Abstract
Colorectal cancer (CRC) incidence increases yearly, and is three to four times higher in developed countries compared to developing countries. The well-known risk factors have been attributed to low physical activity, overweight, obesity, dietary consumption including excessive consumption of red processed meats, alcohol, and low dietary fiber content. There is growing evidence of the interplay between diet and gut microbiota in CRC carcinogenesis. Although there appears to be a direct causal role for gut microbes in the development of CRC in some animal models, the link between diet, gut microbes, and colonic carcinogenesis has been established largely as an association rather than as a cause-and-effect relationship. This is especially true for human studies. As essential dietary factors influence CRC risk, the role of proteins, carbohydrates, fat, and their end products are considered as part of the interplay between diet and gut microbiota. The underlying molecular mechanisms of colon carcinogenesis mediated by gut microbiota are also discussed. Human biological responses such as inflammation, oxidative stress, deoxyribonucleic acid (DNA) damage can all influence dysbiosis and consequently CRC carcinogenesis. Dysbiosis could add to CRC risk by shifting the effect of dietary components toward promoting a colonic neoplasm together with interacting with gut microbiota. It follows that dietary intervention and gut microbiota modulation may play a vital role in reducing CRC risk.
Keywords: colorectal cancer, colon carcinogenesis, diet, gut microbiota, protein, fat, carbohydrate, bacteria interaction
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer and the second most deadly cancer in the world, with about 1.8 million new cases and almost 881,000 deaths in 2018, comprising 5.8% of all cancer deaths that year (Rawla et al., 2019). The CRC global burden is expected to increase by 60% by 2030, to approximately 2.2 million new cases and 1.1 million deaths per annum (Rawla et al., 2019). CRC incidence is three to four times higher in developed countries than developing countries, reflecting the state of CRC as a marker of socioeconomic development (Bray et al., 2018). The known risk factors are low physical activity; overweight and obesity; dietary habits including excessive consumption of red, processed meats and alcohol, and low dietary fibers (World Cancer Research Fund/American Institute for Cancer Research, 2018). The rapid rise of CRC incidence among individuals younger than 50 years old especially in high-income countries (Araghi et al., 2019; Siegel et al., 2019; Vuik et al., 2019) coupled with the fact that most CRC incidents arise sporadically (Yang and Yu, 2018) further point to the influence of lifestyle factors on CRC development.
Human gut microbiota is dominated by three primary phyla, namely Firmicutes (30–50%), Bacteroidetes (20–40%), and Actinobacteria (1–10%) (Gagnière et al., 2016). Strict anaerobes such as Bifidobacterium, Fusobacterium, Bacteroides, Eubacterium, Peptostreptococcus, and Atopobium are the major groups of bacteria in the human gut, whereas facultative anaerobes such as Lactobacilli, Enterococci, Streptococci, and Enterobacteriaceae are present in numbers that are 1,000-fold lower (Davis and Milner, 2009). The gut microbiota changes swiftly in terms of variety and composition during the first year of birth and remains relatively constant upon adulthood. Nevertheless, the composition of the resident microbiota may be altered due to environmental factors, predominantly, by the influence of diet (Chassaing et al., 2017; Jahani-Sherafat et al., 2018; Yang and Yu, 2018). It is increasingly apparent that when dietary components change the gut microbial composition and its diversity, the balance between beneficial and detrimental gut microbiota could be disrupted, and the resulting impaired gut homeostasis can set the stage for cancer development (Davis and Milner, 2009; Yang and Yu, 2018; De Almeida et al., 2019). Indeed, many studies have revealed a consistent link between colorectal carcinogenesis and gut microbiota. Fusobacterium nucleatum (Kostic et al., 2013; Tahara et al., 2014; Fukugaiti et al., 2015; Viljoen et al., 2015; Li et al., 2016; Mima et al., 2016; Tunsjø et al., 2019), Streptococcus gallolyticus (Abdulamir et al., 2010; Butt et al., 2016; Corredoira et al., 2017; Kumar et al., 2017; Kwong et al., 2018), Clostridium difficile (Fukugaiti et al., 2015; Zheng et al., 2017), Clostridium septicum (Corredoira et al., 2017; Kwong et al., 2018), Enterococcus faecalis (Zhou et al., 2016; Rezasoltani et al., 2018; Geravand et al., 2019), Escherichia coli (Buc et al., 2013; Bonnet et al., 2014; Kohoutova et al., 2014; Dejea et al., 2018), Peptostreptococcus stomatis (Zeller et al., 2014; Yu et al., 2017), and Bacteroides fragilis (Boleij et al., 2015; Zhou et al., 2016; Purcell et al., 2017; Dejea et al., 2018; Kwong et al., 2018; Haghi et al., 2019) are differentially enriched in the fecal or colonic mucosa samples of CRC patients relative to healthy individuals, or in the CRC patient’s tumor tissue relative to adjacent healthy tissue, wherein in some cases, CRC disease status is associated with the abundance of CRC-associated gut microbiota. CRC risk is also associated with the seroprevalence of Helicobacter pylori antibodies (Zhang et al., 2012; Epplein et al., 2013; Teimoorian et al., 2018; Butt et al., 2019; ChangxiChen et al., 2019). Table 1 summarizes the common gut microbiota associated with CRC risk obtained from CRC patients’ and healthy subjects’ mucosa, blood, and stool. This is not an exhaustive summary.
Table 1.
Gut microbiota associated with colorectal cancer (CRC) risk.
| Bacteria | Sample type | Method of bacterial analysis | Association | References | ||
|---|---|---|---|---|---|---|
| Phylum | Genus | Species | ||||
| Fusobacteria | Fusobacterium | – | Rectal mucosa, colorectal tissue | qPCR | Significantly higher in CRA patients than in healthy controls, and in tumor tissue than in adjacent normal tissue | (McCoy et al., 2013) |
| Stool sample | 16S rRNA pyrosequencing | Significantly higher in CRC patients than in healthy controls | (Wu et al., 2013) | |||
| nucleatum | Colorectal tissue, stool sample | qPCR | Significantly higher in CRA and CRC patients than in healthy controls | (Kostic et al., 2013) | ||
| Stool sample | qPCR | Significantly higher in CRC patients than in healthy controls or patients with polyps | (Tunsjø et al., 2019) | |||
| Stool sample | qRT-PCR | Significantly higher in CRA patients than in healthy controls | (Fukugaiti et al., 2015) | |||
| Colonic mucosa | qPCR | Significantly higher in tumor tissue than in adjacent normal tissue | (Tahara et al., 2014; Viljoen et al., 2015) | |||
| Colorectal tissue | qPCR | Higher abundance was associated with significantly higher CRC-specific mortality | (Mima et al., 2016) | |||
| Colorectal tissue | FQ-PCR, FISH | Significantly higher in tumor tissue than in adjacent normal tissue; overabundance was significantly associated with lymph node metastasis | (Li et al., 2016) | |||
| Firmicutes | Streptococcus | gallolyticus | Blood | Blood culture test | Patients with history of S. gallolyticus bacteremia had significantly higher CRC risk than those without | (Kwong et al., 2018) |
| Blood | Multiplex serology | Antibody response to pilus protein Gallo2039, Gallo2178 and Gallo2179 was significantly associated with CRC risk | (Butt et al., 2016) | |||
| Blood | Blood culture test | 62.7% of 204 patients with S. gallolyticus bacteremia had concurrent CRN | (Corredoira et al., 2017) | |||
| Colorectal tissue, fecal sample | PCR, ISH | Significantly higher in CRC patients than in healthy controls | (Abdulamir et al., 2010) | |||
| Colorectal tissue | qPCR | Significantly higher in tumor than in adjacent normal tissue | (Kumar et al., 2017) | |||
| Clostridium | difficile | Fecal sample | qRT-PCR | Significantly higher in CRA patients than in healthy controls | (Fukugaiti et al., 2015) | |
| Fecal sample | Multiplex RT-PCR | Significantly higher in CRC patients with lymph node metastasis than those without | (Zheng et al., 2017) | |||
| septicum | Blood | Blood culture test | 45.2% of 42 patients with C. septicum bacteremia had concurrent CRN | (Corredoira et al., 2017) | ||
| Blood | Blood culture test | Patients with history of C. septicum bacteremia had significantly higher CRC risk than those without | (Kwong et al., 2018) | |||
| Enterococcus | faecalis | Stool sample | qRT-PCR | Significantly higher in CRC patients than in healthy controls or patients with polyps | (Geravand et al., 2019) | |
| Stool sample | qRT-PCR | Higher abundance significantly correlated with dysplasia grade | (Rezasoltani et al., 2018) | |||
| Colorectal tissue | qRT-PCR | Significantly higher in tumor tissue than in adjacent normal tissue | (Zhou et al., 2016) | |||
| Escherichia | coli | Colonic tissue | PCR | E. coli of phylogenetic group B2 was significantly higher in CRC patients than in diverticulosis patients | (Buc et al., 2013) | |
| Colorectal tissue | PCR | E. coli of phylogenetic group D was significantly higher in CRC patients than in healthy controls; E. coli of phylogenetic group B2 was significantly higher in patients with advanced CRA than in patients with non-advanced CRA | (Kohoutova et al., 2014) | |||
| Colonic tissue | PCR | Significantly higher in colon cancer tumors than in diverticulosis mucosa and adjacent normal tissue, and in colon cancer patients of stages III/IV than those of stage I | (Bonnet et al., 2014) | |||
| Colonic mucosa | FISH | Significantly higher pks+ E. coli in FAP patients than in healthy controls | (Dejea et al., 2018) | |||
| Peptostreptococcus | stomatis | Stool sample | 16S rRNA sequencing | Significantly higher in CRC patients than in healthy controls | (Zeller et al., 2014) | |
| Stool sample | qPCR | Significantly higher in CRC patients than in healthy controls | (Yu et al., 2017) | |||
| Helicobacter | pylori | Blood | ELISA | Significantly higher seroprevalence of H. pylori antibodies in CRC patients than in healthy controls | (Zhang et al., 2012) | |
| Blood | ELISA | Significantly higher seroprevalence of H. pylori antibodies in patients with CRC and adenomatous polyps than in healthy controls | (Teimoorian et al., 2018) | |||
| Blood | Multiplex serology | Seropositivity of antibodies against VacA was associated with over 2-fold increase in colon cancer risk | (Epplein et al., 2013) | |||
| Expelled air | Carbon-13 urea breath test | Significantly higher prevalence of H. pylori infection in CAP patients than in healthy controls | (ChangxiChen et al., 2019) | |||
| Blood | Multiplex serology | Seropositivity of antibodies against VacA was associated with 11% increase in CRC risk | (Butt et al., 2019) | |||
| Bacteroidetes | Bacteroides | – | Stool sample | 16S rRNA pyrosequencing | Prevalence positively correlated with CRC disease status (based on TNM classification) | (Wu et al., 2013) |
| fragilis | Stool sample | PCR | Significantly higher in CRC patients than in healthy controls | (Haghi et al., 2019) | ||
| Blood | Blood culture test | Patients with history of B. fragilis bacteremia had significantly higher CRC risk than those without | (Kwong et al., 2018) | |||
| Colorectal tissue | qRT-PCR | Significant higher in tumor tissue than in adjacent normal tissue | (Zhou et al., 2016) | |||
| Colonic mucosa | Touchdown PCR | Significantly higher expression of bft gene in stages III/IV CRC patients than in healthy controls | (Boleij et al., 2015) | |||
| Colonic mucosa | qPCR | Presence was significantly associated with low-grade dysplasia, tubular adenomas and serrated polyps | (Purcell et al., 2017) | |||
| Colonic mucosa | FISH | Significantly higher in FAP patients than in healthy controls | (Dejea et al., 2018) | |||
CRC, colorectal cancer; CRA, colorectal adenoma; CRN, colorectal neoplasm*; CAP, colorectal adenomatous polyps; FAP, familial adenomatous polyposis; PCR, polymerase chain reaction; qPCR, quantitative polymerase chain reaction; RT-PCR, real-time polymerase chain reaction; qRT-PCR, quantitative real-time polymerase chain reaction; FQ-PCR, fluorescent quantitative polymerase chain reaction; ELISA, enzyme-linked immunosorbent assay; ISH, in situ hybridization; FISH, fluorescent in situ hybridization; pks, polyketide synthase; VacA, vacuolating toxin A; bft, Bacteroides fragilis toxin.
*includes invasive carcinomas (malignant cells beyond the muscularis mucosa) and premalignant lesions (non-advanced and advanced adenoma).
In this article, an overview of the dietary components of various food classes that have been implicated in the pathogenesis of CRC, the mediating roles of gut microbiota and the different mechanisms involved in CRC initiation or progression are deliberated.
The Interactions Between Diet, Gut Microbiota, and Colorectal Cancer
Protein
Red Meat and Processed Meat
Epidemiological studies have linked excessive processed meat, and to a lesser extent red meat, consumption to increased risk of CRC (Cross et al., 2010; Oostindjer et al., 2014; Demeyer et al., 2016). Reports published by the Word Cancer Research Fund in 2007 and 2018 indicated a strong evidence that a consumption of red and processed meat can increase CRC risk (World Cancer Research Fund/American Institute for Cancer Research, 2018). Processed meat has been classified as group I carcinogen by the World Health Organization’s International Agency for Research on Cancer (2015), that is similar to the risk category of cigarettes and alcohol. Red meat was classified as Group 2A carcinogen, dictating its probable carcinogenicity (Bouvard et al., 2015). In a meta-analysis published in 2017, a 16 and 22% increment of CRC risk was reported for every 100 and 50g/day additional intake of red meat and processed meat, respectively (Zhao et al., 2017). Several mechanisms have been purported to expound the disease-promoting effect of red and processed meat.
N-Nitroso Compounds
N-Nitroso compounds (NOCs) consist of a nitroso group attached to a nitrogen atom and are formed by the reaction of a nitrite compound with amines or amides. NOCs comprise two major chemical classes, namely nitrosamines and nitrosamides. Humans are exposed to the highly mutagenic NOCs either by exogenous or endogenous means. The main source of exogenous NOCs includes meats that have been processed, smoked or cured (Bouvard et al., 2015). Alternatively, NOCs can be produced endogenously in the human gut from the intake of nitrite: amino acids are converted to amines via bacterial decarboxylation, followed by n-nitrosation in the presence of nitrite as nitrosating agent to generate NOCs (Parnaud et al., 2000; Fahrer and Kaina, 2013).
NOCs are multi-site carcinogens that can form DNA adducts—the outcome of covalent binding between reactive electrophilic species and the nucleophilic sites in DNA (Ewa and Danuta, 2017). Malignant transformation is initiated when N-nitrosamines form diazomethane by the activation of p450 isoenzymes (CYP2E1), resulting in the formation of O6-carboxymethyl guanine (O6-CMG) and O6-methylguanine (O6-MeG) DNA adducts, which, when unrepaired, could induce G:C→A:T transition mutation that is typically detected in the K-ras gene associated with human CRC (Fahrer and Kaina, 2013). Red meat was shown to be able to stimulate the production of O6-CMG (Lewin et al., 2006; Hemeryck et al., 2016) and O6-MeG (Le Leu et al., 2015). The formation of DNA adducts may account for the association between dietary NOC intake and rectal cancer (Loh et al., 2011; Zhu et al., 2014).
The Interaction Between N-Nitroso Compounds and Gut Microbiota
Studies have highlighted the involvement of gut microbiota in the production of NOCs (Engemann et al., 2013; Kobayashi, 2018; Yoon and Kim, 2018). Generally, the population of these NOC-producing bacteria is low in healthy individuals, but excessive dietary nitrate and nitrite intake will facilitate the growth of NOC-producing bacteria as nitrate or nitrite are used as electron acceptors during NOC production (Kobayashi, 2018). The resulting microbial dysbiosis can potentially participate in colon carcinogenesis, leading to an elevated CRC risk (Sobhani et al., 2013; Jahani-Sherafat et al., 2018; Zou et al., 2018). The presence of nitrate generated through bowel inflammatory responses was associated with an enrichment of E. coli in the large intestine of colitis mice (Winter et al., 2013). Several studies have associated a significantly higher prevalence of pathogenic strains of E. coli (usually belong to phylogenetic group B2 or D) with CRC (Buc et al., 2013; Bonnet et al., 2014; Kohoutova et al., 2014; Dejea et al., 2018). Nonetheless, it remains unclear whether the bloom of E. coli caused by nitrate or NOCs can contribute to the initiation of intestinal inflammation or colon carcinogenesis.
Heterocyclic Amines and Polycyclic Aromatic Hydrocarbons
When muscle meat is cooked at high temperature, its creatinine or creatine, amino acids, and sugars are converted into heterocyclic amines (HCAs) (Helmus et al., 2013). The common types of HCA in meats cooked at high temperature are 2-amino-1-methyl-6-phenylimidazo(4,5-b) pyridine (PhIP), 2-amino-3,8-dimethylimidazo(4,5-f) quinoxaline (MeIQx), 2-amino-3,4-dimethylimidazo(4,5-f)quinoline (MeIQ), 2-amino-3,4,8-dimethylimidazo(4,5-f) quinoxaline (DiMeIQx), and amino-3-methylimidazo(4,5-f) quinolone (IQ). PhIP, MeIQ, and MeIQx have been categorized by International Agency for Research on Cancer (IARC) as possible human carcinogens (group 2B) while IQ has been classified as probably carcinogenic to humans (group 2A) (Cascella et al., 2018). A colonoscopy-based study among Japanese reported a high MeIQ but not MeIQx and PhIP exposure to be positively associated with an increased risk of CRC in females (Budhathoki et al., 2015). However, PhIP intake but not MeIQx and DiMeIQx showed a significantly associated risk of colorectal adenoma (CRA) in an European population-based study (Rohrmann et al., 2009). Conversely, other studies have reported that a higher intake of any type of HCA (PhIP, MeIQx, and DiMeIQx) had significant associated risk for CRA (Barbir et al., 2012; Chiavarini et al., 2017). A study also reported a significant association between CRC risk and red-meat derived, but not white-meat derived HCAs and PAHs (Helmus et al., 2013). Although the definite contribution of each HCA type to colonic neoplasm remains tentative, the findings so far converge to imply that HCAs as a whole are associated with an increased CRC risk, as corroborated by mice studies (Cheung et al., 2011; Lee et al., 2013).
Incomplete combustion of organic materials from industrial processing and domestic cooking at high temperature produces polycyclic aromatic hydrocarbons (PAHs), which could contaminate food when they are in contact. Thus, meat cooked over an open flame is highly prone to PAH contamination (Zelinkova and Wenzl, 2015). Similar to HCA, PAH, primarily benzo(a)pyrene (B(a)P), could also increase the risk of CRA in humans (Sinha et al., 2005; Chiavarini et al., 2017). It has been shown experimentally that B(a)P could bind directly to DNA to form DNA adducts, as well as induce oxidative and nitrosative stress along with increased expression of pro-inflammatory cytokines and dysregulated wnt/β-catenin signaling in mice colon (Diggs et al., 2013; Ajayi et al., 2016). Moreover, there was a synergistic genotoxic effect of HCA and PAH with a five-fold increase in PhIP-derived DNA adducts when B(a)P and PhIP were used in combination compared to HCA alone (Jamin et al., 2013).
The Interaction Between Heterocyclic Amine and Polycyclic Aromatic Hydrocarbon and Gut Microbiota
Exposure to PhIP (Defois et al., 2018) and B(a)P (Defois et al., 2017) could shift the volatile pattern of human fecal microbiota, indicating a deviation in the microbial metabolic activities that may in the long run disrupt gut homeostasis. Of note, these studies exposed microbiota to doses of HCA and PAH that were higher than expected daily consumption for a very short time (24 h), making the results less reflective of the actual effect of chronic HCA and PAH exposure. In murine models, B(a)P also induced a shift in the abundance and composition of the gut microbiota, in addition to colonic inflammation (Khalil et al., 2010; Ribière et al., 2016). On the other hand, human colon microbiota could directly induce the bioactivations and transformations of PAH into estrogenic metabolites, influencing the toxicity of PAH (Van de Wiele et al., 2005). Human gut microbiota with beta-glucuronidase and glycerol/diol dehydratase activity could transform HCA to HCA-M1, mitigating HCA-associated carcinogenic risk (Zhang et al., 2019). Specifically, Eulonchus halli were able to convert PhIP to PhIP-M1, whose mutagenic potency is only 5% of that of PhIP (Fekry et al., 2016). Just as HCA and PAH can induce dysbiosis to exert detrimental effect in the human body (Khalil et al., 2010; Ribière et al., 2016; Defois et al., 2017; Defois et al., 2018), there are some gut microbiota that could reduce the detrimental effects of dietary HCA and PAH (Van de Wiele et al., 2005; Fekry et al., 2016; Zhang et al., 2019).
Trimethylamine-N-Oxide
Trimethylamine-N-oxide (TMAO) is a gut microbiota-dependent metabolite of saltwater fish, eggs, dairy products, and especially, red meat (Velasquez et al., 2016; Chan et al., 2019; Wang et al., 2019). In the human gut, TMAO precursors including dietary choline, phosphatidylcholine, betaine, and L-carnitine undergo gut microbial degradation to be converted into trimethylamine (TMA). TMA is absorbed and delivered to the liver via the portal circulation, and subsequently reacts with hepatic flavin monooxygenase, primarily FMO3, to produce TMAO (Velasquez et al., 2016; Subramaniam and Fletcher, 2018; Zou et al., 2018).
Elevated TMAO level is associated with a higher mortality risk of chronic kidney disease (Tang et al., 2015; Missailidis et al., 2016), major adverse cardiovascular events such as coronary artery disease (Senthong et al., 2016), myocardial infarction (Tang et al., 2013; Suzuki et al., 2020), heart failure (Tang et al., 2014; Troseid et al., 2015), and liver cancer (Liu et al., 2018b). Besides, an epigenetic interaction network analysis indicated the role of TMAO on colon carcinogenesis, as many genetic pathways implicated in colon carcinogenesis were shared by TMAO (Xu et al., 2015). From the Women’s Health Initiative (WHI) Observational Study, a higher plasma choline concentration was found to be associated with a greater risk of rectal cancer; women with low plasma vitamin B12 in particular, showed significant association between plasma TMAO level and CRC risk (Bae et al., 2014). A male matched case-control study has indicated that a higher serum concentration of choline was significantly associated with a three-fold increase CRC risk (Guertin et al., 2017). However, other studies have reported a null (de Vogel et al., 2011) and even an inverse (Nitter et al., 2014) association between plasma choline concentration and CRC risk.
TMAO has been found to promote inflammatory gene expression in both human aortic endothelial cells and smooth muscle cells via the activation of nuclear factor‐κB (NF‐κB) signaling (Seldin et al., 2016); its concentration was also positively identified to be associated with the concentration of tumor necrosis factor alpha (TNF-α) and its soluble receptors, both of which constitute a key regulator of inflammatory responses (Rohrmann et al., 2015). Additionally, TMAO could upregulate the expression of proinflammatory molecules such as IL-6, CXCL1, and CXCL2 in H. pylori infected-gastric epithelial cells, demonstrating the possible synergistic effect of TMAO and H. pylori in the development of gastritis or gastric ulcers (Wu et al., 2017). TMAO could also activate NLRP3 inflammasome and the production of reactive oxygen species (ROS) in fetal human colon cells by inhibiting ATG16L1-induced autophagy, a process that is vital for the regulation of inflammation (Yue et al., 2017). The roles of TMAO in inflammatory process implicated by these findings provide a plausible mechanism by which TMAO could contribute to colon carcinogenesis.
The Interaction Between Trimethylamine-N-Oxide and Gut Microbiota
The composition of intestinal microbiota influences the production of TMAO from its precursors (Chan et al., 2019). Following antibiotics treatment that suppressed intestinal microbiota, dietary supplementation of TMAO precursors failed to enhance TMAO synthesis in mice (Koeth et al., 2013) or healthy adults (Tang et al., 2013), implying the dependence of TMAO production on the metabolism of gut microbiota. Besides, serum TMAO level could be lowered by a natural compound known as berberine via altering the composition of gut microbiota, in particular Firmicutes and Verrucomicrobia, leading to an anti-atherosclerotic effect (Shi et al., 2018). When compared to a non-TMA producing bacterial species, TMA-producing species brought about a significantly higher serum TMAO in germ-free mice (Romano et al., 2015). In a study involving healthy young men, those with a higher Firmicutes to Bacteroidetes ratio demonstrated a greater response to dietary TMAO, implying the influence of gut microbiota composition on TMAO production (Cho et al., 2017). There are evidences implying the role of gut microbiota as a mediator of the association between diet, TMAO, and diseases, with alteration in the composition or structure of intestinal microbiota influencing TMAO production and hence, affecting the risk of colonic lesions (Koeth et al., 2013; Tang et al., 2013; Romano et al., 2015; Cho et al., 2017; Shi et al., 2018; Chan et al., 2019). Of note, although most of the intestinal microbiota promote TMAO production from its precursors, Eubacterium limosum was shown to be able to metabolize TMA precursors through carnitine demethylation to form a product that cannot be readily converted into TMA, revealing the potential of this gut bacterium in reducing TMAO level in the gut (Kountz et al., 2020).
Heme Iron
Red meat but not white meat, is associated with an elevated risk of CRC, and this has been linked to heme iron (Cross et al., 2010; Bastide et al., 2011; Oostindjer et al., 2014). Heme is enriched in hemoproteins including myoglobin, hemoglobin and cytochrome. Red meat in relation to white meat, has higher concentration of myoglobin, with a 10-fold higher heme content (Bastide et al., 2011). Heme-induced CRC risk is linked to two reactions catalyzed by heme, namely N-nitrosation and lipoperoxidation. The former is characterized by the decarboxylation of amino acids by nitrosating agents to form NOCs (Bastide et al., 2011). In comparison with diet containing a negligible amount of heme, heme-rich red meat and processed meat could significantly increase fecal NOCs level, confirming the contribution of heme to endogenous NOC production (Joosen et al., 2009). Processed meat generally contains a higher amount of NOCs than fresh meat as heme iron in processed meat products is nitrosylated (curing salt contains nitrite or nitrate), resulting in the formation of nitrosyl heme (Cammack et al., 1999). In a cohort study, both nitrosylated and non-nitrosylated heme iron were found to be associated with CRA risk, but a higher risk was associated with the former, implying its higher carcinogenicity. This provides a possible explanation for the stronger link between CRC risk and processed meat intake than fresh meat intake (Bastide et al., 2016). Additionally, consumption of a large amount of red meat also results in the formation of N-nitrosothiols, which together with nitrosyl heme, leads to the accumulation of carboxymethylated adducts (Steinberg, 2019). Indeed, the mutagenicity of NOCs has been attributed to the formation of DNA adducts such as O6-CMG and O6-MeG, which could potentially accelerate the malignant transformation in the colon (Lewin et al., 2006; Bugni et al., 2009; Le Leu et al., 2015).
Lipoperoxidation is characterized by the free-radicals attack of membrane lipids which gives rise to aldehydes such as malondialdehyde (MDA) and 4-hydroxynonenal (4-HNE) (Bastide et al., 2011). Heme-induced lipoperoxidation can result in an increased fecal thiobarbituric acid reactive substances (TBARs). Previously, an increased fecal TBARs level was observed in mice (Martin et al., 2015) and human subjects (Pierre et al., 2013) who were given heme-rich diets, thus, substantiating the role of heme in promoting lipoperoxidation. In a recent study, ex vivo trapping of aldehyde counteracted inflammation and DNA damage in murine colonic epithelial cells, attributing these heme-induced deleterious effects to lipoperoxidation (Martin et al., 2019b).
In addition to NOCs and aldehydes, hemin, a porphyrin with iron bound to chloride derived from a heme group, is also related to colon tumor growth (Kim et al., 2019a). Hemin could exert cytotoxic effect on colonic epithelial cells via the production of ROS such as hydrogen peroxide (Ishikawa et al., 2010; Gemelli et al., 2014). Hemin could also mimic the effect of freeze-dried ham in inducing aberrant crypt foci and mucin depleted foci in rodent models, both of which are the precancerous lesions of the colon (Pierre et al., 2010).
The Interaction Between Heme and Gut Microbiota
The consumption of heme-rich diet was shown to alter the composition of gut microbiota in mice, which was exemplified by a reduction of Firmicutes and Deferribacteres, in addition to an increase of Proteobacteria or Bacteroidetes (IJssennagger et al., 2012; Constante et al., 2017; Martin et al., 2019b). The dysbiosis could reduce the colonic level of butyrate, a short chain fatty acid important for the digestive health, leading to adenoma formation (Constante et al., 2017). Interestingly, the dysbiosis could be ameliorated by the supplementation of calcium to heme-rich diet (Martin et al., 2019b). Other study has demonstrated the ability of gut microbiota to modulate the lipoperoxidation associated with heme-induced colon carcinogenesis (Martin et al., 2015). An antibiotic treatment was able to prevent epithelium damages and hyperproliferation in mice fed with heme-rich diet compared to antibiotics absence, substantiating the involvement of gut microbiota in enhancing heme-induced hyperproliferation and deteriorating the colonic mucus barrier (Ijssennagger et al., 2015).
Other Protein Sources
Fish consumption has no association (Engeset et al., 2007; Lee et al., 2009; Sugawara et al., 2009; Pham et al., 2013) or an inverse association (Wu et al., 2012; Aglago et al., 2019) with CRC risk. The association between egg intake and CRC risk is inconsistent, with some studies reporting a positive association (Aune et al., 2009; Lee et al., 2009) while others reported a null association (Franceschi et al., 1997; Järvinen et al., 2001). On the other hand, dairy products are associated with a decreased colon cancer risk (Huncharek et al., 2008; Aune et al., 2012), particularly cheese and milk (Lee et al., 2009; Aune et al., 2012; Murphy et al., 2013; Barnung et al., 2019).
Several studies have indicated the CRC-promoting effects in red and processed meat but not in other protein sources which also contain the CRC-inducing components found in red and processed meats. The other protein sources such as fish, eggs, and dairy products also contain the precursors of TMAO, choline, phosphatidylcholine, and L-carnitine (Velasquez et al., 2016; Subramaniam and Fletcher, 2018), while baked or grilled fish contain HCA and PAH (Alisson-Silva et al., 2016). The lack of a link between CRC and the consumption of protein sources other than meat may be explained by various health-promoting dietary components. For instance, studies have attributed the protective effect of fish due to its omega-3 polyunsaturated fatty acids (n-3 PUFAs) (Pietrzyk, 2017; Aglago et al., 2019). n-3 PUFAs are known to exhibit an anti-inflammatory effect through the mediation of the expression of inflammatory genes, or by modulating intracellular signaling pathways that regulate T-cell activation, leading to a decreased risk of colon carcinogenesis (Chapkin et al., 2007; Wall et al., 2010). Calcium from dairy products is found to inhibit tumorigenesis in human colon cancer cells and CRC mouse models (Wang et al., 2011; Ju et al., 2012). The CRC-protective effect of calcium has been linked to its ability to reduce lipid peroxidation induced by heme (Hemeryck et al., 2016; Martin et al., 2019b), and to restore the upregulation of inflammatory genes induced by Western diet in the human colons (Protiva et al., 2016). Importantly, only calcium from dairy products, but not the non-dairy products, was associated with a decreased CRC risk (Murphy et al., 2013).
Although it is unclear whether certain health-promoting dietary components could counteract the harmful effects of CRC-associated dietary components, it is evident that colon carcinogenesis is not attributed to a single nutrient but a combination of them, such that the dietary impact of a particular food chemical may be influenced by the absence or presence of another (Pietrzyk, 2017). This may explain why protein sources containing the same carcinogens exhibit opposite effects in CRC.
Carbohydrates
Carbohydrates are macronutrients categorized as simple or complex carbohydrates based on their degree of polymerization (Ludwig et al., 2018). Simple carbohydrates such as monosaccharides, disaccharides, and oligosaccharides are found in sugar-sweetened food and beverage or refined plant-based food, whereas complex carbohydrates including polysaccharides such as dietary fibers and resistant starches are enriched in unrefined plant-based food (Hansen and Sams, 2018; Ludwig et al., 2018). Carbohydrate polymer length influences not only its digestion and absorption into the human body, but also the subsequent impacts on body functions (Ludwig et al., 2018). Thus, simple and complex carbohydrates will be discussed separately in terms of their contributions to CRC.
Complex Carbohydrates
The contribution of dietary fibers in reducing CRC risk has been well established in case-control studies (Dahm et al., 2010b; Luo et al., 2015), meta-analysis (Ben et al., 2014; Gianfredi et al., 2018) and European Prospective Investigation into Cancer and Nutrition (EPIC) studies (Murphy et al., 2012; Bradbury et al., 2014). The protective effect of dietary fibers is attributed to short chain fatty acids (SCFA) such as acetate, propionate, and butyrate, which are formed following the fermentation of fibers by gut microbiota along the colon tract (Wu et al., 2018). Among the different types of SCFA, butyrate has been most extensively studied for its protective efficacy against CRC. Its inhibitory effect against human colon cancer cell proliferation was shown superior compared with acetate and propionate (Zeng et al., 2020).
Butyrate exerts its anti-proliferative effect in CRC cells via several mechanisms. Firstly, butyrate decreases the expression of neuropilin-1, a receptor of vascular endothelial growth factor (VEGF) that is commonly upregulated in colon cancer cells. As VEGF is a key regulator of angiogenesis, the downregulation of neuropillin-1 exerts an inhibitory effect on the expansion of colon cancer cells (Yu et al., 2010; Yu et al., 2011). Second, butyrate induces apoptosis and suppresses the proliferation and invasion of CRC cells by regulating the expression of microRNA such as miR-92a (Hu et al., 2015) and miR-203 (Han et al., 2016). Thirdly, butyrate reduces motility of CRC cells by inhibiting the Akt/ERK signaling pathway (Li et al., 2017), revealing the potential of butyrate as part of the therapeutic strategy for blocking metastatic CRC. The protective effect of butyrate was substantiated in another study that reported a significant downregulation of free fatty acid receptor 2 (FFAR2), a butyrate receptor, in human colon cancer tissues than in healthy tissues, while mice deficient in FFAR2 also developed significantly more colon polyps than wild-type mice (Sivaprakasam et al., 2016).
Interestingly, butyrate stimulates cell growth in normal colonocytes but exerts an anti-proliferative effect in cancerous colonocytes. Such discrepancy in function was termed the “butyrate paradox.” The “Butyrate paradox” is explained by the “Warburg effect” which describes the differential metabolism of butyrate in cancerous and non-cancerous cells: non-cancerous cells mainly undergo oxidative metabolism, using butyrate as a primary energy source, whereas cancerous cells favor glycolysis as a means of metabolism, resulting in an inefficient metabolism of butyrate (Donohoe et al., 2012). In cancerous colonocytes, butyrate also downregulates its own oxidation by reducing the expression of short chain acyl-CoA dehydrogenase (SCAD), an enzyme that is responsible for butyrate oxidation (Han et al., 2018). Accordingly, butyrate could accumulate and function as a histone deacetylase inhibitor to stall the proliferation of cancer cells (Donohoe et al., 2012). A corroborative study has shown that butyrate suppressed the proliferation of the underlying colonic stem cells by inhibiting histone deacetylase only in damaged colonocytes but not in normal colonocytes (Kaiko et al., 2016). Hence, although butyrate serves as a primary source of energy for the proliferation of normal colon cells, it inhibits the growth of cancerous colonocytes, which highlights the tremendous advantages of dietary fiber intake.
The Interaction Between Complex Carbohydrates and Gut Microbiota
Studies have provided evidence that dietary carbohydrates are able to modify gut microbiota and hence, could modulate the physiological conditions in the colonic environment. For instance, children from rural African villages whose diet consists of mostly fibers showed a significant enrichment in Bacteroidetes compared with Italian children. Within the Bacteroidetes phylum, several cellulose-degrading bacteria from the genus Prevotella were found to be completely lacking in European children (De Filippo et al., 2010). A dominance of Prevotella, along with depletion of Bacteroides was also found in the gut microbiota of Bangladeshi children compared with children from the United States (Lin et al., 2013), as well as in native Africans compared with African Americans (Ou et al., 2013). Indeed, diet serves as a driving force for shaping the intestinal microbiome, where long-term adherence to fiber-rich food leads to the abundance of Prevotella, whereas adherence to Western diet low in fiber results in abundance of Bacteroides (Wu et al., 2011; De Filippis et al., 2016; Gorvitovskaia et al., 2016). Bacteroides species, in particular Bacteroides fragilis, were found to be prevalent in the colonic mucosa of CRC patients (Boleij et al., 2015; Haghi et al., 2019). Their ability to induce DNA damage via ROS production in colonic epithelial cells (Goodwin et al., 2011) and colitis along with colon tumors in mice (Wu et al., 2009) has also been documented, indicating the possible role of Bacteroides species in promoting colonic neoplasm in individuals with low fiber intake.
On the other hand, although Prevotella is frequently linked to high fiber diet, strains such as Prevotella copri and Prevotella intestinalis have been linked to HIV-associated (Dillon et al., 2016) or intestinal inflammatory conditions (Scher et al., 2013; Iljazovic et al., 2020). Given Prevotella constitutes a large genus with great species diversity, more studies are warranted to clarify its beneficial or detrimental roles in the human body, including the mechanisms underlying its interaction with dietary components to clarify its role in the pathogenesis of CRC (Ley, 2016; Larsen, 2017). Other studies have reported the association of dietary fiber with a lower risk for F. nucleatum-positive CRC but not for F. nucleatum-negative CRC, suggesting the role of F. nucleatum as a mediator of the association between dietary fibers and colorectal neoplasms (Mehta et al., 2017; Liu et al., 2018a). Whether or not this hypothesis can be generalized to Bacteroides or Prevotella remains to be explored.
As discussed above, the protective effect of dietary fibers could be largely attributed to butyrate production. Of note, the fermentation of dietary fibers to produce butyrate is largely mediated by gut microbiota including Faecalibacterium prausnitzii, Eubacterium rectale, Roseburia faecis, E. halli, and others (Baxter et al., 2019). Thus, it is relevant to propose that the gut microbiome could influence the dietary impact of butyrate. A smaller population of butyrate-producing bacteria such as Roseburia, Clostridium, and Eubacterium was observed in advanced CRA patients along with a lower production of butyrate, highlighting the importance of gut microbiota in modulating the production of butyrate to protect hosts from colonic neoplasm (Chen et al., 2013). Conversely, butyrate could change the composition of gut microbiota to attenuate the detrimental effect of high-fat diet, resulting in an improve intestinal barrier and attenuated obesity or steatohepatitis (Zhou et al., 2017; Fang et al., 2019). Similarly, sodium butyrate supplementation was shown to beneficially restore the dysbiosis in CRC liver metastasis mouse model, resulting in a better host immune system characterized by an increase in natural killer T cells and T helper 17 cells (Ma et al., 2020). Hence, the interaction between butyrate and gut microbiota appears to be bidirectional. More investigations would need to be conducted to define the mechanistic link between dietary butyrate, gut microbiota, and CRC.
Simple Carbohydrate
A conclusive link between high sugar intake and CRC risk in healthy humans has not been reported by cohort studies (Galeone et al., 2012; Tasevska et al., 2012; Pacheco et al., 2019), but a moderately heightened risk did emerge in smaller case-control studies (Pou et al., 2012; Wang et al., 2014; Chun et al., 2015). Nonetheless, the detrimental effect of simple carbohydrates on CRC is more evident in animal studies. Sucrose supplementation aggravated colonic inflammation in colitic rats by inducing DNA changes in the colon mucosal cells (Mahmoud, 2011). Ingestion of high-fructose corn syrup could enhance colon tumorigenesis via the action of ketohexokinase, a fructose-converting enzyme that changes the tumor cell metabolism to increase the production of fatty acids needed for tumor growth. Importantly, the enhanced tumor growth was observed in the absence of obesity, supporting the detrimental role of simple sugars in the etiology of CRC independently from their effect on obesity (Goncalves et al., 2019). This finding points to the consequences of consumption of simple sugars, especially of high-fructose corn syrup that is widely used as a sweetener in carbonated drinks, condiments, and baked foods (Payne et al., 2012).
Simple carbohydrates, especially monosaccharides, are easily hydrolyzed and absorbed in the small intestine, resulting in a rapid rise in blood glucose level. Although a consistent link between total sugar intake and CRC risk has not been established, a number of studies did find a positive association between glycemic index (GI) and glycemic load (GL) with CRC risk (Gnagnarella et al., 2008; Sieri et al., 2015). The GI measures the elevation in blood sugar level following consumption of a particular food independent of quantity, while GL takes into account of both GI and the quantity of available carbohydrates in a portion of food consumed (Vega-López et al., 2018). Interestingly, GI has been significantly linked to CRC risk more frequently than GL (George et al., 2009; Choi et al., 2012; Turati et al., 2015). Two studies reported that high carbohydrate intake from high GI food was significantly associated with increased CRC risk, but high carbohydrate intake from low GI food was significantly associated with decreased CRC risk, indicating the greater dependence of CRC risk on the ability of carbohydrate-rich food to post-prandially raise blood glucose level rather than the overall amount of carbohydrates consumed (Sieri et al., 2015; Sieri et al., 2017). In fact, hyperglycemia (high blood sugar level) and hyperinsulinemia (high insulin level) resulting from high GI-diet could contribute to the initiation or progression of CRC through the induction of DNA damage in colon cells (Othman et al., 2013; Othman et al., 2014), or the action of insulin-like growth factor (Aleksandrova et al., 2013) which has a known role in the pathogenesis and progression of CRC (Vigneri et al., 2015; Kasprzak and Adamek, 2019). Other etiological hypotheses for the CRC-promoting effect of high GI/GL diet include insulin resistance, oxidative stress and abnormal sex hormone production (Sieri et al., 2017; Li et al., 2019), but these mechanisms have not been extensively studied.
The Interaction Between Simple Carbohydrates and Gut Microbiota
The association between simple carbohydrate consumption and microbiota-mediated CRC risk remains poorly documented. Martinez-Medina et al. (2014) reported an increased colonization of adherent-invasive E. coli and mucin-degrading bacterium Ruminococcus torques in the gut of mice fed with high-fat, high-sugar Western diet. The change in microbiota composition subjected the mice to an increased susceptibility to inflammation, as reflected by the decreased mucus thickness and an increased release of pro-inflammatory cytokines (Martinez-Medina et al., 2014). Of note, the study examined the combined effect of a high-fat and a high-sugar diet, hence it cannot be concluded whether the microbial dysbiosis was induced by fat or sugar exposure. Nevertheless, it has been postulated that a prolonged exposure to fructose and sugar substitutes through a Western diet can subject gut microbiota to extensive conditioning, leading to the formation of “Western gut microbiome” characterized by low microbial genetic and phylogenic diversity (Payne et al., 2012; Segata, 2015). Supporting this hypothesis, studies have shown that individuals living in non-urban settings harbor a gut microbiome of greater diversity and complexity, relative to individuals from urban-industrialized settings (Obregon-Tito et al., 2015; Rampelli et al., 2015). The loss or depletion of certain gut microbiota may in the long run lead to microbial dysbiosis or aberrant host-microbe interactions, and ultimately, disorders (Payne et al., 2012).
Fat
Epidemiological studies examining the link between dietary fat intake and CRC risk are sparse and to date, have not drawn a definitive conclusion regarding the CRC-promoting effect of dietary fats. While total dietary fat intake is infrequently linked to CRC risk (Dahm et al., 2010a; Williams et al., 2010; Kim and Park, 2018), an elevated CRC risk has been detected among individuals with a high saturated fat intake (Chun et al., 2015; Tayyem et al., 2015; Kim et al., 2017b). In contrast, consumption of n-3 polyunsaturated fat (n-3 PUFA) has been inversely associated with CRC (Zhong et al., 2013; Kim and Kim, 2020). A more consistent link between fat intake and colon carcinogenesis has been inferred from mice studies, that showed an associated increased risk due to an altered expression of inflammatory mediators (Padidar et al., 2012; Day et al., 2013).
Investigations of the dietary fat-associated CRC risk often cite bile acids as being responsible for increasing CRC risk. Human primary bile acids, namely cholic acid (CA) and chenodeoxycholic acid (CDCA), are synthesized in the liver from cholesterol. Conjugated with glycine and taurine, the primary bile acids are secreted into the hepatobiliary system and enter the duodenum to emulsify dietary fats after a meal. Subsequently, the majority of the primary bile acids will be deconjugated and reabsorbed, but a small amount can escape and enter the colon, where they are biotransformed by colonic bacteria via 7α-dehydroxylation to form secondary bile acids such as deoxycholic acid (DCA) and lithocholic acid (LCA). Most human gut microbiota that participate in the 7α-dehydroxylation belong to the genus Clostridium (Ocvirk and O’Keefe, 2017; Zou et al., 2018).
Given bile acids are cholesterol derivatives, their synthesis is likely to be promoted by a high-fat diet that is also rich in cholesterol. A high-fat diet will upregulate bile discharge for the emulsification of excessive dietary fats, which further raises the bile acid level (Ajouz et al., 2014). A study reported an increased fecal bile acid concentration in mice fed with high-fat, low-fiber Western diet, which was observed along with a defective bile acid transport and an increased colon tumor number (Dermadi et al., 2017). Accumulation of fecal bile acid was also observed in DCA-treated mice, along with a significantly increased intestinal inflammation (Xu et al., 2020). Extending to human studies, African Americans who consumed a high-fat diet were shown to have a 3–4 times higher level of secondary bile acids than native Africans who subsisted on a low-fat diet, providing a possible explanation for the much higher CRC risk among African Americans (Ou et al., 2012). In the follow-up study that involved switching African Americans to a high-fiber, low-fat diet for 2 weeks, the dietary change led to a suppressed secondary bile acid synthesis and showed a remarkable decrease in colonic mucosal inflammation and proliferation biomarkers of cancer risk (O’Keefe et al., 2015).
Although the exact mechanism of how bile acids induce the pre-cancerous state of colonocytes is unclear, it has been hypothesized that bile acids as cholesterol derivatives with detergent-like properties, could damage the intestinal epithelium when they are present at high concentration. Such destruction will trigger inflammation and a compensatory hyperproliferation of undifferentiated cells, which drives their transition into a precancerous state (Nguyen et al., 2018). Moreover, DCA and LCA could induce cancer stem cell growth in the colonic epithelium via the modulation of M3R and Wnt/β-catenin signaling. Given cancer stem cells are notorious for their ability to initiate and sustain tumor growth or proliferation, this finding provides a probable mechanism on how bile acids promote CRC (Farhana et al., 2016). Interestingly, it has been hypothesized that bile acid could exert a dichotomous effect on the apoptosis of colonocytes (Nguyen et al., 2018): a short-term exposure to high concentration of bile acid was able to induce apoptosis, primarily via the production of ROS (Ignacio Barrasa et al., 2011), whereas a prolonged exposure gave rise to colon carcinogenesis (Bernstein et al., 2011), which can be attributed to the inhibited accumulation of tumor suppressor p53 (Qiao et al., 2001), or the activation of PI3K/Akt signaling (Raufman et al., 2008). The effect of bile acids on CRC development was shown to be mediated by the farnesoid X receptor (FXR), a primary bile acid nuclear receptor. One study reported that inactivation of FXR could increase cancer risk by inducing bile acid dysregulation (Dermadi et al., 2017). Conversely, in another study, the ability of DCA to compromise colonic epithelial restitution appeared to be mediated by the activation of FXR, and such effect was linked to colonic barrier dysfunction and intestinal inflammation, both of which could increase susceptibility to CRC (Mroz et al., 2018). Although the role of FXR remains incompletely defined, these studies pinpoint the importance of FXR in mediating bile acid-associated CRC risk.
Although DCA and LCA are notorious for their tumorigenic effect especially in the course of CRC development, it is vital to note that not all bile acids could cause adverse effects. Ursodeoxycholic acid (UDCA), a secondary bile acid used as the first-line therapy for primary biliary cirrhosis, is found to have profound chemopreventive effect against colorectal carcinogenesis (Serfaty et al., 2010). The antiproliferative action of UDCA in colon cancer cells has been well documented and attributed to its ability to regulate the production of ROS (Kim et al., 2017a), to suppress the pro-proliferative c-Myc proteins (Peiro-Jordan et al., 2012), or to sustain the hyperphosphorylation of ERK1 kinase (Krishna-Subramanian et al., 2012). UDCA could also reverse DCA-induced effect on colonic epithelial cells by inhibiting DCA-induced secretion of epithelial defensins (Lajczak et al., 2017). Evidently, while other secondary bile acids drive CRC progression, UDCA emerges as a potential chemopreventive agent for CRC. Their differential actions on CRC-related inflammatory signals or growth factors are likely to account for such contrasting effect (Serfaty et al., 2010).
The Interaction Between Dietary Fat and Gut Microbiota
Several studies have associated the prolonged intake of high-fat diet with a shift in the relative proportion of Firmicutes to Bacteroidetes (F/B ratio), where Firmicutes dominate at the expense of Bacteroidetes in most cases (Murphy et al., 2010; Islam et al., 2011; Taira et al., 2015). Given the shift in the F/B ratio has been repeatedly linked to obese individuals (Ferrer et al., 2013; Kasai et al., 2015; Koliada et al., 2017), it could be contended that the dysbiosis is more likely to be associated with the host obese state rather than the high-fat diet itself. However, it was found that even in the absence of an obese genotype, mice fed with high-fat diet demonstrated profound changes in microbial communities characterized by increase in Firmicutes and decrease in Bacteroidetes (Hildebrandt et al., 2009). A high-fat diet could also promote tumorigenesis in the murine small intestine independently of obesity by inducing a dysbiosis that was associated with an attenuated antimicrobial host defense (Schulz et al., 2014). These findings collectively show that microbial dysbiosis is inducible by high-fat diet alone, and such dysbiosis could promote colon carcinogenesis independently of obesity.
Moreover, a high-fat diet could increase the proportion of the phylum Actinobacteria with an accompanying increase in the expression of proinflammatory cytokines and a decrease in tight junction proteins (Kim et al., 2019b). Given Actinobacteria are known mucin-degrading bacteria (Tailford et al., 2015), an increase in abundance could induce gut barrier impairment and subsequent colonic inflammation, which may help explain the CRC-promoting effect of dietary fat in the colon. In mice, a high-fat diet also diminished the beneficial gut microbiota including Bifidobacterium, Lactobacillus, and Akkermansia (Kim et al., 2012; Lecomte et al., 2015; He et al., 2018), all of which play significant roles in mediating the intestinal metabolism and immunity (Naito et al., 2018). The high-fat diet-induced reduction of these beneficial gut microbiota could possibly increase the susceptibility to inflammation, facilitating subsequent neoplastic progression.
As conversion of bile acids into secondary bile acids involves the action of gut microbiota, changes in the composition of gut microbiota can potentially influence the metabolic effect of bile acids in the host. A dysbiosis characterized by a decrease in the ratio between Faecalibacterium prausntizii and E. coli was associated with an impaired bile acid metabolism in patients with inflammatory bowel diseases (IBD), as reflected by their higher level of fecal bile acids (Duboc et al., 2013). In a recent metagenomics analysis, a lower abundance of genes of bile-metabolizing Firmicutes was detected in the gut microbiota of IBD individuals, again linking microbial dysbiosis with the disease state (Das et al., 2019). Of note, the interaction between bile acids and gut microbiota is bidirectional as bile acids serve as antimicrobial agents that help shape the gut microbiome structure (Ridlon et al., 2016). Administration of cholic acid into rats could expand Firmicutes to approximately 95% of the total gut microbiome in relation to 54% in control rats (Islam et al., 2011). DCA treatment could induce a dysbiosis characterized by an increase in opportunistic pathogens and a decrease in Lactobacillus, Lactococcus, and Roseburia, which was linked to intestinal tumorigenesis (Cao et al., 2017). Indeed, while gut microbiota can affect the metabolism of bile acid, bile acid can shape the composition of gut microbiota.
Recently, Bilophila wadsworthia, a sulfur-metabolizing microbe that convert dietary sulfur into genotoxic hydrogen sulfide (H2S) have been associated with the development of CRC (David et al., 2014; Ijssennagger et al., 2016; Nguyen et al., 2020). Excessive gut-derived H2S could break down the disulfide bonds of the mucus bilayer of the gastrointestinal tract and expose gut epithelium to immunogenic luminal bacteria (Ijssennagger et al., 2016). Moreover, it could cause epithelial DNA damage, promote alterations in immune cell populations associated with inflammation and CRC. David et al. (2014) reported that participants fed with a high-meat, high-fat diet for several days showed an increase in Bilophila, which coincided with an increased abundance of microbial DNA and RNA encoding for H2S-producing enzymes (David et al., 2014). In a large cohort of patients with precancerous polyps and CRC, Yachida et al. (2019) found that DCA concentration was significantly increased in subjects with multiple polypoid (MP, more than three adenomas) adenomas with low grade dysplasia as compared to healthy controls; and Bilophila wadsworthia was the only species that was significantly associated with DCA increase in this MP group (Yachida et al., 2019). Nguyen et al. (2020) reported that long-term adherence to a dietary pattern associated with sulfur-metabolizing bacteria in stool was associated with an increased risk of distal CRC in men but how this bacteria contribute to CRC pathogenesis remains unclear (Nguyen et al., 2020).
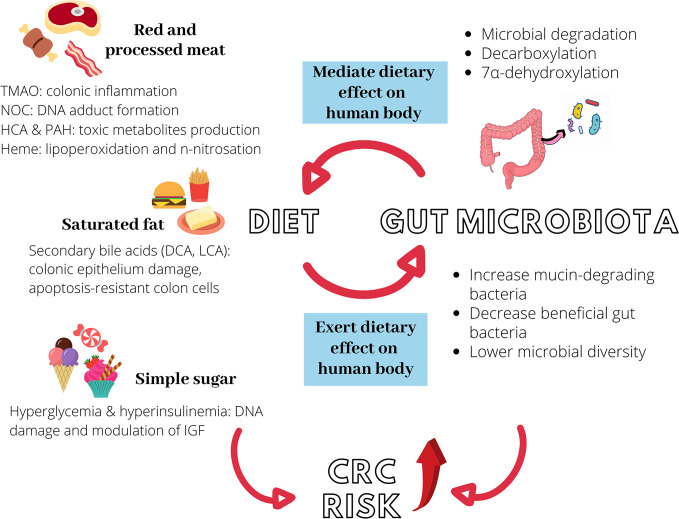
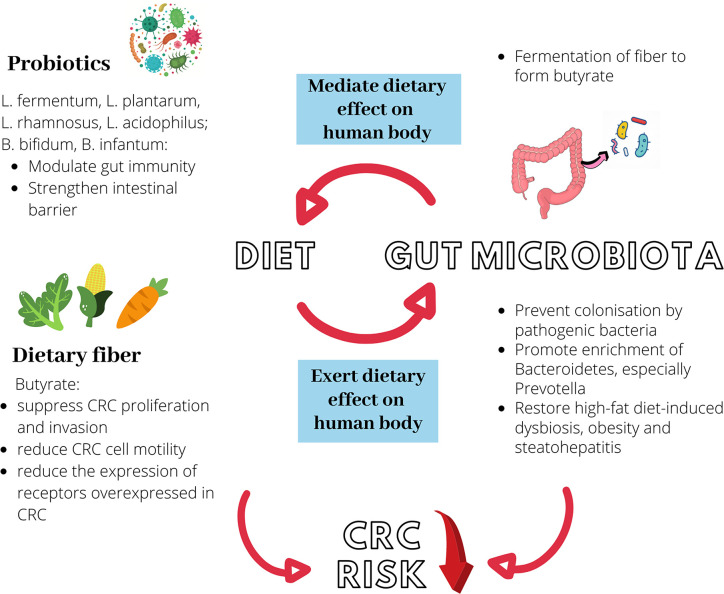
Figure 1 illustrates the interactions between diet, gut microbiota, and increased risk of CRC risk. Table 2 recapitulates the interactions between dietary compounds and gut microbiota that purportedly influence CRC risk.
Figure 1.
Diet, gut microbiota, and increased colorectal cancer (CRC) risk. Red and processed meat, saturated fat, and simple sugar could independently promote colon carcinogenesis via different mechanisms. Similarly, they can induce microbial dysbiosis in the intestine, further elevating CRC risk. Gut microbiota modulates the metabolism of ingested food via different processes to produce carcinogenic metabolites such as NOC, TMAO, and secondary bile acids. The interaction between diet and gut microbiota is hence bidirectional. TMAO, trimethylamine-N-oxide; NOC, N-nitroso compounds, HCA, heterocyclic amines; PAH, polycyclic aromatic hydrocarbons; DCA, deoxycholic acid; LCA, lithocholic acid; IGF, insulin-like growth factor.
Table 2.
Interactions between dietary compounds and gut microbiota that purportedly influence colorectal cancer (CRC) risk.
| Food type | Compounds involved | Action of dietary compounds on gut microbiota | References | Action of gut microbiota on dietary compounds | References |
|---|---|---|---|---|---|
| Red and processed meat | N-nitroso compounds (NOCs) | Promote the growth of NOC-producing bacteria, leading to disease- causing dysbiosis | (Kobayashi, 2018) | – | – |
| Heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs) | Alter the abundance, composition, or metabolic activities of gut microbiota, accompanied by colonic inflammation | (Khalil et al., 2010; Ribière et al., 2016; Defois et al., 2017; Defois et al., 2018) | Bioactivate and transform HCAs and PAHs into compounds with lower toxicity | (Van de Wiele et al., 2005; Fekry et al., 2016; Zhang et al., 2019) | |
| Trimethylamine-N-oxide (TMAO) | – | – | Involved in TMAO synthesis; microbial composition could define body response toward TMAO intake | (Koeth et al., 2013; Tang et al., 2013; Romano et al., 2015; Cho et al., 2017) | |
| Heme | Promote the enrichment of Proteobacteria and Bacteroidetes; reduce Firmicutes and Deferribacteres; promote adenoma formation; decrease fecal butyrate level | (IJssennagger et al., 2012; Constante et al., 2017; Martin et al., 2019b) | Increase heme-induced lipoperoxidation, hyperproliferation and exacerbation of colonic mucus barrier | (Ijssennagger et al., 2015; Martin et al., 2015) | |
| Dietary fibers | Butyrate | Promote the enrichment of Bacteroidetes, especially Prevotella; restore high-fat diet-induced dysbiosis, resulting in an improved host immune response and intestinal barrier as well as attenuated obesity and steatohepatitis | (De Filippo et al., 2010; Lin et al., 2013; Ou et al., 2013; Zhou et al., 2017; Fang et al., 2019; Ma et al., 2020) | Mediate the fermentation of dietary fiber to form butyrate | (Chen et al., 2013; Baxter et al., 2019) |
| Simple sugar | – | Promote the enrichment of pathogenic and mucin degrading bacteria; form “Western gut microbiome” characterized by low genetic and phylogenic diversity | (Payne et al., 2012; Martinez-Medina et al., 2014; Segata, 2015) | – | – |
| Fats | Bile acids | Increase the Firmicutes to Bacteroidetes ratio, which was linked to obesity; promote the enrichment of mucin-degrading Actinobacteria; decrease beneficial gut microbiota such as Bifidobacterium, Lactobacillus, and Akkermansia | (Murphy et al., 2010; Islam et al., 2011; Kim et al., 2012; Lecomte et al., 2015; Taira et al., 2015; Cao et al., 2017; He et al., 2018) | Mediate the conversion of bile acids into secondary bile acids; dysbiosis is associated with impaired bile acid metabolism and inflammatory bowel diseases | (Duboc et al., 2013; Zou et al., 2018; Das et al., 2019) |
The Underlying Molecular Mechanisms of Colon Carcinogenesis Mediated by Gut Microbiota
Inflammation and Host Defense Mechanism
The connection between inflammation and malignant diseases has been well-established based on evidence from epidemiological, genetic, or pharmacological studies. In the case of colon malignancies, IBDs especially ulcerative colitis and Crohn’s disease exhibit consistent association with an elevated risk of CRC (Choi et al., 2019; Zhou et al., 2019; Olén et al., 2020). IBD-associated CRC is characterized by early onset (Keller et al., 2019), increased formation of synchronous, and poorly differentiated tumors (Reynolds et al., 2017) as well as elevated mortality rate (Sebastian et al., 2014), in relation to sporadic CRC.
Importantly, recent studies have indicated the role of gut microbiota in mediating inflammatory responses during the course of colon carcinogenesis, most of which are through the activation of nuclear factor-κB (NF-κB) signaling pathway. NF-κB are a family of transcription factors that actively regulate genes of various immune and inflammatory responses, and strong evidence has indicated its involvement in the pathogenesis of IBD and IBD-associated cancers (Liu et al., 2017). In a mice study, colon tumors with a higher abundance of Fusobacterium nucleatum had a higher nuclear translocation of the p65 NF-κB subunit, representing an increase in the activation of NF-κB pathway (Kostic et al., 2013). Importantly, the tumorigenic property of F. nucleatum was indicated as its administration into ApcMin/+ mice and human CRC cell lines accelerated the colonic tumorigenesis, which was attributed to the activation of NF-κB that in turn induced miR21 expression (Yang et al., 2017). Analysis of colonic epithelial tissue of CRC patients showed a higher expression of NF-κB in the S. gallolyticus-seropositive group compared to the S. gallolyticus-seronegative group (Abdulamir et al., 2009). In the follow-up study, the colorectal tissue of S. gallolyticus-seropositive CRC patients had a higher expression of IL-1 and COX-2, both of which constitute the products of NF-κB activity (Abdulamir et al., 2010). Likewise, infection of human macrophages with CRC-associated E. coli strains promoted a sustained COX-2 expression (Raisch et al., 2015). These studies together underscore the role of gut microbiota together with the involvement of NF-κB during the course of colon carcinogenesis.
The infection of colonocytes by certain gut microbiota can activate a wealth of immune cells that together mediate the colonic inflammatory responses. Enterotoxigenic B. fragilis for instance, could induce distal colon tumorigenesis by recruiting polymorphonuclear immature myeloid cells following NF-κB activation (Chung et al., 2018). Peptostreptococcus anaerobius interacts with colonic cells via α2/β1 integrin, a receptor that is commonly overexpressed in CRC to promote a pro-inflammatory state, characterized by an expansion of tumor-associated macrophages, myeloid-derived suppressor cells, and granulocytic tumor-associated neutrophils (Long et al., 2019). Macrophages of Enterococcus faecalis-colonized mice could produce pro-inflammatory cytokine TNF-α, which in turn increased the colon epithelial cell production of netrin-1, a neuronal guidance molecule capable of inhibiting apoptosis to accelerate malignant transformation (Yang et al., 2012).
Obesity is known to produce a chronic, low-grade state of inflammation. Some of the mediator for inflammation are cytokines and inflammation-related molecules (Hursting et al., 2012). A study reported that increased body mass index (BMI) was associated with increase in two proinflammatory colonic cytokines, namely TNF-α and interleukin 6 (IL6), while obesity coincided with precancerous changes in the transcriptome (Pfalzer et al., 2018). Considering the existing correlation between obesity and gut microbiota changes (Boulangé et al., 2016), finding from Pfalzer et al. (2018) implies that inflammation may be one of the mechanisms of how obesity-associated dysbiosis contributes to increased CRC risk.
Although the above describe mainly the detrimental effects of microbiome, Parabacteroides distasonis, a commensal organism, has been shown to exert an anti-inflammatory effect. When fed to BALB/C mice, P. distasonis could reduce the severity of intestinal inflammation of acute and chronic colitis (Kverka et al., 2011). Likewise, Koh et al. (2020) has reported the beneficial role of P. distasonis in attenuating colonic tumorigenesis and maintaining intestinal epithelial barrier in azoxymethane (AOM)-treated mice (Koh et al., 2020).
Bacterial Toxin
CRC-associated gut microbiota also exerts tumorigenic effect through the production of genotoxin, which induces DNA or chromosomal damage to facilitate malignant transformation. Interestingly, the production of genotoxin is not restricted to only the typically pathogenic bacteria but also commensal bacteria. E. coli constitutes a normal component of the gut microbiome, but certain strains that acquire pathogen-like features can produce cyclomodulin genotoxin including colibactin, cytotoxic necrotizing factor (CNF), and cytolethal distending toxin (CDT) (Kurnick et al., 2019), all of which have been examined for their promoting effect in CRC. The pathogenicity island encoding colibactin, known as polyketide synthase (pks), are detected in up to 66.7% of CRC patients (Arthur et al., 2012). Moreover, experimental studies show that colibactin could sustain tumor growth by generating DNA cross links in cellulo, which were later transformed into DNA double-strand breaks (Bossuet-Greif et al., 2018; Kawanishi et al., 2019; Wilson et al., 2019), or by favoring the emergence of senescent cells (Cougnoux et al., 2014; Dalmasso et al., 2014). Senescent cells are cells with an irreversible cell cycle arrest. Although early-stage senescence usually protects cells against malignant transformation, a long-term senescence stage changes cellular microenvironment leading to cancer development (Zeng et al., 2018). In the case of CRC, colibactin-induced cellular senescence could lead to the continuous secretion of growth factors that promote tumor growth (Cougnoux et al., 2014; Dalmasso et al., 2014). On the other hand, CNF-encoding gene was found significantly more prevalent in the resection specimens of CRC patients than diverticulosis patients, suggesting the specific role of CNF in promoting colon cancer (Buc et al., 2013). Like colibactin, CNF could induce cellular senescence in human colon cells. Of note, such senescence was reversible, where the polyploid cells re-entered cell cycle, depolyploidised and eventually produced more aneuploid progeny. Given aneuploidy is the hallmark of solid tumor development, the reversible senescence induced by CNF is relevant to colon tumorigenesis (Zhang et al., 2018b). Likewise, CDT that are produced by pathogenic E. coli could drive colon carcinogenesis in genetically altered premalignant human colon epithelial cells (Graillot et al., 2016). Another gram-negative bacterium, Salmonella enterica, also produces CDT, which has been classified as typhoid toxin due to being a unique virulence factor of S. enterica subspecies enterica serotype Typhi (Miller and Wiedmann, 2016). Typhoid toxin of S. enterica was found to synergize with the loss of the adenomatous polyposis coli (APC) gene to promote microenvironment conducive for malignant transformation, purportedly through the inhibition of DNA repair and DNA damage‐induced cell cycle arrest (Martin et al., 2019a).
Besides E. coli, other types of CRC-associated gut microbiota also produce CRC-promoting cytotoxins. The gene encoding B. fragilis toxin was detected in the colonic mucosa of both the early-stages and late-stages CRC patients, with a 100% prevalence in the latter (Boleij et al., 2015). Studies investigating the tumorigenicity of B. fragilis toxin reported its capability to disrupt or cleave E-cadherin, leading to barrier permeability dysfunction, activation of Wnt/βcatenin and NF-κB signaling pathways as well as expression of IL-8 and IL-17, which altogether form a carcinogenic inflammatory cascade (Wu et al., 2007; Hwang et al., 2013; Chung et al., 2018). B. fragilis toxin could also upregulate spermine oxidase, a polyamine catabolic enzyme and subsequently led to the generation of ROS and DNA damage (Goodwin et al., 2011). Although the overall H. pylori seroprevalence was not associated with CRC risk, seropositivity to a specific H. pylori protein called VacA significantly increased the odds of developing CRC (Epplein et al., 2013; Butt et al., 2019). It was posited that VacA cytotoxin may contribute to CRC by disrupting the ionic equilibrium in enterocytes, primarily through the modulation of chloride concentration in the cellular microenvironment (Ponzetto and Figura, 2019). This mechanism, however, remains as a postulation; the effect of H. pylori on CRC is far from clear as previous studies only assessed the antibody responses against VacA in serum samples but did not confirm the presence of H. pylori or its associated protein in colorectal tissue samples (Epplein et al., 2013; Butt et al., 2019).
Bacterial Adherence Factor
Throughout their phylogenetic evolution, bacteria gradually attained virulence factors such as adhesins, pili, and flagella to develop their ability to breach the gut mucosal barrier, as well as to adhere to and to invade intestinal epithelial cells (Gagnière et al., 2016). Studies have elucidated the mechanism to which F. nucleatum utilizes its adhesins to bind to and invade host cells: Fusobacterium adhesin A (FadA) binds and shifts away the vascular endothelial cadherin at the endothelial cell-cell junctions to enable the passage of F. nucleatum through the loosened junctions of endothelium (Fardini et al., 2011), whereas fibroblast activation protein 2 (Fap2) binds to the D-galactose-β (1-3)-N-acetyl-D-galactosamine (Gal-GalNAc) carbohydrate moiety, which is overexpressed in CRC host, to promote F. nucleatum enrichment (Abed et al., 2016). Of note, experimental evidence has indicated that the interaction between bacterial adhesins and their receptors on host cells does not only facilitate bacterial attachment, but also its subsequent pathogenic activities via the modulation of different mechanisms. FadA could bind and interact with E-cadherin to induce β-catenin signaling, pro-inflammatory cytokines, and CRC tumor growth in xenograft mice (Rubinstein et al., 2013). A higher expression of FadA was detected in patients with CRC and precancerous adenomas in comparison with non-CRC individuals, further corroborated the facilitative role of FadA in F. nucleatum-associated colon carcinogenesis (Rubinstein et al., 2013; Kashani et al., 2020). Similarly, the binding of Fap2 to the human inhibitory receptor T-cell immunoreceptor with Ig and tyrosine based inhibitory motif domains (TIGIT) potentially sustain tumor growth by reducing natural killer cell cytotoxicity and tumor infiltrating lymphocyte cell activities (Gur et al., 2015).
E. coli, another CRC-associated gut microbe, also has its adherence and disease-promoting effect mediated by its afimbrial adhesin (afa). Diffusely-adhering E. coli expressing afa demonstrates the potential as a pathobiont that promotes IBD or intestinal cancer progression due to its ability to induce intestinal lesions, pro-inflammatory responses, and angiogenesis (Servin, 2014). A study has shown afa-possessing E. coli confer better adherence and invasion of intestinal epithelial cells than the afa-negative clones. Moreover, afa had the ability to upregulate the expression of VEGF, which could be linked to angiogenesis and tumor development (Prorok-Hamon et al., 2014). The prevalence of afa-possessing E. coli was also found to be higher in CRC as compared to healthy patients, indicating the potential role of afa in mediating the pathogenesis of E. coli (Prorok-Hamon et al., 2014; Eklof et al., 2017).
The role of pil3 pilus is essential to the attachment of S. gallolyticus to human mucus-producing cells or to the colonization of murine colon (Martins et al., 2015). Interestingly, pil3 bound equally well to the human mucins MUC2 which predominates in healthy colon, and to MUC5AC which is overexpressed only in cancerous colon. It was posited that the ability of S. gallolyticus to bind MUC2 mucin via pil3 facilitates commensal colonization, while binding to MUC5AC confers a growth advantage over other colon microbiota species in the tumor microenvironment. This helps explain the higher carriage rate of S. gallolyticus in the presence of colon tumors (Martins et al., 2016).
Oxidative Stress and DNA Repair Defects
As discussed above, dysbiotic microbiota provokes chronic gut inflammation via different mechanisms. These chronic inflammatory cells may stimulate the release of endogenous ROS and nitrogen species (RONs), which are responsible for the accumulation of different types of DNA damage including single and double strand DNA breaks, DNA crosslinks, thymine glycol, and abasic sites (Ray and Kidane, 2016). One of the gut microbiotas that is capable of triggering such detrimental inflammatory cascade is E. faecalis. E. faecalis could produce ROS such as extracellular superoxide, which induced tumor-associated chromosomal instability, anaphase bridging, and multipolar mitosis in human colonic epithelial cells (Wang and Huycke, 2007; Wang et al., 2008). P. anaerobius interacts with toll-like receptor (TLR) 2 and 4 on colon cells to stimulate an increased ROS level, rate of cholesterol biosynthesis, and colon cell proliferation (Tsoi et al., 2017). Of note, the effect of ROS in carcinogenesis is dichotomous; while it contributes to tumor growth and survival, it induces the apoptosis of cancer cells when present at excessively high level (Lin et al., 2018). There is increasing evidence that ROS involvement in various pathways can lead to the natural resolution of inflammation (Chelombitko, 2018). Hence, the microbiota-induced tumorigenic effect observed in the aforementioned studies could be interpreted as a consequence of oxidative stress, which occurs with prolonged ROS overproduction that could not be compensated by antioxidant systems, rather than the direct tumor promoting effect of ROS itself.
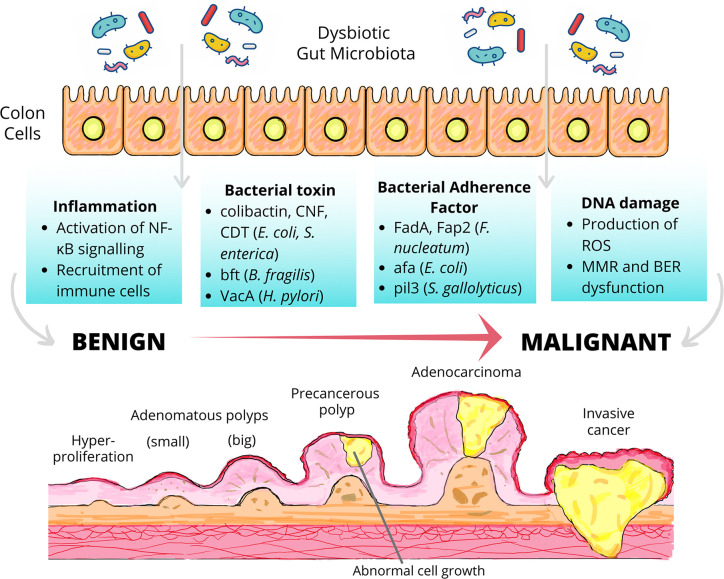
The DNA damage caused by ROS could be repaired by several DNA repair mechanisms including the DNA mismatch repair system (MMR) and base excision repair system (BER), both of which are highly conserved from bacteria to humans (Bridge et al., 2014). The disruption of either of these antioxidant mechanisms by dysbiotic microbiota has been shown to promote carcinogenesis by the accumulation of oxidative stress, which is responsible for the severe cellular and tissue damage as well as chronic inflammation (Chelombitko, 2018). Studies have uncovered the detrimental effect of enteropathogenic E. coli (EPEC), which has been shown to significantly reduce the expression of two key MMR proteins, namely MSH2 and MLH1 via a post-translation mechanism involving the EPEC effector protein EspF. The MMR dysfunction could also induce microsatellite instability, a phenomenon characterized by the accumulation of DNA replication errors particularly in the area of short repetitive DNA stretches (Maddocks et al., 2009; Maddocks et al., 2013). Considering the fact that microsatellite instability is detected in up to 20% of CRC (Nojadeh et al., 2018), investigations into how other gut microbiota cause MMR dysfunction become a matter of great clinical importance. Besides, it has been proposed that dysbiotic microbiota may promote the accumulation of carcinogenic BER intermediates, primarily AP sites, leading to genomic instability and colon carcinogenesis (Ray and Kidane, 2016). Moreover, the polymorphism of BER genes could modulate CRC risk, presumably, by influencing the BER processes (Brevik et al., 2010; Kabzinski et al., 2016). Nonetheless, whether or not specific gut microbiota could interfere with BER, causing its loss of biological function and subsequently influence risk of colon carcinogenesis is yet to be explored. Figure 2 summarizes the mechanisms to which dysbiosis may set the stage for colon carcinogenesis.
Figure 2.
Dysbiosis and colon carcinogenesis. Dysbiotic gut microbiota may drive the malignant transformation of colon cells via the induction of inflammation, the secretion of bacterial toxin, the action of bacterial adherence factors and the induction of DNA damage. The transformation of early neoplastic lesions (adenomatous polyps) to colorectal cancer (CRC) may take up to 15 years depending on the characteristics of the lesions and other risk factors including body weight, gender, physical inactivity, etc. (De Palma et al., 2019). NF-κB, nuclear factor-κB; CNF, cytotoxic necrotizing factor; CDT, cytolethal distending toxin; bft, Bacteroides fragilis toxin; VacA, vacuolating toxin A; FadA, Fusobacterium adhesin A; Fap2, fibroblast activation protein 2; afa, afimbrial adhesin; pil3, pilus 3; ROS, reactive oxygen species; MMR, mismatch repair system, BER, base excision repair system.
Possible Preventive and Therapeutic Strategy for Colorectal Cancer: the Probiotics
Probiotics are typically defined as living microorganisms, which when administered in adequate amounts, confer health benefits to the host. The potential contribution of probiotics to the preventative or therapeutic strategies for CRC is attributed to its ability to first, inhibit colonization by pathogenic bacteria; second, to modulate the gut immunity; and third, to strengthen the gut barrier (Fong et al., 2020). The inhibitory effect of probiotics against pathogenic bacteria has been demonstrated by several studies. The consumption of Bacillus bacteria was shown to inhibit intestinal colonization by Staphylococcus aureus via the interference of its quorum sensing signaling (Piewngam et al., 2018). Clostridium butyricum exhibited inhibitive effect against biofilm formation by enterotoxigenic B. fragilis, via the regulation of several B. fragilis virulence and efflux pump-related genes (Shi et al., 2020). Specific Lactobacillus strains, namely Lactobacillus fermentum 88 and Lactobacillus plantarum 9, demonstrated high adhesion values to the human enteric cell line HT29 while inhibiting the adhesion of E. coli to HT29 (Gharbi et al., 2019). Pre-treatment with Lactobacillus rhamnosus GG prior to the experimental induction of periodontitis in mouse model also exerted protective effect against F. nucleatum and Porphyromonas gingivalis-induced caecum dysbiosis, as well as significantly reduced intestinal inflammation (Gatej et al., 2020).
As mentioned, probiotics play an immunomodulatory role in the gut and can reduce colonic inflammation. Through the suppression of Wnt/β‑catenin signaling, Lactobacillus species was shown to ameliorate colonic inflammation and tumor growth in azoxymethane (AOM) and dextran sulfate sodium (DSS)-induced CRC murine model (Ghanavati et al., 2020). Treatment with a specific strain of L. rhamnosus decreased tumor incidence by inhibiting inflammation and promoting apoptosis (Gamallat et al., 2016). In APCMin/+ mouse model of colon cancer, L. plantarum strain YYC-3 prevented colon tumor development, putatively by suppressing the production of inflammatory cytokines and infiltration of inflammatory cells (Yue et al., 2020). Administration of a mixture of Lactobacillus acidophilus, L. rhamnosus and Bifidobacterium bifidum decreased colitis and resulted in a 40% lower number of tumors than the control group (Mendes et al., 2018).
It is known that a dysregulation of tight junction proteins including occludin, claudins, junctional adhesion molecules, and zona occludens (ZO) can lead to a leaky epithelial barrier, setting the stage for intestinal inflammation and IBD-associated CRC (Landy et al., 2016). The ability of probiotics to enhance gut barrier integrity can hence play a preventive role. A study previously reported that the probiotic E. coli Nissle 1917 could enhance intestinal barrier function via the upregulation and redistribution of the tight junction proteins ZO-1, ZO-2, and claudin-14 (Alvarez et al., 2016). A probiotic mixture comprising Bifidobacterium, L. acidophilus, and Enterococcus attenuated colitis in mice by upregulating the expression levels of occludin and claudin-4 (Zhang et al., 2018a). In 1,2-dimethylhydrazine dihydrochloride (DMH)-induced CRC mouse model, administration of L. acidophilus, B. bifidum, and Bifidobacterium infantum enhanced TLR2 signaling and gut mucosa epithelial barrier integrity, both of which correlated with decreased tumor incidence (Kuugbee et al., 2016). Figure 3 illustrates the interactions between diet, gut microbiota, and decreased risk of CRC.
Figure 3.
Diet, gut microbiota, and decreased colorectal cancer (CRC) risk. The fermentation of dietary fiber by gut microbiota results in the production of butyrate. Butyrate exerts inhibitory effect against colon carcinogenesis through several mechanisms, including the restoration of gut dysbiosis induced by high-fat diet. Probiotics such as Lactobacillus and Bifidobacterium prevents gut colonization by pathogenic bacteria, modulates gut immunity, and maintains gut barrier integrity.
Conclusion And FUture Directions
This report has examined recent scientific findings that highlighted the active participation of gut microbiota in the pathogenesis of CRC via different types of mechanisms. The purported mechanisms, however, do not indicate whether the state of the gut microbiota is a cause or a consequence of colon carcinogenesis. CRC-associated microbiota have long been grouped into driver species comprising pro-carcinogenic gut bacteria that initiate CRC development, or passenger species comprising opportunistic pathogens that outcompete the driver species in the tumor microenvironment (Tjalsma et al., 2012). In that sense, driver species can be regarded as the initiator of colon carcinogenesis while the passenger species is the consequence which further aggravates tumor progression after gaining colonization advantage in the established tumor microenvironment. Several recent studies however, redefine the roles of CRC-associated microbiota differently from what was originally proposed: E. coli, initially thought to be a driver species, may be a passenger species capable of replacing other gut microbiota through the action of colibactin (Wassenaar, 2018); S. gallolyticus, initially thought to be a passenger species, may be a driver species capable of inducing colon carcinogenesis on its own (Pasquereau-Kotula et al., 2018). Indeed, the existing scientific evidence is insufficient to provide a definitive answer for the cause-or-effect debate revolving around the role of gut microbiota in CRC. With more robust studies that could decipher the mechanisms underlying the pathogenicity of CRC-associated gut microbiota, the causative role of particular gut microbiota may one day be established, analogous to how H. pylori has been proven to be a strong risk factor for the development of gastric cancer (Wroblewski et al., 2010). Investigations into the exact effect of microbial dysbiosis on CRC development is a subject of tremendous clinical importance as gut microbiota is postulated to contribute to CRC progression and maintenance, as well as to define patients’ prognosis (Mima et al., 2016; Wei et al., 2016; Chen et al., 2019) and response to anti-cancer therapies (Pouncey et al., 2018; Lin et al., 2019; Villéger et al., 2019).
Evidence from epidemiological, animal, and human cell line studies also strongly support the influence of dietary factors on CRC risk. The findings so far converge to indicate that CRC risk could be reduced by an increased intake of dietary fiber while an elevated CRC risk is associated with the excessive intake of red and processed meat, saturated fats and to a smaller extent, simple sugar. These dietary components exert their detrimental effect by altering the composition and diversity of the gut microbial community to increase dysbiosis-associated CRC risk. On the other hand, dietary impact on the human body is itself mediated by the gut microbiota activity, which means dysbiosis triggered by any factor can add to CRC risk by shifting the effect of dietary components toward promoting colonic neoplasm. In either direction of this two-way interaction, dietary components mediate the risk of malignant transformation in the colon by interacting with gut microbiota. Of note, the evidence of dietary impacts on gut microbiota obtained from animal studies must be interpreted with caution as the gut microbiota of in-bred animal may not reflect the real-life gut microbiota of humans, which is shaped by many factors other than diet (Nguyen et al., 2015). Additionally, many human studies linking dietary habits, gut microbiota and CRC risk are cross-sectional. There is a pressing need to establish more well-designed longitudinal studies that assess the gut microbiota composition, dietary habits and gastrointestinal health status across different life stages, in order to determine the causal effects of dysbiosis and dietary compounds on CRC development and progression. It would also be of interest to determine if a stool-based screening of microbial dysbiosis can be utilized as a non-invasive and affordable CRC screening tool, which is eminently useful in resource-poor regions where colonoscopy is not readily available. Certainly, a standardized protocol with higher specificity and sensitivity must be developed before such screening tool can be implemented.
Probiotics have long been posited as a prophylactic and even therapeutic measure in colon carcinogenesis. While probiotics have demonstrated great health benefits, it should be noted that probiotics use is accompanied by risk; host response toward gut microbiome intervention varies from individual to individual, with likelihood of adverse effect among individuals with impaired gut barrier and compromised immunity (Doron and Snydman, 2015). More studies are warranted to confirm the risk and benefits associated with probiotics use in individuals with underlying medical conditions, to ensure that only probiotics with definitive protective effects against CRC are integrated into the clinical management of CRC. A personalized microbiome therapy taking into account the host genetics, physiology, and immunity will contribute to a higher success rate of such intervention.
Author Contributions
YL and MC designed the study and wrote the manuscript. YN, WL, and SP reviewed and revised the manuscript. MC and WL acquired the funding. All authors contributed to the article and approved the submitted version.
Funding
This article is funded by the matched fund of Sunway Medical Centre and Sunway University: GRTEX-OTR-CBP-SMC-001-2019.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Abdulamir A. S., Hafidh R. R., Mahdi L. K., Al-jeboori T., Abubaker F. (2009). Investigation into the controversial association of Streptococcus gallolyticus with colorectal cancer and adenoma. BMC Cancer. 9, 403. 10.1186/1471-2407-9-403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdulamir A. S., Hafidh R. R., Bakar F. A. (2010). Molecular detection, quantification, and isolation of Streptococcus gallolyticus bacteria colonizing colorectal tumors: Inflammation-driven potential of carcinogenesis via IL-1, COX-2, and IL-8. Mol. Cancer. 9, 249–249. 10.1186/1476-4598-9-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abed J., Emgård J. E. M., Zamir G., Faroja M., Almogy G., Grenov A., et al. (2016). Fap2 mediates Fusobacterium nucleatum colorectal adenocarcinoma enrichment by binding to tumor-expressed Gal-GalNAc. Cell Host Microbe 20 (2), 215–225. 10.1016/j.chom.2016.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aglago E. K., Huybrechts I., Murphy N., Casagrande C., Nicolas G., Pischon T., et al. (2019). Consumption of fish and long-chain n-3 polyunsaturated fatty acids is associated with reduced risk of colorectal cancer in a large European cohort. Clin. Gastroenterol. Hepatol. 18 (3), 654–666.e6. 10.1016/j.cgh.2019.06.031 [DOI] [PubMed] [Google Scholar]
- Ajayi B. O., Adedara I. A., Farombi E. O. (2016). Benzo(a)pyrene induces oxidative stress, pro-inflammatory cytokines, expression of nuclear factor-kappa B and deregulation of wnt/beta-catenin signaling in colons of BALB/c mice. Food Chem. Toxicol. 95, 42–51. 10.1016/j.fct.2016.06.019 [DOI] [PubMed] [Google Scholar]
- Ajouz H., Mukherji D., Shamseddine A. (2014). Secondary bile acids: An underrecognized cause of colon cancer. World J. Surg. Oncol. 12 (1), 164. 10.1186/1477-7819-12-164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandrova K., Nimptsch K., Pischon T. (2013). Influence of obesity and related metabolic alterations on colorectal cancer risk. Curr. Nutr. Rep. 2 (1), 1–9. 10.1007/s13668-012-0036-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alisson-Silva F., Kawanishi K., Varki A. (2016). Human risk of diseases associated with red meat intake: Analysis of current theories and proposed role for metabolic incorporation of a non-human sialic acid. Mol. Aspects Med. 51, 16–30. 10.1016/j.mam.2016.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez C.-S., Badia J., Bosch M., Giménez R., Baldomà L. (2016). Outer membrane vesicles and soluble factors released by probiotic Escherichia coli Nissle 1917 and commensal ECOR63 enhance barrier function by regulating expression of tight junction proteins in intestinal epithelial cells. Front. Microbiol. 7, 1981. 10.3389/fmicb.2016.01981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araghi M., Soerjomataram I., Bardot A., Ferlay J., Cabasag C. J., Morrison D. S., et al. (2019). Changes in colorectal cancer incidence in seven high-income countries: A population-based study. Lancet Gastroenterol. Hepatol. 4 (7), 511–518. 10.1016/S2468-1253(19)30147-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthur J. C., Perez-Chanona E., Mühlbauer M., Tomkovich S., Uronis J. M., Fan T.-J., et al. (2012). Intestinal inflammation targets cancer-inducing activity of the microbiota. Sci. (New York N.Y.) 338 (6103), 120–123. 10.1126/science.1224820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aune D., De Stefani E., Ronco A. L., Boffetta P., Deneo-Pellegrini H., Acosta G., et al. (2009). Egg consumption and the risk of cancer: A multisite case-control study in Uruguay. Asian Pac. J. Cancer Prev. 10 (5), 869–876. [PubMed] [Google Scholar]
- Aune D., Lau R., Chan D. S. M., Vieira R., Greenwood D. C., Kampman E., et al. (2012). Dairy products and colorectal cancer risk: A systematic review and meta-analysis of cohort studies. Ann. Oncol. 23 (1), 37–45. 10.1093/annonc/mdr269 [DOI] [PubMed] [Google Scholar]
- Bae S., Ulrich C. M., Neuhouser M. L., Malysheva O., Bailey L. B., Xiao L., et al. (2014). Plasma choline metabolites and colorectal cancer risk in the Women’s Health Initiative Observational Study. Cancer Res. 74 (24), 7442–7452. 10.1158/0008-5472.CAN-14-1835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbir A., Linseisen J., Hermann S., Kaaks R., Teucher B., Eichholzer M., et al. (2012). Effects of phenotypes in heterocyclic aromatic amine (HCA) metabolism–related genes on the association of HCA intake with the risk of colorectal adenomas. Cancer Causes Control. 23 (9), 1429–1442. 10.1007/s10552-012-0017-8 [DOI] [PubMed] [Google Scholar]
- Barnung R. B., Jareid M., Lukic M., Oyeyemi S. O., Rudolfsen J. H., Sovershaeva E., et al. (2019). High lactose whey cheese consumption and risk of colorectal cancer - The Norwegian Women and Cancer Study. Sci. Rep. 9 (1), 296. 10.1038/s41598-018-36445-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastide N. M., Pierre F. H. F., Corpet D. E. (2011). Heme iron from meat and risk of colorectal cancer: A meta-analysis and a review of the mechanisms involved. Cancer Prev. Res. (Phila) 4 (2), 177–184. 10.1158/1940-6207.CAPR-10-0113 [DOI] [PubMed] [Google Scholar]
- Bastide N., Morois S., Cadeau C., Kangas S., Serafini M., Gusto G., et al. (2016). Heme iron intake, dietary antioxidant capacity, and risk of colorectal adenomas in a large cohort study of French women. Cancer Epidemiol. Biomarkers Prev. 25 (4), 640–647. 10.1158/1055-9965.EPI-15-0724 [DOI] [PubMed] [Google Scholar]
- Baxter N. T., Schmidt A. W., Venkataraman A., Kim K. S., Waldron C., Schmidt T. M. (2019). Dynamics of human gut microbiota and short-chain fatty acids in response to dietary interventions with three fermentable fibers. mBio 10 (1), e02566–e02518. 10.1128/mBio.02566-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Q., Sun Y., Chai R., Qian A., Xu B., Yuan Y. (2014). Dietary fiber intake reduces risk for colorectal adenoma: A meta-analysis. Gastroenterology 146 (3), 689–699.e686. 10.1053/j.gastro.2013.11.003 [DOI] [PubMed] [Google Scholar]
- Bernstein C., Holubec H., Bhattacharyya A. K., Nguyen H., Payne C. M., Zaitlin B., et al. (2011). Carcinogenicity of deoxycholate, a secondary bile acid. Arch. Toxicol. 85 (8), 863–871. 10.1007/s00204-011-0648-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boleij A., Hechenbleikner E. M., Goodwin A. C., Badani R., Stein E. M., Lazarev M. G., et al. (2015). The Bacteroides fragilis toxin gene is prevalent in the colon mucosa of colorectal cancer patients. Clin. Infect. Dis. 60 (2), 208–215. 10.1093/cid/ciu787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnet M., Buc E., Sauvanet P., Darcha C., Dubois D., Pereira B., et al. (2014). Colonization of the human gut by E. coli and colorectal cancer risk. Clin. Cancer Res. 20 (4), 859–867. 10.1158/1078-0432.CCR-13-1343 [DOI] [PubMed] [Google Scholar]
- Bossuet-Greif N., Vignard J., Taieb F., Mirey G., Dubois D., Petit C., et al. (2018). The colibactin genotoxin generates DNA interstrand cross-links in infected cells. mBio 9 (2), e02393–e02317. 10.1128/mBio.02393-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulangé C. L., Neves A. L., Chilloux J., Nicholson J. K., Dumas M.-E. (2016). Impact of the gut microbiota on inflammation, obesity, and metabolic disease. Genome Med. 8 (1), 42–42. 10.1186/s13073-016-0303-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouvard V., Loomis D., Guyton K. Z., Grosse Y., Ghissassi F. E., Benbrahim-Tallaa L., et al. (2015). Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 16 (16), 1599–1600. 10.1016/s1470-2045(15)00444-1 [DOI] [PubMed] [Google Scholar]
- Bradbury K. E., Appleby P. N., Key T. J. (2014). Fruit, vegetable, and fiber intake in relation to cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Am. J. Clin. Nutr. 100 (suppl_1), 394S–398S. 10.3945/ajcn.113.071357 [DOI] [PubMed] [Google Scholar]
- Bray F., Ferlay J., Soerjomataram I., Siegel R. L., Torre L. A., Jemal A. (2018). Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68 (6), 394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- Brevik A., Joshi A. D., Corral R., Onland-Moret N. C., Siegmund K. D., Le Marchand L., et al. (2010). Polymorphisms in base excision repair genes as colorectal cancer risk factors and modifiers of the effect of diets high in red meat. Cancer Epidemiol. Biomarkers Prev. 19 (12), 3167–3173. 10.1158/1055-9965.Epi-10-0606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge G., Rashid S., Martin S. A. (2014). DNA mismatch repair and oxidative DNA damage: Implications for cancer biology and treatment. Cancers (Basel) 6 (3), 1597–1614. 10.3390/cancers6031597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buc E., Dubois D., Sauvanet P., Raisch J., Delmas J., Darfeuille-Michaud A., et al. (2013). High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PloS One 8 (2), e56964. 10.1371/journal.pone.0056964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budhathoki S., Iwasaki M., Yamaji T., Sasazuki S., Takachi R., Sakamoto H., et al. (2015). Dietary heterocyclic amine intake, NAT2 genetic polymorphism, and colorectal adenoma risk: the colorectal adenoma study in Tokyo. Cancer Epidemiol. Biomarkers Prev. 24 (3), 613–620. 10.1158/1055-9965.EPI-14-1051 [DOI] [PubMed] [Google Scholar]
- Bugni J. M., Meira L. B., Samson L. D. (2009). Alkylation-induced colon tumorigenesis in mice deficient in the Mgmt and Msh6 proteins. Oncogene 28 (5), 734–741. 10.1038/onc.2008.426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt J., Romero-Hernández B., Pérez-Gómez B., Willhauck-Fleckenstein M., Holzinger D., Martin V., et al. (2016). Association of Streptococcus gallolyticus subspecies gallolyticus with colorectal cancer: Serological evidence. Int. J. Cancer. 138 (7), 1670–1679. 10.1002/ijc.29914 [DOI] [PubMed] [Google Scholar]
- Butt J., Varga M. G., Blot W. J., Teras L., Visvanathan K., Le Marchand L., et al. (2019). Serologic response to Helicobacter pylori proteins associated with risk of colorectal cancer among diverse populations in the United States. Gastroenterology 156 (1), 175–186.e172. 10.1053/j.gastro.2018.09.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cammack R., Joannou C. L., Cui X.-Y., Torres Martinez C., Maraj S. R., Hughes M. N. (1999). Nitrite and nitrosyl compounds in food preservation. Biochim. Biophys. Acta 1411 (2), 475–488. 10.1016/S0005-2728(99)00033-X [DOI] [PubMed] [Google Scholar]
- Cao H., Xu M., Dong W., Deng B., Wang S., Zhang Y., et al. (2017). Secondary bile acid-induced dysbiosis promotes intestinal carcinogenesis. Int. J. Cancer. 140 (11), 2545–2556. 10.1002/ijc.30643 [DOI] [PubMed] [Google Scholar]
- Cascella M., Bimonte S., Barbieri A., Del Vecchio V., Caliendo D., Schiavone V., et al. (2018). Dissecting the mechanisms and molecules underlying the potential carcinogenicity of red and processed meat in colorectal cancer (CRC): An overview on the current state of knowledge. Infect. Agent Cancer. 13, 3–3. 10.1186/s13027-018-0174-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan C. W. H., Law B. M. H., Waye M. M. Y., Chan J. Y. W., So W. K. W., Chow K. M. (2019). Trimethylamine-N-oxide as one hypothetical link for the relationship between intestinal microbiota and cancer - where we are and where shall we go? J. Cancer 10 (23), 5874–5882. 10.7150/jca.31737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ChangxiChen, Mao Y., Du J., Xu Y., Zhu Z., Cao H. (2019). Helicobacter pylori infection associated with an increased risk of colorectal adenomatous polyps in the Chinese population. BMC Gastroenterol. 19 (1), 14. 10.1186/s12876-018-0918-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapkin R. S., Davidson L. A., Ly L., Weeks B. R., Lupton J. R., McMurray D. N. (2007). Immunomodulatory effects of (n-3) fatty acids: Putative link to inflammation and colon cancer. J. Nutr. 137 (1), 200S–204S. 10.1093/jn/137.1.200S [DOI] [PubMed] [Google Scholar]
- Chassaing B., Vijay-Kumar M., Gewirtz A. T. (2017). How diet can impact gut microbiota to promote or endanger health. Curr. Opin. Gastroenterol. 33 (6), 417–421. 10.1097/MOG.0000000000000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelombitko M. A. (2018). Role of reactive oxygen species in inflammation: A minireview. Moscow Univ. Biol. Sci. Bull. 73 (4), 199–202. 10.3103/S009639251804003X [DOI] [Google Scholar]
- Chen H. M., Yu Y. N., Wang J. L., Lin Y. W., Kong X., Yang C. Q., et al. (2013). Decreased dietary fiber intake and structural alteration of gut microbiota in patients with advanced colorectal adenoma. Am. J. Clin. Nutr. 97 (5), 1044–1052. 10.3945/ajcn.112.046607 [DOI] [PubMed] [Google Scholar]
- Chen Y., Lu Y., Ke Y., Li Y. (2019). Prognostic impact of the Fusobacterium nucleatum status in colorectal cancers. Med. (Baltimore) 98 (39), e17221. 10.1097/md.0000000000017221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung C., Loy S., Li G. X., Liu A. B., Yang C. S. (2011). Rapid induction of colon carcinogenesis in cyp1a-humanized mice by 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine and dextran sodium sulfate. Carcinogenesis 32 (2), 233–239. 10.1093/carcin/bgq235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiavarini M., Bertarelli G., Minelli L., Fabiani R. (2017). Dietary intake of meat cooking-related mutagens (HCAs) and risk of colorectal adenoma and cancer: A systematic review and meta-analysis. Nutrients 9 (5), 514. 10.3390/nu9050514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho C. E., Taesuwan S., Malysheva O. V., Bender E., Tulchinsky N. F., Yan J., et al. (2017). Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: A randomized controlled trial. Mol. Nutr. Food Res. 61 (1), 1600324. 10.1002/mnfr.201600324 [DOI] [PubMed] [Google Scholar]
- Choi Y., Giovannucci E., Lee J. E. (2012). Glycaemic index and glycaemic load in relation to risk of diabetes-related cancers: A meta-analysis. Br. J. Nutr. 108 (11), 1934–1947. 10.1017/s0007114512003984 [DOI] [PubMed] [Google Scholar]
- Choi C.-H. R., Al Bakir I., Ding N.-S., Lee G.-H., Askari A., Warusavitarne J., et al. (2019). Cumulative burden of inflammation predicts colorectal neoplasia risk in ulcerative colitis: A large single-centre study. Gut 68 (3), 414–422. 10.1136/gutjnl-2017-314190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun Y. J., Sohn S.-K., Song H. K., Lee S. M., Youn Y. H., Lee S., et al. (2015). Associations of colorectal cancer incidence with nutrient and food group intakes in Korean adults: A case-control study. Clin. Nutr. Res. 4 (2), 110–123. 10.7762/cnr.2015.4.2.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung L., Thiele Orberg E., Geis A. L., Chan J. L., Fu K., DeStefano Shields C. E., et al. (2018). Bacteroides fragilis toxin coordinates a pro-carcinogenic inflammatory cascade via targeting of colonic epithelial cells. Cell Host Microbe 23 (2), 203–214.e205. 10.1016/j.chom.2018.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constante M., Fragoso G., Calvé A., Samba-Mondonga M., Santos M. M. (2017). Dietary heme induces gut dysbiosis, aggravates colitis, and potentiates the development of adenomas in mice. Front. Microbiol. 8, 1809. 10.3389/fmicb.2017.01809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corredoira J., Grau I., Garcia-Rodriguez J. F., Garcia-Pais M. J., Rabunal R., Ardanuy C., et al. (2017). Colorectal neoplasm in cases of Clostridium septicum and Streptococcus gallolyticus subsp. Gallolyticus bacteraemia. Eur. J. Intern. Med. 41, 68–73. 10.1016/j.ejim.2017.02.009 [DOI] [PubMed] [Google Scholar]
- Cougnoux A., Dalmasso G., Martinez R., Buc E., Delmas J., Gibold L., et al. (2014). Bacterial genotoxin colibactin promotes colon tumour growth by inducing a senescence-associated secretory phenotype. Gut 63 (12), 1932–1942. 10.1136/gutjnl-2013-305257 [DOI] [PubMed] [Google Scholar]
- Cross A. J., Ferrucci L. M., Risch A., Graubard B. I., Ward M. H., Park Y., et al. (2010). A large prospective study of meat consumption and colorectal cancer risk: An investigation of potential mechanisms underlying this association. Cancer Res. 70 (6), 2406–2414. 10.1158/0008-5472.CAN-09-3929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahm C. C., Keogh R. H., Lentjes M. A., Spencer E. A., Key T. J., Greenwood D. C., et al. (2010. a). Intake of dietary fats and colorectal cancer risk: Prospective findings from the UK dietary cohort consortium. Cancer Epidemiol. 34 (5), 562–567. 10.1016/j.canep.2010.07.008 [DOI] [PubMed] [Google Scholar]
- Dahm C. C., Keogh R. H., Spencer E. A., Greenwood D. C., Key T. J., Fentiman I. S., et al. (2010. b). Dietary fiber and colorectal cancer risk: A nested case–control study using food diaries. J. Natl. Cancer Inst. 102 (9), 614–626. 10.1093/jnci/djq092 [DOI] [PubMed] [Google Scholar]
- Dalmasso G., Cougnoux A., Delmas J., Darfeuille-Michaud A., Bonnet R. (2014). The bacterial genotoxin colibactin promotes colon tumor growth by modifying the tumor microenvironment. Gut Microbes 5 (5), 675–680. 10.4161/19490976.2014.969989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das P., Marcišauskas S., Ji B., Nielsen J. (2019). Metagenomic analysis of bile salt biotransformation in the human gut microbiome. BMC Genomics 20 (1), 517–517. 10.1186/s12864-019-5899-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- David L. A., Maurice C. F., Carmody R. N., Gootenberg D. B., Button J. E., Wolfe B. E., et al. (2014). Diet rapidly and reproducibly alters the human gut microbiome. Nature 505 (7484), 559–563. 10.1038/nature12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C. D., Milner J. A. (2009). Gastrointestinal microflora, food components and colon cancer prevention. J. Nutr. Biochem. 20 (10), 743–752. 10.1016/j.jnutbio.2009.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day S. D., Enos R. T., McClellan J. L., Steiner J. L., Velázquez K. T., Murphy E. A. (2013). Linking inflammation to tumorigenesis in a mouse model of high-fat-diet-enhanced colon cancer. Cytokine 64 (1), 454–462. 10.1016/j.cyto.2013.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Almeida C. V., de Camargo M. R., Russo E., Amedei A. (2019). Role of diet and gut microbiota on colorectal cancer immunomodulation. World J. Gastroenterol. 25 (2), 151–162. 10.3748/wjg.v25.i2.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Filippis F., Pellegrini N., Vannini L., Jeffery I. B., La Storia A., Laghi L., et al. (2016). High-level adherence to a mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 65 (11), 1812–1821. 10.1136/gutjnl-2015-309957 [DOI] [PubMed] [Google Scholar]
- De Filippo C., Cavalieri D., Di Paola M., Ramazzotti M., Poullet J. B., Massart S., et al. (2010). Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. U. S. A. 107 (33), 14691–14696. 10.1073/pnas.1005963107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Palma F. D. E., D’Argenio V., Pol J., Kroemer G., Maiuri M. C., Salvatore F. (2019). The molecular hallmarks of the serrated pathway in colorectal cancer. Cancers (Basel) 11 (7), 1017. 10.3390/cancers11071017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vogel S., Schneede J., Ueland P. M., Vollset S. E., Meyer K., Fredriksen Å., et al. (2011). Biomarkers related to one-carbon metabolism as potential risk factors for distal colorectal adenomas. Cancer Epidemiol. Biomarkers Prev. 20 (8), 1726–1735. 10.1158/1055-9965.EPI-11-0359 [DOI] [PubMed] [Google Scholar]
- Defois C., Ratel J., Denis S., Batut B., Beugnot R., Peyretaillade E., et al. (2017). Environmental pollutant benzo[a]pyrene impacts the volatile metabolome and transcriptome of the human gut microbiota. Front. Microbiol. 8, 1562. 10.3389/fmicb.2017.01562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defois C., Ratel J., Garrait G., Denis S., Le Goff O., Talvas J., et al. (2018). Food chemicals disrupt human gut microbiota activity and impact intestinal homeostasis as revealed by in vitro systems. Sci. Rep. 8 (1), 11006. 10.1038/s41598-018-29376-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejea C. M., Fathi P., Craig J. M., Boleij A., Taddese R., Geis A. L., et al. (2018). Patients with familial adenomatous polyposis harbor colonic biofilms containing tumorigenic bacteria. Sci. (New York N.Y.) 359 (6375), 592–597. 10.1126/science.aah3648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demeyer D., Mertens B., De Smet S., Ulens M. (2016). Mechanisms linking colorectal cancer to the consumption of (processed) red meat: A review. Crit. Rev. Food Sci. Nutr. 56 (16), 2747–2766. 10.1080/10408398.2013.873886 [DOI] [PubMed] [Google Scholar]
- Dermadi D., Valo S., Ollila S., Soliymani R., Sipari N., Pussila M., et al. (2017). Western diet deregulates bile acid homeostasis, cell proliferation, and tumorigenesis in colon. Cancer Res. 77 (12), 3352–3363. 10.1158/0008-5472.Can-16-2860 [DOI] [PubMed] [Google Scholar]
- Diggs D. L., Myers J. N., Banks L. D., Niaz M. S., Hood D. B., Roberts L. J., et al. (2013). Influence of dietary fat type on benzo(a)pyrene [b(a)p] biotransformation in a b(a)p-induced mouse model of colon cancer. J. Nutr. Biochem. 24 (12), 2051–2063. 10.1016/j.jnutbio.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon S. M., Lee E. J., Kotter C. V., Austin G. L., Gianella S., Siewe B., et al. (2016). Gut dendritic cell activation links an altered colonic microbiome to mucosal and systemic T-cell activation in untreated HIV-1 infection. Mucosal Immunol. 9 (1), 24–37. 10.1038/mi.2015.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohoe D. R., Collins ,.L. B., Wali A., Bigler R., Sun W., Bultman S. J. (2012). The Warburg effect dictates the mechanism of butyrate-mediated histone acetylation and cell proliferation. Mol. Cell. 48 (4), 612–626. 10.1016/j.molcel.2012.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doron S., Snydman D. R. (2015). Risk and safety of probiotics. Clin. Infect. Dis. 60 Suppl 2:Suppl 2, S129–S134. 10.1093/cid/civ085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duboc H., Rajca S., Rainteau D., Benarous D., Maubert M. A., Quervain E., et al. (2013). Connecting dysbiosis, bile-acid dysmetabolism and gut inflammation in inflammatory bowel diseases. Gut 62 (4), 531–539. 10.1136/gutjnl-2012-302578 [DOI] [PubMed] [Google Scholar]
- Eklof V., Lofgren-Burstrom A., Zingmark C., Edin S., Larsson P., Karling P., et al. (2017). Cancer-associated fecal microbial markers in colorectal cancer detection. Int. J. Cancer. 141 (12), 2528–2536. 10.1002/ijc.31011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engemann A., Focke C., Humpf H. U. (2013). Intestinal formation of N-nitroso compounds in the pig cecum model. J. Agric. Food Chem. 61 (4), 998–1005. 10.1021/jf305040e [DOI] [PubMed] [Google Scholar]
- Engeset D., Andersen V., Hjartåker A., Lund E. (2007). Consumption of fish and risk of colon cancer in the Norwegian women and cancer (NOWAC) study. Br. J. Nutr. 98 (3), 576–582. 10.1017/S0007114507721487 [DOI] [PubMed] [Google Scholar]
- Epplein M., Pawlita M., Michel A., Peek R. M., Jr., Cai Q., Blot W. J. (2013). Helicobacter pylori protein-specific antibodies and risk of colorectal cancer. Cancer Epidemiol. Biomarkers Prev. 22 (11), 1964–1974. 10.1158/1055-9965.Epi-13-0702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewa B., Danuta M.-Š. (2017). Polycyclic aromatic hydrocarbons and pah-related DNA adducts. J. Appl. Genet. 58 (3), 321–330. 10.1007/s13353-016-0380-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahrer J., Kaina B. (2013). O6 -methylguanine-DNA methyltransferase in the defense against N-nitroso compounds and colorectal cancer. Carcinogenesis 34 (11), 2435–2442. 10.1093/carcin/bgt275 [DOI] [PubMed] [Google Scholar]
- Fang W., Xue H., Chen X., Chen K., Ling W. (2019). Supplementation with sodium butyrate modulates the composition of the gut microbiota and ameliorates high-fat diet-induced obesity in mice. J. Nutr. 149 (5), 747–754. 10.1093/jn/nxy324 [DOI] [PubMed] [Google Scholar]
- Fardini Y., Wang X., Témoin S., Nithianantham S., Lee D., Shoham M., et al. (2011). Fusobacterium nucleatum adhesin FadA binds vascular endothelial cadherin and alters endothelial integrity. Mol. Microbiol. 82 (6), 1468–1480. 10.1111/j.1365-2958.2011.07905.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhana L., Nangia-Makker P., Arbit E., Shango K., Sarkar S., Mahmud H., et al. (2016). Bile acid: A potential inducer of colon cancer stem cells. Stem Cell Res. Ther. 7 (1), 181. 10.1186/s13287-016-0439-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekry M. I., Engels C., Zhang J., Schwab C., Lacroix C., Sturla S. J., et al. (2016). The strict anaerobic gut microbe Eubacterium hallii transforms the carcinogenic dietary heterocyclic amine 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP). Environ. Microbiol Rep. 8 (2), 201–209. 10.1111/1758-2229.12369 [DOI] [PubMed] [Google Scholar]
- Ferrer M., Ruiz A., Lanza F., Haange S. B., Oberbach A., Till H., et al. (2013). Microbiota from the distal guts of lean and obese adolescents exhibit partial functional redundancy besides clear differences in community structure. Environ. Microbiol. 15 (1), 211–226. 10.1111/j.1462-2920.2012.02845.x [DOI] [PubMed] [Google Scholar]
- Fong W., Li Q., Yu J. (2020). Gut microbiota modulation: A novel strategy for prevention and treatment of colorectal cancer. Oncogene 39 (26), 4925–4943. 10.1038/s41388-020-1341-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franceschi S., Favero A., La Vecchia C., Negri E., Conti E., Montella M., et al. (1997). Food groups and risk of colorectal cancer in Italy. Int. J. Cancer. 72 (1), 56–61. [DOI] [PubMed] [Google Scholar]
- Fukugaiti M. H., Ignacio A., Fernandes M. R., Ribeiro Júnior U., Nakano V., Avila-Campos M. J. (2015). High occurrence of Fusobacterium nucleatum and Clostridium difficile in the intestinal microbiota of colorectal carcinoma patients. Braz. J. Microbiol. 46 (4), 1135–1140. 10.1590/S1517-838246420140665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnière J., Raisch J., Veziant J., Barnich N., Bonnet R., Buc E., et al. (2016). Gut microbiota imbalance and colorectal cancer. World J. Gastroenterol. 22 (2), 501–518. 10.3748/wjg.v22.i2.501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galeone C., Pelucchi C., La Vecchia C. (2012). Added sugar, glycemic index and load in colon cancer risk. Curr. Opin. Clin. Nutr. Metab. Care 15 (4), 368–373. 10.1097/MCO.0b013e3283539f81 [DOI] [PubMed] [Google Scholar]
- Gamallat Y., Meyiah A., Kuugbee E. D., Hago A. M., Chiwala G., Awadasseid A., et al. (2016). Lactobacillus rhamnosus induced epithelial cell apoptosis, ameliorates inflammation and prevents colon cancer development in an animal model. BioMed. Pharmacother. 83, 536–541. 10.1016/j.biopha.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Gatej S. M., Bright R., Weyrich L. S., Marino V., Christophersen C. T., Gibson R. J., et al. (2020). Probiotic Lactobacillus rhamnosus GG protects against P. gingivalis and F. nucleatum gut dysbiosis. J. Int. Acad. Periodontol. 22 (2), 18–27. [PubMed] [Google Scholar]
- Gemelli C., Dongmo B. M., Ferrarini F., Grande A., Corsi L. (2014). Cytotoxic effect of hemin in colonic epithelial cell line: Involvement of 18 kDa translocator protein (TSPO). Life Sci. 107 (1-2), 14–20. 10.1016/j.lfs.2014.04.026 [DOI] [PubMed] [Google Scholar]
- George S. M., Mayne S. T., Leitzmann M. F., Park Y., Schatzkin A., Flood A., et al. (2009). Dietary glycemic index, glycemic load, and risk of cancer: A prospective cohort study. Am. J. Epidemiol. 169 (4), 462–472. 10.1093/aje/kwn347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geravand M., Fallah P., Yaghoobi M. H., Soleimanifar F., Farid M., Zinatizadeh N., et al. (2019). Investigation of Enterococcus faecalis population in patients with polyp and colorectal cancer in comparison of healthy individuals. Arq Gastroenterol. 56 (2), 141–145. 10.1590/s0004-2803.201900000-28 [DOI] [PubMed] [Google Scholar]
- Ghanavati R., Akbari A., Mohammadi F., Asadollahi P., Javadi A., Talebi M., et al. (2020). Lactobacillus species inhibitory effect on colorectal cancer progression through modulating the Wnt/β-catenin signaling pathway. Mol. Cell Biochem. 470 (1), 1–13. 10.1007/s11010-020-03740-8 [DOI] [PubMed] [Google Scholar]
- Gharbi Y., Fhoula I., Ruas-Madiedo P., Afef N., Boudabous A., Gueimonde M., et al. (2019). In-vitro characterization of potentially probiotic Lactobacillus strains isolated from human microbiota: Interaction with pathogenic bacteria and the enteric cell line HT29. Ann. Microbiol. 69 (1), 61–72. 10.1007/s13213-018-1396-1 [DOI] [Google Scholar]
- Gianfredi V., Salvatori T., Villarini M., Moretti M., Nucci D., Realdon S. (2018). Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. Int. J. Food Sci. Nutr. 69 (8), 904–915. 10.1080/09637486.2018.1446917 [DOI] [PubMed] [Google Scholar]
- Gnagnarella P., Gandini S., La Vecchia C., Maisonneuve P. (2008). Glycemic index, glycemic load, and cancer risk: A meta-analysis. Am. J. Clin. Nutr. 87 (6), 1793–1801. 10.1093/ajcn/87.6.1793 [DOI] [PubMed] [Google Scholar]
- Goncalves M. D., Lu C., Tutnauer J., Hartman T. E., Hwang S.-K., Murphy C. J., et al. (2019). High-fructose corn syrup enhances intestinal tumor growth in mice. Science 363 (6433), 1345–1349. 10.1126/science.aat8515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin A. C., Destefano Shields C. E., Wu S., Huso D. L., Wu X., Murray-Stewart T. R., et al. (2011). Polyamine catabolism contributes to enterotoxigenic Bacteroides fragilis-induced colon tumorigenesis. Proc. Natl. Acad. Sci. U. S. A. 108 (37), 15354–15359. 10.1073/pnas.1010203108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorvitovskaia A., Holmes S. P., Huse S. M. (2016). Interpreting Prevotella and Bacteroides as biomarkers of diet and lifestyle. Microbiome 4 (1), 15. 10.1186/s40168-016-0160-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graillot V., Dormoy I., Dupuy J., Shay J. W., Huc L., Mirey G., et al. (2016). Genotoxicity of cytolethal distending toxin (CDT) on isogenic human colorectal cell lines: Potential promoting effects for colorectal carcinogenesis. Front. Cell Infect. Microbiol. 6, 34. 10.3389/fcimb.2016.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guertin K. A., Li X. S., Graubard B. I., Albanes D., Weinstein S. J., Goedert J. J., et al. (2017). Serum trimethylamine N-oxide, carnitine, choline, and betaine in relation to colorectal cancer risk in the alpha tocopherol, beta carotene cancer prevention study. Cancer Epidemiol. Biomarkers Prev. 26 (6), 945–952. 10.1158/1055-9965.EPI-16-0948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gur C., Ibrahim Y., Isaacson B., Yamin R., Abed J., Gamliel M., et al. (2015). Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity 42 (2), 344–355. 10.1016/j.immuni.2015.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haghi F., Goli E., Mirzaei B., Zeighami H. (2019). The association between fecal enterotoxigenic B. fragilis with colorectal cancer. BMC Cancer. 19 (1), 879. 10.1186/s12885-019-6115-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han R., Sun Q., Wu J., Zheng P., Zhao G. (2016). Sodium butyrate upregulates miR-203 expression to exert anti-proliferation effect on colorectal cancer cells. Cell. Physiol. Biochem. 39 (5), 1919–1929. 10.1159/000447889 [DOI] [PubMed] [Google Scholar]
- Han A., Bennett N., Ahmed B., Whelan J., Donohoe D. R. (2018). Butyrate decreases its own oxidation in colorectal cancer cells through inhibition of histone deacetylases. Oncotarget 9 (43), 27280–27292. 10.18632/oncotarget.25546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen N. W., Sams A. (2018). The microbiotic highway to health-new perspective on food structure, gut microbiota, and host inflammation. Nutrients 10 (11), 1590. 10.3390/nu10111590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He C., Cheng D., Peng C., Li Y., Zhu Y., Lu N. (2018). High-fat diet induces dysbiosis of gastric microbiota prior to gut microbiota in association with metabolic disorders in mice. Front. Microbiol. 9, 639. 10.3389/fmicb.2018.00639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmus D. S., Thompson C. L., Zelenskiy S., Tucker T. C., Li L. (2013). Red meat-derived heterocyclic amines increase risk of colon cancer: A population-based case-control study. Nutr. Cancer. 65 (8), 1141–1150. 10.1080/01635581.2013.834945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemeryck L. Y., Rombouts C., Hecke T. V., Van Meulebroek L., Bussche J. V., De Smet S., et al. (2016). In vitro DNA adduct profiling to mechanistically link red meat consumption to colon cancer promotion. Toxicol. Res. (Camb) 5 (5), 1346–1358. 10.1039/c6tx00079g [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt M. A., Hoffmann C., Sherrill-Mix S. A., Keilbaugh S. A., Hamady M., Chen Y.-Y., et al. (2009). High-fat diet determines the composition of the murine gut microbiome independently of obesity. Gastroenterology 137 (5), 1716–1724.e1242. 10.1053/j.gastro.2009.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu S., Liu L., Chang E. B., Wang J. Y., Raufman J. P. (2015). Butyrate inhibits pro-proliferative miR-92a by diminishing c-myc-induced miR-17-92a cluster transcription in human colon cancer cells. Mol. Cancer. 14, 180. 10.1186/s12943-015-0450-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huncharek M., Muscat J., Kupelnick B. (2008). Colorectal cancer risk and dietary intake of calcium, vitamin D, and dairy products: A meta-analysis of 26,335 cases from 60 observational studies. Nutr. Cancer. 61 (1), 47–69. 10.1080/01635580802395733 [DOI] [PubMed] [Google Scholar]
- Hursting S. D., Digiovanni J., Dannenberg A. J., Azrad M., Leroith D., Demark-Wahnefried W., et al. (2012). Obesity, energy balance, and cancer: New opportunities for prevention. Cancer Prev. Res. (Phila) 5 (11), 1260–1272. 10.1158/1940-6207.Capr-12-0140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang S., Gwon S.-Y., Kim M. S., Lee S., Rhee K.-J. (2013). Bacteroides fragilis toxin induces IL-8 secretion in HT29/C1 cells through disruption of e-cadherin junctions. Immune Netw. 13 (5), 213–217. 10.4110/in.2013.13.5.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ignacio Barrasa J., Olmo N., Perez-Ramos P., Santiago-Gomez A., Lecona E., Turnay J., et al. (2011). Deoxycholic and chenodeoxycholic bile acids induce apoptosis via oxidative stress in human colon adenocarcinoma cells. Apoptosis 16 (10), 1054–1067. 10.1007/s10495-011-0633-x [DOI] [PubMed] [Google Scholar]
- Ijssennagger N., Belzer C., Hooiveld G. J., Dekker J., van Mil S. W. C., Müller M., et al. (2015). Gut microbiota facilitates dietary heme-induced epithelial hyperproliferation by opening the mucus barrier in colon. Proc. Natl. Acad. Sci. U. S. A. 112 (32), 10038–10043. 10.1073/pnas.1507645112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IJssennagger N., Derrien M., van Doorn G. M., Rijnierse A., van den Bogert B., Müller M., et al. (2012). Dietary heme alters microbiota and mucosa of mouse colon without functional changes in host-microbe cross-talk. PloS One 7 (12), e49868–e49868. 10.1371/journal.pone.0049868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IJssennagger N., van der Meer R., van Mil S. W. C. (2016). Sulfide as a mucus barrier-breaker inflammatory bowel disease? Trends Mol Med. 22 (3), 190–199. 10.1016/j.molmed.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Iljazovic A., Roy U., Gálvez E. J. C., Lesker T. R., Zhao B., Gronow A., et al. (2020). Perturbation of the gut microbiome by Prevotella spp. Enhances host susceptibility to mucosal inflammation. Mucosal Immunol. 10.1038/s41385-020-0296-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa S.-i., Tamaki S., Ohata M., Arihara K., Itoh M. (2010). Heme induces DNA damage and hyperproliferation of colonic epithelial cells via hydrogen peroxide produced by heme oxygenase: A possible mechanism of heme-induced colon cancer. Mol. Nutr. Food Res. 54 (8), 1182–1191. 10.1002/mnfr.200900348 [DOI] [PubMed] [Google Scholar]
- Islam K. S., Fukiya S., Hagio M., Fujii N., Ishizuka S., Ooka T., et al. (2011). Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology 141 (5), 1773–1781. 10.1053/j.gastro.2011.07.046 [DOI] [PubMed] [Google Scholar]
- Jahani-Sherafat S., Alebouyeh M., Moghim S., Ahmadi Amoli H., Ghasemian-Safaei H. (2018). Role of gut microbiota in the pathogenesis of colorectal cancer; a review article. Gastroenterol. Hepatol Bed Bench. 11 (2), 101–109. [PMC free article] [PubMed] [Google Scholar]
- Jamin E. L., Riu A., Douki T., Debrauwer L., Cravedi J.-P., Zalko D., et al. (2013). Combined genotoxic effects of a polycyclic aromatic hydrocarbon (B(a)P) and an heterocyclic amine (PhIP) in relation to colorectal carcinogenesis. PloS One 8 (3), e58591. 10.1371/journal.pone.0058591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järvinen R., Knekt P., Hakulinen T., Rissanen H., Heliövaara M. (2001). Dietary fat, cholesterol and colorectal cancer in a prospective study. Br. J. Cancer 85 (3), 357–361. 10.1054/bjoc.2001.1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joosen A. M. C. P., Kuhnle G. G. C., Aspinall S. M., Barrow T. M., Lecommandeur E., Azqueta A., et al. (2009). Effect of processed and red meat on endogenous nitrosation and DNA damage. Carcinogenesis 30 (8), 1402–1407. 10.1093/carcin/bgp130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju J., Kwak Y., Hao X., Yang C. S. (2012). Inhibitory effects of calcium against intestinal cancer in human colon cancer cells and Apc(Min/+) mice. Nutr. Res. Pract. 6 (5), 396–404. 10.4162/nrp.2012.6.5.396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabzinski J., Mucha B., Cuchra M., Markiewicz L., Przybylowska K., Dziki A., et al. (2016). Efficiency of base excision repair of oxidative DNA damage and its impact on the risk of colorectal cancer in the Polish population. Oxid. Med. Cell Longev. 2016, 3125989. 10.1155/2016/3125989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiko G. E., Ryu S. H., Koues O. I., Collins P. L., Solnica-Krezel L., Pearce E. J., et al. (2016). The colonic crypt protects stem cells from microbiota-derived metabolites. Cell 165 (7), 1708–1720. 10.1016/j.cell.2016.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasai C., Sugimoto K., Moritani I., Tanaka J., Oya Y., Inoue H., et al. (2015). Comparison of the gut microbiota composition between obese and non-obese individuals in a Japanese population, as analyzed by terminal restriction fragment length polymorphism and next-generation sequencing. BMC Gastroenterol. 15, 100. 10.1186/s12876-015-0330-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashani N., Bezmin Abadi A. T., Rahimi F., Forootan M. (2020). FadA-positive Fusobacterium nucleatum is prevalent in biopsy specimens of iranian patients with colorectal cancer. New Microbes New Infect. 34, 100651. 10.1016/j.nmni.2020.100651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasprzak A., Adamek A. (2019). Insulin-like growth factor 2 (IGF2) signaling in colorectal cancer-from basic research to potential clinical applications. Int. J. Mol. Sci. 20 (19), 4915. 10.3390/ijms20194915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawanishi M., Hisatomi Y., Oda Y., Shimohara C., Tsunematsu Y., Sato M., et al. (2019). In vitro genotoxicity analyses of colibactin-producing E. coli isolated from a Japanese colorectal cancer patient. J. Toxicol. Sci. 44 (12), 871–876. 10.2131/jts.44.871 [DOI] [PubMed] [Google Scholar]
- Keller D. S., Windsor A., Cohen R., Chand M. (2019). Colorectal cancer in inflammatory bowel disease: Review of the evidence. Tech Coloproctol. 23 (1), 3–13. 10.1007/s10151-019-1926-2 [DOI] [PubMed] [Google Scholar]
- Khalil A., Villard P. H., Dao M. A., Burcelin R., Champion S., Fouchier F., et al. (2010). Polycyclic aromatic hydrocarbons potentiate high-fat diet effects on intestinal inflammation. Toxicol. Lett. 196 (3), 161–167. 10.1016/j.toxlet.2010.04.010 [DOI] [PubMed] [Google Scholar]
- Kim Y., Kim J. (2020). Intake or blood levels of n-3 polyunsaturated fatty acids and risk of colorectal cancer: A systematic review and meta-analysis of prospective studies. Cancer Epidemiol. Biomarkers Prev. 29 (2), 288–299. 10.1158/1055-9965.EPI-19-0931 [DOI] [PubMed] [Google Scholar]
- Kim M., Park K. (2018). Dietary fat intake and risk of colorectal cancer: A systematic review and meta-analysis of prospective studies. Nutrients 10 (12), 1963. 10.3390/nu10121963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K.-A., Gu W., Lee I.-A., Joh E.-H., Kim D.-H. (2012). High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PloS One 7 (10), e47713. 10.1371/journal.pone.0047713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E. K., Cho J. H., Kim E., Kim Y. J. (2017. a). Ursodeoxycholic acid inhibits the proliferation of colon cancer cells by regulating oxidative stress and cancer stem-like cell growth. PloS One 12 (7), e0181183. 10.1371/journal.pone.0181183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Oh S.-W., Kim Y.-S., Kwon H., Joh H.-K., Lee J.-E., et al. (2017. b). Association between dietary fat intake and colorectal adenoma in Korean adults: A cross-sectional study. Med. (Baltimore) 96 (1), e5759–e5759. 10.1097/MD.0000000000005759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Yin K., Falcon D. M., Xue X. (2019. a). The interaction of Hemin and Sestrin2 modulates oxidative stress and colon tumor growth. Toxicol. Appl. Pharmacol. 374, 77–85. 10.1016/j.taap.2019.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. J., Kim S.-E., Kim A. R., Kang S., Park M.-Y., Sung M.-K. (2019. b). Dietary fat intake and age modulate the composition of the gut microbiota and colonic inflammation in C57BL/6J mice. BMC Microbiol. 19 (1), 193. 10.1186/s12866-019-1557-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi J. (2018). Effect of diet and gut environment on the gastrointestinal formation of N-nitroso compounds: A review. Nitric. Oxide 73, 66–73. 10.1016/j.niox.2017.06.001 [DOI] [PubMed] [Google Scholar]
- Koeth R. A., Wang Z., Levison B. S., Buffa J. A., Org E., Sheehy B. T., et al. (2013). Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 19 (5), 576–585. 10.1038/nm.3145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh G. Y., Kane A. V., Wu X., Crott J. W. (2020). Parabacteroides distasonis attenuates tumorigenesis, modulates inflammatory markers and promotes intestinal barrier integrity in azoxymethane-treated A/J mice. Carcinogenesis 41 (7), 909–917. 10.1093/carcin/bgaa018 [DOI] [PubMed] [Google Scholar]
- Kohoutova D., Smajs D., Moravkova P., Cyrany J., Moravkova M., Forstlova M., et al. (2014). Escherichia coli strains of phylogenetic group B2 and D and bacteriocin production are associated with advanced colorectal neoplasia. BMC Infect. Dis. 14 (1), 733. 10.1186/s12879-014-0733-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koliada A., Syzenko G., Moseiko V., Budovska L., Puchkov K., Perederiy V., et al. (2017). Association between body mass index and Firmicutes/Bacteroidetes ratio in an adult Ukrainian population. BMC Microbiol. 17 (1), 120. 10.1186/s12866-017-1027-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostic A. D., Chun E., Robertson L., Glickman J. N., Gallini C. A., Michaud M., et al. (2013). Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe 14 (2), 207–215. 10.1016/j.chom.2013.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kountz D. J., Behrman E. J., Zhang L., Krzycki J. A. (2020). MtcB, a member of the MttB superfamily from the human gut acetogen Eubacterium Limosum, is a cobalamin-dependent carnitine demethylase. J. Biol. Chem. 295 (34), 11971–11981. 10.1074/jbc.RA120.012934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishna-Subramanian S., Hanski M. L., Loddenkemper C., Choudhary B., Pagès G., Zeitz M., et al. (2012). UDCA slows down intestinal cell proliferation by inducing high and sustained erk phosphorylation. Int. J. Cancer. 130 (12), 2771–2782. 10.1002/ijc.26336 [DOI] [PubMed] [Google Scholar]
- Kumar R., Herold J. L., Schady D., Davis J., Kopetz S., Martinez-Moczygemba M., et al. (2017). Streptococcus gallolyticus subsp. gallolyticus promotes colorectal tumor development. PloS Pathog. 13 (7), e1006440. 10.1371/journal.ppat.1006440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurnick S. A., Mannion A. J., Feng Y., Madden C. M., Chamberlain P., Fox J. G. (2019). Genotoxic Escherichia coli strains encoding colibactin, cytolethal distending toxin, and cytotoxic necrotizing factor in laboratory rats. Comp. Med. 69 (2), 103–113. 10.30802/aalas-cm-18-000099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuugbee E. D., Shang X., Gamallat Y., Bamba D., Awadasseid A., Suliman M. A., et al. (2016). Structural change in microbiota by a probiotic cocktail enhances the gut barrier and reduces cancer via TLR2 signaling in a rat model of colon cancer. Dig Dis. Sci. 61 (10), 2908–2920. 10.1007/s10620-016-4238-7 [DOI] [PubMed] [Google Scholar]
- Kverka M., Zakostelska Z., Klimesova K., Sokol D., Hudcovic T., Hrncir T., et al. (2011). Oral administration of Parabacteroides distasonis antigens attenuates experimental murine colitis through modulation of immunity and microbiota composition. Clin. Exp. Immunol. 163 (2), 250–259. 10.1111/j.1365-2249.2010.04286.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwong T. N. Y., Wang X., Nakatsu G., Chow T. C., Tipoe T., Dai R. Z. W., et al. (2018). Association between bacteremia from specific microbes and subsequent diagnosis of colorectal cancer. Gastroenterology 155 (2), 383–390.e388. 10.1053/j.gastro.2018.04.028 [DOI] [PubMed] [Google Scholar]
- Lajczak N. K., Saint-Criq V., O’dwyer A. M., Perino A., Adorini L., Schoonjans K., et al. (2017). Bile acids deoxycholic acid and ursodeoxycholic acid differentially regulate human β-defensin-1 and-2 secretion by colonic epithelial cells. FASEB J. 31 (9), 3848–3857. 10.1096/fj.201601365R [DOI] [PubMed] [Google Scholar]
- Landy J., Ronde E., English N., Clark S. K., Hart A. L., Knight S. C., et al. (2016). Tight junctions in inflammatory bowel diseases and inflammatory bowel disease associated colorectal cancer. World J. Gastroenterol. 22 (11), 3117–3126. 10.3748/wjg.v22.i11.3117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen J. M. (2017). The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology 151 (4), 363–374. 10.1111/imm.12760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Leu R. K., Winter J. M., Christophersen C. T., Young G. P., Humphreys K. J., Hu Y., et al. (2015). Butyrylated starch intake can prevent red meat-induced o6-methyl-2-deoxyguanosine adducts in human rectal tissue: A randomised clinical trial. Br. J. Nutr. 114 (2), 220–230. 10.1017/s0007114515001750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecomte V., Kaakoush N. O., Maloney C. A., Raipuria M., Huinao K. D., Mitchell H. M., et al. (2015). Changes in gut microbiota in rats fed a high fat diet correlate with obesity-associated metabolic parameters. PloS One 10 (5), e0126931. 10.1371/journal.pone.0126931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.-A., Shu X. O., Yang G., Li H., Gao Y.-T., Zheng W. (2009). Animal origin foods and colorectal cancer risk: A report from the Shanghai women’s health study. Nutr. Cancer. 61 (2), 194–205. 10.1080/01635580802419780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. J., Hong Y.-J., Kim J. Y., Lee K. W., Kwon O. (2013). Dietary Chlorella protects against heterocyclic amine-induced aberrant gene expression in the rat colon by increasing fecal excretion of unmetabolized PhIP. Food Chem. Toxicol. 56, 272–277. 10.1016/j.fct.2013.01.028 [DOI] [PubMed] [Google Scholar]
- Lewin M. H., Bailey N., Bandaletova T., Bowman R., Cross A. J., Pollock J., et al. (2006). Red meat enhances the colonic formation of the DNA adduct o6-carboxymethyl guanine: Implications for colorectal cancer risk. Cancer Res. 66 (3), 1859–1865. 10.1158/0008-5472.Can-05-2237 [DOI] [PubMed] [Google Scholar]
- Ley R. E. (2016). Gut microbiota in 2015: Prevotella in the gut: Choose carefully. Nat. Rev. Gastroenterol. Hepatol 13 (2), 69–70. 10.1038/nrgastro.2016.4 [DOI] [PubMed] [Google Scholar]
- Li Y.-Y., Ge Q.-X., Cao J., Zhou Y.-J., Du Y.-L., Shen B., et al. (2016). Association of Fusobacterium nucleatum infection with colorectal cancer in Chinese patients. World J. Gastroenterol. 22 (11), 3227–3233. 10.3748/wjg.v22.i11.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Ding C., Meng T., Lu W., Liu W., Hao H., et al. (2017). Butyrate suppresses motility of colorectal cancer cells via deactivating Akt/ERK signaling in histone deacetylase dependent manner. J. Pharmacol. Sci. 135 (4), 148–155. 10.1016/j.jphs.2017.11.004 [DOI] [PubMed] [Google Scholar]
- Li W., Zhang X., Sang H., Zhou Y., Shang C., Wang Y., et al. (2019). Effects of hyperglycemia on the progression of tumor diseases. J. Exp. Clin. Cancer Res. 38 (1), 327. 10.1186/s13046-019-1309-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin A., Bik E. M., Costello E. K., Dethlefsen L., Haque R., Relman D. A., et al. (2013). Distinct distal gut microbiome diversity and composition in healthy children from Bangladesh and the United States. PloS One 8 (1), e53838–e53838. 10.1371/journal.pone.0053838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S., Li Y., Zamyatnin A. A., Jr, Werner J., Bazhin A. V. (2018). Reactive oxygen species and colorectal cancer. J. Cell. Physiol. 233 (7), 5119–5132. 10.1002/jcp.26356 [DOI] [PubMed] [Google Scholar]
- Lin C., Cai X., Zhang J., Wang W., Sheng Q., Hua H., et al. (2019). Role of gut microbiota in the development and treatment of colorectal cancer. Digestion 100 (1), 72–78. 10.1159/000494052 [DOI] [PubMed] [Google Scholar]
- Liu T., Zhang L., Joo D., Sun S.-C. (2017). Nf-κb signaling in inflammation. Signal Transduct Target Ther. 2 (1), 17023. 10.1038/sigtrans.2017.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Tabung F. K., Zhang X., Nowak J. A., Qian Z. R., Hamada T., et al. (2018. a). Diets that promote colon inflammation associate with risk of colorectal carcinomas that contain Fusobacterium nucleatum. Clin. Gastroenterol. Hepatol. 16 (10), 1622–1631.e1623. 10.1016/j.cgh.2018.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z.-Y., Tan X.-Y., Li Q.-J., Liao G.-C., Fang A.-P., Zhang D.-M., et al. (2018. b). Trimethylamine N-oxide, a gut microbiota-dependent metabolite of choline, is positively associated with the risk of primary liver cancer: A case-control study. Nutr. Metab. (Lond). 15, 81. 10.1186/s12986-018-0319-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loh Y. H., Jakszyn P., Luben R. N., Mulligan A. A., Mitrou P. N., Khaw K.-T. (2011). N-nitroso compounds and cancer incidence: The European Prospective Investigation into Cancer and Nutrition (EPIC)–Norfolk study. Am. J. Clin. Nutr. 93 (5), 1053–1061. 10.3945/ajcn.111.012377 [DOI] [PubMed] [Google Scholar]
- Long X., Wong C. C., Tong L., Chu E. S. H., Ho Szeto C., Go M. Y. Y., et al. (2019). Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat. Microbiol. 4 (12), 2319–2330. 10.1038/s41564-019-0541-3 [DOI] [PubMed] [Google Scholar]
- Ludwig D. S., Hu F. B., Tappy L., Brand-Miller J. (2018). Dietary carbohydrates: Role of quality and quantity in chronic disease. BMJ 361, k2340. 10.1136/bmj.k2340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo W.-P., Fang Y.-J., Lu M.-S., Zhong X., Chen Y.-M., Zhang C.-X. (2015). High consumption of vegetable and fruit colour groups is inversely associated with the risk of colorectal cancer: A case–control study. Br. J. Nutr. 113 (7), 1129–1138. 10.1017/S0007114515000331 [DOI] [PubMed] [Google Scholar]
- Ma X., Zhou Z., Zhang X., Fan M., Hong Y., Feng Y., et al. (2020). Sodium butyrate modulates gut microbiota and immune response in colorectal cancer liver metastatic mice. Cell Biol. Toxicol. 36 (5), 509–515. 10.1007/s10565-020-09518-4 [DOI] [PubMed] [Google Scholar]
- Maddocks O. D. K., Short A. J., Donnenberg M. S., Bader S., Harrison D. J. (2009). Attaching and effacing Escherichia coli downregulate DNA mismatch repair protein in vitro and are associated with colorectal adenocarcinomas in humans. PloS One 4 (5), e5517–e5517. 10.1371/journal.pone.0005517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddocks O. D. K., Scanlon K. M., Donnenberg M. S. (2013). An Escherichia coli effector protein promotes host mutation via depletion of DNA mismatch repair proteins. mBio 4 (3), e00152. 10.1128/mBio.00152-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoud R. H. (2011). The impact of vitamin B6 supplementation on experimental colitis and colonic mucosal DNA content in female rats fed high-sucrose diet. Aust. J. Basic Appl. Sci. 5, 1051–1060. [Google Scholar]
- Martin O. C., Lin C., Naud N., Tache S., Raymond-Letron I., Corpet D. E., et al. (2015). Antibiotic suppression of intestinal microbiota reduces heme-induced lipoperoxidation associated with colon carcinogenesis in rats. Nutr. Cancer. 67 (1), 119–125. 10.1080/01635581.2015.976317 [DOI] [PubMed] [Google Scholar]
- Martin O. C. B., Bergonzini A., D’Amico F., Chen P., Shay J. W., Dupuy J., et al. (2019. a). Infection with genotoxin-producing Salmonella Enterica synergises with loss of the tumour suppressor APC in promoting genomic instability via the PI3K pathway in colonic epithelial cells. Cell Microbiol. 21 (12), e13099. 10.1111/cmi.13099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin O. C. B., Olier M., Ellero-Simatos S., Naud N., Dupuy J., Huc L., et al. (2019. b). Haem iron reshapes colonic luminal environment: Impact on mucosal homeostasis and microbiome through aldehyde formation. Microbiome 7 (1), 72. 10.1186/s40168-019-0685-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Medina M., Denizot J., Dreux N., Robin F., Billard E., Bonnet R., et al. (2014). Western diet induces dysbiosis with increased E coli in CEABAC10 mice, alters host barrier function favouring AIEC colonisation. Gut 63 (1), 116–124. 10.1136/gutjnl-2012-304119 [DOI] [PubMed] [Google Scholar]
- Martins M., Aymeric L., du Merle L., Danne C., Robbe-Masselot C., Trieu-Cuot P., et al. (2015). Streptococcus gallolyticus pil3 pilus is required for adhesion to colonic mucus and for colonization of mouse distal colon. J. Infect. Dis. 212 (10), 1646–1655. 10.1093/infdis/jiv307 [DOI] [PubMed] [Google Scholar]
- Martins M., Porrini C., du Merle L., Danne C., Robbe-Masselot C., Trieu-Cuot P., et al. (2016). The pil3 pilus of Streptococcus gallolyticus binds to intestinal mucins and to fibrinogen. Gut Microbes 7 (6), 526–532. 10.1080/19490976.2016.1239677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy A. N., Araújo-Pérez F., Azcárate-Peril A., Yeh J. J., Sandler R. S., Keku T. O. (2013). Fusobacterium is associated with colorectal adenomas. PloS One 8 (1), e53653–e53653. 10.1371/journal.pone.0053653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta R. S., Nishihara R., Cao Y., Song M., Mima K., Qian Z. R., et al. (2017). Association of dietary patterns with risk of colorectal cancer subtypes classified by Fusobacterium nucleatum in tumor tissue. JAMA Oncol. 3 (7), 921–927. 10.1001/jamaoncol.2016.6374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes M. C. S., Paulino D. S., Brambilla S. R., Camargo J. A., Persinoti G. F., Carvalheira J. B. C. (2018). Microbiota modification by probiotic supplementation reduces colitis associated colon cancer in mice. World J. Gastroenterol. 24 (18), 1995–2008. 10.3748/wjg.v24.i18.1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller R., Wiedmann M. (2016). Dynamic duo-the Salmonella cytolethal distending toxin combines ADP-ribosyltransferase and nuclease activities in a novel form of the cytolethal distending toxin. Toxins (Basel) 8 (5), 121. 10.3390/toxins8050121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mima K., Nishihara R., Qian Z. R., Cao Y., Sukawa Y., Nowak J. A., et al. (2016). Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut 65 (12), 1973–1980. 10.1136/gutjnl-2015-310101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Missailidis C., Hallqvist J., Qureshi A. R., Barany P., Heimburger O., Lindholm B., et al. (2016). Serum trimethylamine-N-oxide is strongly related to renal function and predicts outcome in chronic kidney disease. PloS One 11 (1), e0141738. 10.1371/journal.pone.0141738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroz M. S., Lajczak N. K., Goggins B. J., Keely S., Keely S. J. (2018). The bile acids, deoxycholic acid and ursodeoxycholic acid, regulate colonic epithelial wound healing. Am. J. Physiol. Gastrointest. Liver Physiol. 314 (3), G378–G387. 10.1152/ajpgi.00435.2016 [DOI] [PubMed] [Google Scholar]
- Murphy E. F., Cotter P. D., Healy S., Marques T. M., O’Sullivan O., Fouhy F., et al. (2010). Composition and energy harvesting capacity of the gut microbiota: Relationship to diet, obesity and time in mouse models. Gut 59 (12), 1635–1642. 10.1136/gut.2010.215665 [DOI] [PubMed] [Google Scholar]
- Murphy N., Norat T., Ferrari P., Jenab M., Bueno-de-Mesquita B., Skeie G., et al. (2012). Dietary fibre intake and risks of cancers of the colon and rectum in the European Prospective Investigation into Cancer and Nutrition (EPIC). PloS One 7 (6), e39361. 10.1371/journal.pone.0039361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy N., Norat T., Ferrari P., Jenab M., Bueno-de-Mesquita B., Skeie G., et al. (2013). Consumption of dairy products and colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). PloS One 8 (9), e72715–e72715. 10.1371/journal.pone.0072715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naito Y., Uchiyama K., Takagi T. (2018). A next-generation beneficial microbe: Akkermansia muciniphila. J. Clin. Biochem. Nutr. 63 (1), 33–35. 10.3164/jcbn.18-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T. L., Vieira-Silva S., Liston A., Raes J. (2015). How informative is the mouse for human gut microbiota research? Dis. Model Mech. 8 (1), 1–16. 10.1242/dmm.017400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T. T., Ung T. T., Kim N. H., Jung Y. D. (2018). Role of bile acids in colon carcinogenesis. World J. Clin. cases 6 (13), 577–588. 10.12998/wjcc.v6.i13.577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L. H., Ma W., Wang D. D., Cao Y., Mallick H., Gerbaba T. K., et al. (2020). Association between sulfur-metabolizing bacterial communities in stool and risk of distal colorectal cancer in men. Gastroenterology 158 (5), 1313–1325. 10.1053/j.gastro.2019.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitter M., Norgård B., de Vogel S., Eussen S. J. P. M., Meyer K., Ulvik A., et al. (2014). Plasma methionine, choline, betaine, and dimethylglycine in relation to colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Ann. Oncol. 25 (8), 1609–1615. 10.1093/annonc/mdu185 [DOI] [PubMed] [Google Scholar]
- Nojadeh J. N., Behrouz Sharif S., Sakhinia E. (2018). Microsatellite instability in colorectal cancer. EXCLI J. 17, 159–168. 10.17179/excli2017-948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obregon-Tito A. J., Tito R. Y., Metcalf J., Sankaranarayanan K., Clemente J. C., Ursell L. K., et al. (2015). Subsistence strategies in traditional societies distinguish gut microbiomes. Nat. Commun. 6 (1), 6505. 10.1038/ncomms7505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ocvirk S., O’Keefe S. J. (2017). Influence of bile acids on colorectal cancer risk: Potential mechanisms mediated by diet - gut microbiota interactions. Curr. Nutr. Rep. 6 (4), 315–322. 10.1007/s13668-017-0219-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olén O., Erichsen R., Sachs M. C., Pedersen L., Halfvarson J., Askling J., et al. (2020). Colorectal cancer in Crohn’s disease: A Scandinavian population-based cohort study. Lancet Gastroenterol. Hepatol. 5 (5), 475–484. 10.1016/S2468-1253(20)30005-4 [DOI] [PubMed] [Google Scholar]
- Oostindjer M., Alexander J., Amdam G. V., Andersen G., Bryan N. S., Chen D., et al. (2014). The role of red and processed meat in colorectal cancer development: A perspective. Meat Sci. 97 (4), 583–596. 10.1016/j.meatsci.2014.02.011 [DOI] [PubMed] [Google Scholar]
- O’Keefe S. J. D., Li J. V., Lahti L., Ou J., Carbonero F., Mohammed K., et al. (2015). Fat, fibre and cancer risk in African Americans and rural Africans. Nat. Commun. 6 (1), 6342. 10.1038/ncomms7342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Othman E. M., Leyh A., Stopper H. (2013). Insulin mediated DNA damage in mammalian colon cells and human lymphocytes in vitro. Mutat. Res. 745-746, 34–39. 10.1016/j.mrfmmm.2013.03.006 [DOI] [PubMed] [Google Scholar]
- Othman E. M., Hintzsche H., Stopper H. (2014). Signaling steps in the induction of genomic damage by insulin in colon and kidney cells. Free Radic. Biol. Med. 68, 247–257. 10.1016/j.freeradbiomed.2013.12.010 [DOI] [PubMed] [Google Scholar]
- Ou J., DeLany J. P., Zhang M., Sharma S., O’Keefe S. J. (2012). Association between low colonic short-chain fatty acids and high bile acids in high colon cancer risk populations. Nutr. Cancer. 64 (1), 34–40. 10.1080/01635581.2012.630164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou J., Carbonero F., Zoetendal E. G., DeLany J. P., Wang M., Newton K., et al. (2013). Diet, microbiota, and microbial metabolites in colon cancer risk in rural Africans and African Americans. Am. J. Clin. Nutr. 98 (1), 111–120. 10.3945/ajcn.112.056689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco L. S., Anderson C. A. M., Lacey J. V., Jr., Giovannucci E. L., Lemus H., Araneta M. R. G., et al. (2019). Sugar-sweetened beverages and colorectal cancer risk in the California Teachers Study. PloS One 14 (10), e0223638. 10.1371/journal.pone.0223638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padidar S., Farquharson A. J., Williams L. M., Kearney R., Arthur J. R., Drew J. E. (2012). High-fat diet alters gene expression in the liver and colon: Links to increased development of aberrant crypt foci. Dig. Dis. Sci. 57 (7), 1866–1874. 10.1007/s10620-012-2092-9 [DOI] [PubMed] [Google Scholar]
- Parnaud G., Pignatelli B., Peiffer G., Taché S., Corpet D. E. (2000). Endogenous N-nitroso compounds, and their precursors, present in bacon, do not initiate or promote aberrant crypt foci in the colon of rats. Nutr. Cancer. 38 (1), 74–80. 10.1207/S15327914NC381_11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasquereau-Kotula E., Martins M., Aymeric L., Dramsi S. (2018). Significance of Streptococcus gallolyticus subsp. gallolyticus association with colorectal cancer. Front. Microbiol. 9, 614. 10.3389/fmicb.2018.00614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne A. N., Chassard C., Lacroix C. (2012). Gut microbial adaptation to dietary consumption of fructose, artificial sweeteners and sugar alcohols: Implications for host-microbe interactions contributing to obesity. Obes Rev. 13 (9), 799–809. 10.1111/j.1467-789X.2012.01009.x [DOI] [PubMed] [Google Scholar]
- Peiro-Jordan R., Krishna-Subramanian S., Hanski M. L., Luscher-Firzlaff J., Zeitz M., Hanski C. (2012). The chemopreventive agent ursodeoxycholic acid inhibits proliferation of colon carcinoma cells by suppressing c-Myc expression. Eur. J. Cancer Prev. 21 (5), 413–422. 10.1097/CEJ.0b013e32834ef16f [DOI] [PubMed] [Google Scholar]
- Pfalzer A. C., Leung K., Crott J. W., Kim S. J., Tai A. K., Parnell L. D., et al. (2018). Incremental elevations in TNFα and IL6 in the human colon and procancerous changes in the mucosal transcriptome accompany adiposity. Cancer Epidemiol. Biomarkers Prev. 27 (12), 1416–1423. 10.1158/1055-9965.Epi-18-0121 [DOI] [PubMed] [Google Scholar]
- Pham N. M., Mizoue T., Tanaka K., Tsuji I., Tamakoshi A., Matsuo K., et al. (2013). Fish consumption and colorectal cancer risk: An evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn. J. Clin. Oncol. 43 (9), 935–941. 10.1093/jjco/hyt094 [DOI] [PubMed] [Google Scholar]
- Pierre F. H., Santarelli R. L., Allam O., Tache S., Naud N., Gueraud F., et al. (2010). Freeze-dried ham promotes azoxymethane-induced mucin-depleted foci and aberrant crypt foci in rat colon. Nutr. Cancer. 62 (5), 567–573. 10.1080/01635580903532408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierre F. H. F., Martin O. C. B., Santarelli R. L., Taché S., Naud N., Guéraud F., et al. (2013). Calcium and α-tocopherol suppress cured-meat promotion of chemically induced colon carcinogenesis in rats and reduce associated biomarkers in human volunteers. Am. J. Clin. Nutr. 98 (5), 1255–1262. 10.3945/ajcn.113.061069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzyk Ł. (2017). Food properties and dietary habits in colorectal cancer prevention and development. Int. J. Food Prop. 20 (10), 2323–2343. 10.1080/10942912.2016.1236813 [DOI] [Google Scholar]
- Piewngam P., Zheng Y., Nguyen T. H., Dickey S. W., Joo H.-S., Villaruz A. E., et al. (2018). Pathogen elimination by probiotic Bacillus via signalling interference. Nature 562 (7728), 532–537. 10.1038/s41586-018-0616-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponzetto A., Figura N. (2019). Colon cancer risk and vaca toxin of helicobacter pylori. Gastroenterology 156 (8), 2356. 10.1053/j.gastro.2018.11.083 [DOI] [PubMed] [Google Scholar]
- Pou S. A., Diaz Mdel P., Osella A. R. (2012). Applying multilevel model to the relationship of dietary patterns and colorectal cancer: An ongoing case-control study in Cordoba, Argentina. Eur. J. Nutr. 51 (6), 755–764. 10.1007/s00394-011-0255-7 [DOI] [PubMed] [Google Scholar]
- Pouncey A. L., Scott A. J., Alexander J. L., Marchesi J., Kinross J. (2018). Gut microbiota, chemotherapy and the host: The influence of the gut microbiota on cancer treatment. Ecancermedicalscience 12, 868. 10.3332/ecancer.2018.868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prorok-Hamon M., Friswell M. K., Alswied A., Roberts C. L., Song F., Flanagan P. K., et al. (2014). Colonic mucosa-associated diffusely adherent afaC+ Escherichia coli expressing lpfA and pks are increased in inflammatory bowel disease and colon cancer. Gut 63 (5), 761–770. 10.1136/gutjnl-2013-304739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protiva P., Pendyala S., Nelson C., Augenlicht L. H., Lipkin M., Holt P. R. (2016). Calcium and 1,25-dihydroxyvitamin D3 modulate genes of immune and inflammatory pathways in the human colon: A human crossover trial. Am. J. Clin. Nutr. 103 (5), 1224–1231. 10.3945/ajcn.114.105304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell R. V., Pearson J., Aitchison A., Dixon L., Frizelle F. A., Keenan J. I. (2017). Colonization with enterotoxigenic Bacteroides fragilis is associated with early-stage colorectal neoplasia. PloS One 12 (2), e0171602–e0171602. 10.1371/journal.pone.0171602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiao D., Gaitonde S. V., Qi W., Martinez J. D. (2001). Deoxycholic acid suppresses p53 by stimulating proteasome-mediated p53 protein degradation. Carcinogenesis 22 (6), 957–964. 10.1093/carcin/22.6.957 [DOI] [PubMed] [Google Scholar]
- Raisch J., Rolhion N., Dubois A., Darfeuille-Michaud A., Bringer M.-A. (2015). Intracellular colon cancer-associated Escherichia coli promote protumoral activities of human macrophages by inducing sustained COX-2 expression. Lab. Invest. 95 (3), 296–307. 10.1038/labinvest.2014.161 [DOI] [PubMed] [Google Scholar]
- Rampelli S., Schnorr S. L., Consolandi C., Turroni S., Severgnini M., Peano C., et al. (2015). Metagenome sequencing of the Hadza hunter-gatherer gut microbiota. Curr. Biol. 25 (13), 1682–1693. 10.1016/j.cub.2015.04.055 [DOI] [PubMed] [Google Scholar]
- Raufman J.-P., Shant J., Guo C. Y., Roy S., Cheng K. (2008). Deoxycholyltaurine rescues human colon cancer cells from apoptosis by activating EGFR-dependent PI3K/Akt signaling. J. Cell. Physiol. 215 (2), 538–549. 10.1002/jcp.21332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawla P., Sunkara T., Barsouk A. (2019). Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Prz Gastroenterol. 14 (2), 89–103. 10.5114/pg.2018.81072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray D., Kidane D. (2016). Gut microbiota imbalance and base excision repair dynamics in colon cancer. J. Cancer. 7 (11), 1421–1430. 10.7150/jca.15480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds I. S., O’Toole A., Deasy J., McNamara D. A., Burke J. P. (2017). A meta-analysis of the clinicopathological characteristics and survival outcomes of inflammatory bowel disease associated colorectal cancer. Int. J. Colorectal Dis. 32 (4), 443–451. 10.1007/s00384-017-2754-3 [DOI] [PubMed] [Google Scholar]
- Rezasoltani S., Asadzadeh Aghdaei H., Dabiri H., Akhavan Sepahi A., Modarressi M. H., Nazemalhosseini Mojarad E. (2018). The association between fecal microbiota and different types of colorectal polyp as precursors of colorectal cancer. Microb. Pathog. 124, 244–249. 10.1016/j.micpath.2018.08.035 [DOI] [PubMed] [Google Scholar]
- Ribière C., Peyret P., Parisot N., Darcha C., Déchelotte P. J., Barnich N., et al. (2016). Oral exposure to environmental pollutant benzo[a]pyrene impacts the intestinal epithelium and induces gut microbial shifts in murine model. Sci. Rep. 6, 31027. 10.1038/srep31027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridlon J. M., Harris S. C., Bhowmik S., Kang D.-J., Hylemon P. B. (2016). Consequences of bile salt biotransformations by intestinal bacteria. Gut Microbes. 7 (1), 22–39. 10.1080/19490976.2015.1127483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrmann S., Hermann S., Linseisen J. (2009). Heterocyclic aromatic amine intake increases colorectal adenoma risk: Findings from a prospective European cohort study. Am. J. Clin. Nutr. 89 (5), 1418–1424. 10.3945/ajcn.2008.26658 [DOI] [PubMed] [Google Scholar]
- Rohrmann S., Linseisen J., Allenspach M., von Eckardstein A., Müller D. (2015). Plasma concentrations of trimethylamine-N-oxide are directly associated with dairy food consumption and low-grade inflammation in a German adult population. J. Nutr. 146 (2), 283–289. 10.3945/jn.115.220103 [DOI] [PubMed] [Google Scholar]
- Romano K. A., Vivas E. I., Amador-Noguez D., Rey F. E. (2015). Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. mBio 6 (2), e02481–e02414. 10.1128/mBio.02481-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinstein M. R., Wang X., Liu W., Hao Y., Cai G., Han Y. W. (2013). Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe 14 (2), 195–206. 10.1016/j.chom.2013.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher J. U., Sczesnak A., Longman R. S., Segata N., Ubeda C., Bielski C., et al. (2013). Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife 2, e01202–e01202. 10.7554/eLife.01202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz M. D., Atay Ç., Heringer J., Romrig F. K., Schwitalla S., Aydin B., et al. (2014). High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity. Nature 514 (7523), 508–512. 10.1038/nature13398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebastian S., Hernández H. V., Myrelid P., Kariv R., Tsianos E., Toruner M., et al. (2014). Colorectal cancer in inflammatory bowel disease: results of the 3rd ECCO pathogenesis scientific workshop (I). J. Crohns Colitis 8 (1), 5–18. 10.1016/j.crohns.2013.04.008 [DOI] [PubMed] [Google Scholar]
- Segata N. (2015). Gut microbiome: Westernization and the disappearance of intestinal diversity. Curr. Biol. 25 (14), R611–R613. 10.1016/j.cub.2015.05.040 [DOI] [PubMed] [Google Scholar]
- Seldin M. M., Meng Y., Qi H., Zhu W., Wang Z., Hazen S. L., et al. (2016). Trimethylamine N-oxide promotes vascular inflammation through signaling of mitogen-activated protein kinase and nuclear factor- κB. J. Am. Heart Assoc. 5 (2), e002767. 10.1161/jaha.115.002767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senthong V., Wang Z., Li Xinmin S., Fan Y., Wu Y., Wilson Tang W. H., et al. (2016). Intestinal microbiota-generated metabolite trimethylamine-N-oxide and 5-year mortality risk in stable coronary artery disease: The contributory role of intestinal microbiota in a COURAGE-like patient cohort. J. Am. Heart Assoc. 5 (6), e002816. 10.1161/JAHA.115.002816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serfaty L., Bissonnette M., Poupon R. (2010). Ursodeoxycholic acid and chemoprevention of colorectal cancer. Gastroenterol. Clin. Biol. 34 (10), 516–522. 10.1016/j.gcb.2010.05.005 [DOI] [PubMed] [Google Scholar]
- Servin A. L. (2014). Pathogenesis of human diffusely adhering Escherichia coli expressing Afa/Dr adhesins (Afa/Dr DAEC): Current insights and future challenges. Clin. Microbiol. Rev. 27 (4), 823–869. 10.1128/CMR.00036-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y., Hu J., Geng J., Hu T., Wang B., Yan W., et al. (2018). Berberine treatment reduces atherosclerosis by mediating gut microbiota in apoE-/- mice. Biomed. Pharmacother. 107, 1556–1563. 10.1016/j.biopha.2018.08.148 [DOI] [PubMed] [Google Scholar]
- Shi D.-S., Rhee K.-J., Eom Y.-B. (2020). Effect of probiotic Clostridium butyricum NCTC 7423 supernatant on biofilm formation and gene expression of Bacteroides Fragilis. J. Microbiol Biotechnol. 30 (3), 368–377. 10.4014/jmb.2001.01027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel R. L., Torre L. A., Soerjomataram I., Hayes R. B., Bray F., Weber T. K., et al. (2019). Global patterns and trends in colorectal cancer incidence in young adults. Gut 68 (12), 2179. 10.1136/gutjnl-2019-319511 [DOI] [PubMed] [Google Scholar]
- Sieri S., Krogh V., Agnoli C., Ricceri F., Palli D., Masala G., et al. (2015). Dietary glycemic index and glycemic load and risk of colorectal cancer: Results from the EPIC-Italy study. Int. J. Cancer. 136 (12), 2923–2931. 10.1002/ijc.29341 [DOI] [PubMed] [Google Scholar]
- Sieri S., Agnoli C., Pala V., Grioni S., Brighenti F., Pellegrini N., et al. (2017). Dietary glycemic index, glycemic load, and cancer risk: Results from the EPIC-Italy study. Sci. Rep. 7 (1), 9757. 10.1038/s41598-017-09498-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R., Peters U., Cross A. J., Kulldorff M., Weissfeld J. L., Pinsky P. F., et al. (2005). Meat, meat cooking methods and preservation, and risk for colorectal adenoma. Cancer Res. 65 (17), 8034–8041. 10.1158/0008-5472.CAN-04-3429 [DOI] [PubMed] [Google Scholar]
- Sivaprakasam S., Gurav A., Paschall A. V., Coe G. L., Chaudhary K., Cai Y., et al. (2016). An essential role of Ffar2 (Gpr43) in dietary fibre-mediated promotion of healthy composition of gut microbiota and suppression of intestinal carcinogenesis. Oncogenesis 5 (6), e238. 10.1038/oncsis.2016.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobhani I., Amiot A., Le Baleur Y., Levy M., Auriault M.-L., Van Nhieu J. T., et al. (2013). Microbial dysbiosis and colon carcinogenesis: Could colon cancer be considered a bacteria-related disease? Therap Adv. Gastroenterol. 6 (3), 215–229. 10.1177/1756283X12473674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg P. (2019). Red meat-derived nitroso compounds, lipid peroxidation products and colorectal cancer. Foods 8 (7), 252. 10.3390/foods8070252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam S., Fletcher C. (2018). Trimethylamine N-oxide: Breathe new life. Br. J. Pharmacol. 175 (8), 1344–1353. 10.1111/bph.13959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugawara Y., Kuriyama S., Kakizaki M., Nagai M., Ohmori-Matsuda K., Sone T., et al. (2009). Fish consumption and the risk of colorectal cancer: The Ohsaki Cohort Study. Br. J. Cancer 101 (5), 849–854. 10.1038/sj.bjc.6605217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki T., Heaney L. M., Jones D. J. L., Ng L. L. (2020). Trimethylamine N-oxide and risk stratification after acute myocardial infarction. Clin. Chem. 63 (1), 420–428. 10.1373/clinchem.2016.264853 [DOI] [PubMed] [Google Scholar]
- Tahara T., Yamamoto E., Suzuki H., Maruyama R., Chung W., Garriga J., et al. (2014). Fusobacterium in colonic flora and molecular features of colorectal carcinoma. Cancer Res. 74 (5), 1311–1318. 10.1158/0008-5472.CAN-13-1865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tailford L. E., Crost E. H., Kavanaugh D., Juge N. (2015). Mucin glycan foraging in the human gut microbiome. Front. Genet. 6, 81:81. 10.3389/fgene.2015.00081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taira T., Yamaguchi S., Takahashi A., Okazaki Y., Yamaguchi A., Sakaguchi H., et al. (2015). Dietary polyphenols increase fecal mucin and immunoglobulin a and ameliorate the disturbance in gut microbiota caused by a high fat diet. J. Clin. Biochem. Nutr. 57 (3), 212–216. 10.3164/jcbn.15-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W. H. W., Wang Z., Levison B. S., Koeth R. A., Britt E. B., Fu X., et al. (2013). Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N. Engl. J. Med. 368 (17), 1575–1584. 10.1056/NEJMoa1109400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W. H., Wang Z., Fan Y., Levison B., Hazen J. E., Donahue L. M., et al. (2014). Prognostic value of elevated levels of intestinal microbe-generated metabolite trimethylamine-N-oxide in patients with heart failure: Refining the gut hypothesis. J. Am. Coll. Cardiol. 64 (18), 1908–1914. 10.1016/j.jacc.2014.02.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W. H., Wang Z., Kennedy D. J., Wu Y., Buffa J. A., Agatisa-Boyle B., et al. (2015). Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ. Res. 116 (3), 448–455. 10.1161/circresaha.116.305360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasevska N., Jiao L., Cross A. J., Kipnis V., Subar A. F., Hollenbeck A., et al. (2012). Sugars in diet and risk of cancer in the NIH-AARP Diet and Health Study. Int. J. Cancer. 130 (1), 159–169. 10.1002/ijc.25990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tayyem R. F., Bawadi H. A., Shehadah I. N., Abu-Mweis S. S., Agraib L. M., Bani-Hani K. E., et al. (2015). Macro- and micronutrients consumption and the risk for colorectal cancer among Jordanians. Nutrients 7 (3), 1769–1786. 10.3390/nu7031769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teimoorian F., Ranaei M., Hajian-Tilaki K., Shokri Shirvani J., Vosough Z. (2018). Association of Helicobacter pylori infection with colon cancer and adenomatous polyps. Iran J. Pathol. 13 (3), 325–332. [PMC free article] [PubMed] [Google Scholar]
- Tjalsma H., Boleij A., Marchesi J. R., Dutilh B. E. (2012). A bacterial driver-passenger model for colorectal cancer: Beyond the usual suspects. Nat. Rev. Microbiol. 10 (8), 575–582. 10.1038/nrmicro2819 [DOI] [PubMed] [Google Scholar]
- Troseid M., Ueland T., Hov J. R., Svardal A., Gregersen I., Dahl C. P., et al. (2015). Microbiota-dependent metabolite trimethylamine-N-oxide is associated with disease severity and survival of patients with chronic heart failure. J. Intern. Med. 277 (6), 717–726. 10.1111/joim.12328 [DOI] [PubMed] [Google Scholar]
- Tsoi H., Chu E. S. H., Zhang X., Sheng J., Nakatsu G., Ng S. C., et al. (2017). Peptostreptococcus anaerobius induces intracellular cholesterol biosynthesis in colon cells to induce proliferation and causes dysplasia in mice. Gastroenterology 152 (6), 1419–1433.e1415. 10.1053/j.gastro.2017.01.009 [DOI] [PubMed] [Google Scholar]
- Tunsjø H. S., Gundersen G., Rangnes F., Noone J. C., Endres A., Bemanian V. (2019). Detection of Fusobacterium nucleatum in stool and colonic tissues from norwegian colorectal cancer patients. Eur. J. Clin. Microbiol. Infect. Dis. 38 (7), 1367–1376. 10.1007/s10096-019-03562-7 [DOI] [PubMed] [Google Scholar]
- Turati F., Galeone C., Gandini S., Augustin L. S., Jenkins D. J., Pelucchi C., et al. (2015). High glycemic index and glycemic load are associated with moderately increased cancer risk. Mol. Nutr. Food Res. 59 (7), 1384–1394. 10.1002/mnfr.201400594 [DOI] [PubMed] [Google Scholar]
- Van de Wiele T., Vanhaecke L., Boeckaert C., Peru K., Headley J., Verstraete W., et al. (2005). Human colon microbiota transform polycyclic aromatic hydrocarbons to estrogenic metabolites. Environ. Health Perspect. 113 (1), 6–10. 10.1289/ehp.7259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega-López S., Venn B. J., Slavin J. L. (2018). Relevance of the glycemic index and glycemic load for body weight, diabetes, and cardiovascular disease. Nutrients 10 (10), 1361. 10.3390/nu10101361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasquez M. T., Ramezani A., Manal A., Raj D. S. (2016). Trimethylamine N-oxide: The good, the bad and the unknown. Toxins (Basel) 8 (11), 326. 10.3390/toxins8110326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigneri P. G., Tirrò E., Pennisi M. S., Massimino M., Stella S., Romano C., et al. (2015). The insulin/IGF system in colorectal cancer development and resistance to therapy. Front. Oncol. 5, 230. 10.3389/fonc.2015.00230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viljoen K. S., Dakshinamurthy A., Goldberg P., Blackburn J. M. (2015). Quantitative profiling of colorectal cancer-associated bacteria reveals associations between Fusobacterium spp., enterotoxigenic Bacteroides fragilis (ETBF) and clinicopathological features of colorectal cancer. PloS One 10 (3), e0119462–e0119462. 10.1371/journal.pone.0119462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villéger R., Lopès A., Carrier G., Veziant J., Billard E., Barnich N., et al. (2019). Intestinal microbiota: A novel target to improve anti-tumor treatment? Int. J. Mol. Sci. 20 (18), 4584. 10.3390/ijms20184584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuik F. E. R., Nieuwenburg S. A. V., Bardou M., Lansdorp-Vogelaar I., Dinis-Ribeiro M., Bento M. J., et al. (2019). Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 68 (10), 1820. 10.1136/gutjnl-2018-317592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall R., Ross R. P., Fitzgerald G. F., Stanton C. (2010). Fatty acids from fish: The anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr. Rev. 68 (5), 280–289. 10.1111/j.1753-4887.2010.00287.x [DOI] [PubMed] [Google Scholar]
- Wang X., Huycke M. M. (2007). Extracellular superoxide production by Enterococcus faecalis promotes chromosomal instability in mammalian cells. Gastroenterology 132 (2), 551–561. 10.1053/j.gastro.2006.11.040 [DOI] [PubMed] [Google Scholar]
- Wang X., Allen T. D., May R. J., Lightfoot S., Houchen C. W., Huycke M. M. (2008). Enterococcus faecalis induces aneuploidy and tetraploidy in colonic epithelial cells through a bystander effect. Cancer Res. 68 (23), 9909–9917. 10.1158/0008-5472.CAN-08-1551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J.-L., Lin Y.-W., Chen H.-M., Kong X., Xiong H., Shen N., et al. (2011). Calcium prevents tumorigenesis in a mouse model of colorectal cancer. PloS One 6 (8), e22566–e22566. 10.1371/journal.pone.0022566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Uchida K., Ohnaka K., Morita M., Toyomura K., Kono S., et al. (2014). Sugars, sucrose and colorectal cancer risk: The Fukuoka colorectal cancer study. Scand. J. Gastroenterol. 49 (5), 581–588. 10.3109/00365521.2013.822091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Bergeron N., Levison B. S., Li X. S., Chiu S., Jia X., et al. (2019). Impact of chronic dietary red meat, white meat, or non-meat protein on trimethylamine N-oxide metabolism and renal excretion in healthy men and women. Eur. Heart J. 40 (7), 583–594. 10.1093/eurheartj/ehy799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassenaar T. M. (2018). E. coli and colorectal cancer: A complex relationship that deserves a critical mindset. Crit. Rev. Microbiol. 44 (5), 619–632. 10.1080/1040841X.2018.1481013 [DOI] [PubMed] [Google Scholar]
- Wei Z., Cao S., Liu S., Yao Z., Sun T., Li Y., et al. (2016). Could gut microbiota serve as prognostic biomarker associated with colorectal cancer patients’ survival? A pilot study on relevant mechanism. Oncotarget 7 (29), 46158–46172. 10.18632/oncotarget.10064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams C. D., Satia J. A., Adair L. S., Stevens J., Galanko J., Keku T. O., et al. (2010). Associations of red meat, fat, and protein intake with distal colorectal cancer risk. Nutr. Cancer. 62 (6), 701–709. 10.1080/01635581003605938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson M. R., Jiang Y., Villalta P. W., Stornetta A., Boudreau P. D., Carrá A., et al. (2019). The human gut bacterial genotoxin colibactin alkylates DNA. Science 363 (6428), eaar7785. 10.1126/science.aar7785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter S. E., Winter M. G., Xavier M. N., Thiennimitr P., Poon V., Keestra A. M., et al. (2013). Host-derived nitrate boosts growth of E. coli in the inflamed gut. Science 339 (6120), 708–711. 10.1126/science.1232467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Cancer Research Fund/American Institute for Cancer Research (2018). Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report. Available at: dietandcancerreport.org. [Google Scholar]
- Wroblewski L. E., Peek R. M., Jr., Wilson K. T. (2010). Helicobacter pylori and gastric cancer: Factors that modulate disease risk. Clin. Microbiol. Rev. 23 (4), 713–739. 10.1128/CMR.00011-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Rhee K.-J., Zhang M., Franco A., Sears C. L. (2007). Bacteroides fragilis toxin stimulates intestinal epithelial cell shedding and gamma-secretase-dependent E-cadherin cleavage. J. Cell. Sci. 120 (Pt 11), 1944–1952. 10.1242/jcs.03455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Rhee K.-J., Albesiano E., Rabizadeh S., Wu X., Yen H.-R., et al. (2009). A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses.1. Nat. Med. 15 (9), 1016–1022. 10.1038/nm.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu G. D., Chen J., Hoffmann C., Bittinger K., Chen Y.-Y., Keilbaugh S. A., et al. (2011). Linking long-term dietary patterns with gut microbial enterotypes. Science 334 (6052), 105. 10.1126/science.1208344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Feng B., Li K., Zhu X., Liang S., Liu X., et al. (2012). Fish consumption and colorectal cancer risk in humans: A systematic review and meta-analysis. Am. J. Med. 125 (6), 551–559.e555. 10.1016/j.amjmed.2012.01.022 [DOI] [PubMed] [Google Scholar]
- Wu N., Yang X., Zhang R., Li J., Xiao X., Hu Y., et al. (2013). Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb. Ecol. 66 (2), 462–470. 10.1007/s00248-013-0245-9 [DOI] [PubMed] [Google Scholar]
- Wu D., Cao M., Peng J., Li N., Yi S., Song L., et al. (2017). The effect of trimethylamine N-oxide on Helicobacter pylori-induced changes of immunoinflammatory genes expression in gastric epithelial cells. Int. Immunopharmacol. 43, 172–178. 10.1016/j.intimp.2016.11.032 [DOI] [PubMed] [Google Scholar]
- Wu X., Wu Y., He L., Wu L., Wang X., Liu Z. (2018). Effects of the intestinal microbial metabolite butyrate on the development of colorectal cancer. J. Cancer. 9 (14), 2510–2517. 10.7150/jca.25324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R., Wang Q., Li L. (2015). A genome-wide systems analysis reveals strong link between colorectal cancer and trimethylamine N-oxide (TMAO), a gut microbial metabolite of dietary meat and fat. BMC Genomics 16 Suppl 7, S4. 10.1186/1471-2164-16-s7-s4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M., Cen M., Shen Y., Zhu Y., Cheng F., Tang L., et al. (2020). Deoxycholic acid-induced gut dysbiosis disrupts bile acid enterohepatic circulation and promotes intestinal inflammation. Dig. Dis. Sci. 10.1007/s10620-020-06208-3 [DOI] [PubMed] [Google Scholar]
- Yachida S., Mizutani S., Shiroma H., Shiba S., Nakajima T., Sakamoto T., et al. (2019). Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 25 (6), 968–976. 10.1038/s41591-019-0458-7 [DOI] [PubMed] [Google Scholar]
- Yang J., Yu J. (2018). The association of diet, gut microbiota and colorectal cancer: What we eat may imply what we get. Protein Cell. 9 (5), 474–487. 10.1007/s13238-018-0543-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Wang X., Moore D. R., Lightfoot S. A., Huycke M. M. (2012). Tnf-α mediates macrophage-induced bystander effects through Netrin-1. Cancer Res. 72 (20), 5219–5229. 10.1158/0008-5472.CAN-12-1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Weng W., Peng J., Hong L., Yang L., Toiyama Y., et al. (2017). Fusobacterium nucleatum increases proliferation of colorectal cancer cells and tumor development in mice by activating toll-like receptor 4 signaling to nuclear factor-κb, and up-regulating expression of microRNA-21. Gastroenterology 152 (4), 851–866.e824. 10.1053/j.gastro.2016.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon K., Kim N. (2018). The effect of microbiota on colon carcinogenesis. J. Cancer Prev. 23 (3), 117–125. 10.15430/JCP.2018.23.3.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu D. C., Waby J. S., Chirakkal H., Staton C. A., Corfe B. M. (2010). Butyrate suppresses expression of neuropilin I in colorectal cell lines through inhibition of Sp1 transactivation. Mol. Cancer. 9, 276. 10.1186/1476-4598-9-276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu D. C., Bury J. P., Tiernan J., Waby J. S., Staton C. A., Corfe B. M. (2011). Short-chain fatty acid level and field cancerization show opposing associations with enteroendocrine cell number and neuropilin expression in patients with colorectal adenoma. Mol. Cancer. 10, 27. 10.1186/1476-4598-10-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Feng Q., Wong S. H., Zhang D., Liang Q. Y., Qin Y., et al. (2017). Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut 66 (1), 70–78. 10.1136/gutjnl-2015-309800 [DOI] [PubMed] [Google Scholar]
- Yue C., Yang X., Li J., Chen X., Zhao X., Chen Y., et al. (2017). Trimethylamine N-oxide prime NLRP3 inflammasome via inhibiting ATG16L1-induced autophagy in colonic epithelial cells. Biochem. Biophys. Res. Commun. 490 (2), 541–551. 10.1016/j.bbrc.2017.06.075 [DOI] [PubMed] [Google Scholar]
- Yue Y., Ye K., Lu J., Wang X., Zhang S., Liu L., et al. (2020). Probiotic strain Lactobacillus plantarum YYC-3 prevents colon cancer in mice by regulating the tumour microenvironment. BioMed. Pharmacother. 127, 110159. 10.1016/j.biopha.2020.110159 [DOI] [PubMed] [Google Scholar]
- Zelinkova Z., Wenzl T. (2015). The occurrence of 16 EPA PAHs in food - a review. Polycycl Aromat Compd. 35 (2-4), 248–284. 10.1080/10406638.2014.918550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeller G., Tap J., Voigt A. Y., Sunagawa S., Kultima J. R., Costea P. I., et al. (2014). Potential of fecal microbiota for early-stage detection of colorectal cancer. Mol. Syst. Biol. 10 (11), 766. 10.15252/msb.20145645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng S., Shen W. H., Liu L. (2018). Senescence and cancer. Cancer Transl. Med. 4 (3), 70–74. 10.4103/ctm.ctm_22_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng H., Hamlin S., Safratowich B., Cheng W.-H., Johnson L. (2020). Superior inhibitory efficacy of butyrate over propionate and acetate against human colon cancer cell proliferation via cell cycle arrest and apoptosis. Curr. Dev. Nutr. 4 (suppl 2), 364–364. 10.1093/cdn/nzaa044063 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Hoffmeister M., Weck M. N., Chang-Claude J., Brenner H. (2012). Helicobacter pylori infection and colorectal cancer risk: Evidence from a large population-based case-control study in Germany. Am. J. Epidemiol. 175 (5), 441–450. 10.1093/aje/kwr331 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Zhao X., Zhu Y., Ma J., Ma H., Zhang H. (2018. a). Probiotic mixture protects dextran sulfate sodium-induced colitis by altering tight junction protein expressions and increasing Tregs. Mediators Inflamm. 2018, 9416391. 10.1155/2018/9416391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Aung K. M., Uhlin B. E., Wai S. N. (2018. b). Reversible senescence of human colon cancer cells after blockage of mitosis/cytokinesis caused by the CNF1 cyclomodulin from Escherichia coli. Sci. Rep. 8 (1), 17780. 10.1038/s41598-018-36036-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lacroix C., Wortmann E., Ruscheweyh H.-J., Sunagawa S., Sturla S. J., et al. (2019). Gut microbial beta-glucuronidase and glycerol/diol dehydratase activity contribute to dietary heterocyclic amine biotransformation. BMC Microbiol. 19 (1), 99. 10.1186/s12866-019-1483-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Z., Feng Q., Yin Z., Shuang J., Bai B., Yu P., et al. (2017). Red and processed meat consumption and colorectal cancer risk: A systematic review and meta-analysis. Oncotarget 8 (47), 83306–83314. 10.18632/oncotarget.20667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Luo Y., Lv Y., Huang C., Sheng Q., Zhao P., et al. (2017). Clostridium difficile colonization in preoperative colorectal cancer patients. Oncotarget 8 (7), 11877–11886. 10.18632/oncotarget.14424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X., Fang Y.-J., Pan Z.-Z., Li B., Wang L., Zheng M.-C., et al. (2013). Dietary fat, fatty acid intakes and colorectal cancer risk in Chinese adults: A case–control study. Eur. J. Cancer Prev. 22 (5), 438–447. 10.1097/CEJ.0b013e32835e88c4 [DOI] [PubMed] [Google Scholar]
- Zhou Y., He H., Xu H., Li Y., Li Z., Du Y., et al. (2016). Association of oncogenic bacteria with colorectal cancer in South China. Oncotarget 7 (49), 80794–80802. 10.18632/oncotarget.13094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou D., Pan Q., Xin F.-Z., Zhang R.-N., He C.-X., Chen G.-Y., et al. (2017). Sodium butyrate attenuates high-fat diet-induced steatohepatitis in mice by improving gut microbiota and gastrointestinal barrier. World J. Gastroenterol. 23 (1), 60–75. 10.3748/wjg.v23.i1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q., Shen Z.-F., Wu B.-S., Xu C.-B., He Z.-Q., Chen T., et al. (2019). Risk of colorectal cancer in ulcerative colitis patients: A systematic review and meta-analysis. Gastroenterol. Res. Pract. 2019, 5363261. 10.1155/2019/5363261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Wang P. P., Zhao J., Green R., Sun Z., Roebothan B., et al. (2014). Dietary N-nitroso compounds and risk of colorectal cancer: A case-control study in Newfoundland and Labrador and Ontario, Canada. Br. J. Nutr. 111 (6), 1109–1117. 10.1017/S0007114513003462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou S., Fang L., Lee M.-H. (2018). Dysbiosis of gut microbiota in promoting the development of colorectal cancer. Gastroenterol. Rep. (Oxf) 6 (1), 1–12. 10.1093/gastro/gox031 [DOI] [PMC free article] [PubMed] [Google Scholar]