Abstract
Background
The signs and symptoms of Zika virus infection are usually mild and self-limited. However, the disease has been linked to neurological complications such as Guillain-Barré syndrome and peripheral nerve involvement, and also to abortion and fetal deaths due to vertical transmission, resulting in various congenital malformations in newborns, including microcephaly. This review aimed to describe the o signs and symptoms that characterize the congenital Zika syndrome.
Methods and findings
A systematic review was performed with a protocol and described according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. The search strategy yielded 2,048 studies. After the exclusion of duplicates and application of inclusion criteria, 46 studies were included. The main signs and symptoms associated with the congenital Zika syndrome were microcephaly, parenchymal or cerebellar calcifications, ventriculomegaly, central nervous system hypoplasia or atrophy, arthrogryposis, ocular findings in the posterior and anterior segments, abnormal visual function and low birthweight for gestational age.
Conclusions
Zika virus infection during pregnancy can cause a series of changes in the growth and development of children, while impacting the healthcare system due to the severity of cases. Our findings outline the disease profile in newborns and infants and may contribute to the development and updating of more specific clinical protocols.
Introduction
Zika virus (ZIKV) is a flavivirus of the family Flaviviridae, isolated initially in non-human primates in Uganda (1947), and in humans (1954) in Nigeria, Africa [1–4].
The first recorded outbreak was on the Yap Islands of Micronesia in 2007, followed by an epidemic in French Polynesia in 2013 and 2014 [5]. In Brazil, the first cases of the disease were reported in May 2015 [6].
Compared to other arboviruses such as dengue and chikungunya, ZIKV infection involves additional transmission routes. Besides transmission by Aedes mosquitoes, the risk of ZIKV spread may even be greater because the virus can also be transmitted via sexual relations, blood transfusions, and vertical transmission, and ZIKV has also been detected in urine and saliva [7–11].
The laboratory diagnosis of ZIKV infection is limited by the high cost and cross-reaction with other flaviviruses [12,13], and then protocols for clinical diagnosis, in the context of simultaneous infection by other arboviruses, need to be implemented to define cases of ZIKV infection among pregnant women who have a rash [14].
Most individuals infected with the Zika virus either do not develop symptoms or have mild and self-limited signs [15–17]. However, the disease has been linked to several neurologic manifestations in children and adults such as Guillain-Barré syndrome and peripheral nerve involvement, and ophthalmic complications such as retinal and optic nerve abnormalities. Vertical transmission has been associated with spontaneous abortion and stillbirth, and also with congenital malformations in newborns including but not limited to microcephaly [5,15,18–33].
According to the Brazilian Information System on Live Births (SINASC), the prevalence of microcephaly from 2000 to 2014, prior to ZIKV circulation, was 5.5 per 100,000 live births. However, in 2015, with the introduction of the virus and the onset of the first cases of microcephaly, the prevalence rate increased to 54.6 per 100,000 live births, i.e., an increase of 9.8 times [34].
The emergency committee of the World Health Organization (WHO) declared Zika a Public Health Emergency of International Concern in February 2016. The emergence of a disease with potentially severe impact on pregnant women and newborns triggered the search for global partnerships and the joint efforts of governments and experts to describe the infection’s pathophysiology and deal with the related clinical and social challenges [35,36].
The association between ZIKV infection and cases of microcephaly was first reported in 2015 in Brazil [28]. Detection of ZIKA infection during pregnancy has been found to be harmful to the fetus and can lead to fetal death and other abnormalities in newborns [15,19,37].
Microcephaly is only one of the possible complications found in neonates exposed to ZIKV during pregnancy and comprising the congenital Zika syndrome (CZS) [28,38–41]. There is sufficient evidence to support a causal link between ZIKV and congenital anomalies, at both the population and individual levels [38,42–49].
The systematic reviews published to date have addressed causality, transplacental transmission of ZIKV, the effect of sexual transmission, and antibody-dependent enhancement of viral teratogenicity, a different approach from that of the present review [38,42–49]. This review aimed to determine the signs and symptoms that characterize the congenital Zika syndrome and contribute to a more accurate and timely diagnosis.
Methods
Literature search
This review was performed with a protocol and described according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement [50] and is registrered in PROSPERO (CRD42020151754) in 27 October 2019. We used PICO (population, intervention, comparison, outcome) as a search strategy tool as described in S1 Table.
A systematic search was conducted in Medical Literature Analysis and Retrieval System Online (MEDLINE), Latin American and Caribbean Health Sciences Literature, Scientific Electronic Library Online, Web of Science, Excerpta Medica Database (EMBASE), Scopus databases, and Biblioteca Virtual em Saúde (BVS) to identify studies assessing signs and symptoms associated with congenital Zika virus syndrome. Additionally, manual search was performed for bibliographic references of the selected articles and grey literature databases were also included to minimize publication bias [51–55].
The search descriptors used for MEDLINE were as follows: “Zika or zikv” and “pregnan*” or “children or newborn or infant” and “congenital or congenital abnormalities” or “birth defects or malformations or microcephaly”. The search strategy was adapted according to the characteristics of each database. The complete search strategies used are presented in S3 Appendix.
There were no language restrictions in the database searches.
Selection
Article selection was performed by two authors independently (DAF and WB), and disagreements were resolved by discussion and consensus. Studies were included if they reported data describing signs and symptoms of fetal growth impairment and altered development in children exposed to Zika virus during pregnancy, among laboratory-confirmed mothers and/or children < = 2 years old. First, the titles and abstracts retrieved by the search were read and excluded as follows: editorials, letters, guidelines, and reviews. Secondly, studies potentially eligible for inclusion were read in full text and the same inclusion and exclusion criteria were applied.
Data extraction and quality assessment
Data were extracted by two authors independently (DAF and WB), and reviewed by the other (MDW). Discrepancies were resolved by discussion and consensus reached between the authors. A standardized data extraction form was made for the review. This form, available upon request, included the following sections: identification of the study (authors, journal and year of publication, language); study characteristics (design, total number of patients, period); study population (age, gestational age at infection, diagnostic method, differential diagnosis, pregnancy outcomes, birthweight, and head circumference); and analytical method. Assessment of the methodological quality of the observational studies was based on the Methodological Index for Non-Randomized Studies (MINORS) [56]. The instrument consists of 12 items, the first eight being specific for noncomparative studies. To assess the quality of case reports, we used JBI (Joanna Briggs Institute) critical appraisal checklist for case reports [57]. Each article was evaluated by two authors (MDW and DAF) independently, and disagreements were resolved by consensus.
Data synthesis and analysis
The studies were described according to country, study and sample characteristics, clinical examination, imaging tests, autopsy findings, complementary tests (laboratory, radiography, electrocardiography), and placental alterations.
Results
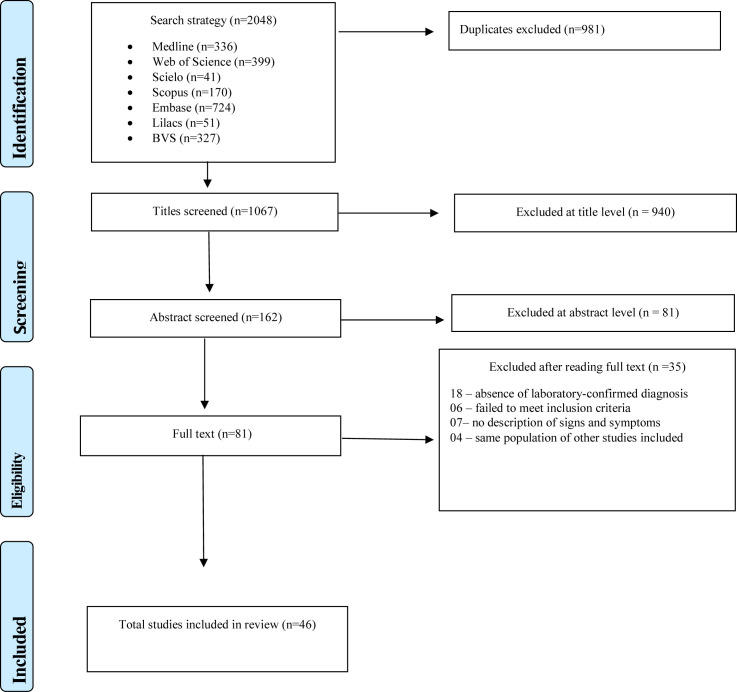
The search strategy yielded 2,048 studies. After exclusion of duplicates and application of inclusion criteria to the titles, abstracts, and full text, 81 studies were eligible for full text reading. Based on the full text reading, 46 articles were included in this review (Fig 1).
Fig 1. Flowchart of review process.
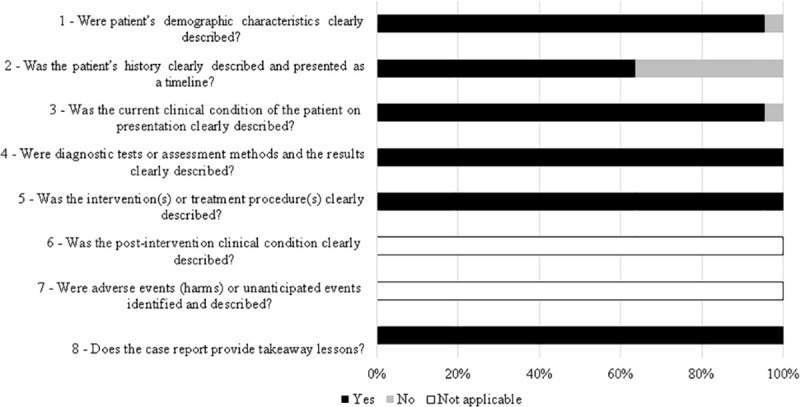
Among the articles, more than 90% presented end points appropriate to their aim and consecutive inclusion of patients according to Minors. Less than 20% of the studies reported adequately on the following criteria: “loss to follow-up less than 5%”, “prospective calculation of the study size”, “an adequate control group”, “Contemporary groups”, “baseline equivalence of groups” and “adequate statistical analyses” (Fig 2). From all case reports 36% did not describe patient´s history adequately. The other items were adequate in more than 90% of studies and two were not applicable (Fig 3).
Fig 2. Quality assessment of the studies included in the systematic review based on Methodological Index for Non-Randomized Studies (MINORS).
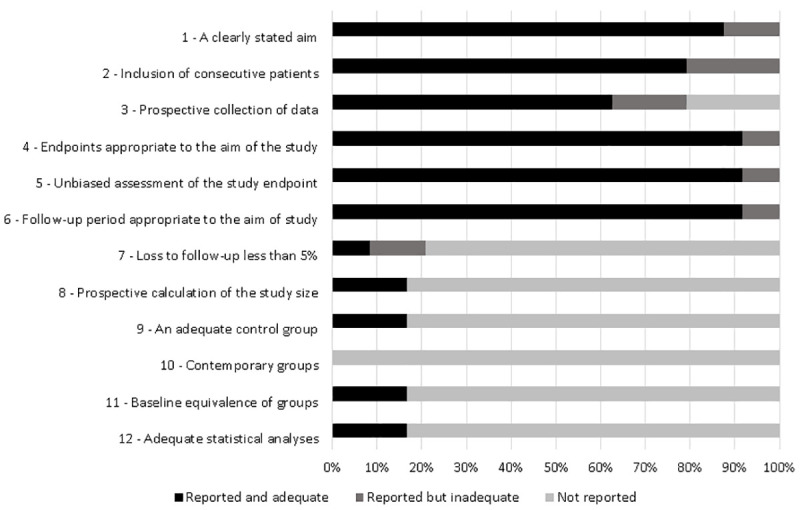
Fig 3. Quality assessment of the studies included in the systematic review based on JBI (Joanna Briggs Institute) critical appraisal checklist for case reports.
Most of the studies were performed in Brazil (59%), the epicenter of reported cases. Regarding study design, most of the studies were case reports (n = 22) or case series (n = 20), and there were two cohort studies, one case-control, and one cross-sectional study. All the studies reported at least one laboratory method for the diagnosis of women and/or children exposed to Zika virus during pregnancy. Most of the studies described signs and symptoms in children exposed to Zika virus in the first and second trimesters (Table 1).
Table 1. Characteristics of the studies included.
| Author | Country | Type of study | Sample size | Diagnostic method (ZIKV) | Torch | Mother’s age (average) | Gestational age of infection (average) | Gestational age of outcome of pregnancy (average) | Outcome of pregnancy | Weight Grams (mean) | Cephalic perimeter (Centimetermean) | Sex ratio M/F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pomar et al (2017) [58] | French Guiana | Cohort | 700 | RT-PCR*¥€, IgM*#, IgG*# | Yes | 28 | 1st trimester: 80, 2nd trimester:96, 3rd trimester:125 | - | Therapeutic abortion:2, Fetal death 9:, Live birth:125, Ongoing pregnancy: 165 | - | - | - |
| Honein et al (2017) [59] | EUA | Case series | 442 | RT-PCR*#¶, IgM*#, PRNT€¥ | No | - | - | Fetal death:5, Live birth:21 | - | - | - | |
| Brasil et al (2016) [19] | Brazil | Cohort | 207 | RT-PCR* | Yes | 31 | 1st trimester:16, 2nd trimester:27, 3rd trimester:24 | 37.9 | Miscarriage:7, Fetal death:2, Live birth:49 | - | - | - |
| de Araújo et al (2016) [23] | Brazil | Case-control | 94 | RT-PCR*#¶, IgM*#, PRNT* | Yes | 24 | 36.37 | Fetal death:1, Live birth:31, †3 | 2077 | - | 0.74 | |
| Zin et al (2017) [60] | Brazil | Case series | 112 | RT-PCR*€¥ | Yes | - | 1st trimester:14, 2nd trimester: 8, 3rd trimester:2 | - | Live birth:24 | - | - | - |
| Aragão et al (2017) [61] | Brazil | Case series | 12 | IgM# | Yes | - | 1st trimester: 6, 2nd trimester:3, Without symptoms:3 | 38.16 | Live birth:12 | - | 29.04 | 1.4 |
| Ventura et al (2017) [62] | Brazil | Cross-sectional | 32 | IgM¶ | Yes | 26 | 1st trimester:13, 2nd trimester:9, 3rd trimester 3, Without symptoms:1 | 37.9 | Live birth:32 | 2627 | 28.7 | 1.28 |
| Schaub et al (2017) [63] | Martinique | Case series | 8 | RT-PCR*¥ | Yes | 26 | 1st trimester:6, Without symptoms: 2 | 28.12 | Therapeutic abortion:7, Live birth:1 | 1218 | 22.69 | 1 |
| Carvalho et al (2016) [64] | Brazil | Case series | 19 | RT-PCR, IgM | Yes | 26 | 1st trimester:11, 2nd trimester:2, Without symptoms:6 | 38.83 | Fetal death:1, Live birth:18 | 2554,6 | - | 0.9 |
| Aragão et al (2017) [65] | Brazil | Case series | 23 | IgM*#, IgG*# | Yes | - | 1st trimester:, 2ndtrimester:, 3rd trimester, Without symptoms: | 37.43 | Live birth:23 | - | 28.91 | 1.3 |
| Hazin et al (2016) [66] | Brazil | Case series | 23 | IgM# | Yes | - | - | - | Live birth:23 | - | - | 1.3 |
| Oliveira-Szejnfeld et al (2016) [67] | Brazil | Case series | 45 | RT-PCR*ᵹ◊¥ | Yes | - | - | 39.1 | Fetal death:3, Live birth:14 | - | 28.93 | - |
| Besnard et al (2016) [68] | French Polynesian | Case series | 19 | RT-PCR¥ | Yes | - | - | - | Therapeutic abortion:11, Live birth:8 | - | - | - |
| van der Linden et al (2016) [69] | Brazil | Case series | 7 | IgM¶ | Yes | - | 1st trimester:4, Without symptoms:3 | - | Live birth:7 | - | 28.85 | - |
| Melo et al (2016) [70] | Brazil | Case series | 11 | RT-PCR¥◊, PRNT# | Yes | - | 1st trimester:9, 2nd trimester:1, Without symptoms:1 | 39.09 | Therapeutic abortion1:, Fetal death:2, Live birth:8 | - | 24.36 | - |
| Van der Linden et al (2017) [71] | Brazil | Case series | 13 | IgM#¶ | Yes | - | 1st trimester:4, 2nd trimester:2, Without symptoms:8 | 38.3 | Live birth:13 | 2971 | 32.23 | 2.25 |
| Sanín-Blair et al (2017) [72] | Colombia | Case report | 3 | RT-PCR¥ | No | 23 | 1st trimester: 3 | - | Ongoing pregnancy: 3 | - | - | - |
| Meneses et al (2017) [73] | Brazil | Case series | 87 | PRNT# | Yes | 24 | 1st trimester:47, 2ndtrimester:17, 3rd trimester:2 | 38.5 | Live birth:87†3 | 2575 | 28.1 | - |
| Fernandez et al (2017) [74] | EUA | Case report | 4 | RT-PCR#◊ | Yes | - | 25.25 | Therapeutic abortion:4 | - | - | 1 | |
| Martines et al (2016) [40] | Brazil | Case report | 5 | RT-PCR◊¶, Immunohistochemistry◊ | Yes,1 no | 26 | 1st trimester: 5 | 27.4 | Miscarriage:2, Live birth:3, †2, ‡1 | 2399 | 29.66 | 0.5 |
| Sousa et al (2017) [75] | Brazil | Case series | 7 | RT-PCR◊¶ | No | - | 1st trimester: 7 | 36 | Live birth:7† | - | - | 1.33 |
| Guillemette-Artur et al (2016) [76] | French Polynesia | Case report | 3 | RT-PCR¥, IgM# | Yes | - | 1st trimester:2 | 29.2 | Therapeutic abortion:4 | - | - | 0.5 |
| Castro et al (2017) [77] | Brazil | Case series | 8 | RT-PCR¥ | Yes | 29 | 1st trimester: 6 | 38.27 | Live birth:8 | - | 25.17 | - |
| Ventura et al (2016) [78] | Brazil | Case series | 40 | IgM¶ | Yes | 26 | 1st trimester: 13, 2nd trimester: 11, 3rd trimester:3 | Pre-term 11 Term 28 Post-term 1 |
Live birth:24 | 2674 | 29.5 | 1.1 |
| Parra-Saavedra et al (2017) [79] | Colombia | Case series | 17 | RT-PCR*€¥ | No | 24 | 1st trimester: 10, 2nd trimester:4, Without symptoms:3 | 31 | Live birth:17 | 2198 | 27.14 | 0 |
| Del Campo et al (2017) [80] | Brazil | Case series | 83 | IgM#¶ | Yes | - | - | - | Live birth:12 | - | - | - |
| Chimelli et al (2017) [81] | Brazil | Case series | 10 | RT-PCR¥*◊, Immunohistochemistry◊ | Yes | - | 1st trimester:6, 2nd trimester: 3, 3rd trimester1 | 37.5 | Fetal death:3, Live birth:7 | - | 31.3 | 1.5 |
| Schaub et al (2017) [82] | France | Case series | 14 | RT-PCR*¥¶€ | Yes | - | 1st trimester: 13, 2nd trimester:1 | 27.36 | Miscarriage:12, Fetal death:1, Live birth:1 | - | - | - |
| Mattar et al (2017) [83] | Colombia | Case report | 1 | RT-PCR€, IgM* | Yes | 33 | 2nd trimester: 1 | 39 | Live birth:1 | - | 27.5 | - |
| Culjat et al (2016) [84] | EUA | Case report | 1 | RT-PCR€, IgM*#, PRNT€ | Yes | 32 | 1st trimester: 1 | 39 | Live birth:1 | 2063 | 27.3 | 0 |
| Souza et al (2016) [85] | Brazil | Case report | 1 | RT-PCR¥, IgM*¶ | Yes | 17 | 2nd trimester: 1 | 39 | Live birth:1 | 2565 | 28 | - |
| Perez et al (2016) [86] | Spain | Case report | 1 | RT-PCR*ᵹ◊¥, IgM*, IgG*, PRNT* | Yes | 20 | 1st trimester:1 | 21 | Therapeutic abortion:1 | 295 | 17 | 0 |
| Van der Linden et al (2017) [87] | Brazil | Case report | 2 | IgM¶ | Yes | - | 1st trimester: 2 | 35.5 | Live birth:23 | 1925 | 1 | |
| Souza et al (2016) [88] | Brazil | Case report | 2 | RT-PCR*# | Yes | 27 | Without symptoms:2 | 38.5 | Live birth:23 | 2445 | 35.25 | 0 |
| Vorona et al (2016) [89] | EUA | Case report | 1 | RT-PCR*¥ | No | 50 | 1st trimester:1 | - | Therapeutic abortion:1 | - | - | - |
| Zacharias et al (2017) [90] | EUA | Case report | 1 | RT-PCR◊ᵹ€ | No | - | 36 | Live birth:1† | 1885 | 28.5 | - | |
| Werner et al (2016) [91] | Brazil | Case report | 1 | RT-PCR*#, IgM* | Yes | 31 | 1st trimester:1, 2nd trimester:, 3rd trimester, Without symptoms: | 37 | Live birth:1 | 2450 | 28 | - |
| Freitas et al (2016) [92] | Brazil | Case report | 1 | IgM# | No | - | 38 | Live birth:1† | 1892 | - | - | |
| Moron et al (2016) [93] | Brazil | Case report | 1 | IgG# | Yes | 31 | 2nd trimester: 1 | - | Live birth:1 | - | 30.5 | 0 |
| Frutos et al (2017) [94] | Argentina | Case report | 1 | RT-PCR*¥, IgM¶# | Yes | 27 | 1st trimester: 1 | - | Live birth:1 | 3390 | 31 | - |
| Acosta-Reyes et al (2017) [95] | Colombia | Case report | 2 | RT-PCR¥◊ | Yes | 19 | 1st trimester: 1, 2ndtrimester:1 | 23.5 | Therapeutic abortion:2 | - | - | - |
| Vesnaver et al (2016) [96] | Slovenia | Case report | 1 | RT-PCR#◊€, Immunohistochemistry◊ | Yes | 25 | 1st trimester: 1 | 32 | Fetal death:1 | 1470 | 26 | 1 |
| Sarno et al (2016) [97] | Brazil | Case report | 1 | RT-PCR◊, IgM* | Yes | 20 | Without symptoms:1 | 32 | Fetal death:1 | 930 | - | - |
| Driggers et al (2016) [45] | EUA | Case report | 1 | RT-PCR*#. IgM#*, IgG#* | Yes | 33 | 1st trimester: 1 | 21 | Therapeutic abortion:1 | - | - | - |
| Oliveira et al (2016) [98] | Brazil | Case report | 2 | RT-PCR¥ | No | - | - | - | Ongoing pregnancy: 2 | 1098 | 23.75 | - |
| Narero et al (2016) [99] | Panama | Case report | 1 | RT-PCR#, IgM* | Yes | 20 | - | 32 | Live birth:1† | 1020 | 23 | 1 |
Blood / serum / mother urine
*, Child blood / serum
#, Child tissues
◊Amniotic fluid
¥, Liquor
¶Placenta
€, Neonatal death
†, Post neonatal death
‡ Not reported -
Regarding study design, most of the studies were case reports (n = 22) or case series (n = 20), and there were two cohort studies, one case-control, and one cross-sectional study. All the studies reported at least one laboratory method for the diagnosis of women and/or children exposed to Zika virus during pregnancy. Most of the studies described signs and symptoms in children exposed to Zika virus in the first and second trimesters (Table 1).
Regarding clinical signs, microcephaly was described in 21 articles [19,23,40,59,60,62,63,65,69,71,73,76,78,80,84,87,90,92,93,99,100], hypertonicity in eight [19,62,63,71,80,87,93,94], seizures in seven [19,40,62,70,71,73,84], and neurological crying/irritability in the early months of life in six [19,71,80,83,87,94] (Table 2). A frequently observed clinical sign was arthrogryposis, reported in 12 articles [40,61,69,71,73,75,80,85–87,90,92]. Other osteoskeletal signs included clubfoot [85,87] and hip dysplasia [19,71]. Morphological changes of the head were described in ten articles [19,40,65,69,71,73,80,83,84,87] and overriding sutures or closed fontanels in five [70,71,80,83,84].
Table 2. Clinical signs of children exposed to ZIKV in pregnancy.
| Clinical signs | Children exposed to ZIKV | Studies N = 46 | ||||
|---|---|---|---|---|---|---|
| Minᵹ | Max£ | n (%) | ||||
| Neurological abnormalities | Microcephaly | 1 | 87 | 21 (46) | [19,23,40,59,60,62,63,65,69,71,73,76,78,80,84,87,90,92,93,99,100] | |
| Hypertonicity | 1 | 58 | 8 (17) | [19,62,63,71,80,87,93,94] | ||
| Seizures | 1 | 87 | 7 (15) | [19,40,62,70,71,73,84] | ||
| Neurological crying/irritability during first months of life | 1 | 58 | 6 (13) | [19,71,80,83,87,94] | ||
| Hyperexcitability/hyperreflexia | 1 | 58 | 5 (11) | [19,70,80,84,87] | ||
| Asymmetrical tonic neck reflex | 1 | 13 | 4 (9) | [70,71,83,87] | ||
| Clenched fists | 12 | 58 | 2 (4) | [19,80] | ||
| Distal tremors | 12 | 58 | 2 (4) | [19,80] | ||
| Centrally decreased muscle tone (upper extremities) | 1 | 58 | 2 (4) | [19,84] | ||
| Neurological impairment | 1 | 58 | 2 (4) | [19,83] | ||
| Encephalocele | 1 | 26 | 2 (4) | [59,99] | ||
| Altered visual fixation and pursuit | 2 | 13 | 2 (4) | 16–17 | ||
| Abnormal posturing | 1 (2) | [19] | ||||
| Altered motor reflexes | 1 (2) | [19] | ||||
| Hemiparesis | 1 (2) | [19] | ||||
| Hypoactivity | 1 (2) | [19] | ||||
| Hydrocephalus | 1 (2) | [86] | ||||
| Cortical blindness | 1 (2) | [84] | ||||
| Osteoskeletal abnormalities | Arthrogryposis | 1 | 87 | 12 (26) | [40,61,69,71,73,75,80,85–87,90,92] | |
| Hip dysplasia | 13 | 58 | 2 (4) | [19,71] | ||
| Clubfoot | 1 | 13 | 2 (4) | [85,87] | ||
| Knee fovea | 1 (2) | [19] | ||||
| Cortical thumb | 1 (2) | [19] | ||||
| Elbow fovea | 1 (2) | [19] | ||||
| Polydactyly | 1 (2) | [19] | ||||
| Hand contractures / Camptodactyly | 1 (2) | [80] | ||||
| Feet malposition / contractures | 1 (2) | [80] | ||||
| Prominent calcaneus | 1 (2) | [80] | ||||
| Ophthalmic abnormalities | Posterior segment abnormalities | Retinal abnormalities & | 1 | 16 | 10(22) | [60,62,69–71,73,78,84,87,92] |
| Optic nerve abnormalities# | 1 | 15 | [60,62,69,70,78,84,87,92] | |||
| Abnormal visual function | 1 | 32 | 5 (11) | [62,63,71,80,84] | ||
| Extrinsic eye motility | Strabismus | ¨ | 30 | 5 (11) | [62,70,80] ¨ | |
| Nystagmus | 6 | 9 | [60,62] | |||
| Anterior segment abnormalities | Cataract | 1 | 1 | 4 (9) | [70,98] | |
| Glaucoma | 1 | 1 | [87,92] | |||
| Refractive error | Astigmatism | 2 (4) | [62] | |||
| Myopia | [62,87] | |||||
| Hyperopia | [62] | |||||
| Abnormalities in other systems | Morphological changes of the headΦ | 1 | 87 | 10 (22) | [19,40,65,69,71,73,80,83,84,87] | |
| Small for gestational age (SGA) | 1 | 58 | 6 (13) | [19,23,69,84,85,90] | ||
| Overriding sutures or closed fontanels | 1 | 13 | 5 (11) | [70,71,80,83,84] | ||
| Hearing abnormalities | 1 | 58 | 4 (9) | [19,59,63,87] | ||
| Unilateral diaphragmatic paralysis | 3 | 87 | 3 (7) | [40,70,73] | ||
| Dystonic movement | 32 | 58 | 2 (4) | [19,62] | ||
| Dysphagia | 13 | 58 | 2 (4) | [19,71] | ||
| Bilateral cryptorchidism. | 1 | 3 | 2 (4) | [40,84] | ||
| Large for gestational age (LGA) | 1 (2) | [19] | ||||
| Head lag | 1 (2) | [19] | ||||
| Failure to gain weight | 1 (2) | [19] | ||||
| Sacral dimple | 1 (2) | [19] | ||||
| Congenital heart disease | 1 (2) | [19] | ||||
| Dyskinesia | 1 (2) | [71] | ||||
| Increased deep tendon reflexes | 1 (2) | [80] | ||||
| Multiple dimples | 1 (2) | [80] | ||||
| Ambiguous genitalia | 1 (2) | [75] | ||||
| Coronal hypospadias | 1 (2) | [84] | ||||
ᵹ: minimum number of children investigated per article.
£: maximum number of children investigated per article.
&: Pigmented, chorioretinal atrophy and/or coloboma
#: Pallor, atrophy, increased excavation, hypoplasia and/or coloboma
¨: No information on number of children
Φ verlapping cranial sutures, prominent occipital bone, excess nuchal skin, craniofacial disproportion with depression of frontal and parietal bones
The most frequent ophthalmic abnormalities occurred in the posterior segment, found in 22% of the reviewed articles which included lesions of the retina (focal pigmentary retina mottling, chorioretinal atrophy and/or coloboma) and optic nerve (pallor, atrophy, increased excavation, hypoplasia and/or coloboma) [31,60,62,69,69,70,84,87,92]. Abnormalities of visual function were described in 11% of the articles [62,69,80,82,84], as well as extrinsic ocular motility (nystagmus and strabismus) [60,62,70,80]. Abnormalities in the anterior segment (cataract and glaucoma) appeared in 9% of the articles [70,87,94] and refractive error (myopia, hyperopia and astigmatism) in 4% [62,87].
Lesions in other organ systems were also observed, to a lesser extent: cardiovascular system, [19], genitourinary system (ambiguous genitalia [75] and bilateral cryptorchidism [40,84]), and gastrointestinal system (dysphagia [19,71]) (Table 2). Other clinical features included small for gestational age (SGA) in six studies [19,23,69,84,85,90], hearing abnormalities in four [19,59,63,87], and unilateral diaphragmatic paralysis in three articles [40,70,73] (Table 2).
Three articles described the association between congenital ZIKV infection, microcephaly, and other adverse pregnancy outcomes [19,23,58]. One case-control study demonstrated the association between microcephaly and ZIKV in neonates tested by Zika virus-specific IgM and quantitative RT-PCR in serum and cerebrospinal fluid. In addition to microcephaly, this study detected congenital malformations through abnormal brain findings on imaging tests in children with virus in the serum or cerebrospinal fluid and serum only [23]. One cohort study described adverse pregnancy outcomes, including cases of fetal loss in every trimester [19]. Another cohort study identified an association between ZIKV infection and CNS (central nervous system) anomalies, cerebral hyperechogenicity, and intrauterine fetal death [58] (Table 3).
Table 3. Clinical signs and adverse pregnancy outcomes associated with Zika Virus (ZIKV) exposure in pregnancy.
| Outcomes | OR/RR | Adjusted OR | Study | Country |
|---|---|---|---|---|
| Microcephaly /ZIKV detected in serum or cerebrospinal fluid samples | 55.5 (8.6-∞) | 59.2 (9-∞)* | [23] | Brazil |
| 55,6 (8.5-∞)** | ||||
| Microcephaly /abnormal brain imaging findings | 113.3 (14.5-∞) | |||
| Microcephaly /normal brain imaging findings | 24.7 (2.9-∞) | |||
| Central Nervous System anomaly | 2.11 (1.18–4.13) | [58] | French Guiana | |
| Corpus callosum anomaly | 2.21 (1.08–5.26) | |||
| Cerebral hyperechogenicity | 3.98 (1.48–11.49) | |||
| Intrauterine fetal death | 3.98 (1.09–15.17) | |||
| Adverse pregnancy outcomes | 4.03 (1.96–8.32) | [19] | Brazil |
* maternal education
** maternal age
Imaging tests were used in 31 (67%) of the articles reviewed to detect altered signs potentially associated with Zika virus syndrome: ultrasound (80%), computed tomography (55%), magnetic resonance imaging (29%), and transfontanelar ultrasound (23%). Fourteen (45%) and 12 (39%) studies used three and two imaging methods, respectively (Table 4). The most frequent signs observed in imaging tests were located in the central nervous system: ventriculomegaly described in 35 articles [19,23,45,58,64–71,73,74,76,78–80,82–85,87,89–94,96,98,100,101]; parenchymal or cerebellar calcification (n = 33) [19,23,45,59,62–71,73,74,76,78–80,82–85,87,91,93,94,96–98,100,101]; microcephaly (n = 32) [19,40,45,58,59,63,64,66,67,70,73,74,76,79,82–87,89,91,93,94,96–101]; hypoplasia or atrophy of the cerebral cortex, cerebellum, or brainstem (n = 29) [19,45,62–67,69–71,73,74,76,79,80,82,84,85,87,89,91,93–96,98,100,101]; abnormal cortical formation (n = 27) [19,23,40,58,65–67,69–71,73,74,76,78–82,84,87,90–93,100,101]; corpus callosum anomaly (n = 18) [45,58,62,65,67–70,74,76,79,80,82,91,92,94,96,98]; and hydrocephalus (n = 3) [40,63,86] (Table 4). Cardiomegaly and diaphragmatic paralysis were detected by chest x-ray [102].
Table 4. Signs detected on imaging tests of children exposed to Zika Virus (ZIKV) in pregnancy.
| Signs | Type of test* | Children exposed to ZIKV | Studies N = 46 | |||
|---|---|---|---|---|---|---|
| Minᵹ | Max£ | n (%) | ||||
| Neurological alterations | Ventriculomegaly/ increased fluid spaces | US, TU, CT, MRI | 1 | 81 | 35 (76) | [19,23,45,58,64–71,73,74,76,78–80,82–85,87,89–94,96,98,100,101] |
| Parenchymal or cerebellar calcification | US, TU, CT, MRI | 1 | 81 | 33 (72) | [19,23,45,59,62–71,73,74,76,78–80,82–85,87,91,93,94,96–98,100,101] | |
| Microcephaly | US, TU, CT, MRI | 1 | 79 | 32 (70) | [19,40,45,58,59,63,64,66,67,70,73,74,76,79,82–87,89,91,93,94,96–101] | |
| Hypoplasia or atrophy of cerebral cortex, cerebellum, brainstem | US, TU, CT, MRI | 1 | 41 | 29 (63) | [19,45,62–67,69–71,73,74,76,79,80,82,84,85,87,89,91,93–96,98,100,101] | |
| Abnormal cortical formation (encephalomalacic changes, abnormal gyration, lissencephaly) | US, TU, CT, MRI | 1 | 81 | 27 (59) | [19,23,40,58,65–67,69–71,73,74,76,78–82,84,87,90–93,100,101] | |
| Corpus callosum anomaly | US, TU, CT, MRI | 1 | 32 | 18 (39) | [45,58,62,65,67–70,74,76,79,80,82,91,92,94,96,98] | |
| Cysts or pseudocysts | US, TU, MRI | 1 | 41 | 8 (17) | [19,63,68,76,87,88,96,101] | |
| Increased cisterna magna | US, CT, MRI | 1 | 41 | 7 (15) | [19,65,69,85,93,96,98] | |
| Fetal Dandy-Walker malformation | US, TU, CT, MRI | 1 | 30 | 3 (7) | [64,73,90] | |
| Hemorrhage | US, TU, MRI | 1 | 41 | 3 (7) | [19,45,96] | |
| Hydrocephalus | US, MRI | 1 | 8 | 3 (7) | [40,63,86] | |
| Posterior fossa anomaly | US, TU | 14 | 27 | 2 (4) | [58,82] | |
| Cerebellar abnormalities | US, MRI | 17 | 24 | 2 (4) | [78,79] | |
| Anencephaly | US | 2 | 4 | 2 (4) | [74,95] | |
| Lenticulostriate vasculopathy | TU | 2 | 2 | 2 (4) | [87,88] | |
| Supratentorial dilatation | US, TU, MRI | 1 (2) | [19] | |||
| Ischemic parenchymal lesions | US, MRI | 1 (2) | [19] | |||
| Abnormal middle cerebral artery | US | 1 (2) | [19] | |||
| Brachycephaly | US | 1 (2) | [19] | |||
| Cerebral hyperechogenicity | US, TU | 1 (2) | [58] | |||
| Abnormal pons | US | 1 (2) | [82] | |||
| Polymalformative syndrome (encephalocele, anophthalmia, arthrogryposis, fetal hydrops) | US | 1 (2) | [82] | |||
| Holoprosencephaly | US | 1 (2) | [74] | |||
| Schizencephaly | US | 1 (2) | [95] | |||
| Hydranencephaly | US | 1 (2) | [97] | |||
| Encephalocele | US | 1 (2) | [99] | |||
| Colpocephaly | TU, MRI | 1 (2) | [91] | |||
| Alterations in other systems | Polyhydramnios/oligohydramnios | US | 1 | 41 | 7 (15) | [19,58,64,70,74,90,100] |
| Intrauterine growth restriction | US, TU, CT, MRI | 1 | 41 | 7 (15) | [19,63,64,82,85,91,97] | |
| Arthrogryposis | US, TU, CT, MRI | 1 | 41 | 6 (13) | [19,40,64,70,74,86] | |
| Clubfoot | US, TU, CT, MRI | 17 | 41 | 3 (7) | [19,64,79] | |
| Premature closure of fontanelle | CT, MRI | 1 | 6 | 3 (7) | [93,65,91] | |
| Hepatomegaly/liver calcifications | US, TU, CT, MRI | 8 | 27 | 3 (7) | [58,63] | |
| Liver/spleen echogenicity | US | 27 | 41 | 2 (4) | [19,58] | |
| Intestinal hyperechogenicity | US | 4 | 27 | 2 (4) | [58,68] | |
| Small for gestational age (SGA) | US, TU | 3 | 27 | 2 (4) | [40,58] | |
| Genitourinary tract anomaly | US | 3 | 27 | 2 (4) | [40,58] | |
| Subcutaneous edema | US | 1 | 1 | 2 (4) | [96,97] | |
| Hydrothorax | US | 1 | 1 | 2 (4) | [96,97] | |
| Fetal macrosomia | US | 1 (2) | [19] | |||
| Abnormal umbilical artery flow | US | 1 (2) | [19] | |||
| Placental insufficiency | US | 1 (2) | [19] | |||
| Tachyarrhythmia | US | 1 (2) | [58] | |||
| Cardiomyopathy | US | 1 (2) | [58] | |||
| Hyperechogenicity of aortic valve, mitral valve, and aortic root | US, TU, CT, MRI | 1 (2) | [64] | |||
| Thymic calcifications | US, TU, CT, MRI | 1 (2) | [64] | |||
| Ascites | US | 1 (2) | [97] | |||
*US: pelvic or obstetric ultrasound; TU: transfontanelar ultrasound: CT: computed tomography, MRI: magnetic resonance imaging.
ᵹ: minimum number of children investigated per article.
£: maximum number of children investigated per article.
Additional lesions observed with imaging tests were: polyhydramnios or oligohydramnios [19,58,64,70,74,90,100] and intrauterine growth restriction [19,63,64,82,85,91,97], described in seven articles. As the clinical examination indicated, osteoskeletal lesions were also frequent: arthrogryposis (n = 6) [19,40,64,70,74,86] and clubfoot [19,64,79] (n = 3). Other organ systems were involved, although less frequently: gastrointestinal (intestinal hyperechogenicity (n = 2) [58,68], liver calcifications and hepatomegaly (n = 2) [19,58], cardiovascular (tachyarrhythmia and cardiomyopathy (n = 1) [58], respiratory (hydrothorax (n = 1), and genitourinary (genitourinary tract anomaly (n = 2) [40,58] (Table 4).
The following other lesions were observed on imaging tests in one study [19] and can help elucidate the natural history of Zika virus infection: abnormal middle cerebral artery, abnormal umbilical artery flow, and placental insufficiency (Table 4).
Eight studies [40,58,68,81,84,90,93,103] reported the placenta’s characteristics, especially in cases of fetal death. There were calcifications in five articles [40,68,81,93,103], and vascular alterations such as villous infarction [40,81,93] and scattered intervillous thrombi [84,93].
Seven articles reported data on miscarriage and autopsy in neonatal and fetal death: microcephaly (n = 6) [40,45,75,81,90,97], calcifications (n = 4) [40,75,81,90], CNS hypoplasia (n = 4) [40,45,75,81], ventriculomegaly (n = 3) [40,75,81], arthrogryposis (n = 5) [40,75,81,90,97], and pulmonary hypoplasia (n = 2) [40,75,90] (Table 5).
Table 5. Autopsy findings of children exposed to Zika Virus (ZIKV) in pregnancy.
| Autopsy findings | Children exposed to ZIKV | Studies N = 46 | |||
|---|---|---|---|---|---|
| Minᵹ | Max£ | n (%) | |||
| Neurological findings | Microcephaly | 1 | 10 | 6 (13) | [40,45,75,81,90,97] |
| Calcifications | 1 | 10 | 4 (9) | [40,75,81,90] | |
| CNS hypoplasia | 1 | 10 | 4 (9) | [40,45,75,81] | |
| Ventriculomegaly | 3 | 10 | 3 (7) | [40,75,81] | |
| Inflammatory infiltrate in leptomeninges and brain | 1 | 7 | 3 (7) | [40,45,75] | |
| Vascular congestion in leptomeninges or brain | 3 | 7 | 2 (4) | [40,75] | |
| Anterior spinal horn cell loss | 1 (2) | [81] | |||
| Pachygyria | 1 (2) | [75] | |||
| Cerebral gliosis | 1 (2) | [75] | |||
| Lissencephaly | 1 (2) | [40] | |||
| Holoprosencephaly | 1 (2) | [40] | |||
| Cerebral necrosis | 1 (2) | [40] | |||
| Hydrocephalus | 1 (2) | [40] | |||
| Malformation of cortical development with agyria | 1 (2) | [90] | |||
| Dandy-Walker syndrome | 1 (2) | [90] | |||
| Findings in other systems | Arthrogryposis | 1 | 10 | 5 (11) | [40,75,81,90,97] |
| Pulmonary hypoplasia | 1 | 3 | 3 (7) | [40,75,90] | |
| Pulmonary hemorrhage | 3 | 7 | 2 (4) | [40,75] | |
| Virus detected in fetal tissues | 3 | 7 | 2 (4) | [40,63] | |
| Hydropic degeneration of liver | 1 | 7 | 2 (4) | [75,90] | |
| Neurogenic muscle atrophy | 1 (2) | [40] | |||
| Inflammatory infiltrate in lung | 1 (2) | [75] | |||
| Liver apoptosis | 1 (2) | [75] | |||
| Liver steatosis | 1 (2) | [75] | |||
| Intrauterine growth restriction | 1 (2) | [75] | |||
| Ventricular septal defect | 1 (2) | [90] | |||
ᵹ: minimum number of children investigated per article.
£: maximum number of children investigated per article.
Neurological signs and symptoms were the ones most frequently described in both the imaging tests (Table 4) and autopsies (Table 5).
Discussion
In our review, the main signs and symptoms associated with congenital Zika virus syndrome were microcephaly, parenchymal or cerebellar calcifications, ventriculomegaly, CNS hypoplasia or atrophy; arthrogryposis; ophthalmic findings mainly focal pigmentary retina mottling, chorioretinal atrophy and/or coloboma, pallor, atrophy, increased excavation, hypoplasia and/or coloboma of optic nerve and abnormal visual function and low birthweight for gestational age.
Microcephaly was the most frequent sign found in neonates exposed to ZIKV during pregnancy among the articles in our review [28,38–41]. Forty one studies reported microcephaly [19,23,40,45,58–60,62–67,69,70,70,71,73–76,79–87,89–94,96–101]. Other studies, using different methodologies, have reported similar results [104–106], including increased prevalence of microcephaly among children exposed to ZIKV in other systematic review [47] when compared to the prevalence in other studies of unexposed children in Brazil and Europe [107,108].
Parenchymal or cerebellar calcification were described in 37 studies of our review [19,23,40,45,59,62–71,73–76,78–85,87,90,91,93,94,96–98,100,101] and also in other review which reported a prevalence of 42.6% [47]. These findings may also be found in congenital infections known by the mnemonic TORCH (Toxoplasmosis, Rubella, Cytomegalovirus (CMV) and Herpes. However, the distribution of intracranial calcifications differs in each congenital infection: typically larger, denser and subcortical in congenital ZIKV, punctate and periventricular or cortical in CMV, diffuse and widely distributed in congenital toxoplasmosis and at basal ganglia in rubella [41,109–111]. Besides that it should be noted that some neurological changes (calcifications and cerebral atrophy) in congenital Zika syndrome are similar to other syndromes of infectious and also genetic etiology, such as Aicardi-Goutières syndrome [112].
Ventriculomegaly was described in 32 studies reviewed [19,23,45,56,56,58,63–74,76,78–80,82–84,87–94,96,98,100], an important sign regarding the risk of developing hydrocephalus and the need for surgical intervention for ventriculoperitoneal shunt, which was also observed in other studies [47,113]. In our study, hydrocephalus was associated with severe signs and symptoms, such as: epilepsy, motor dysfunction, cognitive dysfunction, arthrogryposis (one-third of cases), and visual and hearing disorders [40,66,82,86,95,101], in agreement with Linden (2019) [113], who identified severe neurological disorders and cognitive dysfunction in one-third of children who progressed with hydrocephalus.
Congenital infections such as those involving Toxoplasma gondii and cytomegalovirus have also been associated with serious brain alterations such as calcifications and ventriculomegaly [114,115]. However, unlike these other infections, ZIKV infection is known to be associated with severe microcephaly, with partially collapsed skull, thin cerebral cortex with subcortical calcifications, macular scars, and retinal changes as a result of the important viral tropism for fetal neural and ocular progenitor cells [116]. In addition, congenital contractures (bone deformities) are also associated with ZIKV infection during pregnancy, although observed less frequently [117]. In short, these findings can also occur in similar congenital syndromes associated with other infectious diseases, such as toxoplasmosis, syphilis, varicella, parvovirus B1, rubella, cytomegalovirus, and herpes simplex [23,42,58,118] but the signs and symptoms presented by CZS seem to be more serious.
The osteoskeletal system was the second most frequently altered organ system in newborns exposed in uterus to ZIKV and arthrogryposis was described in 18 studies reviewed [19,40,61,64,69–71,73–75,80,81,85–87,90,92,97], as observed by other studies, mainly in more severe cases [15,47,79,113].
Anatomical [60,62,69–71,73,78,84,87,92] and functional [62,63,71,80,84] changes of the eye were described in 12 articles, such as posterior and anterior segment abnormalities, extrinsic eye motility and abnormal visual function. Many of these anatomical changes may impact the child’s visual function in the future, since they affect prime areas of the eye. Importantly, since the child’s first contact with the environment is through eyesight, children with visual impairment commonly experience delayed neuropsychomotor development, which, alongside the syndrome’s other signs and symptoms, hinder the child’s ability to integrate with his or her surroundings [119]. These ocular findings were described also in other studies descripted [47,120–122].
TORCH infections have also been associated with serious ophthalmic alterations. In congenital toxoplasmosis infection, chorioretinal lesions are usually bilateral and can present with active lesions or regressed scar [60,123]. Congenital cytomegalovirus and herpes virus infections can also manifest with active ocular inflammation. In Zika virus infection, however, there has been no active ocular inflammation cases reported so far [123]. There is usually not pigmentary mottling seen outside of areas of chorioretinal atrophy in congenital toxoplasmosis infection, as seen in zika virus infection [60]. In congenital rubella infection, the pigment mottling is usually diffused compared with the focal pigment mottling seen in zika virus infection [60]. Congenital cytomegalovirus can present with chorioretinal lesions similar to congenital toxoplasmosis but less heavily pigmentated and with pale or small optic disc [124,125]. Optic nerve hypoplasia, commonly seen in ZIKV congenital infection, is rarely seen in rubella, toxoplasmosis and herpes congenital infections [60].
The pathophysiology of ZIKV infection and the mechanism of the virus’ passage across the placental barrier are still under investigation [48]. The exact timing of placental and fetal infection in relation to maternal viremia is also still unclear, as is the correlation between prolonged viremia and the development of congenital Zika syndrome [48]. Placental alterations were reported in eight studies [40,58,68,81,84,90,93,103], but the role of placental viral infection in determining the syndrome’s severity has not been determined to date, as stated by other authors who found mild and nonspecific pathological findings in the placenta in pregnancies with ZIKV infection [126–129].
The effects of ZIKV on the fetus are more frequent and severe when maternal infection occurs in the first and second trimesters of pregnancy, resulting in: spontaneous abortion; therapeutic abortion due to major congenital malformation; various congenital malformations; fetal death; and neonatal and post-neonatal deaths [19,42,59,60], as corroborated by other studies [107,130–133]. Notably, the total number of abortions in Brazil, the epicenter of ZIKV cases, may be underestimated, since therapeutic abortion is prohibited by law, even though a recent study did not find an increase in hospitalizations due to complications of abortion during the epidemic [77]. In addition to adverse pregnancy outcomes and deaths, our review presents evidence that early maternal infection during pregnancy is associated with higher likelihood of congenital abnormalities such as microcephaly, ophthalmic lesions, osteoskeletal malformations, and various brain alterations [58,88] as described in other studies [19,129,130,133–141].
Among the imaging tests performed, obstetric ultrasound was the most frequent, in addition to transfontanelar ultrasound (TU), computed tomography (CT), and magnetic resonance imaging (MRI) of the newborn (Table 4). Transfontanelar ultrasound, CT, and MRI were reported less frequently, possibly due to the limited access to those exams in some settings. Obstetric ultrasound proved to be useful for tracking ZIKV-related brain injury in prenatal care in pregnant women exposed to ZIKV. Although less accurate than CT and MRI it is available in many health facilities [142,143].
One point to highlight in our review is the anatomopathological analysis. It was possible to notice either the severity of the systemic impairment of the cases that died, especially those whose maternal infection occurred in the first trimester of pregnancy and the correspondence of clinical and anatomopathological findings.
Low birthweight and intrauterine growth restriction were common findings in the studies in the current review [19,63,64,69,82,85,89–91], representing a risk for children exposed to ZIKV during pregnancy. A recent study found that prevalence of Low birthweight in infants with CZS was more than four times that of the overall sample of live births [144].
Gastrointestinal disorders were reported [19,58,64,75,90], including liver disorders [58,68], intestinal alterations, and dysphagia [68,71]. Dysphagia can increase the risk of bronchoaspiration, resulting in aspiration pneumonia or death from asphyxiation, requiring gastrostomy in the affected infants [113,145]. Structural changes in the genitourinary system were reported [40,58,75,84] and were also described by Villamil-Gómez (2019) in fetal autopsies [146]. Bladder impairment and possible kidney damage such as very low bladder capacity, bladder hyperactivity with increased consistency, high bladder pressure during the filling phase, and high postvoid residual volume (PVR) and/or recurrent urinary tract infection were reported in older children [147]. Congenital cardiovascular anomalies were identified in children exposed to ZIKV such as cardiomyopathy, hyperechogenicity of aortic valve, mitral valve, and aortic root [19,58,64,100]. Other studies have also described cardiological symptoms and imaging findings such as complex congenital heart disease, echocardiographic abnormalities, and cardiac overload [148–151].
Pulmonary alterations were less common, mostly detected by autopsy and thus tending to be more severe [40,75,90]. Other abnormalities such as hydrothorax [96,97] and diaphragmatic paralysis [40,73,98] were reported. A recent study investigating the cause of diaphragmatic paralysis in three infants with CZS reported phrenic nerve dysfunction detected by electromyography [113]. Hearing abnormalities were reported in some studies [19,59,63,87], highlighting the need for specific tests for early detection, since they can further impair the child’s interaction with the environment and affect neurodevelopment, as described by Leal et al. (2016) [152].
Congenital Zika syndrome and all its effects on children according to age group still need to be evaluated in light of new findings. Our review supported the characterization of the syndrome in infants up to six months of age since the initial reporting of cases. Recent studies have identified neurological disorders such as delay in neurodevelopment, mainly in the domain of language in children exposed to ZIKV who were asymptomatic at birth [133,153]. Such findings are relevant, since there is evidence that ZIKV can continue to replicate in the infant’s brain after birth [154], and that cerebral growth of infants exposed during pregnancy can decelerate, even after birth [69].
Cohort studies are needed to characterize the syndrome’s signs and symptoms according to age group in order to assess the impact on children’s cognitive development. Recent studies indicate that neurological changes can negatively impact the children’s motor and cognitive levels, with serious consequences for the social life of the patients and their families. Most of these children display severe motor dysfunction [155,156], delayed functional performance [132], difficulties in eating and sleeping, visual and auditory abnormalities, seizures [156], swallowing dysfunction, movement abnormalities, and epilepsy [153]. Complications associated with respiratory infections, dysphagia, and epilepsy can be fatal for the most severely affected infants [97,64,135].
Congenital Zika syndrome is a serious public health problem, both because of the clinical severity of the cases and the extent of functional impairment. Absence of signs and symptoms at birth in exposed infants does not rule out their appearance later in childhood, thus highlighting the importance of structuring healthcare networks for comprehensive monitoring and care of these children. The high prevalence of asymptomatic cases at birth (65 to 83%) [5,157] can delay the identification of the association between congenital syndromes (with or without late onset) and ZIKV infection in the mother during pregnancy. Efforts are needed to provide care and support for all the needs of children with congenital Zika syndrome and their families, as well as effective organization of healthcare and social services.
The ZIKV reemergence in regions with autochthonous transmission and the introduction of the virus in areas with established vector mosquito infestation may increase the risk of the development of congenital Zika syndrome in all regions of the world, especially in Africa, the Americas, Southeast Asia and the Western Pacific [158].
In the absence of effective vaccines, licensed to date [161,162], and considering the complexity of effective vector control, innovative intersectoral strategies that transcend exclusive vector chemical control actions should be incorporated in areas with viral circulation [159–164]. Prevention strategies such as the use of repellents by pregnant women and condoms by sexual partners, both for travelers to regions with ZIKV circulation, and for residents of risk areas, as well as the implementation of strict screening protocols in the donation system of blood should be implemented. In addition, pregnant women and those intending to become pregnant may be advised to avoid unnecessary travel to endemic regions [165].
One limitation to the study was the low number of comparative clinical studies. The inclusion of case series and case reports, with lower levels of scientific evidence, is justified for the investigation of new and rare diseases such as congenital Zika syndrome, since evidence based on clinical case reports is necessary to understand the natural history of a new illness [166]. We chose to include only studies with laboratory confirmation of cases, seeking accurate estimates of maternal-fetal transmission and risk of symptomatic congenital infection. This criterion excluded other studies published during the period analyzed.
Conclusion
The review of clinical, imaging, and anatomopathological findings allowed the characterization of congenital Zika syndrome, especially in children born to mothers with laboratory-confirmed ZIKV infection during pregnancy.
Our results show that the congenital Zika syndrome encompasses several malformations mainly in the neurological, osteoskeletal, and visual systems, although the syndrome can affect other organ systems. ZIKV infection is also associated with several adverse pregnancy outcomes, including fetal loss.
We highlight the following findings: (a) in the neurological system: ventriculomegaly, parenchymal or cerebellar calcification, microcephaly, hypoplasia or atrophy of the cerebral cortex, cerebellum, and brainstem, abnormal cortical formation, corpus callosum anomaly, hydrocephalus, hypertonicity, and seizures; (b) in the osteoskeletal system: arthrogryposis and clubfoot; and (c) in the visual system: ophthalmic changes in the posterior and anterior segments and abnormal visual function.
Congenital Zika syndrome also impacts the health system and the families’ daily lives, requiring collaboration between levels of healthcare and inter-sector cooperation aimed at comprehensive care for these children. The current review’s findings are thus essential for understanding the disease profile in patients and to assist the development and updating of more specific clinical protocols.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
We are grateful for support from the Coordination for the Improvement of Higher Education Personnel (CAPES).
Abbreviations
- ZIKV
Zika virus
- CNS
central nervous system
- SINASC
System on Live Births
- WHO
World Health Organization
- PICO
population, intervention, comparison, outcome
- MINORS
Methodological Index for Non-Randomized Studies
- JBI
Joanna Briggs Institute) critical appraisal checklist for case reports
- TORCH
Toxoplasmosis, Rubella, Cytomegalovirus and Herpes
- CMV
Cytomegalovirus
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Dick GWA, Kitchen SF, Haddow AJ. Zika Virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952. September 1;46(5):509–20. 10.1016/0035-9203(52)90042-4 [DOI] [PubMed] [Google Scholar]
- 2.MacNamara FN. Zika virus: A report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans R Soc Trop Med Hyg. 1954. March 1;48(2):139–45. 10.1016/0035-9203(54)90006-1 [DOI] [PubMed] [Google Scholar]
- 3.Marchette NJ, Garcia R, Rudnick A. Isolation of Zika Virus from Aedes Aegypti Mosquitoes in Malaysia. Am J Trop Med Hyg. 1969. May 1;18(3):411–5. 10.4269/ajtmh.1969.18.411 [DOI] [PubMed] [Google Scholar]
- 4.Smithburn KC, Haddow AJ. Ntaya Virus. A Hitherto Unknown Agent Isolated from Mosquitoes Collected in Uganda. Proc Soc Exp Biol Med. 1951. May 1;77(1):130–3. 10.3181/00379727-77-18700 [DOI] [PubMed] [Google Scholar]
- 5.Duffy MR, Chen T-H, Hancock WT, Powers AM, Kool JL, Lanciotti RS, et al. Zika Virus Outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009. June 11;360(24):2536–43. 10.1056/NEJMoa0805715 [DOI] [PubMed] [Google Scholar]
- 6.Hennessey M, Fischer M, Staples JE. Zika Virus Spreads to New Areas—Region of the Americas, May 2015–January 2016. Am J Transplant. 2016. March 1;16(3):1031–4. 10.15585/mmwr.mm6503e1 [DOI] [PubMed] [Google Scholar]
- 7.Al BDF et. Probable Non–Vector-borne Transmission of Zika Virus, Colorado, USA—Volume 17, Number 5—May 2011—Emerging Infectious Disease journal—CDC. [cited 2017 Oct 23]; Available from: https://wwwnc.cdc.gov/eid/article/17/5/10-1939_article [DOI] [PMC free article] [PubMed]
- 8.Gourinat A-C, O’Connor O, Calvez E, Goarant C, Dupont-Rouzeyrol M. Detection of Zika Virus in Urine. Emerg Infect Dis. 2015. January;21(1):84–6. 10.3201/eid2101.140894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Musso D, Roche C, Robin E, Nhan T, Teissier A, Cao-Lormeau V-M. Potential Sexual Transmission of Zika Virus. Emerg Infect Dis. 2015. February;21(2):359–61. 10.3201/eid2102.141363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Musso D, Gubler DJ. Zika Virus. Clin Microbiol Rev. 2016. July;29(3):487–524. 10.1128/CMR.00072-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishiura H, Kinoshita R, Mizumoto K, Yasuda Y, Nah K. Transmission potential of Zika virus infection in the South Pacific. Int J Infect Dis. 2016. April;45:95–7. 10.1016/j.ijid.2016.02.017 [DOI] [PubMed] [Google Scholar]
- 12.Johnson AJ, Martin DA, Karabatsos N, Roehrig JT. Detection of Anti-Arboviral Immunoglobulin G by Using a Monoclonal Antibody-Based Capture Enzyme-Linked Immunosorbent Assay. J Clin Microbiol. 2000. May;38(5):1827–31. 10.1128/JCM.38.5.1827-1831.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodriguez-Morales AJ, Villamil-Gómez WE, Franco-Paredes C. The arboviral burden of disease caused by co-circulation and co-infection of dengue, chikungunya and Zika in the Americas. Travel Med Infect Dis. 2016. June;14(3):177–9. 10.1016/j.tmaid.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 14.Ximenes RA de A, Miranda-Filho D de B, Brickley EB, Montarroyos UR, Martelli CMT, de Araújo TVB, et al. Zika virus infection in pregnancy: Establishing a case definition for clinical research on pregnant women with rash in an active transmission setting. PLoS Negl Trop Dis [Internet]. 2019. October 7 [cited 2020 Oct 14];13(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6797234/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brasil P, Calvet GA, Siqueira AM, Wakimoto M, de Sequeira PC, Nobre A, et al. Zika Virus Outbreak in Rio de Janeiro, Brazil: Clinical Characterization, Epidemiological and Virological Aspects. PLoS Negl Trop Dis. 2016. April;10(4):e0004636 10.1371/journal.pntd.0004636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faluyi U, Obadare O, Sangem A, Onuegbu CA, Medavarapu S. Complications Associated with Zika Virus Infection: A Systematic Review Study. Am Sci Res J Eng Technol Sci ASRJETS. 2016. August 28;24(1):151–61. [Google Scholar]
- 17.WHO. Zika virus [Internet]. World Health Organization. 2019 [cited 2019 Oct 1]. Available from: https://www.who.int/news-room/fact-sheets/detail/zika-virus
- 18.Braga JU, Bressan C, Dalvi APR, Calvet GA, Daumas RP, Rodrigues N, et al. Accuracy of Zika virus disease case definition during simultaneous Dengue and Chikungunya epidemics. PLOS ONE. 2017. June 26;12(6):e0179725 10.1371/journal.pone.0179725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brasil P, Pereira JP Jr, Moreira ME, Ribeiro Nogueira RM, Damasceno L, Wakimoto M, et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N Engl J Med. 2016. December 15;375(24):2321–34. 10.1056/NEJMoa1602412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brito C. Zika Virus: A New Chapter in the History of Medicine. Acta Médica Port. 2016. December 31;28(6):679–80. [DOI] [PubMed] [Google Scholar]
- 21.Cardoso CW, Paploski IAD, Kikuti M, Rodrigues MS, Silva MMO, Campos GS, et al. Outbreak of Exanthematous Illness Associated with Zika, Chikungunya, and Dengue Viruses, Salvador, Brazil. Emerg Infect Dis. 2015. December;21(12):2274–6. 10.3201/eid2112.151167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Microcephaly Epidemic Research Group. Microcephaly in Infants, Pernambuco State, Brazil, 2015. Emerg Infect Dis. 2016. June;22 (6):1090–3. 10.3201/eid2206.160062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Araujo TVB, Rodrigues LC, de Alencar Ximenes RA, de Barros Miranda-Filho D, Montarroyos UR, de Melo APL, et al. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: preliminary report of a case-control study. Lancet Infect Dis. 2016. December;16(12):1356–63. 10.1016/S1473-3099(16)30318-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Souza WV, Barreto de Araujo TV, Militao Albuquerque M de FP, Braga MC, de Alencar Ximenes RA, Miranda-Filho D de B, et al. Microcephaly in Pernambuco State, Brazil: epidemiological characteristics and evaluation of the diagnostic accuracy of cutoff points for reporting suspected cases. Cad Saude Publica. 2016. January;32(4):e00017216 10.1590/0102-311X00017216 [DOI] [PubMed] [Google Scholar]
- 25.Freitas B de P, Dias JR de O, Prazeres J, Sacramento GA, Ko AI, Maia M, et al. Ocular Findings in Infants With Microcephaly Associated With Presumed Zika Virus Congenital Infection in Salvador, Brazil. JAMA Ophthalmol. 2016. May 1;134(5):529–35. 10.1001/jamaophthalmol.2016.0267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Musso D, Nilles EJ, Cao-Lormeau V-M. Rapid spread of emerging Zika virus in the Pacific area. Clin Microbiol Infect. 2014. October 1;20(10):O595–6. 10.1111/1469-0691.12707 [DOI] [PubMed] [Google Scholar]
- 27.Oehler E, Watrin L, Larre P, Leparc-Goffart I, Lastere S, Valour F, et al. Zika virus infection complicated by Guillain-Barre syndrome—case report, French Polynesia, December 2013. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2014. March 6;19(9). 10.2807/1560-7917.es2014.19.9.20720 [DOI] [PubMed] [Google Scholar]
- 28.Oliveira WK de. Increase in Reported Prevalence of Microcephaly in Infants Born to Women Living in Areas with Confirmed Zika Virus Transmission During the First Trimester of Pregnancy—Brazil, 2015. MMWR Morb Mortal Wkly Rep [Internet]. 2016. [cited 2017 Oct 23];65 Available from: https://www.cdc.gov/mmwr/volumes/65/wr/mm6509e2.htm 10.15585/mmwr.mm6509e2 [DOI] [PubMed] [Google Scholar]
- 29.PAHO/WHO. Epidemiological Alert Neurological syndrome, congenital malformations, and Zika virus infection. Implications for public health in the Americas. [Internet]. 2015. Available from: http://www.paho.org/hq/index.php?option=com_docman&task=doc_download&Itemid=&gid=32405&lang=en. [Google Scholar]
- 30.Ventura C., Maia M., Martins T., Patriota F., Agra C., Ventura L., et al. Variables related to the ophthalmoscopic findings identified in infants with presumed zika virus congenital infection. Ophthalmologica. 2016;236:33 10.1016/j.ijfoodmicro.2016.07.012 [DOI] [PubMed] [Google Scholar]
- 31.Ventura CV, Maia M, Ventura BV, Linden VVD, Araujo EB, Ramos RC, et al. Ophthalmological findings in infants with microcephaly and presumable intra-uterus Zika virus infection. Arq Bras Oftalmol. 2016. February;79(1):1–3. 10.5935/0004-2749.20160002 [DOI] [PubMed] [Google Scholar]
- 32.Lannuzel A, Fergé J-L, Lobjois Q, Signate A, Rozé B, Tressières B, et al. Long-term outcome in neuroZika: When biological diagnosis matters. Neurology. 2019. 21;92(21):e2406–20. 10.1212/WNL.0000000000007536 [DOI] [PubMed] [Google Scholar]
- 33.da Silva IRF, Frontera JA, Bispo de Filippis AM, Nascimento OJM do, RIO-GBS-ZIKV Research Group. Neurologic Complications Associated With the Zika Virus in Brazilian Adults. JAMA Neurol. 2017. 01;74(10):1190–8. 10.1001/jamaneurol.2017.1703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Marinho F, Araújo VEM de, Porto DL, Ferreira HL, Coelho MRS, Lecca RCR, et al. Microcefalia no Brasil: prevalência e caracterização dos casos a partir do Sistema de Informações sobre Nascidos Vivos (Sinasc), 2000–2015. Epidemiol Serv Saúde. 2016. December;25(4):701–12. 10.5123/S1679-49742016000400004 [DOI] [PubMed] [Google Scholar]
- 35.Bastos LFCS. OPAS/OMS Brasil—OMS declara fim de Emergência de Saúde Pública Internacional, mas diz que resposta ao zika e suas consequências deve continuar | OPAS/OMS [Internet]. Pan American Health Organization / World Health Organization; 2016. [cited 2017 Oct 23]. Available from: http://www.paho.org/bra/index.php?option=com_content&view=article&id=5297:oms-declara-fim-de-emergencia-de-saude-publica-internacional-mas-diz-que-resposta-ao-zika-e-suas-consequencias-deve-continuar&Itemid=812 [Google Scholar]
- 36.WHO. La Directora General de la OMS resume el resultado del Comité de Emergencia sobre el virus de Zika [Internet]. WHO; 2016. [cited 2017 Oct 23]. Available from: http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/es/ [Google Scholar]
- 37.Microcephaly Epidemic Research Group. Microcephaly in Infants, Pernambuco State, Brazil, 2015—Volume 22, Number 6—June 2016—Emerging Infectious Disease journal—CDC. 2016 [cited 2017 Oct 22]; Available from: https://wwwnc.cdc.gov/eid/article/22/6/16-0062_article [DOI] [PMC free article] [PubMed]
- 38.Abbasi A-N. Zika virus infection; vertical transmission and fetal congenital anomalies. J Ayub Med Coll Abbottabad JAMC. 2016. March;28(1):1–2. [PubMed] [Google Scholar]
- 39.De Barros Miranda-Filho D, Martelli CMT, De Alencar Ximenes RA, Araújo TVB, Rocha MAW, Ramos RCF, et al. Initial description of the presumed congenital Zika syndrome. Am J Public Health. 2016;106(4):598–600. 10.2105/AJPH.2016.303115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martines RB, Bhatnagar J, de Oliveira Ramos AM, Davi HPF, Iglezias SD, Kanamura CT, et al. Pathology of congenital Zika syndrome in Brazil: a case series. Lancet Lond Engl. 2016. August 27;388(10047):898–904. 10.1016/S0140-6736(16)30883-2 [DOI] [PubMed] [Google Scholar]
- 41.Russell K. Update: Interim Guidance for the Evaluation and Management of Infants with Possible Congenital Zika Virus Infection—United States, August 2016. MMWR Morb Mortal Wkly Rep [Internet]. 2016. [cited 2017 Dec 3];65 Available from: https://www.cdc.gov/mmwr/volumes/65/wr/mm6533e2.htm 10.15585/mmwr.mm6533e2 [DOI] [PubMed] [Google Scholar]
- 42.Krauer F, Riesen M, Reveiz L, Oladapo OT, Martínez-Vega R, Porgo TV, et al. Zika Virus Infection as a Cause of Congenital Brain Abnormalities and Guillain–Barré Syndrome: Systematic Review. PLoS Med [Internet]. 2017. January 3;14(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207634/ 10.1371/journal.pmed.1002203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coelho AVC, Crovella S. Microcephaly Prevalence in Infants Born to Zika Virus-Infected Women: A Systematic Review and Meta-Analysis. Int J Mol Sci. 2017. August 5;18(8). 10.3390/ijms18081714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Counotte MJ, Egli-Gany D, Riesen M, Abraha M, Porgo TV, Wang J, et al. Zika virus infection as a cause of congenital brain abnormalities and Guillain-Barre syndrome: From systematic review to living systematic review. F1000Research. 2018;7:196 10.12688/f1000research.13704.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Driggers RW, Ho C-Y, Korhonen EM, Kuivanen S, Jaaskelainen AJ, Smura T, et al. Zika Virus Infection with Prolonged Maternal Viremia and Fetal Brain Abnormalities. N Engl J Med. 2016. June 2;374(22):2142–51. 10.1056/NEJMoa1601824 [DOI] [PubMed] [Google Scholar]
- 46.Duarte G, Moron AF, Timerman A, Fernandes CE, Mariani Neto C, de Almeida Filho GL, et al. Zika Virus Infection in Pregnant Women and Microcephaly. Rev Bras Ginecol E Obstet. 2017. May;39(5):235–48. 10.1055/s-0037-1603450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nithiyanantham SF, Badawi A. Maternal infection with Zika virus and prevalence of congenital disorders in infants: systematic review and meta-analysis. Can J Public Health Rev Can Sante Publique. 2019. May 10; 10.17269/s41997-019-00215-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robinson N, Mayorquin Galvan EE, Zavala Trujillo IG, Zavala-Cerna MG. Congenital Zika syndrome: Pitfalls in the placental barrier. Rev Med Virol. 2018. September;28(5):e1985 10.1002/rmv.1985 [DOI] [PubMed] [Google Scholar]
- 49.Wilder-Smith A, Chang CR, Leong WY. Zika in travellers 1947–2017: a systematic review. J Travel Med. 2018. July 1;25(1). 10.1093/jtm/tay044 [DOI] [PubMed] [Google Scholar]
- 50.Galvão TF, Pansani T de SA, Harrad D. Principais itens para relatar Revisões sistemáticas e Meta-análises: A recomendação PRISMA. Epidemiol E Serviços Saúde. 2015. June;24(2):335–42. [Google Scholar]
- 51.OpenGrey [Internet]. [cited 2019 Sep 27]. Available from: http://www.opengrey.eu/
- 52.Egger M, Smith GD, Douglas GA, editors. Systematic reviews in health care: meta-analysis in context. 2. ed, [Nachdr.]. London: BMJ Books; 2009. 487 p. (Medical research). [Google Scholar]
- 53.Higgins J, Thomas J, Cumpdton M, Li T, Page M, Welch V. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane, 2019. Available from. [Internet]. Version 6.0 (updated July 2019). 2019. Available from: www.training.cochrane.org/handbook [Google Scholar]
- 54.Paez A. Gray literature: An important resource in systematic reviews. J Evid-Based Med. 2017;10(3):233–40. 10.1111/jebm.12266 [DOI] [PubMed] [Google Scholar]
- 55.Balshem H, Stevens A, Ansari M, Norris S, Kansagara D, Shamliyan T, et al. Finding Grey Literature Evidence and Assessing for Outcome and Analysis Reporting Biases When Comparing Medical Interventions: AHRQ and the Effective Health Care Program In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. [cited 2020 Sep 19]. (AHRQ Methods for Effective Health Care). Available from: http://www.ncbi.nlm.nih.gov/books/NBK174882/ [PubMed] [Google Scholar]
- 56.Slim B Karen, Nini E, Forestier D, Kwiatkowski F, Panis Y, ChipponiHIPPONI J. Development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 57.critical-appraisal-tools—Critical Appraisal Tools | Joanna Briggs Institute [Internet]. [cited 2020 Apr 27]. Available from: https://joannabriggs.org/critical-appraisal-tools
- 58.Pomar L, Malinger G, Benoist G, Carles G, Ville Y, Rousset D, et al. Association between Zika virus and fetopathy: a prospective cohort study in French Guiana. Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2017. June;49(6):729–36. 10.1002/uog.17404 [DOI] [PubMed] [Google Scholar]
- 59.Honein MA, Dawson AL, Petersen EE, Jones AM, Lee EH, Yazdy MM, et al. Birth Defects Among Fetuses and Infants of US Women With Evidence of Possible Zika Virus Infection During Pregnancy. Jama-J Am Med Assoc. 2017. January 3;317(1):59–68. 10.1001/jama.2016.19006 [DOI] [PubMed] [Google Scholar]
- 60.Zin A.A., Tsui I., Rossetto J., Vasconcelos Z., Adachi K., Valderramos S., et al. Screening criteria for ophthalmic manifestations of congenital zika virus infection. JAMA Pediatr. 2017;171(9):847–54. 10.1001/jamapediatrics.2017.1474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aragão MFVV, Brainer-Lima AM, Holanda AC, van der Linden V, Vasco Aragao L, Silva Junior MLM, et al. Spectrum of Spinal Cord, Spinal Root, and Brain MRI Abnormalities in Congenital Zika Syndrome with and without Arthrogryposis. Am J Neuroradiol. 2017. May;38(5):1045–53. 10.3174/ajnr.A5125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ventura LO, Ventura CV, Lawrence L, van der Linden V, van der Linden A, Gois AL, et al. Visual impairment in children with congenital Zika syndrome. J AAPOS. 2017;21(4):295–299.e2. 10.1016/j.jaapos.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 63.Schaub B., Vouga M., Najioullah F., Gueneret M., Monthieux A., Harte C., et al. Analysis of blood from Zika virus-infected fetuses: a prospective case series. Lancet Infect Dis. 2017;17(5):520–7. 10.1016/S1473-3099(17)30102-0 [DOI] [PubMed] [Google Scholar]
- 64.Carvalho FHC, Cordeiro KM, Peixoto AB, Tonni G, Moron AF, Feitosa FEL, et al. Associated ultrasonographic findings in fetuses with microcephaly because of suspected Zika virus (ZIKV) infection during pregnancy. Prenat Diagn. 2016. September;36(9):882–7. 10.1002/pd.4882 [DOI] [PubMed] [Google Scholar]
- 65.Aragão MF, Van Der Linden V, Brainer-Lima AM, Coeli RR, Rocha MA, Da Silva PS, et al. Clinical features and neuroimaging (CT and MRI) findings in presumed Zika virus related congenital infection and microcephaly: Retrospective case series study. BMJ Online [Internet]. 2016;353 Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84964345444&doi=10.1136%2fbmj.i1901&partnerID=40&md5=2c66e63d65731eb21e8ad3d80fc48add [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hazin AN, Poretti A, Di Cavalcanti Souza Cruz D, Tenorio M, van der Linden A, Pena LJ, et al. Computed Tomographic Findings in Microcephaly Associated with Zika Virus. N Engl J Med. 2016. June 2;374(22):2193–5. 10.1056/NEJMc1603617 [DOI] [PubMed] [Google Scholar]
- 67.De Oliveira-Szejnfeld PS, Levine D, De Oliveira Melo AS, Amorim MMR, Batista AGM, Chimelli L, et al. Congenital brain abnormalities and Zika virus: What the radiologist can expect to see prenatally and postnatally. Radiology. 2016;281(1):203–18. 10.1148/radiol.2016161584 [DOI] [PubMed] [Google Scholar]
- 68.Besnard M, Eyrolle-Guignot D, Guillemette-Artur P, Lastere S, Bost-Bezeaud F, Marcelis L, et al. Congenital cerebral malformations and dysfunction in fetuses and newborns following the 2013 to 2014 Zika virus epidemic in French Polynesia. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2016;21(13). 10.2807/1560-7917.ES.2016.21.13.30181 [DOI] [PubMed] [Google Scholar]
- 69.van der Linden V, Rolim Filho EL, Lins OG, van der Linden A, Viana Vasco Aragao M de F, Brainer-Lima AM, et al. Congenital Zika syndrome with arthrogryposis: retrospective case series study. Bmj-Br Med J. 2016. August 9;354:i3899 10.1136/bmj.i3899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Oliveira Melo AS, Aguiar RS, Amorim MMR, Arruda MB, De Oliveira Melo F, Ribeiro STC, et al. Congenital Zika virus infection: Beyond neonatal microcephaly. JAMA Neurol. 2016;73(12):1407–16. 10.1001/jamaneurol.2016.3720 [DOI] [PubMed] [Google Scholar]
- 71.van der Linden V, Pessoa A, Dobyns W, Barkovich AJ, Junior H van der L, Filho ELR, et al. Description of 13 Infants Born During October 2015-January 2016 With Congenital Zika Virus Infection Without Microcephaly at Birth—Brazil. MMWR Morb Mortal Wkly Rep. 2016. December 2;65(47):1343–8. 10.15585/mmwr.mm6547e2 [DOI] [PubMed] [Google Scholar]
- 72.Sanín-Blair J.E., Gutiérrez-Márquez C., Herrera D.A., Vossough A. Fetal Magnetic Resonance Imaging Findings in Prenatal Zika Virus Infection. Fetal Diagn Ther. 2017;42(2):153–7. 10.1159/000454860 [DOI] [PubMed] [Google Scholar]
- 73.Meneses J.D.A., Ishigami A.C., De Mello L.M, De Albuquerque L.L., De Brito C.A.A., Cordeiro M.T., et al. Lessons Learned at the Epicenter of Brazil’s Congenital Zika Epidemic: Evidence from 87 Confirmed Cases. Clin Infect Dis. 2017;64(10):1302–8. 10.1093/cid/cix166 [DOI] [PubMed] [Google Scholar]
- 74.Fernandez MP, Parra Saad E, Ospina Martinez M, Corchuelo S, Mercado Reyes M, Herrera MJ, et al. Ocular Histopathologic Features of Congenital Zika Syndrome. JAMA Ophthalmol. 2017. November 1;135(11):1163–9. 10.1001/jamaophthalmol.2017.3595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sousa A.Q., Cavalcante D.I.M., Franco L.M., Araújo F.M.C., Sousa E.T., Valença-Junior J.T, et al. Postmortem findings for 7 neonates with congenital Zika virus infection. Emerg Infect Dis. 2017;23(7):1164–7. 10.3201/eid2307.162019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guillemette-Artur P, Besnard M, Eyrolle-Guignot D, Jouannic J-M, Garel C. Prenatal brain MRI of fetuses with Zika virus infection. Pediatr Radiol. 2016. June;46(7):1032–9. 10.1007/s00247-016-3619-6 [DOI] [PubMed] [Google Scholar]
- 77.Castro MC, Han QC, Carvalho LR, Victora CG, França GVA. Implications of Zika virus and congenital Zika syndrome for the number of live births in Brazil. Proc Natl Acad Sci. 2018. June 12;115(24):6177–82. 10.1073/pnas.1718476115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ventura C.V., Maia M., Travassos S.B., Martins T.T., Patriota F, Nunes M.E., et al. Risk factors associated with the ophthalmoscopic findings identified in infants with presumed zika virus congenital infection. JAMA Ophthalmol. 2016;134(8):912–8. 10.1001/jamaophthalmol.2016.1784 [DOI] [PubMed] [Google Scholar]
- 79.Parra-Saavedra M, Reefhuis J, Piraquive JP, Gilboa SM, Badell ML, Moore CA, et al. Serial Head and Brain Imaging of 17 Fetuses With Confirmed Zika Virus Infection in Colombia, South America. Obstet Gynecol. 2017. July;130(1):207–12. 10.1097/AOG.0000000000002105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Del Campo M, Feitosa IML, Ribeiro EM, Horovitz DDG, Pessoa ALS, Franca GVA, et al. The phenotypic spectrum of congenital Zika syndrome. Am J Med Genet A. 2017. April;173(4):841–57. 10.1002/ajmg.a.38170 [DOI] [PubMed] [Google Scholar]
- 81.Chimelli L, Melo ASO, Avvad-Portari E, Wiley CA, Camacho AHS, Lopes VS, et al. The spectrum of neuropathological changes associated with congenital Zika virus infection. Acta Neuropathol (Berl). 2017. June;133(6):983–99. [DOI] [PubMed] [Google Scholar]
- 82.Schaub B., Gueneret M., Jolivet E., Decatrelle V, Yazza S., Gueye H., et al. Ultrasound imaging for identification of cerebral damage in congenital Zika virus syndrome: a case series. Lancet Child Adolesc Health. 2017;1(1):45–55. 10.1016/S2352-4642(17)30001-9 [DOI] [PubMed] [Google Scholar]
- 83.Mattar S, Ojeda C, Arboleda J, Arrieta G, Bosch I, Botia I, et al. Case report: microcephaly associated with Zika virus infection, Colombia. BMC Infect Dis. 2017. June;17(1):423–423. 10.1186/s12879-017-2522-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Culjat M, Darling SE, Nerurkar VR, Ching N, Kumar M, Min SK, et al. Clinical and Imaging Findings in an Infant With Zika Embryopathy. Clin Infect Dis. 2016. September 15;63(6):805–11. 10.1093/cid/ciw324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Souza ASR, Cordeiro MT, Meneses JA, Honorato E, Araujo Júnior E, Castanha PMS, et al. Clinical and laboratory diagnosis of congenital zika virus syndrome and diaphragmatic unilateral palsy: Case report. Rev Bras Saude Materno Infant. 2016;16(4):467–73. [Google Scholar]
- 86.Perez S, Tato R, Cabrera JJ, Lopez A, Robles O, Paz E, et al. Confirmed case of Zika virus congenital infection, Spain, March 2016. Euro Surveill Bull Eur Sur Mal Transm Eur Commun Dis Bull. 2016. June 16;21(24). [DOI] [PubMed] [Google Scholar]
- 87.Van der Linden V, Van der Linden H van der J, Leal M de C, Rolim ELF, Linden A van der, Aragao M de FVV, et al. Discordant clinical outcomes of congenital Zika virus infection in twin pregnancies. Arq Neuropsiquiatr. 2017. June;75(6):381–6. 10.1590/0004-282X20170066 [DOI] [PubMed] [Google Scholar]
- 88.Souza AS, Dias CM, Braojos Braga FDC, Bernardes Terzian AC, Estofolete CF, Oliani AH, et al. Fetal Infection by Zika Virus in the Third Trimester: Report of 2 Cases. Clin Infect Dis. 2016. December 15;63(12):1622–5. 10.1093/cid/ciw613 [DOI] [PubMed] [Google Scholar]
- 89.Vorona G.A., Lanni S.M. Fetal Magnetic Resonance Imaging Evaluation of a 21-Week Fetus With Zika Virus Infection. Pediatr Neurol. 2016;65:98–9. 10.1016/j.pediatrneurol.2016.07.014 [DOI] [PubMed] [Google Scholar]
- 90.Zacharias N, Whitty J, Noblin S, Tsakiri S, Garcia J, Covinsky M, et al. First Neonatal Demise with Travel-Associated Zika Virus Infection in the United States of America. Ajp Rep. 2017. April;7(2):68–73. 10.1055/s-0037-1601890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Werner H, Sodre D, Hygino C, Guedes B, Fazecas T, Nogueira R, et al. First-trimester intrauterine Zika virus infection and brain pathology: prenatal and postnatal neuroimaging findings. Prenat Diagn. 2016. August;36(8):785–9. 10.1002/pd.4860 [DOI] [PubMed] [Google Scholar]
- 92.de Paula Freitas B., Ko A.I., Khouri R., Mayoral M., Henriques D.F., Maia M., et al. Glaucoma and Congenital Zika Syndrome. Ophthalmology. 2017;124(3):407–8. 10.1016/j.ophtha.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 93.Moron A.F., Cavalheiro S., Milani H.J.F., Sarmento S.G.P., Tanuri C, de Souza F.F., et al. Microcephaly associated with maternal Zika virus infection. BJOG Int J Obstet Gynaecol. 2016;123(8):1265–9. 10.1111/1471-0528.14072 [DOI] [PubMed] [Google Scholar]
- 94.Frutos MGL, Ochoa JH, Barbás MG, Lucchini HD, Moya M, Malinger G. New Insights into the Natural History of Congenital Zika Virus Syndrome Fetal Diagn Ther [Internet]. 2017;((Lovagnini Frutos M.G.; Ochoa J.H.; Barbás M.G.; Lucchini H.D.; Moya M.; Malinger G.) aUniversity Maternity Hospital (HUMN), Córdoba National University, bDiagnus SA. Prenatal Diagnosis Center, and cCentral Laboratory Department, Ministry of Health, Córdoba, Argentina; dDivision of Ultrasound in Obstetrics&Gynecology, Lis Maternity Hospital, Tel Aviv Sourasky Medical Center, eSackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel: ). Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L618299728 [Google Scholar]
- 95.Acosta-Reyes J, Navarro E, Herrera MJ, Goenaga E, Ospina ML, Parra E, et al. Severe neurologic disorders in 2 fetuses with Zika virus infection, Colombia. Emerg Infect Dis. 2017;23(6):982–4. 10.3201/eid2306.161702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Vesnaver T.V., Tul N., Mehrabi S., Parissone F., Štrafela P., Mlakar J., et al. Zika virus associated microcephaly/micrencephaly—fetal brain imaging in comparison with neuropathology. BJOG Int J Obstet Gynaecol. 2017;124(3):521–5. 10.1111/1471-0528.14423 [DOI] [PubMed] [Google Scholar]
- 97.Sarno M, Sacramento GA, Khouri R, do Rosario MS, Costa F, Archanjo G, et al. Zika Virus Infection and Stillbirths: A Case of Hydrops Fetalis, Hydranencephaly and Fetal Demise. PLoS Negl Trop Dis. 2016. February;10(2):e0004517 10.1371/journal.pntd.0004517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Melo AO, Malinger G, Ximenes R, Szejnfeld P, Sampaio S, A.M. B de F. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol Off J Int Soc Ultrasound Obstet Gynecol. 2016;47(1):6–7. [DOI] [PubMed] [Google Scholar]
- 99.Norero Vega X, Castaño G E, Estripeaut C D, Sáez-Llorens X, Reyes O, Bissot A. Zika y defecto del tubo neural. Pediátr Panamá. 2016. April;45(1):23–5. [Google Scholar]
- 100.Castro JD Vieira, Pereira LP, Dias DA, Aguiar LB, Maia JC, Costa JIF, et al. Presumed Zika virus-related congenital brain malformations: the spectrum of CT and MRI findings in fetuses and newborns. Arq Neuropsiquiatr. 2017. October;75(10):703–10. 10.1590/0004-282X20170134 [DOI] [PubMed] [Google Scholar]
- 101.Sanin-Blair J., Cumplido A., Gutierrez-Marin J., Campo-Campo M., Garcia-Posada R., Londoño A., et al. Fetal ultrasound findings in zika infection. Preliminary report in a Colombian selected population. J Matern Fetal Neonatal Med. 2016;29:163–4. 10.3109/14767058.2014.991917 [DOI] [PubMed] [Google Scholar]
- 102.Souza ASR, de Souza AI, de Lourdes Loreto Faquin S, dos Santos Neto OG, Honorato E, Mattos AGL, et al. Altered intrauterine ultrasound, fetal head circumference growth and neonatal outcomes among suspected cases of congenital Zika syndrome in Brazil. Rev Bras Saude Materno Infant. 2016;16:S7–15. [Google Scholar]
- 103.Vesnaver T.V., Tul N, Mlakar J., Mehrabi S., Zupanc T.A., Popović M. Microcephaly caused by Zika virus—MRI of the fetal brain and correlation with neuropathology. Neuroradiology. 2016;58(1):S66–7. [Google Scholar]
- 104.Cragan JD. Baseline Prevalence of Birth Defects Associated with Congenital Zika Virus Infection—Massachusetts, North Carolina, and Atlanta, Georgia, 2013–2014. MMWR Morb Mortal Wkly Rep [Internet]. 2017. [cited 2017 Jun 17];66 Available from: https://www.facebook.com/CDCMMWR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pomar L, Vouga M, Lambert V, Pomar C, Hcini N, Jolivet A, et al. Maternal-fetal transmission and adverse perinatal outcomes in pregnant women infected with Zika virus: prospective cohort study in French Guiana. BMJ. 2018. October 31;k4431 10.1136/bmj.k4431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rodó C, Suy A, Sulleiro E, Soriano-Arandes A, Maiz N, García-Ruiz I, et al. Pregnancy outcomes after maternal Zika virus infection in a non-endemic region: prospective cohort study. Clin Microbiol Infect. 2019. May 1;25(5):633.e5–633.e9. [DOI] [PubMed] [Google Scholar]
- 107.Brady OJ, Osgood-Zimmerman A, Kassebaum NJ, Ray SE, de Araújo VEM, da Nóbrega AA, et al. The association between Zika virus infection and microcephaly in Brazil 2015–2017: An observational analysis of over 4 million births. PLoS Med [Internet]. 2019. March 5 [cited 2019 Nov 18];16(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6400331/ 10.1371/journal.pmed.1002755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Morris JK, Rankin J, Garne E, Loane M, Greenlees R, Addor M-C, et al. Prevalence of microcephaly in Europe: population based study. BMJ. 2016. September;354:i4721–i4721. 10.1136/bmj.i4721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Averill LW, Kandula VVR, Akyol Y, Epelman M. Fetal Brain Magnetic Resonance Imaging Findings In Congenital Cytomegalovirus Infection With Postnatal Imaging Correlation. Semin Ultrasound CT MRI. 2015. December;36(6):476–86. 10.1053/j.sult.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 110.Parmar H, Ibrahim M. Pediatric Intracranial Infections. Neuroimaging Clin N Am. 2012. November;22(4):707–25. 10.1016/j.nic.2012.05.016 [DOI] [PubMed] [Google Scholar]
- 111.Levine D., Jani J.C., Castro-Aragon I., Cannie M. How does imaging of congenital zika compare with imaging of other to rch infections? Radiology. 2017;285(3):744–61. 10.1148/radiol.2017171238 [DOI] [PubMed] [Google Scholar]
- 112.La Piana R, Uggetti C, Roncarolo F, Vanderver A, Olivieri I, Tonduti D, et al. Neuroradiologic patterns and novel imaging findings in Aicardi-Goutières syndrome. Neurology. 2016. January 5;86(1):28–35. 10.1212/WNL.0000000000002228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Van der Linden V, Petribu NC de L, Pessoa A, Faquini I, Paciorkowski AR, Linden H van der, et al. Association of Severe Hydrocephalus With Congenital Zika Syndrome. JAMA Neurol. 2019. February 1;76(2):203–10. 10.1001/jamaneurol.2018.3553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cherry JD. Cutaneous manifestations of infectious diseases In: Cherry J D, Harrison G J, Kaplan S L, Hotez P J, & Steinbach W J eds Feigin and Cherry’s textbook of pediatric infectious diseases. 7th ed Philaderphia: Elsevier-Sanders; 2014. p. 741–68. [Google Scholar]
- 115.Simeone RM, Shapiro-Mendoza CK, Meaney-Delman D, Petersen EE, Galang RR, Oduyebo T, et al. Possible Zika Virus Infection Among Pregnant Women—United States and Territories, May 2016. MMWR Morb Mortal Wkly Rep. 2016. May 27;65(20):514–9. 10.15585/mmwr.mm6520e1 [DOI] [PubMed] [Google Scholar]
- 116.Moore CA, Staples JE, Dobyns WB, Pessoa A, Ventura CV, da Fonseca EB, et al. Congenital Zika Syndrome: Characterizing the Pattern of Anomalies for Pediatric Healthcare Providers. JAMA Pediatr. 2017. March 1;171(3):288–95. 10.1001/jamapediatrics.2016.3982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Coyne C.B., Lazear H.M. Zika virus-reigniting the TORCH. Nat Rev Microbiol. 2016;14(11):707–15. 10.1038/nrmicro.2016.125 [DOI] [PubMed] [Google Scholar]
- 118.Nahmias AJ, Walls KW, John A Stewart, Herrmann KL Jr, WJF. The ToRCH complex-perinatal infections associated with toxoplasma and rubella, cytomegol- and herpes simplex viruses. Pediatr Res. 1971. August;5(8):405–6. [Google Scholar]
- 119.Salt A, Sargent J. Common visual problems in children with disability. Arch Dis Child. 2014. December 1;99(12):1163–8. 10.1136/archdischild-2013-305267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Moore C.A., Staples J.E., Dobyns W.B., Pessoa A., Ventura C.V., Da Fonseca E.B., et al. Characterizing the pattern of anomalies in congenital zika syndrome for pediatric clinicians. JAMA Pediatr. 2017;171(3):288–95. 10.1001/jamapediatrics.2016.3982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zare Mehrjardi M, Poretti A, Huisman TAGM, Werner H, Keshavarz E, Araujo Junior E. Neuroimaging findings of congenital Zika virus infection: a pictorial essay. Jpn J Radiol. 2017. March;35(3):89–94. 10.1007/s11604-016-0609-4 [DOI] [PubMed] [Google Scholar]
- 122.Tsui I, Moreira MEL, Rossetto JD, Vasconcelos Z, Gaw SL, Neves LM, et al. Eye Findings in Infants With Suspected or Confirmed Antenatal Zika Virus Exposure. Pediatrics [Internet]. 2018. October [cited 2020 Feb 15];142(4). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6317824/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tsui I, Neves LM, Adachi K, Gaw SL, Pereira JP, Brasil P, et al. Overlapping Spectrum of Retinochoroidal Scarring in Congenital Zika Virus and Toxoplasmosis Infections. Ophthalmic Surg Lasers Imaging Retina. 2019. December 1;50(12):779–84. 10.3928/23258160-20191119-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Capretti MG, Marsico C, Guidelli Guidi S, Ciardella A, Simonazzi G, Galletti S, et al. Neonatal and long-term ophthalmological findings in infants with symptomatic and asymptomatic congenital cytomegalovirus infection. J Clin Virol. 2017. December 1;97:59–63. 10.1016/j.jcv.2017.11.001 [DOI] [PubMed] [Google Scholar]
- 125.Lyons CJ, Lambert SR. Taylor and Hoyt’s Pediatric Ophthalmology and Strabismus E-Book. Elsevier Health Sciences; 2016. 1181 p. [Google Scholar]
- 126.Adibi JJ, Marques ETAJ, Cartus A, Beigi RH. Teratogenic effects of the Zika virus and the role of the placenta. Lancet Lond Engl. 2016. April 9;387(10027):1587–90. 10.1016/S0140-6736(16)00650-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cugola FR, Fernandes IR, Russo FB, Freitas BC, Dias JLM, Guimarães KP, et al. The Brazilian Zika virus strain causes birth defects in experimental models. Nature. 2016;534(7606):267–71. 10.1038/nature18296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Liang B, Guida JP, Costa ML, Mysorekar IU. Host and viral mechanisms of congenital Zika syndrome. Virulence. 2019. January 1;10(1):768–75. 10.1080/21505594.2019.1656503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shapiro-Mendoza C.K., Rice M.E., Galang R.R, Fulton A.C., VanMaldeghem K., Prado M.V., et al. Pregnancy Outcomes After Maternal Zika Virus Infection During Pregnancy—U.S. Territories, January 1, 2016-April 25, 2017. MMWR Morb Mortal Wkly Rep. 2017;66(23):615–21. 10.15585/mmwr.mm6623e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cauchemez S, Besnard M, Bompard P, Dub T, Guillemette-Artur P, Eyrolle-Guignot D, et al. Association between Zika virus and microcephaly in French Polynesia, 2013–15: a retrospective study. Lancet Lond Engl. 2016. May 21;387(10033):2125–32. 10.1016/S0140-6736(16)00651-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hoen B, Schaub B, Funk AL, Ardillon V, Boullard M, Cabié A, et al. Pregnancy Outcomes after ZIKV Infection in French Territories in the Americas. N Engl J Med. 2018. March 15;378(11):985–94. 10.1056/NEJMoa1709481 [DOI] [PubMed] [Google Scholar]
- 132.Lima GP, Rozenbaum D, Pimentel C, Frota ACC, Vivacqua D, Machado ES, et al. Factors associated with the development of Congenital Zika Syndrome: a case-control study. BMC Infect Dis. 2019. March 22;19(1):277 10.1186/s12879-019-3908-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pool K-L, Adachi K, Karnezis S, Salamon N, Romero T, Nielsen-Saines K, et al. Association Between Neonatal Neuroimaging and Clinical Outcomes in Zika-Exposed Infants From Rio de Janeiro, Brazil. JAMA Netw Open. 2019. July 3;2(7):e198124–e198124. 10.1001/jamanetworkopen.2019.8124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cuevas E.L., Tong V.T., Rozo N., Valencia D., Pacheco O., Gilboa S.M., et al. Preliminary Report of Microcephaly Potentially Associated with Zika Virus Infection During Pregnancy—Colombia, January-November 2016. MMWR Morb Mortal Wkly Rep. 2016;65(49):1409–13. 10.15585/mmwr.mm6549e1 [DOI] [PubMed] [Google Scholar]
- 135.Franca GVA, Schuler-Faccini L, Oliveira WK, Henriques CMP, Carmo EH, Pedi VD, et al. Congenital Zika virus syndrome in Brazil: a case series of the first 1501 livebirths with complete investigation. Lancet Lond Engl. 2016. August 27;388(10047):891–7. 10.1016/S0140-6736(16)30902-3 [DOI] [PubMed] [Google Scholar]
- 136.Halai U-A, Nielsen-Saines K, Moreira ML, de Sequeira PC, Pereira JPJ, Zin A de A, et al. Maternal Zika Virus Disease Severity, Virus Load, Prior Dengue Antibodies, and Their Relationship to Birth Outcomes. Clin Infect Dis. 2017. September 15;65(6):877–83. 10.1093/cid/cix472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Huang L-M. How can we deal with Zika virus infection? J Formos Med Assoc Taiwan Yi Zhi. 2016. April;115(4):221–2. 10.1016/j.jfma.2016.03.001 [DOI] [PubMed] [Google Scholar]
- 138.Molnar Z, Kennedy S. Risks of Zika virus during the first trimester of pregnancy. Nat Rev Neurol. 2016. June;12(6):315–U13. 10.1038/nrneurol.2016.71 [DOI] [PubMed] [Google Scholar]
- 139.Reynolds MR, Jones AM, Petersen EE, Lee EH, Rice ME, Bingham A, et al. Vital Signs: Update on Zika Virus-Associated Birth Defects and Evaluation of All U.S. Infants with Congenital Zika Virus Exposure—U.S. Zika Pregnancy Registry, 2016. MMWR Morb Mortal Wkly Rep. 2017. April 7;66(13):366–73. 10.15585/mmwr.mm6613e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Santa Rita TH, Barra RB, Peixoto GP, Mesquita PG, Barra GB. Association between suspected Zika virus disease during pregnancy and giving birth to a newborn with congenital microcephaly: A matched case-control study. BMC Res Notes [Internet]. 2017;10(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85028940762&doi=10.1186%2fs13104-017-2796-1&partnerID=40&md5=2159741163da422abe8173ec65521ec6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Schuler-Faccini L, Ribeiro EM, Feitosa IML, Horovitz DDG, Cavalcanti DP, Pessoa A, et al. Possible Association Between Zika Virus Infection and Microcephaly—Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016. January 29;65(3):59–62. 10.15585/mmwr.mm6503e2 [DOI] [PubMed] [Google Scholar]
- 142.Mulkey SB, Bulas DI, Vezina G, Fourzali Y, Morales A, Arroyave-Wessel M, et al. Sequential Neuroimaging of the Fetus and Newborn With In Utero Zika Virus Exposure. JAMA Pediatr. 2019. 01;173(1):52–9. 10.1001/jamapediatrics.2018.4138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ribeiro BG, Werner H, Lopes FPPL, Hygino da Cruz LC, Fazecas TM, Daltro PAN, et al. Central Nervous System Effects of Intrauterine Zika Virus Infection: A Pictorial Review. RadioGraphics. 2017. Oct 1;37(6):1840–50. 10.1148/rg.2017170023 [DOI] [PubMed] [Google Scholar]
- 144.Carvalho-Sauer R, Costa M da CN, Barreto FR, Teixeira MG. Congenital Zika Syndrome: Prevalence of low birth weight and associated factors. Bahia, 2015–2017. Int J Infect Dis. 2019. May 1;82:44–50. 10.1016/j.ijid.2019.02.040 [DOI] [PubMed] [Google Scholar]
- 145.Moura da Silva AA, Santos Ganz JS, Sousa P da S, Rodovalho Doriqui MJ, Costa Ribeiro MR, Freitas Carvalho Branco M dos R, et al. Early Growth and Neurologic Outcomes of Infants with Probable Congenital Zika Virus Syndrome. Emerg Infect Dis. 2016. November;22(11):1953–6. 10.3201/eid2211.160956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Villamil-Gómez WE, Padilla-Ruiz D, Mendoza A, Álvarez Á, Baldrich-Gomez O, Posso H, et al. Urinary bladder agenesis and renal hypoplasia potentially related to in utero Zika virus infection. Int J Infect Dis. 2019. August 1;85:54–6. 10.1016/j.ijid.2019.05.021 [DOI] [PubMed] [Google Scholar]
- 147.Costa Monteiro LM, Cruz GN de O, Fontes JM, de Araujo GF, Ventura T, Monteiro AC, et al. Neurogenic bladder in the settings of congenital Zika syndrome: a confirmed and unknown condition for urologists. J Pediatr Urol [Internet]. 2019. April [cited 2019 Nov 4]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S1477513119300907 [DOI] [PubMed] [Google Scholar]
- 148.Angelidou A, Michael Z, Hotz A, Friedman K, Emani S, LaRovere K, et al. Is There More to Zika? Complex Cardiac Disease in a Case of Congenital Zika Syndrome. Neonatology. 2018;113(2):177–82. 10.1159/000484656 [DOI] [PubMed] [Google Scholar]
- 149.Cavalcanti DD, Alves LV, Furtado GJ, Santos CC, Feitosa FG, Ribeiro MC, et al. Echocardiographic findings in infants with presumed congenital Zika syndrome: Retrospective case series study. PloS One. 2017;12(4):e0175065 10.1371/journal.pone.0175065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Orofino DHG, Passos SRL, de Oliveira RVC, Farias CVB, Leite M de FMP, Pone SM, et al. Cardiac findings in infants with in utero exposure to Zika virus- a cross sectional study. PLoS Negl Trop Dis [Internet]. 2018. March 26 [cited 2019 Nov 6];12(3). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5886696/ 10.1371/journal.pntd.0006362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Santana MB, Lamas CC, Athayde JG, Calvet G, Moreira J, De Lorenzo A. Congenital Zika syndrome: is the heart part of its spectrum? Clin Microbiol Infect. 2019. August;25(8):1043–4. 10.1016/j.cmi.2019.03.020 [DOI] [PubMed] [Google Scholar]
- 152.Leal MC, Muniz LF, Ferreira TSA, Santos CM, Almeida LC, Van Der Linden V, et al. Hearing Loss in Infants with Microcephaly and Evidence of Congenital Zika Virus Infection—Brazil, November 2015-May 2016. MMWR Morb Mortal Wkly Rep. 2016. September 2;65(34):917–9. 10.15585/mmwr.mm6534e3 [DOI] [PubMed] [Google Scholar]
- 153.Pessoa A, van der Linden V, Yeargin-Allsopp M, Carvalho MDCG, Ribeiro EM, Van Naarden Braun K, et al. Motor Abnormalities and Epilepsy in Infants and Children With Evidence of Congenital Zika Virus Infection. Pediatrics. 2018. February;141(Suppl 2):S167–79. 10.1542/peds.2017-2038F [DOI] [PubMed] [Google Scholar]
- 154.Bhatnagar J, Rabeneck DB, Martines RB, Reagan-Steiner S, Ermias Y, Estetter LBC, et al. Zika Virus RNA Replication and Persistence in Brain and Placental Tissue. Emerg Infect Dis. 2017. March;23(3):405–14. 10.3201/eid2303.161499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Melo A, Gama GL, Da Silva Júnior RA, De Assunção PL, Tavares JS, Da Silva MB, et al. Motor function in children with congenital Zika syndrome. Dev Med Child Neurol [Internet]. 2019. April 4 [cited 2019 Nov 4]; Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/dmcn.14227 [DOI] [PubMed] [Google Scholar]
- 156.Satterfield-Nash A. Health and Development at Age 19–24 Months of 19 Children Who Were Born with Microcephaly and Laboratory Evidence of Congenital Zika Virus Infection During the 2015 Zika Virus Outbreak—Brazil, 2017. MMWR Morb Mortal Wkly Rep [Internet]. 2017. [cited 2019 Nov 2];66 Available from: https://www.cdc.gov/mmwr/volumes/66/wr/mm6649a2.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Flamand C, Fritzell C, Matheus S, Dueymes M, Carles G, Favre A, et al. The proportion of asymptomatic infections and spectrum of disease among pregnant women infected by Zika virus: systematic monitoring in French Guiana, 2016. Eurosurveillance [Internet]. 2017. November 2 [cited 2019 Nov 19];22(44). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5710134/ 10.2807/1560-7917.ES.2017.22.44.17-00102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.WHO. COUNTRIES AND TERRITORIES WITH CURRENT OR PREVIOUS ZIKA VIRUS TRANSMISSION [Internet]. 2019 [cited 2020 Oct 9]. Available from: https://www.who.int/emergencies/diseases/zika/countries-with-zika-and-vectors-table.pdf
- 159.Achee NL, Gould F, Perkins TA, Jr RCR, Morrison AC, Ritchie SA, et al. A Critical Assessment of Vector Control for Dengue Prevention. PLoS Negl Trop Dis. 2015. May 7;9(5):e0003655 10.1371/journal.pntd.0003655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ant TH, Herd CS, Geoghegan V, Hoffmann AA, Sinkins SP. The Wolbachia strain wAu provides highly efficient virus transmission blocking in Aedes aegypti. PLOS Pathog. 2018. January 25;14(1):e1006815 10.1371/journal.ppat.1006815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Caprara A, De Oliveira Lima JW, Rocha Peixoto AC, Vasconcelos Motta CM, Soares Nobre JM, Sommerfeld J, et al. Entomological impact and social participation in dengue control: a cluster randomized trial in Fortaleza, Brazil. Trans R Soc Trop Med Hyg. 2015. February;109(2):99–105. 10.1093/trstmh/tru187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Jr RCR, Achee N, Barrera R, Burkot TR, Chadee DD, Devine GJ, et al. Quantifying the Epidemiological Impact of Vector Control on Dengue. PLoS Negl Trop Dis. 2016. May 26;10(5):e0004588 10.1371/journal.pntd.0004588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Quintero J, Brochero H, Manrique-Saide P, Barrera-Pérez M, Basso C, Romero S, et al. Ecological, biological and social dimensions of dengue vector breeding in five urban settings of Latin America: a multi-country study. BMC Infect Dis. 2014. January 21;14:38 10.1186/1471-2334-14-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.WHO, editor. Handbook for integrated vector management. Geneva: World Health Organization; 2012. 68 p. [Google Scholar]
- 165.Vouga M, Chiu Y-C, Pomar L, de Meyer SV, Masmejan S, Genton B, et al. Dengue, Zika and chikungunya during pregnancy: pre- and post-travel advice and clinical management. J Travel Med [Internet]. 2019. October 16 [cited 2020 Oct 14];26(8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6927317/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Oliveira MAP, Velarde GC. Entendendo a pesquisa clínica V: relatos e séries de casos. 2015;4. [Google Scholar]