Abstract
Introduction
Wearable robots controlled using electromyography could motivate greater use of the affected upper extremity after stroke and enable bimanual activities of daily living to be completed independently.
Methods
We have developed a myoelectric untethered robotic glove (My-HERO) that provides five-finger extension and grip assistance.
Results
The myoelectric controller detected the grip and release intents of the 9 participants after stroke with 84.7% accuracy. While using My-HERO, all 9 participants performed better on the Fugl-Meyer Assessment-Hand (8.4 point increase, scale out of 14, p < 0.01) and the Chedoke Arm and Hand Activity Inventory (8.2 point increase, scale out of 91, p < 0.01). Established criteria for clinically meaningful important differences were surpassed for both the hand function and daily living task assessments. The majority of participants provided satisfaction and usability questionnaire scores above 70%. Seven participants desired to use My-HERO in the clinic and at home during their therapy and daily routines.
Conclusions
People with hand impairment after stroke value that myoelectric untethered robotic gloves enhance their motion and bimanual task performance and motivate them to use their muscles during engaging activities of daily living. They desire to use these gloves daily to enable greater independence and investigate the effects on neuromuscular recovery.
Keywords: Wearable robotics, exoskeletons, soft robotics, stroke, hand therapy, activities of daily living, rehabilitation, assistive technology
Introduction
Wearable robots are advancing and merging the fields of rehabilitation and assistive technology. These tools help occupational and physical therapists and people with motor impairments to practice a wider selection of functional movements in more diverse environments, thereby making therapy more intensive, efficacious, engaging and transferable to peoples’ personal rehabilitation goals. The “always-available” assistance provided by wearable robots could also immediately eliminate barriers to living independently. With robot use, we can reduce the perceived mental and physical effort required to use affected limbs, so the user performs more activities of daily living (ADLs) independently and the proper muscle activations and movement patterns are reinforced.
Efficacy of assistive wearable hand robots
Five percent of the population has difficulty lifting and grasping everyday objects like a bag of groceries, a cup or a pencil, which amounts to 19.9 million people in the United States alone.1 Rigid and soft robotic orthoses are being developed to assist their arms and hands to perform these and additional upper extremity tasks independently.2,3 For people with hand paralysis after spinal cord injury, Soekadar et al.4 showed that a wheelchair-mounted robotic hand exoskeleton controlled using electroencephalography and electrooculography enabled people with limited grip strength after spinal cord injury to perform better on unimanual upper extremity assessments of daily living tasks using the Toronto Rehabilitation Institute – Hand Function Test.5,6 Cappello et al.7 showed similar performance on this assessment once the objects were interposed in the hand, using a pneumatically-actuated robotic glove that was tethered to rigid components on a table and was controlled by the researcher. For people with hand impairment following stroke, hand extension assistance is critical since the hand is often clenched in a fist. After stroke, people often use walkers or canes instead of wheelchairs or do not use mobility aids at all, so untethered systems are more suitable. Peters et al.8 showed that a rigid-joint, myoelectric, untethered, elbow-wrist-finger orthosis could enhance performance on four daily living tasks specifically chosen to match the device’s capabilities, if the user has finger extension and low tone and spasticity. The system also surpassed criteria for clinically meaningful important differences on the Fugl-Meyer Assessment of Upper Extremity (FMA-UE) function. Recently, untethered robotic gloves with soft and rigid components have been found to enhance performance on a small set of grasping and lifting daily living tasks for people after stroke, even if the user has high tone and spasticity and no finger extension.9–11 However, the effectiveness of the assistance provided by wearable robots needs further evaluation with people with varying levels of hand impairment after stroke using a standardized set of daily living tasks.
Detecting intent to move the hand after stroke
People with severe hand impairment after stroke can regain hand function by using their affected hand throughout their therapy and daily routines.12 However, the affected hand is generally unused because even with intense effort, using the hand results in tasks being performed slowly and with low quality. As a result, people adapt by performing tasks one-handed, requesting caregiver assistance or avoiding tasks altogether. With robotic assistance, the level of effort could be reduced and task performance could be improved. Concurrently, it is important for the user to initiate the proper muscle and movement patterns to stimulate motor learning and neuroplasticity.13–16 Thresholds, linear discriminant analysis, decision trees and support vector machines have been used to detect the intents of people after stroke to extend their hand and grasp objects from their finger motion, force and electromyography (EMG) signals.17–22 These studies have found mixed results about the possibility of accurately detecting hand extension, multiple grasp postures and individual finger flexion for people with severe hand impairment after stroke. However, their grip signal (i.e. mass hand flexion) is often detectable through forearm flexor EMG and thumb flexion force measurement.20 Previous studies have yet to evaluate how well people with no finger extension after stroke can use EMG signals to control a robotic glove’s hand extension and grip assistance during a number of daily living tasks. By creating untethered robotic gloves and integrating them with easy to use myoelectric controllers, we can provide people after stroke with a tool for rehabilitating the upper extremity while performing daily routines more independently. By evaluating the system with people after stroke in daily living tasks, we can provide them and their therapists with guidance on the optimal use cases and motivate future experiments in novel therapy programs, environments and populations with hand impairment.
Organization of this article
In the Materials and Methods section, we describe the novel untethered robotic glove and its myoelectric calibration and control algorithm that were designed specifically for people with severe hand impairment after stroke. We then describe the participant inclusion criteria and the study protocol. In the Results section, we report how well people after stroke performed standardized assessments of hand function and daily living tasks with and without the myoelectric untethered robotic glove. We report their usability feedback following these trials. We provide a dataset of forearm EMG, acceleration and orientation recordings from people with severe hand impairment after stroke while performing grasp tasks and daily living tasks to support the research community in designing robotic gloves and control algorithms.
Materials and methods
My-HERO: Myoelectric untethered robotic glove
Mechatronics design
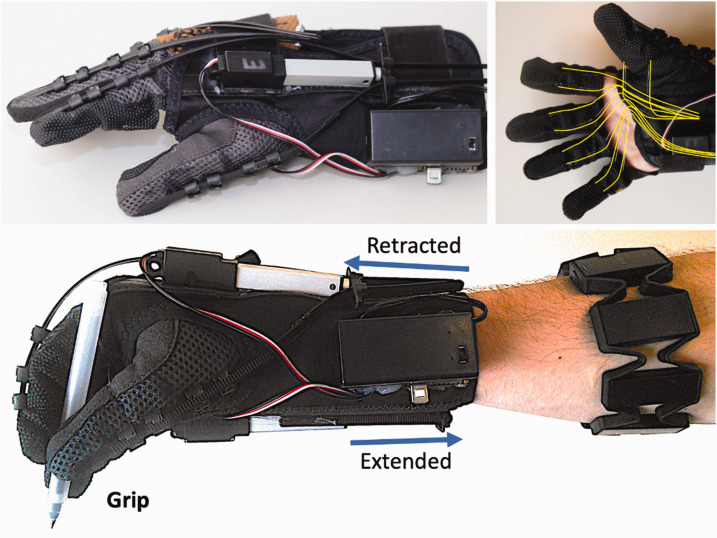
The Myoelectric untethered Hand Extension and grip Robot Orthosis (My-HERO) is shown in Figure 1. My-HERO is a battery-powered, untethered, robotic glove that senses the user’s intent to grasp or release objects from their forearm EMG signals. My-HERO uses one dorsal and one palmar linear actuator (Actuonix, L12-R, 210:1, 80 N max force, 50 mm stroke length) to exert mechanical forces on all five fingers to assist hand extension (i.e. five-finger extension and thumb abduction) and grip strength (i.e. five-finger flexion and thumb opposition and adduction). The first version, HERO Glove, showed that the actuator and cable tie tendon mechanism increases finger extension for both flaccid and clenched hands and the open palm design can be donned by people with flaccid and clenched hands after stroke.3 A wrist brace and a linear actuator on the palmar side of the forearm were added for the second version, the HERO Grip Glove, which enabled people after stroke to extend their fingers fully and then grip a water bottle, wooden block, a fork and a pen more securely.9 Assessments showed participants were ‘more or less satisfied’ with the HERO Grip Glove’s usability. The most requested improvements were for a more accurate control mode that did not require use of the unaffected hand, flexion assistance for all five fingers and stronger grip force, especially for small diameter objects like pens and forks.
Figure 1.
My-HERO, the myoelectric untethered robotic glove. (Top Left) My-HERO provides five-finger extension and grip assistance and supports the wrist. (Top Right) My-HERO consists of an open-palm glove and foldable wrist brace secured in place with two Velcro straps. (Bottom) The two linear actuators mounted to the wrist brace attach to adjustable cable tie tendons for finger extension assistance and wire tendons sewn into the glove for grip assistance (highlighted in yellow in the top right figure). Mounted to the wrist brace is a 9 V battery and a Bluetooth microcontroller that communicates with an eight-channel electromyography armband that is used to detect the user’s intent.
My-HERO addresses these requests by:
Adding wire tendons for ring and little finger flexion and thumb adduction to provide palm curvature and greater grip force
Integrating an untethered EMG recording device and a myoelectric calibration and control algorithm with the robotic glove for muscle-initiated assistance
My-HERO uses the same foldable wrist brace design as the HERO Grip Glove, so that the wrist is supported and the same donning technique of inserting the thumb and then each individual finger can be used for flaccid and clenched hands.9 The battery pack (9 V Energizer Lithium battery) and Bluetooth-enabled microcontroller (tinyTILE Intel Curie) are relocated to the proximal end of the wrist brace for improved aesthetics and to reduce the arm torque required to lift the glove. A size medium glove is used to provide better fit on the thumb. Right and left-handed robotic gloves were manufactured. The total weight of My-HERO (consisting of the Thalmic Labs Myo Armband and the robotic glove with the battery included) is 377 g. The armband’s EMG, acceleration and orientation data are transmitted through Bluetooth to a laptop computer at 200 Hz to create a dataset of stroke participants’ forearm muscle and motion signals during hand function assessments and daily living tasks. The computer detects the user’s intent from the EMG data. The computer uses Cloud and Bluetooth protocols to communicate with the on-board microcontroller, which commands the actuators to move to a fully extended or fully retracted position using a 50 Hz pulse-width modulation signal, with a delay less than 0.5 seconds. The software for the computer program, app and glove is available in the Supplementary Materials.
Myoelectric control
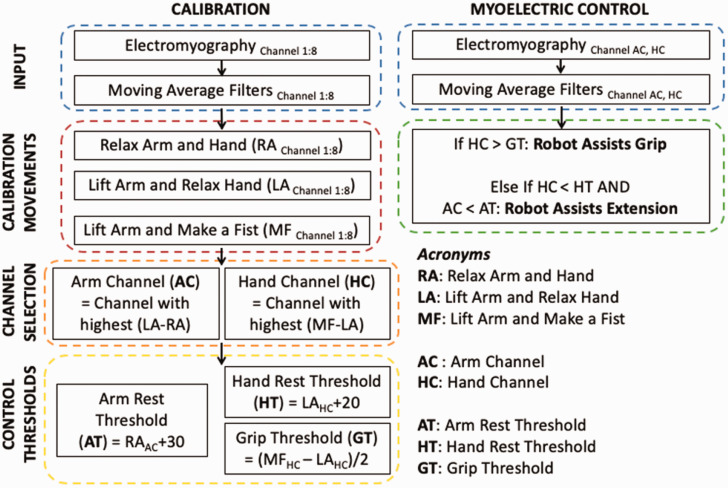
The myoelectric control algorithm calibrates automatically, then detects the user’s intent to grasp or release and commands My-HERO to assist grip or extension. The myoelectric control algorithm, shown in Figure 2, was motivated by a previous study with a robotic glove where people with limited or no finger extension after stroke generated EMG signals while grasping objects.23
Figure 2.
Myoelectric calibration and control algorithm used to control My-HERO. Users activate their forearm flexor muscles to trigger grip assistance and relax their hand and arm to trigger hand extension. In this way, people after stroke without forearm extensor muscle activation or selective activation of forearm flexor muscles can grasp and release objects of a variety of shapes and sizes.
There were three major challenges in designing an appropriate myoelectric control scheme. First, people without active finger extension after stroke often generate no observable EMG signal while attempting to extend their fingers. For example, EMG signals collected from our study participants are shown in Supplementary Figure S1. Second, their arm motions generate large EMG signals on multiple armband channels, so reaching for an object would trigger the glove to close before the user could accurately position their hand around it. Third, maintaining a grip EMG signal for more than five seconds was fatiguing, causing users to drop objects midair.
The proposed myoelectric algorithm resolves the challenges discussed above. Throughout calibration and robot control, an electrode-specific moving averaging filter with a window of 250 ms (i.e. summing the absolute values of 50 consecutive data points) was used, as in.20 Inertial measurement unit (IMU) data was not used. The user is seated at a table with their affected forearm and hand resting on the table. They are asked to follow an automated set of text instructions, which display consecutively on the computer screen for 10 seconds. The instructions were also read aloud and demonstrated by a researcher because the user interface was not optimized for visual, cognitive or other impairments. The first on-screen instruction is for the user to “relax your arm and hand” and the following instructions are “lift your arm and relax your hand” and “lift your arm and make a fist”. Users were free to choose how they lifted their forearm off of the table, regardless of if this included shoulder internal rotation or elbow flexion. The last 5 seconds of data under each condition are averaged to automatically find the electrode most sensitive to hand gripping relative to arm motion (Hand Channel), the electrode most sensitive to arm motion (Arm Channel) and the corresponding thresholds for arm relaxation (Arm Rest Threshold), hand relaxation (Hand Rest Threshold) and hand grasping (Grip Threshold). To trigger hand extension assistance, the user relaxes their shoulder, elbow and hand muscles so that the EMG signals on the Arm Channel and Hand Channel are below the Arm Rest Threshold and Hand Rest Threshold. To trigger grip assistance, the user attempts to grasp an object so that the EMG signal on the Hand Channel increases above the Grip Threshold. The user can keep hold of the object in two ways: by maintaining a small hand EMG signal or by keeping their arm lifted. To release the object the user again relaxes their shoulder, elbow and hand muscles. Moving the arm without attempting to grasp does not trigger grip assistance. Powering My-HERO off and then back on retracts both actuators, bringing the robot to its slack position.
Our control algorithm does not require the Myo armband to be positioned in a specific orientation, but for the purpose of creating a usable dataset with standardized conditions the armband was positioned so its illuminated logo was centered on the dorsal side of the forearm with the horizontal light closest to the distal end. The Myo armband enters sleep mode and stops recording data if the user does not synchronize it within one minute of putting it on. The study participants were able to produce the EMG output required to synchronize with the armband by activating their flexor synergy for approximately five seconds. Two additional participants (P10 and P11) with a CMSA - Stage 1 of Arm and CMSA - Stage 1 of Hand were recruited but excluded from this study because the Myo Connect software did not recognize their attempts to synchronize the armband.
Study procedures
Participants
A convenience sample of people in the chronic phase after stroke was recruited by therapist referral.
Inclusion criteria
People over 6 months post-stroke
Chedoke-McMaster Stroke Assessment (CMSA) – Stage of Hand24 between 1 and 4, inclusive (moderate to severe hand impairment)
Participant produces the required EMG output to synchronize the EMG armband with the computer
Study design
This study was approved by the University Health Network Institutional Review Board #16-6198. The study used a pre-post crossover design. The authors administered the study methods for all stroke participants after being trained by an occupational therapist.
Each participant provided informed consent to participate in the study. Each participant completed the Fugl-Meyer Assessment–Hand (FMA-Hand)25 and the Chedoke Arm and Hand Activity Inventory (CAHAI-13)26 to evaluate how well they could perform standardized hand function and daily living task assessments with and without My-HERO. The participants were randomized so that half completed the FMA-Hand and CAHAI-13 assessments using the glove and then without wearing the glove and the other half completed these assessments first without wearing the glove, to minimize training and fatigue biases. Each assessment was administered and scored by the authors during the study and the scores were reviewed for correctness using the video recordings. No training period was completed prior to these assessments. The Quebec User Evaluation of Satisfaction with Assistive Technology Version 2.0 (QUEST)27 and Usefulness, Satisfaction and Ease of Use questionnaire (USE)28 were completed by the participants directly after using My-HERO to reduce memory effects. The participants were scheduled on a day when they did not have therapy. The study was a single session of 2 hours.
Outcome measures descriptions
The FMA-Hand is a standardized assessment comprised of seven hand motions or grasps, each scored as 0 (unable to perform), 1 (partially performs) or 2 (fully performs), for a total score out of 14.25 The seven tasks evaluate how well the participant is able to flex their hand from an extended position, extend their hand from a flexed position, demonstrate a hook grasp, and forcefully grasp paper, a pencil, a small can and a tennis ball using key, tripod, cylindrical and spherical grips. This assessment was chosen because it evaluates how well the glove’s assistance immediately remediates impaired hand function. The FMA-UE was not used because it could not be completed for each participant within their study session timeframe. The FMA-Hand has been used in stroke rehabilitation studies to measure hand function pre- and post-therapy and with and without robotic assistance.8,29,30
The FMA-Hand was also used in this study to assess how well people after stroke were able to control the glove to apply finger extension and grip assistance. For each of the seven tasks, the researcher verbally commanded the participants to grip, hold the grip and then relax their hand. The audio-visual recordings were synchronized with the computer’s data recordings and the time that elapsed between the verbal command and the glove’s motors initiating assistance was recorded as the intent detection time.
The CAHAI-13 is a stroke-specific standardized assessment comprised of 13 bimanual daily living tasks, each scored from 1 (affected hand does not contribute in the task) to 7 (the task is performed safely, without modification, assistive devices or aids including My-HERO, and within reasonable time), for a total score out of 91 and a minimum score of 13.26 The thirteen tasks evaluate how well the affected arm and hand contribute to opening a jar, using a telephone, drawing a line with a pencil and ruler, pouring a glass of water, wringing out a washcloth, doing up five buttons, drying their back with a towel, putting toothpaste on a toothbrush, cutting with a fork and knife, using a zipper, cleaning eyeglasses, picking up a container and carrying a weighted bag. This assessment was chosen because it evaluates how well the glove enables people after stroke to incorporate their affected upper extremity into daily living tasks that they practice during therapy and may perform with My-HERO when using it at home. For cleanliness and safety, the washcloth was not wetted, the container was empty, and the weighted grocery bag was instructed to be grasped and lifted from the floor to the table by the affected hand but not carried up any stairs.
The QUEST is a standardized questionnaire that is comprised of 12 Likert scale questions, each scored from 1 (not satisfied at all) to 5 (very satisfied).27 In this study, 8 of the 12 questions were used since the other 4 questions apply to services provided with an assistive device. This usability assessment was chosen because its feedback directly informs engineering specifications (i.e. dimensions, weight), directly assesses ease of use, comfort and effectiveness and requires the user to select the most important satisfaction items.
The USE is a standardized assessment comprised of 30 questions each scored from 1 (strongly disagree) to 7 (strongly agree) and is used to understand stroke participants’ perspectives on the device’s usefulness, ease of use, ease of learning and satisfaction.28 Additional questions were asked about the stroke participants’ interest in purchasing the device, as in Yap et al.,10 and about their interest in using the device in the clinic and at home for exercise and throughout their daily routines.
Data analysis
The Shapiro-Wilk test was used to evaluate if the FMA-Hand, CAHAI-13, QUEST and USE datasets were normally distributed (α = 0.05).7 The participants’ summated FMA-Hand, CAHAI-13, QUEST and USE questionnaire scores were all normally distributed so their means are reported and a paired t-test was used to determine if the with glove versus without glove comparisons were statistically significant (α = 0.05).31,32
Results
Participants
Nine people with chronic severe hand impairment after stroke completed the Fugl-Meyer Assessment-Hand (FMA-Hand) and Chedoke Arm and Hand Activity Inventory-13 (CAHAI-13) with and without My-HERO. The participants ranged in age (between 35 to 85 years), time since stroke (10 months to 34 years) and hemiparetic side. Each participant could initiate shoulder flexion and elbow flexion and extension (Chedoke McMaster Stroke Assessment (CMSA)-Stage of Arm 2 to 7, out of 7). Each participant, except P1, could initiate finger flexion and P1 had preserved finger flexion reflexes even though he could not move the hand (CMSA-Stage of Hand 2 to 3, out of 7). Six participants (P1, 2, 3, 4, 5, 9) could not extend any fingers without assistance and the other three participants could not extend either the thumb or the index finger. Five participants (P2, 3, 4, 5, 8) had clenched hands and considerable flexor tone that resisted passive finger extension. Further details of the participants’ demographics and hand and arm function are provided in Table 1.
Table 1.
Demographics and hand and arm function of participants after stroke.
| Participant | Time since stroke | CMSA - Hand | CMSA - Arm | Affected/dominant hand | Gender | Age (years) |
|---|---|---|---|---|---|---|
| P1 | 10 mo | 2 | 2 | R/R | M | 48 |
| P2 | 1yr, 9 mo | 2 | 2 | R/R | M | 52 |
| P3 | 2yr, 2 mo | 2 | 2 | L/R | M | 65 |
| P4 | 3yr, 10 mo | 2 | 2 | L/R | M | 59 |
| P5 | 26yr, 4 mo | 2 | 2 | L/R | F | 71 |
| P6 | 17yr, 3 mo | 2 | 7 | L/L | F | 50 |
| P7 | 8yr, 1 mo | 3 | 3 | L/R | M | 58 |
| P8 | 34yr, 11 mo | 3 | 3 | L/R | M | 85 |
| P9 | 16yr, 8 mo | 3 | 4 | L/R | M | 35 |
Demographics and hand and arm function of participants after stroke. The participants are ordered according to their level of hand function, then arm function, then time since stroke. The Chedoke McMaster Stroke Assessment (CMSA) Stage of Arm (CMSA-Arm) and CMSA-Hand measure the level of motor recovery in the affected arm and hand, each scored on a scale from 1 to 7. Breakdown of the CMSA scoring metric: 1 – flaccid paralysis, 2 – spasticity is present and is felt as a resistance to passive movement, no voluntary movement is present but a faciftory stimulus will elicit the limb synergies reflexly, 3 – spasticity is marked and synergistic movements can be elicited voluntarily, 4 – spasticity decreases and synergy patterns can be reversed if movement takes place in the weaker synergy first, 5 – spasticity wanes, but is evident with rapid movement and at the extremes of range, 6 – coordination and patterns of movement are near normal, 7 – normal.
Accurate intent detection using EMG
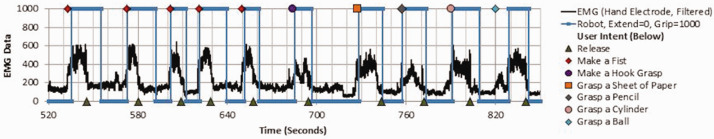
The intent detection time was specified as the time from the researcher’s verbal command for the participant to “grasp” or “release” to My-HERO’s activation of grip or extension assistance. My-HERO was 84.7% (SD 10.8) accurate in detecting the users’ intent and triggering grip or extension assistance within a five second period after the corresponding verbal command. Five seconds was long enough for the user to process the verbal command, reposition if needed and initiate an intent, but short enough that the robot responded as the user expected and the user did not initiate a second grasp attempt. The average time from the researcher’s verbal “grasp” or “release” command to My-HERO’s initiation of grip or extension assistance was 2.2 s (SD 0.7) and 3.7 s (SD 1.9). Triggering extension assistance required more time than grip assistance because the user had to concentrate on relaxing their shoulder, elbow and hand as opposed to initiating their forearm flexors. False positives did not occur often, with grip assistance incorrectly triggered on 4.3% of the occasions where the participant was instructed to maintain their hand in extension and extension assistance incorrectly triggered on 2.8% of the occasions where the participant was instructed to maintain a grip. Further details on the intent detection accuracy are shown in Table 2. The EMG waveforms and intent predictions from P1 (participant with no active finger flexion or extension) are shown in Figure 3. The EMG, acceleration and orientation dataset for all participants, collected during the FMA-Hand and CAHAI-13 with and without the glove, is available in the Supplementary Materials. No objects were released while the arm was lifted, during both the FMA-Hand and CAHAI-13. P5 and P8 were the first two study participants and required manual tuning of the constant values that were added to the myoelectric controller’s thresholds prior to the FMA-Hand, since it was difficult for them to trigger robot extension otherwise. Similar constant values to those used for P5 and P8 were chosen (i.e. Control thresholds of +30 and +20 in Figure 2) and remained unchanged for the remainder of the study participants.
Table 2.
Intent detection accuracy of the myoelectric controller.
| Participant | Intent detection accuracy (%) | Average time to detect grip (s), (SD) | Average time to detect release (s), (SD) | False positives: grip triggered (%), extension triggered (%) |
|---|---|---|---|---|
| P1 | 75.0 | 2.8, (2.5) | 6.2, (4.1) | 0, 0 |
| P2 | 69.6 | 2.5 (1.6) | 7.0, (2.4) | 0, 8.3 |
| P3 | 89.5 | 2.8 (2.0) | 2.1, (2.2) | 0, 0 |
| P4 | 95.0 | 1.8 (0.6) | 2.6, (3.0) | 30, 0 |
| P5 | 100.0 | 1.8 (1.0) | 1.7, (1.2) | 0, 0 |
| P6 | 94.1 | 0.9 (0.6) | 2.3, (2.5) | 0, 0 |
| P7 | 87.5 | 2.1 (2.6) | 2.9, (3.4) | 0, 10 |
| P8 | 75.0 | 3.2 (2.6) | 3.7, (3.2) | 0, 0 |
| P9 | 76.9 | 2.0 (1.4) | 4.5, (4.9) | 8.3, 7.1 |
| Mean (SD) | 84.7 (10.8) | 2.2 (0.7) | 3.7 (1.9) | 4.3 (SD 10.0), 2.8 (SD 4.3) |
Figure 3.
User intent versus robot assistance during the Fugl-Meyer Assessment-Hand. The myoelectric controller detects the user’s intent to grasp and release objects and triggers My-HERO to provide hand grip or extension assistance. This figure shows the timing of the verbal commands given to Participant 1 to grip or release, which signify his intents during the Fugl-Meyer Assessment-Hand tasks. The timing of the robot’s initiation of grip or extension assistance and the filtered EMG signal (i.e. summing the absolute values of 50 consecutive signals) from the Hand Channel are shown. This data was used in determining the accuracy of the myoelectric controller’s intent detection algorithm. For this participant, nine of ten grip intents and six of ten extension intents were correctly detected within 5 seconds of the verbal command (i.e. ball grasp delayed at 820 s; release delayed at 546 s, 580 s, 628 s, 802 s) and My-HERO was successfully triggered to assist him during each daily task.
My-HERO enhances hand function and performance of daily living tasks
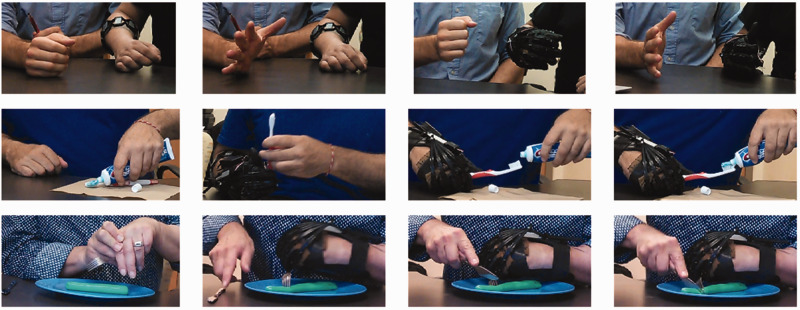
All nine participants scored higher on the FMA-Hand while using My-HERO and the average score increase was 8.4 points (SD 2.1, p < 0.01). All nine participants surpassed the established clinically meaningful significant difference threshold of 4.25 points while using My-HERO.33 The FMA-Hand results are shown in Table 3. The robot improved mass finger extension for each participant, whether the hand was flaccid or presented with high flexor tone and spasticity. The wrist brace held the wrist in a neutral position. With My-HERO, each participant could extend all five fingers further and hold the paper, pencil and cylinder securely. With My-HERO, eight participants could grasp the ball, but only three could hold the ball securely because the palmar linear actuator and palmar aspect of the wrist brace interfered with holding the ball. No participants could create a hook grip with My-HERO because its underactuated extension mechanism extends each finger joint. Only one participant could create a partial hook grip without My-HERO. Without My-HERO, most participants could not create the hand extension required for the starting position of any grip task and scored zero on these tasks as a result. The participants with clenched hands could hold the paper, cylinder and ball securely once the researcher positioned their fingers over the object; however, this required considerable force and the objects could not be released.
Table 3.
Hand function and daily living task assessments with and without robot assistance from My-HERO.
| Participant | FMA-Hand | FMA-Hand with My-HERO | Δ FΜΑ-Ηand | CAHAI-13 | CAHAI-13 with My-HERO | Δ CAHAI-13 |
|---|---|---|---|---|---|---|
| P1 | 0 | 11 | 11 | 22 | 36 | 14 |
| P2 | 2 | 11 | 9 | 26 | 37 | 11 |
| P3 | 2 | 12 | 10 | 25 | 34 | 9 |
| P4 | 2 | 7 | 5 | 30 | 31 | 1 |
| P5 | 2 | 12 | 10 | 18 | 24 | 6 |
| P6 | 2 | 8 | 6 | 54 | 64 | 10 |
| P7 | 4 | 11 | 7 | 38 | 39 | 1 |
| P8 | 3 | 11 | 8 | 24 | 25 | 1 |
| P9 | 2 | 12 | 10 | 38 | 59 | 21 |
| Mean (SD) | 2.1 (1.1) | 10.6 (1.8) | 8.4 (2.1), p < 0.01 | 30.6 (11.1) | 38.8 (13.9) | 8.2 (6.8), p < 0.01 |
Fugl-Meyer Assessment-Hand (FMA-Hand) and Chedoke Arm and Hand Activity Inventory-13 (CAHAI-13) results with and without robot assistance. For the FMA-Hand participants attempted to flex all their fingers to make a fist, then extend all their fingers, then make a hook grasp. Participants then attempted to hold a sheet of paper, a pencil, a cylinder and a ball securely against gravity and then against a tug. Breakdown of the FMA-Hand scoring metric: 0 - not able to complete, 1 – partially able to complete, 2 – able to fully complete; total score out of 14.
For the CAHAI-13, participants attempted to complete thirteen standardized functional activities while attempting to meaninfully incorporate their affected upper extremity. Breakdown of the CAHAI scoring metric: 1 – not able to use affected hand, 2 – able to stabilize the object with the affected hand and complete the task with physical assistance, 3 – able to stabilize and manipulate the object with the affected arm and hand with physical assistance, 4 – all components completed with the affected hand with only light touch assistance, 5 – all components completed with only verbal cueing and help donning additional orthoses, 6 – all components completed without assistance, but with support from assistive devices (e.g. glove), 7 – all components completed safely, quickly, and smoothly; total score out of 91 (minimum of 13).
All nine participants scored higher on the CAHAI-13 while using My-HERO and the average score increase amongst all participants was 8.2 points (SD 6.8, p < 0.01). Five of the nine participants surpassed the clinically meaningful important difference threshold of 6.3 points while using My-HERO.26 The CAHAI-13 results are shown in Table 3. With My-HERO, the average performance increased on all thirteen tasks (listed in terms of the affected hand’s typical contribution): reaching and grasping the jar, reaching and grasping the phone, grasping, positioning and stabilizing the ruler, holding the cup, holding the washcloth stable while it was twisted, stabilizing the shirt while the buttons were done up, holding the towel end, holding the toothbrush while toothpaste was applied, holding the fork to stabilize food, holding the coat end while the zipper was aligned and pulled, holding and lifting the eyeglasses, holding and lifting the container with both hands and holding and lifting the weighted grocery bag with the affected hand. With My-HERO, participants were able to complete an average of 3 (SD 2) additional tasks while incorporating their affected hand and could simply reach out and grasp objects without wrestling them into their clenched hand. Notably, My-HERO enabled six participants to dry their back, five participants to cut food, and two participants to hold a weighted grocery bag, a cup, eyeglasses, clothing and a toothbrush in their affected hand. Both hand extension and grip force assistance were key to performing tasks more independently because with extension assistance the objects did not need to be interposed by the other hand and with grip strength users were able to hold objects that were tugged, twisted and weighted. The affected hand was most often used for grasping, lifting and stabilizing objects, while the other hand was most often used for the task components requiring dexterous finger and wrist manipulation. Performance scores were lowest for opening the heavy and slippery 8.6 cm width glass coffee jar, which was the largest diameter object, because participants required greater thumb abduction assistance and control over the amount of force applied. Images captured during the FMA-Hand and CAHAI-13 are shown in Figure 4.
Figure 4.
Daily living tasks performed without and with My-HERO. (Left) Participants performing tasks without My-HERO and (Right) while using My-HERO. (Top) P1 is unable to perform mass hand flexion and mass hand extension unassisted. With My-HERO’s assistance, P1 can open and close his hand. (Middle) P2 attempts to apply toothpaste one-handed but the toothbrush tips over. Using My-HERO, P2 is able to hold the toothbrush while applying toothpaste. (Bottom) P3 cannot grip a fork with his affected hand despite numerous attempts to position the fork with the unaffected hand. Using My-HERO, P3 is able to hold the fork and use it to stabilize his food while cutting it with a knife.
My-HERO satisfies usability needs of most participants after stroke
Four participants were ‘quite satisfied’ with My-HERO (rating over 80% of scale), three participants were ‘more or less satisfied’ (rating over 60%) and two participants were ‘not very satisfied’ (rating over 40%), as assessed using QUEST. Weight and safety and security were given average ratings above 80%, ease of use, durability and comfort were given average ratings above 70%, and size, ease of adjusting and effectiveness were given average ratings above 60%. Interestingly, the participants had varied opinions on which were the three most important features, with 6 participants selecting ease of use, 6 selecting effectiveness, 5 selecting comfort, 3 selecting adjustability and 2 selecting weight.
Each participant’s overall score, as a percentage, was similar between USE and QUEST. The results from the QUEST, USE and additional questions are shown in Tables 4 and 5. P5 and P8 did not complete USE because they had reached the end of the two-hour study period. The average USE rating was 76% (SD 8.8) and the scores for Usefulness, Ease of Use, Ease of Learning and Satisfaction all averaged above 70%. Scores above 70% generally mean that the device will be accepted in the field.17
Table 4.
My-HERO - Quebec User Evaluation with Assistive Technology version 2.0 (QUEST).
| Participant | Size | Weight | Ease of donning | Safe and secure | Durability | Ease of use | Comfort | Effective | Overall average |
|---|---|---|---|---|---|---|---|---|---|
| P1 | 3 | 3 | 3 | 4 | 4 | 3 | 4 | 3 | 3.38 |
| P2 | 5 | 5 | 3 | 5 | 5 | 5 | 5 | 4 | 4.63 |
| P3 | 5 | 5 | 4 | 5 | 4 | 4 | 4 | 4 | 4.38 |
| P4 | 4 | 4 | 5 | 4 | 3 | 4 | 4 | 4 | 4.00 |
| P5 | 2 | 3 | 2 | 4 | 3 | 2 | 3 | 2 | 2.63 |
| P6 | 2 | 3 | 4 | 4 | 4 | 4 | 4 | 4 | 3.63 |
| P7 | 4 | 5 | 4 | 4 | 4 | 4 | 4 | 4 | 4.13 |
| P8 | 2 | 5 | 2 | 4 | 2 | 1 | 2 | 2.57 | |
| P9 | 2 | 3 | 4 | 4 | 2 | 4 | 4 | 3.5 | 3.31 |
| Mean (SD) | 3.2 | 4 | 3.4 | 4.2 | 3.6 | 3.6 | 3.7 | 3.4 | 3.63 (0.73) |
Quebec User Evaluation with Assistive Technology Version 2.0 (QUEST) results. Breakdown of the QUEST Likert-scale questionnaire scores: 1 – not satisfied at all, 2 – not very satisfied, 3 – more or less satisfied, 4 – quite satisfied, 5 – very satisfied.
Bold values represent: Overall average sum of all the previous values.
Table 5.
My-HERO - Usefulness, Ease of Use and Satisfaction (USE) and Desire to Use questionnaires.
| Participant | Useful-ness | Ease of use |
Ease of learning |
Satisfaction | Use overall average |
Desire to use in clinic |
Desire to use for home exercise |
Desire to use for daily routines |
Desire to purchase |
|---|---|---|---|---|---|---|---|---|---|
| P1 | 4.4 | 4.5 | 4.8 | 4.3 | 4.5 | 4 | 6 | 6 | 5 |
| P2 | 4.1 | 5.6 | 6.8 | 6.1 | 5.5 | 7 | 7 | 7 | 7 |
| P3 | 6.1 | 5.7 | 5.8 | 6.6 | 6.0 | 7 | 7 | 7 | 6 |
| P4 | 5.3 | 4.9 | 5.0 | 5.4 | 5.1 | 6 | 7 | 7 | 6 |
| P5 | n/a | n/a | n/a | n/a | n/a | 2 | 1 | 2 | 1 |
| P6 | 4.1 | 5.3 | 7.0 | 6.0 | 5.4 | 7 | 7 | 5 | 7 |
| P7 | 7.0 | 4.8 | 6.8 | 6.1 | 6.0 | 7 | 7 | 7 | 5 |
| P8 | n/a | n/a | n/a | n/a | n/a | 1 | 1 | 1 | 1 |
| P9 | 4.4 | 4.5 | 5.0 | 4.6 | 4.6 | 6 | 6 | 3 | 3 |
| Mean (SD) | 5.1 | 5.1 | 5.9 | 5.6 | 5.3 (0.6) | 5.2 | 5.4 | 5.0 | 4.6 |
Usefulness, Ease of Use and Satisfaction (USE) and Desire to Use questionnaire results. The USE questionnaire has 8 questions regarding Usefulness, 11 questions regarding Ease of Use, 4 questions regarding Ease of Learning and 7 questions regarding Satisfaction. Breakdown of the Likert-scale USE questionnaire and additional questions regarding Desire to Use and Desire to Purchase: 1– strongly disagreee, 7– strongly agree. P5 and P8 did not complete the USE questionnaire because the two-hour study period had elapsed.
Bold values represent USE overall average sum of all the previous values.
P2 said “I’ve never been able to do this” while holding the toothbrush. P9 wrote that the “Grip strength is good. [I] like the sensor for the nerves”. P6 wrote “It was like exercise for my hand and finger. I liked and enjoyed working with that”.
The participants that were quite satisfied or more or less satisfied with My-HERO (QUEST rating over 60%) desired to use My-HERO in a rehabilitation clinic and at home for exercises and assistance during their daily routines. They desired to purchase My-HERO, and the median cited cost they were willing to pay was $200 CAD. No apparent differences were seen between participants that performed the assessments using the glove first versus without the glove first.
Each participant donned the armband within two minutes and the glove within five minutes, with assistance from one researcher. Each participant doffed the glove and armband independently within 2 minutes. The participants’ main feedback was that the glove should be tailored to the shape and size of the individual’s hand, that greater thumb abduction assistance and reduced material at the palm would make it easier to grasp large objects and that providing support for wrist supination would help in properly orienting the hand for a grasp. The participants appreciated that My-HERO was untethered as they were not wheelchair users and desired to use My-HERO during daily routines. They were satisfied with the ease of use of the myoelectric control algorithm and perceived that this control mode would be useful for exercising and rehabilitating the hand as well as for assistance to incorporate the affected hand in daily routines. After using My-HERO, they were satisfied that the affected hand was now in a more extended and relaxed shape and that they had performed engaging hand exercises where they focused on initiating hand motion.
Discussion
This study demonstrates that myoelectric robotic gloves can enable people after stroke to integrate their affected hand meaningfully into daily living tasks and complete more tasks independently. The majority of participants were satisfied with My-HERO, desired to purchase it and found it to be useful and easy to use. Our developments and findings provide therapists and people after stroke with exciting opportunities for integrating myoelectric robotic gloves into their rehabilitation programs and daily routines.
Our novel contributions to the wearable robotics, stroke rehabilitation and assistive technology fields are:
My-HERO is a novel untethered robotic glove that supports the wrist, has no rigid joints, and assists five-finger extension, five-finger flexion, and thumb abduction, adduction and opposition
My-HERO integrates this robotic glove with an untethered EMG armband and uses a myoelectric control algorithm that calibrates automatically and uses hand flexion and hand and arm relaxation to enable people without hand extension after stroke to accurately trigger grip and hand extension assistance
For the first time:
Nine people with severe hand impairment after stroke performed standardized assessments of hand function (FMA-Hand) and bimanual daily living tasks (CAHAI-13) while using an untethered robotic glove
Nine people with severe hand impairment after stroke surpassed clinically meaningful important differences on the FMA-Hand and five surpassed clinically meaningful important differences on the CAHAI-13 while using a myoelectric untethered robotic glove
The usability of a myoelectric untethered robotic glove was evaluated by people after stroke using standardized satisfaction (QUEST) and usability (USE) questionnaires
A dataset of forearm electromyography, acceleration and orientation recordings from people with hand impairment after stroke was collected during the FMA-Hand and CAHAI-13 and is available to help advance rehabilitation engineering
People with severe hand impairment after stroke find myoelectric robotic gloves usable
This work builds on the research community’s efforts in designing stroke-specific myoelectric control algorithms and deploying myoelectric robotic hand orthoses to remediate abilities related to upper extremity impairment. We contribute a controller that can be used by people with severe hand impairment after stroke (i.e. without finger extension) in thirteen daily living tasks which involve standing and sitting and the arm to be lifted and at rest. The controller has a straightforward calibration and implementation for researchers to integrate when testing novel robot designs with people after stroke. Of particular interest, one of our participants was unable to produce finger flexion or extension motion yet was able to control My-HERO. The controller is intuitive to use since there was no training period, yet all participants were still able to control My-HERO during each assessment.
Our myoelectric control algorithm was 84.7% accurate in detecting the grip and release intents of people with limited or no hand extension after stroke. This work provides further evidence to,18,20,21 that showed that people could control a robotic hand orthosis after stroke with 83-85% accuracy using individually calibrated myoelectric control algorithms. We selected the grip-relax controller for ease of operation after considering the neuromuscular commonalities amongst our subset of the stroke population. We relied on the glove’s jointless actuation mechanism to conform to various object shapes. We hypothesize that the participants understood the control algorithm well, as we observed that they did not hesitate before activating the assistance and quickly corrected intent detection errors by griping stronger or relaxing further. We did not observe increases in EMG activity as My-HERO extended the relaxed hand, which provides initial evidence that hand robots do not elicit spastic responses when extending fingers that are flaccid or have high tone. We suspect that the control algorithm’s accuracy is not very sensitive to small changes in the thresholds (i.e. ±50% of the constant values chosen) since we did not need to modify the constant values after the first two participants. However, we did not evaluate this systematically and improvements in accuracy may be possible using machine learning. Further, our task set did not require movement throughout the entire shoulder, elbow, and wrist workspaces. A task-specific ‘arm channel’ selection algorithm could improve task performance for participants with arm control (e.g. CMSA- Stage of Arm of 4 and above) and it could be useful to disable the arm lift detection feature until muscle fatigue is detected. Our participants commonly used the robot-assisted hemiplegic hand as the supporting hand, where individual finger motion and grip force modulation is less important for task completion. However, combining dexterous robots, sensor fusion from IMU, force, bend and dense electromyography sensors on the forearm and hand, classification algorithms for controlling grasp type and force, and user training programs may enable people with hemiplegic hands to perform delicate tasks, in-hand manipulation and multiple tasks at once.34–37 We contribute a dataset from extension and flexion motions and daily living tasks with and without robot-assistance to inform the open-source development of novel myoelectric controllers, especially those that incorporate machine learning and reinforcement learning.
Robotic gloves enable independence in daily living tasks
Our results and Supplementary Video show how well users with stroke-affected shoulders, elbows, wrists and hands performed daily living tasks with and without My-HERO. Our stroke participants were quite satisfied with the robotic glove and were able to use their affected arm and hand meaningfully in daily living tasks with it. All participants surpassed established clinically meaningful important difference thresholds on the FMA-Hand. The FMA-Hand improvements were large for all participants since they could not extend their hand to the starting hand postures for the grasp tasks without assistance. This may make My-HERO an engaging and useful tool for whole-hand stretching and range of motion exercises to reduce contractures and tone, in comparison to exoskeletons that move only the index and middle finger8 or the index finger and thumb.4 The majority of participants surpassed clinically meaningful important difference thresholds on the CAHAI-13. The CAHAI-13 score improvements were greatest for participants with higher levels of arm function, yet those with lower levels of arm function were also satisfied with My-HERO, which supports previous observations.9 Further studies are required to compare if My-HERO’s underactuated whole hand movement assistance (i.e. finger extension and flexion, thumb abduction, adduction, and opposition, palm curvature) enables people after stroke to grasp more everyday objects and use neurotypical grasp postures more often (i.e. grasping a pencil with a tripod grasp, grasping a ball with a spherical grasp), in comparison to devices that actuate only select fingers.4,8,38 The participants that contributed low usability scores had their strokes over 20 years ago. They taught us how they modified tasks similar to the CAHAI-13 when performing them one-handed or with assistance at home. They were interested in using an improved version of the glove if it was affordable, aesthetically pleasing, fully extended all clenched fingers, fully abducted highly toned thumbs, did not obstruct the palm and could be donned independently on clenched hands. The main challenge to independent donning was in inserting a toned ring or little finger. This is an open challenge in full-hand robotic orthosis design that may be improved by incorporating Velcro straps as well as by providing donning training to the user and caregiver. Creating a robotic glove that meets all of these requests is an open challenge that robotic glove developers are working toward for people after stroke, muscular dystrophy and spinal cord injury.3,4,7,8,10,13,39–42 Our contribution to these works is a lightweight (377 g), myoelectric untethered robotic glove that supports extension and grip for all five fingers and is effective and usable as demonstrated by people with severe hand impairment after stroke on standardized assessments of hand function and performance on thirteen bimanual daily living tasks. These efficacious results motivate independent, multicenter controlled trials to be conducted to validate how well myoelectric untethered robotic gloves enable independence at home and stimulate neuromuscular recovery after stroke.
Conclusions
Considerations for using robotic gloves at home as assistive and rehabilitation devices
In future studies, it will be useful to integrate My-HERO with other technologies and interventions such as electroencephalography, arm supports, elbow and shoulder exoskeletons and functional electrical stimulation to reach higher performance levels on these daily living tasks and on activities of daily living. To adhere to users’ budgets while integrating these additional technologies, new methods for manufacturing, distributing, servicing and reimbursing assistive technologies will need to be created. We intend to integrate My-HERO into rehabilitation studies that are structured in a similar way to constraint-induced movement therapy protocols, but without constraining the unaffected upper extremity.43,44 These therapy protocols will have an in-clinic portion to repetitively practice incorporating the gloved hand into activities of daily living and therapy goals. These protocols will include a transfer package of prescribed home exercises and daily routines to complete using the gloved hand. Home exercises and daily routines incorporating user-initiated assistance from robotic gloves may enhance the promising recovery effects shown when robotic hand orthoses are used during in-clinic therapy.13–17 Before home studies can take place, we will need to make sure the user has the assistance or capability required to don the glove and we will need to create communications protocols for the EMG signals to command the glove without a computer intermediary. We will then be able to study how well people after stroke use My-HERO over multiple days in their home environment, how physical and mental fatigue and individual-specific daily routines affect the myoelectric controller’s accuracy, and how well rehabilitation programs that combine therapy and assistive technology enhance engagement, adherence, neuromuscular recovery and independence.
Supplemental Material
Supplemental material, sj-pdf-1-jrt-10.1177_2055668320964050 for Myoelectric untethered robotic glove enhances hand function and performance on daily living tasks after stroke by Aaron Yurkewich, Illya J Kozak, Andrei Ivanovic, Daniel Rossos, Rosalie H Wang, Debbie Hebert and Alex Mihailidis in Journal of Rehabilitation and Assistive Technologies Engineering
Supplemental material, sj-pdf-2-jrt-10.1177_2055668320964050 for Myoelectric untethered robotic glove enhances hand function and performance on daily living tasks after stroke by Aaron Yurkewich, Illya J Kozak, Andrei Ivanovic, Daniel Rossos, Rosalie H Wang, Debbie Hebert and Alex Mihailidis in Journal of Rehabilitation and Assistive Technologies Engineering
Acknowledgements
Special thanks go to the individuals who have experienced a stroke or spinal cord injury who tested and provided insights on My-HERO. Further acknowledgments go to the Intelligent Assistive Technology and Systems Lab (IATSL), Neil Squire Society – Makers Making Change, and occupational therapists Sylvia Haycock, Jaclyn Dawe and Lovely Chaudhary for their recommendations and feedback. Debbie Hebert was a lively and inspiring friend, mentor, educator and researcher that trained clinicians and researchers of many disciplines about the principles of occupational therapy and patient-centred care. She was a driving force behind the high-quality research and therapy provided at the University of Toronto and Toronto Rehabilitation Institute over the past 41 years and in the years to come.
Ethics approval and consent to participate: The study was approved by the University Health Network Institutional Review Board and all methods were carried out in accordance with the approved study protocol. The participants provided written informed consent before participation and consented to the publishing of their collected data.
Contributorship: AY and IJK designed the robotic glove. AY, AJI and DR designed the myoelectric controller and communications software. AY designed the experiment with suggestions and feedback provided by IJK, AI, DH, RHW and AM. AY and IJK conducted the experiment and analyzed and interpreted the data. AY prepared the manuscript with critical feedback provided by IJK, DH, RHWand AM. IJK and AY developed the video and dataset. All authors approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the University of Toronto, Toronto Rehabilitation Institute (TRI), Natural Sciences and Engineering Research Council of Canada (NSERC), Canadian Partnership for Stroke Recovery (CPSR), European Commission under grant H2020 ICT 871767 REHYB, India Canada-IMPACTS Networks of Centres of Excellence (NCE) and AGE-WELL NCE Inc.
ORCID iD: Aaron Yurkewich https://orcid.org/0000-0002-5168-8146
Supplemental material: Supplemental material for this article is available online.
Data and materials availability
The following Supplementary Materials are available at:https://github.com/AYurkewich/My-HERO
Datasets of EMG, acceleration and orientation recorded during the FMA-Hand and CAHAI-13 assessments
Python software for recording the Myo armband data and detecting the user’s intent
Android software for communicate between Python and the robotic glove
Arduino software used on-board the robotic glove
Supplementary Movie S1 and Supplementary Figure S1
References
- 1.Bernstein R. Nearly 1 in 5 people have a disability in the U.S. Suitland: US Census Bureau Reports, 2012, pp. 1–2.
- 2.Bos RA, Haarman CJW, Stortelder T, et al. A structured overview of trends and technologies used in dynamic hand orthoses. J Neuroeng Rehabil 2016; 13: 62 http://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-016-0168-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yurkewich A, Hebert D, Wang RH, et al. Hand extension robot orthosis (HERO) glove: development and testing with stroke survivors with severe hand impairment. IEEE Trans Neural Syst Rehabil Eng 2019; 27: 916–926. [DOI] [PubMed] [Google Scholar]
- 4.Soekadar SR, Witkowski M, Gómez C, et al. Hybrid EEG/EOG-based brain/neural hand exoskeleton restores fully independent daily living activities after quadriplegia. Sci Robot 2016; 1: eaag3296. [DOI] [PubMed] [Google Scholar]
- 5.Paley J, Eva G, Duncan EAS. In-order-to analysis : an alternative to classifying different levels of occupational activity. Br J Occup Ther 2006; 69: 161–168. [Google Scholar]
- 6.Kapadia N, Zivanovic V, Verrier M, et al. Toronto rehabilitation institute–hand function test: assessment of gross motor function in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil 2012; 18: 167–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cappello L, Meyer JT, Galloway KC, et al. Assisting hand function after spinal cord injury with a fabric-based soft robotic glove. J Neuroeng Rehabil 2018; 15: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peters HT, Otr L, Page SJ, et al. Giving them a hand : wearing a myoelectric elbow-wrist-hand orthosis reduces upper extremity impairment in chronic stroke. Arch Phys Med Rehabil 2017; 98: 1821–1827. [DOI] [PubMed] [Google Scholar]
- 9.Yurkewich A, Kozak IJ, Hebert D, et al. Hand extension robot orthosis (HERO) grip glove: enabling independence amongst persons with severe hand impairments after stroke. J Neuroeng Rehabil 2020; 17: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yap HK, Lim JH, Nasrallah F, et al. Design and preliminary feasibility study of a soft robotic glove for hand function assistance in stroke survivors. Front Neurosci 2017; 11: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gasser BW, Bennett DA, Durrough CM, et al. Design and preliminary assessment of vanderbilt hand exoskeleton. IEEE Int Conf Rehabil Robot 2017; 2017: 1537–1542. [DOI] [PubMed] [Google Scholar]
- 12.Taub E, Uswatte G, Bowman MH, et al. Constraint-induced movement therapy combined with conventional neurorehabilitation techniques in chronic stroke patients with plegic hands: a case series. Arch Phys Med Rehabil 2013; 94: 86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fischer HC, Triandafilou KM, Thielbar KO, et al. Use of a portable assistive glove to facilitate rehabilitation in stroke survivors with severe hand impairment. IEEE Trans Neural Syst Rehabil Eng 2016; 24: 344–351. [DOI] [PubMed] [Google Scholar]
- 14.Bernocchi P, Mulè C, Vanoglio F, et al. Topics in stroke rehabilitation home-based hand rehabilitation with a robotic glove in hemiplegic patients after stroke : a pilot feasibility study. Top Stroke Rehabil 2018; 25: 114–116. [DOI] [PubMed] [Google Scholar]
- 15.Susanto E, Tong RK, Ockenfeld C, et al. Efficacy of robot-assisted fingers training in chronic stroke survivors: a pilot randomized-controlled trial. J Neuroeng Rehabil 2015; 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu XL, Tong KY, Wei XJ, et al. The effects of post-stroke upper-limb training with an electromyography (EMG)-driven hand robot. J Electromyogr Kinesiol 2013; 23: 1065–1074. [DOI] [PubMed] [Google Scholar]
- 17.Radder B, Prange-Lasonder GB, Kottink AIR, et al. Feasibility of a wearable soft-robotic glove to support impaired hand function in stroke patients. J Rehabil Med 2018; 50: 598–606. [DOI] [PubMed] [Google Scholar]
- 18.Lee SW, Wilson K, Lock BA, et al. Subject-specific myoelectric pattern classification of functional hand movements for stroke survivors. IEEE Trans Neural Syst Rehabil Eng 2012; 100: 130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meeker C, Park S, Bishop L, et al. EMG pattern classification to control a hand orthosis for functional grasp assistance after stroke. In: IEEE International Conference on Rehabilitation Robotics Piscataway: IEEE, 2017, pp. 1203–1210. [DOI] [PubMed]
- 20.Park S, Meeker C, Weber LM, et al. Multimodal sensing and interaction for a robotic hand orthosis. IEEE Robot Autom Lett 2018; 4: 315–322. [Google Scholar]
- 21.Lu Z, Tong K-Y, Zhang X, et al. Myoelectric pattern recognition for controlling a robotic hand: a feasibility study in stroke. IEEE Trans Biomed Eng 2019; 66: 365–372. [DOI] [PubMed] [Google Scholar]
- 22.Polygerinos P, Galloway KC, Sanan S, et al. EMG controlled soft robotic glove for assistance during activities of daily living. In: 2015 IEEE International Conference on Rehabilitation Robotics Piscataway: IEEE, 2015, pp. 55–60.
- 23.Yurkewich A, Kozak IJ, Hebert D, et al. Do stroke survivors activate their muscles to supplement the Hand Extension Robot Orthosis (HERO) glove’s assistance. RehabWeek. 2019.
- 24.Miller P, Huijbregts M, Barreca C, et al. Chedoke-McMaster stroke assessment—development, validation and administration manual Hamilton: McMaster University, Tech Rep, 2nd ed., 2008, www.sralab.org/sites/default/files/2017- 07/CMSA Manual and Score Form.pdf
- 25.Page SJ, Levine P, Hade E. Psychometric properties and administration of the wrist/hand subscales of the Fugl-Meyer assessment in minimally-impaired upper extremity hemiparesis in stroke. Arch Phys Med Rehabil 2012; 93: 2373–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller P, Masters L, Gowland C, et al. Development of the Chedoke arm and hand activity inventory: theoretical constructs, item generation, and selection. Top Stroke Rehabil 2005; 11: 31–42. [DOI] [PubMed] [Google Scholar]
- 27.Demers L, Weiss-Lambrou R, Ska B. The Quebec user evaluation of satisfaction with assistive technology (QUEST 2.0): an overview and recent progress. TAD 2002; 14: 101–105. [Google Scholar]
- 28.Lund AM. Measuring usability with the USE questionnaire. Usability Interface 2001; 8: 3–6. [Google Scholar]
- 29.Sanford J, Moreland J, Swanson LR, et al. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther 1993; 73: 36–43. [DOI] [PubMed] [Google Scholar]
- 30.Thielbar KO, Triandafilou KM, Fischer HC, et al. Benefits of using a voice and EMG-driven actuated glove to support occupational therapy for stroke survivors. IEEE Trans Neural Syst Rehabil Eng 2017; 25: 297–305. [DOI] [PubMed] [Google Scholar]
- 31.Warmbrod JR. Reporting and interpreting scores derived from Likert-type scales. JAE 2014; 55: 30–47. [Google Scholar]
- 32.Xiloyannis M, Chiaradia D, Frisoli A, et al. Physiological and kinematic effects of a soft exosuit on arm movements. J Neuroeng Rehabil 2019; 16: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Page SJ, Fulk GD, Boyne P. Clinically important differences for the upper-extremity Fugl-Meyer scale in people with minimal to moderate impairment due to chronic stroke. Phys Ther 2012; 92: 791–798. [DOI] [PubMed] [Google Scholar]
- 34.Roche AD, Rehbaum H, Farina D, et al. Prosthetic myoelectric control strategies: a clinical perspective. Curr Surg Rep 2014; 2: 44. [Google Scholar]
- 35.Smurr LM, Gulick K, Yancosek K, et al. Managing the upper extremity amputee: a protocol for success. J Hand Ther 2008; 21: 160–176. [DOI] [PubMed] [Google Scholar]
- 36.Cordella F, Ciancio AL, Sacchetti R, et al. Literature review on needs of upper limb prosthesis users. Front Neurosci 2016; 10: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee SW, Wilson KM, Lock BA, et al. Subject-specific myoelectric pattern classification of functional hand movements for stroke survivors. IEEE Trans Neural Syst Rehabil Eng 2011; 19: 558–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Radder B, Prange-Lasonder GB, Kottink AIR, et al. The effect of a wearable soft-robotic glove on motor function and functional performance of older adults. Assist Technol 2020; 32: 9–15. [DOI] [PubMed] [Google Scholar]
- 39.Nycz CJ, Butzer T, Lambercy O, et al. Design and characterization of a lightweight and fully portable remote actuation system for use with a hand exoskeleton. IEEE Robot Autom Lett 2016; 1: 976–983. [Google Scholar]
- 40.Polygerinos P, Wang Z, Galloway KC, et al. Soft robotic glove for combined assistance and at-home rehabilitation. Rob Auton Syst 2015; 73: 135–143. [Google Scholar]
- 41.Ates S, Mora-Moreno I, Wessels M, et al. Combined active wrist and hand orthosis for home use: lessons learned. In: 2015 IEEE International Conference on Rehabilitation Robotics Piscataway: IEEE, 2015, pp. 398–403.
- 42.Rose CG, O'Malley MK. Hybrid Rigid-Soft hand exoskeleton to assist functional dexterity. IEEE Robot Autom Lett 2019; 4: 73–80. [Google Scholar]
- 43.Bowman MH, Taub E, Uswatte G, et al. A treatment for a chronic stroke patient with a plegic hand combining CI therapy with conventional rehabilitation procedures: case report. NeuroRehabilitation 2006; 21: 167–176. [PubMed] [Google Scholar]
- 44.Ward N, Brander F, Kate K. Intensive upper limb neurorehabilitation in chronic stroke: outcomes from the queen square programme. J Neurol Neurosurg Psychiatry 2019; 90: 498–506. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jrt-10.1177_2055668320964050 for Myoelectric untethered robotic glove enhances hand function and performance on daily living tasks after stroke by Aaron Yurkewich, Illya J Kozak, Andrei Ivanovic, Daniel Rossos, Rosalie H Wang, Debbie Hebert and Alex Mihailidis in Journal of Rehabilitation and Assistive Technologies Engineering
Supplemental material, sj-pdf-2-jrt-10.1177_2055668320964050 for Myoelectric untethered robotic glove enhances hand function and performance on daily living tasks after stroke by Aaron Yurkewich, Illya J Kozak, Andrei Ivanovic, Daniel Rossos, Rosalie H Wang, Debbie Hebert and Alex Mihailidis in Journal of Rehabilitation and Assistive Technologies Engineering