Abstract
Background:
Device utilisation ratios (DUR) correlate with device-associated complications and rates of infection. We implemented a hospital-wide Daily Interdisciplinary Safety Huddle (DISH) with infection control and device components. The aim of this study was to evaluate the impact of DISH on DURs and rates of infection for indwelling urinary catheters (IUC) and central venous catheters (CVC).
Methods:
A quasi-experimental study assessing DURs and rates of infection before and after implementation of DISH. At DISH, usage of IUC and CVC is reported by managers and the infection preventionist reviews indications and plans for removal. Data before and after implementation were compared. Paired T-test was used to assess for differences between both groups.
Results:
DISH was successfully implemented at a community hospital. The average DUR for IUC in intensive care unit (ICU) and non-ICU settings was reduced from 0.56 to 0.35 and 0.27 to 0.12, respectively. CVC DUR decreased from 0.29 to 0.26 in the ICU and 0.14 to 0.12 in non-ICU settings. Catheter-associated urinary tract infections (CAUTIs) decreased by 87% and central line-associated bloodstream infections (CLABSIs) by 96%.
Conclusion:
DISH was associated with hospital-wide reductions in DUR and device-associated healthcare-associated infections. Reduction of CLABSIs and CAUTIs had estimated cost savings of $688,050. The impact was more profound in non-ICU settings. To our knowledge, an infection prevention hospital-wide safety huddle has not been reported in the literature. DISH increased device removal, accountability and promoted a culture of safety.
Keywords: Catheter-associated urinary tract infection, central venous catheters, infection prevention, quality improvement, nosocomial infection, healthcare-associated infections, acute care, implementation science
Background
Healthcare-associated infections (HAIs) are preventable causes of morbidity and mortality in hospitalised patients (Centers for Disease Control and Prevention, n.d.). The Centers for Disease Prevention and Control (CDC), Infectious Diseases Society of America (IDSA) and Society of Healthcare Epidemiology of America (SHEA) have published evidence-based recommendations for the prevention of these nosocomial infections (Gould et al., 2010; Hooton et al., 2010; Lo et al., 2014; Marschall et al., 2014; O’Grady et al., 2011). The widespread implementation of these guidelines and strategies, along with increased awareness of human and financial cost of HAIs have led to a decline in incidence of HAIs over the past several years. Recent data have shown a decrease in central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI) (CDC, 2016). Between 2008 and 2014, there was a 50% decrease in CLABSIs, but no change in overall CAUTIs between 2009 and 2014 (CDC, 2016). Prevention strategies remain an important area of research and novel approaches must be investigated.
Interventions that increase provider awareness of devices and indications can impact device utilisation rates (DUR). Huddles have been shown to improve communication and accountability in multiple hospital settings, including operating rooms, emergency departments and intensive care units (ICU) (Criscitelli, 2015; Donnelly et al., 2017; Menon et al., 2017; Townsend et al., n.d.). A comprehensive hospital-wide Daily Interdisciplinary Safety Huddle (DISH) with components of infection prevention was implemented at an urban community hospital in January 2015. At this huddle, device census and plans for removal are reported by all hospital units. DISH serves as a forum to reinforce removal of devices when indications are no longer met. The aim of the present study was to evaluate the impact of this huddle on device utilisation and rates of infection for central venous catheters (CVCs) and indwelling urinary catheters (IUCs).
Methods
Study design and setting
We conducted a quasi-experimental study at a 151-bed community hospital. Our facility is a community teaching hospital located in the west side of Chicago that provides medical, surgical, paediatric and obstetrics-gynaecology inpatient services. Surveillance data before the implementation of DISH were reviewed, including DURs for IUCs and CVCs, along with CAUTI and CLABSI events reported to the CDC National Healthcare Safety Network (NHSN). Our pre-intervention period was from 1 January 2011 to 31 December 2014 and the post-intervention period was from 1 January 2015 to 31 December 2018.
Intervention
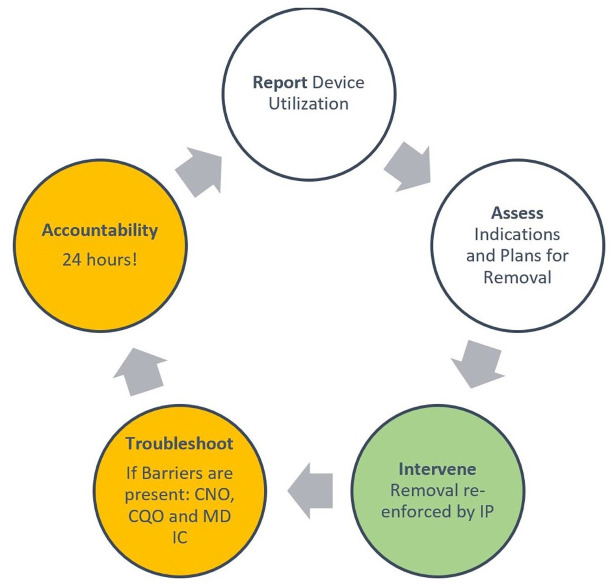
DISH is a 15-min meeting that occurs every morning at 08:00. Before the meeting, a data collection tool is used by the overnight shift to update isolation census and device census for CVCs and IUCs. Indications, duration and plans for removal are reported in the daily online survey (Table 1). This report is used at DISH. Representatives of all hospital units and departments participate at the hospital-wide huddle (Table 2). Individual unit leaders report the state of their unit, including key infection control (IC) variables such as isolation needs and daily use of CVCs and IUCs. The infection preventionist (IP) reviews indications, duration and plans for removal reported in the survey and at DISH for each device. The Ann Arbor Criteria for appropriate urinary catheter use guided IP recommendations for the use of IUCs, external urinary devices and removal of devices (Meddings et al., 2015). The Healthcare Infection Control Practices Advisory Committee recommendations were used for CVC maintenance and removal was advised when no clinical need for vasopressors, total parenteral nutrition or other caustic medications were needed (O’Grady et al., 2011). When removal of the device is recommended by IP, follow-up from the unit manager is required at the next DISH meeting. If barriers for removal are present, administration leaders present at the huddle—such as the Chief Quality Officer (CQO), Chief Nursing Officer (CNO) or the Medical Director of Infection Prevention—are involved in finding solutions (Figure 1). Resolution is expected by the next DISH session in 24 h.
Table 1.
Components of daily device survey.
| Daily online CVC survey | Daily online IUC survey |
|---|---|
| Present on admission (Yes or No) Date of placement Site Type of device Indication Plans for removal Barriers for removal if present |
Present on admission (Yes or No) Date of placement Type of device Indication Plans for removal Barriers for removal if present |
Table 2.
Participants at DISH.
| DISH participant | Role in DISH |
|---|---|
| Administrator on call | Performs roll call |
| Emergency room | Census and expected admissions |
| Medical-surgical units | Census, CVC, IUC, isolation census, fall risk, sitter and bed needs |
| Intensive care unit | Census, CVC, IUC, isolation census, fall risk, sitter and bed needs |
| Newborn | Census, CVC, IUC, isolation census, fall risk, sitter and bed needs |
| Paediatrics | Census, CVC, IUC, isolation census, fall risk, sitter and bed needs |
| Mother-baby unit | Census, CVC, IUC, isolation census, fall risk, sitter and bed needs |
| Psychiatry | Census, fall risk and bed needs |
| Operating room services | Census, types of procedures, bed needs |
| Discharge planning | Expected discharged before 11:00 |
| Laboratory | Active issues that may impact clinical services |
| Pharmacy | Active issues that may impact clinical services |
| Quality measures | Sepsis and ER throughput |
| Health information management | Missing documentation |
| Infection control | Reports CAUTI and CLABSI free days, along with any new initiative such as hand hygiene campaigns. Asks further questions on devices, recommending removal when indicated |
| Environmental services | Active issues |
| Facilities management | Active issues |
| Security | Active issues |
| Telecommunications | Active issues |
| Administrative leaders (Chief Quality Officer, Chief Nursing Officer, Medical Director of Infection Control) | Accountability and problem solving |
CAUTI, catheter-associated urinary tract infection; CLABSI, central line-associated bloodstream infection; CVC, central venous catheter; IUC, indwelling urinary catheter.
Figure 1.
Infection prevention components of the daily interdisciplinary safety huddle.
Data collection and analysis
DUR, calculated by dividing the number of device-days by patient-days per unit, and rates of CLABSI and CAUTI were compared before and after our comprehensive HAI reduction intervention. Contingency tables were constructed by individual unit and hospital-wide data. Statistical analysis using a paired T-test was performed to assess for statistical differences between the mean DURs before and after our interventions. Test statistics were considered significant if P values were < 0.05. Our study was reviewed and approved by the Institutional Review Board at the University of Illinois at Chicago.
Results
DISH with IC components was successfully implemented at our community hospital. There was a reduction in IUC and CVC DUR after the implementation of DISH in all hospital units. The mean DUR for IUC in the ICU was reduced from 0.56 to 0.35 (P = 0.01) and from 0.27 and 0.12 (P = 0.004) in non-ICU settings (Tables 3 and 4, Figures 2 and 3). These reductions in use of the IUC were statistically significant in each unit. The reduction in CVC DUR was not statistically significant. The rate of CAUTIs decreased from 1.27 to 0.16 per 1000 IUC days, corresponding to an 87% decrease. The only CAUTI in the post-intervention group occurred in the second quarter of 2016. Our facility has since remained free of CAUTIs. CVC DUR decreased from 0.29 to 0.26 (P = 0.59) in the ICU and 0.14 to 0.12 (P = 0.53) in non-ICU settings. CLABSI rates fell by 96%, from 3.66 to 0.16 per 1000 CVC days (Table 5). The only CLABSI in the post-intervention group occurred in the second quarter of 2016. Our facility has since remained free of CLABSIs.
Table 3.
Utilisation of devices in ICU settings before and after DISH.
| Year | IUC device-days | Patient-days | IUC utilisation rate | CVC device-days | Patient-days | CVC utilisation rate | |
|---|---|---|---|---|---|---|---|
| Before | 2011 | 2429 | 3531 | 0.69 | 1103 | 3531 | 0.31 |
| 2012 | 2074 | 3513 | 0.59 | 1016 | 3513 | 0.29 | |
| 2013 | 1458 | 2685 | 0.54 | 772 | 2665 | 0.29 | |
| 2014 | 1151 | 2594 | 0.44 | 669 | 2594 | 0.26 | |
| After | 2015 | 754 | 2010 | 0.38 | 658 | 2010 | 0.33 |
| 2016 | 934 | 1915 | 0.49 | 648 | 1915 | 0.34 | |
| 2017 | 1022 | 2907 | 0.35 | 731 | 2907 | 0.25 | |
| 2018 | 636 | 3277 | 0.19 | 472 | 3277 | 0.14 |
Table 4.
Utilisation of devices in non-ICU settings before and after DISH.
| Year | IUC device-days | Patient-days | IUC utilisation rate | CVC device-days | Patient-days | CVC utilisation rate | |
|---|---|---|---|---|---|---|---|
| Before | 2011 | 2429 | 7561 | 0.32 | 1103 | 7561 | 0.15 |
| 2012 | 2074 | 6470 | 0.32 | 1016 | 6470 | 0.16 | |
| 2013 | 1458 | 6006 | 0.24 | 772 | 6006 | 0.13 | |
| 2014 | 1151 | 5740 | 0.2 | 669 | 5740 | 0.12 | |
| After | 2015 | 1200 | 6695 | 0.18 | 1308 | 6695 | 0.2 |
| 2016 | 490 | 5587 | 0.09 | 547 | 5587 | 0.1 | |
| 2017 | 592 | 6854 | 0.09 | 796 | 6854 | 0.12 | |
| 2018 | 429 | 7587 | 0.06 | 517 | 7587 | 0.07 |
Figure 2.
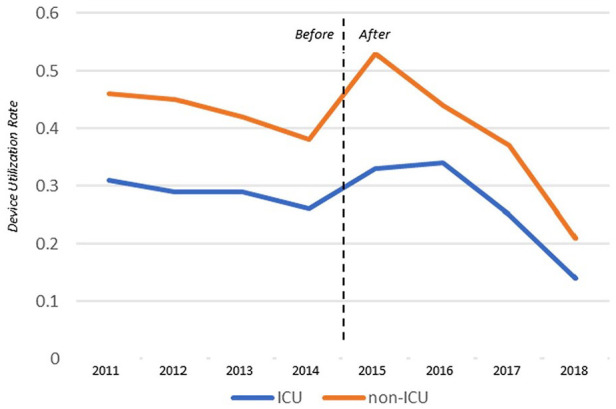
Device utilisation ratio for indwelling urinary catheters in ICU and non-ICU settings. ICU, intensive care unit.
Figure 3.
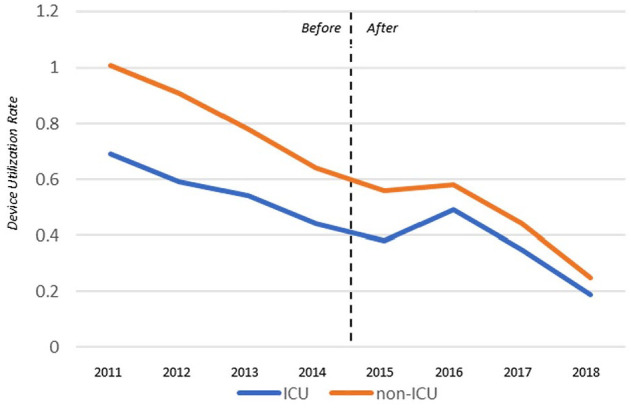
Device utilisation ratio for central venous catheters in ICU and non-ICU settings. ICU, intensive care unit.
Table 5.
Rates of hospital-acquired infections.
| CAUTI (n) | Rate | CLABSI (n) | Rate | |
|---|---|---|---|---|
| Before | 9 | 1.27/1000 IUC days | 13 | 3.66/1000 CVC days |
| After | 1 | 0.16/1000 IUC days | 1 | 0.16/1000 CVC days |
CAUTI, catheter-associated urinary tract infection; CLABSI, central line-associated bloodstream infection; CVC, central venous catheter; IUC, indwelling urinary catheter.
Discussion
A hospital-wide huddle with IC and device utilisation components was successfully implemented at a community hospital. DISH served as a forum for discussion of device removals and promotion of infection prevention priorities. Our hospital experienced a reduction in utilisation of devices after implementation of DISH, with more effect in non-ICU settings. There was a statistically significant reduction in utilisation of IUCs that led to an 87% reduction in CAUTIs. Despite a modest non-statistically significant decrease in CVC utilisation, a 96% reduction in CLABSIs occurred. With an estimated cost of $48,108 per event, the reduction in CLABSIs led to an estimated cost savings of $577,257 (AHRQ, n.d.). CAUTIs may cost approximately $13,793 per event; thus our reduction in CAUTIs had estimated savings of $110,793 (AHRQ, n.d.). This led to a total of $688,050 in cost avoidance (AHRQ, n.d.; Scott, 2009).
Evidence-based recommendations by major societies play an important role in the prevention of CAUTIs and CLABSIs (Gould et al., 2010; Lo et al., 2014; Marschall et al., 2014; O’Grady et al., 2011). These interventions primarily focus on device maintenance. Strategies for early device removal and prevention of device placement can contribute significantly to patient safety. Simply put, you cannot have device infections without devices. Thus, there is increasing interest in DURs and its correlation with device complications such as reportable infections and non-reportable complications such as pain, mobility, trauma and bleeding (Fakih et al., 2016). Clinical and surveillance definitions are challenging and have changed in recent years. DUR is constant and does not share these limitations (Fakih et al., 2016). We used device utilisation as one of our key quality metrics and an important part of our comprehensive HAI reduction strategy. Furthermore, DUR may impact other key quality initiatives. A recent survey of 297 patients with IUC devices reported negative comments in 87% of patients (Trautner et al., 2019). These included catheter malfunction, pain, interference with daily activities and immobility. IUC DUR may correlate with quality variables beyond infection, such as patient satisfaction, early mobility and discharge.
We report that our hospital-wide safety huddle was a key component of our hospital’s HAI prevention strategy. DISH is cost-effective, requires no major capital investment or additional training, and can bring major cost savings and return of investment with only a 15-min daily commitment by key hospital staff and mechanisms to ensure accountability. Reductions in HAI and DUR can have a significant effect on length of stay, patient satisfaction, cost, morbidity and mortality. DISH represents a forum where IPs can promote device removal and keep individual units accountable for device utilisation. The effects of DISH go beyond these important outcomes, as it also serves as an opportunity to promote a culture of safety and awareness of key IC priorities. Our facility has remained CAUTI and CLABSI-free for > 4 years. DISH was an important part of our journey to zero.
Our study had limitations. It was performed in one site and other interventions such as nursing education on CAUTI and CLABSI prevention bundles and nurse-driven catheter removal protocols may have contributed to reduced DUR and rates of infection as well. NHSN definitions have evolved during the study period and may have contributed to reduced rates of infection, but the formula to calculate DUR remains constant.
Acknowledgments
The authors acknowledge the contributions of their frontline nursing staff and the support of their hospital administration and leaders.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
ORCID iD: Alfredo J Mena Lora  https://orcid.org/0000-0002-8337-757X
https://orcid.org/0000-0002-8337-757X
References
- AHRQ. (n.d.) Estimating the Additional Hospital Inpatient Cost and Mortality Associated With Selected Hospital-Acquired Conditions. Available at: https://www.ahrq.gov/hai/pfp/haccost2017-results.html (accessed 10 November 2019).
- Centers for Disease Control and Prevention. (n.d.) Hospital Acquired Infections (HAIs). Available at: https://www.cdc.gov/hai/surveillance/index.html.
- Centers for Disease Control and Prevention. (2016) National and State Healthcare-Associated Infections Progress Report. Atlanta, GA: CDC; Available at: www.cdc.gov/hai/progress-report/index.html. [Google Scholar]
- Criscitelli T. (2015) Fostering a Culture of Safety: The OR Huddle. AORN Journal 102(6): 656–659. [DOI] [PubMed] [Google Scholar]
- Donnelly LF, Cherian SS, Chua KB, Thankachan S, Millecker LA, Koroll AG, Bisset GS., 3rd (2017) The Daily Readiness Huddle: a process to rapidly identify issues and foster improvement through problem-solving accountability. Pediatric Radiology 47(1): 22–30. [DOI] [PubMed] [Google Scholar]
- Fakih MG, Gould CV, Trautner BW, Meddings J, Olmsted RN, Krein SL, Saint S. (2016) Beyond Infection: Device Utilization Ratio as a Performance Measure for Urinary Catheter Harm. Infection Control and Hospital Epidemiology 37(3): 327–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. and Healthcare Infection Control Practices Advisory Committee. (2010) Guideline for prevention of catheter-associated urinary tract infections 2009. Infection Control and Hospital Epidemiology 31(4): 319–326. [DOI] [PubMed] [Google Scholar]
- Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, Saint S, Schaeffer AJ, Tambayh PA, Tenke P, Nicolle LE and Infectious Diseases Society of America. (2010) Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clinical Infectious Diseases 50(5): 625–63. [DOI] [PubMed] [Google Scholar]
- Lo E, Nicolle LE, Coffin SE, Gould C, Maragakis LL, Meddings J, Pegues DA, Pettis AM, Saint S, Yokoe DS. (2014) Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals: 2014 Update. Infection Control & Hospital Epidemiology 35(S2): S32–S47. [PubMed] [Google Scholar]
- Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O’Grady NP, Pettis AM, Rupp ME, Sandora T, Maragakis LL, Yokoe DS and Society for Healthcare Epidemiology of America. (2014) Strategies to Prevent Central Line-Associated Bloodstream Infections in Acute Care Hospitals: 2014 Update. Infection Control & Hospital Epidemiology 35(S2): S89–S107. [PubMed] [Google Scholar]
- Meddings J, Saint S, Fowler KE, Gaies E, Hickner A, Krein SL, Bernstein SJ. (2015) The Ann Arbor Criteria for Appropriate Urinary Catheter Use in Hospitalized Medical Patients: Results Obtained by Using the RAND/UCLA Appropriateness Method. Annals of Internal Medicine 162(9 Suppl.): S1–34. [DOI] [PubMed] [Google Scholar]
- Menon S, Singh H, Giardina TD, Rayburn WL, Davis BP, Russo EM, Sittig DF. (2017) Safety huddles to proactively identify and address electronic health record safety. Journal of the American Medical Informatics Association 24(2): 261–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad II, Randolph AG, Rupp ME, Saint S. and Healthcare Infection Control Practices Advisory Committee (HICPAC). (2011) Guidelines for the prevention of intravascular catheter-related infections. Clinical Infectious Diseases 52(9): e162–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott RD. (2009) The Direct Medical costs of Healthcare-Associated Infections in U.S. Hospitals and the Benefits of Prevention. Atlanta, GA: CDC; Available at: https://www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf. [Google Scholar]
- Townsend CS, McNulty M, Grillo-Peck A. (n.d.) Implementing Huddles Improves Care Coordination in an Academic Health Center. Professional Case Management 22(1): 29–35. [DOI] [PubMed] [Google Scholar]
- Trautner BW, Saint S, Fowler KE, Van J, Rosen T, Colozzi J, Chopra V, Lescinskas E, Krein SL. (2019) What do patients say about their experience with urinary catheters and peripherally inserted central catheters? American Journal of Infection Control 47(9): 1130–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]