Classical ethical questions often arise during the transplant allocation process due to an inadequate number of donor organs relative to potential recipients. One such question is how to weigh the benefit for one recipient versus a potentially greater good for the overall population following an alternative allocation. Such questions are very topical given that the United Network for Organ Sharing (UNOS) implemented a new heart transplant allocation system in the United States in October 2018.1 This system further stratified disease acuity of the most ill patients in an attempt to increase allocation of organs to the sickest patients. As with prior versions, however, it was based largely on specific therapies given to the patient (e.g., dose and number of inotrope agents, right heart catheter, or temporary mechanical circulatory support (MCS) devices). Thus, the new heart allocation system is still based on subjective physician decision making, allowing bias as well as center-specific and regional variations in practice patterns to influence which patients receive heart transplants. In contrast, other organ allocation systems, such as those used for liver and lungs, rely on allocation scores largely based on objective parameters such as laboratory and test results to determine disease severity. When the new heart allocation system was developed, it was thought that the available data were inadequate to develop such an objective heart allocation score. The consequences of the current approach, based on subjective treatment decisions, are evident in the following patient scenario. If a potential heart transplant recipient has a cardiac index of 1.7 L/min/m2 with a systolic blood pressure <90 mm Hg and pulmonary capillary wedge pressure of 20 mm Hg, some physicians may consider escalation to an intra-aortic balloon pump, earning a UNOS Status 2 for transplant listing for their patient, whereas other physicians may consider initiation of inotropes, leading to their patient receiving a lower priority Status 3 on the transplant list.
One concern is that physicians may implement therapies not necessarily based on severity of illness but simply in an effort to move their patients up on the list and access a transplant faster. This practice is often described as “gaming the system.” However, the situation is far more complex than the word “gaming” would suggest.
Gaming the system implies an undercurrent of something nefarious: bending the rules put in place with intent to achieve an outcome favorable to the perpetrator. The negative connotations of this word are evident in the dictionary description where gaming the system is using “knowledge of the rules to obtain benefits from a situation, especially in an unfair way.”2 Physicians may be influenced by a desire to grow the volume at their transplant center, particularly since program volume is often the key measure of success. Indeed, “How many transplants have you done this year?” is often the first question transplant clinicians ask one other. Economic benefits could accrue to those physicians practicing at a center with growing volumes. Additionally, the outcomes of programs with low transplant volumes are especially vulnerable to the impact of unexpected deaths which can lead to loss of favorable insurance contracts or regulatory consequences including discontinuation of a program. Likewise, physicians at large programs are more willing to transplant high-risk patients, not only offering hope to patients who otherwise may not be deemed suitable for transplant, but also enhancing the reputation of their program. Thus, we cannot completely discount psychological, economic and regulatory forces that may sway physicians to make decisions that benefit their individual patients and program despite potential harm to patients at other medical centers.
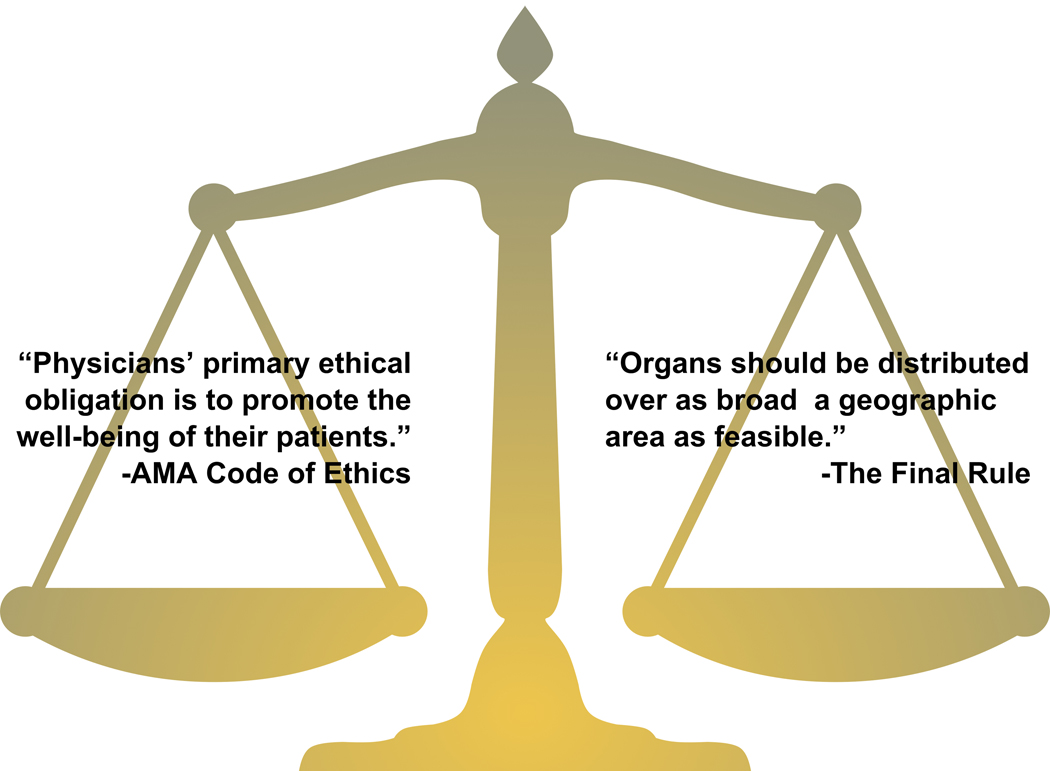
The more complex side of decision making, however, is not aligned with the negative connotations associated with the word ‘gaming.’ Standing at the bedside and watching patients deteriorate from advanced heart failure and progress towards death, transplant physicians feel a pressing need to intervene, to do something to help save their lives. Physicians’ primary ethical obligation is to the well-being of their patients.3 Getting a patient transplanted quickly by attaining the highest transplant status possible aligns with that obligation, which at times can be in conflict with adhering to protocols that are designed to promote fair allocation of donor organs (Figure). Moreover, if transplant physicians interpret the rules too strictly, they are at risk of disadvantaging their patients as other physicians make alternative choices to improve the chances of an organ allocation to the patients at their center.
The Difficult Balance Faced by Heart Transplant Physicians: An Ethical Obligation to Their Individual Patients vs. the Needs of the Broader Population.
The American Medical Association tells all physicians that their primary ethical obligation is to their individual patient. Transplant physicians are also told by regulatory policies (i.e., ‘The Final Rule’) that donor organs are a national resource that must be distributed equitably to the most appropriate patient on the waitlist, sometimes to the detriment of their individual patient.
Historically, clinical practice has shifted with changes in allocation criteria. For example, right heart catheter use increased following adoption of the prior iteration of the heart allocation criteria where right heart catheters in conjunction with two inotropes achieved top priority on the transplant list. When the 2018 heart allocation changes were available for public comment, there was concern that the proposed changes would lead to an increase in the use of extracorporeal membranous oxygenation (ECMO) and temporary MCS because these therapies conferred highest priority on the list.4 Early data suggest that most patients are being transplanted as Status 25 and anecdotally, IABP and Impella use, which confer status 2 listing, may be increasing. The risks associated with transplant from ECMO (Status 1) may be restraining broader adoption of that approach. The decision to initiate temporary MCS may lead to a faster availability of an organ at an acceptable risk, and earlier organ availability could be the deciding factor between life and death for a patient. Is this gaming or advocating? The line is blurred.
Words matter. Describing the behavior of transplant physicians as “gaming” does not recognize the ethical mandate that physicians bear towards their patients and is a gross oversimplification of the influences at play. This is a disservice to the transplant community and we recommend avoidance of it use. Likewise, calling this behavior “patient advocacy” is equally problematic and inadequate. Transplant physicians are inherently challenged when advocating simultaneously for their patients, programs, and societal good. The question is not only “How will physicians game the system?” but also “What will physicians do in order to provide the best outcomes for their patients?” The transplant community would be wise to consider, both in policy development and spoken word, the difficult ethical balance faced by physicians during the allocation process.
Acknowledgments
Funding: Dr. Khazanie has institutional research grant support from National Institutes of Health (K23 HL145122) and the Center for Women’s Health Research, University of Colorado Anschutz Medical Campus. Dr. Drazner is supported by the James M. Wooten Chair in Cardiology at UT Southwestern Medical Center.
Footnotes
Disclosures: Dr. Khazanie has no disclosures. Dr. Drazner was a member of the UNOS Thoracic Organ Transplantation Committee from 2014 to 2017.
Contributor Information
Prateeti Khazanie, Section of Advanced Heart Failure and Transplantation, Division of Cardiology, Department of Medicine, University of Colorado School of Medicine, Aurora, CO.
Mark H. Drazner, Division of Cardiology, Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, TX.
References
- 1.US Department of Health and Human Services. Organ Procurement and Transplantation Network. Adult Heart Allocation. https://optn.transplant.hrsa.gov/learn/professional-education/adult-heart-allocation/. Originally published October 18, 2018. Accessed June 20, 2019.
- 2.Macmillan Dictionary. Game- Definition and Synonyms. https://www.macmillandictionary.com/us/dictionary/american/game_3 Accessed July 27, 2019.
- 3.American Medical Association. Allocating limited health care resources. https://www.ama-assn.org/delivering-care/ethics/allocating-limited-health-care-resources. Accessed May 7, 2019.
- 4.US Department of Health and Human Services. Organ Procurement and Transplantation Network. Modify adult heart allocation 2016 2nd round. https://optn.transplant.hrsa.gov/governance/public-comment/modify-adult-heart-allocation-2016-2nd-round/. Originally published December 2016. Accessed June 4, 2019.
- 5.Lindblad K, Lehman RR. Organ Procurement and Transplantation Network Thoracic Committee. Four-Month Monitoring of Heart Allocation Proposal to Modify the Heart Allocation System. Submitted April 3, 2019. https://optn.transplant.hrsa.gov/media/2924/post-implementation-heart-policy-report_20190417_ready-to-post.pdf. Accessed June 20, 2019.