Abstract
Gliomas are a dismal disease associated with poor survival and high morbidity. Current standard treatments have reached a therapeutic plateau even after combining maximal safe resection, radiation, and chemotherapy. In this setting, stem cells (SCs) have risen as a promising therapeutic armamentarium, given their intrinsic tumor homing as well as their natural or bioengineered antitumor properties. The interplay between stem cells and other therapeutic approaches such as nanoparticles holds the potential to synergize the advantages from the combined therapeutic strategies. Nanoparticles represent a broad spectrum of synthetic and natural biomaterials that have been proven effective in expanding diagnostic and therapeutic efforts, either used alone or in combination with immune, genetic, or cellular therapies. Stem cells have been bioengineered using these biomaterials to enhance their natural properties as well as to act as their vehicle when anticancer nanoparticles need to be delivered into the tumor microenvironment in a very precise manner. Here, we describe the recent developments of this new paradigm in the treatment of malignant gliomas.
Keywords: biomaterials, nanotechnology, nanoparticles, stem cells, glioma, bioengineering, targeting, surface functionalization
Introduction
Gliomas are a dismal entity, associated with poor survival and high morbidity. The current standard of care has reached a therapeutic plateau even after combining maximal safe resection and chemoradiation (Stupp et al., 2005; Cantrell et al., 2019). In this setting, stem cell therapies have risen as a promising therapeutic approach for gliomas; however, there still exist crucial drawbacks holding its pass to an extensive acceptance in clinical applications. The development of nanomedicine is a parallel phenomenon with potential deep implications in the way stem cells will be introduced into human glioma therapy. Stem cells can be engineered using this nanotechnology in different ways in order to increase our understanding about their biology, improve stem cells antitumor properties, and synergize them with other approaches such as chemotherapy, radiation, thermotherapy, etc. (Kim et al., 2011; Mangraviti et al., 2016; Karlsson et al., 2019; Kozielski et al., 2019; Tian et al., 2020). We aim to provide an overview of the foundations of stem cell therapy and nanoparticles to then explore the potential synergy between these two, through an up-to-date analysis of the benefits of coupling both therapeutic approaches.
Gliomas
Gliomas are the most common and devastating primary brain tumors, representing approximately 75% of these. According to the World Health Organization (WHO), gliomas are classified in four histological grades (I–IV), being the glioblastomas the corresponding WHO grade IV tumor. Glioblastoma (GBM) is the most common and aggressive among all gliomas, accounting for 57.3% of the tumors in this group, with around 12,500 new cases diagnosed every year only in United States (Cantrell et al., 2019; Ostrom et al., 2019). Glioblastomas present a median overall survival of 15 months and a 5-year survival rate of only 4.6% even after maximal therapy (Cantrell et al., 2019). Furthermore, most of the patients diagnosed with gliomas of lower grade, such as astrocytomas and oligodentrogliomas grade II and III (anaplastic), will eventually progress and perish because of the disease. Overall, these facts are just the translation of the need to develop novel therapeutic approaches able to help extend survival and improve the quality of life of patients with the diagnosis of glioma.
Limitation of Current Therapies
The current gold standard for the treatment of gliomas includes surgery and chemoradiation. Maximal safe resection is advised in all cases regardless of the WHO grade, given that the overall survival is positively correlated with the extent of resection (EOR) (McGirt et al., 2008, 2009; Chaichana et al., 2014a,b,c; Mahato et al., 2018; Mampre et al., 2018; Marenco-Hillembrand et al., 2020; Suarez-Meade et al., 2020). However, surgery is not curative in any case. Chemotherapy and radiation are required for high-grade gliomas. Anaplastic astrocytomas and oligodendrogliomas (grade III gliomas) will require chemoradiation depending on clinical parameters and tumor molecular characteristics (Caccese et al., 2020). Glioblastoma tumors require postoperative radiotherapy, with concurrent and adjuvant chemotherapy. Unfortunately, despite this multidisciplinary treatment, gliomas will inevitably recur due to their infiltrative nature and high treatment resistance (Cantrell et al., 2019). By the time of surgery, it is estimated that glioma cells have already migrated beyond the macroscopically identifiable tumor, and thereafter, these cells will ultimately seed local recurrence around the surgical cavity (75–80% of cases) and/or non-local recurrence in the reminder 20–25% of cases (Brandes et al., 2009; Chamberlain, 2011; Drumm et al., 2019).
A subset of gliomas cells have been pinpointed as the culprit of this recurrence. The glioma cancer stem cells (CSCs) are a subgroup of malignant cells with the potential of self-renewal, forming tumors that resemble the original pathology, as well as high resistance to current chemotherapeutics and radiation (Singh et al., 2003; Galli et al., 2004; Beier et al., 2007; Li et al., 2009; Cheng L. et al., 2013; Dahan et al., 2014). These cells migrate beyond the macroscopic tumor, infiltrating apparent normal brain parenchyma by the time of surgery and survive even after receiving high-dose radiation and chemotherapy (Li et al., 2009; Lathia et al., 2012). As these cells migrate beyond the tumor bulk to seed further recurrence, a therapeutic strategy able to track these newly developed microscopic glioma foci to deliver antitumor cargoes is of utmost importance. In this setting, the use of neural and mesenchymal stem cells (MSCs) as a therapeutic armamentarium against gliomas represents a potential avenue to achieve this goal and alter the treatment paradigm of this dismal cancer (Pendleton et al., 2013; Li et al., 2014; Smith et al., 2015; Mangraviti et al., 2016).
Stem Cells as Elements of Therapy for Malignant Glioma
Stem cells have risen as a promising therapeutic option for the treatment of malignant gliomas, as they would be able to migrate and home into glioma tumors, including microscopic tumor foci, which harbor the potential to seed future recurrence (Brown et al., 2003; Nakamura et al., 2004; Kim et al., 2005, 2018; Sonabend et al., 2008; Thu et al., 2009; Yong et al., 2009; van Eekelen et al., 2010; Amano et al., 2011; Choi et al., 2011; Kleinschmidt et al., 2011; Ryu et al., 2011; Altanerova et al., 2012; Jiao et al., 2012; Kosaka et al., 2012; Cheng Y. et al., 2013; Huang et al., 2013, 2014; Lee et al., 2013; Balyasnikova et al., 2014; Li et al., 2014; Mooney et al., 2014b; Bryukhovetskiy et al., 2015; de Melo et al., 2015; Martinez-Quintanilla et al., 2015; Morshed et al., 2015; Park et al., 2015; Cheng S. H. et al., 2016; Kim S. J. et al., 2016; Kim S. M. et al., 2016; Liu et al., 2016; Mangraviti et al., 2016; Muroski et al., 2016; Meca-Cortes et al., 2017; Portnow et al., 2017; Hsu et al., 2018; Lang et al., 2018; Pavon et al., 2018; Tirughana et al., 2018; Zhang et al., 2018; Huang R. Y. et al., 2019; Tanrikulu et al., 2019; Allahverdi et al., 2020; Jabbarpour et al., 2020). Stem cells are relatively easy to grow in vitro and can be bioengineered to deliver a wide range of antitumor payloads such as proteins, oncolytic viruses, prodrugs, small interfering RNA (siRNA), and nanoparticles (Brown et al., 2003; Nakamura et al., 2004; Kim et al., 2005, 2018; Sonabend et al., 2008; Thu et al., 2009; Yong et al., 2009; van Eekelen et al., 2010; Amano et al., 2011; Choi et al., 2011; Kleinschmidt et al., 2011; Ryu et al., 2011; Altanerova et al., 2012; Jiao et al., 2012; Kosaka et al., 2012; Cheng Y. et al., 2013; Huang et al., 2013, 2014; Lee et al., 2013; Balyasnikova et al., 2014; Li et al., 2014; Mooney et al., 2014b; Bryukhovetskiy et al., 2015; de Melo et al., 2015; Martinez-Quintanilla et al., 2015; Morshed et al., 2015; Park et al., 2015; Cheng S. H. et al., 2016; Kim S. J. et al., 2016; Kim S. M. et al., 2016; Liu et al., 2016; Mangraviti et al., 2016; Muroski et al., 2016; Meca-Cortes et al., 2017; Portnow et al., 2017; Hsu et al., 2018; Lang et al., 2018; Pavon et al., 2018; Tirughana et al., 2018; Zhang et al., 2018; Huang R. Y. et al., 2019; Tanrikulu et al., 2019; Allahverdi et al., 2020; Jabbarpour et al., 2020).
Stem cells are undifferentiated cells with capacity of self-renewal and differentiation by definition. They can mature along symmetric and asymmetric replication processes. The later type of cell division will result in different hierarchies within stem cell niches, which will now include progenitor cells; these are daughter cells retaining the same stem cells properties but with a de novo limited differentiation ability (Young et al., 2014).
Stem Cell Classification
Stem cells can be designated according to their developmental status as adult, fetal, or embryonic stem cells. Their differentiation potential can further define them as totipotent, pluripotent, or multipotent stem cells. Totipotent stem cells are only found during the very first days of life just after fecundation and have the capacity to derive into any type of human cells, including placental tissues. Once the embryo has reached the blastocyst stage, cells contained inside the inner cell mass are defined as pluripotent, as they can differentiate into any cell of all three germ layers but no placental tissues (Takahashi and Yamanaka, 2006; Qiao et al., 2018; Andres et al., 2019; Klimanskaya, 2019). Eventually, these pluripotent stem cells will restrict their differentiation potential to only one of the three germ cell layers and thereafter will be defined as multipotent stem cells, which can actually be harvested from most of the organs of the human body (Takahashi and Yamanaka, 2006; Qiao et al., 2018; Andres et al., 2019; Klimanskaya, 2019).
Stem cells used in glioma therapy are usually multipotent cells obtained from adult or fetal organs. In particular, neural stem cells (NSCs), mesenchymal stem cells (MSCs), and hematopoietic stem cells (HSCs) are the most common multipotent stem cells used with this purpose (Aboody et al., 2000; Portnow et al., 2017). It is noteworthy, however, that pluripotent cells such as the induced-pluripotent stem cells (iPSC) or embryonic pluripotent stem cells have also been described in cell therapy against glioma (Parker Kerrigan et al., 2018; Table 1).
TABLE 1.
Classification and major features of stem cells reported in glioma therapy.
| Stem cell | Defining criteria | Source/Niche | Linage |
| Pluripotent stem cells: capacity to differentiate into any cell of all three germ layers | |||
| Embryonic stem cells (ECSs) | Markers of pluripotency as found in ICM cells: Transcription factors: Oct4, Nanog, Rex-1 Cell surface markers: SSEA-3, SSE-A4, TRA-1-60, TRA-1-81, alkaline phosphatase |
Blastocyst Morula Growth-arrested embryos Somatic cell nuclear transfer Single blastomere | As defined by pluripotency |
| Induce pluripotent stem cells (iPSCs) | Essentially the same than ECS markers | Reprogrammed adult somatic cells—usually fibroblasts or skin cells. | As defined by pluripotency given than iPSC are functionally equivalent to ECS |
| Multipotent stem cells: capacity to differentiate into cells of one of the three germ layers | |||
| Neural stem cells (NSCs) |
Positive: GFAP, CD133, CD184, and Nestin, Sox1, Sox2, and Pax6 Negative: CD271, CD44, CD24 Immune profile: Absent HLA II |
Subependymal zone (SEZ)—lining the lateral ventricles Dentate gyrus of the hippocampus *Obtained from fetal and adult mammals | Neurons Oligodendrocytes Astrocytes Ependymal cells |
| Mesenchymal stem cells (MSCs) | MSC must comply with ISCT criteria: Positive (>95% +): CD105, CD73, CD90 Negative (<2% –): CD45, CD34, CD14 or CD11b, CD79α, or CD19, HLA DR Adherence to plastic in standard culture conditions In vitro differentiation to osteoblast, adipocytes, and chondroblasts. Immune profile: Absent HLA II |
Adult tissues: adipose tissue, bone marrow, peripheral blood, dental pulp, ligamentum flavum, synovium, endometrium, sweat glands, and milk Fetal tissues: umbilical cord, umbilical cord blood, Wharton jelly, amniotic fluid, chorionic villi, and placenta |
Osteoblast Adipocytes Chondroblast *Differentiation into ectodermal and endodermal linages has also been reported |
| Hematopoietic stem cells (HMSs) |
Negative: CD45R/B220 (B cells), Gr-1 (granulocytes), Mac-1 (macrophages), Ter-119 (erythrocytes) and CD4/CD8 (lymphocytes)—for phenotypic enrichment. Positive: Sca-1, c-Kit, CD150 *They appear as side population in dye exclusion assays due to the high expression of MDR pumps |
Adult tissues: bone marrow, peripheral blood Non-adult tissues: umbilical cord blood, yolk sac, liver, spleen |
Hematopoietic cells |
IMC, inner mass cells; MDR, multidrug resistance.
Development of Stem-Cell-Based Glioma Therapy
The use of stem cells in glioma therapy relies on their tumor-homing properties. This property was first described in 2000 by Aboody et al. The group presented a seminal paper describing the glioma tropism of neural stem cells. The study reported on the capacity of NSC for engrafting into the glioma bulk when intratumor NSC injections were performed, invading normal parenchyma only when tumor cells migrate far from the tumor mass; with this, they also showed the specific NSC ability to track glioma cancer cells infiltrating along healthy tissue. NSCs were also proven to migrate toward glioma tumor masses when implanted distally to these, through ipsilateral, contralateral, and intraventricular NSC injections (Aboody et al., 2000). These abilities and the possibility of being bioengineered to secrete antiglioma cargoes turned NSC into a promising glioma treatment, able to track and tackle this infiltrative malignant tumor. Importantly, NSC showed to retain their stem cell properties and had been proven non-tumorigenic (Snyder et al., 1992). In 2017, the same group published the first phase I clinical trial where NSC-based antiglioma therapy was proven safe; the proof of concept of NSC tumor homing was also demonstrated by the group (Portnow et al., 2017). Unfortunately, despite the encouraging role of NSC in glioma therapy, limited availability of human NSC (hNSC) as well as ethical concerns regarding its use encouraged researchers to seek alternatives sources of stem cells.
Mesenchymal stem cells (MSCs) were first described by Friedenstein more than 50 years ago (Friedenstein et al., 1968, 1970, 1974). He initially isolated MSC from rodent bone marrow and proved that they were able to differentiate into mesenchymal tissue (adipogenic, chondrogenic, and osteogenic differentiation). MSCs ended up being an alternative to the difficult-to-obtain NSC, as they are abundant in several adult and fetal tissues such as bone marrow (BM-MSC) (Friedenstein et al., 1968, 1970, 1974), adipose tissue (A-MSC) (Zuk et al., 2001; Katz et al., 2005; Wagner et al., 2005), umbilical cord (UC-MSC) (Girdlestone et al., 2009), umbilical cord blood, Wharton jelly (Erices et al., 2000; Zeddou et al., 2010), endometrium (Meng et al., 2007), dental pulp (Agha-Hosseini et al., 2010), ligamentum flavum (Chen et al., 2011), etc. (Kassis et al., 2006; Miao et al., 2006; Roubelakis et al., 2007; Poloni et al., 2008; Patki et al., 2010; Ma et al., 2018). MSCs are easy to harvest and isolate even from adult individuals, which would allow for using patient-derived MSC as autografts in glioma patients, thus avoiding ethical dilemmas as well as fears about immune-mediated allograft rejection. In this context where MSCs could be isolated from a variety of tissue sources, cultured following different methodologies, and be defined by using different surface markers, the Mesenchymal and Tissue Stem Cell Committee of the International Society for Cellular Therapy (ISCT) proposed a standard set of minimum criteria defining MSC for both laboratory-based scientific investigations and preclinical studies (Dominici et al., 2006). Thus, every study currently under development should follow these guidelines in order to assure a better cell homogeneity among different laboratories and greater reproducibility.
The first report on the use of MSC in the treatment of gliomas came from Nakamura et al. In 2004, the group demonstrated that MSCs also possessed glioma-homing properties by proving rat-derived BM-MSC homing in a rat glioma model. In 2005, Nakamizo et al. were able to replicate the findings using human BM-MSC on a murine model harboring glioma xenograft derived from commercial human cell lines (U87, U251, and LN229). Furthermore, both groups were able to bioengineer the MSCs to deliver antitumor cargoes. To date, several reports on the use of MSC as key elements for glioma stem cell therapy have been published with exceptional promising results (Table 2; Brown et al., 2003; Nakamura et al., 2004; Kim et al., 2005, 2018; Sonabend et al., 2008; Thu et al., 2009; Yong et al., 2009; van Eekelen et al., 2010; Amano et al., 2011; Choi et al., 2011; Kleinschmidt et al., 2011; Ryu et al., 2011; Altanerova et al., 2012; Jiao et al., 2012; Kosaka et al., 2012; Cheng Y. et al., 2013; Huang et al., 2013, 2014; Lee et al., 2013; Balyasnikova et al., 2014; Li et al., 2014; Mooney et al., 2014b; Bryukhovetskiy et al., 2015; de Melo et al., 2015; Martinez-Quintanilla et al., 2015; Morshed et al., 2015; Park et al., 2015; Cheng S. H. et al., 2016; Kim S. J. et al., 2016; Kim S. M. et al., 2016; Liu et al., 2016; Mangraviti et al., 2016; Muroski et al., 2016; Meca-Cortes et al., 2017; Portnow et al., 2017; Hsu et al., 2018; Lang et al., 2018; Pavon et al., 2018; Tirughana et al., 2018; Zhang et al., 2018; Huang R. Y. et al., 2019; Tanrikulu et al., 2019; Allahverdi et al., 2020; Jabbarpour et al., 2020).
TABLE 2.
Stem cell therapy in glioma.
| Stem cell type | Delivery routes | Applications |
| Neural stem cellsa,b | • Intravascular: vein(Brown et al., 2003) • Intracranial (Mooney et al., 2014b; Morshed et al., 2015) • Intraventricular • Intracerebral (Altanerova et al., 2012; de Melo et al., 2015) |
Prodrug activating enzymes: CD (Portnow et al., 2017), rCE, and hCE1m6 (Mooney et al., 2014b), HSV-TK (Uhl et al., 2005; Tamura et al., 2020) Oncolytic viruses: CRAd-S-pk7 (Morshed et al., 2015) Cargo proteins: IL-4 (Benedetti et al., 2000), IL-12 (Ehtesham et al., 2002), PF-4 (Lee et al., 2003), TRAIL (Balyasnikova et al., 2011), PEX (Kim et al., 2005), BMP4 (Liu et al., 2016), TSP-1 (van Eekelen et al., 2010) Nanoparticles (Mooney et al., 2014b) |
|
||
| Mesenchymal stem cells | ||
| Adipose-derived | • Intranasal (Balyasnikova et al., 2014) • Intracranial (Altanerova et al., 2012; de Melo et al., 2015) |
Prodrug activating enzymes: yeast CD (Altanerova et al., 2012), HSV-TK (Meca-Cortes et al., 2017)(c), (de Melo et al., 2015) Oncolytic viruses: ICOVIR17 (Martinez-Quintanilla et al., 2015) Cargo proteins: TRAIL (Balyasnikova et al., 2014; Tanrikulu et al., 2019) Oligonucleotides: miR-4731 (Allahverdi et al., 2020) |
| Bone marrow-derived | • Intratumoral (Kosaka et al., 2012; Lee et al., 2013): alginate microencapsulated (Kleinschmidt et al., 2011) • Intracarotid (Yong et al., 2009) |
Prodrug activating enzymes: CD (Kosaka et al., 2012), HSV-TK (Amano et al., 2011) Oncolytic viruses: Delta24-RGD (Yong et al., 2009), CRAd (Sonabend et al., 2008)*** Cargo Proteins: IL2 (Nakamura et al., 2004), INF-B (Park et al., 2015), TRAIL (Choi et al., 2011), BMP4 (Li et al., 2014; Mangraviti et al., 2016) Oligonucleotides: miR-124 (Lang et al., 2018; Lee et al., 2013) and miR-145 (Lee et al., 2013), miRNA-584-5p (Kim et al., 2018) Nanoparticles: |
|
||
| Human placenta-derived | • Intratumoral (Lee et al., 2013) |
Cargo proteins: NK4 (Jabbarpour et al., 2020) Oligonucleotides: miR-124 and miR-145 (Lee et al., 2013) Nanoparticles |
|
||
| Umbilical cord-derived | • Intratumoral (Lee et al., 2013) • Intravascular: tail vein (Pavon et al., 2018) |
Cargo proteins: IL12 (Ryu et al., 2011) Oligonucleotides: miR-124 and miR-145 (Lee et al., 2013) Nanoparticles
|
| Amniotic membrane-derived | • Intratumoral (Jiao et al., 2012) | Direct antiglioma properties: increased apoptosis (Jiao et al., 2012) |
| Hematopoietic progenitor cells | • In vitro (Bryukhovetskiy et al., 2015) | Migration in an in vitro model (Bryukhovetskiy et al., 2015) |
CD, cytosine deaminase; rCE, rabbit carboxylesterase; hCE1m6, modified human carboxylesterase; MSN-Dox, doxorubicin loaded-mesoporous silica nanoparticles; FE-Pro, ferumoxide–protamine sulfate complex; FTD, FerraTrack Direct; NIR675, NEO-LIVE, Magnoxide 675 nanoparticles; MSN, mesoporous silica nanoparticles; MTN, magnetic ternary nanohybrid; IO MNP, iron-based magnetic nanoparticles; MNP, mesoporous nanoparticles; NK4, hepatocyte growth factor antagonist; PEG-SPIO, polyethylene glycol-superparamagnetic iron oxide; PF-4, platelet factor 4.
*MSC were found to promote tumor growth.
**2u magnetic disks.
***Only specified as human MSC.
aGMP production and scale-up of these cells have been performed (Tirughana et al., 2018).
bFirst-in human studies have been performed assessing safety of intracranial injection (Portnow et al., 2017).
cModified MSC produced by CRISPR/Cas9.
On the other hand, not all are in agreement, as there has been a risen controversy in which some authors have described that MSCs could eventually support glioma tumor growth. Different types of MSCs such as BM-MSC, A-MSC, and UC-MSC have been associated with these proglioma effects through increased proliferation, cancer cells migration, angiogenesis, transition to epithelial–mesenchymal phenotype, and decreased glioma apoptosis (Iser et al., 2016; Ridge et al., 2017); however, this adverse phenotype would vary on a differential basis depending on specific glioma tumors (Breznik et al., 2017). In this same line, brain tumor-derived MSC (BT-MSC) have also been described in mouse- and human-derived glioma tumors supporting glioma microenvironment (Behnan et al., 2014; Guo et al., 2014; Svensson et al., 2017; Yi et al., 2018). In support to these findings, Shahar et al. showed that higher percentages of human BT-MSC directly correlate with worse patient prognosis (Shahar et al., 2017). Overall, these data would suggest that stem cell therapy should be carefully selected in future translational efforts.
In order to improve different aspects of stem cell therapies against glioma, different approaches have been studied. The use of nanoparticles for stem cell bioengineering is one of these potential approaches and will be discussed in the following section.
Nanoparticles as Elements of Therapy for Malignant Glioma
Nanoparticles (NPs) are defined as nanomaterials sized between 1 and 100 nm in at least one of their external dimensions, which confer them a high surface/volume ratio (European Commission, 2011). Due to this small size, they present significantly different properties when compared to conventional materials of non-nanometric scale. The optical, magnetic, electronic, and biological properties of these nanomaterials can be tuned by size, shape, surface modifications (functionalization), or even by combining them with different materials in order to create new heterostructured nanoparticles (Thimsen et al., 2014; Lee et al., 2017).
In Nano-oncology, nanoparticles represent an important diagnostic and therapeutic tool, as they can be designed to interact with most biological system with great precision and specificity. This is possible due to their particular physicochemical characteristics and the possibility of making them able to target a specific tissue, specific cell types, or a specific cellular compartment (targeted functionalization) (Portney and Ozkan, 2006). The potential benefits of these nanomaterials in medicine have led some of them to obtain Food and Drug Administration (FDA) approval to be investigated under several clinical protocols (Table 3).
TABLE 3.
Advances in the uses of nanoparticles in glioma therapy and diagnosis.
| Use | Experimental setting and nanoparticle type |
Nanocarrier: Drug bioavailability/therapeutic efficacy enhancer
|
Preclinical:
|
| Standalone therapy | Preclinical
|
| Drug sensitizer | Temozolomide: direct attenuation on EGFR and MET signaling, through delivered miRNAs (Meng et al., 2020) |
| Imaging technologies enhancer | Fluorescence: USPION (Denora et al., 2019) |
| Magnetic hyperthermia |
Clinical
|
Preclinical
|
|
| Sonodynamic therapy | Preclinical
|
| Radiotherapy enhancer | Charged particles |
|
|
Photon therapy (X-rays)
|
|
| Photodynamic therapy enhancer | Preclinical
|
| Immunotherapy enhancer | Functionalization with anti-PDL1 (Ruan et al., 2019; Zhang et al., 2019) |
SPION, superparamagnetic iron oxide nanoparticles; USPION, ultrasmall SPION; PLGA, poly-lactide-co-glycolic acid; PEG, polyethylene glycol; RGD, arginyl-glycyl-aspartic tripeptide; TPLN, FONP, fluorescent organic nanoparticles; pSiNPs, porous silicon nanoparticles; terpolymer-lipid nanoparticles; MP, permalloy magnetic particles; FA-AuNC, folic acid gold nanoclusters; AuNP, gold nanoparticles, AgNP, silver nanoparticles; AGuIX, gadolinium-based nanoparticle; 5-ALA, 5-aminolevulinic acid; AuNS, gold nanospheres; ICG, indocyanine green; HSPA5, heat shock protein A5r4t. *Theranostic NP: Possesses diagnostic and therapeutic functions. aImprove CT/MRI imaging and also works as radiosensitizer by AuNS properties and loading an HSPA inhibitor.
Targeted Functionalization
In order to achieve a targeted distribution at a cellular or even intracellular level, NPs can be functionalized via active targeting. Active targeting is achieved by different methods; a method called ligand targeting works by coating the nanoparticles’ surface with one or more ligands such as transferrin, epidermal growth factor (EGF), folic acid, arginyl-glycyl-aspartic tripeptide (RGD) peptide, hyaluronic acid, antibodies, and others (Ruiz-Garcia et al., 2020). These ligands allow NPs to bind specific “receptors” differentially expressed only in certain cancerous blood vessels and/or tumor cells, thus leading to a precise cellular internalization (Maier-Hauff et al., 2007; Kim et al., 2010; Wegscheid et al., 2014; Cheng Y. et al., 2016; Shen et al., 2017; Yu et al., 2017, 2019; Hua et al., 2018; Daniel et al., 2019; Denora et al., 2019; Dufort et al., 2019; Kefayat et al., 2019; Kunoh et al., 2019; Luque-Michel et al., 2019; Rego et al., 2019, 2020; Ruan et al., 2019; Shi et al., 2019; Sousa et al., 2019; Ye et al., 2019; Zhang et al., 2019; Zhao et al., 2019; ZhuGe et al., 2019; Alves et al., 2020; Caban-Toktas et al., 2020; Chung et al., 2020; Ferreira et al., 2020; Kazmi et al., 2020; Liang et al., 2020; Martinez-Rovira et al., 2020; Meng et al., 2020; Roberts et al., 2020; Ullah et al., 2020; Wang H. et al., 2020; Wang X. et al., 2020; Xu et al., 2020; Zhu et al., 2020; see Table 3 for examples of ligand targeting in glioma research).
Another active targeting method to increase functional specificity of NPs that are used as gene delivery systems is the transcriptional targeting, which can occur at a transcriptional or posttranscriptional level (Golombek et al., 2018). Here, the delivered gene includes a tumor-specific promoter (highly functional only in cancer cells), which will secure a well-localized expression of the transgene, limited to occur only inside the cancer cells of interest. Posttranscriptional regulations of the product encoded by the exogenously delivered gene are achieved by controlling RNA splicing, RNA stability, and initiation of the RNA translation once it is present in the cancer cell (Maier-Hauff et al., 2007; Kim et al., 2010; Wegscheid et al., 2014; Cheng Y. et al., 2016; Shen et al., 2017; Yu et al., 2017; Hua et al., 2018; Daniel et al., 2019; Denora et al., 2019; Dufort et al., 2019; Kunoh et al., 2019; Luque-Michel et al., 2019; Ruan et al., 2019; Rego et al., 2019, 2020; Shi et al., 2019; Sousa et al., 2019; Ye et al., 2019; Zhang et al., 2019; Zhao et al., 2019; ZhuGe et al., 2019; Alves et al., 2020; Caban-Toktas et al., 2020; Chung et al., 2020; Ferreira et al., 2020; Kazmi et al., 2020; Liang et al., 2020; Martinez-Rovira et al., 2020; Meng et al., 2020; Roberts et al., 2020; Ullah et al., 2020; Wang H. et al., 2020; Wang X. et al., 2020; Xu et al., 2020; Zhu et al., 2020).
To date, several nanoparticles have shown to be effective in improving different aspects of traditional and novel cancer therapeutic approaches, to the point that several nanocarriers and nanoradiotherapy enhancers are being studied in phase II and III clinical trials (Maier-Hauff et al., 2007; Kim et al., 2010; Wegscheid et al., 2014; Cheng Y. et al., 2016; Shen et al., 2017; Yu et al., 2017; Hua et al., 2018; Daniel et al., 2019; Denora et al., 2019; Dufort et al., 2019; Kunoh et al., 2019; Luque-Michel et al., 2019; Rego et al., 2019, 2020; Ruan et al., 2019; Shi et al., 2019; Sousa et al., 2019; Ye et al., 2019; Zhang et al., 2019; Zhao et al., 2019; ZhuGe et al., 2019; Alves et al., 2020; Caban-Toktas et al., 2020; Chung et al., 2020; Ferreira et al., 2020; Kazmi et al., 2020; Liang et al., 2020; Martinez-Rovira et al., 2020; Meng et al., 2020; Roberts et al., 2020; Ullah et al., 2020; Wang H. et al., 2020; Wang X. et al., 2020; Xu et al., 2020; Zhu et al., 2020). In the next section, we will briefly review the role of nanoparticles as a standalone therapeutic approach for glioma tumors (Table 3), and then, we will review in detail the role of nanoparticles as a tool to further improve stem cell therapy (Table 4).
TABLE 4.
Rational for a combinatorial approach using nanoparticles and stem cell therapy in malignant glioma.
| Rational for nanoparticle-based stem cell therapy in malignant glioma | |
| Drawbacks of using nanoparticles alone |
|
| Potential advantages of using combine therapy |
|
BBB, blood brain barrier; CSC, cancer stem cells.
Classification
Nanoparticles can naturally occur in the environment mediated by biological or geological processes (Sharma et al., 2015), or as incidental by-product of human activities such as smelting or other processes involving the generation of metal fumes (Gonzalez-Pech et al., 2019). In addition, nanoparticles can be artificially synthetized and engineered (Kus et al., 2018). Given the wide variety of existing NPs, classification criteria are also abundant. We present the classification of NPs according to their origin and structure, as they will help understand the terminology used to describe NPs used in cancer research.
Classification of Nanoparticles Based on Its Origin
Organic
Organic nanoparticles are based on natural compounds such as lipids, glycosides, peptides and others, as well as synthetic organic molecules (Romero and Moya, 2012; Tzeng et al., 2016; Kus et al., 2018; Karlsson et al., 2019; Kozielski et al., 2019; Tian et al., 2020). These organic elements can arrange themselves in three-dimensional (3D) structures (Euliss et al., 2006), which is one of the main characteristics that differentiate organic from inorganic nanoparticles, as inorganic NPs do not form these 3D structures in any case (Romero and Moya, 2012). Furthermore, due to the weak interactions that hold many organic NPs together, they present a dynamic nature that allows, for example, for fusion and generation of larger structures depending on external conditions (Romero and Moya, 2012).
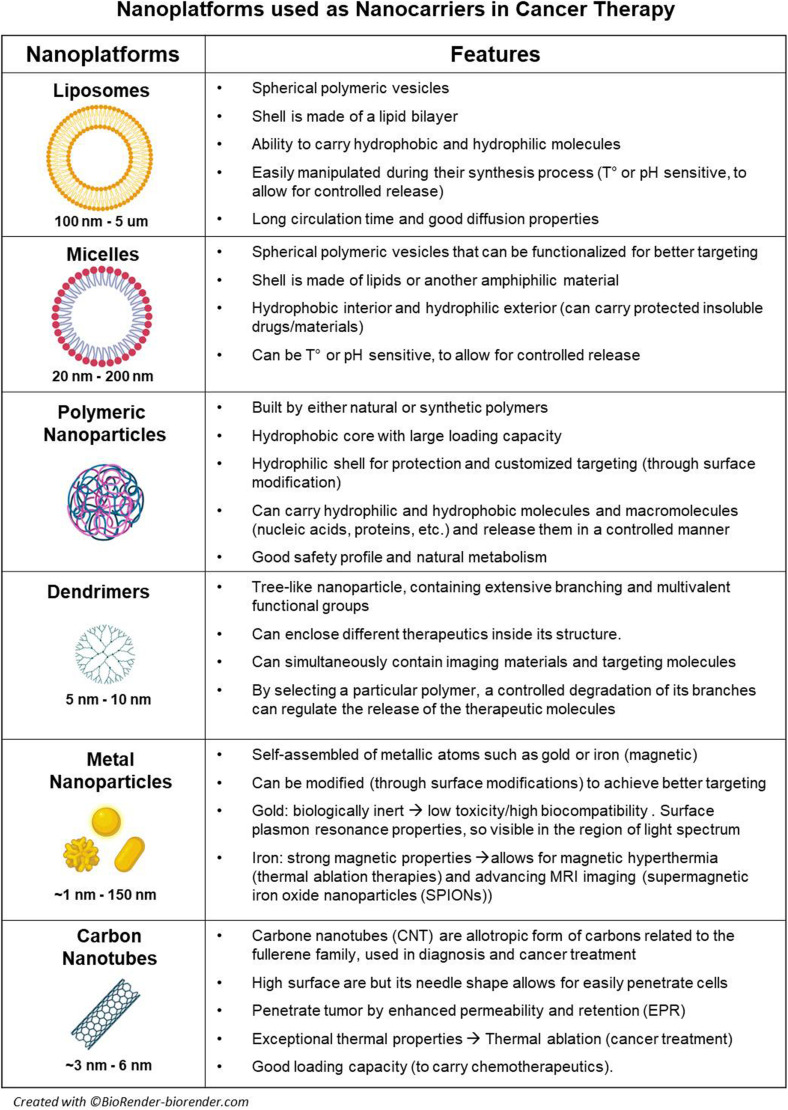
Organic nanoparticles display highly desirable characteristics in the biomedical field (Hussein Kamareddine et al., 2019). They have a dynamic nature and are able to respond to environmental variations in temperature, pH, and UV radiation (Jagannathan et al., 2006; Affram et al., 2017; Hussein Kamareddine et al., 2019). Furthermore, they can easily cross biological barriers and are considered less toxic due to its biodegradability; therefore, they are ideal as drug or gene delivery systems (Jagannathan et al., 2006; Hussein Kamareddine et al., 2019). Liposomes, vesicles, micelles, polymeric NPs, and dendrimers are all among the most common organic nanoparticles (for specific characteristic and applications, see Figure 1); however, among all of them, polymeric NPs are probably the most relevant in cancer research.
FIGURE 1.
Nanoplatforms used as nanocarriers in cancer therapy.
Polymeric NPs, also known as polymeric nanospheres, are commonly defined as solid polymer particles with matrix type structure, where a cargo can be embedded within the polymer matrix or included in the surface (Reis et al., 2006). Based on its origin, polymeric NPs can be classified as natural or synthetic. The first group contains NPs such as chitosan, which is a widely available natural cationic carbohydrate polymer approved by the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for drug and gene delivery and tissue engineering in humans (Lara-Velazquez et al., 2020). The second group, or synthetic polymer-based nanoparticles (SP-NPs), is the most relevant in medicine, as they can be easily synthesized and their properties can be tailored according to specific needs.
SP-NPs are prepared using synthetic polymers (Romero and Moya, 2012), which can be classified in polyesters such as poly(glycolic acid) (PGA), poly(lactic acid) (PLA), poly(caprolactone) (PCL), and poly(lactic-co-glycolic acid) or (PLGA); polyalkyl alcohols such as polyvinyl alcohol or PVA; and polyethers such as poly(ethylene glycol) (PEG) and poly(propylene glycol) (PPG) (Ranganathan et al., 2018). Currently, there are around 15 FDA-approved nanomedicines based on SP-NPs, 6 of them are used in cancer therapy (Bobo et al., 2016; Farjadian et al., 2019). Up to date, glioma research based on SP-NPs has been mainly focused on the development of more effective delivery systems, able to cross the blood brain barrier and specifically target the cancer cells (Ambruosi et al., 2006; Hua et al., 2011; Jiang et al., 2011; Guo et al., 2013; Bishop et al., 2016; Tzeng et al., 2016; Karlsson et al., 2019; Kozielski et al., 2019). This includes the generation of hybrid systems using booth synthetic polymers and natural compounds (Agrawal et al., 2015; Cook et al., 2015; Alex et al., 2016; Wang et al., 2017; Qi et al., 2020), as well as smart nanoparticles able to react according to the surrounded conditions or to specific stimulus (Soppimath et al., 2005; McNeeley et al., 2009; An et al., 2015; Mangraviti et al., 2015; Gao et al., 2016; Ye et al., 2019).
Inorganic
Inorganic nanoparticles present unique physicochemical properties (optical, magnetic, etc.), inertness, high stability, and easy functionalization, which give them different advantages when compared to organic NPs. Due to their cellular internalization ability and low immunogenic response, these nanoparticles were initially used as drug and gene delivery systems (Xu et al., 2006; Evans et al., 2019). Different types of elements and inorganic compounds based on metals [metal NP (mNP)], metalloids, or non-metals such as gold, silver, iron, magnesium, silicon, and others are differentially arranged and/or combined in order to display specific properties. Thus, there are some particular groups of NPs such as magnetic nanoparticles, which are usually based in a core of iron oxide mNP with a large magnetic momentum under an external magnetic field, which allow its use as MRI contrast enhancer and thermotherapy agents (Maier-Hauff et al., 2007; van Landeghem et al., 2009; Wegscheid et al., 2014). Plasmonic nanoparticles refer to mNPs such as gold (Au) or silver (Ag) NPs presenting with surface plasmon resonance (SPR), meaning that NP free electrons can be excited by electromagnetic fields (UV or infrared light) and resonate, creating the possibility to sense these changes (biosensors), produce heat (photothermal ablation/therapy), or create technologies such as surface-enhanced Raman spectroscopy (SERS) (Kaur et al., 2016; Chen et al., 2018; Liu et al., 2018). Quantum dots (Qdots) are another group of inorganic NPs, usually smaller than 50 nm; these semiconductor NPs efficiently produce bioluminescence once excited by UV light, which has led them to be used in single cell and in vivo imaging (Xu et al., 2006; Figure 1).
Carbon Based
These nanoparticles are predominantly composed by carbon, and their discovery revolutionized diverse scientific fields (Cha et al., 2013; Patel et al., 2019). Carbon-based nanomaterials have outstanding properties like high mechanical strength, thermoelectrical conductivity, and flexibility (Cha et al., 2013). These nanoparticles include fullerenes (carbon nanotubes), graphene, and nanodiamonds. Their broad range of properties makes these materials ideal imaging agents for tumor diagnosis (Patel et al., 2019; Figure 1).
Classification of Nanoparticles Base on Their Structure
Single Nanoparticles
Single nanoparticles are made of a single element such as gold, silver, copper, among others, and due to their homogeneity and electrochromic properties, they are widely used in electro-optical applications, energy conversion, and storage (Evans et al., 2019). Diverse systems for synchronized release of multiple drugs for cancer therapy have been designed based on single nanoparticles (Liao et al., 2014).
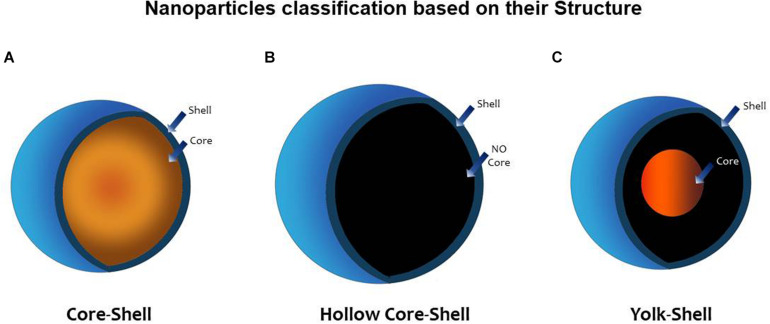
Heterostructured Nanoparticles
In an attempt to increase the performance and functionality of nanomaterials, heterostructured nanoparticles composed of two or more different materials were created. This technology allowed for the design of advanced NPs with additional properties arising from the synergy of the different materials (Wei and Zhao, 2016). One method to concrete this effort was to coat nanoparticles with one or more layers. Nanoparticles created in this way can be classified as core–shell (CS), when a central core (NP) is surrounded by one or more layers of different material [shell(s)], or as yolk–shell (YS). when the a movable core is located in a hollow cavity surrounded by a shell (Purbia and Paria, 2015). A hollow core–shell structure or hollow NP is another term referred to a NP without a core; the resulting empty space inside the shell can then be loaded with drugs, microRNA (miRNA), genes, peptides, and others that can now be released in a controlled manner. Janus nanoparticles are a different type of nanomaterials; they possess a tunable asymmetric structure; their surface has two or more regions with different properties, which confer them unique properties as selective reactivity or directional interactions. The field of application is broad and innovative including its use as sensors, self-propelled carriers, or coatings (Agrawal and Agrawal, 2019; Figure 2).
FIGURE 2.
Nanoparticle classification based on its structure. (A) Core–shell (CS) nanoparticle (NP) possesses a central core (NP) surrounded by one or more layers of different material [shell(s)]. (B) Hollow core–shell structure or (hollow NP) refers to an NP without a core; the resulting empty space inside the shell can then be loaded with drugs, microRNA (miRNA), genes, peptides, and others that can now be released in a controlled manner. (C) Yolk–shell (YS) NP possesses a movable core that is located in a hollow cavity surrounded by a shell (Purbia and Paria, 2015).
Nanoparticles as a Theragnostic Approach in Glioma
Nanoparticles as Radiosensitizers
Cancer tumors frequently contain a chemo and/or radioresistant subpopulation that survives and proliferates after standard treatments, contributing to the recurrence of a more aggressive tumor (Dahan et al., 2014; Yuan et al., 2018). Cancer stem cells (CSCs) represent this treatment-resistant subpopulation, and huge efforts are being focused on developing strategies to make them more amenable to current and novel therapies. The use of radiosensitizers is a potential approach to overcome radioresistance; however, its principal shortcoming is the lack of target specificity, which may lead to low concentrations in tumor tissue and toxic effects in healthy cells.
In this regard, nanoparticles have been tested as radiosensitizers agents and also as radiosensitizers carriers, showing promising results after photon and particle radiation (Caban-Toktas et al., 2020; Chung et al., 2020; Kazmi et al., 2020). For instance, Kunoh et al. developed DNA–gold nanoparticles complexes to work as radiosensitizers; they showed good cellular targeting and being effective in inducing cell death by mitotic catastrophe in glioma CSC after X-ray irradiation (Kunoh et al., 2019). Kefayat et al. also described good performance of folic-acid-coated gold nanocluster in radiosensitizing orthotopic C6 glioma tumor in a murine model (Kefayat et al., 2019). Folic acid receptors are differentially expressed in the luminal side of cancerous blood–brain barrier (BBB) endothelial cells as well as in cancer cells but not in normal tissues, which explain the higher concentration of these NP in glioma tumor when compared to a healthy brain tissue (Kefayat et al., 2019).
Furthermore, in order to target the glioma-resistant population specifically located in the tumor hypoxic niche, Hua et al. developed hypoxia-responsive yolk–shell nanoparticles (liposomes) by encapsulating radiosensitizer hydrophobic drugs [aniopep-2-poly-(metronidazoles)n and doxorubicin (DOX)] in hydrophilic polymers (PEG2000); these NPs were functionalized to target gliomas cells and release its content only under hypoxic conditions, increasing radiosensitization as shown in vitro and in vivo after systematic NP administration (Hua et al., 2018; Table 3).
Nanoparticles as Nanocarriers
The restricted permeability of the BBB has been one of the biggest challenges in the mission of effectively treating brain tumors. In nanomedicine, not all nanoparticles can efficiently cross this biological barrier despite their size and physicochemical characteristics; consequently, previously discussed strategies, such as ligand targeting, or improvements on the enhanced permeability and retention (EPR) effect are required.
While ligand targeting is an active targeting method and required NPs to be designed with this purpose in mind, EPR effect refers to a passive targeting mechanism common to all NPs. EPR effect relies on pathophysiological characteristics of tumor vs. healthy vessels as well as NP size, which is larger than individual conventional chemotherapeutics (usually < 1,000 Da). Due to their relatively larger size, NPs are not able to penetrate normal blood vessels but can easily cross diseased vessels such as those presented in brain tumors, leading to a selected distribution into cancer tissues. NP with diameters of at least 5–10 nm present reduced kidney excretion (by exceeding the clearance renal threshold of 40,000 Da), prolonged blood half-life, and better accumulation in the tissue of interest. For instance, the plasma half-life of doxorubicin increases from 5–10 min to 2–3 days when this is encapsulated into liposomes. In order to achieve better results from the application of organic nanoparticles such as liposomes, micelles, etc., some polymers such as PEG can be used to decrease NP aggregation and opsonization by plasma proteins, thus adding to the improved blood half-life (Hua et al., 2018).
Unfortunately, EPR effect is highly heterogeneous at inter- and intraindividual level, changing over time in the same tumor and even being dissimilar among different brain tumor lesions for the same patient. This, altogether, has led to clinical outcomes that does not match with preclinical results. In order to overcome these drawbacks, additional strategies to enhance BBB disruption and facilitate NP penetration have been applied. These strategies include pharmacological and physical methods such as sonoporation and radiation. Radiation can increase vascular permeability due to increased secretion of vascular endothelial growth factor (VEGF) and fibroblast growth factor (FGF) (Lee et al., 1995; Park et al., 2001). Thus, Lammers et al. (2007) showed a positive effect in the accumulation of DOX-loaded polymeric NP sized between 5 and 10 nm (31 and 65 kDa, respectively) when tumors were primed with different doses of radiation.
Overall, all the previously described strategies should be carefully weighted when trying to optimize the use of nanoparticles as nanocarriers. In this setting, when applied to an orthotopic glioblastoma model, the use of functionalized biodegradable polymeric nanoparticles coated or loaded with anticancer drug has been able to confer longer survivals in preclinical models (Yu et al., 2019). Among all the different nanocarriers (Figure 1), liposomes have been largely used. Preclinical studies using liposomes loaded with doxorubicin or coated with temozolomide showed higher concentrations of these drugs inside the brain when compared with the plasmatic levels; in these same models, survival benefit was also described (Zhao et al., 2018; Li et al., 2019). Noteworthy, liposomal doxorubicin has been clinically used in primary and recurrent high-grade glioma patients, and good biodistribution and decent outcomes were obtained; however, none of the studies were randomized controlled trials (RCTs) and were published just before or after the publication of the Stupp protocol (Fabel et al., 2001; Hau et al., 2004).
Overall, these results point the use of nanocarriers as a promising enhancer of effective therapies for the treatment of patients with glioma (Table 3).
Nanomachines
Nanomachines or nanobots are molecular self-propelled nanodevices considered as smart delivery systems that respond to specific triggers (Khawaja, 2011; Jager and Giacomelli, 2015; Saxena et al., 2015; Fu et al., 2017). DNA nanorobots are nanometric devices controlled by an aptamer-encoded logic gate, able to sense specific stimulus such as intracellular pH or cell surface ligands in order to activate and reconfigure its structure for delivery of different payloads. Li et al. reported on a DNA nanorobot created through the DNA origami method; this was programmed to unfold itself upon binding to caveolin molecules expressed in cancerous blood vessel endothelial cells in order to deliver thrombin into tumor vessels. The authors were able to prove this concept in a murine model of breast cancer, successfully inducing intratumorally vascular thrombosis that resulted in tumor necrosis and growth tumor inhibition (Li et al., 2018). This technology is revolutionizing the traditional way of treating different tumors and is a promising strategy to improve prognosis on brain tumor patients. Other novel approach introduced as a promising tool in the armamentarium for the treatment of glioma tumors is the use of stem cells. Along the next section, we will describe how the above-described nanotechnology has been coupled to engineer improved stem cell therapies for the treatment of brain cancer (Table 3).
Applications of Nanoparticles in Stem Cell Glioma Therapy
Nanomedicine has extend the reach to several cancer treatment approaches such as radiotherapy, chemotherapy, immunotherapy, and others. In the case of stem cell therapies, improvements in several aspects are clearly needed. In an attempt to consolidate the translational potential of this approach, nanoparticles have been used to enhance safety and efficacy, stem cell tumor homing, and in vivo tracking after stem cell delivery. On the other hand, apart from nanoparticle surface modifications performed in an attempt to improve pharmacokinetics and pharmacodynamics parameters, stem cells appear as a reasonable option to overcome the suboptimal penetration, distribution, and retention associated to some nanomaterials when used as therapeutic nanocarriers. The use of stem cells in this context definitely add another option for a more targeted nanoparticle delivery. Thus, the benefit obtained from this combined approach using nanoparticles and stem cells is bidirectional.
Nanoparticles for Stem Cells Genetic Engineering
Stem cells are known by their ability to serve as vehicles of antitumor cargoes. For this purpose, viral gene vectors have been traditionally used to transduce stem cells with a high degree of gene delivery efficiency resulting in constant payload production (anticancer proteins, cytokines, antibodies, viral vectors, etc.). Although newer generations of viral vectors present better safety profiles, these vectors have been associated with immunotoxicity as a response to viral proteins production or potential viral replication. They also would carry the hypothetical risk of uncontrolled viral genome integration and insertional mutagenesis, latent virus activation, and inflammatory responses leading to demyelination or neurodegeneration (Dewey et al., 1999; Mangraviti et al., 2016). In this setting, nanoparticle-based gene delivery represents an attractive non-viral strategy to bioengineer stem cells. Different from commercially available reagents such as Lipofectamine 2000 (Thermo Fisher Scientific, Waltham, MA) nanoparticles may represent a less toxic and more effective approach for gene delivery.
Our group reported on the use of biodegradable polymeric nanoparticles based on poly(beta-amino ester)s (PBAEs) to enable effective BMP4 gene delivery on human A-MSC, allowing for higher transfection rates than those of commercially available reagents. Transfected MSC retained their multipotency and their tumor-homing capacity and were functional, leading to extended survival in a rat orthotopic GBM model (Yong et al., 2009). Huang et al. also reported on the use of nanoparticles for stem cell bioengineering; using hyaluronic acid (HA)-decorated superparamagnetic iron oxide nanoparticles as part of a magnetic ternary nanohybrid (MTN), the group was able to construct tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-secreting human mesenchymal stromal cell (hMSC). Decoration with CD44-binding HA and magnetic forces were used in this approach to increase cellular uptake of MTN. Impairment in tumor-homing properties were not observed (Huang R. Y. et al., 2019). Overall, nanoparticles raise as an option of safe and efficient gene delivery for stem cell; thus, helping stem cell therapy to achieve its maximal therapeutic potential.
Nanoparticles as Stem Cells Payloads
In the treatment of several malignancies, different nanoplatforms acting themselves as anticancer agents (Mooney et al., 2014a) or as carriers for these anticancer drugs (Mooney et al., 2014b) have been delivered locally and systemically. Recent advances in nanomedicine have allowed tuning nanoparticles properties in such a way that crossing the BBB and reaching brain tumors is now possible. However, there is a fine line between three factors: (1) the ideal size that a nanoparticle must have to easily cross the BBB (up to150 nm, optimal passage if < 15 nm) (Gao and Jiang, 2006), (2) being big enough to still be able to carry enough payload, and (3) being small enough to avoid engulfment by the mononuclear phagocyte system but still contain all the necessary ligands to assure specific cancer targeting (Owens and Peppas, 2006).
Furthermore, even if researchers could secure that nanoparticles reach the glioma tumor bulk, there exist other potential drawbacks that are imperative to highlight; they are related to the presence and location of glioma cancer stem cells (1) Nanoparticles are neither able to track infiltrative glioma cells leaving the tumor bulk to colonize distal healthy brain parenchyma nor (2) to reach the necrotic glioma core where blood flow is impaired. These areas do not present an EPR effect, which would facilitate nanoparticles to distribute across other areas of the tumor. Allowing nanoparticles to access the hypoxic central core would be crucial, as the treatment-resistant subpopulation of glioma cancer cells would predominantly locate in that area (Table 4). Even after active targeting strategies including ligand targeting and microenvironment-related targeting (delivering payload depending on pH, temperature, etc.) (Koo et al., 2006; Bernardi et al., 2008; Madhankumar et al., 2009; Hadjipanayis et al., 2010; Wang et al., 2011), nanoparticles alone are still insufficient and would be unlikely to overcome the above-mentioned roadblocks.
In this scenario, coupling stem cell therapy to nanotherapeutics offers the possibility to solve the previously stated dilemma regarding the inadequate distribution of therapeutic nanoparticles to the hypoxic glioma core and distant infiltrative tumor foci. Thus, stem cells could extend the reach for nanoparticles to penetrate these areas. This approach implies nanoparticles to be conjugated to stem cell surfaces or internalized before migrating toward malignant gliomas. Furthermore, the internalization of nanoparticles inside stem cells would allow them to be up to fivefold larger than the usual nanoparticles used in cancer therapy, without entailing problems in crossing the BBB or a higher risk to be engulfed by macrophages or lymphocytes (Koo et al., 2006; Bernardi et al., 2008; Madhankumar et al., 2009; Hadjipanayis et al., 2010; Wang et al., 2011). This increase in the nanoparticles’ longitudinal size translates into an approximately 125-fold increase in the nanoparticle load potential (by a volume-based, three-dimensional factor of 5) (Koo et al., 2006; Bernardi et al., 2008; Madhankumar et al., 2009; Hadjipanayis et al., 2010; Wang et al., 2011).
In this same line, the Aboody group demonstrated that neural stem cells were able to improve intracranial nanoparticle retention and tumor-selective distribution in an in vivo model by coupling huge nanoparticles to NSC surface (Mooney et al., 2014b). Taking advantage from the significant differences in the environmental pH between tumor and healthy tissues, the Aboody group loaded FDA-approved NSC cell with pH−sensitive doxorubicin−loaded mesoporous silica nanoparticles (MSN−Dox); the authors were able to tune nanoparticles properties to delay doxorubicin toxicity, allowing NSC to home into glioma tumors and deliver its payload only after arriving at the acidic tumor microenvironment. The approach led to a significant difference in survival when studied in a preclinical in vivo model (Cheng Y. et al., 2013). The same group also evaluated the role of NSC loaded with gold nanorods (AuNRs) to improve plasmonic photothermal therapy (aka thermal ablation), where the nanoparticles help to convert light into heat, aiming to eliminate cancerous tumor cells. The authors found that intratumor injections of AuNR-loaded NSC improved AuNRs distribution inside the tumor bulk when compared to locally injected free AuNRs in a brain metastasis heterotopic in vivo model (Mooney et al., 2014a).
The role of mesenchymal stem cells as nanoparticle carriers has also been investigated. Polymeric nanoparticles (paclitaxel-encapsulated PLGA nanoparticles) were loaded into BM-MSC. Osteogenesis, adipogenesis (chondrogenesis was not evaluated), and tumor homing were not affected by nanoparticle inclusion. The approach was associated with improved survival in a rat orthotopic glioma model when the modified MSCs were injected in the contralateral hemisphere (Wang et al., 2018). A similar approach to the one described by the Aboody group was performed on modified MSCs by loading them with gold nanoparticles (nanostarts) to improve phototherapy. Although studied in a heterotopic model of prostate cancer, the results support the use of MSC to maximize clinically relevant gold nanoparticles’ optical–electronic properties by increasing nanoparticle intratumor distribution (Huang L. et al., 2019).
Nanoparticles to Modulate Stem Cell Tumor Homing
Several tumor cytokines and stem cells surface proteins have been involved in enhancing MSC migration toward glioma tumors; however, no specific mechanism has been described yet. Tumor cytokines such as endothelial cell growth factor (EGF), platelet-derived growth factor (PDGF), VEGF, tumor growth factor β1 (TGF-β1), interleukin 8 (IL-8), monocyte chemoattractant protein-1 (MCP-1), and stromal cell-derived factor 1 alpha (SDF-1α) as well as stem cells surface proteins such as CD44, CXC chemokine receptor 4 (CXCR-4), integrin α4, and TGF-β receptors have been associated with increased MSC homing in gliomas (Young et al., 2014; Yamazoe et al., 2015).
The impact on stem cell behavior after being loaded with nanoparticles for different purposes has not been the principal focus of research. However, there already exist reports describing the increase in migration toward cancer cells after loading hMSC with iron oxide nanoparticles. This would be related to the overexpression of EGFR observed after nanoparticle inclusion and the characteristic elevated production of EGF by colon cancer cells used in the in vitro Boyden chamber experiments (Chung et al., 2011). Interestingly, the same trend has been observed when human BM-MSC were labeled with ferucarbotran nanoparticles and protamine. Using cellular magnetic resonance imagining (MRI) to track the labeled stem cells, increased BM-MSC migration toward in vitro and in vivo glioma models was found, and the SDF-1/CXCR4 signaling axis was associated to this phenomenon (Chien et al., 2011).
Nanoparticles for Tracking Stem Cells During Glioma Therapy
Stem-cell-based therapies rely on the ability of the grafted cells to target the organ of interest. In case of malignant gliomas, it is crucial to ensure stem cell tumor homing. In the preclinical setting, conventional methods for tracking migration and final fade of stem cells are traditionally based on bioluminescence imaging; however, poor spatial distribution and lack of translational applicability made necessary to establish a reasonably translational method that can be easily applied in a clinical setup.
Cellular MRI-based tracking technologies have risen as gold standard for non-invasive, real-time monitoring of transplanted stem cells (Kim et al., 2011). This approach would allow the study of stem cell biodistribution, migration, survival, and even differentiation with high spatial resolution and without the need for ionizing radiation. To make this possible, stem cells will require being labeled with magnetic nanoparticles. Although several options exit, magnetic iron oxide nanoparticles such superparamagnetic iron oxide nanoparticles (SPIONs) have been commonly used for this purpose (Cromer Berman et al., 2011).
The conjugation of stem cells and SPIONs has allowed for tracking MSC migration and homing into glioma tumors in a rodent glioma model without compromising such migratory capacity (Wu et al., 2008; Menon et al., 2012). NSCs have also been widely studied in this regard (Spina et al., 1975; Neri et al., 2008). After 1 month of follow-up, it was demonstrated that SPIONs would not impair multipotency, cell survival, or proliferation (Agha-Hosseini et al., 2010). Furthermore, a NSC migration speed of 50–70 μm/day has been calculated after the cells were loaded with ferumoxide (SPION + dextran) (Flexman et al., 2011). Clinically relevant results were those presented by Thu et al. The group showed that loading FDA-approved NSC with ferumoxide–protamine complex nanoparticles did not impaired humor-homing properties in a murine glioma model (Thu et al., 2009; Auffinger et al., 2013). Gutova et al. also reported on similar findings when using ultrasmall superparamagnetic iron oxide nanoparticles (USPIONs) in clinically graded nanoparticles and FDA-approved NSC (Gutova et al., 2013). Currently, different complementary imaging modalities and nanoparticles stem-cell coupling techniques are being studied (Egawa et al., 2015; Cheng S. H. et al., 2016; Qiao et al., 2018).
Even when this approach was first evaluated in the clinical setting around 2006 (Zhu et al., 2006) and has been used in different pathologies and other cancers (de Vries et al., 2005), glioma patients have not yet harnessed the benefit of the clinical applicability of this technology. This could be related to the difficulties in obtaining long-term follow-up of nanoparticle-labeled stem cells, as their self-renewal capacity render less nanoparticle concentration through each replicative cell cycle.
Challenge, Potential Pitfalls, and Future Perspective
Challenge and pitfalls associated with this relatively novel approach is proper of any disruptive technology. The ethical concerns associated with the use of particular stem cells, while seemingly addressed with modern techniques, need to be further discussed before extensive use can be assumed (Ramos-Zúñiga et al., 2012). Clinical endeavors utilizing stem cells as potential therapeutic tools in glioma patients have already glimpsed relative success. In this setting, careful and individualized selection of specific types of stem cell will be key in in future clinical applications for these patients. For instance, we concentrate our efforts in the application of adipose-derived MSCs, which can be easily obtained from the same patient. Although still in preclinical phase, we expect them to be rapidly bioengineered and used for autologous transplantation, thus allowing for an individualized and expedited process so the patients can therapeutically receive them even at time of surgery.
The introduction of the nanotechnology in stem cell therapies has shown to be beneficial and hopefully will keep turning stem cell therapies into a less worrisome and more controlled therapeutic strategy. To date, we have explored NP for stem cell bioengineering and cell tracking; however, we believe that their malleability allows for further uses such as the ones previously described, alone or in combination, and even for stem cell functionalization (Kim et al., 2011; Bishop et al., 2016; Mangraviti et al., 2016; Wilson et al., 2017a, b; Tian et al., 2020).
Finally, the combination of these therapies should not be limited to only nanoparticles and stem cells; this combined approach will need to explore if further value can be obtained by coupling with additional fields such as radiotherapy, thermotherapy, targeted systemic therapies, focused ultrasound, and other novel diagnostic techniques such as ultrahigh magnetic strength imaging and novel radiotracers in order to maximize its benefits.
Author Contributions
HR-G and KA-E screened titles for relevance and abstracted the data from the eligible full text articles. SK, AQ-H, and DT critically revised the manuscript with input from the entire team. HR-G and KA-E created the figures and tables. HR-G, KA-E, and DT worked on study conception and design. All authors analyzed and interpreted the data, drafted the manuscript, and read and approved the final draft.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This publication was made possible through the support of the Eveleigh Family Career Development Award for Cancer Research at Mayo Clinic in Florida. AQ-H was supported by the Mayo Clinic Professorship, the Mayo Clinic Clinician Investigator award, the Florida Department of Health Cancer Research Chair Fund, and the NIH (R43CA221490, R01CA200399, R01CA195503, and R01CA216855).
References
- Aboody K. S., Brown A., Rainov N. G., Bower K. A., Liu S., Yang W., et al. (2000). Neural stem cells display extensive tropism for pathology in adult brain: evidence from intracranial gliomas. Proc. Natl. Acad. Sci. U.S.A. 97 12846–12851. 10.1073/pnas.97.23.12846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Affram K., Udofot O., Singh M., Krishnan S., Reams R., Rosenberg J., et al. (2017). Smart thermosensitive liposomes for effective solid tumor therapy and in vivo imaging. PLoS One 12:e0185116. 10.1371/journal.pone.0185116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agha-Hosseini F., Jahani M. A., Jahani M., Mirzaii-Dizgah I., Ali-Moghaddam K. (2010). In vitro isolation of stem cells derived from human dental pulp. Clin. Transplant. 24 E23–E28. [DOI] [PubMed] [Google Scholar]
- Agrawal G., Agrawal R. (2019). Janus nanoparticles: recent advances in their interfacial and biomedical applications. ACS Appl. Nano Mater. 2 1738–1757. 10.1021/acsanm.9b00283 [DOI] [Google Scholar]
- Agrawal U., Chashoo G., Sharma P. R., Kumar A., Saxena A. K., Vyas S. P. (2015). Tailored polymer-lipid hybrid nanoparticles for the delivery of drug conjugate: dual strategy for brain targeting. Colloids Surf. B Biointerfaces 126 414–425. 10.1016/j.colsurfb.2014.12.045 [DOI] [PubMed] [Google Scholar]
- Alex A. T., Joseph A., Shavi G., Rao J. V., Udupa N. (2016). Development and evaluation of carboplatin-loaded PCL nanoparticles for intranasal delivery. Drug Deliv. 23 2144–2153. 10.3109/10717544.2014.948643 [DOI] [PubMed] [Google Scholar]
- Allahverdi A., Arefian E., Soleimani M., Ai J., Nahanmoghaddam N., Yousefi-Ahmadipour A., et al. (2020). MicroRNA-4731-5p delivered by AD-mesenchymal stem cells induces cell cycle arrest and apoptosis in glioblastoma. J. Cell. Physiol. 235 8167–8175. 10.1002/jcp.29472 [DOI] [PubMed] [Google Scholar]
- Altanerova V., Cihova M., Babic M., Rychly B., Ondicova K., Mravec B., et al. (2012). Human adipose tissue-derived mesenchymal stem cells expressing yeast cytosinedeaminase::uracil phosphoribosyltransferase inhibit intracerebral rat glioblastoma. Int. J. Cancer 130 2455–2463. 10.1002/ijc.26278 [DOI] [PubMed] [Google Scholar]
- Alves S. R., Colquhoun A., Wu X. Y., de Oliveira Silva D. (2020). Synthesis of terpolymer-lipid encapsulated diruthenium(II,III)-anti-inflammatory metallodrug nanoparticles to enhance activity against glioblastoma cancer cells. J. Inorg. Biochem. 205:110984. 10.1016/j.jinorgbio.2019.110984 [DOI] [PubMed] [Google Scholar]
- Amano S., Gu C., Koizumi S., Tokuyama T., Namba H. (2011). Timing of ganciclovir administration in glioma gene therapy using HSVtk gene-transduced mesenchymal stem cells. Cancer Genom. Proteomics 8 245–250. [PubMed] [Google Scholar]
- Ambruosi A., Gelperina S., Khalansky A., Tanski S., Theisen A., Kreuter J. (2006). Influence of surfactants, polymer and doxorubicin loading on the anti-tumour effect of poly(butyl cyanoacrylate) nanoparticles in a rat glioma model. J. Microencapsul. 23 582–592. 10.1080/02652040600788080 [DOI] [PubMed] [Google Scholar]
- An S., He D., Wagner E., Jiang C. (2015). Peptide-like polymers exerting effective glioma-targeted siRNA delivery and release for therapeutic application. Small 11 5142–5150. 10.1002/smll.201501167 [DOI] [PubMed] [Google Scholar]
- Andres M., Bratt-Leal A. Z., Wang Y., Loring J. F. (2019). “Induced pluripotent stem cels,” in Principles of Regenerative Medicine. 3rd Edition ed, ed. Atala A. (Amsterdam: ElSevier; ). [Google Scholar]
- Auffinger B., Morshed R., Tobias A., Cheng Y., Ahmed A. U., Lesniak M. S. (2013). Drug-loaded nanoparticle systems and adult stem cells: a potential marriage for the treatment of malignant glioma? Oncotarget 4 378–396. 10.18632/oncotarget.937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balyasnikova I. V., Ferguson S. D., Han Y., Liu F., Lesniak M. S. (2011). Therapeutic effect of neural stem cells expressing TRAIL and bortezomib in mice with glioma xenografts. Cancer Lett. 310, 148–159. 10.1016/j.canlet.2011.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balyasnikova I. V., Prasol M. S., Ferguson S. D., Han Y., Ahmed A. U., Gutova M., et al. (2014). Intranasal delivery of mesenchymal stem cells significantly extends survival of irradiated mice with experimental brain tumors. Mol. Ther. 22 140–148. 10.1038/mt.2013.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnan J., Isakson P., Joel M., Cilio C., Langmoen I. A., Vik-Mo E. O., et al. (2014). Recruited brain tumor-derived mesenchymal stem cells contribute to brain tumor progression. Stem Cells 32 1110–1123. 10.1002/stem.1614 [DOI] [PubMed] [Google Scholar]
- Beier D., Hau P., Proescholdt M., Lohmeier A., Wischhusen J., Oefner P. J., et al. (2007). CD133(+) and CD133(-) glioblastoma-derived cancer stem cells show differential growth characteristics and molecular profiles. Cancer Res. 67 4010–4015. 10.1158/0008-5472.can-06-4180 [DOI] [PubMed] [Google Scholar]
- Benedetti S., Pirola B., Pollo B., Magrassi L., Bruzzone M. G., Rigamonti D., et al. (2000). Gene therapy of experimental brain tumors using neural progenitor cells. Nat Med. 6, 447–450. 10.1038/74710 [DOI] [PubMed] [Google Scholar]
- Bernardi R. J., Lowery A. R., Thompson P. A., Blaney S. M., West J. L. (2008). Immunonanoshells for targeted photothermal ablation in medulloblastoma and glioma: an in vitro evaluation using human cell lines. J. Neuro Oncol. 86 165–172. 10.1007/s11060-007-9467-3 [DOI] [PubMed] [Google Scholar]
- Bishop C. J., Majewski R. L., Guiriba T. R., Wilson D. R., Bhise N. S., Quiñones-Hinojosa A., et al. (2016). Quantification of cellular and nuclear uptake rates of polymeric gene delivery nanoparticles and DNA plasmids via flow cytometry. Acta Biomater. 37 120–130. 10.1016/j.actbio.2016.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobo D., Robinson K. J., Islam J., Thurecht K. J., Corrie S. R. (2016). Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharm. Res. 33 2373–2387. 10.1007/s11095-016-1958-5 [DOI] [PubMed] [Google Scholar]
- Brandes A. A., Tosoni A., Franceschi E., Sotti G., Frezza G., Amistà P., et al. (2009). Recurrence pattern after temozolomide concomitant with and adjuvant to radiotherapy in newly diagnosed patients with glioblastoma: correlation With MGMT promoter methylation status. J. Clin. Oncol. 27 1275–1279. 10.1200/jco.2008.19.4969 [DOI] [PubMed] [Google Scholar]
- Breznik B., Motaln H., Vittori M., Rotter A., Lah Turnsek T. (2017). Mesenchymal stem cells differentially affect the invasion of distinct glioblastoma cell lines. Oncotarget 8 25482–25499. 10.18632/oncotarget.16041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A. B., Yang W., Schmidt N. O., Carroll R., Leishear K. K., Rainov N. G., et al. (2003). Intravascular delivery of neural stem cell lines to target intracranial and extracranial tumors of neural and non-neural origin. Hum. Gene Ther. 14 1777–1785. 10.1089/104303403322611782 [DOI] [PubMed] [Google Scholar]
- Bryukhovetskiy I. S., Mischenko P. V., Tolok E. V., Zaitcev S. V., Khotimchenko Y. S., Bryukhovetskiy A. S. (2015). Directional migration of adult hematopoeitic progenitors to C6 glioma in vitro. Oncol. Lett. 9 1839–1844. 10.3892/ol.2015.2952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caban-Toktas S., Sahin A., Lule S., Esendagli G., Vural I., Karli Oguz K., et al. (2020). Combination of Paclitaxel and R-flurbiprofen loaded PLGA nanoparticles suppresses glioblastoma growth on systemic administration. Int. J. Pharm. 578:119076. 10.1016/j.ijpharm.2020.119076 [DOI] [PubMed] [Google Scholar]
- Caccese M., Padovan M., D’Avella D., Chioffi F., Gardiman M. P., Berti F., et al. (2020). Anaplastic Astrocytoma: State of the art and future directions. Crit. Rev. Oncol. Hematol. 153:103062 10.1016/j.critrevonc.2020.103062 [DOI] [PubMed] [Google Scholar]
- Cantrell J. N., Waddle M. R., Rotman M., Peterson J. L., Ruiz-Garcia H., Heckman M. G., et al. (2019). Progress toward long-term survivors of glioblastoma. Mayo Clin. Proc. 94 1278–1286. 10.1016/j.mayocp.2018.11.031 [DOI] [PubMed] [Google Scholar]
- Cha C. Y., Shin S. R., Annabi N., Dokmeci M. R., Khademhosseini A. (2013). Carbon-based nanomaterials: multifunctional materials for biomedical engineering. ACS Nano 7 2891–2897. 10.1021/nn401196a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaichana K. L., Cabrera-Aldana E. E., Jusue-Torres I., Wijesekera O., Olivi A., Rahman M., et al. (2014a). When gross total resection of a glioblastoma is possible, how much resection should be achieved? World Neurosurg. 82 e257–e265. [DOI] [PubMed] [Google Scholar]
- Chaichana K. L., Jusue-Torres I., Lemos A. M., Gokaslan A., Cabrera-Aldana E. E., Ashary A., et al. (2014b). The butterfly effect on glioblastoma: is volumetric extent of resection more effective than biopsy for these tumors? J. Neuro Oncol. 120 625–634. 10.1007/s11060-014-1597-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaichana K. L., Jusue-Torres I., Navarro-Ramirez R., Raza S. M., Pascual-Gallego M., Ibrahim A., et al. (2014c). Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol. 16 113–122. 10.1093/neuonc/not137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain M. C. (2011). Radiographic patterns of relapse in glioblastoma. J. Neuro Oncol. 101 319–323. 10.1007/s11060-010-0251-4 [DOI] [PubMed] [Google Scholar]
- Chen Y., Bian X., Aliru M., Deorukhkar A. A., Ekpenyong O., Liang S., et al. (2018). Hypoxia-targeted gold nanorods for cancer photothermal therapy. Oncotarget 9 26556–26571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. T., Wei J. D., Wang J. P., Lee H. H., Chiang E. R., Lai H. C., et al. (2011). Isolation of mesenchymal stem cells from human ligamentum flavum: implicating etiology of ligamentum flavum hypertrophy. Spine 36 E1193–E1200. [DOI] [PubMed] [Google Scholar]
- Cheng L., Huang Z., Zhou W., Wu Q., Donnola S., Liu J. K., et al. (2013). Glioblastoma stem cells generate vascular pericytes to support vessel function and tumor growth. Cell 153 139–152. 10.1016/j.cell.2013.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng S. H., Yu D., Tsai H. M., Morshed R. A., Kanojia D., Lo L. W., et al. (2016). Dynamic in vivo SPECT imaging of neural stem cells functionalized with radiolabeled nanoparticles for tracking of glioblastoma. J. Nuclear Med. 57 279–284. 10.2967/jnumed.115.163006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Morshed R., Cheng S. H., Tobias A., Auffinger B., Wainwright D. A., et al. (2013). Nanoparticle-programmed self-destructive neural stem cells for glioblastoma targeting and therapy. Small 9 4123–4129. 10.1002/smll.201301111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Muroski M. E., Petit D., Mansell R., Vemulkar T., Morshed R. A., et al. (2016). Rotating magnetic field induced oscillation of magnetic particles for in vivo mechanical destruction of malignant glioma. J. Control Release 223 75–84. 10.1016/j.jconrel.2015.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien L. Y., Hsiao J. K., Hsu S. C., Yao M., Lu C. W., Liu H. M., et al. (2011). In vivo magnetic resonance imaging of cell tropism, trafficking mechanism, and therapeutic impact of human mesenchymal stem cells in a murine glioma model. Biomaterials 32 3275–3284. 10.1016/j.biomaterials.2011.01.042 [DOI] [PubMed] [Google Scholar]
- Choi S. A., Hwang S. K., Wang K. C., Cho B. K., Phi J. H., Lee J. Y., et al. (2011). Therapeutic efficacy and safety of TRAIL-producing human adipose tissue-derived mesenchymal stem cells against experimental brainstem glioma. Neuro Oncol. 13 61–69. 10.1093/neuonc/noq147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung K., Ullah I., Kim N., Lim J., Shin J., Lee S. C., et al. (2020). Intranasal delivery of cancer-targeting doxorubicin-loaded PLGA nanoparticles arrests glioblastoma growth. J. Drug Target. 28 617–626. 10.1080/1061186x.2019.1706095 [DOI] [PubMed] [Google Scholar]
- Chung T. H., Hsiao J. K., Hsu S. C., Yao M., Chen Y. C., Wang S. W., et al. (2011). Iron oxide nanoparticle-induced epidermal growth factor receptor expression in human stem cells for tumor therapy. ACS Nano 5 9807–9816. 10.1021/nn2033902 [DOI] [PubMed] [Google Scholar]
- Cook R. L., Householder K. T., Chung E. P., Prakapenka A. V., DiPerna D. M., Sirianni R. W. (2015). A critical evaluation of drug delivery from ligand modified nanoparticles: confounding small molecule distribution and efficacy in the central nervous system. J. Control. Release 220(Pt A), 89–97. 10.1016/j.jconrel.2015.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cromer Berman S. M., Walczak P., Bulte J. W. (2011). Tracking stem cells using magnetic nanoparticles. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 3 343–355. 10.1002/wnan.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahan P., Gala J. M., Delmas C., Monferran S., Malric L., Zentkowski D., et al. (2014). Ionizing radiations sustain glioblastoma cell dedifferentiation to a stem-like phenotype through survivin: possible involvement in radioresistance. Cell Death Dis. 5:e1543. 10.1038/cddis.2014.509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel J., Montaleytang M., Nagarajan S., Picard S., Clermont G., Lazar A. N., et al. (2019). Hydrophilic fluorescent nanoprodrug of paclitaxel for glioblastoma chemotherapy. ACS Omega 4 18342–18354. 10.1021/acsomega.9b02588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Melo S. M., Bittencourt S., Ferrazoli E. G., da Silva C. S., da Cunha F. F., da Silva F. H., et al. (2015). The anti-tumor effects of adipose tissue mesenchymal stem cell transduced with HSV-Tk Gene on U-87-driven brain tumor. PLoS One 10:e0128922. 10.1371/journal.pone.0128922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries I. J., Lesterhuis W. J., Barentsz J. O., Verdijk P., van Krieken J. H., Boerman O. C., et al. (2005). Magnetic resonance tracking of dendritic cells in melanoma patients for monitoring of cellular therapy. Nat. Biotechnol. 23 1407–1413. 10.1038/nbt1154 [DOI] [PubMed] [Google Scholar]
- Denora N., Lee C., Iacobazzi R. M., Choi J. Y., Song I. H., Yoo J. S., et al. (2019). TSPO-targeted NIR-fluorescent ultra-small iron oxide nanoparticles for glioblastoma imaging. Eur. J. Pharm. Sci. 139:105047. 10.1016/j.ejps.2019.105047 [DOI] [PubMed] [Google Scholar]
- Dewey R. A., Morrissey G., Cowsill C. M., Stone D., Bolognani F., Dodd N. J., et al. (1999). Chronic brain inflammation and persistent herpes simplex virus 1 thymidine kinase expression in survivors of syngeneic glioma treated by adenovirus-mediated gene therapy: implications for clinical trials. Nat. Med. 5 1256–1263. 10.1038/15207 [DOI] [PubMed] [Google Scholar]
- Dominici M., Le Blanc K., Mueller I., Slaper-Cortenbach I., Marini F., Krause D., et al. (2006). Minimal criteria for defining multipotent mesenchymal stromal cells. the international society for cellular therapy position statement. Cytotherapy 8 315–317. 10.1080/14653240600855905 [DOI] [PubMed] [Google Scholar]
- Drumm M. R., Dixit K. S., Grimm S., Kumthekar P., Lukas R. V., Raizer J. J., et al. (2019). Extensive brainstem infiltration, not mass effect, is a common feature of end-stage cerebral glioblastomas. Neuro Oncol. 22 470–479. 10.1093/neuonc/noz216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufort S., Appelboom G., Verry C., Barbier E. L., Lux F., Brauer-Krisch E., et al. (2019). Ultrasmall theranostic gadolinium-based nanoparticles improve high-grade rat glioma survival. J. Clin. Neurosci. 67 215–219. 10.1016/j.jocn.2019.05.065 [DOI] [PubMed] [Google Scholar]
- Egawa E. Y., Kitamura N., Nakai R., Arima Y., Iwata H. (2015). A DNA hybridization system for labeling of neural stem cells with SPIO nanoparticles for MRI monitoring post-transplantation. Biomaterials 54 158–167. 10.1016/j.biomaterials.2015.03.017 [DOI] [PubMed] [Google Scholar]
- Ehtesham M., Kabos P., Kabosova A., Neuman T., Black K. L., Yu J. S. (2001). The use of interleukin 12-secreting neural stem cells for the treatment of intracranial glioma. Cancer Res. 62, 5657–5663. [PubMed] [Google Scholar]
- Erices A., Conget P., Minguell J. J. (2000). Mesenchymal progenitor cells in human umbilical cord blood. Br. J. Haematol. 109 235–242. 10.1046/j.1365-2141.2000.01986.x [DOI] [PubMed] [Google Scholar]
- Euliss L. E., DuPont J. A., Gratton S., DeSimone J. (2006). Imparting size, shape, and composition control of materials for nanomedicine. Chem. Soc. Rev. 35 1095–1104. 10.1039/b600913c [DOI] [PubMed] [Google Scholar]
- European Commission (2011). Commission Recommendation of 18 October 2011 on the definition of nanomaterial 2011/696/EU. Off. J. Eur. Union 275 38–40. [Google Scholar]
- Evans R. C., Ellingworth A., Cashen C. J., Weinberger C. R., Sambur J. B. (2019). Influence of single-nanoparticle electrochromic dynamics on the durability and speed of smart windows. Proc. Natl. Acad. Sci. U.S.A. 116 12666–12671. 10.1073/pnas.1822007116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabel K., Dietrich J., Hau P., Wismeth C., Winner B., Przywara S., et al. (2001). Long-term stabilization in patients with malignant glioma after treatment with liposomal doxorubicin. Cancer 92 1936–1942. [DOI] [PubMed] [Google Scholar]
- Farjadian F., Ghasemi A., Gohari O., Roointan A., Karimi M., Hamblin M. R. (2019). Nanopharmaceuticals and nanomedicines currently on the market: challenges and opportunities. Nanomedicine 14 93–126. 10.2217/nnm-2018-0120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira N. N., Granja S., Boni F. I., Ferreira L. M. B., Reis R. M., Baltazar F., et al. (2020). A novel strategy for glioblastoma treatment combining alpha-cyano-4-hydroxycinnamic acid with cetuximab using nanotechnology-based delivery systems. Drug Deliv. Transl. Res. 10 594–609. doi: 10.1007/s13346-020-00713-8 [DOI] [PubMed] [Google Scholar]
- Flexman J. A., Cross D. J., Tran L. N., Sasaki T., Kim Y., Minoshima S. (2011). Quantitative analysis of neural stem cell migration and tracer clearance in the rat brain by MRI. Mol. Imaging Biol. 13 104–111. 10.1007/s11307-010-0311-3 [DOI] [PubMed] [Google Scholar]
- Friedenstein A. J., Chailakhjan R. K., Lalykina K. S. (1970). The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 3 393–403. 10.1111/j.1365-2184.1970.tb00347.x [DOI] [PubMed] [Google Scholar]
- Friedenstein A. J., Chailakhyan R. K., Latsinik N. V., Panasyuk A. F., Keiliss-Borok I. V. (1974). Stromal cells responsible for transferring the microenvironment of the hemopoietic tissues. Cloning in vitro and retransplantation in vivo. Transplantation 17 331–340. 10.1097/00007890-197404000-00001 [DOI] [PubMed] [Google Scholar]
- Friedenstein A. J., Petrakova K. V., Kurolesova A. I., Frolova G. P. (1968). Heterotopic of bone marrow. Analysis of precursor cells for osteogenic and hematopoietic tissues. Transplantation 6 230–247. [PubMed] [Google Scholar]
- Fu J. L., Stankeviciute G., Oh S. W., Collins J., Zhong Y. H., Zhang T. (2017). Self-assembled nucleic acid nanostructures for cancer theranostic medicines. Curr. Top. Med. Chem. 17 1815–1828. 10.2174/1568026617666161122115722 [DOI] [PubMed] [Google Scholar]
- Galli R., Binda E., Orfanelli U., Cipelletti B., Gritti A., De Vitis S., et al. (2004). Isolation and characterization of tumorigenic, stem-like neural precursors from human glioblastoma. Cancer Res. 64 7011–7021. 10.1158/0008-5472.can-04-1364 [DOI] [PubMed] [Google Scholar]
- Gao K., Jiang X. (2006). Influence of particle size on transport of methotrexate across blood brain barrier by polysorbate 80-coated polybutylcyanoacrylate nanoparticles. Int. J. Pharm. 310 213–219. 10.1016/j.ijpharm.2005.11.040 [DOI] [PubMed] [Google Scholar]
- Gao S., Tian H., Xing Z., Zhang D., Guo Y., Guo Z., et al. (2016). A non-viral suicide gene delivery system traversing the blood brain barrier for non-invasive glioma targeting treatment. J. Control. Release 243 357–369. 10.1016/j.jconrel.2016.10.027 [DOI] [PubMed] [Google Scholar]
- Girdlestone J., Limbani V. A., Cutler A. J., Navarrete C. V. (2009). Efficient expansion of mesenchymal stromal cells from umbilical cord under low serum conditions. Cytotherapy 11 738–748. 10.3109/14653240903079401 [DOI] [PubMed] [Google Scholar]
- Golombek S. K., May J. N., Theek B., Appold L., Drude N., Kiessling F., et al. (2018). Tumor targeting via EPR: strategies to enhance patient responses. Adv. Drug Deliv. Rev. 130 17–38. 10.1016/j.addr.2018.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Pech N. I., Stebounova L. V., Ustunol I. B., Park J. H., Renee Anthony T., Peters T. M., et al. (2019). Size, composition, morphology, and health implications of airborne incidental metal-containing nanoparticles. J. Occup. Environ. Hygiene 16 387–399. 10.1080/15459624.2018.1559925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K. T., Fu P., Juerchott K., Motaln H., Selbig J., Lah T., et al. (2014). The expression of Wnt-inhibitor DKK1 (Dickkopf 1) is determined by intercellular crosstalk and hypoxia in human malignant gliomas. J. Cancer Res. Clin. Oncol. 140 1261–1270. 10.1007/s00432-014-1642-2 [DOI] [PubMed] [Google Scholar]
- Guo W., Li A., Jia Z., Yuan Y., Dai H., Li H. (2013). Transferrin modified PEG-PLA-resveratrol conjugates: in vitro and in vivo studies for glioma. Eur. J. Pharmacol. 718 41–47. 10.1016/j.ejphar.2013.09.034 [DOI] [PubMed] [Google Scholar]
- Gutova M., Frank J. A., D’Apuzzo M., Khankaldyyan V., Gilchrist M. M., Annala A. J., et al. (2013). Magnetic resonance imaging tracking of ferumoxytol-labeled human neural stem cells: studies leading to clinical use. Stem Cells Transl. Med. 2 766–775. 10.5966/sctm.2013-0049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjipanayis C. G., Machaidze R., Kaluzova M., Wang L., Schuette A. J., Chen H., et al. (2010). EGFRvIII antibody-conjugated iron oxide nanoparticles for magnetic resonance imaging-guided convection-enhanced delivery and targeted therapy of glioblastoma. Cancer Res. 70 6303–6312. 10.1158/0008-5472.can-10-1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hau P., Fabel K., Baumgart U., Rummele P., Grauer O., Bock A., et al. (2004). Pegylated liposomal doxorubicin-efficacy in patients with recurrent high-grade glioma. Cancer 100 1199–1207. 10.1002/cncr.20073 [DOI] [PubMed] [Google Scholar]
- Hsu F. T., Wei Z. H., Hsuan Y. C., Lin W., Su Y. C., Liao C. H., et al. (2018). MRI tracking of polyethylene glycol-coated superparamagnetic iron oxide-labelled placenta-derived mesenchymal stem cells toward glioblastoma stem-like cells in a mouse model. Artif. Cells Nanomed. Biotechnol. 46 S448–S459. [DOI] [PubMed] [Google Scholar]
- Hua L., Wang Z., Zhao L., Mao H. L., Wang G. H., Zhang K. R., et al. (2018). Hypoxia-responsive lipid-poly-(hypoxic radiosensitized polyprodrug) nanoparticles for glioma chemo- and radiotherapy. Theranostics 8 5088–5105. 10.7150/thno.26225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua M. Y., Liu H. L., Yang H. W., Chen P. Y., Tsai R. Y., Huang C. Y., et al. (2011). The effectiveness of a magnetic nanoparticle-based delivery system for BCNU in the treatment of gliomas. Biomaterials 32 516–527. 10.1016/j.biomaterials.2010.09.065 [DOI] [PubMed] [Google Scholar]
- Huang L., Xu C., Xu P., Qin Y., Chen M., Feng Q., et al. (2019). Intelligent photosensitive mesenchymal stem cells and cell-derived microvesicles for photothermal therapy of prostate cancer. Nanotheranostics 3 41–53. 10.7150/ntno.28450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R. Y., Lin Y. H., Lin S. Y., Li Y. N., Chiang C. S., Chang C. W. (2019). Magnetic ternary nanohybrids for nonviral gene delivery of stem cells and applications on cancer therapy. Theranostics 9 2411–2423. 10.7150/thno.29326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., Zhang F., Wang H., Niu G., Choi K. Y., Swierczewska M., et al. (2013). Mesenchymal stem cell-based cell engineering with multifunctional mesoporous silica nanoparticles for tumor delivery. Biomaterials 34 1772–1780. 10.1016/j.biomaterials.2012.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., Zhang F., Wang Y., Sun X., Choi K. Y., Liu D., et al. (2014). Design considerations of iron-based nanoclusters for noninvasive tracking of mesenchymal stem cell homing. ACS Nano 8 4403–4414. 10.1021/nn4062726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussein Kamareddine M., Ghosn Y., Tawk A., Elia C., Alam W., Makdessi J., et al. (2019). Organic nanoparticles as drug delivery systems and their potential role in the treatment of chronic myeloid leukemia. Technol. Cancer Res. Treat. 18 1533033819879902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iser I. C., Ceschini S. M., Onzi G. R., Bertoni A. P., Lenz G., Wink M. R. (2016). Conditioned medium from adipose-derived stem cells (ADSCs) promotes epithelial-to-mesenchymal-like transition (EMT-like) in glioma cells in vitro. Mol. Neurobiol. 53 7184–7199. 10.1007/s12035-015-9585-4 [DOI] [PubMed] [Google Scholar]
- Jabbarpour Z., Kiani J., Keshtkar S., Saidijam M., Ghahremani M. H., Ahmadbeigi N. (2020). Effects of human placenta-derived mesenchymal stem cells with NK4 gene expression on glioblastoma multiforme cell lines. J. Cell. Biochem. 121 1362–1373. 10.1002/jcb.29371 [DOI] [PubMed] [Google Scholar]
- Jagannathan R., Irvin G., Blanton T., Jagannathan S. (2006). Organic nanoparticles: preparation, self-assembly, and properties. Adv. Funct. Mater. 16 747–753. 10.1002/adfm.200600003 [DOI] [Google Scholar]
- Jager E., Giacomelli F. C. (2015). Soft matter assemblies as nanomedicine platforms for cancer chemotherapy: a journey from market products towards novel approaches. Curr. Top. Med. Chem. 15 328–344. 10.2174/1568026615666150130152300 [DOI] [PubMed] [Google Scholar]
- Jiang X., Xin H., Sha X., Gu J., Jiang Y., Law K., et al. (2011). PEGylated poly(trimethylene carbonate) nanoparticles loaded with paclitaxel for the treatment of advanced glioma: in vitro and in vivo evaluation. Int. J. Pharm. 420 385–394. 10.1016/j.ijpharm.2011.08.052 [DOI] [PubMed] [Google Scholar]
- Jiao H., Guan F., Yang B., Li J., Song L., Hu X., et al. (2012). Human amniotic membrane derived-mesenchymal stem cells induce C6 glioma apoptosis in vivo through the Bcl-2/caspase pathways. Mol. Biol. Rep. 39 467–473. 10.1007/s11033-011-0760-z [DOI] [PubMed] [Google Scholar]
- Karlsson J., Rui Y., Kozielski K. L., Placone A. L., Choi O., Tzeng S. Y., et al. (2019). Engineered nanoparticles for systemic siRNA delivery to malignant brain tumours. Nanoscale 11 20045–20057. 10.1039/c9nr04795f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassis I., Zangi L., Rivkin R., Levdansky L., Samuel S., Marx G., et al. (2006). Isolation of mesenchymal stem cells from G-CSF-mobilized human peripheral blood using fibrin microbeads. Bone Marrow Transplant. 37 967–976. 10.1038/sj.bmt.1705358 [DOI] [PubMed] [Google Scholar]
- Katz A. J., Tholpady A., Tholpady S. S., Shang H., Ogle R. C. (2005). Cell surface and transcriptional characterization of human adipose-derived adherent stromal (hADAS) cells. Stem Cells 23 412–423. 10.1634/stemcells.2004-0021 [DOI] [PubMed] [Google Scholar]
- Kaur P., Aliru M. L., Chadha A. S., Asea A., Krishnan S. (2016). Hyperthermia using nanoparticles–Promises and pitfalls. Int. J. Hyperther. 32 76–88. 10.3109/02656736.2015.1120889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazmi F., Vallis K. A., Vellayappan B. A., Bandla A., Yukun D., Carlisle R. (2020). Megavoltage radiosensitization of gold nanoparticles on a glioblastoma cancer cell line using a clinical platform. Int. J. Mol. Sci. 21:429. 10.3390/ijms21020429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kefayat A., Ghahremani F., Motaghi H., Amouheidari A. (2019). Ultra-small but ultra-effective: folic acid-targeted gold nanoclusters for enhancement of intracranial glioma tumors’ radiation therapy efficacy. Nanomed Nanotechnol. 16 173–184. 10.1016/j.nano.2018.12.007 [DOI] [PubMed] [Google Scholar]
- Khawaja A. M. (2011). The legacy of nanotechnology: revolution and prospects in neurosurgery. Int. J. Surg. 9 608–614. 10.1016/j.ijsu.2011.10.002 [DOI] [PubMed] [Google Scholar]
- Kim D. H., Rozhkova E. A., Ulasov I. V., Bader S. D., Rajh T., Lesniak M. S., et al. (2010). Biofunctionalized magnetic-vortex microdiscs for targeted cancer-cell destruction. Nat. Mater. 9 165–171. 10.1038/nmat2591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim R., Lee S., Lee J., Kim M., Kim W. J., Lee H. W., et al. (2018). Exosomes derived from microRNA-584 transfected mesenchymal stem cells: novel alternative therapeutic vehicles for cancer therapy. BMB Rep. 51 406–411. 10.5483/bmbrep.2018.51.8.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. J., Lewis B., Steiner M. S., Bissa U. V., Dose C., Frank J. A. (2016). Superparamagnetic iron oxide nanoparticles for direct labeling of stem cells and in vivo MRI tracking. Contrast Med. Mol. Imaging 11 55–64. 10.1002/cmmi.1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. K., Cargioli T. G., Machluf M., Yang W., Sun Y., Al-Hashem R., et al. (2005). PEX-producing human neural stem cells inhibit tumor growth in a mouse glioma model. Clin. Cancer Res. 11 5965–5970. 10.1158/1078-0432.ccr-05-0371 [DOI] [PubMed] [Google Scholar]
- Kim S. M., Jeong C. H., Woo J. S., Ryu C. H., Lee J. H., Jeun S. S. (2016). In vivo near-infrared imaging for the tracking of systemically delivered mesenchymal stem cells: tropism for brain tumors and biodistribution. Int. J. Nanomed. 11 13–23. 10.2147/ijn.s97073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T., Momin E., Choi J., Yuan K., Zaidi H., Kim J., et al. (2011). Mesoporous silica-coated hollow manganese oxide nanoparticles as positive T1 contrast agents for labeling and MRI tracking of adipose-derived mesenchymal stem cells. J. Am. Chem. Soc. 133 2955–2961. 10.1021/ja1084095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinschmidt K., Klinge P. M., Stopa E., Wallrapp C., Glage S., Geigle P., et al. (2011). Alginate encapsulated human mesenchymal stem cells suppress syngeneic glioma growth in the immunocompetent rat. J. Microencapsul. 28 621–627. 10.3109/02652048.2011.599441 [DOI] [PubMed] [Google Scholar]
- Klimanskaya I. (2019). “Embryonic stem cells: derivation, properties and challenges,” in Principles of Regenerative Medicine. 3rd Edition ed, ed. Atala A. (Amsterdam: ElSevier; ). [Google Scholar]
- Koo Y. E., Reddy G. R., Bhojani M., Schneider R., Philbert M. A., Rehemtulla A., et al. (2006). Brain cancer diagnosis and therapy with nanoplatforms. Adv. Drug Deliv. Rev. 58 1556–1577. 10.1016/j.addr.2006.09.012 [DOI] [PubMed] [Google Scholar]
- Kosaka H., Ichikawa T., Kurozumi K., Kambara H., Inoue S., Maruo T., et al. (2012). Therapeutic effect of suicide gene-transferred mesenchymal stem cells in a rat model of glioma. Cancer Gene Ther. 19 572–578. 10.1038/cgt.2012.35 [DOI] [PubMed] [Google Scholar]
- Kozielski K. L., Ruiz-Valls A., Tzeng S. Y., Guerrero-Cazares H., Rui Y., Li Y., et al. (2019). Cancer-selective nanoparticles for combinatorial siRNA delivery to primary human GBM in vitro and in vivo. Biomaterials 209 79–87. 10.1016/j.biomaterials.2019.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunoh T., Shimura T., Kasai T., Matsumoto S., Mahmud H., Khayrani A. C., et al. (2019). Use of DNA-generated gold nanoparticles to radiosensitize and eradicate radioresistant glioma stem cells. Nanotechnology 30:055101. 10.1088/1361-6528/aaedd5 [DOI] [PubMed] [Google Scholar]
- Kus M., Alic T. Y., Kirbiyik C., Baslak C., Kara K., Kara D. A. (2018). “Chapter 24 - synthesis of nanoparticles,” in Handbook of Nanomaterials for Industrial Applications, ed. Mustansar Hussain C. (Amsterdam: Elsevier; ), 392–429. [Google Scholar]
- Lammers T., Peschke P., Kuhnlein R., Subr V., Ulbrich K., Debus J., et al. (2007). Effect of radiotherapy and hyperthermia on the tumor accumulation of HPMA copolymer-based drug delivery systems. J. Control. Release 117 333–341. 10.1016/j.jconrel.2006.10.032 [DOI] [PubMed] [Google Scholar]
- Lang F. M., Hossain A., Gumin J., Momin E. N., Shimizu Y., Ledbetter D., et al. (2018). Mesenchymal stem cells as natural biofactories for exosomes carrying miR-124a in the treatment of gliomas. Neuro Oncol. 20 380–390. 10.1093/neuonc/nox152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Velazquez M., Alkharboosh R., Norton E. S., Ramirez-Loera C., Freeman W. D., Guerrero-Cazares H., et al. (2020). Chitosan-based non-viral gene and drug delivery systems for brain cancer. Front. Neurol. 11:740 10.3389/fneur.2020.00740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lathia J. D., Li M., Hall P. E., Gallagher J., Hale J. S., Wu Q., et al. (2012). Laminin alpha 2 enables glioblastoma stem cell growth. Ann. Neurol. 72 766–778. 10.1002/ana.23674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Elkahloun A. G., Messina S. A., Ferrari N., Xi D., Smith C. L., et al. (2003). Cellular and genetic characterization of human adult bone marrow-derived neural stem-like cells: a potential antiglioma cellular vector. Cancer Res. 63, 8877–8889. [PubMed] [Google Scholar]
- Lee H. K., Finniss S., Cazacu S., Bucris E., Ziv-Av A., Xiang C., et al. (2013). Mesenchymal stem cells deliver synthetic microRNA mimics to glioma cells and glioma stem cells and inhibit their cell migration and self-renewal. Oncotarget 4 346–361. 10.18632/oncotarget.868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. H., Warner C. M., Jin H. E., Barnes E., Poda A. R., Perkins E. J., et al. (2017). Production of tunable nanomaterials using hierarchically assembled bacteriophages. Nat. Protoc. 12 1999–2013. 10.1038/nprot.2017.085 [DOI] [PubMed] [Google Scholar]
- Lee Y. J., Galoforo S. S., Berns C. M., Erdos G., Gupta A. K., Ways D. K., et al. (1995). Effect of ionizing radiation on AP-1 binding activity and basic fibroblast growth factor gene expression in drug-sensitive human breast carcinoma MCF-7 and multidrug-resistant MCF-7/ADR cells. J. Biol. Chem. 270 28790–28796. 10.1074/jbc.270.48.28790 [DOI] [PubMed] [Google Scholar]
- Li Q., Wijesekera O., Salas S. J., Wang J. Y., Zhu M., Aprhys C., et al. (2014). Mesenchymal stem cells from human fat engineered to secrete BMP4 are nononcogenic, suppress brain cancer, and prolong survival. Clin. Cancer Res. 20 2375–2387. 10.1158/1078-0432.ccr-13-1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S. P., Jiang Q., Liu S. L., Zhang Y. L., Tian Y. H., Song C., et al. (2018). A DNA nanorobot functions as a cancer therapeutic in response to a molecular trigger in vivo. Nat. Biotechnol. 36 258–264. 10.1038/nbt.4071 [DOI] [PubMed] [Google Scholar]
- Li X. T., Tang W., Xie H. J., Liu S., Song X. L., Xiao Y., et al. (2019). The efficacy of RGD modified liposomes loaded with vinorelbine plus tetrandrine in treating resistant brain glioma. J. Liposome Res. 29 21–34. 10.1080/08982104.2017.1408649 [DOI] [PubMed] [Google Scholar]
- Li Z., Bao S., Wu Q., Wang H., Eyler C., Sathornsumetee S., et al. (2009). Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell. 15 501–513. 10.1016/j.ccr.2009.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K., Li Z., Luo Y., Zhang Q., Yin F., Xu L., et al. (2020). Intelligent nanocomposites with intrinsic blood-brain-barrier crossing ability designed for highly specific MR imaging and sonodynamic therapy of glioblastoma. Small 16:e1906985. [DOI] [PubMed] [Google Scholar]
- Liao L. Y., Liu J., Dreaden E. C., Morton S. W., Shopsowitz K. E., Hammond P. T., et al. (2014). A convergent synthetic platform for single-nanoparticle combination cancer therapy: ratiometric loading and controlled release of cisplatin, doxorubicin, and camptothecin. J. Am. Chem. Soc. 136 5896–5899. 10.1021/ja502011g [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., He H., Xiao D., Yin S., Ji W., Jiang S., et al. (2018). Recent advances of plasmonic nanoparticles and their applications. Materials 11:1833. 10.3390/ma11101833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yin F., Zhao M., Zhou C., Ren J., Huang Q., et al. (2016). The homing and inhibiting effects of hNSCs-BMP4 on human glioma stem cells. Oncotarget 7 17920–17931. 10.18632/oncotarget.7472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luque-Michel E., Sebastian V., Larrea A., Marquina C., Blanco-Prieto M. J. (2019). Co-encapsulation of superparamagnetic nanoparticles and doxorubicin in PLGA nanocarriers: development, characterization and in vitro antitumor efficacy in glioma cells. Eur. J. Pharm. Biopharm. 145 65–75. 10.1016/j.ejpb.2019.10.004 [DOI] [PubMed] [Google Scholar]
- Ma Y., Li M., Liu J., Pang C., Zhang J., Li Y., et al. (2018). Location, isolation, and identification of mesenchymal stem cells from adult human sweat glands. Stem Cells Int. 2018 2090276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhankumar A. B., Slagle-Webb B., Wang X., Yang Q. X., Antonetti D. A., Miller P. A., et al. (2009). Efficacy of interleukin-13 receptor-targeted liposomal doxorubicin in the intracranial brain tumor model. Mol. Cancer Ther. 8 648–654. 10.1158/1535-7163.mct-08-0853 [DOI] [PubMed] [Google Scholar]
- Mahato D., De Biase G., Ruiz-Garcia H. J., Grover S., Rosenfeld S., Quiñones-Hinojosa A., et al. (2018). Impact of facility type and volume on post-surgical outcomes following diagnosis of WHO grade II glioma. J. Clin. Neurosci. 58 34–41. 10.1016/j.jocn.2018.10.078 [DOI] [PubMed] [Google Scholar]
- Maier-Hauff K., Rothe R., Scholz R., Gneveckow U., Wust P., Thiesen B., et al. (2007). Intracranial thermotherapy using magnetic nanoparticles combined with external beam radiotherapy: results of a feasibility study on patients with glioblastoma multiforme. J. Neuro Oncol. 81 53–60. 10.1007/s11060-006-9195-0 [DOI] [PubMed] [Google Scholar]
- Mampre D., Ehresman J., Pinilla-Monsalve G., Osorio M. A. G., Olivi A., Quinones-Hinojosa A., et al. (2018). Extending the resection beyond the contrast-enhancement for glioblastoma: feasibility, efficacy, and outcomes. Br. J. Neurosurg. 32 528–535. 10.1080/02688697.2018.1498450 [DOI] [PubMed] [Google Scholar]
- Mangraviti A., Tzeng S. Y., Gullotti D., Kozielski K. L., Kim J. E., Seng M., et al. (2016). Non-virally engineered human adipose mesenchymal stem cells produce BMP4, target brain tumors, and extend survival. Biomaterials 100 53–66. 10.1016/j.biomaterials.2016.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangraviti A., Tzeng S. Y., Kozielski K. L., Wang Y., Jin Y., Gullotti D., et al. (2015). Polymeric nanoparticles for nonviral gene therapy extend brain tumor survival in vivo. ACS Nano 9 1236–1249. 10.1021/nn504905q [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marenco-Hillembrand L., Prevatt C., Suarez-Meade P., Ruiz-Garcia H., Quinones-Hinojosa A., Chaichana K. L. (2020). Minimally invasive surgical outcomes for deep-seated brain lesions treated with different tubular retraction systems: a systematic review and meta-analysis. World Neurosurg. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Martinez-Quintanilla J., He D., Wakimoto H., Alemany R., Shah K. (2015). Encapsulated stem cells loaded with hyaluronidase-expressing oncolytic virus for brain tumor therapy. Mol. Therapy 23 108–118. 10.1038/mt.2014.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Rovira I., Seksek O., Dokic I., Brons S., Abdollahi A., Yousef I. (2020). Study of the intracellular nanoparticle-based radiosensitization mechanisms in F98 glioma cells treated with charged particle therapy through synchrotron-based infrared microspectroscopy. Analyst 145 2345–2356. 10.1039/c9an02350j [DOI] [PubMed] [Google Scholar]
- McGirt M. J., Chaichana K. L., Attenello F. J., Weingart J. D., Than K., Burger P. C., et al. (2008). Extent of surgical resection is independently associated with survival in patients with hemispheric infiltrating low-grade gliomas. Neurosurgery 63 700–708. 10.1227/01.neu.0000325729.41085.73 [DOI] [PubMed] [Google Scholar]
- McGirt M. J., Chaichana K. L., Gathinji M., Attenello F. J., Than K., Olivi A., et al. (2009). Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J. Neurosurg. 110 156–162. 10.3171/2008.4.17536 [DOI] [PubMed] [Google Scholar]
- McNeeley K. M., Karathanasis E., Annapragada A. V., Bellamkonda R. V. (2009). Masking and triggered unmasking of targeting ligands on nanocarriers to improve drug delivery to brain tumors. Biomaterials 30 3986–3995. 10.1016/j.biomaterials.2009.04.012 [DOI] [PubMed] [Google Scholar]
- Meca-Cortes O., Guerra-Rebollo M., Garrido C., Borros S., Rubio N., Blanco J. (2017). CRISPR/Cas9-mediated knockin application in cell therapy: a non-viral procedure for bystander treatment of glioma in mice. Mol. Ther. Nucleic Acids 8 395–403. 10.1016/j.omtn.2017.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X., Ichim T. E., Zhong J., Rogers A., Yin Z., Jackson J., et al. (2007). Endometrial regenerative cells: a novel stem cell population. J. Transl. Med. 5:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X., Zhao Y., Han B., Zha C., Zhang Y., Li Z., et al. (2020). Dual functionalized brain-targeting nanoinhibitors restrain temozolomide-resistant glioma via attenuating EGFR and MET signaling pathways. Nat. Commun. 11:594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon L. G., Pratt J., Yang H. W., Black P. M., Sorensen G. A., Carroll R. S. (2012). Imaging of human mesenchymal stromal cells: homing to human brain tumors. J. Neuro Oncol. 107 257–267. 10.1007/s11060-011-0754-7 [DOI] [PubMed] [Google Scholar]
- Miao Z., Jin J., Chen L., Zhu J., Huang W., Zhao J., et al. (2006). Isolation of mesenchymal stem cells from human placenta: comparison with human bone marrow mesenchymal stem cells. Cell Biol. Int. 30 681–687. 10.1016/j.cellbi.2006.03.009 [DOI] [PubMed] [Google Scholar]
- Mooney R., Roma L., Zhao D., Van Haute D., Garcia E., Kim S. U., et al. (2014a). Neural stem cell-mediated intratumoral delivery of gold nanorods improves photothermal therapy. ACS Nano 8 12450–12460. 10.1021/nn505147w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney R., Weng Y., Tirughana-Sambandan R., Valenzuela V., Aramburo S., Garcia E., et al. (2014b). Neural stem cells improve intracranial nanoparticle retention and tumor-selective distribution. Future Oncol. 10 401–415. 10.2217/fon.13.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morshed R. A., Gutova M., Juliano J., Barish M. E., Hawkins-Daarud A., Oganesyan D., et al. (2015). Analysis of glioblastoma tumor coverage by oncolytic virus-loaded neural stem cells using MRI-based tracking and histological reconstruction. Cancer Gene Ther. 22 55–61. 10.1038/cgt.2014.72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muroski M. E., Morshed R. A., Cheng Y., Vemulkar T., Mansell R., Han Y., et al. (2016). Controlled payload release by magnetic field triggered neural stem cell destruction for malignant glioma treatment. PLoS One 11:e0145129. 10.1371/journal.pone.0145129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura K., Ito Y., Kawano Y., Kurozumi K., Kobune M., Tsuda H., et al. (2004). Antitumor effect of genetically engineered mesenchymal stem cells in a rat glioma model. Gene Ther. 11 1155–1164. 10.1038/sj.gt.3302276 [DOI] [PubMed] [Google Scholar]
- Neri M., Maderna C., Cavazzin C., Deidda-Vigoriti V., Politi L. S., Scotti G., et al. (2008). Efficient in vitro labeling of human neural precursor cells with superparamagnetic iron oxide particles: relevance for in vivo cell tracking. Stem Cells 26 505–516. 10.1634/stemcells.2007-0251 [DOI] [PubMed] [Google Scholar]
- Ostrom Q. T., Cioffi G., Gittleman H., Patil N., Waite K., Kruchko C., et al. (2019). CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2012-2016. Neuro Oncol. 21(Suppl. 5), v1–v100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens D. E., Peppas N. A. (2006). Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int. J. Pharm. 307 93–102. 10.1016/j.ijpharm.2005.10.010 [DOI] [PubMed] [Google Scholar]
- Park J. H., Ryu C. H., Kim M. J., Jeun S. S. (2015). Combination therapy for gliomas using temozolomide and interferon-beta secreting human bone marrow derived mesenchymal stem cells. J. Korean Neurosurg. Soc. 57 323–328. 10.3340/jkns.2015.57.5.323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. S., Qiao L., Su Z. Z., Hinman D., Willoughby K., McKinstry R., et al. (2001). Ionizing radiation modulates vascular endothelial growth factor (VEGF) expression through multiple mitogen activated protein kinase dependent pathways. Oncogene 20 3266–3280. 10.1038/sj.onc.1204258 [DOI] [PubMed] [Google Scholar]
- Parker Kerrigan B. C., Hossain A., Yamashita S., Lang F. F. (2018). Stem cell therapy of gliomas. Prog. Neurol. Surg. 32 124–151. 10.1159/000469686 [DOI] [PubMed] [Google Scholar]
- Patel K. D., Singh R. K., Kim H. W. (2019). Carbon-based nanomaterials as an emerging platform for theranostics. Mater. Horiz. 6 434–469. 10.1039/c8mh00966j [DOI] [Google Scholar]
- Patki S., Kadam S., Chandra V., Bhonde R. (2010). Human breast milk is a rich source of multipotent mesenchymal stem cells. Hum. Cell. 23 35–40. 10.1111/j.1749-0774.2010.00083.x [DOI] [PubMed] [Google Scholar]
- Pavon L. F., Sibov T. T., de Souza A. V., da Cruz E. F., Malheiros S. M. F., Cabral F. R., et al. (2018). Tropism of mesenchymal stem cell toward CD133(+) stem cell of glioblastoma in vitro and promote tumor proliferation in vivo. Stem Cell Res. Ther. 9:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendleton C., Li Q., Chesler D. A., Yuan K., Guerrero-Cazares H., Quinones-Hinojosa A. (2013). Mesenchymal stem cells derived from adipose tissue vs bone marrow: in vitro comparison of their tropism towards gliomas. PLoS One 8:e58198. 10.1371/journal.pone.0058198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poloni A., Rosini V., Mondini E., Maurizi G., Mancini S., Discepoli G., et al. (2008). Characterization and expansion of mesenchymal progenitor cells from first-trimester chorionic villi of human placenta. Cytotherapy 10 690–697. 10.1080/14653240802419310 [DOI] [PubMed] [Google Scholar]
- Portney N. G., Ozkan M. (2006). Nano-oncology: drug delivery, imaging, and sensing. Anal. Bioanal. Chem. 384 620–630. 10.1007/s00216-005-0247-7 [DOI] [PubMed] [Google Scholar]
- Portnow J., Synold T. W., Badie B., Tirughana R., Lacey S. F., D’Apuzzo M., et al. (2017). Neural stem cell-based anticancer gene therapy: a first-in-human study in recurrent high-grade glioma patients. Clin. Cancer Res. 23 2951–2960. 10.1158/1078-0432.ccr-16-1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purbia R., Paria S. (2015). Yolk/shell nanoparticles: classifications, synthesis, properties, and applications. Nanoscale 7 19789–19873. 10.1039/c5nr04729c [DOI] [PubMed] [Google Scholar]
- Qi N., Zhang Y., Tang X., Li A. (2020). Cationic/anionic polyelectrolyte (PLL/PGA) coated vesicular phospholipid gels (VPGs) loaded with cytarabine for sustained release and anti-glioma effects. Drug Des. Devel. Ther. 14 1825–1836. 10.2147/dddt.s248362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiao Y., Gumin J., MacLellan C. J., Gao F., Bouchard R., Lang F. F., et al. (2018). Magnetic resonance and photoacoustic imaging of brain tumor mediated by mesenchymal stem cell labeled with multifunctional nanoparticle introduced via carotid artery injection. Nanotechnology 29:165101. 10.1088/1361-6528/aaaf16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Zúññiga R., González-Pérez O., Macías-Ornelas A., Capilla-González V., Quiñones-Hinojosa A. (2012). Ethical implications in the use of embryonic and adult neural stem cells. Stem Cells Int. 2012:470949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranganathan B., Miller C., Sinskey A. (2018). Biocompatible synthetic and semi-synthetic polymers - a patent analysis. Pharm. Nanotechnol. 6 28–37. 10.2174/2211738505666171023152549 [DOI] [PubMed] [Google Scholar]
- Rego G. N. A., Mamani J. B., Souza T. K. F., Nucci M. P., Silva H. R. D., Gamarra L. F. (2019). Therapeutic evaluation of magnetic hyperthermia using Fe3O4-aminosilane-coated iron oxide nanoparticles in glioblastoma animal model. Einstein 17:eAO4786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rego G. N. A., Nucci M. P., Mamani J. B., Oliveira F. A., Marti L. C., Filgueiras I. S., et al. (2020). Therapeutic efficiency of multiple applications of magnetic hyperthermia technique in glioblastoma using aminosilane coated iron oxide nanoparticles: in vitro and in vivo study. Int. J. Mol. Sci. 21:958. 10.3390/ijms21030958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis C. P., Neufeld R. J., Ribeiro A. J., Veiga F. (2006). Nanoencapsulation I. Methods for preparation of drug-loaded polymeric nanoparticles. Nanomedicine 2 8–21. 10.1016/j.nano.2005.12.003 [DOI] [PubMed] [Google Scholar]
- Ridge S. M., Sullivan F. J., Glynn S. A. (2017). Mesenchymal stem cells: key players in cancer progression. Mol. Cancer 16:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts R., Smyth J. W., Will J., Roberts P., Grek C. L., Ghatnekar G. S., et al. (2020). Development of PLGA nanoparticles for sustained release of a connexin43 mimetic peptide to target glioblastoma cells. Mater. Sci. Eng. C Mater. Biol. Appl. 108:110191. 10.1016/j.msec.2019.110191 [DOI] [PubMed] [Google Scholar]
- Romero G., Moya S. E. (2012). “Chapter 4 - synthesis of organic nanoparticles,” in Frontiers of Nanoscience, Vol. 4 eds de la Fuente J. M., Grazu V. (Amsterdam: Elsevier; ), 115–141. 10.1016/b978-0-12-415769-9.00004-2 [DOI] [Google Scholar]
- Roubelakis M. G., Pappa K. I., Bitsika V., Zagoura D., Vlahou A., Papadaki H. A., et al. (2007). Molecular and proteomic characterization of human mesenchymal stem cells derived from amniotic fluid: comparison to bone marrow mesenchymal stem cells. Stem Cells Dev. 16 931–952. 10.1089/scd.2007.0036 [DOI] [PubMed] [Google Scholar]
- Ruan S., Xie R., Qin L., Yu M., Xiao W., Hu C., et al. (2019). Aggregable nanoparticles-enabled chemotherapy and autophagy inhibition combined with anti-PD-L1 antibody for improved glioma treatment. Nano Lett. 19 8318–8332. 10.1021/acs.nanolett.9b03968 [DOI] [PubMed] [Google Scholar]
- Ruiz-Garcia H., Alvarado-Estrada K., Schiapparelli P., Quinones-Hinojosa A., Trifiletti D. M. (2020) Engineering three-dimensional tumor models to study glioma cancer stem cells and tumor microenvironment. Front. Cell. Neurosci. 14:558381 10.3389/fncel.2020.558381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu C. H., Park S. H., Park S. A., Kim S. M., Lim J. Y., Jeong C. H., et al. (2011). Gene therapy of intracranial glioma using interleukin 12-secreting human umbilical cord blood-derived mesenchymal stem cells. Hum. Gene Ther. 22 733–743. 10.1089/hum.2010.187 [DOI] [PubMed] [Google Scholar]
- Saxena S., Pramod B. J., Dayananda B. C., Nagaraju K. (2015). Design, architecture and application of nanorobotics in oncology. Indian J. Cancer 52 236–241. 10.4103/0019-509x.175805 [DOI] [PubMed] [Google Scholar]
- Shahar T., Rozovski U., Hess K. R., Hossain A., Gumin J., Gao F., et al. (2017). Percentage of mesenchymal stem cells in high-grade glioma tumor samples correlates with patient survival. Neuro Oncol. 19 660–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma V. K., Filip J., Zboril R., Varma R. S. (2015). Natural inorganic nanoparticles–formation, fate, and toxicity in the environment. Chem. Soc. Rev. 44 8410–8423. 10.1039/c5cs00236b [DOI] [PubMed] [Google Scholar]
- Shen Y., Wu C., Uyeda T. Q. P., Plaza G. R., Liu B., Han Y., et al. (2017). Elongated nanoparticle aggregates in cancer cells for mechanical destruction with low frequency rotating magnetic field. Theranostics 7 1735–1748. 10.7150/thno.18352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi D., Mi G., Shen Y., Webster T. J. (2019). Glioma-targeted dual functionalized thermosensitive Ferri-liposomes for drug delivery through an in vitro blood-brain barrier. Nanoscale 11 15057–15071. 10.1039/c9nr03931g [DOI] [PubMed] [Google Scholar]
- Singh S. K., Clarke I. D., Terasaki M., Bonn V. E., Hawkins C., Squire J., et al. (2003). Identification of a cancer stem cell in human brain tumors. Cancer Res. 63 5821–5828. [PubMed] [Google Scholar]
- Smith C. L., Chaichana K. L., Lee Y. M., Lin B., Stanko K. M., O’Donnell T., et al. (2015). Pre-exposure of human adipose mesenchymal stem cells to soluble factors enhances their homing to brain cancer. Stem Cells Transl. Med. 4 239–251. 10.5966/sctm.2014-0149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder E. Y., Deitcher D. L., Walsh C., Arnold-Aldea S., Hartwieg E. A., Cepko C. L. (1992). Multipotent neural cell lines can engraft and participate in development of mouse cerebellum. Cell 68 33–51. 10.1016/0092-8674(92)90204-p [DOI] [PubMed] [Google Scholar]
- Sonabend A. M., Ulasov I. V., Tyler M. A., Rivera A. A., Mathis J. M., Lesniak M. S. (2008). Mesenchymal stem cells effectively deliver an oncolytic adenovirus to intracranial glioma. Stem Cells 26 831–841. 10.1634/stemcells.2007-0758 [DOI] [PubMed] [Google Scholar]
- Soppimath K. S., Tan D. C.-W., Yang Y.-Y. (2005). pH-triggered thermally responsive polymer core–shell nanoparticles for drug delivery. Adv. Mater. 17 318–323. 10.1002/adma.200401057 [DOI] [Google Scholar]
- Sousa F., Dhaliwal H. K., Gattacceca F., Sarmento B., Amiji M. M. (2019). Enhanced anti-angiogenic effects of bevacizumab in glioblastoma treatment upon intranasal administration in polymeric nanoparticles. J. Control. Release 309 37–47. 10.1016/j.jconrel.2019.07.033 [DOI] [PubMed] [Google Scholar]
- Spina G., Quarenghi F., Rodenghi F., Matscher R., Lavagnini A. (1975). [Gastrokinetic effect of Vincamine]. Farmaco Prat. 30 512–522. [PubMed] [Google Scholar]
- Stupp R., Mason W. P., van den Bent M. J., Weller M., Fisher B., Taphoorn M. J., et al. (2005). Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 352 987–996. [DOI] [PubMed] [Google Scholar]
- Suarez-Meade P., Marenco-Hillembrand L., Prevatt C., Murguia-Fuentes R., Mohamed A., Alsaeed T., et al. (2020). Awake vs. asleep motor mapping for glioma resection: a systematic review and meta-analysis. Acta Neurochir. 162 1709–1720. 10.1007/s00701-020-04357-y [DOI] [PubMed] [Google Scholar]
- Svensson A., Ramos-Moreno T., Eberstal S., Scheding S., Bengzon J. (2017). Identification of two distinct mesenchymal stromal cell populations in human malignant glioma. J. Neuro Oncol. 131 245–254. 10.1007/s11060-016-2302-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K., Yamanaka S. (2006). Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126 663–676. 10.1016/j.cell.2006.07.024 [DOI] [PubMed] [Google Scholar]
- Tamura R., Miyoshi H., Morimoto Y., Oishi Y., Sampetrean O., Iwasawa C., et al. (2020). Gene therapy using neural stem/progenitor cells derived from human induced pluripotent stem cells: visualization of migration and bystander killing effect. Hum. Gene Ther. 31, 352–366. 10.1089/hum.2019.326 [DOI] [PubMed] [Google Scholar]
- Tanrikulu B., Ziyal I., Bayri Y. (2019). In vitro effects of mesenchymal stem cells and various agents on apoptosis of glioblastoma cells. Turkish neurosurgery 29 26–32. [DOI] [PubMed] [Google Scholar]
- Thimsen E., Johnson M., Zhang X., Wagner A. J., Mkhoyan K. A., Kortshagen U. R., et al. (2014). High electron mobility in thin films formed via supersonic impact deposition of nanocrystals synthesized in nonthermal plasmas. Nat. Commun. 5:5822. [DOI] [PubMed] [Google Scholar]
- Thu M. S., Najbauer J., Kendall S. E., Harutyunyan I., Sangalang N., Gutova M., et al. (2009). Iron labeling and pre-clinical MRI visualization of therapeutic human neural stem cells in a murine glioma model. PLoS One 4:e7218. 10.1371/journal.pone.0007218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian M., Ticer T., Wang Q., Walker S., Pham A., Suh A., et al. (2020). Adipose-derived biogenic nanoparticles for suppression of inflammation. Small 16:e1904064. [DOI] [PubMed] [Google Scholar]
- Tirughana R., Metz M. Z., Li Z., Hall C., Hsu D., Beltzer J., et al. (2018). GMP production and scale-up of adherent neural stem cells with a quantum cell expansion system. Mol. Ther. Methods Clin. Dev. 10 48–56. 10.1016/j.omtm.2018.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzeng S. Y., Wilson D. R., Hansen S. K., Quiñones-Hinojosa A., Green J. J. (2016). Polymeric nanoparticle-based delivery of TRAIL DNA for cancer-specific killing. Bioeng. Transl. Med. 1 149–159. 10.1002/btm2.10019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhl M., Weiler M., Wick W., Jacobs A. H., Weller M., Herrlinger U. (2005). Migratory neural stem cells for improved thymidine kinase-based gene therapy of malignant gliomas. Biochem. Biophys. Res. Commun. 328, 125–129. 10.1016/j.bbrc.2004.12.164 [DOI] [PubMed] [Google Scholar]
- Ullah I., Chung K., Bae S., Li Y., Kim C., Choi B., et al. (2020). Nose-to-brain delivery of cancer-targeting paclitaxel-loaded nanoparticles potentiates anti-tumor effects in malignant glioblastoma. Mol. Pharm. 17 1193–1204. 10.1021/acs.molpharmaceut.1029b01215 [DOI] [PubMed] [Google Scholar]
- van Eekelen M., Sasportas L. S., Kasmieh R., Yip S., Figueiredo J. L., Louis D. N., et al. (2010). Human stem cells expressing novel TSP-1 variant have anti-angiogenic effect on brain tumors. Oncogene 29 3185–3195. 10.1038/onc.2010.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Landeghem F. K., Maier-Hauff K., Jordan A., Hoffmann K. T., Gneveckow U., Scholz R., et al. (2009). Post-mortem studies in glioblastoma patients treated with thermotherapy using magnetic nanoparticles. Biomaterials 30 52–57. 10.1016/j.biomaterials.2008.09.044 [DOI] [PubMed] [Google Scholar]
- Wagner W., Wein F., Seckinger A., Frankhauser M., Wirkner U., Krause U., et al. (2005). Comparative characteristics of mesenchymal stem cells from human bone marrow, adipose tissue, and umbilical cord blood. Exp. Hematol. 33 1402–1416. 10.1016/j.exphem.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Wang C. H., Chiou S. H., Chou C. P., Chen Y. C., Huang Y. J., Peng C. A. (2011). Photothermolysis of glioblastoma stem-like cells targeted by carbon nanotubes conjugated with CD133 monoclonal antibody. Nanomedicine 7 69–79. 10.1016/j.nano.2010.06.010 [DOI] [PubMed] [Google Scholar]
- Wang H., Li L., Ye J., Wang R., Wang R., Hu J., et al. (2020). Improving the oral bioavailability of an anti-glioma prodrug CAT3 using novel solid lipid nanoparticles containing oleic acid-CAT3 conjugates. Pharmaceutics 12:E126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang N., Sun P., Lv M., Tong G., Jin X., Zhu X. (2017). Mustard-inspired delivery shuttle for enhanced blood-brain barrier penetration and effective drug delivery in glioma therapy. Biomater. Sci. 5 1041–1050. 10.1039/c7bm00133a [DOI] [PubMed] [Google Scholar]
- Wang X., Gao J., Ouyang X., Wang J., Sun X., Lv Y. (2018). Mesenchymal stem cells loaded with paclitaxel-poly(lactic-co-glycolic acid) nanoparticles for glioma-targeting therapy. Int. J. Nanomed. 13 5231–5248. 10.2147/ijn.s167142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Tian Y., Liao X., Tang Y., Ni Q., Sun J., et al. (2020). Enhancing selective photosensitizer accumulation and oxygen supply for high-efficacy photodynamic therapy toward glioma by 5-aminolevulinic acid loaded nanoplatform. J. Coll. Interf. Sci. 565 483–493. 10.1016/j.jcis.2020.01.020 [DOI] [PubMed] [Google Scholar]
- Wegscheid M. L., Morshed R. A., Cheng Y., Lesniak M. S. (2014). The art of attraction: applications of multifunctional magnetic nanomaterials for malignant glioma. Expert Opin. Drug Deliv. 11 957–975. 10.1517/17425247.2014.912629 [DOI] [PubMed] [Google Scholar]
- Wei C., Zhao Y. S. (2016). Photonic applications of metal-dielectric heterostructured nanomaterials. ACS Appl. Mater. Inter. 8 3703–3713. 10.1021/acsami.5b08086 [DOI] [PubMed] [Google Scholar]
- Wilson D. R., Mosenia A., Suprenant M. P., Upadhya R., Routkevitch D., Meyer R. A., et al. (2017a). Continuous microfluidic assembly of biodegradable poly(beta-amino ester)/DNA nanoparticles for enhanced gene delivery. J. Biomed. Mater. Res. A 105 1813–1825. 10.1002/jbm.a.36033 [DOI] [PubMed] [Google Scholar]
- Wilson D. R., Routkevitch D., Rui Y., Mosenia A., Wahlin K. J., Quinones-Hinojosa A., et al. (2017b). A triple-fluorophore-labeled nucleic acid pH nanosensor to investigate non-viral gene delivery. Mol. Ther. 25 1697–1709. 10.1016/j.ymthe.2017.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Hu J., Zhou L., Mao Y., Yang B., Gao L., et al. (2008). In vivo tracking of superparamagnetic iron oxide nanoparticle-labeled mesenchymal stem cell tropism to malignant gliomas using magnetic resonance imaging. Laboratory investigation. J. Neurosurg. 108 320–329. 10.3171/jns/2008/108/2/0320 [DOI] [PubMed] [Google Scholar]
- Xu B., Zhang Q., Luo X., Ning X., Luo J., Guo J., et al. (2020). Selenium nanoparticles reduce glucose metabolism and promote apoptosis of glioma cells through reactive oxygen species-dependent manner. Neuroreport 31 226–234. 10.1097/wnr.0000000000001386 [DOI] [PubMed] [Google Scholar]
- Xu Z. P., Zeng Q. H., Lu G. Q., Yu A. B. (2006). Inorganic nanoparticles as carriers for efficient cellular delivery. Chem. Eng. Sci. 61 1027–1040. 10.1016/j.ces.2005.06.019 [DOI] [Google Scholar]
- Yamazoe T., Koizumi S., Yamasaki T., Amano S., Tokuyama T., Namba H. (2015). Potent tumor tropism of induced pluripotent stem cells and induced pluripotent stem cell-derived neural stem cells in the mouse intracerebral glioma model. Int. J. Oncol. 46 147–152. 10.3892/ijo.2014.2702 [DOI] [PubMed] [Google Scholar]
- Ye C., Pan B., Xu H., Zhao Z., Shen J., Lu J., et al. (2019). Co-delivery of GOLPH3 siRNA and gefitinib by cationic lipid-PLGA nanoparticles improves EGFR-targeted therapy for glioma. J. Mol. Med. 97 1575–1588. 10.1007/s00109-019-01843-4 [DOI] [PubMed] [Google Scholar]
- Yi D., Xiang W., Zhang Q., Cen Y., Su Q., Zhang F., et al. (2018). Human glioblastoma-derived mesenchymal stem cell to pericytes transition and angiogenic capacity in glioblastoma microenvironment. Cell. Physiol. Biochem. 46 279–290. 10.1159/000488429 [DOI] [PubMed] [Google Scholar]
- Yong R. L., Shinojima N., Fueyo J., Gumin J., Vecil G. G., Marini F. C., et al. (2009). Human bone marrow-derived mesenchymal stem cells for intravascular delivery of oncolytic adenovirus Delta24-RGD to human gliomas. Cancer Res. 69 8932–8940. 10.1158/0008-5472.can-08-3873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J. S., Morshed R. A., Kim J. W., Balyasnikova I. V., Ahmed A. U., Lesniak M. S. (2014). Advances in stem cells, induced pluripotent stem cells, and engineered cells: delivery vehicles for anti-glioma therapy. Expert Opin. Drug Deliv. 11 1733–1746. 10.1517/17425247.2014.937420 [DOI] [PubMed] [Google Scholar]
- Yu D., Khan O. F., Suva M. L., Dong B., Panek W. K., Xiao T., et al. (2017). Multiplexed RNAi therapy against brain tumor-initiating cells via lipopolymeric nanoparticle infusion delays glioblastoma progression. Proc. Natl. Acad. Sci. U.S.A. 114 E6147–E6156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M. A., Su D. Y., Yang Y. Y., Qin L., Hu C., Liu R., et al. (2019). D-T7 peptide-modified PEGylated bilirubin nanoparticles loaded with cediranib and paclitaxel for antiangiogenesis and chemotherapy of glioma. ACS Appl. Mater. Inter. 11 176–186. 10.1021/acsami.8b16219 [DOI] [PubMed] [Google Scholar]
- Yuan J. Z., Levitin H. M., Frattini V., Bush E. C., Boyett D. M., Samanamud J., et al. (2018). Single-cell transcriptome analysis of lineage diversity in high-grade glioma. Genome Med. 10:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeddou M., Briquet A., Relic B., Josse C., Malaise M. G., Gothot A., et al. (2010). The umbilical cord matrix is a better source of mesenchymal stem cells (MSC) than the umbilical cord blood. Cell Biol. Int. 34 693–701. 10.1042/cbi20090414 [DOI] [PubMed] [Google Scholar]
- Zhang P., Miska J., Lee-Chang C., Rashidi A., Panek W. K., An S., et al. (2019). Therapeutic targeting of tumor-associated myeloid cells synergizes with radiation therapy for glioblastoma. Proc. Natl. Acad. Sci. U.S.A. 116 23714–23723. 10.1073/pnas.1906346116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Xiang W., Yi D. Y., Xue B. Z., Wen W. W., Abdelmaksoud A., et al. (2018). Current status and potential challenges of mesenchymal stem cell-based therapy for malignant gliomas. Stem Cell Res. Ther. 9:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Liu P., Ma J., Li D., Yang H., Chen W., et al. (2019). Enhancement of radiosensitization by silver nanoparticles functionalized with polyethylene glycol and aptamer As1411 for glioma irradiation therapy. Int. J. Nanomed. 14 9483–9496. 10.2147/ijn.s224160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao M., Zhao M., Fu C., Yu Y., Fu A. (2018). Targeted therapy of intracranial glioma model mice with curcumin nanoliposomes. Int. J. Nanomed. 13 1601–1610. 10.2147/ijn.s157019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Cao X., Cai X., Tian Y., Wang D., Qi J., et al. (2020). Pifithrin-mu incorporated in gold nanoparticle amplifies pro-apoptotic unfolded protein response cascades to potentiate synergistic glioblastoma therapy. Biomaterials 232:119677. 10.1016/j.biomaterials.2019.119677 [DOI] [PubMed] [Google Scholar]
- Zhu J., Zhou L., XingWu F. (2006). Tracking neural stem cells in patients with brain trauma. N. Engl. J. Med. 355 2376–2378. 10.1056/nejmc055304 [DOI] [PubMed] [Google Scholar]
- ZhuGe D. L., Wang L. F., Chen R., Li X. Z., Huang Z. W., Yao Q., et al. (2019). Cross-linked nanoparticles of silk fibroin with proanthocyanidins as a promising vehicle of indocyanine green for photo-thermal therapy of glioma. Artif. Cells Nanomed. Biotechnol. 47 4293–4304. 10.1080/21691401.2019.1699819 [DOI] [PubMed] [Google Scholar]
- Zuk P. A., Zhu M., Mizuno H., Huang J., Futrell J. W., Katz A. J., et al. (2001). Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 7 211–228. 10.1089/107632701300062859 [DOI] [PubMed] [Google Scholar]