Abstract
Objectives/Hypothesis
Olfactory dysfunction has been observed as one of the clinical manifestations in COVID‐19 patients. We aimed to conduct a systematic review and meta‐analysis to estimate the overall pooled prevalence of olfactory dysfunction in COVID‐19 patients.
Study Design
Systematic review and meta‐analyses.
Methods
PubMed, Scopus, Web of Science, Embase, and Google Scholar databases were searched to identify studies published between 1 December 2019 and 23 July 2020. We used random‐effects model to estimate the pooled prevalence with 95% confidence intervals (CIs). Heterogeneity was assessed using the I 2 statistic and Cochran's Q test. Robustness of the pooled estimates was checked by different subgroup and sensitivity analyses This study is registered with PROSPERO (CRD42020183768).
Results
We identified 1162 studies, of which 83 studies (n = 27492, 61.4% female) were included in the meta‐analysis. Overall, the pooled prevalence of olfactory dysfunction in COVID‐19 patients was 47.85% [95% CI: 41.20–54.50]. We observed olfactory dysfunction in 54.40% European, 51.11% North American, 31.39% Asian, and 10.71% Australian COVID‐19 patients. Anosmia, hyposmia, and dysosmia were observed in 35.39%, 36.15%, and 2.53% of the patients, respectively. There were discrepancies in the results of studies with objective (higher prevalence) versus subjective (lower prevalence) evaluations. The discrepancy might be due to false‐negative reporting observed in self‐reported health measures.
Conclusions
The prevalence of olfactory dysfunction in COVID‐19 patients was found to be 47.85% based on high‐quality evidence. Due to the subjective measures of most studies pooled in the analysis, further studies with objective measures are advocated to confirm the finding.
Level of Evidence
2 Laryngoscope, 131:865–878, 2021
Keywords: Coronavirus, COVID‐19, olfactory, smell, meta‐analysis
INTRODUCTION
The world has recently been afflicted by severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2), which causes coronavirus disease 2019 (COVID‐19). China witnessed the first case of pneumonia of unknown origin reported on 8th December 2019 from Wuhan City, Hubei province, 1 and within a very short period, it started to spread globally. World Health Organization (WHO) declared COVID‐19 a public health emergency of international concern on 30th January 2020 and a global pandemic disease on 11th March 2020. As of 23rd October 2020, it has become a global pandemic with over 1.1 million deaths and 41.5 million confirmed cases worldwide. 2 As its nature and characteristics are unknown, understanding its presenting symptoms may help in earlier diagnosis. Current accumulated data indicate fever, cough, dyspnea, myalgia, arthralgia, and diarrhea to be the most predominant symptoms of SARS‐CoV‐2 infection. 1 , 3
Initially, a handful of studies reported the observation of olfactory dysfunction in COVID‐19 patients. 4 , 5 , 6 Following that the Ear, Nose, and Throat Society of UK and British Rhinological Society came up with an anecdotal report on the association between SARS‐CoV‐2 infection and olfactory dysfunction, in addition to urging new‐onset anosmia to be investigated for SARS‐CoV‐2 infection while taking precautionary isolation. 7 Similarly, the American Academy of Otolaryngology on 22 March 2020 advocated anosmia, hyposmia, and dysgeusia to be added as symptoms upon screening for COVID‐19 with measure such as precautionary isolation advised. 8 With the mounting evidence of olfactory dysfunction as a plausible symptom of COVID‐19, the Centers for Disease Control and Prevention has added olfactory dysfunction as part of COVID‐19's list of presenting symptoms. 9
With more cases being reported, 10 it is becoming apparent that the prevalence of olfactory dysfunction in COVID‐19 patients varies widely across the range. An earlier meta‐analysis by Tong et al. 11 revealed the prevalence of olfactory dysfunction in COVID‐19 patients was 52.73% based on 10 studies with 1627 patients available at that time. Remarkably, the authors stated that this figure is an underestimation due to the different type of assessment tools, which may be compounded by the smaller number of studies. Hence, another meta‐analysis evaluating newer available studies and a larger pool of patients is required to present a more representative figure of the global prevalence of olfactory dysfunction among COVID‐19 patients.
MATERIALS AND METHODS
We conducted a systematic review and meta‐analysis of the literature in accordance with the PRISMA guideline to identify studies that presented the prevalence of olfactory dysfunction in patients with COVID‐19, worldwide. 12 This study is registered with PROSPERO, number CRD42020183768.
Data Sources and Searches
PubMed, Scopus, Web of Science, Embase, and Google Scholar databases were searched to identify studies published between 1 December 2019 and 23 July 2020 without language restrictions. The following key terms were searched: coronavirus, COVID‐19, COVID19, nCoV, SARS‐CoV‐2, SARS‐CoV2, olfaction, olfactory, smell, anosmia, hyposmia, dysosmia, cacosmia, and parosmia. Complete details of the search strategy are in the Supporting Table 1. In addition to the published studies, preprints were also considered if data of interest were reported. Review articles, case reports, opinions, and perspectives were excluded. Data reported by news reports and press releases or data collected from websites or databases were not considered. To ensure a robust search procedure, references of the included studies were also reviewed. Duplicate studies were excluded by using EndNote X8 software.
Study Selection
To identify eligible studies, articles of interest were screened based on the title and abstract, followed by full text by two authors (J.S. and M.A.I.) independently. Disagreements about inclusion were discussed and resolved by consensus.
Data Extraction and Quality Assessment
Data extraction was done independently by two authors (J.S. and M.A.I.). From each eligible study, we extracted the following information into a predefined Excel spreadsheet: first author's last name; study design; country of the participants; data collection period; total number of COVID‐19 patients; number of female COVID‐19 patients; age; COVID‐19 confirmation procedure; confirmatory procedure of olfactory dysfunction; olfactory symptoms after the onset of illness; and number of recovered patients from olfactory dysfunction.
Random‐effects model was used to obtain the pooled prevalence and 95% confidence intervals (CIs) of olfactory dysfunction in patients with COVID‐19. The quality of included studies was assessed independently by two authors (J.S. and M.A.I.) using the Joanna Briggs Institute (JBI) critical appraisal tools. 13 The studies were classified as low‐quality (high‐risk of bias) if the overall score was ≤50%. 14 To assess publication bias, a funnel plot presenting prevalence estimate against the standard error was constructed and the asymmetry of the funnel plot was confirmed with Egger's test.
Data Synthesis and Analysis
Heterogeneity between studies was assessed using the I 2 statistic (I 2 > 75% indicating substantial heterogeneity) in addition to using the Cochran's Q test to identify the significance of heterogeneity. As subgroups, the prevalence of olfactory dysfunction in COVID‐19 patients from different geographical regions and in different types, including anosmia, hyposmia, and dysosmia were analyzed. To identify the source of heterogeneity and to check the robustness of the results, sensitivity analyses were performed through the following strategies: i) excluding small studies (n < 100); ii) excluding the low‐quality studies (high‐risk of bias); iii) excluding studies not reporting COVID‐19 confirmation assay; iv) considering only cross‐sectional studies, and v) excluding outlier studies. In addition, to identify the outlier studies and the sources of heterogeneity, a Galbraith plot was constructed. All the analyses and plots were generated by using metaprop codes in meta (version 4.11–0) and metafor (version 2.4–0) packages of R (version 3.6.3) in RStudio (version 1.2.5033). 15
RESULTS
Study Selection
Our search initially identified 1162 studies. After removing 738 studies [duplicate studies (n = 631), review articles (n = 69), case reports (n = 19), and non‐human studies (n = 19)]; titles and abstracts of 424 studies were screened for eligibility, of which 341 studies were excluded as those did not comply with the objective of this study. Therefore, 83 studies were included in the systematic review and meta‐analysis (Fig. 1).
Fig 1.
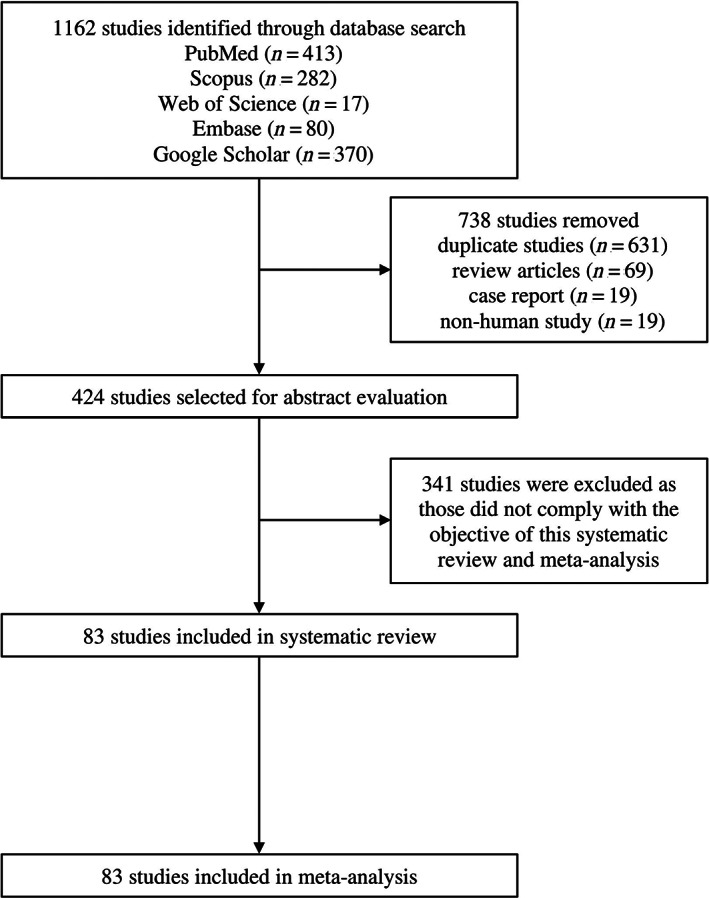
PRISMA flow diagram of study selection.
Study Characteristics
Detailed characteristics and references of the included studies are presented in Table I. Overall, this meta‐analysis reports data from 27492 COVID‐19 patients (61.4% female). Ages of the COVID‐19 patients included in this meta‐analysis ranged from 28.0 ± 16.4 to 70.2 ± 13.9 years. Studies were from 27 countries, including Spain, Germany, Italy, France, Ireland, Belgium, Romania, Switzerland, UK, Netherlands, Poland, Israel, China, Saudi Arabia, Turkey, Iraq, Iran, Pakistan, Singapore, Korea, Uruguay, Argentina, Bolivia, Venezuela, Australia, Canada, and USA. Among the included studies, 97.5% confirmed COVID‐19 patients by using the RT‐PCR method, whereas the method was not reported in two of the studies.
TABLE I.
Major Characteristics of the Included Studies.
| No. | Study IDReference | Study Design | Country | Data Collection Period | Total Number of COVID‐19 Patients (Female) | Age (years) (Mean ± SD/Median (IQR)/Range | COVID‐19 Confirmation Procedure | Type of Assessment for Olfactory Dysfunction (Subjective/Objective) | Method of Assessment for Olfactory Dysfunction |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Abalo‐Lojo 2020 16 | Cross‐sectional | Spain | NR | 131 (75) | 50.4 ± NR | RT‐PCR | Subjective | Self‐reported |
| 2 | Agarwal 2020 17 | Cross‐sectional | USA | 1 March–4 April 2020 | 16 (4) | 67.0 (38.0–95.0) | RT‐PCR | NR | NR |
| 3 | Alshami 2020 18 | Cross‐sectional | Saudi Arabia | 16 March–18 April 2020 | 128 (69) | 39.6 ± 15.5 | RT‐PCR | Subjective | Telephone questionnaire survey |
| 4 | Altin 2020 19 | Case–control | Turkey | 25 March–20 April 2020 | 81 (40) | 54.1 ± 16.9 | RT‐PCR | Objective | Sniffin' Sticks test |
| 5 | Beltrán‐Corbellini 2020 20 | Case–control | Spain | 23–25 March 2020 | 79 (31) | 61.6 ± 17.4 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 6 | Biadsee 2020 21 | Cross‐sectional | Israel | 25 March–15 April 2020 | 128 (70) | 36.2 ± NR | RT‐PCR | Subjective | Telephone questionnaire survey |
| 7 | Brandsetter 2020 22 | Cross‐sectional | Germany | NR | 31 (26) | 18.0–65.0 | RT‐PCR | Subjective | Self‐reported |
| 8 | Carignan 2020 23 | Case–control | Canada | 10–23 March 2020 | 134 (81) | 57.2 (42.6–64.4) | RT‐PCR | Subjective | Telephone interview |
| 9 | Cervilla 2020 24 | Cross‐sectional | Spain | March–May 2020 | 51 (44) | 43.8 ± 10.7 | RT‐PCR | Subjective | Telephone questionnaire survey |
| 10 | Chary 2020 25 | Cross‐sectional | France | 25 March–18 April 2020 | 115 (81) | 47.0 (20.0–83.0) | RT‐PCR | Subjective | Telephone interview |
| 11 | Chiesa‐Estomba 2020 26 | Cross‐sectional | Spain, Uruguay, Argentina, and Venezuela | NR | 542 (324) | 34.0 ± 11.0 | RT‐PCR | Subjective | Online questionnaire survey |
| 12 | Chiesa‐Estomba 2020a 27 | Cross‐sectional | Spain, Belgium, France, Canada, and UK | NR | 751 (477) | 41.0 ± 13.0 | RT‐PCR | Subjective | Online questionnaire survey |
| 13 | Chua 2020 28 | Cross‐sectional | Singapore | 23 March–4 April 2020 | 31 (NR) | NR | RT‐PCR | Subjective | Self‐reported |
| 14 | D'Ascanio 2020 29 | Cross‐sectional | Italy | 1 February–24 April | 43 (14) | 58.1 ± 15.7 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 15 | Dawson 2020 30 | Cross‐sectional | USA | March–April 2020 | 42 (NR) | NR | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 16 | De Maria 2020 31 | Cross‐sectional | Italy | NR | 95 (NR) | NR | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 17 | Dell'Era 2020 32 | Cross‐sectional | Italy | 10–30 March 2020 | 355 (163) | 50.0 (40.0–59.5) | RT‐PCR | Subjective | In person interview or telephone questionnaire survey |
| 18 | Durrani 2020 33 | Cross‐sectional | Pakistan | 20 March–10 April 2020 | 30 (6) | 44.0 (7.0–81.0) | RT‐PCR | Subjective | Self‐reported |
| 19 | Freni 2020 34 | Cross‐sectional | Italy | NR | 50 (20) | 37.7 ± 17.9 | RT‐PCR | Subjective | Online questionnaire survey |
| 20 | Gelardi 2020 35 | Cross‐sectional | Italy | NR | 72 (33) | 49.7 (19.0–70.0) | RT‐PCR | Subjective | Self‐reported |
| 21 | Giacomelli 2020 4 | Cross‐sectional | Italy | 19 March 2020 | 59 (19) | 60.0 (50.0–74.0) | NR | Subjective | Self‐reported questionnaire survey |
| 22 | Gorzkowski 2020 36 | Cross‐sectional | France | 1 March–31 March 2020 | 229 (147) | 39.7 ± 13.7 | RT‐PCR | Subjective | Telephone questionnaire survey |
| 23 | Güner 2020 37 | Cross‐sectional | Turkey | 10 March–10 April 2020 | 222 (90) | 50.6 ± 16.5 | RT‐PCR | Subjective | Self‐reported |
| 24 | Haehner 2020 38 | Cross‐sectional | Germany | NR | 34 (16) | 43.2 ± 11.6 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 25 | Hintschih 2020 39 | Cross‐sectional | Germany | NR | 41 (28) | 37 (NR) | RT‐PCR | Subjective | Online questionnaire survey |
| 26 | Hornuss 2020 40 | Cross‐sectional | Germany | April 2020 | 45 (20) | 56.0 ± 16.9 | RT‐PCR | Objective | Sniffin' Sticks test |
| 27 | Jalessi 2020 41 | Cross‐sectional | Iran | February–March 2020 | 92 (30) | 52.9 ± 13.2 | RT‐PCR | Subjective | Self‐reported |
| 28 | Karadaş 2020 42 | Cross‐sectional | Turkey | April–May 2020 | 239 (106) | 46.4 ± 15.4 | RT‐PCR | Subjective | Self‐reported |
| 29 | Kerr 2020 43 | Cross‐sectional | Ireland | 24 March 2020 | 46 (27) | 36.5 (27.0–48.0) | RT‐PCR | Subjective | Self‐reported |
| 30 | Kim 2020 44 | Cross‐sectional | Korea | 12–16 March 2020 | 172 (106) | 26.0 (22.0–47.0) | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 31 | Klopfenstein 2020 45 | Cross‐sectional | France | 1–17 March 2020 | 114 (36) | 47.0 ± 16.0) | RT‐PCR | NR | NR |
| 32 | Lapostolle 2020 46 | Cross‐sectional | France | 24 March–6 April 2020 | 1487 (752) | 44.0 (32.0–57.0) | RT‐PCR | Subjective | Telephone interview |
| 33 | Lazar 2020 47 | Cross‐sectional | Romania | 28 March 2020 | 100 (49) | 41.0 (NR) | RT‐PCR | Subjective | Medical record review |
| 34 | Lechien 2020 48 | Cross‐sectional | France, Italy, Spain, Belgium, and Switzerland | 22 March–10 April 2020 | 1420 (962) | 39.0 ± 12.0 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 35 | Lechien 2020a 49 | Cross‐sectional | Belgium | NR | 86 (56) | 41.7 ± 11.8 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 36 | Lechien 2020b 50 | Cross‐sectional | European countries | 22 March–3 June 2020 | 2581 (1624) | 44.5 ± 16.4 | RT‐PCR | Subjective | Self‐reported |
| 37 | Lechien 2020c 51 | Cross‐sectional | Belgium, Italy, France, and Spain | NR | 417 (263) | 36.9 ± 11.4 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 38 | Lee 2020 52 | Cross‐sectional | Canada | 16 March–15 April 2020 | 56 (33) | 38.0 (31.8–47.2) | RT‐PCR | Subjective | Telephone questionnaire survey |
| 39 | Levinson 2020 53 | Cross‐sectional | Israel | 10–23 March 2020 | 42 (19) | 34.0 (15.0–82.0) | RT‐PCR | Subjective | Telephone questionnaire survey |
| 40 | Liang 2020 54 | Cross‐sectional | China | 16 March–12 April 2020 | 86 (42) | 25.5 (6.0–57.0) | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 41 | Lombardi 2020 55 | Cross‐sectional | Italy | 24 February–31 March 2020 | 139 (82) | NR | RT‐PCR | Subjective | Self‐reported |
| 42 | Luers 2020 56 | Cross‐sectional | Germany | 22–28 March 2020 | 72 (31) | 38.0 ± 13.0 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 43 | Luigetti 2020 57 | Cross‐sectional | Italy | 14 March–20 April 2020 | 213 (76) | 70.2 ± 13.9 | RT‐PCR | Subjective | Self‐reported |
| 44 | Magnavita 2020 58 | Cross‐sectional | Italy | 27 March–30 April 2020 | 82 (56) | NR | RT‐PCR | Subjective | Self‐reported questionnaire |
| 45 | Mao 2020 59 | Cross‐sectional | China | 16 January–19 February 2020 | 214 (127) | 52.7 ± 15.5 | RT‐PCR | NR | NR |
| 46 | Martin‐Sanz 2020 60 | Case control | Spain | 15 March–7 April 2020 | 215 (171) | 42.9 ± 0.6 | RT‐PCR | Objective | VAS |
| 47 | Meini 2020 61 | Cross‐sectional | Italy | April 2020 | 100 (40) | 65.0 ± 15.0 | RT‐PCR | Subjective | Telephone interview |
| 48 | Menni 2020 5 | Cross‐sectional | UK | 24–29 March 2020 | 579 (400) | 40.79 ± 11.84 | RT‐PCR | Subjective | Smartphone‐based App survey |
| 49 | Menni 2020a 62 | Cross‐sectional | UK | 24 March–21 April 2020 | 6452 (4638) | 41.2 ± 12.1 | RT‐PCR | Subjective | Smartphone‐based App survey |
| USA | 726 (567) | 44.6 ± 14.3 | |||||||
| 50 | Mercante 2020 63 | Cross‐sectional | Italy | 5–23 March 2020 | 204 (94) | 52.6 ± 14.4 | RT‐PCR | Subjective | Telephone questionnaire survey |
| 51 | Merza 2020 64 | Cross‐sectional | Iraq | 18 March–7 April 2020 | 15 (6) | 28.0 ± 16.4 | RT‐PCR | NR | NR |
| 52 | Moein 2020 65 | Case–control | Iran | 21–23 March 2020 | 60 (20) | 46.5 ± 12.1 | RT‐PCR | Objective | UPSIT |
| 53 | Noh 2020 66 | Cross‐sectional | Korea | NR | 199 (130) | 38.0 ± 13.1 | RT‐PCR | Subjective | In person interview |
| 54 | Otte 2020 67 | Cross‐sectional | Germany | NR | 50 (NR) | 43.2 (23.0–69.0) | RT‐PCR | Objective | Sniffin' sticks test |
| 55 | Paderno 2020 68 | Cross‐sectional | Italy | 27 March–1 April 2020 | 508 (223) | 55.0 ± 15.0 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 56 | Parente‐Arias 2020 69 | Cross‐sectional | Spain | 3–24 March 2020 | 151 (98) | 55.2 (18.0–88.0) | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 57 | Patel 2020 70 | Cross‐sectional | UK | 1 March–1 April 2020 | 141 (58) | 45.6 (20.0–93.0) | RT‐PCR | Subjective | Telephone interview |
| 58 | Petrocelli 2020 71 | Cross‐sectional | Italy | 16 April–2 May 2020 | 300 (225) | 43.6 ± 12.2 | RT‐PCR | Objective | Olfactory threshold and identification test |
| 59 | Peyrony 2020 72 | Cross‐sectional | France | 9 March–4 April 2020 | 225 (150) | 62.0 (48.0–71.0) | RT‐PCR | Subjective | Self‐reported |
| 60 | Qiu 2020 73 | Cross‐sectional | China, France and Germany | 15 March–5 April 2020 | 394 (NR) | NR | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 61 | Romero‐Sánchez 2020 74 | Cross‐sectional | Spain | 1 March–1 April 2020 | 841 (368) | 66.4 ± 14.9 | RT‐PCR | Subjective | Medical record review |
| 62 | Sakalli 2020 75 | Cross‐sectional | Turkey | NR | 172 (88) | 37.8 ± 12.5 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 63 | Sayin 2020 76 | Case–control | Turkey | NR | 64 (39) | 37.7 ± 11.3 | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 64 | Seo 2020 77 | Cross‐sectional | Korea | 28 April 2020 | 62 (NR) | NR | RT‐PCR | Objective | CC‐SIT |
| 65 | Sierpiński 2020 78 | Cross‐sectional | Poland | 17–18 April 2020 | 1942 (1169) | 50.0 (NR) | RT‐PCR | Subjective | Telephone interview |
| 66 | Song 2020 79 | Cross‐sectional | China | 27 January–10 March 2020 | 1172 (595) | 61.0 (48.0–68.0) | RT‐PCR | Subjective | Telephone interview |
| 67 | Speth 2020 80 | Cross‐sectional | Switzerland | 3 March–17 April 2020 | 103 (53) | 46.8 ± 15.9 | RT‐PCR | Subjective | Telephone interview |
| 68 | Tomlins 2020 81 | Cross‐sectional | UK | 10–30 March 2020 | 95 (35) | 75.0 (59.0–82.0) | RT‐PCR | NR | NR |
| 69 | Tostmann 2020 82 | Cross‐sectional | Netherlands | 10–30 March 2020 | 79 (NR) | NR | NR | Subjective | Self‐reported questionnaire survey |
| 70 | Trubiano 2020 83 | Cross‐sectional | Australia | 1–22 April 2020 | 28 (14) | 55.0 (46.0–63.5) | RT‐PCR | Subjective | Medical record review |
| 71 | Tudrej 2020 84 | Cross‐sectional | Switzerland | 24 March–14 April 2020 | 198 (NR) | NR | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 72 | Vacchiano 2020 85 | Cross‐sectional | Italy | NR | 108 (46) | 59.0 (18.0–83.0) | RT‐PCR | Subjective | Telephone questionnaire survey |
| 73 | Vaira 2020 86 | Cross‐sectional | Italy | 31 March–6 April 2020 | 72 (45) | 49.2 ± 13.7 | RT‐PCR | Objective | CCCRC |
| 74 | Vaira 2020a 87 | Cross‐sectional | Italy | 9–10 April 2020 | 33 (22) | 47.2 ± 10 | RT‐PCR | Objective | CCCRC |
| 75 | Vaira 2020b 88 | Cross‐sectional | Italy | NR | 345 (199) | 48.5 ± 12.8 (23–88) | RT‐PCR | Objective | CCCCRC |
| 76 | Wee 2020 89 | Cross‐sectional | Singapore | 26 March–10 April 2020 | 154 (NR) | NR | RT‐PCR | Subjective | Self‐reported questionnaire survey |
| 77 | Wi 2020 90 | Cross‐sectional | Korea | 15 April 2020 | 111 (57) | 41.3 ± 19.0 | RT‐PCR | Subjective | Medical record review |
| 78 | Yan 2020 91 | Cross‐sectional | USA | 3 March–8 April 2020 | 128 (67) | 53.5 (40.0–65.0) | RT‐PCR | Subjective | Self‐reported |
| 79 | Yan 2020a 92 | Cross‐sectional | Germany, USA, Bolivia and Venezuela | NR | 59 (29) | 18.0–79.0 | RT‐PCR | Subjective | Online questionnaire survey |
| 80 | Yan 2020b 93 | Cross‐sectional | USA | 9 March–29 April 2020 | 46 (NR) | NR | RT‐PCR | Subjective | Medical record review |
| 81 | Zayet 2020 94 | Cross‐sectional | France | 26 February–14 March 2020 | 70 (41) | 56.7 ± 19.3 | RT‐PCR | Subjective | Self‐reported questionnaire |
| 82 | Zayet 2020a 95 | Case–control | France | 30 March–3 April 2020 | 95 (79) | 39.8 ± 12.2 | RT‐PCR | Subjective | Medical record review |
| 83 | Zou 2020 96 | Cross‐sectional | China | 1 February–3 March 2020 | 81 (43) | 58.0 (50.0–68.5) | RT‐PCR | Subjective | Medical record review |
AAO‐HNS = American academy of otolaryngology–head and neck surgery; CC‐SIT = cross‐cultural smell identification test; CCCRC = Connecticut chemosensory clinical research center orthonasal olfaction test; IQR = interquartile range; NR = not reported; RT‐PCR = reverse transcription polymerase chain reaction; SD = standard deviation; UPSIT = University of Pennsylvania smell identification test; VAS = visual analog scale..
Outcomes
Overall, the pooled prevalence of olfactory dysfunction in COVID‐19 patients was 47.85% [95% CI: 41.20–54.50] (Fig. 2). From the subgroup analyses, we observed olfactory dysfunction in 54.40% European, 51.11% North American, 31.39% Asian, and 10.71% Australian COVID‐19 patients (Table II, Supporting Figure 1). In addition, anosmia, hyposmia, and dysosmia were observed in 35.39%, 36.15%, and 2.53% of the COVID‐19 patients, respectively (Table II, Supporting Figure 2). Interestingly, the prevalence of olfactory dysfunction was observed higher in COVID‐19 patients on objective rather than subjective evaluations (72.10% vs. 44.53%) (Table II, Supporting Figure 3). Based on the clinical severity, olfactory dysfunction was higher in non‐severe patients compared to severe patients with COVID‐19 (47.48% vs. 9.02%) (Table II, Supporting Figure 4).
Fig 2.
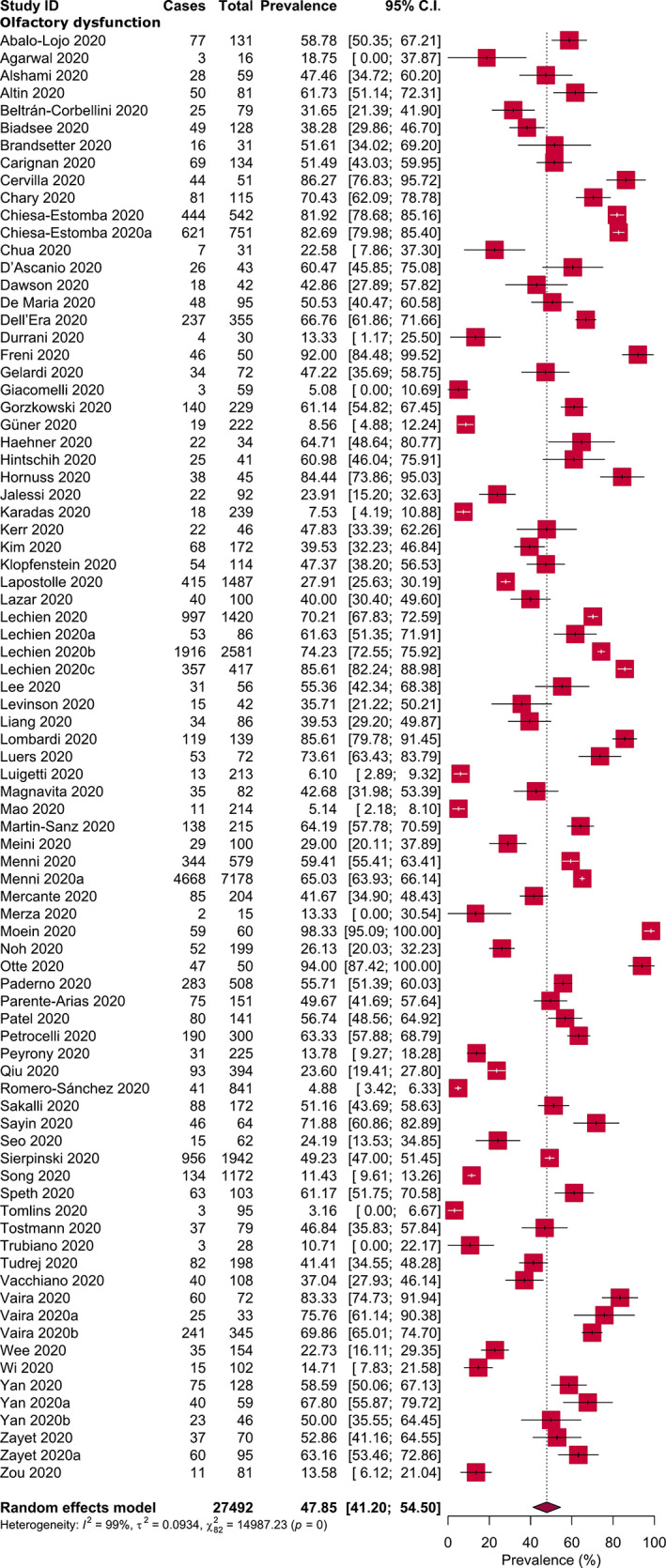
Prevalence of olfactory dysfunction in COVID‐19 patients. [Color figure can be viewed in the online issue, which is available at www.laryngoscope.com.]
TABLE II.
Pooled Prevalence of Olfactory Dysfunction in Different Subgroups of COVID‐19 Patients.
| Subgroups of COVID‐19 Patients | Olfactory Dysfunction Prevalence [95% CIs] (%) | Number of Studies Analyzed | Total Number of COVID‐19 Patients | Heterogeneity | Publication Bias, Egger's Test (P Value) | |
|---|---|---|---|---|---|---|
| I 2 (%) | P Value | |||||
| Olfactory dysfunction in different regions | ||||||
| Europe | 54.40 [46.19–62.61] | 49 | 20,738 | 99 | <.0001 | .19 |
| North America | 51.11 [41.10–61.13] | 7 | 1,148 | 87 | <.0001 | NA |
| Asia | 31.39 [18.26–44.51] | 22 | 3,477 | 99 | <.0001 | .66 |
| Australia | 10.71 [0.00–22.17] | 1 | 28 | NA | NA | NA |
| Different types of olfactory dysfunction | ||||||
| Anosmia | 35.39 [27.73–43.04] | 43 | 10,979 | 99 | <.0001 | .11 |
| Hyposmia | 36.15 [27.65–44.64] | 24 | 5,200 | 98 | <.0001 | .003 |
| Dysosmia | 2.53 [0.0–6.0] | 1 | 79 | NA | NA | NA |
| Evaluation types of olfactory dysfunction | ||||||
| Subjective | 44.53 [37.59–51.47] | 73 | 26,229 | 99 | <.0001 | .60 |
| Objective | 72.10 [59.41–84.79] | 10 | 1,263 | 97 | <.0001 | .33 |
| Olfactory dysfunction based on clinical severity | ||||||
| Severe | 9.02 [2.67–15.38] | 4 | 687 | 85 | .001 | NA |
| Non‐severe | 47.48 [21.34–73.62] | 8 | 5,135 | 100 | <.0001 | NA |
CIs = confidence intervals; NA = not applicable.
Detailed quality assessment of the included studies is shown in the Supporting information (Supporting Table 2, Supporting Table 3). Briefly, 95.1% of the included studies were of high‐quality (low‐risk of bias). Overall, very high levels of heterogeneity (ranging from 87% to 99%) were observed during the estimation of olfactory dysfunctions in the main analysis as well as in different subgroup analyses. Visual inspection of the funnel plot and Egger's test results showed that there was no significant publication bias (P = .84) (Fig. 3).
Fig 3.
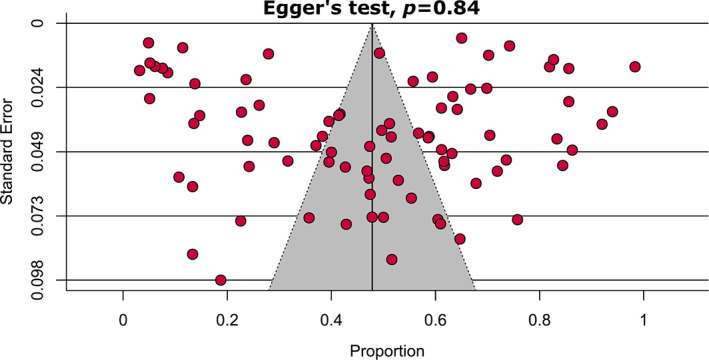
Funnel plot on the prevalence of olfactory dysfunction in COVID‐19 patients. [Color figure can be viewed in the online issue, which is available at www.laryngoscope.com.]
Sensitivity analyses on assessing olfactory dysfunction in COVID‐19 patients excluding small studies, low‐quality studies, studies where COVID‐19 confirmation test was not reported, considering only cross‐sectional studies, and excluding outlier studies showed very marginal differences in overall pooled prevalence (Table III, Supporting Figure 5). Overall, our sensitivity analyses indicated that the results of olfactory dysfunction prevalence in COVID‐19 patients are robust and reliable. As the source of heterogeneity, from the Galbraith plot, three studies were identified as the source of heterogeneity (Supporting Figure 6).
TABLE III.
Sensitivity Analyses.
| Strategies of Sensitivity Analyses | Olfactory Dysfunction Prevalence [95% Cis] (%) | Difference of Pooled Prevalence Compared to the Main Result | Number of Studies Analyzed | Total Number of COVID‐19 Patients | Heterogeneity | |
|---|---|---|---|---|---|---|
| I 2 (%) | P Value | |||||
| Excluding small studies | 46.03 [37.08–54.97] | 3.8% lower | 43 | 25,162 | 100 | <.0001 |
| Excluding low‐quality studies | 49.03 [42.21–55.85] | 2.5% higher | 79 | 27,146 | 99 | <.0001 |
| Excluding studies where COVID‐19 confirmation test was not reported | 48.40 [41.67–55.12] | 1.1% higher | 81 | 27,354 | 99 | <.0001 |
| Considering only cross‐sectional studies | 46.66 [39.87–53.44] | 2.5% lower | 77 | 26,979 | 99 | <.0001 |
| Excluding outlier studies | 47.28 [40.61–53.95] | 1.2% lower | 80 | 27,297 | 99 | <.0001 |
CIs = confidence intervals.
DISCUSSION
The route of entry of SARS‐CoV‐2 to the olfactory neuron is via the olfactory epithelium found at the nasal roof. 97 This region is exposed the most to inspired air during inspiration after it passes the nasal valve and moves upwards. The sensory neurons found at the olfactory epithelium are accountable for detecting as well as transmitting information of odors to the brain. It is noteworthy that the unique property of olfactory epithelium is its basal cell, which can regenerate throughout life. 98 , 99
The novel SARS‐CoV‐2 infection was discovered and delineated by Zhou et al. 100 on 3rd February 2020. They described that SARS‐CoV‐2 enters the cell through angiotensin‐converting enzyme 2 (ACE2). It is postulated that SARS‐CoV infiltrates cells via the interplay between its spike (S) protein and the ACE2 protein on the target cells. 101 , 102 Interestingly, the number of ACE2 cells is similar both in nasal and oral tissues, as well as lung and colon tissues, 103 although it is postulated that nasal and oral tissues may be the first site of entry by SARS‐CoV‐2. The two genes accountable for anosmia following SARS‐CoV‐2 infection are ACE2 and TMPRSS2. 104 SARS‐CoV‐2 has been shown to enter the brain via olfactory bulb on transgenic mice causing transneuronal spread and was discovered abundantly in the olfactory bulb following infection. 105 In addition, autopsy samples taken from patients with SARS showed SARS‐CoV‐2 in the brain samples. The mode of entry into the brain is postulated to be via olfactory bulb. 106 , 107 Previous experience had led to a revelation that coronaviruses have shown to share a similar structure as well as an infective pathway. 108 Hence, structural changes in the olfactory bulb ought to be assessed. 109 It is noteworthy that, reduction in the volume of olfactory bulb has been reported to result from a prior infection‐related olfactory dysfunction. 110 There are several possible mechanisms for olfactory dysfunction following SARS‐CoV‐2 infection. Among the countless existing theories, the most notable ones include olfactory cleft syndrome and postviral anosmia syndrome. 111 The former theory advocates on mucosal obstruction at the olfactory cleft results in conduction impairment of smell, 112 while the latter proposes on a neural loss mechanism whereby direct injury to the olfactory sensory neurons preceding viral infection. 113
It is noteworthy that postviral olfactory loss (PVOL) is not a novel phenomenon. Numerous virus has been advocated to enable olfactory dysfunction, including influenza virus, adenovirus, parainfluenza virus, respiratory syncytial virus, coxsackievirus, adenovirus, poliovirus, enterovirus, and herpesvirus. 114 , 115 , 116 , 117 Suguira et al. 115 in an earlier study supported parainfluenza virus (PIV) type 3 to be the primary virus responsible for PVOL. Subsequent research revealed a similar finding, whereby PIV‐3 was the leading culprit behind PVOL. 116 Tian et al. 117 studied the Sendai virus (SeV), the murine counterpart of the PIV on olfactory function and regenerative ability of the olfactory epithelium. In addition, they found that SeV impairs olfaction and persists in the olfactory epithelium and olfactory body, thus hindering the regenerative ability as well as the normal physiologic function of olfactory sensory neurons.
Suzuki et al. 114 found rhinovirus to be the predominant cause of PVOL followed by PIV‐2, Epstein–Barr virus, and coronavirus, which was identified in one patient. PIV‐3 was not, however, studied in their sample. Coronavirus was not considered in many studies as the involvement of coronavirus in PVOL was not extensively reported, and it is challenging to isolate coronavirus. 115 In addition, the challenge faced by many researchers in identifying the virus responsible for PVOL is following the delay of patients with the olfactory loss to visiting the clinic, believing the notion that PVOL will resolve spontaneously. A noteworthy study by Potter et al. 118 shed more light on the interaction between virus and host in PVOL related condition. Potter et al. suggested that a seasonal pattern emerged among influenza and non‐influenza related PVOL indicating not only variations of potency and virulence of virus but also on host susceptibility as a factor in determining the progression and manifestation of the infection. Olfactory disorders related to non‐influenza virus peaked in warmer months compared to colder months.
In our meta‐analysis, all 83 studies revealed a strong association between olfactory dysfunction and SARS‐COV‐2 infection. Overall nasal symptoms among COVID‐19 positive patients have been scarcely reported. 3 , 119 Chen et al. 3 in their series, reported only 4% of their patients had rhinorrhea; while Guan et al. 119 reported 5% of their patients demonstrated nasal obstruction. Scanty reported data on olfactory dysfunction had been attributed by either overlooked nasal symptoms by physicians, 51 or the possibility of different virus sequences leading to the various presentations. 120 The latter theory was supported based on a study by Benvenuto et al. 120 who compared genomes of 15 virus sequences from patients in various regions in China with other coronaviruses. The possibility that olfactory, as well as gustatory dysfunction, prevails among the European community has emerged. 51 in addition, lack of awareness among Asian patients in addition to unnoticed olfactory loss could have contributed to the low number of reported cases among Asian patients. Recent epiphany on olfactory dysfunction among Asian patients accruing the surge in cases has enabled olfactory dysfunction to be included in suspect case criteria for SARS‐CoV‐2 infection, allowing test to be carried out in these patients, while isolation is implemented concomitantly. 28
Female predominance was revealed among our patients (61.4%). Similarly, previous studies have shown olfactory loss postviral prevails among female patients. 121 , 122 This notion is attributed to gender‐related variation in the inflammatory process. 123 Increase in numbers of female patients can be attributed by greater tendency of females to volunteer for studies. In addition, female patients are found to be more sensitive in detecting chemosensory alteration.
Most studies involved online questionnaire either through an online application, online survey, smartphone‐based App filled up by patients or clinicians, whereas objective assessment of olfactory assessment was utilized in four studies whereby Sniffin test, University of Pennsylvania smell identification test (UPSIT), and Connecticut chemosensory clinical research center orthonasal olfaction test (CCCRC) were performed. It is noteworthy that, in our meta‐analysis, we found prevalence of olfactory dysfunction among objectively evaluated studies to be higher (72.10%) as compared to the subjectively evaluated studies (44.53%). This could be attributed by the fact that most COVID‐19 patients are unaware of their olfactory dysfunction leading to possibility of underestimation. Moein et al. 65 reported 98% of their patients were found to have olfactory dysfunction post UPSIT, of which only 35% were initially aware of their symptoms. Generally, loss of smell is only perceived upon significant loss of smell such as anosmia. Thus, it is worth noting that the prevalence of olfactory dysfunction may be higher if tested objectively. Quantitative testing of olfactory disturbance may provide rapid and cheap modality to screen COVID‐19 in a large population. Interestingly, Moein et al. 124 reported that time of testing is the most important factor in explaining the prevalence variations among studies apart from variations in question and types of olfactory testing. They found that 61% of the earlier 96% of patients who demonstrated olfactory disturbance, when retested during the late acute phase showed an improvement.
Although the jarring increase in the number of cases daily, which led to a surge in research as well as publications, we obtained only 83 studies on olfactory dysfunction in SARS‐CoV‐2 infection. This may be attributed by the fact that the substantial available peer‐reviewed studies report on hospitalized patients, which means that the self‐limiting, 125 as well as the mild group of patients, are omitted from the various studies. The notion that olfactory manifestation predominately affects the milder form of SARS‐CoV‐2 infection is inevitable. Yan et al. 92 found that most patients with olfactory disturbance with positive SARS‐CoV‐2 infection were treated as out‐patient or ambulatory and not requiring hospitalization. Yet, it is imperative to keep in mind that the nature of this virus is yet to be explored, and owing to the varying genome in virus sequencing, all SARS‐CoV‐2 infection positive patients with olfactory disturbance should not be taken lightly. Villalba et al. 126 reported on two patients who presented with anosmia as the initial symptom of SARS‐CoV‐2 infection had to be hospitalized, and unfortunately, one patient succumbed. Varying reports are available on the outcome following the PVOL. Yan et al. 92 and Klopfenstein et al. 45 demonstrated 74% and 98% resolution of olfactory symptoms and linked this short‐lived manifestation to the unique ability of olfactory epithelium to regenerate and repair following viral clearance.
In our meta‐analysis, none of the authors mentioned on specific treatment directed to smell impairment. The role of intranasal steroids is debatable in this situation accruing the possibility of triggering upper respiratory tract infection. Oral steroids used traditionally to treat idiopathic anosmia ought to be averted by all means to avoid further risk of immunosuppression in SARS‐CoV‐2 infection patients. 112 The outcome of olfactory loss revealed persistence of symptoms mentioned in some of the studies. Duration of olfactory dysfunction remains a conundrum as the nature of this novel pandemic is still a mystery. Heretofore, PVOL habitually has been shown to have a good prognosis. Despite still premature, several anecdotal reports have revealed on total or partial recuperation of olfactory loss over a few months. 127 This is owing to the fact that a longer time for regeneration following damage to olfactory neurons is required. Albeit considered innocuous, olfactory disturbance has been related to a number of detrimental effects notably on quality of life, impacts social interaction, and depression. Astonishingly, several high‐profile studies have related olfactory disturbance to a 5‐year mortality rate. 128 , 129 , 130 , 131 The unique neuroplasticity potential found in olfactory system opens to novel possibility of olfactory recovery via numerous modalities such as olfactory training. 132
Implications for Clinical Practice
The characteristics of an ideal screening tool are high probability of detecting disease (highly sensitive) and high probability of excluding disease when it is negative (highly specific). Besides being reliable, it must be cost‐effective, simple to perform, and widely available. 133 , 134 Moreover, an effective screening requires engagement of both target populations and health care providers. As olfactory dysfunction can be simply detected by using questionnaire, 135 it fulfills all these criteria and can be a useful screening tool besides temperature surveillance. Applying a specific questionnaire to detect olfactory dysfunction, especially in those with suspicious flu‐like symptoms, travel history from affected countries, and contact with COVID‐19 patients may enhance the pick‐up rate of infected patients. Furthermore, questionnaire‐based screening tool may easily be assimilated in the global health care system and more so in developing countries where cost is a factor.
Implications for Research
As there is no standardized questionnaire available to screen for olfactory dysfunction, a consensus is required to determine the most suitable questionnaire for a reliable detection. Perhaps a more refined questionnaire based on the available questionnaires can be developed by selecting the relevant questions and compare by comparing them with an objective smell test to choose the most consistent questions. Researches need to be conducted employing the more objective smell test, which will provide us information on specific odor affected by this infection. By identifying the specific associated odor link to the infection, a simple smell test can be developed particularly to screen for COVID‐19. Olfactory dysfunction may serve as prognosticators to triage and stratify patients according to different categories of severity, which can help to detect those who need immediate and urgent hospitalization. Research into this may help in preventing death among COVID‐19 patients.
Strengths
Our study has several strengths. This meta‐analysis was conducted with significant number of studies and hence including a considerable number of participants, resulting in more robust estimates. Majority of the included studies confirmed COVID‐19 subjects by using the RT‐PCR technique, which strengthens our findings. None of the analyses represented significant publication bias demonstrating that we were unlikely to have missed studies that could have altered the findings. All the conducted sensitivity analyses generated similar results to the main findings indicating the robustness of the meta‐analysis results. Based on the quality assessments, 95.1% of the studies were of high methodological quality (low‐risk of bias), which ensured a reliable result.
Limitations
Nevertheless, there are several notable limitations. Based on the search strategy and considered time period, this meta‐analysis could include participants from 27 countries from four continents; therefore, the prevalence may not represent at a global scale and generalization of the findings should be done with care. One of the major limitations in this meta‐analysis is the presence of substantial degrees of heterogeneity. Even though we examined the sources of heterogeneity by subgroup, sensitivity analyses and Galbraith plot, source of heterogeneity could not be fully explained by the factors included in the analyses. Although we comprehensively investigated the prevalence of olfactory dysfunction from the first eight‐month data of the COVID‐19 outbreak, we have somewhat characterized olfactory dysfunctions in severe versus non‐severe COVID‐19 patients due to the limited number of studies.
Another major limitation is majority of the studies used self‐reported data. When self‐reported health measures are used, both underestimation due to false negative reporting and overestimation due to false positive reporting may possibly transpire, and the results should be interpreted with caution. A meta‐analysis involving studies with large number of patients may minimize the potential bias but an amplification of the compromised methodology cannot entirely be excluded.
CONCLUSION
This meta‐analysis found the prevalence of olfactory dysfunction was 47.85% of the COVID‐19 patients based on the high quality of evidence, which suggests it as a significant initial symptom of SARS‐CoV‐2 infection. Due to the subjective measures of most studies pooled in the analysis, further studies with objective evaluations are recommended to confirm the finding.
Supporting information
Supporting Figure 1 Subgroup analyses: Prevalence of olfactory dysfunction in COVID‐19 patients from (A) Europe, (B) North America, (C) Asia, and (D) Australia.
Supporting Figure 2 Subgroup analyses: Prevalence of (A) anosmia, (B) hyposmia, and (C) dysosmia in patients with COVID‐19.
Supporting Figure 3 Subgroup analyses: Prevalence of olfactory dysfunction in COVID‐19 patients with (A) subjective and (B) objective olfactory evaluations.
Supporting Figure 4 Subgroup analyses: Prevalence of olfactory dysfunction in (A) severe and (B) non‐severe COVID‐19 patients.
Supporting Figure 5 Sensitivity analyses: Prevalence of olfactory dysfunction in COVID‐19 patients (A) excluding small studies (n < 100), (B) excluding low‐quality studies, (C) excluding studies without COVID‐19 confirmation method being reported, (D) considering only cross‐sectional studies, and (E) excluding outlier studies.
Supporting Figure 6 Galbraith plot identified three studies as the potential sources of heterogeneity.
Supporting Table 1 Search strategy.
Supporting Table 2 Quality assessment of the included cross‐sectional studies.
Supporting Table 3 Quality assessment of the included case–control studies.
Editor's Note: This Manuscript was accepted for publication on November 18, 2020.
Jeyasakthy Saniasiaya and Md Asiful Islam should be considered joint first author. Author order was determined alphabetically.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Coronavirus disease 2019 (COVID‐19) Weekly Epidemiological Update. October 23, 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed October 26, 2020.
- 3. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Giacomelli A, Pezzati L, Conti F, et al. Self‐reported olfactory and taste disorders in patients With severe acute respiratory coronavirus 2 infection: a cross‐sectional study. Clin Infect Dis 2020;71:889–890. 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Menni C, Valdes A, Freydin MB, et al. Loss of smell and taste in combination with other symptoms is a strong predictor of COVID‐19 infection. medRxiv 2020. 10.1101/2020.04.05.20048421. [DOI] [Google Scholar]
- 6. Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and ageusia: common findings in COVID‐19 patients. Laryngoscope 2020;130:1787. 10.1002/lary.28692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Xydakis MS, Dehgani‐Mobaraki P, Holbrook EH, et al. Smell and taste dysfunction in patients with COVID‐19. Lancet Infect Dis 2020;20(9):1015–1016. 10.1016/S1473-3099(20)30293-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kowalski LP, Sanabria A, Ridge JA, et al. COVID‐19 pandemic: effects and evidence‐based recommendations for otolaryngology and head and neck surgery practice. Head Neck 2020;42:1259–1267. 10.1002/hed.26164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. CDC . Coronavirus disease 2019 (COVID‐19)—symptoms. Available at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Accessed July 30, 2020.
- 10. Hjelmesæth J, Skaare D. Loss of smell or taste as the only symptom of COVID‐19. Tidsskr nor Laegeforen 2020;140. 10.4045/tidsskr.20.0287. [DOI] [PubMed] [Google Scholar]
- 11. Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The prevalence of olfactory and gustatory dysfunction in COVID‐19 patients: a systematic review and meta‐analysis. Otolaryngol Head Neck Surg 2020;163:1–11. [DOI] [PubMed] [Google Scholar]
- 12. Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med 2009;6:1–6. [PMC free article] [PubMed] [Google Scholar]
- 13. Moola S, Munn Z, Tufanaru C, et al. Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. Joanna Briggs Institute: JBI; 2020. Ch. 7. Available from https://synthesismanual.jbi.global. [Google Scholar]
- 14. Kundu S, Marzan M, Gan SH, Islam MA. Prevalence of antibiotic‐resistant pulmonary tuberculosis in Bangladesh: a systematic review and meta‐analysis. Antibiotics 2020;9:710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Viechtbauer W. Conducting meta‐analyses in R with the metafor package. J Stat Softw 2010;36:1–48. [Google Scholar]
- 16. Abalo‐Lojo JM, Pouso‐Diz JM, Gonzalez F. Taste and smell dysfunction in COVID‐19 patients. Ann Otol Rhinol Laryngol 2020;129:1041–1042. 10.1177/0003489420932617. [DOI] [PubMed] [Google Scholar]
- 17. Aggarwal S, Garcia‐Telles N, Aggarwal G, Lavie C, Lippi G, Henry BM. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID‐19): early report from the United States. Diagnosis 2020;7:91–96. [DOI] [PubMed] [Google Scholar]
- 18. Alshami AA, Alattas RA, Anan HF, Alhalimi A, Alfaraj A, al Qahtani H. Silent disease and loss of taste and smell are common manifestations of SARS‐COV‐2 infection in a quarantine facility: first report from Saudi Arabia. medRxiv 2020;15:e0241258. 10.1101/2020.05.13.20100222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Altin F, Cingi C, Uzun T, Bal C. Olfactory and gustatory abnormalities in COVID‐19 cases. Eur Arch Otorhinolaryngol 2020;277:2775–2781. 10.1007/s00405-020-06155-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Beltrán‐Corbellini Á, Chico‐García JL, Martínez‐Poles J, et al. Acute‐onset smell and taste disorders in the context of Covid‐19: a pilot multicenter PCR‐based case‐control study. Eur J Neurol 2020;27:1738–1741. 10.1111/ene.14273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Biadsee A, Biadsee A, Kassem F, Dagan O, Masarwa S, Ormianer Z. Olfactory and Oral manifestations of COVID‐19: sex‐related symptoms‐a potential pathway to early diagnosis. Otolaryngol Head Neck Surg 2020;163:722–728. 10.1177/0194599820934380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brandstetter S, Roth S, Harner S, et al. Symptoms and immunoglobulin development in hospital staff exposed to a SARS‐CoV‐2 outbreak. Pediatr Allergy Immunol 2020;31:841–847. 10.1111/pai.13278. [DOI] [PubMed] [Google Scholar]
- 23. Carignan A, Valiquette L, Grenier C, et al. Anosmia and dysgeusia associated with SARS‐CoV‐2 infection: an age‐matched case−control study. Can Med Assoc J 2020;192:E702–E707. 10.1503/cmaj.200869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cervilla MT, Gutierrez I, Romero M, Garcia‐Gomez J. Olfactory dysfunction quantified by olfactometry in patients with SARS‐Cov‐2 infection. Res Sq 2020. 10.21203/rs.21203.rs-35796/v21201. [DOI] [Google Scholar]
- 25. Chary E, Carsuzaa F, Trijolet J‐P, et al. Prevalence and recovery from olfactory and gustatory dysfunctions in Covid‐19 infection: a prospective multicenter study. Am J Rhinol Allergy 2020;34:686–693. 10.1177/1945892420930954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chiesa‐Estomba CM, Lechien JR, Portillo‐Mazal P, et al. Olfactory and gustatory dysfunctions in COVID‐19. First reports of Latin‐American ethnic patients. Am J Otolaryngol. 2020;41:102605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chiesa‐Estomba CM, Lechien JR, Radulesco T, et al. Patterns of smell recovery in 751 patients affected by the COVID‐19 outbreak. Eur J Neurol 2020;27:2318–2321. 10.1111/ene.14440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chua AJK, Yun Chan EC, Loh J, Charn TC. Acute olfactory loss is specific for Covid‐19 at the emergency department. Ann Emerg Med 2020;76:550–551. 10.1016/j.annemergmed.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. D'Ascanio L, Pandolfini M, Cingolani C, et al. Olfactory dysfunction in COVID‐19 patients: prevalence and prognosis for recovering sense of smell. Otolaryngol Head Neck Surg 2020;019459982094353. 10.1177/0194599820943530. [DOI] [PubMed] [Google Scholar]
- 30. Dawson P, Rabold EM, Laws RL, et al. Loss of taste and smell as distinguishing symptoms of COVID‐19. medRxiv 2020. 10.1101/2020.2005.2013.20101006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. De Maria A, Varese P, Dentone C, Barisione E, Bassetti M. High prevalence of olfactory and taste disorder during SARS‐CoV‐2 infection in outpatients. J Med Virol 2020. 10.1002/jmv.25995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dell'Era V, Farri F, Garzaro G, Gatto M, Aluffi Valletti P, Garzaro M. Smell and taste disorders during COVID‐19 outbreak: a cross‐sectional study on 355 patients. Head Neck 2020;42:1591–1596. 10.1002/hed.26288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Durrani M, Inam ul Haq UK, Yousaf A. Chest X‐rays findings in COVID 19 patients at a university teaching hospital‐a descriptive study. Pak J Med Sci 2020;36:S22–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Freni F, Meduri A, Gazia F, et al. Symptomatology in head and neck district in coronavirus disease (COVID‐19): a possible neuroinvasive action of SARS‐CoV‐2. Am J Otolaryngol 2020;41:102612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gelardi M, Trecca E, Cassano M, Ciprandi G. Smell and taste dysfunction during the COVID‐19 outbreak: a preliminary report. Acta Biomed 2020;91:230–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gorzkowski V, Bevilacqua S, Charmillon A, et al. Evolution of olfactory disorders in COVID‐19 patients. Laryngoscope 2020;130:2667–2673. 10.1002/lary.28957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Güner R, Hasanoğlu İ, Kayaaslan B, et al. COVID‐19 experience of the major pandemic response center in the capital: results of the pandemic's first month in Turkey. Turk J Med Sci 2020;7:1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Haehner A, Draf J, Draeger S, Hummel T. Predictive value of sudden olfactory loss in the diagnosis of COVID‐19. medRxiv 2020;82:175–180. 10.1101/2020.04.27.20081356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hintschich CA, Wenzel JJ, Hummel T, et al. Psychophysical tests reveal impaired olfaction but preserved gustation in COVID‐19 patients. Int Forum Allergy Rhinol 2020. 10.1002/alr.22655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hornuss D, Lange B, Schroeter N, Rieg S, Kern WV, Wagner D. Anosmia in COVID‐19 patients. medRxiv 2020;26:1426–1427. 10.1101/2020.04.28.20083311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jalessi M, Barati M, Rohani M, et al. Frequency and outcome of olfactory impairment and sinonasal involvement in hospitalized patients with COVID‐19. Neurol Sci 2020;41:2331–2338. 10.1007/s10072-020-04590-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Karadaş Ö, Öztürk B, Sonkaya AR. A prospective clinical study of detailed neurological manifestations in patients with COVID‐19. Neurol Sci 2020;41:1991–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kerr C, Hughes G, Mckenna L, Bergin C. Prevalence of smell and taste dysfunction in a cohort of CoVID19 outpatients managed through remote consultation from a large urban teaching hospital in Dublin, Ireland. Int J Infect Control 2020;2:100076. 10.1016/j.infpip.2020.100076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim GU, Kim MJ, Ra SH, et al. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID‐19. Clin Microbiol Infect 2020;26:948.e1–948.e3. 10.1016/j.cmi.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Klopfenstein T, Toko L, Royer P‐Y, Lepiller Q, Gendrin V, Zayet S. Features of anosmia in COVID‐19. Med mal Infect 2020;50:436–439. 10.1016/j.medmal.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lapostolle F, Schneider E, Vianu I, et al. Clinical features of 1487 COVID‐19 patients with outpatient management in the greater Paris: the COVID‐call study. Intern Emerg Med 2020;15:813–817. 10.1007/s11739-020-02379-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lazar S, Codreanu D, Neculai A, et al. Anosmia – an independent predictor in the persistence of SARS‐CoV‐2 infection? Rom J Infect Dis 2020;23:126–132. [Google Scholar]
- 48. Lechien JR, Chiesa‐Estomba CM, Place S, et al. Clinical and epidemiological characteristics of 1,420 European patients with mild‐to‐moderate coronavirus disease 2019. J Intern Med 2020. 10.1111/joim.13089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lechien JR, Cabaraux P, Chiesa‐Estomba CM, et al. Objective olfactory evaluation of self‐reported loss of smell in a case series of 86 COVID‐19 patients. Head Neck 2020;42:1583–1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lechien J, Chiesa‐Estomba C, Beckers E, et al. Prevalence and recovery of olfactory dysfunction in 1,363 patients with coronavirus disease 2019: a multicenter longitudinal study. Res Sq. 2020;42. 10.21203/rs.3.rs-38504/v1. [DOI] [Google Scholar]
- 51. Lechien JR, Chiesa‐Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild‐to‐moderate forms of the coronavirus disease (COVID‐19): a multicenter European study. Eur Arch Oto‐Rhino‐Laryngol 2020. 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lee DJ, Lockwood J, Das P, Wang R, Grinspun E, Lee JM. Self‐reported anosmia and dysgeusia as key symptoms of COVID‐19. CJEM 2020. 10.1017/cem.2020.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Levinson R, Elbaz M, Ben‐Ami R, et al. Anosmia and dysgeusia in patients with mild SARS‐CoV‐2 infection. medRxiv 2020. 10.1101/2020.04.11.20055483. [DOI] [PubMed] [Google Scholar]
- 54. Liang Y, Xu J, Chu M, et al. Neurosensory dysfunction: a diagnostic marker of early COVID‐19. Int J Infect Dis 2020;98:347–352. 10.1016/j.ijid.2020.06.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lombardi A, Consonni D, Carugno M, et al. Characteristics of 1,573 healthcare workers who underwent nasopharyngeal swab for SARS‐CoV‐2 in Milano, Lombardy, Italy. Clin Microbiol Infect 2020;26:1413.e9–1413.e13. 10.1016/j.cmi.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Luers JC, Rokohl AC, Loreck N, et al. Olfactory and gustatory dysfunction in coronavirus disease 19 (COVID‐19). Clin Infect Dis 2020;71:2262–2264. 10.1093/cid/ciaa525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Luigetti M, Iorio R, Bentivoglio AR, et al. Assessment of neurological manifestations in hospitalized patients with COVID‐19. Eur J Neurol 2020;27:2322–2328. 10.1111/ene.14444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID‐19 epidemic. A cross‐sectional survey. Int J Environ Res Public Health 2020;17:5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020;77:683–690. 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Martin‐Sanz E, Riestra J, Yebra L, et al. Prospective study in 355 patients with suspected COVID‐19 infection. Value of cough, subjective hyposmia, and hypogeusia. Laryngoscope 2020;130:2674–2679. 10.1002/lary.28999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Meini S, Suardi LR, Busoni M, Roberts AT, Fortini A. Olfactory and gustatory dysfunctions in 100 patients hospitalized for COVID‐19: sex differences and recovery time in real‐life. Eur Arch Otorhinolaryngol 2020;277:3519–3523. 10.1007/s00405-020-06102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Menni C, Valdes AM, Freidin MB, et al. Real‐time tracking of self‐reported symptoms to predict potential COVID‐19. Nat Med 2020. 10.1038/s41591-020-0916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mercante G, Ferreli F, De Virgilio A, et al. Prevalence of taste and smell dysfunction in coronavirus disease 2019. JAMA Otolaryngol Head Neck Surg 2020;146:723. 10.1001/jamaoto.2020.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Merza MA, Haleem Al Mezori AA, Mohammed HM, Abdulah DM. COVID‐19 outbreak in Iraqi Kurdistan: the first report characterizing epidemiological, clinical, laboratory, and radiological findings of the disease. Diabetes Metab Syndr 2020;14:547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Moein ST, Hashemian SMR, Mansourafshar B, Khorram‐Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID‐19. Int Forum Allergy Rhinol 2020. 10.1002/alr.22587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Noh JY, Yoon JG, Seong H, et al. Asymptomatic infection and atypical manifestations of COVID‐19: comparison of viral shedding duration. J Infect 2020. 10.1016/j.jinf.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Otte M, Klussmann J, Luers J. Persisting olfactory dysfunction in patients after recovering from COVID‐19. J Infect 2020;81:e58. 10.1016/j.jinf.2020.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Paderno A, Schreiber A, Grammatica A, et al. Smell and taste alterations in Covid‐19: a cross‐sectional analysis of different cohorts. Int Forum Allergy Rhinol 2020. 10.1002/alr.22610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Parente‐Arias P, Barreira‐Fernandez P, Quintana‐Sanjuas A, Patiño‐Castiñeira B. Recovery rate and factors associated with smell and taste disruption in patients with coronavirus disease 2019. Am J Otolaryngol 2020;102648. 10.1016/j.amjoto.2020.102648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Patel A, Charani E, Ariyanayagam D, et al. New onset anosmia and ageusia in adult patients diagnosed with SARS‐CoV‐2. Clin Microbiol Infect 2020;26:1236–1241. 10.1016/j.cmi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Petrocelli M, Ruggiero F, Baietti A, et al. Remote psychophysical evaluation of olfactory and gustatory functions in early‐stage coronavirus disease 2019 patients: the Bologna experience of 300 cases. J Laryngol Oto 2020. 10.1017/S0022215120001358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Peyrony O, Marbeuf‐Gueye C, Truong V, et al. Accuracy of emergency department clinical findings for diagnostic of coronavirus disease‐2019. Ann Emerg Med 2020;76:405–412. 10.1016/j.annemergmed.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Qiu C, Cui C, Hautefort C, et al. Olfactory and gustatory dysfunction as an early identifier of COVID‐19 in adults and children: an international multicenter study. medRxiv 2020;163:714–721. 10.1177/0194599820934376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Romero‐Sánchez CM, Díaz‐Maroto I, Fernández‐Díaz E, et al. Neurologic manifestations in hospitalized patients with COVID‐19: the ALBACOVID registry. Neurology 2020;95:e1060–e1070. 10.1212/WNL.0000000000009937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Sakalli E, Temirbekov D, Bayri E, Alis EE, Erdurak SC, Bayraktaroglu M. Ear nose throat‐related symptoms with a focus on loss of smell and/or taste in COVID‐19 patients. Am J Otolaryngol 2020;41:102622. 10.1016/j.amjoto.2020.102622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sayin İ, Yaşar KK, Yazici ZM. Taste and smell impairment in COVID‐19: an AAO‐HNS anosmia reporting tool‐based comparative study. Otolaryngol Head Neck Surg 2020;163:473–479. 10.1177/0194599820931820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Seo MY, Seok H, Hwang SJ, et al. Olfactory and gustatory dysfunction in mild COVID‐19. SSRN 2020. 10.2139/ssrn.3605257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Sierpiński R, Pinkas J, Jankowski M, et al. Gender differences in the frequency of gastrointestinal symptoms and olfactory or taste disorders among 1,942 non‐hospitalized patients with COVID‐19. Pol Arch Intern Med 2020;130:501–505. [DOI] [PubMed] [Google Scholar]
- 79. Song J, Deng Y‐K, Wang H, et al. Self‐reported taste and smell disorders in patients with COVID‐19: distinct features in China. medRxiv 2020. 10.1101/2020.06.12.20128298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Speth MM, Singer‐Cornelius T, Obere M, Gengler I, Brockmeier SJ, Sedaghat AR. Olfactory dysfunction and Sinonasal symptomatology in COVID‐19: prevalence, severity, timing, and associated characteristics. Otolaryngol Head Neck Surg 2020;163:114–120. 10.1177/0194599820929185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Tomlins J, Hamilton F, Gunning S, Sheehy C, Moran E, MacGowan A. Clinical features of 95 sequential hospitalised patients with novel coronavirus 2019 disease (COVID‐19), the first UK cohort. J Infect 2020;81:e59–e61. 10.1016/j.jinf.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Tostmann A, Bradley J, Bousema T, et al. Strong associations and moderate predictive value of early symptoms for SARS‐CoV‐2 test positivity among healthcare workers, The Netherlands. Euro Surveill 2020;25:2000508. 10.2807/1560-7917.ES.2020.25.16.2000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Trubiano JA, Vogrin S, Kwong JC, Holmes NE. Alterations in smell or taste–classic COVID‐19? Clin Infect Dis 2020;71:2307–2309. 10.1093/cid/ciaa2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Tudrej B, Sebo P, Lourdaux J, et al. Self‐reported loss of smell and taste in SARS‐CoV‐2 patients: primary care data to guide future early detection strategies. J Gen Intern Med 2020;35:2502–2504. 10.1007/s11606-020-05933-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Vacchiano V, Riguzzi P, Volpi L, et al. Early neurological manifestations of hospitalized COVID‐19 patients. Neurol Sci 2020;41:2029–2031. 10.1007/s10072-020-04525-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Vaira LA, Deiana G, Fois AG, et al. Objective evaluation of anosmia and ageusia in COVID‐19 patients: single‐center experience on 72 cases. Head Neck 2020. 10.1002/hed.26204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Vaira LA, Salzano G, Petrocelli M, Deiana G, Salzano FA, De Riu G. Validation of a self‐administered olfactory and gustatory test for the remotely evaluation of COVID‐19 patients in home quarantine. Head Neck 2020. 10.1002/hed.26228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Vaira LA, Hopkins C, Salzano G, et al. Olfactory and gustatory function impairment in COVID‐19 patients: Italian objective multicenter‐study. Head Neck 2020;42:1560–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Wee LE, Chan YFZ, Teo NWY, et al. The role of self‐reported olfactory and gustatory dysfunction as a screening criterion for suspected COVID‐19. Eur Arch Otorhinolaryngol 2020;277:2389–2390. 10.1007/s00405-020-05999-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Wi YM, Lim SJ, Kim S‐H, et al. Response system for and epidemiological features of COVID‐19 in Gyeongsangnam‐Do Province in South Korea. Clin Infect Dis 2020. 10.1093/cid/ciaa967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Yan CH, Faraji F, Prajapati DP, Ostrander BT, DeConde AS. Self‐reported olfactory loss associates with outpatient clinical course in Covid‐19. Int Forum Allergy Rhinol 2020;10:821–831. 10.1002/alr.22592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and Covid‐19 in patients presenting with influenza‐like symptoms. Int Forum Allergy Rhinol 2020;10:806–813. 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Yan CH, Prajapati DP, Ritter ML, DeConde AS. Persistent smell loss following undetectable SARS‐CoV‐2. Otolaryngol Head Neck Surg 2020;163:923–925. 10.1177/0194599820934769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Zayet S, Lepiller Q, Zahra H, et al. Clinical features of COVID‐19 and influenza: a comparative study on Nord Franche‐Comte cluster. Microbes Infect 2020;22:481–488. 10.1016/j.micinf.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Zayet S, Klopfenstein T, Mercier J, et al. Contribution of anosmia and dysgeusia for diagnostic of COVID‐19 in outpatients. Infection 2020. 10.1007/s15010-020-01442-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Zou L, Yu T, Zhang Y, Dai L, Zhang Z, Zhang Z. Olfactory and gustatory dysfunctions in patients With COVID‐19 in Wuhan, China. Res Sq 2020. 10.21203/rs.3.rs-28370/v1. [DOI] [Google Scholar]
- 97. Axel R. The molecular logic of smell. Sci Am 1995;273:154–159. [DOI] [PubMed] [Google Scholar]
- 98. Lin W, Ezekwe EA, Zhao Z, Liman ER, Restrepo D. TRPM5‐expressing microvillous cells in the main olfactory epithelium. BMC Neurosci 2008;9:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Lin W, Ogura T, Margolskee RF, Finger TE, Restrepo D. TRPM5‐expressing solitary chemosensory cells respond to odorous irritants. J Neurophysiol 2008;99:1451–1460. [DOI] [PubMed] [Google Scholar]
- 100. Zhou P, Yang X‐L, Wang X‐G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020;579:270–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Hoffmann M, Kleine‐Weber H, Schroeder S, et al. SARS‐CoV‐2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Li W, Moore MJ, Vasilieva N, et al. Angiotensin‐converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 2003;426:450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Wu C, Zheng M. Single‐cell RNA expression profiling shows that ACE2, the putative receptor of Wuhan 2019‐nCoV, has significant expression in the nasal, mouth, lung and colon tissues, and tends to be co‐expressed with HLA‐DRB1 in the four tissues. Preprints 2020. Available at: https://www.preprints.org/manuscript/202002.0247/v1
- 104. Brann D, Tsukahara T, Weinreb C, Logan DW, Datta SR. Non‐neural expression of SARS‐CoV‐2 entry genes in the olfactory epithelium suggests mechanisms underlying anosmia in COVID‐19 patients. bioRxiv 2020. 10.1101/2020.03.25.009084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol 2008;82:7264–7275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Ding Y, He L, Zhang Q, et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS‐CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol 2004;203:622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis 2005;41:1089–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients. J Med Virol 2020. 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Eliezer M, Hautefort C, Hamel A‐L, et al. Sudden and complete olfactory loss function as a possible symptom of covid‐19. JAMA Otolaryngol Head Neck Surg 2020;146:674–675. 10.1001/jamaoto.2020.0832. [DOI] [PubMed] [Google Scholar]
- 110. Yao L, Yi X, Pinto JM, et al. Olfactory cortex and olfactory bulb volume alterations in patients with post‐infectious olfactory loss. Brain Imaging Behav 2018;12:1355–1362. [DOI] [PubMed] [Google Scholar]
- 111. Altundag A, Temirbekov D, Haci C, Yildirim D, Cayonu M. Olfactory cleft width and volume: possible risk factors for postinfectious olfactory dysfunction. Laryngoscope 2020. 10.1002/lary.28524. [DOI] [PubMed] [Google Scholar]
- 112. Stenner M, Vent J, Hüttenbrink KB, Hummel T, Damm M. Topical therapy in anosmia: relevance of steroid‐responsiveness. Laryngoscope 2008;118:1681–1686. [DOI] [PubMed] [Google Scholar]
- 113. Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID‐19 infection. a novel syndrome. Rhinology 2020;58:289–294. [DOI] [PubMed] [Google Scholar]
- 114. Suzuki M, Saito K, Min WP, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope 2007;117:272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Sugiura TA, Mori J, Nakai Y. Midori. An epidemiological study of postviral olfactory disorder. Acta Otolaryngol 1998;118:191–196. [DOI] [PubMed] [Google Scholar]
- 116. Wang JH, Kwon HJ, Jang YJ. Detection of parainfluenza virus 3 in turbinate epithelial cells of postviral olfactory dysfunction patients. Laryngoscope 2007;117:1445–1449. [DOI] [PubMed] [Google Scholar]
- 117. Tian J, Pinto JM, Cui X, et al. Sendai virus induces persistent olfactory dysfunction in a murine model of PVOD via effects on apoptosis, cell proliferation, and response to odorants. PLoS One 2016;11:e0159033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Potter MR, Chen JH, Lobban NS, Doty RL. Olfactory dysfunction from acute upper respiratory infections: relationship to season of onset. Int Forum Allergy Rhinol 2020;10:706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. W‐j G, Z‐y N, Hu Y, et al. clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Benvenuto D, Giovanetti M, Ciccozzi A, Spoto S, Angeletti S, Ciccozzi M. The 2019‐new coronavirus epidemic: evidence for virus evolution. J Med Virol 2020;92:455–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and taste center. Arch Otolaryngol Head Neck Surg 1991;117:519–528. [DOI] [PubMed] [Google Scholar]
- 122. Jafek BW, Murrow B, Michaels R, Restrepo D, Linschoten M. Biopsies of human olfactory epithelium. Chem Senses 2002;27:623–628. [DOI] [PubMed] [Google Scholar]
- 123. Lefèvre N, Corazza F, Valsamis J, et al. The number of X chromosomes influences inflammatory cytokine production following toll‐like receptor stimulation. Front Immunol 2019;10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Moein ST, Hashemian SM, Tabarsi P, Doty RL. Prevalence and reversibility of smell dysfunction measured psychophysically in a cohort of COVID‐19 patients. Int Forum Allergy Rhinol. 2020;10:1127–1135. 10.1002/alr.22680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID‐19. Lancet 2020;395:1014–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Villalba NL, Maouche Y, Ortiz MBA, et al. Anosmia and Dysgeusia in the absence of other respiratory diseases: should COVID‐19 infection be considered? Eur J Case Rep Intern Med 2020;7:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Hummel T, Whitcroft K, Andrews P, et al. Position paper on olfactory dysfunction. Rhinology 2017;54:1–30. [DOI] [PubMed] [Google Scholar]
- 128. Pinto JM, Wroblewski KE, Kern DW, Schumm LP, McClintock MK. Olfactory dysfunction predicts 5‐year mortality in older adults. PLoS One 2014;9:e107541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Liu B, Luo Z, Pinto JM, et al. Relationship between poor olfaction and mortality among community‐dwelling older adults: a cohort study. Ann Intern Med 2019;170:673–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Van Regemorter V, Hummel T, Rosenzweig F, Mouraux A, Rombaux P, Huart C. Mechanisms linking olfactory impairment and risk of mortality. Front Neurosci 2020;14:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Devanand DP, Lee S, Manly J, et al. Olfactory identification deficits and increased mortality in the community. Ann Neurol 2015;78:401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta‐analysis. Int Forum Allergy Rhinol 2016;6:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Iragorri N, Spackman E. Assessing the value of screening tools: reviewing the challenges and opportunities of cost‐effectiveness analysis. Public Health Rev 2018;39:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID‐19 and the otolaryngologist: preliminary evidence‐based review. Laryngoscope 2020;130:2537–2543. 10.1002/lary.28672. [DOI] [PubMed] [Google Scholar]
- 135. Zou Lq LL, Cuevas M, et al. Self‐reported mini olfactory questionnaire (self‐MOQ): a simple and useful measurement for the screening of olfactory dysfunction. Laryngoscope 2019;130:E786–E790. 10.1002/lary.28419. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Figure 1 Subgroup analyses: Prevalence of olfactory dysfunction in COVID‐19 patients from (A) Europe, (B) North America, (C) Asia, and (D) Australia.
Supporting Figure 2 Subgroup analyses: Prevalence of (A) anosmia, (B) hyposmia, and (C) dysosmia in patients with COVID‐19.
Supporting Figure 3 Subgroup analyses: Prevalence of olfactory dysfunction in COVID‐19 patients with (A) subjective and (B) objective olfactory evaluations.
Supporting Figure 4 Subgroup analyses: Prevalence of olfactory dysfunction in (A) severe and (B) non‐severe COVID‐19 patients.
Supporting Figure 5 Sensitivity analyses: Prevalence of olfactory dysfunction in COVID‐19 patients (A) excluding small studies (n < 100), (B) excluding low‐quality studies, (C) excluding studies without COVID‐19 confirmation method being reported, (D) considering only cross‐sectional studies, and (E) excluding outlier studies.
Supporting Figure 6 Galbraith plot identified three studies as the potential sources of heterogeneity.
Supporting Table 1 Search strategy.
Supporting Table 2 Quality assessment of the included cross‐sectional studies.
Supporting Table 3 Quality assessment of the included case–control studies.


