Abstract
With the advent of Covid-19, health workers have been under constant physical and psychological pressure. Italy was among the first countries to face the health emergency in a period of great uncertainty about the virus and the ways to treat patients. The present study aims to analyse the levels of emotional distress (ED) and psychosomatic symptoms (PS) of Italian frontline health workers during the Covid-19 emergency, and their relationship with the evaluation of the institutional responses received.
A survey was available online during the peak of health system overload. Health workers' ED, PS and perceived overall wellbeing were assessed, along with the perceived adequacy of the emotional support, hygiene and safety measures, and protection received from the national government, regional administration and local hospital. A total of 103 questionnaires were collected [Women: 51.5%; mean age, 41.8 years; SD: ±10,7; high-risk zone: 41.7%]. Correlation analyses were applied to investigate the relationship between the measures of emotional distress and psychosomatic symptoms; ANOVA was applied to compare these measures among groups from different risk zones and with different perceived emotional and safety protection.
About half of the health workers showed medium or high scores on emotional exhaustion, exceeded the cut-off for medium, high or very high psychosomatic symptom burdens, felt they have never or rarely been protected by the institutional responses and judged the emotional support received as inadequate; 32% judged the safety and hygiene measures as insufficient. Significant associations were found between measures of ED, PS and perceived change in personal wellbeing. Differences in perceived institutional support and adequacy of hygiene and safety measures related to significant differences in PS and perceived change in personal wellbeing.
ED and PS were widely experienced by frontline health workers. Physical and psychological symptoms were amplified by the perceived lack of institutional support. Ensuring PS and hygiene and safety measures is essential to prevent worsening of health and psychosomatic symptoms in frontline health workers.
Keywords: Psychology, Covid-19, Health workers, Emotional distress, Psychosomatic symptoms, Emotional support, Safety, Hygiene measures
Psychology; Covid-19; Health workers; Emotional distress; Psychosomatic symptoms; Emotional support; Safety; Hygiene measures
1. Introduction
The COVID-19 outbreak placed tremendous and unprecedented pressure on the health care system worldwide, stretching it beyond its capacities (Carter & May, 2020; Ripp et al., 2020). Recent studies on health care workers report high levels of psychological stress and anxiety (Mazza et al., 2020; Montemurro, 2020), psychosomatic symptoms, and higher risk of burnout (Sasangohar et al., 2020) during the COVID-19 epidemic worldwide, although their extent differs (e.g. Italy: Rossi et al., 2020; Spain: Luceño-Moreno et al., 2020; Great Britain: Hunter et al., 2020; China: Cai et al., 2020; Du et al., 2020; Zhang et al., 2020; USA: Shechter et al., 2020). For instance, in the study by Rossi et al. (2020) among Italian Health workers, severe depression, anxiety and high perceived stress were reported respectively by 24.73%, 19.8% and 21.90% respondents. Luceño-Moreno et al. (2020), in their study among health workers in Spain, report that 58.6% suffered anxiety disorder, 46% depressive disorder and 41.1% feel emotionally drained. In the study by Shechter et al. (2020) among USA health workers at a large medical center in New York City, depressive symptoms, anxiety symptoms and acute stress were reported respectively by 48%, 33% and 7% of the respondents. The study by Du et al. (2020) found that 12.7%, 20.1% and 59% of Chinese health workers in Wuhan had, respectively, at least mild depressive and anxiety symptoms, and moderate to severe levels of perceived stress. Differences related to the different exposure to the health emergency (e.g. work load, overload of the intensive care units, physical and psychological support received) and to methodological differences (e.g. instruments, sample, modalities of recruitment) may explain the different extent of psychological distress reported by the studies. Similar psychosocial impacts were reported during highly contagious diseases such as the AIDS epidemic in the early 1980s, the Severe Acute Respiratory Syndrome (SARS) outbreak of 2003 (Avendano et al., 2003; Masur et al., 2003) and, most recently, the Ebola virus epidemic in West Africa in 2014 and 2015 (Lehmann et al., 2016). Worries about becoming infected, fear of death, increase in hygienic and avoidance behaviors, limited resources, longer shifts, disruptions to sleep and to work-life balance, and occupational hazards associated with exposure to contagious are among the factors cited to explain physical and mental fatigue, stress and anxiety and burnout among health workers (Adams and Walls, 2020).
The importance of supporting them through mental health interventions in times of widespread crisis was documented during the previous SARS pandemic (Maunder et al., 2006; Robertson et al., 2004), and has also been documented during the current COVID-19 pandemic, among Wuhan medical and nursing staff (Kang et al., 2020). Kang et al. (2020) found that health workers express a greater need to obtain help from professionals than from close family and friends, either to alleviate acute mental health disturbances or to improve their physical health. Furthermore, the authors found that clinical personnel who had serious psychological problems, compared to less severely affected groups, had accessed fewer printed psychological advice materials (e.g. office brochures) and less psychological guidance publicised through digital media. Previous responses to Middle East Respiratory Syndrome (MERS) show that medical staff tend to believe that measures such as adopting strict infection control, providing PPE and offering practical guidance help protect their mental health (Khalid et al., 2016).
Scholars argue that ensuring the safety and psychological support of frontline health workers during pandemics or emergencies could represent an essential component of disaster preparedness and of preventing mental health problems in frontline health workers (Emanuel et al., 2020; Martland et al., 2020). More widely, the institutional responses to a pandemic crisis could make a difference in the prevalence of psychological distress among health workers and the general population. However, the role of institutional responses and actions in ensuring psychological and material support to health workers in influencing their wellbeing during the COVID-19 emergency remains unexplored.
2. The current study
The present study aims to analyse the levels of emotional distress and psychosomatic symptoms of Italian frontline health workers during the COVID-19 emergency, and their relationship with the evaluation of the received institutional responses.
Italian health workers were among the first to face the health emergency in a period of great uncertainty about the virus and ways to treat patients and avoid infection. On 31 January 2020, the first two confirmed cases of infection due to COVID-19 were reported in Rome. The expansion of the COVID-19 outbreak began in Lombardy, in northern Italy, and spread throughout the country after about one month (Santacroce et al., 2020). As of 15 October, the disease has resulted in 419.759 reported cases and 36.641 deaths; 35545 of those infected with COVID-19 were health workers [Bulletin of the integrated supervision of the Istituto Superiore di Sanità (ISS, Rome) and Istituto Nazionale di Statistica (ISTAT, Rome), updated 15 October 2020]. 181 physicians and 41 nurses have died, leading to suspicions of inadequate protective measures [National Federation of Surgeons and Dentists Orders (FNOMCEO, Rome), updated 15 October 2020].
The impact of the COVID-19 pandemic on the health of Italian health workers has been little explored. Recent studies report high depression symptoms in a percentage of Italian health workers ranged from 24,73% to 32,8%, high anxiety in a percentage from 19,80%–18.7%, high perceived stress from 8.27% to 27.2% (Mazza et al., 2020; Rossi et al., 2020). Italian frontline health workers have been exposed to a persistent source of distress related to a high workload, as well as inadequate devices and supplies to carry out their professional intervention. There have been too few places available in healthcare facilities for the number of patients in critical condition, insufficient human resources, a chronic shortage of healthcare workers, overcrowding in intensive care units, with some patients dying at home while awaiting admission, a concrete risk of being forced to treat only those with a better prognosis, inadequate information on the contagion, insufficient personal protective equipment (PPE), such as gloves and masks, and a paucity of psychological support (Carenzo et al., 2020; Khanna et al., 2020; Paterlini, 2020). This happened within a health system already suffering from a progressive decrease in resources allocated. Today, Italy is below the average for both total health expenditure per capita (USD 3428 vs USD 3980) and public expenditure (USD 2545 vs USD 3038), ahead of only the Eastern European countries and Spain, Portugal and Greece [Organisation for Economic Cooperation and Development (OECD), updated 10 September 2020].
3. Aims and hypotheses
A first aim of the study was to document the frequency of symptoms of emotional distress and psychosomatic diseases were experienced by frontline health workers, given the high workload, disruptions to work-life balance and occupational hazards associated with exposure to COVID-19. Specifically, we examine the subjective feeling of having suffered a worsening of physical and psychological health, the levels of emotional exhaustion, frequency of negative affect and levels of somatic symptoms, included bruxism, whose association with psychological distress has been repeatedly documented as a consequence of automatic stress responses (Cavallo et al., 2014), also in recent studies during the COVID-19 pandemic (Almeida-Leite et al., 2020).
Furthermore, the following hypotheses guide the study.
First, we expect that significant relationships exist between emotional distress and psychosomatic symptoms expressed by the respondents, based on previous literature which recognizes psychosomatic symptoms as a way of communicating emotions (Kleinman, 1997) and a reflection of underlying psychological distress (Lam et al., 2009; Lind et al., 2014) (hypothesis 1).
Second, we expect that emotional distress and psychosomatic symptoms are related to features of the perceived adequacy of the received institutional responses, in terms of psychological support and hygiene and safety measures. Specifically, we expect that the less the perceived support by the institution (at the level of government, regional administration and local health agency), the higher the probability of a perceived worsening of physical and psychological health among frontline health workers (hypothesis 2).
Furthermore, we make an exploratory examination of the differences among groups in different risk zones (high risk/low risk) in terms of emotional distress, psychosomatic symptoms and the perceived adequacy of institutional responses.
Finally, we make an exploratory examination of the kind of material and immaterial support the Italian frontline health workers feel they needed that they did not receive, in order to further investigate their needs and demands during the COVID-19 emergency.
4. Method
An anonymous electronic survey form was available online from 1 April to19 May 2020, coinciding with the peak of the Italian health system overload. In the first phase of the study (the subject of the current work), emotional distress and psychosomatic symptoms were assessed, along with the perceived adequacy of the institutional responses activated to support medical staff (psychological support, hygiene and safety measures, perceived protection by the national government, the regional administration and hospital agency) during the COVID-19 epidemic. In the second phase of the research (currently ongoing), the health workers' subjective experience of the impact of the health emergency on their lives is investigated through their diary entries, completed periodically.
The subjects were recruited on a voluntary basis following a snowball sampling methodology. Accordingly, a small pool of initial informants (physicians, nurses and social care workers) was asked to share the link to the survey through their social networks with other frontline health workers who could potentially contribute to the study.
All procedures performed in the study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. According to the ethical code of the Italian Psychology Association (AIP) (http://www.aipass.org/node/26) and the Italian Code concerning the protection of personal data (Legislative decree No. 101/2018), participants were informed about the general aim of the research, the anonymity of responses and the voluntary nature of participation, and signed an informed consent. No incentive was given. The project was approved by the Ethics Commission for Research in Psychology of the Department of History, Society and Human Studies of the University of Salento (protocol no. 53162 of 30 April 2020).
5. Instruments
The questionnaire for the first phase of the survey was divided into three sections:
5.1. First section: emotional distress and psychosomatic symptoms
The following instruments were administrated in this section:
Emotional exhaustion: emotional exhaustion (EE – the condition of being emotionally, physically and cognitively drained) is a core symptom of burnout (Shirom, 2010); it was assessed using the 9-item EE scale of the Maslach Burnout Inventory (MBI – Maslach and Jackson, 1981; Maslach et al., 1996), which evaluates feelings of being overwhelmed and exhausted by work. Participants rated each item on a 7-point Likert scale ranging from 0–6. The MBI has shown acceptable levels of reliability and validity in Italian studies (Sirigatti et al., 1988). The total score was categorized into three groups according to the distribution of normative Italian data for health care providers: low score between 0–16, moderate between 17–26 and high greater than 26 (Maslach et al., 1996; Sirigatti et al., 1988).
Negative Affect: negative affect (NA) was assessed using the 10-item NA subscale of Positive and Negative Affect Schedule (PANAS). The NA includes items such as afraid, distressed and nervous. Each item is answered using a 5-point scale, from 1 (very slightly or not at all) to 5 (extremely). Participants were asked to mention the extent to which they had experienced a specific emotion over the previous two weeks. The scale presents good psychometric properties in different countries, including Italy (Terraciano et al., 2003). In this study, the alpha value of the NA subscale is .839.
Somatic Symptoms: somatic symptoms (SS) were assessed using the Somatic Symptom Scale-8 (SSS-8). The SSS-8 is an abbreviated version of the Patient Health Questionnaire-15 (Gierk et al., 2014). It consists of 8 items that assess the burden of common somatic symptoms (e.g. joint pain, headaches, stomach or bowel problems, difficulty falling asleep). Each symptom is scored with a 5-point response option that ranges from 0 (I have not been bothered at all) to 4 (I have been bothered very much). The time frame is the previous 7 days. Cut-off scores identify individuals with no to minimal (0–3), low (4–7), medium (8–11), high (12–15) and very high (16–32) somatic symptom burdens. As recommended by Gierk et al. (2014), we dichotomised the score using 12 as the cut-off value to indicate the presence of a high or very high somatic symptom burden. SSS-8 demonstrated good validity and reliability (α = 0.81). In this sample the alpha value is .744.
Bruxism: bruxism symptoms were assessed through 3 items used in previous studies to assess the prevalence and severity of temporomandibular disorders (Cavallo et al., 2016; Cavallo et al., 2014; Fonseca et al., 1994): did you notice that you grind your teeth during the day? Did you notice that you grind your teeth when you sleep? Have you been told (by family, friends…) that you grind your teeth when you sleep? Respondents are asked to answer using a 5-point Likert scale (0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = always). Severity categories were defined in accordance with the percentile ranks associated with respondents' scores. Bruxism symptoms were classified as high if the sum score was between 9 and 12 points (i.e. between the 92nd and 98th percentile); medium between 6 and 8 points (between the 80th and 90th percentile); and 0 to 5 as none or minimal. In this sample the alpha value of the 3 bruxism-related questions is .82.
Change in psycho-physical wellness state: 2 items constructed ad hoc were used, adapted from a study of Rogowska et al. (2020) where the participants were asked to assess their health compared to the situation before quarantine and other studies aimed at assessing specific changes occurring in life, like changed food habits and quality of social relationships (Sharma and Subramanyam, 2020): in our study, one item concerns their physical health, the other their psychological health and the pre-quarantine situation was specified as “previous three months”: Evaluate how your physical/psychological health has changed overall compared to 3 months ago, considering a scale from 0 (Worsened) to 10 (Improved). An average score was calculated for each item.
5.2. Second section: perceived adequacy of the institution's responses to the COVID-19 epidemic
The following instruments were administrated in this section:
Perceived emotional support: 2 items based on Bonanno et al. (2008) study were adopted to assess the perceived quality of emotional support from the social network: do you think the emotional support given to you is adequate? Do you think the emotional support given to you is helpful? As suggested by the authors, an average score (.82) was calculated to obtain a perceived support index.
Perceived protection measures: an ad hoc 4-item questionnaire based on the items used in studies on SARS (Maunder et al., 2003) and hypothetical influenza pandemics (Dionne et al., 2014) was used. The respondents used a 4-point Likert scale to evaluate the feeling of being protected by national and local government and hospital agencies, and the adequacy of the hygiene safety measures applied in one's work context (1 = never; 4 = always).
Perceived protection needs: one open question was used to explore the need for perceived support (material or immaterial) to work during the pandemic: think about your current working conditions. In your opinion, is there anything you need (from a material or immaterial point of view) that was not offered to you?
Experience of COVID-19 contagion: respondents were asked to indicate whether they had had direct or indirect experience of contagion (themselves, a family member, a patient, a colleague, a friend, an acquaintance).
5.3. Third section: sociodemographic and job characteristics
Sex, age range, professional function, years of working experience, work sector (public or private), region and experience of mandatory quarantine were collected in this final section of the survey.
6. Participants
A total of 103 questionnaires were collected from frontline medical and nursing staff (Women: 51.5%; age range 20–59 years [41.8 ± 10,72]). Since the questionnaire was proposed online and only the people willing to participate in the survey completed the form, the number of questionnaires collected coincides with the number of questionnaires analyzed in the current study. Furthermore, the online questionnaire was set up so that sending it was possible only after having answered all the questions, so there were no missing values among the questionnaires collected. The sociodemographic and job characteristics of the sample, disaggregated by risk zone, are reported in Table 1.
Table 1.
Socio-demographic characteristics of respondents, disaggregated for (high/low) risk-zones.
| Variables | Risk Zone |
Total (n = 103) | Chi-square | p-value | ||
|---|---|---|---|---|---|---|
| High Risk | Low risk | |||||
| Sex | Men | 17 (16.5%) | 33 (32.0%) | 50 (48.5%) | 2.398 | .121 |
| Women | 26 (25.2%) | 27 (26.2%) | 53 (51.5%) | |||
| Age range | 20–29 | 9 (8.7%) | 6 (5.8%) | 15 (14.6%) | 10.142 | .017 |
| 30–39 | 15 (14.6%) | 17 (16.5%) | 32 (31.1%) | |||
| 40–49 | 12 (11.7%) | 10 (9.7%) | 22 (21.4%) | |||
| >50 | 7 (6.8%) | 27 (26.2%) | 34 (33.0%) | |||
| Professional function | Surgeon | 31 (30.1%) | 31 (30.1%) | 62 (60.2%) | 4.370 | .112 |
| Nurse | 6 (5.8%) | 15 (14.6%) | 21 (20.4%) | |||
| General practitioner | 6 (5.8%) | 14 (13.6%) | 20 (19.4%) | |||
| Work experience (in years) | Less than 5 | 22 (21.4%) | 16 (15.5%) | 38 (36.9%) | 6.743 | .034 |
| 6–10 | 4 (3.9%) | 6 (5.8%) | 10 (9.7%) | |||
| More than 10 | 17 (16.5%) | 38 (36.9%) | 55 (53.4%) | |||
| Work sector | Public | 40 (38.8%) | 44 (42.7%) | 84 (81.6%) | 6.455 | .011 |
| Private | 3 (2.9%) | 16 (15.5%) | 19 (18.4%) | |||
| Experience of mandatory quarantine | Yes | 11 (10.7%) | 10 (9.7%) | 21 (20.4%) | 1.226 | .268 |
| No | 32 (31.1%) | 50 (48.5%) | 82 (79.6%) | |||
| Contagion experience | Personal or a family member | 9 (8.7%) | 11 (10.7%) | 20 (19.4%) | 10.302 | .016 |
| Patients or colleagues | 29 (28.2%) | 27 (26.2%) | 56 (54.4%) | |||
| Friends or acquaintances | 5 (4.9%) | 13 (12.6%) | 18 (17.5%) | |||
| No experience | 0 (0.0%) | 9 (8.7%) | 9 (8.7%) | |||
High risk and low risk zones were defined on the basis of an index obtained from the ratio between the number of total cases and the number of inhabitants in each region (Nregions = 21; Min = 0.6; Max = 2.42; Mean = .43; SD = .54). Official sources from the Ministry of Health and the Italian National Institute of Statistics (ISTAT) were used to obtain data on the number of deaths from COVID-19 and the number of inhabitants per region respectively. We determined a high risk zone (red zone) using the percentile rank index (i.e. Liguria: .60; Emilia Romagna: .61; Piemonte: .69; Trento: .81; Lombardia: .86; Valle d'Aosta: .94; Bolzano: 2.42).
On the basis of the risk index, 41.7% of the sample work in a high risk zone (red zone) and 58.2% do not; 20.4% of the participants had experienced mandatory quarantine; 19.4% had experienced contagion personally or through a family member whom they live with, 54.4% through a patient or colleague and 17.5% through friends or acquaintances. Only 8.7% declared no close experience with COVID-19.
7. Data analysis
Descriptive analyses were used to describe the general data associated with the measures of emotional distress, psychosomatic symptoms and perceived adequacy of institutional responses.
Correlational analyses were applied to investigate the relationship between the measures of emotional distress and psychosomatic symptoms.
ANOVA was applied to compare the levels of the measures of emotional distress and psychosomatic symptoms among groups differently characterised in terms of perceived adequacy of institutional support received.
ANOVA was applied to explore differences among groups of different risk zones (high risk/low risk) in terms of emotional distress, psychosomatic symptoms and the perceived adequacy of institutional responses. The latter was analysed considering either the responses to the singular items on the perceived protection measures and a global index obtained by the sum of the responses to the same items.
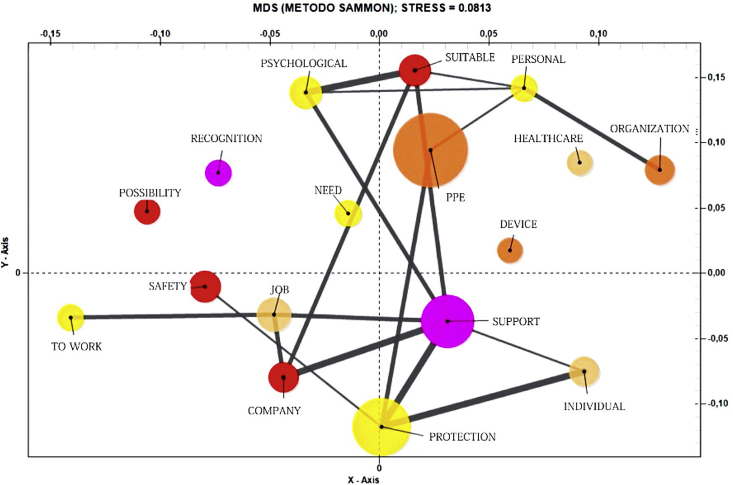
Co-word analysis – performed by T-LAB software (version T-Lab Plus 2020; Lancia, 2020) – was applied to the text collected in response to the open question about unsatisfied needs of perceived support (material or immaterial) to work during the pandemic. Based on the co-occurrence of pairs of words, the analysis allows us to pick out co-occurrence and similarity which, within the text, determine the local meaning of selected key terms. Sammon' s method was used, a type of multidimensional scaling (MDS) that allows one to analyse square matrices which contain proximity values and provides a visual representation of the relationships among the key terms within a factorial space (Lancia, 2020). The degree of correspondence between the distances between points implied by the MDS map and the matrix input is measured (inversely) by a stress function. The lesser the stress value (e.g. < .10), the greater the goodness of the obtained adjustment (Lancia, 2020). In our case, the value of stress is .0813.
8. Results
Descriptive statistics associated with the measures used in this study are reported in Table 2.
Table 2.
Frequency of the variables investigated.
| Variables | Total (n = 103) | |
|---|---|---|
| Emotional exhaustion | Low | 47 (45.6%) |
| Moderate | 27 (26.2%) | |
| High | 29 (28.2%) | |
| Somatic symptom | No to minimal | 21 (20.4%) |
| Low | 26 (25.2%) | |
| Medium | 26 (25.2%) | |
| High | 19 (18.4%) | |
| Very high | 11 (10.7%) | |
| Bruxism symptoms | No to minimal | 74 (71.8%) |
| Medium | 22 (21.4%) | |
| High | 7 (6.8%) | |
| Negative Affect (PANAS) (Response modalities moderately to extremely) |
Afraid | 64 (62.2%) |
| Scared | 53 (51.5%) | |
| Nervous | 63 (61,2%) | |
| Jittery | 48 (46,6%) | |
| Guilty | 14 (13.5%) | |
| Ashamed | 12 (11.6%) | |
| Irritable | 50 (48.6%) | |
| Hostile | 20 (19.4%) | |
| Upset | 54 (52.4%) | |
| Distressed | 43 (41.7%) | |
| Feeling of protection by national government | Never | 19 (18.4%) |
| Rarely | 37 (35.9%) | |
| Sometimes | 39 (37.9%) | |
| Always | 8 (7.8%) | |
| Feeling of protection by regional administration | Never | 19 (18.4%) |
| Rarely | 36 (35.0%) | |
| Sometimes | 41 (39.8%) | |
| Always | 7 (6.8%) | |
| Feeling of protection by hospital agencies | Never | 22 (21.4%) |
| Rarely | 25 (24.3%) | |
| Sometimes | 43 (41.7%) | |
| Always | 13 (12.6%) | |
| Perceived adequacy of the emotional support | Yes | 52 (50.5%) |
| No | 51 (49.5%) | |
| Perceived usefulness of the emotional support | Yes | 66 (64.15%) |
| No | 37 (35.9%) | |
| Feeling of adequacy of the hygiene safety measures | Insufficient | 33 (32.0%) |
| Sufficient | 50 (48.5%) | |
| Highly sufficient | 20 (19.4%) | |
8.1. Emotional distress and psychosomatic symptoms
With respect to the emotional distress and psychosomatic symptoms investigated, 54.4% of the medical staff showed medium (26.2%) or high scores (28.2%) on the emotional exhaustion scale; 54.3% exceeded the cut-off for medium (25,2%), high (18,4%) or very high (10,7%) psychosomatic symptom burdens; 28.2% report medium (21,4%) or high (6,8%) levels of bruxism symptoms. An important part of the sample also reported negative affect (response modality from “moderately” to “extremely”); specifically, 62.2% felt afraid, 61.2% nervous, 52.4% upset, 51.5% scared, 48.6% irritable, 46.6% jittery and 41.7% distressed. An average value of 4 (possible range 0–10) was observed for the perceived worsening of one's physical health (Mean = 4.74; SD = 1.85) and psychological health (Mean = 4.47; SD = 2.17) in the previous three months.
Correlation analysis (Table 3) showed that EE is significantly and positively correlated with negative affect (r = .506; p = < .01), psychosomatic symptoms (r = .428; p = < .01) and bruxism (r = .296; p = < .01, and negatively correlated with the perceived worsening on psychological health (r = -.337; p = .01) and physical health (r = -.318; p = < .01) in the previous three months.
Table 3.
Correlation analysis.
| Measure | EE | NA | SSS-8 | B | PSWS | PHWS |
|---|---|---|---|---|---|---|
| EE | – | |||||
| NA | .506∗∗ | – | ||||
| SSS-8 | .428∗∗ | .416∗∗ | – | |||
| BR | .296∗∗ | .194 | .488∗∗ | – | ||
| PSWS | -.337∗∗ | -.425∗∗ | -.248∗ | -.071 | – | |
| PHWS | -.318∗∗ | -.348∗∗ | -.478∗∗ | -.351∗∗ | .470∗∗ | – |
EE = Emotional exhaustion scale; NA = Negative Affect Scale; SSS-8 = Somatic Symptom Scale-8; BR = Bruxismo items; PSWS = Psychological wellness state; PHWS = Physical wellness state.
∗p < .05; ∗∗p < .01.
8.2. Evaluation of the institutional responses
Significant percentages also emerged from the second area of investigation relating to the adequacy of the national, regional and local response to the COVID-19 epidemic (Table 2). 54.3%, 53,4% and 45,7% of respondents declared that they did feel never or rarely protected by the national government, the regional administration and the local health agency, respectively; 49,5% and 35,9% evaluated respectively no adequate and no helpful the emotional support received and 32% evaluated the safety and hygiene measures as insufficient.
The co-word analysis applied to the terms used by the respondents to describe their unsatisfied material or immaterial needs during the pandemic is shown in Figure 1. The size of the bubbles, which represents the frequency of each keyword within the text, shows that "personal protective equipment" (PPE) had the highest frequency (f = 26), followed by "protection" (f = 18) and "support" (f = 16). The line width, which indicates the strength of the association between the different keywords (the thicker the line, the greater their association in the text segments), shows how these terms are associated with each other; finally, the distance between the bubbles, which indicates the level of association between keywords, shows that PPE tended to occur with terms such as “personal”, “suitable”, “psychological” and “need”, suggesting the psychological value of the safety devices; while “protection” and “support” tended to occur with the terms referring to the working environment (“company” and “job”).
Figure 1.
Dominant keywords in co-word analysis.
8.3. Perceived adequacy of institutional responses and its relationship with health workers' wellbeing
ANOVA showed that the perceived sense of institutional protection significantly varies between groups differently characterised in terms of psychosomatic symptoms [F(1/103) = 5.037; p = < .05] and bruxism [F(1/103) = 6.813; p = < .05] (Table 4). In particular, high perceived adequacy of institutional responses relates to lower scores on psychosomatic symptoms (Mean: 7.33; SD: 4.57), compared to low perceived adequacy (Mean: 9.69; SD: 5.89) and lower scores on bruxism symptoms (Mean: 5.26; SD: 2.80 versus Mean: 6.98; SD: 3.70). Furthermore, groups differently characterised in terms of perceived adequacy of hygiene and safety measures vary in psychosomatic symptoms [F(2/103) = 3.861; p = < .05], and perceived change in psychological health state [F(2/103) = 3.721; p = < .05] and physical health state [F(2/103) = 3.297; p = < .05] in the previous three months. Specifically, health workers who rate the hygiene and safety measures received as highly sufficient: a) manifest lower psychosomatic symptoms (Mean: 7.15; SD: 5.10 versus Mean: 7.80; SD: 5 and Mean: 10.67; SD: 5.76 in the case respectively of perceived sufficient or insufficient measures); and b) perceive a lower worsening of their own state of psychological and physical health state considered on a range from 0 (Worsened) to 10 (Improved) (respectively, psychological wellbeing: Mean: 5.25; SD: 1.65; physical wellbeing: Mean: 5.60; SD: 2.437) compared to those who perceived these measure as sufficient (psychological wellbeing: Mean: 4.96; SD: 1.714; physical wellbeing: Mean: 4.30; SD: 1.94) or insufficient (psychological wellbeing: Mean: 4.09; SD: 2.021; physical wellbeing: Mean: 4.03; SD: 2.172).
Table 4.
Perceived adequacy of institutional responses and its relationship with health workers' wellbeing. Descriptive and ANOVA statistics.
| Measurement tools |
Perceived adequacy of institutional responses |
Perceived hygiene safety measures |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low (n = 48) |
High (n = 55) |
F (p-value) | Insufficient (n = 33) |
Sufficient (n = 50) |
Highly sufficient (n = 20) |
F (p-value) | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |||
| Emotional exhaustion | 21.15 | 12.50 | 17.42 | 11.17 | 2.517 | 22.76 | 14.72 | 19.04 | 10.06 | 14.80 | 10.18 | 2.893 |
| Negative Affect | 24.11 | 7.58 | 22.69 | 6.81 | .990 | 24.64 | 6.84 | 23.00 | 7.40 | 22.60 | 7.56 | .675 |
| Somatic symptom | 9.69 | 5.89 | 7.33 | 4.57 | 5.037∗ | 10.67 | 5.76 | 7.80 | 5.00 | 7.15 | 5.10 | 3.861∗ |
| Bruxism symptoms | 6.98 | 3.70 | 5.26 | 2.80 | 6.813∗ | 6.91 | 3.70 | 6.17 | 3.30 | 5.00 | 2.97 | 1.991 |
| Psychological wellness state | 4.44 | 2.16 | 4.49 | 2.20 | .015 | 4.09 | 2.021 | 4.96 | 1.714 | 5.25 | 1.650 | 3.721∗ |
| Physical wellness state | 4.55 | 1.92 | 4.96 | 1.75 | 1.284 | 4.03 | 2.172 | 4.30 | 1.940 | 5.60 | 2.437 | 3.297∗ |
∗p < .05.
8.4. Differences related to high risk and low risk zones
ANOVA showed that groups belonging to different risk zones vary significantly with respect to EE [F(1/103) = 4.019; p = < .05], with health workers in high risk zones scoring lower (Mean: 16.65; SD: 9.909) than those in to low risk zones (Mean: 21.30; SD: 13.001) (Table 5).
Table 5.
Differences related to high risk and low risk zones. Descriptive and ANOVA statistics.
| Measurement tools |
Risk area |
F (p-value) | |||
|---|---|---|---|---|---|
| High risk area (n = 43) |
Low risk area (n = 60) |
||||
| Mean | SD | Mean | SD | ||
| Emotional exhaustion | 16.65 | 9.909 | 21.38 | 13.001 | 4.019∗ |
| Negative Affect | 23.65 | 6.722 | 23.30 | 7.630 | .059 |
| Somatic symptoms | 9.44 | 5.496 | 7.98 | 5.331 | 1.827 |
| Bruxism symptoms | 3.60 | 3.749 | 2.88 | 3.146 | 1.076 |
| Perceived emotional support | 1.72 | .454 | 1.100 | .896 | 1.304 |
| Psychological wellness state | 4.49 | 2.086 | 4.45 | 2.251 | .008 |
| Physical wellness state | 4.91 | 1.823 | 4.62 | 1.869 | .385 |
| Perceived protection measures | |||||
| By national government | 2.47 | .827 | 2.27 | .899 | 3.515 |
| By regional administration | 2.53 | .882 | 2.22 | .825 | .9.549∗∗ |
| By hospital agency | 2.79 | .888 | 2.22 | .958 | .931 |
| Perceived protection measures Index | 7.79 | 2.144 | 6.70 | 2.196 | 6.300∗ |
| Perceived hygiene safety measures | 1.95 | .615 | 1.82 | .770 | .617 |
∗p < .05; ∗∗p < .01.
Significant differences were found also with respect to the perceived sense of institutional protection [F(2/103) = 6.300; p = < .05] and the perceived sense of regional administration protection [F(2/103) = 9.549; p = < .01]: health workers in high risk zones perceived higher institutional protection (Mean: 7.79; SD: 2.144) than those working in low risk zones (Mean: 6.70; SD: 2.196) and higher protection from their regional administration (Mean: 2.53; SD: .8882 versus Mean: 2.22; SD: .825) (Table 5).
9. Discussion
This study aimed to analyse the levels of emotional distress and psychosomatic symptoms of Italian frontline health workers during the COVID-19 emergency, and their relationship with the evaluation of the institutional responses received.
The findings show that emotional distress and psychosomatic symptoms were widely experienced by Italian frontline medical staff, along with the subjective feeling of having suffered a general worsening of physical and psychological health. Although the cross-sectional nature of the study does not allow us to state that the perceived symptoms and malaise were an effect of the COVID-19 emergency, the findings mirror those of recent studies on the psychological impact of the COVID-19 epidemic on frontline health workers from other countries (e.g. China: Cai et al., 2020; Du et al., 2020; Zhang et al., 2020; Spain: Luceño-Moreno et al., 2020; Great Britain: Hunter et al., 2020; USA: Shechter et al., 2020), as well as previous studies on health workers treating patients with SARS (Avendano et al., 2003; Masur et al., 2003; Maunder et al., 2003). High workload, disruptions to work-life balance, as well as occupational hazards associated with exposure to COVID-19 are commonly recognised factors which may play a principal role in the psychological distress among frontline medical and nursing staff. About one fifth of our sample had experienced contagion personally or through a family member whom they live with and had experienced mandatory quarantine; more than half had experienced the infection of a patient or a colleague. This comes in a period of very high uncertainty about the virus and ways to treat patients and avoid infection, and a lack of general guidelines.
Consistently with hypothesis 1, correlation analysis shows significant relations between measures of emotional distress and psychosomatic symptoms. Although this kind of analysis does not allow one to determine the direction of the association, it is plausible that a circular linkage exists. In their analysis of the impact of the current pandemic on mental health, Xiang et al. (2020) observed that high, uncontrolled stress affected the autonomic nervous system and cortex, potentially leading to psychosomatic and somatic symptoms, which in turn affect psychological problems. Somatic symptoms are hypothesised to represent a way of communicating emotions (Kleinman, 1997) and a consequence of automatic stress responses (Cavallo et al., 2014; Polmann et al., 2019), as found also in previous studies during the COVID-19 pandemic (Almeida-Leite et al., 2020) and SARS (Lam et al., 2009). Many factors may contribute to the expression of psychological distress via physical symptoms, such as professional role (i.e. the need to not manifest discouragement towards patients, colleagues and loved ones), the social-cultural milieu (i.e. the interpretation of health workers as "heroes" committed to saving the nation, which was dominant in the discourses of politicians and journalists) (Cassandro, 2020; Hsin and Macer, 2004; Venuleo et al., 2020a) and social stigma associated with mental health issues among health workers (Chew et al., 2020).
Pressures and distress related to a pandemic emergency constitute only one aspect of the issue. Findings show that more than half of our sample considered themselves not at all or poorly protected by the national government, as well as not at all or poorly protected by their local health agency; the percentage is slightly lower (about 45%) in the case of the regional administration. Almost 50% of respondents judged the emotional support received inadequate; almost 30% rated the safety and hygiene measures received as insufficient. The words most used to describe unsatisfied needs – protection, support and personal protection devices – offer a clear picture of the unfulfilled expectations of frontline health workers, highlighting the paradoxical circumstances of being called to safeguard people's health in the absence of personal physical and psychological protection.
Consistent with hypothesis 2, the findings show that physical and psychological pressure and distress were significantly related to a perceived lack of institutional responses. Specifically, the less the perceived support by the institution (at the level of government, regional administration and local health agency), the higher the probability of experiencing somatic symptoms such as joint pain, headaches, stomach or bowel problems, difficulty falling asleep and bruxism. Furthermore, the less the perceived adequacy of hygiene and safety measures, the higher the likelihood of psychosomatic symptoms as well as a perceived worsening of physical and psychological health in the previous three months. One may suppose that a lack of hygiene and safety measures exposed health workers to greater fear of being infected and to the feeling of being alone, as further sources of distress.
As observed, dissatisfaction with the support received was related significantly to somatic measures, more so than to emotional exhaustion or negative affect. It is plausible that negative feelings toward institutions at different levels (government, regional administration, local health systems) solicited psychological conflicts (e.g. between their roles as health care providers and parents with related fear and guilt about potentially exposing their families to infection; see Maunder et al., 2003) that were difficult to represent to themselves due to their identification with the institutional mission to "save the nation", as “heroes"; a message which strongly characterized institutional and media discourses (Cassandro, 2020). This could also be attributed to the fact that somatization offers the most socially expedient way of communicating distress and dissatisfaction (Kleinman, 1997). Another compatible explanation is that the perceived inadequacy of institutional responses exacerbated concerns related to their somatic symptoms; as suggested by the National Health Commission of the People's Republic of China (2020), some somatic symptoms are similar to those of COVID-19 infection – e.g. gastrointestinal symptoms – and may lead people to suspect that they are infected.
The differences detected among health workers working in high risk or low risk zones deserve comment. Emotional exhaustion was higher among medical and nursing staff working in low risk zones than those in high risk zones. A different result was found in the study of Yuan et al. (2020), showing a significant difference between the group from Hubei Province and the non-endemic provinces in China during the COVID-19 epidemic regarding the degree of anxiety around becoming infected. Our finding is not obvious, but it is understandable. Indeed, if on one hand health workers working in a high risk zone were exposed to greater overwork due to the higher incidence of the coronavirus infection, on the other hand – based on our findings – they were also more satisfied with the protection measures received. It is not surprising, considering the historical differences of economic resources which characterize Northern Italy – the high risk zones, and the low risk zone of Southern Italy, which received also a limited supply of equipment, masks and protective suits for hospitals in the first months of the health emergency. From this perspective, the result is consistent with the idea that the psychological impact of the COVID-19 emergency can be strongly influenced by contextual aspects such as institutional outbreak responses (Venuleo et al., 2020b), calling for a critical reflection on the common representation of a pandemic as a disruptive event that can only produce a disruptive health impact. People's vulnerability is not due only to the natural hazard but is also constructed by social, economic and political conditions (See: Cannon and Müller-Mahn, 2010). As advocated by the World Health Organization (2020) and several scholars (e.g. Ripp et al., 2020; Sim, 2020), institutional responses can play an essential role in preventing psychological and physical problems related to a pandemic crisis among the population and specific vulnerable groups, such as health workers. Duan and Zhu (2020) noted that during lockdown measures, clinical psychiatrists, psychologists and mental health social workers were considered "not essential" personnel and were strongly discouraged from entering isolation wards. This also happened in Italy, where psychological or support health services were interrupted, and offered on the basis of volunteers and local initiatives. Institutions made efforts to protect citizens and to gather and develop the structural and technical resources needed to manage the health emergency (e.g. new doctors and nurses, hospital beds), but marginalised the psychological side of health (Castiglioni and Gaj, 2020) and the impact on it of factors such as work and responsibility overload, grief over the death of patients, fear for their own health and that of their loved ones, and the dilemma of whether to apply for medical leave of absence, or to continue working during this critical period (Li et al., 2020).
We do not expect the worsening of psychological and physical health to end quickly. Studies examining longitudinally the wellbeing impact of previous epidemics such as SARS (Cheng et al., 2004) or other public health emergencies such as earthquakes (Fan et al., 2015) showed that varying degrees of stress disorders were experienced even after the event was over.
10. Conclusive remarks
The acute stress faced by frontline medical and nursing staff during the COVID-19 pandemic emergency, related to working with highly infectious patients in the context of a paucity of material and psychological support and great uncertainty – about the virus and ways to treat patients and avoid infection – needs to be acknowledged.
The discussion above raised the issue of how perceived inadequacy of institutional responses may have fed the already high level of uncertainty faced by health workers, particularly those working on the frontline, influencing their psychological and physical distress.
Providing hygiene and safety measures, psychological support to elaborate the negative affect associated with the death of patients, the responsibility of care and the concern for themselves and their loved ones, guidelines to increase their safety and confidence, and opportunities for them to identify their needs, both at a psychological and a functional level, constitute all important components of mobilising a therapeutic response to crisis scenarios.
Frontline health workers are essential to pandemic response. If they are incapacitated, the ability of countries to respond effectively to the unprecedented challenge imposed by the COVID-19 pandemic will be compromised.
10.1. Limitations
It should be noted that this study has some limitations. First, the limited size and non-randomly selected sample does not allow us to generalize the findings. Cross-national studies may improve our understanding of the impacts of different institutional responses on the health problems of frontline medical and nursing staff and on the constraints and resources that they experienced in responding to the emergency. Second, the cross-sectional design of the study does not allow definitive statements about the relationships between institutional responses and emotional distress and psychosomatic symptoms during the pandemic. Third, the use of self-reported data may be influenced by recall bias and answer accuracy. However, one can argue that, even if unable to offer an objective description of psychological and physical health of frontline medical and nursing staff, self-report measures allow them to detect their perceptions and evaluations of their own health; therefore, they can indicate distress which needs to be seriously considered. Finally, further studies are needed to investigate the role of respondents' psychosocial conditions in moderating or mediating the impact of the institutional responses on the target measures of wellbeing: e.g. the different life situations and the related specific challenges imposed by the pandemic.
Declarations
Author contribution statement
T. Marinaci: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
L. Carpinelli: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data.
C. Venuleo: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
G. Savarese, P. Cavallo: Conceived and designed the experiments; Performed the experiments.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors thank all front-line health care workers that have contributed to this study.
References
- Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- Almeida-Leite C.M., Stuginski-Barbosa J., Conti P.C.R. How psychosocial and economic impacts of COVID-19 pandemic can interfere on bruxism and temporomandibular disorders? J. Appl. Oral Sci. 2020;28 doi: 10.1590/1678-7757-2020-0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avendano M., Derkach P., Swan S. Clinical course and management of SARS in health care workers in Toronto: a case series. CMAJ. 2003;168(13):1649–1660. [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Ho S.M., Chan J.C., Kwong R.S., Cheung C.K., Wong C.P., Wong V.C. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: a latent class approach. Health Psychol. 2008;27(5):659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- Bulletin of the integrated supervision of the Istituto Superiore di Sanità (ISS, Rome) and Istituto Nazionale di Statistica (Istat, Rome) 2020. Sorveglianza Integrata COVID-19 in Italia [Integrated Surveillance COVID-19 in Italy]https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard Retrieved 15th of October, 2020, from: [Google Scholar]
- Cai H., Tu B., Ma J., Chen L., Fu L., Jiang Y., Zhuang Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon T., Müller-Mahn D. Vulnerability, resilience and development discourses in context of climate change. Nat. Hazards. 2010;55(3):621–635. [Google Scholar]
- Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M.…Protti A. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75(7):928–934. doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- Carter D.P., May P.J. Making sense of the US COVID-19 pandemic response: a policy regime perspective. Adm. Theor. Prax. 2020;42(2):265–277. [Google Scholar]
- Cassandro D. 2020. Siamo in guerra! Il coronavirus e le sue metafore [We are at war. The Coronavirus and its metaphors.https://www.internazionale.it/opinione/daniele-cassandro/2020/03/22/coronavirus-metafore-guerra?fbclid=IwAR0kZCnNmLZLENFTAPUIFtkq8bqrabqMe-vEoZpQZ6Wig55XdPEWlzdzRkE L'Internazionale, Retrieved 12th of June, 2020, from: [Google Scholar]
- Castiglioni M., Gaj N. Fostering the reconstruction of meaning among the general population during the COVID-19 pandemic. Front. Psychol. 2020;11:2741. doi: 10.3389/fpsyg.2020.567419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo P., Savarese G., Carpinelli L. Bruxism and health related quality of life in southern Italy's prison inmates. Community Dent. Health. 2014;31:117–122. [PubMed] [Google Scholar]
- Cavallo P., Carpinelli L., Savarese G. Perceived stress and bruxism in university students. BMC Res. Notes. 2016;9(1):514. doi: 10.1186/s13104-016-2311-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Chew N.W., Lee G.K., Tan B.Y., Jing M., Goh Y., Ngiam N.J.…Sharma A.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dionne G., Desjardins D., Lebeau M., Messier S., Dascal A. 2014. Health Care Workers' Risk Perceptions of Personal and Work Activities and Willingness to Report for Work during an Influenza Pandemic. Retrieved 21th of June, 2020, from: SSRN 2405674. [Google Scholar]
- Du J., Dong L., Wang T., Yuan C., Fu R., Zhang L.,., Bouey J. April 3). Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatr. 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatr. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel E.J., Persad G., Upshur R., Thome B., Parker M., Glickman A.…Phillips J.P. Fair allocation of scarce medical resources in the time of COVID-19. N. Engl. J. Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- Fan F., Long K., Zhou Y., Zheng Y., Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol. Med. 2015;45(13):2885–2896. doi: 10.1017/S0033291715000884. [DOI] [PubMed] [Google Scholar]
- Fonseca D.M.D., Bonfante G., Valle A.L.D., Freitas S.F.T.D. Diagnóstico pela anamnese da disfunção craniomandibular. Revista Gaúcha de Odontologia. 1994;42(1):23–28. [Google Scholar]
- Gierk B., Kohlmann S., Kroenke K., Spangenberg L., Zenger M., Brähler E., Löwe B. The somatic symptom scale–8 (SSS-8): a brief measure of somatic symptom burden. JAMA Intern. Med. 2014;174(3):399–407. doi: 10.1001/jamainternmed.2013.12179. [DOI] [PubMed] [Google Scholar]
- Hsin D.H.C., Macer D.R. Heroes of SARS: professional roles and ethics of health care workers. J. Infect. 2004;49(3):210–215. doi: 10.1016/j.jinf.2004.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter E., Price D.A., Murphy E., van der Loeff I.S., Baker K.F., Lendrem D.,., Payne B.A. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395(10234):e77–e78. doi: 10.1016/S0140-6736(20)30970-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R.…Hu S. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalid I., Khalid T.J., Qabajah M.R., Barnard A.G., Qushmaq I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin. Med. Res. 2016;14(1):7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna R.C., Cicinelli M.V., Gilbert S.S., Honavar S.G., Murthy G.S. COVID-19 pandemic: lessons learned and future directions. Indian J. Ophthalmol. 2020;68(5):703–710. doi: 10.4103/ijo.IJO_843_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. University of California Press; Berkeley, CA: 1997. Writing at the Margin: Discourse between Anthropology and Medicine. [Google Scholar]
- Lam M.H.B., Wing Y.K., Yu M.W.M., Leung C.M., Ma R.C., Kong A.P.…Lam S.P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch. Intern. Med. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Lancia F. 2020. User's Manual: Tools for Text Analysis. T-Lab version Plus 2020.https://www.tlab.it/?lang=it Retrieved 21th of June, 2020, from: [Google Scholar]
- Lehmann M., Bruenahl C.A., Addo M.M., Becker S., Schmiedel S., Lohse A.W.…Löwe B. Acute Ebola virus disease patient treatment and health-related quality of life in health care professionals: a controlled study. J. Psychosom. Res. 2016;83:69–74. doi: 10.1016/j.jpsychores.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R.,., Zhou Q. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind A.B., Delmar C., Nielsen K. Struggling in an emotional avoidance culture: a qualitative study of stress as a predisposing factor for somatoform disorders. J. Psychosom. Res. 2014;76(2):94–98. doi: 10.1016/j.jpsychores.2013.11.019. [DOI] [PubMed] [Google Scholar]
- Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 Pandemic. Int. J. Environ. Res. Publ. Health. 2020;17(15):5514. doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martland A.M., Huffines M., Kiersten Henry D.N.P. Surge priority planning COVID-19: critical care staffing and nursing considerations. Chest J. 2020 https://asprtracie.hhs.gov/technical-resources/113/COVID-19-critical-care-surge-resources/99 Retrieved 21th of June, 2020, from: [Google Scholar]
- Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2(2):99–113. [Google Scholar]
- Maslach C., Jackson S.E., Leiter M. third ed. Consulting Psychologists Press; Palo Alto, CA: 1996. Maslach Burnout Inventory Manual. [Google Scholar]
- Masur H., Emanuel E., Lane H.C. Severe acute respiratory syndrome: providing care in the face of uncertainty. JAMA. 2003;289(21):2861–2863. doi: 10.1001/jama.289.21.JED30036. [DOI] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M.…Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. https://www.cmaj.ca/content/168/10/1245.full Retrieved 21th of June, 2020, from: [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S.…Hall L.M. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Publ. Health. 2020;17(9):3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav. Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the people's Republic of China . 2020. Handbook of Prevention and Treatment of the Pneumonia Caused by the Novel Coronavirus (2019-nCoV)http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml Retrieved 12th of June, 2020, from: [Google Scholar]
- National Federation of Surgeons and Dentists Orders (FNOMCEO, Rome) 2020. Elenco dei medici caduti nel corso dell’epidemia COVID-19 [List of the physicians who died during the COVID-19 epidemic]https://portale.fnomceo.it/elenco-dei-medici-caduti-nel-corso-dellepidemia-di-COVID-19/ Retrieved 15 October of 2020, from: [Google Scholar]
- Organisation for Economic Cooperation and Development (OECD) 2020. Health spending.https://data.oecd.org/healthres/health-spending.htm Retrieved 12th of June, 2020, from: [Google Scholar]
- Paterlini M. On the front lines of coronavirus: the Italian response to COVID-19. BMJ. 2020;368:m1065. doi: 10.1136/bmj.m1065. [DOI] [PubMed] [Google Scholar]
- Polmann H., Domingos F.L., Melo G., Stuginski-Barbosa J., Guerra E.N., Porporatti A.L. Association between sleep bruxism and anxiety symptoms in adults: a systematic review. J. Oral Rehabil. 2019;46(5):82–91. doi: 10.1111/joor.12785. [DOI] [PubMed] [Google Scholar]
- Ripp J., Peccoralo L., Charney D. Attending to the emotional wellbeing of the health care workforce in a New York City health system during the COVID-19 pandemic. Acad. Med. 2020:1–4. doi: 10.1097/ACM.0000000000003414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E., Hershenfield K., Grace S.L., Stewart D.E. The psychosocial effects of being quarantined following exposure to SARS: a qualitative study of Toronto health care workers. Can. J. Psychiatr. 2004;49(6):403–407. doi: 10.1177/070674370404900612. [DOI] [PubMed] [Google Scholar]
- Rogowska A.M., Kuśnierz C., Bokszczanin A. Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in polish sample of university students. Psychol. Res. Behav. Manag. 2020;13:797–811. doi: 10.2147/PRBM.S266511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental Health outcomes among front and second line health workers associated with the COVID-19 pandemic in Italy. medRxiv. 2020 doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santacroce L., Charitos I.A., Del Prete R. COVID-19 in Italy: an overview from the first case to date. Electron. J. Gen. Med. 2020;17(6):em235. [Google Scholar]
- Sasangohar F., Jones S.L., Masud F.N., Vahidy F.S., Kash B.A. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth. Analg. 2020;131(1):106–111. doi: 10.1213/ANE.0000000000004866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A.J., Subramanyam M.A. A cross-sectional study of psychological wellbeing of Indian adults during the Covid-19 lockdown: different strokes for different folks. PloS One. 2020;15(9) doi: 10.1371/journal.pone.0238761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S.,., Claassen J. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatr. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirom A. Employee burnout and health: current knowledge and future research paths. In: Houdmont J., Leka S., editors. Vol. 1. Wiley; Chichester, West Sussex, UK: 2010. pp. 59–77. (Contemporary Occupational Health Psychology). [Google Scholar]
- Sim M.R. The COVID-19 pandemic: major risks to healthcare and other workers on the front line. Occup. Environ. Med. 2020;77(5):281–282. doi: 10.1136/oemed-2020-106567. [DOI] [PubMed] [Google Scholar]
- Sirigatti S., Stefanile C., Menoni E. Per un adattamento italiano del Maslach Burnout Inventory (MBI). [Aspects and problems of Italian adaptation of MBI] Bollettino di Psicologia Applicata. 1988;187(188):33–39. [Google Scholar]
- Terraciano A., McCrae R.R., Costa P.T., Jr. Factorial and construct validity of the Italian positive and negative affect Schedule (PANAS) Eur. J. Psychol. Assess. 2003;19(2):131. doi: 10.1027//1015-5759.19.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venuleo C., Gelo C.G.O., Salvatore S. Fear, affective semiosis, and management of the pandemic crisis: Covid-19 as semiotic vaccine? Clin. Neuropsychiatry. 2020;17(2):117–130. doi: 10.36131/CN20200218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venuleo C., Marinaci T., Gennaro A., Palmieri A. The meaning of living in the time of COVID-19. A large sample narrative inquiry. Front. Psychol. 2020;11:2282. doi: 10.3389/fpsyg.2020.577077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. Critical Preparedness, Readiness and Response Actions for COVID-19: Interim Guidance. 22 March 2020 (No. WHO/2019-nCoV/Community_Actions/2020.3) [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatr. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Liao Z., Huang H., Jiang B., Zhang X., Wang Y., Zhao M. Comparison of the indicators of psychological stress in the population of Hubei province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.923767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.R., Wang K., Yin L., Zhao W.F., Xue Q., Peng M.…Chang H. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.