Abstract
Pott’s puffy tumor is a rare and serious complication of frontal sinusitis, characterized by the development of osteomyelitis and subperiostal abscess in the frontal bone. Paranasal sinus osteomas are benign osteoblastic tumors, usually seen in the 3rd and 4th decades of life. In this report, we present a case of Pott’s puffy tumor due to frontal sinus osteoma in an adolescent male patient. In the literature, we found no similar case in the pediatric age group and we wanted to emphasize the development of Pott’s tumor as a rare complication of chronic or recurrent sinusitis and draw attention to the fact that paranasal sinus osteomas may be the underlying cause.
Keywords: Adolescent, osteoma, paranasal sinuses, Pott’s puffy tumor
Abstract
Pott’s puffy tümör frontal sinüzitin nadir ve ciddi bir komplikasyonu olarak görülebilen, frontal kemikte osteomyelit ve subperiostal abse gelişimi ile belirgin bir hastalıktır. Paranazal sinüs osteomları ise genellikle yaşamın 3. ve 4. dekatında görülen selim osteoblastik tümörlerdir. Biz bu yazımızda frontal sinüs osteomuna bağlı gelişen Pott’s puffy tümör tanılı olgumuzu sunmak istedik. Dizinde çocukluk yaş grubunda benzer bir olguya rastlamadığımız için, kronik ya da tekrarlayıcı sinüzit olgularında nadir görülen bir komplikasyon olan Pott’s tümör gelişimine ve bunun altında yatan sebep olarak paranazal sinüs osteomları olabileceğine dikkat çekmek istedik.
Keywords: Ergen, osteom, paranazal sinüsler, Pott’s puffy tümörü
Introduction
Osteomas are the most common bone tumor in the facial region, and also the most common benign tumors of the paranasal sinuses. The most frequent facial site affected by osteomas is the mandibula. Paranasal sinus osteomas are most commonly observed in the frontal sinus, followed by the ethmoid sinus (1). Osteomas are slow-growing tumors with well-defined borders. The etiology of osteomas has not been identified clearly; they may be traumatic, infective or embryonic (2). The majority of patients are asymptomatic. In symptomatic patients, endonasal endoscopic and/or open surgical treatment is performed. The most common symptoms include progressive headache, facial pain, epistaxis, photophobia, hyposmia or anosmia. The gold standard investigation in diagnosis and treatment planning is computed tomography (CT). Paranasal sinus osteomas may lead to chronic sinusitis, development of mucocele, and intraorbital and intracranial complications depending on the localization and size (1, 3, 4).
Pott’s puffy tumor may be observed as a rare and serious complication of frontal sinusitis and is characterized by progressively increasing edema and swelling in the forehead secondary to the development of osteomyelitis and a subperiosteal abscess in the frontal bone. It is rarely observed in early childhood and frequently occurs in adolescence. It leads to serious complications in the absence of early diagnosis and treatment. Appropriate broad-spectrum antibiotic treatment, and if necessary, surgical drainage should be performed without loss of time to prevent complications (5). In this article, we aimed to draw attention to the development of Pott’s puffy tumor as a complication of frontal sinusitis, and to the fact that paranasal sinus osteomas may also be observed in the pediatric age group as an underlying cause in cases of complicated sinusitis.
Case
A 15-year-old male patient presented to an external center with headache and swelling that started in his left eye and occurred in his right eye and forehead on the next day. The laboratory tests performed in the external center showed a white blood cell (WBC) value of 15 600/mm3 and a C-reactive protein (CRP) value of 5.6 (normal: 0–0.5) mg/dL. A diagnosis of acute frontal sinusitis was made with an examination and the laboratory findings, and oral amoxicillin-clavulanate treatment was initiated at a dosage of 60 mg/kg/day. Netilmicin sulfate eye drops and sodium fusidate ophthalmic ointment treatment was initiated because of conjunctivitis. The patient, whose headache and swelling in the left eye and forehead continued during treatment, presented to our hospital when his symptoms did not regress.
At the time of presentation, the patient’s vital findings were as follows: body temperature: 36.8°C, blood pressure: 110/70 mm Hg, apical heartbeat: 74 beats/min. On physical examination, his oropharynx was hyperemic, there was periorbital edema and 2x2 cm of local swelling infraorbitally, hyperemia and local increase in the heat (Fig. 1a). There was marked postnasal purulent discharge and tenderness on the frontal region with palpation. The initial laboratory findings were as follows: WBC: 8.99 (74.5% neutrophil, 16% lymphocyte, 7.7% monocyte), hemoglobin (Hb): 15 g/dL, hematocrit (Hct): 42.2%, mean corpuscular volume (MCV): 92.9 fL, platelets (Plt): 333 000, CRP: 102 (normal: 0–8) mg/dL, erythrocyte sedimentation rate (ESR): 52 mm/h. Routine biochemical tests were found to be normal.
Figure 1.
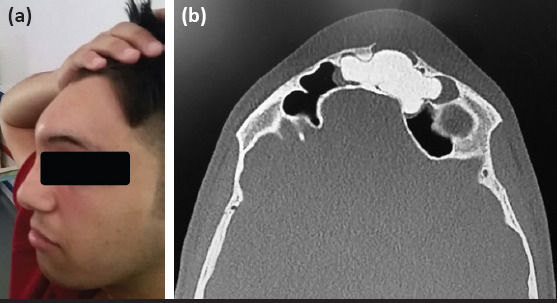
(a) The appearence of swelling, approximately 2x2 cm, in the frontal area. (b) The mass eroding the left frontal sinus anterior wall on paranasal sinus tomography
Treatment with intravenous ceftriaxone (75 mg/kg/day) and teicoplanin (a loading dosage of 16 mg/kg/day on the first day and a maintenance dosage of 8 mg/kg/day subsequently) was initiated with a prediagnosis of Pott’s puffy tumor as a complication of frontal sinusitis. The paranasal sinus CT revealed increased mucosal thickness and appearance of a collection and a sclerotic lesion (osteoma?) in both frontal sinuses (with a size of 42x28 mm with lobulated contours in the widest part in the coronal plane extending to the left ethmoid cells on the left side), and an erosion in the anterior wall of the frontal sinus adjacent to the lesion described (Fig. 1b). On the second day of hospitalization, the patient was consulted by Opthalmology and Otorhinolaryngology clinics. The opthalmology consultation resulted as follows: “Full vision, eye movements are free and painless in all directions, no cell was observed in the anterior camera on biomicroscopic examination and bilateral fundi are natural.” The patient was assessed by the otorhinolaryngology department and it was thought that excision of the mass, which was thought to be an osteoma, would be appropriate, because it eroded the anterior wall of the frontal sinus, and the sinusitis that developed was complicated by the development of subperiostal abscess (Pott’s tumor). In the follow-up, the edema around the patient’s eye and forehead reduced, and his headache improved. He was discharged with oral antibiotherapy after treatment with IV ceftriaxone and teicoplanin for 10 days. Following outpatient follow-up with antibiotherapy, the patient was hospitalized by the otorhinolaryngology department for surgery, mass excision was performed, and a histopathologic examination of the tissue obtained was found to be compatible with osteoma. Written consent was obtained from the patient who participated in the study and from his family.
Discussion
Pott’s puffy tumor is a clinical picture characterized by the development of osteomyelitis and a subperostal abscess in the frontal bone secondary to frontal sinus infection. Dissemination of the infection in the frontal sinus occurs by way of the thin wall of the sinus directly or of small veins draining sinus mucosa (6). The first case was described by Percival Pott in 1768 (7). Pott’s puffy tumor may also develop following cranial trauma or fronto-nasal surgery. The most common symptoms in Pott’s puffy tumor include headache, swelling in the frontal region, periorbital edema, as observed in our patient, and signs such as fever, vomiting, rhinorrhea, lethargy, and photophobia may also accompany. Frequently, the causative agents include staphylococci, streptococci and anaerobic mcroorganisms (8, 9). The development of the frontal sinus after birth starts at about 2 years of age, and the frontal sinus can be radiologically visualized after the age of 6 years. Development of the frontal sinus continues until late adolescence, and it reaches its widest size approximately by the age of 20 years. Therefore, Pott’s puffy tumor as a complication of frontal sinusitis is frequently observed in adolescents, though it may occur in all age groups (10). In the differential diagnosis, soft tissue infections such as carbuncle and infected sebaceous cyst, benign tumors such as dermoid cyst and lypoma, malignant tumors such as metastatic or aggressive frontal meningioma, frontal sinus mucocele, superficial temporal artery pseudoaneurysm, and preseptal cellulitis should be considered. A surgical consultation should be requested in terms of subperiosteal abscess drainage. Patients should be followed up with antibiotic treatment and close monitoring in terms of complications (11). Early diagnosis and treatment are important because serious orbital and cranial complications including periorbital cellulitis, orbital cellulitis, orbital abscess, meningitis, subdural empyema, intracranial abscess, and venous sinus thrombosis may occur. Cranial imaging must be requested in cases of clinical suspicion (12).
Paranasal sinus osteomas are the most common benign tumors of the paranasal sinuses. These tumors are slow-growing, osteoblastic tumors with well-defined borders. The incidence ranges between 0.43% and 1%. Generally, they are detected in the 3rd and 4th decades of life (3). The most commonly involved sinus is the frontal sinus, followed by the ethmoid sinus. Involvement of the sphenoid sinus is considerably rare. Osteomas with a size larger than 3 cm are called giant osteomas. Osteomas are generally asymptomatic and detected incidentally in radiologic examinations (1). In symptomatic cases, the most common symptoms include headache, epistaxis, facial pain, and facial deformity. If they extend towards the orbita, they may lead to signs such as diplopia and proptosis. If they extend towards the intracranial region, they may lead to complications such as cerebral abscess, meningitis, and hemiparesis (3). They may be seen on direct radiography, but CT is the gold standard because it also visualizes small lesions (2). Surgical excision is needed if the lesion is large and disrupts sinus drainage and becomes symptomatic by compressing surrounding tissues or if the osteoma, Sphenoid sinus osteomas should be excised because of their adjacency to the visual pathways, independent of the tumor size. Depending on the location and size of osteomas and the surgeon’s experience, open or endonasal endoscopic surgery or combined surgical treatment may be performed. Recurrence after surgery occurs rarely (3, 4). Giant paranasal sinus osteomas, which are symptomatic and require surgical excision, are observed rarely in the pediatric age group. In the literature, a giant osteoma with a size of 30x25x15 mm in the right ethmoid sinus was found a 12-year-old male patient who presented with frontal headache and increased lacrimation, and it was excised endoscopically (13). Again, a giant orbitoethmoidal osteoma, which manifested with progressive proptosis and limitation in eye movements in a 16-year-old male patient, had to be excised surgically (14). Our patient was a 15-year-old male patient and he had a giant osteoma with a size of 42x28 mm in the frontal sinus. In the literature, development of Pott’s puffy tumor secondary to frontal sinus osteoma was described in an 85-year-old woman who presented with progressive swelling in the frontal region that did not respond to oral flucloxacillin, metronidazole, and co-amoxiclav treatment. This patient was treated with combined surgical methods and broad-spectrum antibiotic combination treatment (15). When we reviewed the present literature, we could not find any case of paranasal sinus osteoma complicated by the development of Pott’s puffy tumor in the pediatric age group. We presented this case to emphasize that symptomatic paranasal sinus osteomas might also occur in children, be complicated by the development of Pott’s puffy tumor, and early diagnosis and treatment are important to prevent intracranial and intraorbital complications.
Footnotes
Informed Consent: Written consent was obtained from the patient who participated in the study and from the patient’s family.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - F.K., N.Ö., K.A.; Design - F.K., N.Ö., K.A., İ.E.Ç., B.E.E.; Supervision - N.Ö., F.K.; Data Collection and/or Processing - F.K., N.Ö., K.A., İ.E.Ç., B.E.E; Analysis and/or Interpretation - N.Ö., F.K.; Literature Review - N.Ö., K.A.; Writing - N.Ö.; Critical Review - F.K., N.Ö., K.A., İ.E.Ç., B.E.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Hasta Onamı: Yazılı hasta onamı çalışmaya katılan hastadan ve hastanın ailesinden alınmıştır.
Hakem Değerlendirmesi: Dış bağımsız.
Yazar Katkıları: Fikir - F.K., N.Ö., K.A.; Tasarım - F.K., N.Ö., K.A., İ.E.Ç., B.E.E.; Denetleme - N.Ö., F.K.; Veri Toplanması ve/veya İşlemesi - F.K., N.Ö., K.A., İ.E.Ç., B.E.E.; Analiz ve/veya Yorum - N.Ö., F.K.; Literatür Taraması - N.Ö., K.A.; Yazıyı Yazan - N.Ö.; Eleştirel İnceleme - F.K., N.Ö., K.A., İ.E.Ç., B.E.E.
Çıkar Çatışması: Yazarlar çıkar çatışması bildirmemişlerdir.
Mali Destek: Yazarlar bu çalışma için mali destek almadıklarını beyan etmişlerdir.
References
- 1.Flora B, Girolamo SD, Passali FM, et al. Paranasal sinüs osteoma:case series and review of literature. Glob J Oto. 2019;19:556017. [Google Scholar]
- 2.Chahed H, Hachicha H, Bachraoui R, et al. Paranasal sinus osteomas:Diagnosis and treatment. Rev Stomatol Chir Maxillofac Chir Orale. 2016;117:306–10. doi: 10.1016/j.revsto.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Keskin İG, İla K, İşeri M, Öztürk M. Paranasal Sinus Osteomas. Türkiye Klinikleri J m-Med Sci. 2013;33:1250–8. [Google Scholar]
- 4.Strek P, Zagólski O, Składzień J, Kurzyński M, Dyduch G. Osteomas of the paranasal sinuses:surgical treatment options. Med Sci Monit. 2007;13:CR244–50. [PubMed] [Google Scholar]
- 5.Özkaya Parlakay A, Kara A, Cengiz AB, Ceyhan M. Puffy frontal edema:a serious life-threatening finding of Pott's puffy tumor:case report. Turkiye Klinikleri J Med Sci. 2012;32:850–3. [Google Scholar]
- 6.Verbon A, Husni RN, Gordon SM, Lavertu P, Keys TF. Pott's puffy tumor due to Haemophilus influenzae:case report and review. Clin Infec Dis. 1996;23:1305–7. doi: 10.1093/clinids/23.6.1305. [DOI] [PubMed] [Google Scholar]
- 7.Babu RP, Todor R, Kasoff SS. Pott's puffy tumor:the forgotten entity. Case report J Neurosurg. 1996;84:110–2. doi: 10.3171/jns.1996.84.1.0110. [DOI] [PubMed] [Google Scholar]
- 8.Minutilli E, Pompucci A, Anile C, et al. Cutaneous fistula is a rare presentation of Pott's puffy tumour. J Plast Reconstr Aesthet Surg. 2008;61:1246–8. doi: 10.1016/j.bjps.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 9.Shehu BB, Mahmud MR. Pott's puffy tumour:a case report. Ann Afr Med. 2008;7:138–40. doi: 10.4103/1596-3519.55663. [DOI] [PubMed] [Google Scholar]
- 10.Park IH, Song JS, Choi H, et al. Volumetric study in the development of paranasal sinuses by CT imaging in Asian:a pilot study. Int J Pediatr Otorhinolaryngol. 2010;74:1347–50. doi: 10.1016/j.ijporl.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Podolsky-gondim GG, Santos M, Carneiro VM, Augusto LP, Pacheco Neto R, Oliveira RS. Neurosurgical Management of Pott's Puffy Tumor in an Obese Adolescent with Asthma:Case Report with a Brief Review of the Literature. Cureus. 2018;10:e2836. doi: 10.7759/cureus.2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells RG, Sty JR, Landers AD. Radiologic evaluation of Pott puffy tumour. JAMA. 1986;255:1331–3. [PubMed] [Google Scholar]
- 13.Alotaibi N, Hanss J, Benoudiba F, Bobin S, Racy E. Endoscopic removal of large orbito-ethmoidal osteoma in pediatric patient:Case report. Int J Surg Case Rep. 2013;4:1067–70. doi: 10.1016/j.ijscr.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abou Al-Shaar H, El Arjani T, Timms MS, Al-Otaibi F. Giant orbitoethmoidal osteoma:when an open surgical approach is required. Case Rep Otolaryngol. 2015;2015:∐38. doi: 10.1155/2015/872038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan MM, Khwaja S, Bhatt YM, Karagama Y. Pott's Puffy Tumor Complicating Frontal Sinus Osteoma-A Case For Combined Approach Surgery. Otolaryngology. 2014;4:152. [Google Scholar]


