Abstract
Objective
To investigate the effect of replacing sitting with standing on cardiovascular risk factors tested in clinical trials.
Methods
We searched databases from inception up to August 28, 2019, for studies examining the effect of replacing sitting with standing on fasting blood glucose, fasting insulin, and lipid levels; blood pressure; body fat mass; weight; and waist circumference in healthy adults. Differences in mean ± SD values were used for pooling the data and calculating the mean differences and CIs.
Results
The search found 3507 abstracts. Nine clinical trials (8 randomized and 1 nonrandomized) with 877 (64.4% [n=565] women) participants met all inclusion criteria. The mean ± SD age was 45.34±5.41 years; mean follow-up was 3.81 months, and mean difference in standing time between the intervention and control groups was 1.33 hours per day. The follow-up fasting blood glucose and body fat mass values were slightly but significantly lower than baseline records in the intervention groups compared with control groups (−2.53; 95% CI, −4.27 to −0.79 mg/dL; and −0.75; 95% CI, −0.91 to −0.59 kg). The analysis for fasting insulin levels, lipid levels, blood pressure, weight, and waist circumference revealed no significant differences.
Conclusion
Replacing sitting with standing can result in very small but statistically significant decreases in fasting blood glucose levels and body fat mass with no significant effect on lipid levels, blood pressure, weight, and waist circumference. Replacing sitting with standing can be used as an adjunctive intervention to decrease the burden of cardiovascular risk factors but cannot be used as an alternative to physical activity to decrease sedentary time.
Abbreviations and Acronyms: BFM, body fat mass; BMI, body mass index; CVD, cardiovascular disease; FBG, fasting blood glucose; FI, fasting insulin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein; TC, total cholesterol; TG, triglycerides; WC, waist circumference
Cardiovascular disease (CVD), especially ischemic heart disease, is the leading cause of death worldwide.1 The number of deaths from CVD has increased globally from 5.74 to 8.14 million from 1990 to 2013, while the number of crude deaths has decreased from 9.266 per 1000 to 7.556 per 1000 during the same period.2 Major modifiable risk factors for CVD explain most CVD events and several factors coexist because they share similar causes, namely sedentary lifestyle and poor diet. The CVD risk factors representing the spectrum of cardiometabolic dysregulation include elevated blood glucose levels; insulin resistance; abnormal lipid levels; increased waist circumference (WC), waist to hip ratio, and body fat mass (BFM); and high blood pressure.3,4 Accordingly, attenuating these risk factors through lifestyle changes such as increasing physical activity and decreasing sedentary time5 could play a major role in reducing the burden of CVD.
Sedentary behavior, defined as time spent with a low rate of energy expenditure (≤1.5 metabolic equivalent tasks)6,7 during waking hours and commonly represented by sitting time, is associated with CVD and with CVD risk factors, including obesity, diabetes, hypertension, and hyperlipidemia.8, 9, 10, 11, 12 In modern society, adults are highly sedentary, while they might be physically active by the definition of having 150 or more minutes of moderate to vigorous physical activity per week. It is shown that the average monitored sitting time is about 7.7 hours per day in the United States (equal to 54.9% of waking hours)13 and self-reported sitting time is 5.15 hours per day in European countries.14
In recent years, more studies have been focusing on testing the effect of replacing sedentary time with different kinds of activities as an intervention to improve CVD risk factors and mortality.15 Observational data have consistently demonstrated that shorter sedentary time, or sitting time, is associated with healthier measures of WC, body mass index (BMI), triglyceride (TG) levels, and 2-hour plasma glucose levels.16, 17, 18 It also has been shown that replacing sitting with other activities including walking has a significant association with reduced CVD mortality.15 However, the overwhelming evidence supporting the hypothesis that avoiding sedentary time improves CVD risk factors is observational in nature and therefore more prone to bias because people who avoid sedentary behavior tend to be more physically active and healthier.19, 20, 21
Nevertheless, in recent years there has been increased emphasis on standing to reduce sedentary time, under the assumption that nonsitting activities with minimal additional caloric expenditure, such as just standing, would be beneficial.22 Although replacing sitting with standing may help prevent weight gain,22 the effect of standing vs sitting to control CVD risk factors is controversial.23, 24, 25, 26, 27, 28
Therefore, we aimed to systematically review and first, demonstrate how much evidence has been produced to examine the actual effect of using widely growing standing desks on health, and second, quantitatively synthesize the effect of replacing sitting time with standing on sedentary lifestyle–related CVD risk factors in adults as tested in randomized and nonrandomized controlled trials.
Methods
This systematic review and meta-analysis was designed according to the Cochrane Handbook of Systematic Reviews and is approved by Mayo Clinic Institutional Review Board. The study is being reported based on the 2015 Preferred Reporting Items for Systematic Reviews and Meta-analysis statement.29
Studies were eligible if they met all of the following criteria. (1) Design: published and unpublished experiments with a parallel randomized or nonrandomized comparison group or crossover clinical trials. (2) Participants: nonpregnant and nonlactating healthy adults. (3) Intervention: replacing sitting time with standing for at least 30 minutes per day. (4) Comparison: sitting without any significant break including standing or walking. (5) Outcome: changes in CVD risk factors, including obesity measures (weight, WC, waist to hip ratio, and BFM), cardiometabolic biomarkers (fasting blood glucose (FBG), fasting insulin (FI), and lipids), and systemic blood pressure. (6) Follow-up: a minimum of 5 consecutive days. We had no time or language restriction.
An expert librarian searched different databases, including MEDLINE, EMBASE, Scopus, Turning Research Into Practice Database, Web of Science, Google Scholar, and Cumulative Index of Nursing and Allied Health Literature since inception up to August 28, 2019. The Supplemental Appendix (available online at https://mcpiqojournal.org) shows the search strategy and the terms used for searching MEDLINE.
We searched through the references of the included studies and similar studies for additional reports. Trial registries were other sources of the handsearching for finding gray literature, specifically unpublished studies, as defined by the Cochrane handbook.30 No ongoing trial was found in our search. The authors of included studies were also contacted for any similar published or unpublished studies. Before finalizing the analysis, we updated our search for the studies with publication dates after completion of our original search.
Three independent investigators (F.S., J.R.M.-I., and M.S.) reviewed the titles and abstracts of the studies, which were identified through the original search, in parallel and using an online reference manager software (Covidence). Duplicates were removed by the librarian and also during the screening by the software. Disagreements were resolved using consensus and, if not possible, using arbitration as appropriate by the senior investigator (F.L.-J.). The investigators then assessed the full text of the included titles and abstracts for eligibility, independently and in parallel, to capture the most relevant studies for data extraction and analysis. The κ statistic was used to examine the agreement between investigators in each stage of the screening.
A database was prepared with all predefined variables to collect and to be used independently and in duplicate by investigators for the data extraction. Two investigators extracted the data of the included studies, and the third investigator evaluated the results to examine and confirm the concordance between the 2 investigators. The extracted data included study characteristics (author, year of publication, design, location of the study, and risk of bias), participant characteristics (including number of participants, age, sex, and health status), intervention characteristics (including time spent standing in a day and follow-up of the participants in different groups), and mean ± SD of baseline and follow-up of both the intervention and control groups for different cardiometabolic biomarkers and blood pressure. In case additional information was needed, the authors of the study would be contacted by email.
The Cochrane Collaboration’s tool was used to assess the risk of bias in individual studies. The investigators independently answered the following questions for each study: Was the allocation sequence adequately generated? Was allocation adequately concealed? Was the knowledge of the allocated interventions adequately prevented during the study? Were incomplete outcome data adequately addressed? Are reports of the study free of suggestion of selective outcome reporting? Was the study apparently free of other problems that could put it at a risk of bias? The reviewers would answer “yes” to the questions if they found evidence of controlling that bias in the study, the answer “no” meant the study could not control the bias, and “unclear” was used when the reviewers were not able to draw a conclusion regarding the presence or absence of that bias in the study. The number of yes, no, and unclear responses resulted in the overall risk of bias in each study. The studies were also assessed for risk of bias in outcome measurement and analysis.
We calculated the difference in mean ± SD of the baseline and follow-up for both the intervention and control groups in each study and for each risk factor. RevMan, version 5.3, Cochrane Collaboration tool, was used to pool the data across individual studies using a random-effect inverse variance model. The result of the meta-analysis for each risk factor was reported in mean difference and 95% CI. To analyze between-study heterogeneity we used different forest plots and calculated the I2 statistic. The forest plots were inspected visually and I2 values greater than 75% were classified as considerable heterogeneity. In case considerable heterogeneity was discovered between studies, we would use subgroup analysis and sensitivity analysis, if possible, to explain the source of the heterogeneity. Prespecified subgroup analyses were defined based on the duration of standing in the intervention groups, duration of follow-up of participants, and characteristics of participants, such as sex or age.
Results
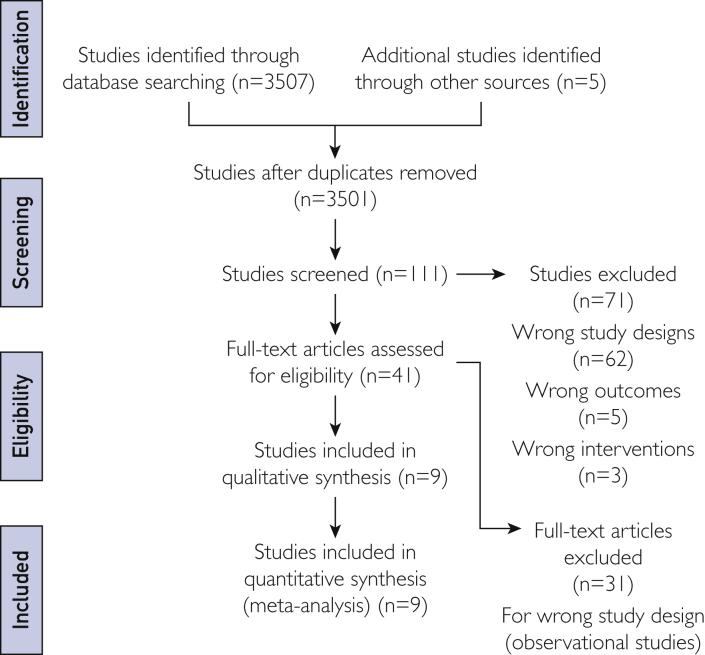
The original search by the librarian identified 3507 studies, of which 41 met the primary inclusion criteria for full-text assessment. After reviewing the full text, the reviewers agreed on 9 studies with 877 participants for data extraction and pooled analysis. Figure 1 shows the number of studies excluded at each stage of the screening and details the reasons for excluding these studies. All studies were done after 2012, and most were conducted in Australia. The mean ± SD age of participants was 45.34±5.41 years, mean follow-up was 3.81 months, and 64.4% (565 of 877) of the participants were women. The mean ± SD difference in standing time between baseline and follow-up in the intervention group was 1.33 hours per day more than the control group. The Table24,26,31, 32, 33, 34, 35, 36, 37 shows the characteristics of studies included in the systematic review and meta-analysis.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram details the literature search and number of included and excluded studies with reasons for exclusion in each stage.
Table.
Baseline Characteristics of Studies That Examined the Effect of Replacing Sitting Time With Standing on Different Cardiovascular Risk Factors
| Reference, year | No. of Participants (intervention, control) | Participants’ Mean Age (y) | Follow-up (mo) | Δ Time of Standing (h/d), intervention − control | Study Design | Setting (PICO) | Study Location | Risk of Bias in Individual Studies |
|---|---|---|---|---|---|---|---|---|
| Aadahl et al,31 2014 | 81, 68 | 52 | 6 | 0.44 | RCT |
Participants: Sedentary adults recruited from the population-based Health 2010 Study who self-reported at least 3.5 h of daily leisure-time sedentary behaviors, had comprehension of Danish language, self-reported maximum 8 h/wk of vigorous physical activity without a handicap or functional limitation Intervention: 4 individual theory-based counseling sessions to encourage for more standing and less sitting Comparison: Participants with usual lifestyle in the control group Outcomes: Sitting time, breaks in sitting time, BMI, weight, waist circumference, body fat, total cholesterol, HDL-C, LDL-C, triglycerides, fasting blood glucose, fasting insulin, fasting HbA1c, HOMA |
Denmark | Low |
| Alkhajah et al,32 2012 | 18, 13 | 36.2 | 3 | 3.54 | RCT |
Participants: Offıce workers who used a nonadjustable work surface and desktop computer Intervention: Installation of commercially available sit–stand workstation Comparisone: Participants doing usual day-to-day activities Outcomes: Changes in sitting and standing time, fasting total cholesterol, HDL-C, triglycerides, fasting glucose |
Australia | Unclear |
| Butler et al33 2018 | 21, 21 | 22.7 | 0.7 | 0.71 | CRCT |
Participants: Healthy college students Intervention: Installing standing desks Comparisone: Participants who were seated Outcomes: Changes in fasting glucose, fasting triglycerides, HDL-C, blood pressure (systolic and diastolic) |
||
| Danquah et al,34 2016 | 173, 144 | 45.5 | 3 | 0.716 | RCT |
Participants: Practitioners and health workers in municipalities and private workplaces Intervention: Appointment of local ambassadors, management support, environmental changes, a lecture, a workshop to encourage for more standing and less sitting Comparison: Participants in control group who did not receive the interventions Outcomes: Changes in waist circumference and body fat percentage |
Denmark and Greenland | Low |
| Graves et al,26 2015 | 23, 21 | 38.6 | 2 | 1.21 | RCT |
Participants: Asymptomatic full-time office workers Intervention: Installing sit-stand workstation on participants’ workplace desk for 8 wk Comparison: Participants in control group who did not receive interventions Outcomes: Sitting, standing, and walking time; vascular outcomes including endothelial dysfunction, carotid artery intima media thickness, systolic and diastolic blood pressure; fasting blood glucose, total cholesterol, triglycerides, musculoskeletal discomfort/pain, anthropometric, sociodemographic, work-related and office environment characteristics, acceptability and feasibility of using sit-stand workstation |
England | Unclear |
| Healy et al,35 2013 | 18, 18 | 43.2 | 1 | 2.13 | NRCT |
Participants: Sample of community-dwelling Australian adults Interventions: 45-min researcher-led consultation, holding workshops, installing dual display sit-stand workstations, 30-min face-to-face consultation with each intervention participant, followed by 3 telephone calls (1/wk) Comparison: Participants in control group who were advised to maintain usual work practices Outcomes: Changes in sitting, standing, and moving time; weight, waist circumference, hip circumference, fat-free mass, fat mass, total cholesterol, triglycerides, HDL-C, LDL-C, fasting glucose, fasting insulin, systolic and diastolic blood pressure |
Australia | Unclear |
| Healy et al,36 2017 | 136, 95 | 45.6 | 12 | 0.6 | RCT |
Participants: Staff of a large single public service organization Intervention: Senior management support, recruitment of team champion, emails from team champion promoting the intervention messages, installing sit-stand workstations, health coaching, goal setting and tracking Comparison: Participants in control group who were advised to maintain usual work practices Outcomes: Cardiometabolic risk score, changes in weight, fat mass, waist circumference, HDL-C, LDL-C, triglycerides, fasting blood glucose, fasting insulin, HOMA, systolic and diastolic blood pressure |
Australia | Low |
| MacEwen et al,37 2017 | 15, 10 | 45.48 | 3 | 1.31 | RCT |
Participants: Overweight/obese sedentary office workers, mean BMI of 35.8 kg/m2 Intervention: Installing height-adjustable desks Comparison: Participants in seated work posture Outcomes: Changes in weight, BMI, waist circumference, body fat mass, systolic and diastolic blood pressure, total cholesterol, triglycerides, HDL-C, LDL-C, fasting blood glucose, HbA1c, Vo2max, aortic augmentation index, subendocardial variablity, behavioral outcomes |
||
| Thorp et al,24 2014 | 23, 23 | 48.2 | 0.17 | 3.91 | Crossover RCT |
Participants: Overweight/obese sedentary office workers, 17 men and 6 women, BMI= 29.6 kg/m2 Intervention: Installing electric height-adjustable workstation Comparison: Participants in seated work posture Outcomes: Changes in weight, waist circumference, fasting glucose, fasting insulin, fasting triglycerides |
Australia | Low |
BMI = body mass index; CRCT = controlled randomized clinical trial; HbA1c, glycated hemoglobin; HDL-C = high-density lipoprotein cholesterol; HOMA = homeostatic model assessment; LDL-C = low-density lipoprotein cholesterol; NRCT = nonrandomized clinical trial; PICO = participants, intervention, comparison, outcomes; RCT = randomized controlled trial; Vo2max, maximum oxygen consumption.
Five of 9 studies had a low risk of bias and 4 had an intermediate risk of bias. The outcome-level risk of bias assessment within individual studies revealed that obesity measures and cardiometabolic biomarkers in all studies were made by staff blinded to group allocation, and in 4 studies, the measurement of blood pressure was blinded to group allocation. None of the studies reported incomplete data. The overall outcome-level risk of bias across the studies was low.
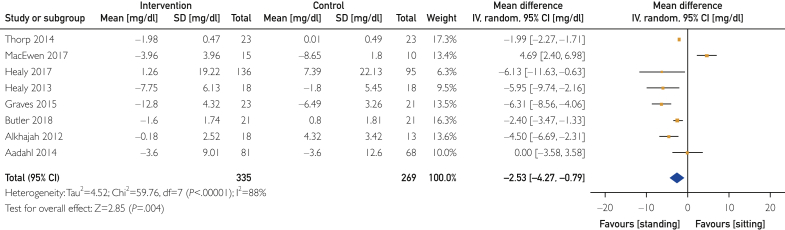
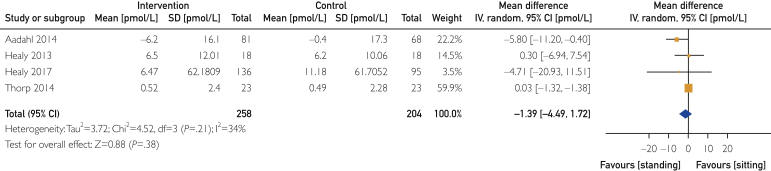
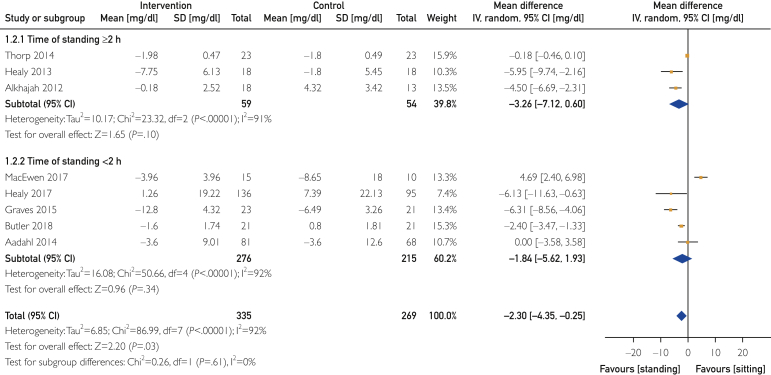
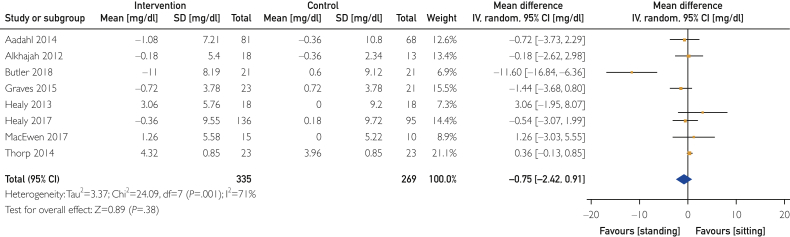
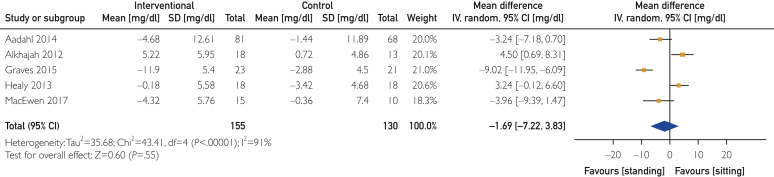
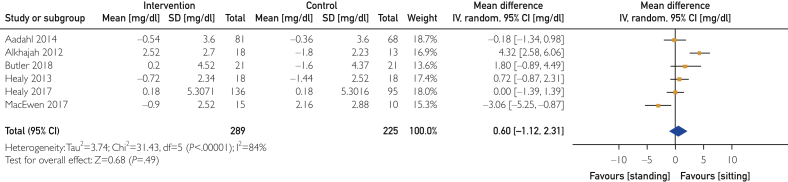
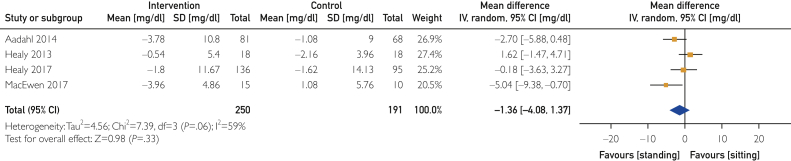
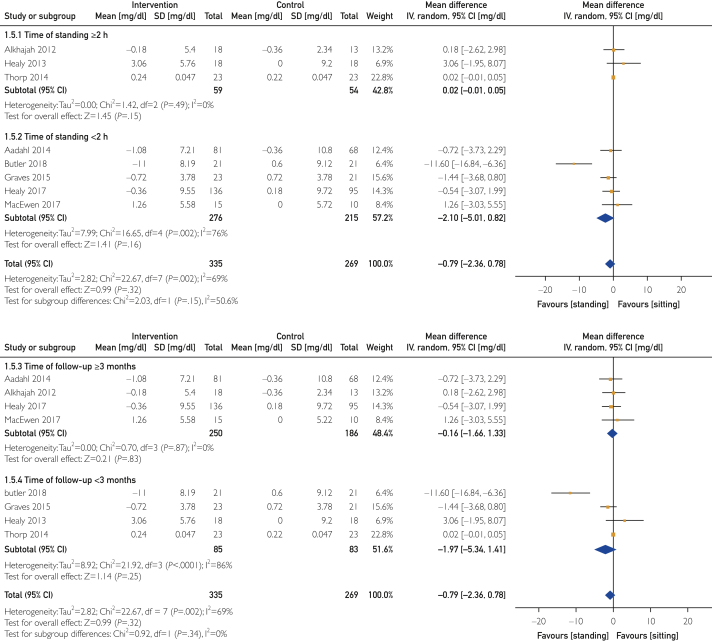
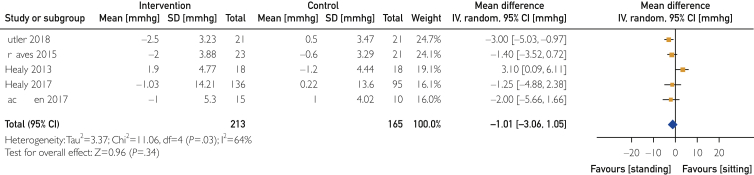
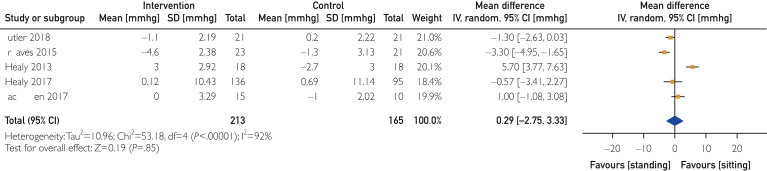
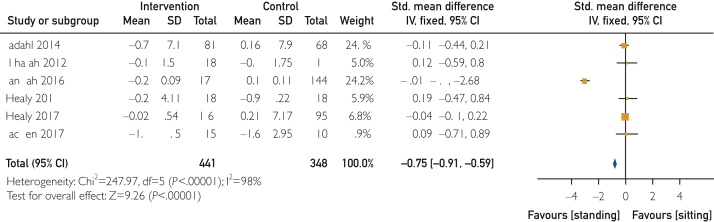
Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14 are forest plots that detail the differences between baseline and follow-up for both intervention and control groups followed by the mean difference (intervention − control) and 95% CI of each risk factor in each study. The risk factors include FBG, FI, TG, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), weight, WC, BFM, systolic blood pressure, and diastolic blood pressure.
Figure 2.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on fasting blood glucose level. SI conversion factor: To convert glucose values to mmol/L, multiply by 0.0555.
Figure 3.
The weighted mean difference and 95% CI of the effect of replacing sitting with standing on fasting blood glucose levels in different subgroups. SI conversion factor: To convert glucose values to mmol/L, multiply by 0.0555.
Figure 4.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on fasting blood insulin level.
Figure 5.
The weighted mean difference and 95% CI of the effect of replacing sitting with standing on triglyceride levels in different subgroups. SI conversion factor: To convert triglyceride values to mmol/L, multiply by 0.0113.
Figure 6.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on low-density lipoprotein cholesterol level. SI conversion factor: To convert low-density lipoprotein cholesterol values to mmol/L, multiply by 0.0259.
Figure 7.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on triglyceride level. SI conversion factor: To convert triglyceride values to mmol/L, multiply by 0.0113.
Figure 8.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on total cholesterol level. SI conversion factor: To convert total cholesterol values to mmol/L, multiply by 0.0259.
Figure 9.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on high-density lipoprotein cholesterol level. SI conversion factor: To convert high-density lipoprotein cholesterol values to mmol/L, multiply by 0.0259.
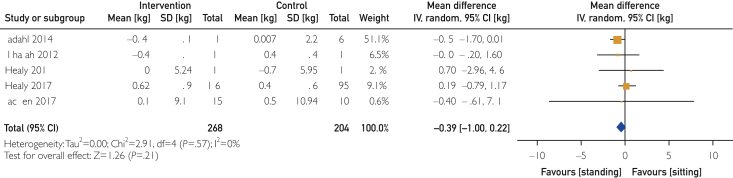
Figure 10.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on systolic blood pressure.
Figure 11.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on diastolic blood pressure.
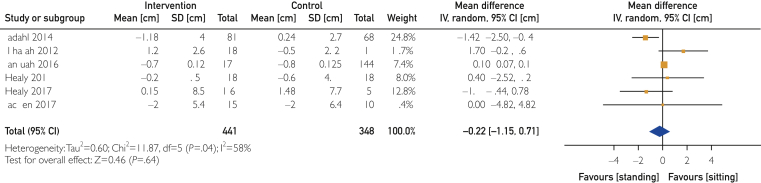
Figure 12.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on body fat mass. STD = standardized.
Figure 13.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on weight.
Figure 14.
The overall weighted mean difference and 95% CI of the effect of replacing sitting with standing on waist circumference.
Standing decreased FBG and BFM values in the intervention groups compared with the control groups (−2.53; 95% CI, −4.27 to −0.79 mg/dL [to convert to mmol/L, multiply by 0.0555]; and −0.75, 95% CI, −0.91 to −0.59 kg, respectively). Measurements of other risk factors did not change significantly (Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14).
Examination of heterogeneity among studies for different risk factors showed that between-study heterogeneity for FI was not important (I2=34%), whereas for systolic blood pressure, WC, LDL-C, and TG values, it was moderate to substantial (I2=64%, 58%, 59%, and 71%, respectively) and for FBG, TC, HDL-C, and diastolic blood pressure values was considerable (I2=88%, 91%, 84%, and 92%, respectively).
The strength of our recommendations using the Grading of Recommendations, Assessment, Development and Evaluations system was moderate.38,39 The risk of bias was low in most studies, mainly in those that were included for FBG and BFM; the results of the studies were direct (low level of indirectness); the results of the studies were consistent because heterogeneity was less than 75% among most studies (low to moderate level of inconsistency); the results were imprecise about nonsignificant outcomes (broad CIs); and finally, the publication bias was low (mainly for FBG and BFM; we used different studies for different outcomes; therefore, having a funnel plot for all included studies was not possible).
Discussion
The present study aimed to investigate the effect of replacing sitting time with standing on CVD risk factors through a systematic review and meta-analysis. The results of the study demonstrated that replacing an average of 1.33 hours of sitting per day with standing for an average of 4 months can modestly decrease FBG and BFM values. There were no significant changes in FI, body weight, WC, blood lipid levels (including TG, TC, HDL-C, and LDL-C), or blood pressure after replacing sitting with standing.
Body Fat Mass
Our results showed a small but significant effect of replacing sitting with standing on BFM. It has been shown that increasing daily energy expenditure, even with substituting sitting with slow-pace walking, which is not classified as an exercise, has a promising effect on body composition, in particular, body fat content.40,41 We have recently demonstrated that standing expends significantly more energy (0.15 kcal/min) than sitting and standing for 6 hours per day for a year could have a significant effect on energy expenditure,22 emphasizing that standing can theoretically decrease BFM over time. The relatively short mean duration of standing and the low-intensity nature of the intervention could potentially explain the small amount of change in BFM that was observed in this study.
Waist Circumference
The nonsignificant results for WC (P=0.64) and weight (P=0.21) could be explained by reviewing the limitations in methods and instruments of the original studies and the importance of the variables. Weight is an inaccurate measure for evaluating body composition at the individual level.42,43 Additionally, manual measurement of WC is prone to numerous errors and has shown significant inter- and intraobserver variability, limiting the ability to detect small differences in WC over time.44,45 This can explain the significant reduction in WC that was observed in the study by Aadahl et al,31 which contrasted with the other studies that did not report significant changes in WC. It is also possible that small changes in the amount of visceral fat may not be reflected in changes in WC. Despite these differences, there is also the possibility that standing vs sitting may not lead to significant weight loss or improvements in the distribution of fat, particularly with modest durations of standing or because of substitution of fat with muscle. In contrast, observational studies have shown a significant reduction in weight and BMI in people who use sit-stand desks in comparison to the people who work seated.46,47
Fasting Blood Glucose
A modest effect on FBG level was observed when replacing sitting with standing. Muscle has a significant role in the regulation of blood glucose. Muscle contraction increases the number of glucose receptors and glucose uptake.48 Standing involves more muscles than sitting,49 and this can be a physiologic explanation of our results. However, considering the small difference in the number and intensity of muscle contractions between sitting and standing, the difference in glucose uptake between these 2 postures is expected to be small. Overall, the result of this study suggests some benefits for the prevention of diabetes and at least theoretically for the management of patients with diabetes.
Our study also showed no effect of standing on blood lipid level, similar to what prior studies have shown on the effect of replacing sitting with either aerobic exercise or light-intensity activities on blood lipid levels.9,50,51
Blood Pressure
The present study did not show a significant change in blood pressure after replacing sitting with standing, unlike observational studies that showed the opposite results for the effect of replacing sitting time with standing in sedentary individuals.46 The lack of blood pressure reduction could be because participants of those studies were not hypertensive and changes in blood pressure in normotensive people who are physically active may be minimal or negligible.35,36 Furthermore, standard 1-time blood pressure measurements may not be able to detect small changes in blood pressure.
The potential benefits of standing to replace sitting may not be limited to short-term modifications in CVD risk factors. Standing as a major component of nonexercise activity thermogenesis can help decrease sedentary time.31,45 In addition, the substitution of sitting with standing can increase daily energy expenditure,46,47 which can prevent weight gain in the long term. Although considering that this intervention has minimal effect on CVD risk factors, the definition of a nonsitting position while also performing no active movements should be revised. Also, the effect of replacing sitting with standing on CVD risk factors can be different in samples with different body composition, BMI, baseline level of physical activity, age, or sex.
This is the first systematic review and meta-analysis on the effect on CVD risk factors of replacing sitting time with standing as an exclusive intervention. Prior systematic reviews have assessed the effects of a range of activities from standing to moderate to vigorous physical activities on CVD risk factors.
In a systematic review by Batacan et al,52 the effects of light-intensity activities were shown to have a trivial effect on CVD risk factors in healthy individuals, consistent with our findings. As discussed, that systematic review did not separate different kinds of light-intensity activities from each other to assess for any differential effects on CVD risk factors.
Another systematic review and meta-analysis by Chastin et al9 assessed the effect on CVD risk factors of breaking sitting time with a combination of activities with different intensities. They conducted a meta-analysis (pooling the data from 2 randomized controlled trials) focused on the effect of different kinds of activities on blood glucose levels and showed that breaking sitting time with standing does not have an effect on lowering blood glucose levels. However, our present study reports the results of a meta-analysis of several CVD risk factors, including blood glucose, blood lipid, and blood pressure values, using 8 randomized controlled trials. Our findings provide objective evidence of the effect of using standing as an intervention for a sedentary lifestyle on CVD risk factors.
Our study has several limitations. The number of studies that met inclusion criteria was small; however, all were clinical trials and most studies had a low risk of bias, thus increasing the quality of the meta-analysis. Between-study heterogeneity for more than half the factors was considerable and subgroup and sensitivity analyses were not possible to be conducted. The results for FBG and BFM were significant but effect sizes were modest. However, the observed effects are not trivial, and standing can be suggested as an adjunct preventive modification for sedentary lifestyles. Our meta-analysis was not significant for several CVD risk factors, which challenges both the effect of replacing sitting with standing on CVD risk and also the definition of sedentary behavior, which is currently “sitting or lying down for a long period.” Generalizing the results of the study to people from different cultures and with different extents of dysregulation in CVD risk factors should be done with more caution because all participants of the included studies were healthy and from Denmark and Australia. Because the intensity of the intervention was low, the duration of the intervention and time of follow-up may not have been enough to make a significant change in risk factors. The average standing time in the intervention group was 1.25 hours per day and the average of follow-up was 4 months, representing a low dose and duration for the intervention under study and limiting the potential effect size, if any. However, the study by Alkhajah et al32 did not show substantial decreases in risk factors, and some measures, such as TG or TC, showed increases in the intervention group.
Regarding the time of follow-up, Healy et al36 with 12 months of follow-up did not report significant changes for almost all factors. A robust randomized ontrolled trial with both longer time of standing and duration of follow-up might be able to resolve some of these questions. Given the modest, negligible, or absent effect of standing vs sitting on CVD risk factors, the assumption that simply replacing sitting with standing time without meaningful differences in physical activity will decrease CVD may be inaccurate. In the meantime, until further prospective and experimental evidence proves beneficial effects of standing vs sitting on measures of cardiometabolic regulation or outcomes, the strategies to decrease sedentary time need to include physical activity.
Conclusion
Our study shows that replacing sitting time with standing in healthy adults could decrease FBG and BFM. However, there is no significant change on the remaining cardiovascular risk factors such as lipid, blood pressure, weight, and WC values. This can suggest that replacing sitting with standing can be used as an adjunctive intervention to decrease the burden of cardiovascular risk factors but cannot be used as an alternative to physical activity to decrease sedentary time. Future studies are needed to evaluate both the financial and clinical impact of this intervention on different groups of participants.
Footnotes
Grant Support: This work was supported by project FNUSA-ICRC (no. CZ.1.05/1.1.00/02.0123), project no. LQ1605 from the National Program of Sustainability II (MEYS CR), and project ICRC-ERA-Human Bridge (no. 316345) and funded by the 7th Framework Program of the European Union, and National Institutes of Health/National Heart, Lung, and Blood Institute grant (no. HL-126638 to TPO).
Potential Competing Interests: The authors declare no competing interests.
Supplemental material can be found online at https://mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
.
.
References
- 1.Vishram J.K.K. Prognostic interactions between cardiovascular risk factors. Dan Med J. 2014;61(7):B4892. [PubMed] [Google Scholar]
- 2.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bundhun P.K., Wu Z.J., Chen M.H. Impact of modifiable cardiovascular risk factors on mortality after percutaneous coronary intervention: a systematic review and meta-analysis of 100 studies. Medicine (Baltimore) 2015;94(50):e2313. doi: 10.1097/MD.0000000000002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta P.K., Wei J., Wenger N.K. Ischemic heart disease in women: a focus on risk factors. Trends Cardiovasc Med. 2015;25(2):140–151. doi: 10.1016/j.tcm.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dempsey P.C., Owen N., Biddle S.J., Dunstan D.W. Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr Diabetes Rep. 2014;14(9):522. doi: 10.1007/s11892-014-0522-0. [DOI] [PubMed] [Google Scholar]
- 6.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37:540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 7.Jette M., Sidney K., Blümchen G. Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol. 1990;13(8):555–565. doi: 10.1002/clc.4960130809. [DOI] [PubMed] [Google Scholar]
- 8.Wilmot E.G., Edwardson C.L., Achana F.A., et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 9.Chastin S.F., Egerton T., Leask C., Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity (Silver Spring) 2015;23(9):1800–1810. doi: 10.1002/oby.21180. [DOI] [PubMed] [Google Scholar]
- 10.Barnes A.S. Obesity and sedentary lifestyles: risk for cardiovascular disease in women. Tex Heart Inst J. 2012;39(2):224–227. [PMC free article] [PubMed] [Google Scholar]
- 11.Honda T., Chen S., Kishimoto H., Narazaki K., Kumagai S. Identifying associations between sedentary time and cardio-metabolic risk factors in working adults using objective and subjective measures: a cross-sectional analysis. BMC Public Health. 2014;14:1307. doi: 10.1186/1471-2458-14-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henson J., Yates T., Biddle S.J., et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56(5):1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- 13.Matthews C.E., Chen K.Y., Freedson P.S., et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennie J.A., Chau J.Y., van der Ploeg H.P., Stamatakis E., Do A., Bauman A. The prevalence and correlates of sitting in European adults-a comparison of 32 Eurobarometer-participating countries. Int J Behav Nutr Phys Act. 2013;10:107. doi: 10.1186/1479-5868-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stamatakis E., Gale J., Bauman A., Ekelund U., Hamer M., Ding D. Sitting time, physical activity, and risk of mortality in adults [erratum in: J Am Coll Cardiol. 2019;73(21):2789] J Am Coll Cardiol. 2019;73(16):2062–2072. doi: 10.1016/j.jacc.2019.02.031. [DOI] [PubMed] [Google Scholar]
- 16.Peddie M.C., Bone J.L., Rehrer N.J., Skeaff C.M., Gray A.R., Perry T.L. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr. 2013;98(2):358–366. doi: 10.3945/ajcn.112.051763. [DOI] [PubMed] [Google Scholar]
- 17.Healy G.N., Dunstan D.W., Salmon J., et al. Breaks in sedentary time beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 18.Dunstan D.W., Kingwell B.A., Larsen R., et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hulsegge G., Looman M., Smit H.A., Daviglus M.L., van der Schouw Y.T., Verschuren W.M. Lifestyle changes in young adulthood and middle age and risk of cardiovascular disease and all-cause mortality: the Doetinchem Cohort Study. J Am Heart Assoc. 2016;5(1):e002432. doi: 10.1161/JAHA.115.002432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buman M.P., Winkler E.A., Kurka J.M., et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2013;179(3):323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 21.Chu P., Pandya A., Salomon J.A., Goldie S.J., Hunink M.G. Comparative effectiveness of personalized lifestyle management strategies for cardiovascular disease risk reduction. J Am Heart Assoc. 2016;5(3):e002737. doi: 10.1161/JAHA.115.002737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saeidifard F., Medina-Inojosa J.R., Supervia M., et al. Differences of energy expenditure while sitting versus standing: a systematic review and meta-analysis. Eur J Prev Cardiol. 2018;25(5):522–538. doi: 10.1177/2047487317752186. [DOI] [PubMed] [Google Scholar]
- 23.Healy G.N., Winkler E.A., Owen N., Anuradha S., Dunstan D.W. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36(39):2643–2649. doi: 10.1093/eurheartj/ehv308. [DOI] [PubMed] [Google Scholar]
- 24.Thorp A.A., Kingwell B.A., Sethi P., Hammond L., Owen N., Dunstan D.W. Alternating bouts of sitting and standing attenuate postprandial glucose responses. Med Sci Sports Exerc. 2014;46(11):2053–2061. doi: 10.1249/MSS.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 25.Henson J., Davies M.J., Bodicoat D.H., et al. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study. Diabetes Care. 2016;39(1):130–138. doi: 10.2337/dc15-1240. [DOI] [PubMed] [Google Scholar]
- 26.Graves L., Murphy R., Shepherd S.O., Cabot J., Hopkins N.D. Evaluation of sit-stand workstations in an office setting: a randomised controlled trial. BMC Public Health. 2015;15:1145. doi: 10.1186/s12889-015-2469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duvivier B.M., Schaper N.C., Bremers M.A., et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PloS One. 2013;8:e55542.. doi: 10.1371/journal.pone.0055542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bailey D.P., Locke C.D. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport. 2015;18(3):294–298. doi: 10.1016/j.jsams.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 29.Moher D., Shamseer L., Clarke M., et al. PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Higgins J.P., Green S. In: Cochrane Book Series. Higgins J.P.T., Green S., editors. The Cochrane Collaboration; 2005. Cochrane Handbook for Systematic Reviews of Interventions. ISBN: 978-0-470-69951-5. [Google Scholar]
- 31.Aadahl M., Linneberg A., Moller T.C., et al. Motivational counseling to reduce sitting time: a community-based randomized controlled trial in adults. Am J Prev Med. 2014;47(5):576–586. doi: 10.1016/j.amepre.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 32.Alkhajah T.A., Reeves M.M., Eakin E.G., Winkler E.A., Owen N., Healy G.N. Sit-stand workstations: a pilot intervention to reduce office sitting time. Am J Prev Med. 2012;43(3):298–303. doi: 10.1016/j.amepre.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 33.Butler K.M., Ramos J.S., Buchanan C.A., Dalleck L.C. Can reducing sitting time in the university setting improve the cardiometabolic health of college students? Diabetes Metab Syndr Obes. 2018;11:603–610. doi: 10.2147/DMSO.S179590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Danquah I.H., Kloster S., Holtermann A., et al. Take a Stand!–a multi-component intervention aimed at reducing sitting time among office workers–a cluster randomized trial. Int J Epidemiol. 2017;46(1):128–140. doi: 10.1093/ije/dyw009. [DOI] [PubMed] [Google Scholar]
- 35.Healy G.N., Eakin E.G., LaMontagne A.D., et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med. 2013;57(1):43–48. doi: 10.1016/j.ypmed.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 36.Healy G.N., Winkler E., Eakin E.G., et al. A cluster RCT to reduce workers' sitting time: impact on cardiometabolic biomarkers. Med Sci Sports Exerc. 2017;49(10):2032–2039. doi: 10.1249/MSS.0000000000001328. [DOI] [PubMed] [Google Scholar]
- 37.MacEwen B.T., Saunders T.J., MacDonald D.J., Burr J.F. Sit-stand desks to reduce workplace sitting time in office workers with abdominal obesity: a randomized controlled trial. J Phys Act Health. 2017;14(9):710–715. doi: 10.1123/jpah.2016-0384. [DOI] [PubMed] [Google Scholar]
- 38.Balshem H., Helfand M., Schünemann H.J., et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 39.Murad M.H. Clinical practice guidelines: a primer on development and dissemination. Mayo Clinic Proc. 2017;92(3):423–433. doi: 10.1016/j.mayocp.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Wood P.D. Impact of experimental manipulation of energy intake and expenditure on body composition. Crit Rev Food Sci Nutr. 1993;33(4-5):369–373. doi: 10.1080/10408399309527635. [DOI] [PubMed] [Google Scholar]
- 41.Hanson S., Jones A. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br J Sports Med. 2015;49(11):710–715. doi: 10.1136/bjsports-2014-094157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Batsis J.A., Mackenzie T.A., Bartels S.J., Sahakyan K.R., Somers V.K., Lopez-Jimenez F. Diagnostic accuracy of body mass index to identify obesity in older adults: NHANES 1999–2004. Int J Obes (Lond) 2016;40(5):761–767. doi: 10.1038/ijo.2015.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sahakyan K.R., Somers V.K., Rodriguez-Escudero J.P., et al. Normal-weight central obesity: implications for total and cardiovascular mortalitymortality risk in persons with normal-weight central obesity. Ann Intern Med. 2015;163(11):827–835. doi: 10.7326/M14-2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Medina-Inojosa J., Somers V., Jenkins S., et al. Validation of a white-light 3D body volume scanner to assess body composition. Obes Open Access. 2017;3(1) doi: 10.16966/2380-5528.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medina-Inojosa J., Somers V.K., Ngwa T., Hinshaw L., Lopez-Jimenez F. Reliability of a 3D body scanner for anthropometric measurements of central obesity. Obes Open Access. 2016;2(3) doi: 10.16966/2380-5528.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carr L.J., Swift M., Ferrer A., Benzo R. Cross-sectional examination of long-term access to sit-stand desks in a professional office setting. Am J Prev Med. 2016;50(1):96–100. doi: 10.1016/j.amepre.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 47.Chaput J.P., Saunders T.J., Tremblay M.S., Katzmarzyk P.T., Tremblay A., Bouchard C. Workplace standing time and the incidence of obesity and type 2 diabetes: a longitudinal study in adults. BMC Public Health. 2015;15:111. doi: 10.1186/s12889-015-1353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Santos J., Benite-Ribeiro S., Queiroz G., Duarte J.A. The interrelation between aPKC and glucose uptake in the skeletal muscle during contraction and insulin stimulation. Cell Biochem Funct. 2014;32(3):621–624. doi: 10.1002/cbf.3081. [DOI] [PubMed] [Google Scholar]
- 49.Tikkanen O., Haakana P., Pesola A.J., et al. Muscle activity and inactivity periods during normal daily life. PloS One. 2013;8(1):e52228. doi: 10.1371/journal.pone.0052228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cai M., Zou Z. Effect of aerobic exercise on blood lipid and glucose in obese or overweight adults: a meta-analysis of randomised controlled trials. Obes Res Clin Pract. 2016;10(5):589–602. doi: 10.1016/j.orcp.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 51.Kelley G.A., Kelley K.S., Tran Z.V. Aerobic exercise, lipids and lipoproteins in overweight and obese adults: a meta-analysis of randomized controlled trials. Int J Obes (Lond) 2005;29(8):881–893. doi: 10.1038/sj.ijo.0802959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Batacan R.B., Duncan M.J., Dalbo V.J., Tucker P.S., Fenning A.S. Effects of light intensity activity on CVD risk factors: a systematic review of intervention studies. BioMed Res Int. 2015;2015:596367. doi: 10.1155/2015/596367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
.
.