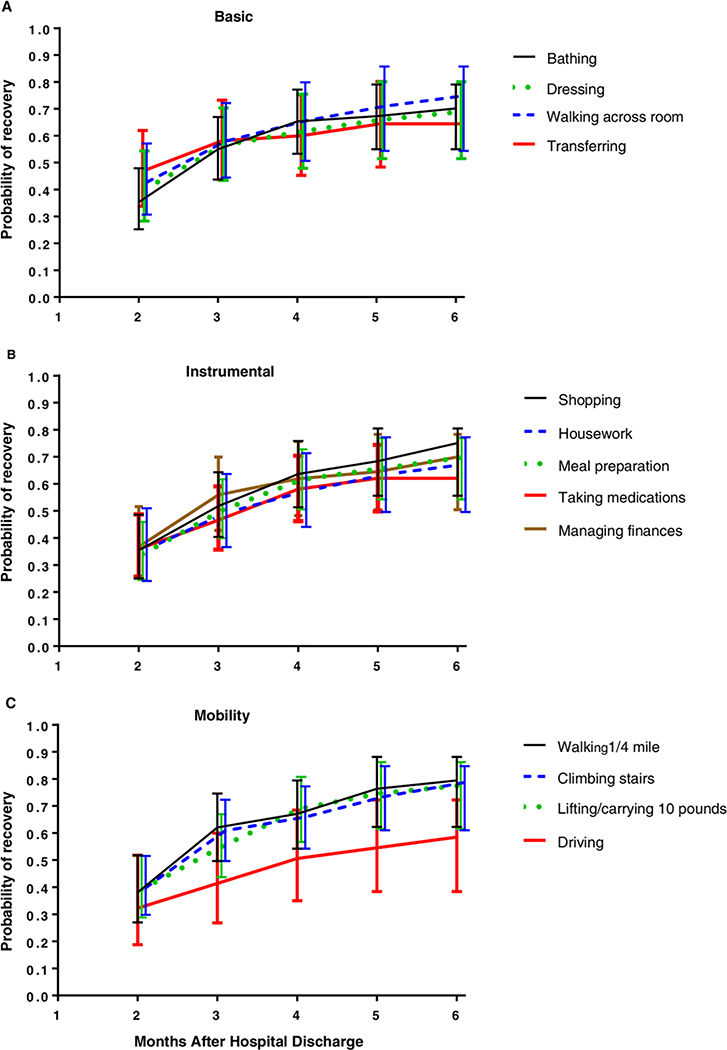
Figure 3 shows the cumulative probability of recovery in disability among participants with incident disability in basic, instrumental, and mobility activities in panels A, B, and C, respectively. Mean time to recovery varied between 1.3 and 2.0 months across activities. Recovery trajectories were comparable for each activity within a domain, with the exception of driving, for which recovery was less common compared with the other mobility activities. Supplementary Figure S4 likewise shows the cumulative probability of recovery in disability among participants with incident disability in basic, instrumental, and mobility activities who were at home at their first monthly follow-up interview.
Figure 3.
Cumulative probability of recovery after hospitalization for acute medical illness for each basic, instrumental, and mobility activity. We used Kaplan-Meyer survival curves to evaluate time to recovery for each activity among incident disability cases at the first monthly interview after hospitalization with follow-up starting from month 2 after hospitalization. The cumulative probability of recovery for each activity was estimated after accounting for censoring due to mortality and loss to follow-up. Data for basic, instrumental, and mobility activities are shown in panels A, B, and C, respectively. Error bars denote standard deviations.
Supplementary Figure S5 shows the proportion of participants with incident disability in basic, instrumental, and mobility activities who were nondisabled in the specific activity 6 months after hospitalization in panels A, B, and C, respectively. Recovery was often incomplete even 6 months after hospital discharge. For example, the proportion nondisabled at 6 months was just 65.4% for bathing, 65.4% for meal preparation, 57.8% for taking medications, 76.1% for walking a quarter mile, and 54.8% for driving. Supplementary Figure S6 likewise shows the proportion of participants with incident disability who were at home at their first monthly follow-up interview after hospital discharge and were nondisabled in the specific activity 6 months after hospitalization. Recovery was again often incomplete.
DISCUSSION
Through examination of more than 500 medical hospitalizations among initially community-living older persons participating in the PEP, we found that disability in specific functional activities important to leaving the home to access care and self-managing chronic health conditions such as transferring from a chair, driving, and taking medications is frequently present in the 6 months after hospital discharge. We also found that disabilities across basic, instrumental, and mobility activities are often new following hospitalization and that recovery from disability in these activities is often incomplete and even when complete, slow to occur. These findings apply even to persons residing at home, and not in a nursing home, 1 month after hospital discharge. Transitional- and post-acute care services should therefore be designed to support functionally disabled persons, many of whom will have new needs to which they are unaccustomed for extended time periods after hospitalization.
Findings extend the literature in a number of ways. We have identified common disabilities in function after medical hospitalization at the task level, many of which are important to accessing care and self-managing health. These include disabilities in walking across a room (prevalence 19% at first monthly follow-up interview after hospitalization), transferring from a chair (prevalence 18%), walking a quarter mile (prevalence 65%), preparing meals (prevalence 53%), and taking medications (prevalence 41%). We have also shown that many of these disabilities are new and last for prolonged periods of time following hospitalization, suggesting that many older persons will require extended support. For example, 31% of participants had new disability in bathing at the first monthly follow-up interview, more than one-third of whom could not bathe independently even 6 months after discharge.
Findings extend to patients at home at the time of the first monthly follow-up after hospitalization who may not have around-the-clock support for basic and instrumental activities. For example, 16% of such persons had new disability taking medications, and 32% had new difficulty walking a quarter mile. These results extend previous work finding decrements in self-reported basic activities after medical hospitalizations,[3, 21–23] albeit at a more granular level by month and across multiple functional tasks including instrumental and mobility activities.
Our study found that the long-term prevalence of disability at the task level is higher than after hospitalizations for elective intra-abdominal surgery,[12] including for gastric and colorectal cancer,[11] and lower than after hospitalizations for hip fractures,[19, 20, 42] as might be expected based on the types of patients experiencing these events and their planned versus unplanned nature. Our results are also consistent with previous research finding worse long-term community mobility following medical hospitalizations compared with surgical hospitalizations, many of which were elective.[43]
The current study has a number of strengths. Functional status was assessed prospectively before hospitalization, thereby avoiding any potential concerns that bias in recall of preadmission functional status could influence determinations of disability incidence. Function was also determined monthly following hospitalization across basic, instrumental, and mobility domains with minimal loss to follow-up, permitting granular descriptions of disability prevalence, incidence, and recovery at the task level. Assessments of these tasks were shown to have moderate to high test-retest reliability.[24] The PEP also includes information on a broad range of factors including geriatric impairments, living situation, social support, and other variables that help contextualize study findings.
Results should be interpreted in the context of the following potential limitations. First, measures of function were based on participant self-report rather than objective measurements. However, self-reported function is strongly associated with adverse health outcomes[3, 8] and often used to guide coverage determinations in the Medicare program.[44] Second, formal statistical comparisons of recovery across functional activities were not possible because participants in each sample of incident disability differed. Third, the study does not include surgical hospitalizations or hospitalizations for severe medical illnesses requiring stays in an intensive care unit because these patient subgroups are distinct with unique recovery trajectories based on previous analyses.[12, 20, 29]
Our findings have implications for clinical practice and research. The many patients who have disability after hospitalization may have undue difficulty leaving their homes to access office-based ambulatory care and may therefore benefit from care delivered to the home. These include persons initially discharged home from the hospital as well as those who eventually return home after a nursing home stay. Interventions for these patients can include provider house calls,[45] home-based laboratory and radiology testing, and telehealth.[46] Unfortunately, delivery of these services has been hampered by poor reimbursement rates by payers,[47] limited workforce capacity,[47] and regulatory restrictions limiting qualification for these options.[44, 46] These restrictions have often also extended to nonskilled providers such as home health aides and homemakers,[48] who can help patients self-manage their health through many means including meal preparation and medication management.
In the absence of these resources, patients may benefit from greater access to home-delivered medications and meals in the post-hospital period,[49] especially if they live alone, as was the case for more than two-fifths of study participants. These home services may also be needed for prolonged periods of time well beyond the 30-day period that has been the focus of hospitals’ readmission prevention efforts to date. Our analysis characterized post-hospitalization disability starting in the month after hospitalization and still found it to be common and frequently unresolved even 5 months later.
Findings also suggest that discharge planning should include preparation for life after serious illness resulting in hospitalization. Planning discussions around hospitalization frequently include topics related to life-sustaining treatment,[50] but patients may also benefit from ensuring that necessary supports are in place to manage basic, instrumental, and mobility activities for extended time periods after returning home, if necessary.
Further research is needed to understand the determinants of disability in individual functional tasks after hospitalization including the hospitalization experience itself[8, 51, 52] and care received following hospital discharge. These findings can inform development of data-driven interventions to reduce incident disability and hasten recovery in function after hospitalization.
In conclusion, we found that many community-living older persons discharged from the hospital after acute medical illness have disability in specific functional activities important to leaving the home to access care and self-managing health conditions. We also found that these disabilities are often new following hospitalization and that recovery from disability is frequently incomplete 6 months after discharge, even among persons who return home in the month after hospitalization. As our health system increasingly moves from volume to value, transitional and post-acute care models will need to adapt in turn to help recently hospitalized patients overcome specific disabilities in efficient and effective ways.
Supplementary Material
ACKNOWLEDGMENTS
Financial Disclosure
The work for this report was funded by grant R01AG17560 from the National Institute on Aging (NIA). The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center, funded by grant P30AG21342 from the NIA. At the time this research was conducted, Kumar Dharmarajan was supported by grant K23AG048331 from the NIA and the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. Thomas M. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the NIA.
Sponsor’s Role
This study was funded by the National Institute on Aging that had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; in the preparation, review, and approval of the manuscript; or in the decision to submit it for publication.
Footnotes
Conflict of Interest
Kumar Dharmarajan is the chief scientific officer of Clover Health, a Medicare Advantage company. The other authors have declared no conflicts of interest for this article.
REFERENCES
- [1].Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996; 156:645–652. [PubMed] [Google Scholar]
- [2].Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004; 292:2115–2124. [DOI] [PubMed] [Google Scholar]
- [3].Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008; 56:2171–2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Boyd CM, Ricks M, Fried LP, et al. Functional decline and recovery of activities of daily living in hospitalized, disabled older women: the Women’s Health and Aging Study I. J Am Geriatr Soc. 2009; 57:1757–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010; 304:1919–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Barry LC, Murphy TE, Gill TM. Depression and functional recovery after a disabling hospitalization in older persons. J Am Geriatr Soc. 2011; 59:1320–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Loyd C, Beasley TM, Miltner RS, Clark D, King B, Brown CJ. Trajectories of community mobility recovery after hospitalization in older adults. J Am Geriatr Soc. 2018; 66:1399–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “she was probably able to ambulate, but I’m not sure”. JAMA. 2011; 306:1782–1793. [DOI] [PubMed] [Google Scholar]
- [9].Depalma G, Xu H, Covinsky KE, et al. Hospital readmission among older adults who return home with unmet need for ADL disability. Gerontologist. 2013; 53:454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of Independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg. 2016; 151:e161689. [DOI] [PubMed] [Google Scholar]
- [11].Amemiya T, Oda K, Ando M, et al. Activities of daily living and quality of life of elderly patients after elective surgery for gastric and colorectal cancers. Ann Surg. 2007; 246:222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004; 199:762–772. [DOI] [PubMed] [Google Scholar]
- [13].Van Cleave JH, Egleston BL, McCorkle R. Factors affecting recovery of functional status in older adults after cancer surgery. J Am Geriatr Soc. 2011; 59:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Finlayson E, Zhao S, Boscardin WJ, Fries BE, Landefeld CS, Dudley RA. Functional status after colon cancer surgery in elderly nursing home residents. J Am Geriatr Soc. 2012; 60:967–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kwon S, Symons R, Yukawa M, Dasher N, Legner V, Flum DR. Evaluating the association of preoperative functional status and postoperative functional decline in older patients undergoing major surgery. Am Surg. 2012; 78:1336–1344. [PMC free article] [PubMed] [Google Scholar]
- [16].Brinson Z, Tang VL, Finlayson E. Postoperative functional outcomes in older adults. Curr Surg Rep 2016; 4(6): pii 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Eastwood EA, Magaziner J, Wang J, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002; 50:1240–1249. [DOI] [PubMed] [Google Scholar]
- [18].Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. 2013; 178:418–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990; 45:M101–M107. [DOI] [PubMed] [Google Scholar]
- [20].Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000; 55:M498–M507. [DOI] [PubMed] [Google Scholar]
- [21].Barnes DE, Mehta KM, Boscardin WJ, et al. Prediction of recovery, dependence or death in elders who become disabled during hospitalization. J Gen Intern Med. 2013; 28:261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chodos AH, Kushel MB, Greysen SR, et al. Hospitalization-associated disability in adults admitted to a safety-net hospital. J Gen Intern Med. 2015; 30:1765–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zaslavsky O, Zisberg A, Shadmi E. Impact of functional change before and during hospitalization on functional recovery 1 month following hospitalization. J Gerontol A Biol Sci Med Sci. 2015; 70:381–386. [DOI] [PubMed] [Google Scholar]
- [24].Gill TM. Disentangling the disabling process: insights from the precipitating events project. Gerontologist. 2014; 54:533–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001; 135:313–321. [DOI] [PubMed] [Google Scholar]
- [26].Gill TM, Hardy SE, Williams CS. Underestimation of disability in community-living older persons. J Am Geriatr Soc. 2002; 50:1492–1497. [DOI] [PubMed] [Google Scholar]
- [27].Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011; 378:1408–1413. [DOI] [PubMed] [Google Scholar]
- [28].Ehlenbach WJ, Larson EB, Curtis JR, et al. Physical function and disability after acute care and critical illness hospitalizations in a prospective cohort of older adults. J Am Geriatr Soc. 2015; 63:2061–2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015; 175:523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Brummel NE, Balas MC, Morandi A, Ferrante LE, Gill TM, Ely EW. Understanding and reducing disability in older adults following critical illness. Crit Care Med. 2015; 43:1265–1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gill TM, Gahbauer EA, Murphy TE, Han L, Allore HG. Risk factors and precipitants of long-term disability in community mobility: a cohort study of older persons. Ann Intern Med. 2012; 156:131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Folstein MF, Folstein SE, McHugh PR . “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198. [DOI] [PubMed] [Google Scholar]
- [33].Spaeth EB, Fralick FB, Hughes WF Jr. Estimation of loss of visual efficiency. AMA Arch Ophthalmol. 1955; 54:462–468. [DOI] [PubMed] [Google Scholar]
- [34].Lichtenstein MJ, Bess FH, Logan SA. Validation of screening tools for identifying hearing-impaired elderly in primary care. JAMA. 1988; 259:2875–2878. [PubMed] [Google Scholar]
- [35].Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006; 166:418–423. [DOI] [PubMed] [Google Scholar]
- [36].Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993; 5:179–193. [DOI] [PubMed] [Google Scholar]
- [37].Hardy SE, Gill TM. Factors associated with recovery of independence among newly disabled older persons. Arch Intern Med. 2005; 165:106–112. [DOI] [PubMed] [Google Scholar]
- [38].Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The Physical Activity Scale for the Elderly (PASE): evidence for validity. J Clin Epidemiol 1999; 52:643–651. [DOI] [PubMed] [Google Scholar]
- [39].Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000; 55:M221–M231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Gill TM, Murphy TE, Barry LC, Allore HG. Risk factors for disability subtypes in older persons. J Am Geriatr Soc. 2009; 57:1850–1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. [PubMed] [Google Scholar]
- [42].Dyer SM, Crotty M, Fairhall N, et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016; 16:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009; 150:372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Rotenberg J, Kinosian B, Boling P, Taler G, Independence at Home Learning Collaborative Writing Group. Home-based primary care: beyond extension of the independence at home demonstration. J Am Geriatr Soc 2018; 66:812–817. [DOI] [PubMed] [Google Scholar]
- [45].Daschle T, Dorsey ER. The return of the house call. Ann Intern Med. 2015; 162:587–588. [DOI] [PubMed] [Google Scholar]
- [46].Centers for Medicare & Medicaid Services. MLN booklet: telehealth services. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf Accessed September 7, 2019.
- [47].Klein S, Hostetter M, McCarthy D. An overview of home-based primary care: learning from the field. Issue Brief (Commonw Fund). 2017; 15:1–20. [PubMed] [Google Scholar]
- [48].Hewko SJ, Cooper SL, Huynh H, et al. Invisible no more: a scoping review of the health care aide workforce literature. BMC Nurs 2015; 14:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Gualtieri MC, Donley AM, Wright JD, Vega SS. Home delivered meals to older adults: a critical review of the literature. Home Healthc Now. 2018; 36:159–168. [DOI] [PubMed] [Google Scholar]
- [50].Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: a systematic review of the literature. J Am Geriatr Soc. 2015; 63:341–350. [DOI] [PubMed] [Google Scholar]
- [51].OʼBrien MR, Rosenthal MS, Dharmarajan K, et al. Balloon animals, guitars, and fewer blood draws: applying strategies from pediatrics to the treatment of hospitalized adults. Ann Intern Med. 2015; 162:726–727. [DOI] [PubMed] [Google Scholar]
- [52].Goldwater DS, Dharmarajan K, McEwan BS, et al. Is posthospital syndrome a result of hospitalization-induced allostatic overload? J Hosp Med 2018. 10.12788/jhm.2986. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.