Abstract
The novel coronavirus-2019 (COVID-19) pandemic primarily affects the respiratory system. Elderly individuals with comorbidity are severely affected. Survivors weaned from mechanical ventilation are at a higher risk of developing post-intensive care syndrome (PICS). This scoping review, based on 40 recent publications, highlights pulmonary rehabilitation (PR) in COVID-19. There is a paucity of high-quality research on this topic. However, rehabilitation societies including the Turkish Society of Physical Medicine and Rehabilitation have issued PR recommendations in COVID-19 pneumonia with productive cough can benefit from diaphragmatic breathing, pursed-lip breathing, and resistance-breathing training. Besides, those in mechanical ventilation and post-PICS COVID-19 cases, oxygen therapy, early mobilization, airway clearance, aerobic exercise, gradual-graded limb muscle resistance exercise, nutritional and psychological interventions should be consideration. During PR, careful evaluation of vital signs and exercise-induced symptoms is also required. When in-person PR is not possible, telerehabilitation should be explored. However, the long-term effects of PR in COVID-19 need further evaluation.
Keywords: COVID-19, coronavirus, pandemics, pulmonary rehabilitation, review
Introduction
The novel coronavirus-2019 (COVID-19) pandemic originated in Wuhan, China in late December 2019, and rapidly spread to more than 200 countries all around the globe. Currently, there are more than 19.6 million confirmed cases with 727,435 fatalities.[1] The most common presenting features of COVID-19 are like those in influenza fever, dry cough, sore throat, malaise, myalgia, arthralgia, nasal congestion, sneezing, and runny nose.[2-4] However, different uncommon presentations have been reported including abdominal pain, lack of appetite, vomiting, diarrhea, altered taste sensation and ageusia, bilateral pneumonia, pleural effusion, radiological lung consolidation, altered liver function, lymphadenopathy, acute kidney injury, neurological manifestations and vascular (venous and arterial) thrombosis.[2-6] On the other hand, children may remain asymptomatic and most are only detected on laboratory testing. Nevertheless, some may develop Kawasaki-like signs or Guillain-Barré syndrome, and the course of COVID-19 may be worse in some young cases.[3-5] The main concern in COVID-19 is the involvement of the lungs and respiratory system which may result in dyspnea, low blood oxygen saturation, and respiratory failure, thereby, requiring mechanical ventilation,[3,4] mostly in those having comorbid conditions such as diabetes mellitus, obesity, ischemic heart disease, cancer, post-surgery, and chronic obstructive pulmonary disease (COPD).[3,5]
Patients on mechanical ventilation may also have complicating ventilator-associated pneumonia, acute respiratory distress syndrome (ARDS), pulmonary edema, and atelectasis, pulmonary embolism with right-sided heart failure.[7] These complications may lead to prolonged length of stay in intensive care units (ICUs), prolonged duration of mechanical ventilation, and higher mortality rate.[7] Patients who stay in the ICU are also at risk of developing post-intensive care syndromes (PICS) which are defined as “physical, cognition, and mental impairments that occur during ICU stay, after ICU discharge or hospital discharge, as well as in the long-term follow up of ICU patients”.[8] In addition, COVID-19 patients with extensive lung and respiratory involvements, who are treated under the ICU support, are prone to development of above-mentioned complications. There is evidence that early rehabilitation may improve short-term physical outcomes and quality of life (QoL) in patients with PICS.[9]
Considering that most patients of COVID-19 requiring ICU care have respiratory involvement, we aim to explore whether pulmonary rehabilitation (PR) is an effective intervention in these patients to improve outcomes and reduce mortality. The 2013 American Thoracic Society (ATS)/European Respiratory Society (ERS) Statement defines PR as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long- term adherence of health-enhancing behaviors.”[10] Participation in PR enhances exercise capacity, reduces depression and anxiety, improves Health Related QoL (HRQoL), fatigue, and the strength of respiratory muscles in patients with various forms of respiratory disorders.[10] These improvements are observed in patients with COPD,[11] idiopathic pulmonary fibrosis[12] interstitial lung disease, stroke.[13,14] and lung cancer.[15] Also, PR may have a role in survivors of ARDS, obesity-related respiratory disorders, before and after lung resection, and respiratory impairment related to spinal cord Injury.[16]
In this review, we discuss the role of PR and its recommended strategies in patients with COVID-19 in the light of an extensive review of the literature.
Patients and Methods
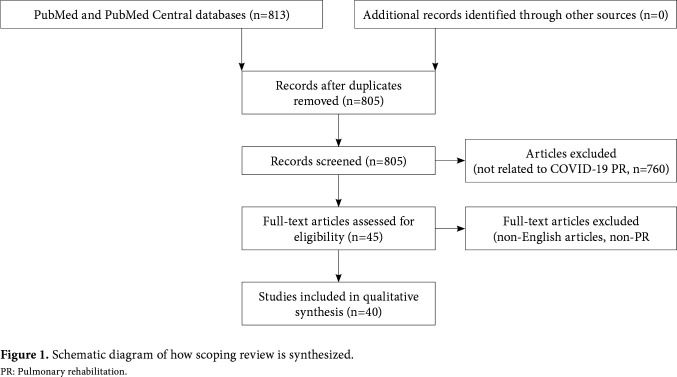
An online literature search was conducted between April 8th, 2020 and August 10th, 2020 using Medline and PubMed Central, restricted to English language. The keywords were as follows: “respiratory rehabilitation” “pulmonary rehabilitation”, “chest physiotherapy”, “chest exercises”, “deep breathing exercises”, “respiratory muscle training”, “cough assistance”, “novel coronavirus”, “SARS-CoV-2” and “COVID-19”. The Boolean Logic (AND, OR and NOT) was employed to generate different combinations of search strings. The websites of The American College of Chest Physicians, American Lung Association, Canadian Thoracic Society, ERS, International Society of Physical Medicine and Rehabilitation and Thoracic Society of Australia and New Zealand (TSANZ) were explored for further insight. Excluded were articles describing clinical features, epidemiology, lung transplantation in COVID-19, COVID-19 non-PR, rehabilitation protocols, and consequences of COVID-19. Articles other than English were excluded. A flowchart (Figure 1) was developed for reporting scoping reviews of research related to PR of COVID-19. The Critical Appraisal Skills Program (CASP) checklist was used to asses articles included.
Figure 1. Schematic diagram of how scoping review is synthesized. PR: Pulmonary rehabilitation.
Results
The literature search resulted in a total of 813 articles (PubMed - 107, PubMed Central - 706). On screening, 40 articles including five consensus-based guidelines specifically discussing PR articles on COVID-19 were selected for this review (Table 1).[17-50] Table 2 lists the consensus-based guidelines.[51-56] The remaining articles regarded clinical features of COVID-19 or rehabilitation strategies other than PR were not included. Of the selected 40 published papers, only one was a randomized-controlled trial (RCT) from China which documented the efficacy of PR in elderly COVID-19 survivors discharged from hospital. The remaining 39 articles were guidelines, perspectives, perspective and analysis, opinion letter, correspondence, letter to editor, cross-sectional study, review paper, recommendations, and position papers. We were unable to find any specific guidelines on PR in COVID-19 on any professional society website. Only the RCT described the usefulness of PR on respiratory function, HRQoL, mobility, and psychological function in elderly COVID-19 survivors discharged from the hospitals in China.[17] The study included one 10-min session, twice per week for a total of six weeks. The outcome parameters included forced expiratory volume in 1 second, (FEV1)/forced vital capacity (FVC), diffusing lung capacity for carbon monoxide (DLCO), 6-min walk test (6MWT), HRQoL (assessed by Short Form-36 [SF-36]), activities of daily living (ADLs) based on Functional Independence Measure (FIM), and mental status tests (Self-Rating Anxiety Scale [SAS] and Self-Rating Depression Scale [SDS]).[17]
Table 1. Summary of manuscripts published on pulmonary rehabilitation in patients with COVID-19.
| Author (s) | Country | Manuscript type | Summary |
| Liu et al.[17] | China | Experimental study | Quasi-experimental study on pulmonary rehabilitation in elderly COVID-19 survivors, weaned off from mechanical ventilation and discharged from hospitals in China. Participants underwent PR over 6 weeks. Improvement was seen in respiratory function (FEV1/FVC), QoL, level of anxiety, physical function (SF-36). There was no significant change in depression. |
| Lazzeri et al.[18] | Italy | Perspective | A position paper authored collaboratively by the Italian Association of Respiratory Therapists and Italian Association of Physiotherapists. The aim was to provide guidelines to the rehabilitation team members working in an inpatient facility that could also be effective in managing severe COVID-19 under ICU support |
| McNeary and Maltser[19] | USA | Emerging issue | A position paper describing CAN report in inpatient rehabilitation facilities, which seems to be effective in COVID-19 cases |
| Smith et al.[20] | England | Perspective | This article describes the clinical presentation of PICS and provides recommendations for physical examination, outcome measures, plan of care, and intervention strategies. It also stresses the importance of educating patients and family, coordinating community resources, and CBR service. The current challenges for patients developing PICS are also discussed. |
| Li[21] | China | Expert opinion | The rehabilitation team should be included in COVID-19 management as any other national disaster that happened before. |
| Mohamed and Alawna[22] | Turkey | Review | Increased aerobic capacity could lead to short-term improvement of immune (an increased function of immune cells and immunoglobulins level) and respiratory system (acting as an antibiotic, antioxidant, and antimycotic, restoring normal lung tissue elasticity and strength) in COVID-19 patients. Aerobic exercise minimizes anxiety and depression. |
| Polastri et al.[23] | Italy | Editorial | Early rehabilitation for COVID-19 patients with respiratory, physical, and psychological impairments is required. Pulmonary rehabilitation algorithm for chronic lung diseases could be useful in COVID-19 patients. However, COVID-19 specific rehabilitation (inpatient, outpatient, and telerehabilitation) setting is required to develop. Inviting technology and reorganizing health system is required to serve increased patient load. |
| Zhu et al.[24] | China | Letter to editor (case report based) | After weaning from ventilation, postural change and prone position improves alveolar gas exchange and reduce pulmonary bacterial infection; spontaneous deep breathing maintains lung recruitment; early post ICU mobilization improves respiratory and diaphragmatic muscle strength; psychological intervention and sleep promotion improve anxiety and depression. |
| Sheehy[25] | Canada | Expert opinion | Major PR should not be at an early stage of lung involvement. |
| Rivera-Lillo et al.[26] Chile | Letter to editor | COVID-19 survivors with long-term pulmonary sequelae and associated comorbidities are straining on the existing healthcare facilities. Developing a trained multidisciplinary rehabilitation team is a must serve the COVID-19 survivors for improved functionality and QoL. | |
| You et al.[27] | China | Letter to editor (case series based) | COVID-19 survivors are documented to have impaired lung function and GGO on chest CT and X-ray. Pulmonary fibrosis can develop in critically ill patients and is linked to impaired lung function, however, to confirm it, long-term study is required. Long-term follow-up outcomes of lung function in COVID-19 survivors help us developing a guideline specific to the disorder. |
| Mo et al.[28] | China | Letter to editor | In COVID-19 survivors, impairment of diffusion capacity and restrictive ventilatory defect both are associated with the severi-ty of the disease. Spirometry and diffusion capacity should be measured in routine clinical follow-up in severe cases. |
| Zha et al.[29] | China | Letter to editor (case report based) | Follow-up of two patients depicted, non-abnormality on both chest radiology and function tests in young COVID-19 case, whereas, the same were eventful in older COVID-19 survivor due to lung fibrosis that could affect patients overall physical abilities |
| Curci et al.[301 | Italy | Cross-sectional study | Based-on oxygen saturation and patients wearing masks - PR could include posture changes (FiO2 >40 and <60%). Bedside, ROM for joints, stretching & pumping exercises for limbs with some exceptions, breathing control, chest-abdomen coordination exercises (promote proper recruitment of diaphragm muscle), clearance techniques; patients without oxygen support devices or wearing nasal cannula (FiO2>21 and <40%) - rehabilitation protocol includes active exercises performed at bedside, balance training in statics and dynamics, program to prevent fall, low-intensity exercises of limb and trunk muscles. Patients able to maintain standing, having adequate muscle strength and respiratory function, walking training could be performed. COVID-19 with FiO2 >21 and <40% further participate in thoracic expansion training, forced inspiration-expiration, incentive spirometer, and bottle Positive Expiratory Pressure utilization. |
| Estraneo and Ciapetti[311 | Italy | Letter to editor | Severe COVID-19 cases develop functional motor deficits impacting weaning from mechanical ventilation, long-term outcomes, and hospital mortality. So, early recognition of neuromuscular impairment and plan for their rehabilitation improve respiratory function and overall clinical outcome. |
| Brugliera et al.[321 | Italy | Perspective | Nutritional management of COVID-19 patients improves clinical outcomes. Nutritional support and the proper rehabilitation including PR improve the likelihood of recovery in COVID-19 patients. |
| Severin et al.[331 | US | Review | Screening of respiratory muscle performance could add value while planning PR in COVID-19 patients with compromised lung function. |
| Pancera et al.[341 | Italy | Case report | Pulmonary rehabilitation in COVID-19 under ventilation due to ARDS including respiratory care, early mobilization, and neuromuscular electrical stimulation started in a rehabilitation center can lead to early weaning from ventilation support, the tracheal cannula removal, and recovering walking capacity followed by increased respiratory muscles strength and function and quadriceps muscle volume in later follow-up. |
| Tay et al.[351 | Singapore | Case report | Robotic therapies prove useful in PR of post-critical care COVID-19 patients as well. |
| Chen et al.[361 | China | Opinion article | Robotic therapies prove useful in PR of post-critical care COVID-19 patients as well. |
| Antonelli and Donelli[371 | Italy | Corre-spondence | Eight-segment traditional Chinese rehabilitation program in association with conventional PR and PNF could improve lung function in COVID-19 |
| Simpson et al.[381 | Canada | Analysis and perspective | Existing Spa facilities could be successfully utilized for post-COVID-19 PR. |
| Bhutani and Robinson[391 | Canada | Position statement | This paper highlights that COVID-19 associated critical illness will greatly impact the existing healthcare facilities. There is a need to design strategies to mitigate the strain, both in acute and post-acute phases. Health care professionals working with COVID-19 need to cooperative across disciplines |
| Bryant et al.[401 | USA | Letter to editor (based-on clinical experience) | Veterans are eligible for the Telehealth program through internet connection from their homes using iPADs, smartphones or computers if they: (1) are medically stable and receiving optimal medical management; (2) have no severe cognitive impairments; (3) able to use a computer and e-mail or have a family member to assist them; and (4) have correctable (glasses or hearing aids) visual and auditory impairments. Instead of assessing 6MWT, manual muscle test, grip strength, and gait, 1-STS to assess exercise capacity and cardiovascular responses, 5 times STS test to assess and monitor muscle strength. Alongside, correct inhaler use, breathing patterns, coughing can be assessed easily with the virtual connection. Questionnaires including Dyspnea Modified Medical Research Council Scale, St. George Respiratory Questionnaire, the COPD Assessment Test, Cardiac Self-Efficacy Scale, Duke Activity Status Index, Rate Your Plate, Extent of Adherence Patient Health Questionnaire-9, and Activities of Daily Living can be administered through Telehealth without difficulty. |
| lannaccone et al.[41] | Italy | Short communication | Reorganization of hospital setup and treatment of patients through different units is required when there is an increased flow of patients. In post-COVID-19 unit, postural variation should be performed several times a day. Patients with ARDS can benefit from prolonged prone positioning (even for >12 hours/day) and during non-invasive ventilation, however, pronation procedure should be interrupted during poor oxygenation. There should be different paths for staff and patients of COVID-19 and non-COVID-19. After hospital discharge, telemedicine was used to follow-up with patients at home. |
| Salawu et al.[42] | UK | Review | Tele-rehabilitation could be useful for PR, psychological support, and nutrition advice for COVID-19 patients, however, those unable to participate in a telerehabilitation program and having balance deficits require face-to-face assessment. COVID-19 patients following discharge from hospital, supervised multidisciplinary telerehabilitation programs should be an integral component of the follow-up. |
| Yang et al.[43] | China | Review | In COVID-19, pulmonary rehabilitation should be individualized and multidisciplinary approach and cooperation is required. |
| Kiekens et al.[44] | Italy | Position paper | In this position paper, from the northern Italy region, the proceeding of a webinar on COVID-19 is summarized. The Webinar was organized by the Italian Society of Physical and Rehabilitation Medicine, regarding respiratory care in acute and post-acute phases. They were also concerned about the impairments that might develop during intubation, for example, muscle weakness, contracture, joint stiffness, dysphagia, poor QoL, amongst others. |
| Yang and Yang'45] | China | Nonspecified | Pulmonary rehabilitation has been mentioned as safe, simple, satisfactory and saving lives. |
| Simonelli et al.[46] | Italy | Short communication | Unexpected and urgent organizational change and roles of Respiratory Physiotherapists' regarding Cardio-Pulmonary Rehabilitation service in COVID-19 emergency in seen in a Northern Italian rehabilitation hospital. RPTs remodeled tasks included: oxygen therapy monitoring, non-invasive ventilation, continuous positive airways pressure delivery, change of posture to improve oxygenation, patients' functional assessment to evaluate motor conditions, and exercise-induced oxygen desaturation. This reorganization badly impacts over professional skills of RPTs, but it could provide practical insights to other facilities facing this crisis like COVID-19. |
| Gitkind et al.[47] | USA | Perspective | Referring patients for rehabilitation should be judged case-case, based-on discussion with other professionals in the multidisciplinary team, less time consuming than before because of patient overload at emergency, rehabilitation specialist now is considered an integral part of a treating team, therapy period should also be readjusted. |
| Wang et al.[48] | US | Analysis-perspective | Pulmonary rehabilitation in COVID-19 should include management of nutrition, air-way, posture, clearance technique, oxygen therapy, breathing exercises, stretching, manual therapy, and physical activity. Outpatient PR should be considered for all patients hospitalized with COVID-19. |
| Vitacca et al.'19 | Italy | Position paper | Consensus promoted by the Italian societies of respiratory health care professionals reveled hospital facilities could be reorganized, and; alongside PR for COVID-19 cases there should a separate path for non-COVID-19 cases PR rehabilitation |
| Grigoletto et al.'50] | Brazil | Editorial | Policy-makers, health care professionals, and healthcare providers should take initiatives to mobilize resources towards building and expanding rehabilitation services including PR to serve the COVID-19 survivors better returning to normal life. |
| CARM: Chinese Association of Rehabilitation Medicine; Respiratory rehabilitation committee of CARM; Cardiopulmonary rehabilitation Group of CSPMR (Chinese Society of Physical Medicine and Rehabilitation); SF-36: Short form 36; FEV1: Forced expiratory volume in one second; FVC: Forced vital capacity; ICU: Intensive care unit; CAN: Conditions, actions and need; CBR: Community based rehabilitation; PICS: Post intensive care syndrome; PR: Pulmonary rehabilitation; QoL: Quality of life; GGO: Ground-glass opacity; ROM: Range-of-motion; FiO2: High inspiratory oxygen fraction; ARDS: Acute respiratory distress syndrome; PNF: Proprioceptive neuromuscular facilitation; VHA: Veterans Health Administration; 6MWT: 6-min walk test; 1-STS: 1-min Sit-to-Stand test. | |||
Table 2. Guidelines recommending pulmonary rehabilitation in patients with COVID-19.
| Guidelines | Country | Summary |
| CARM; Respiratory rehabilitation committee of CARM; Cardiopulmonary rehabilitation Group of CSPMR,[51] and Zhao et al.[52] | China | The five main recommendations for PR in elderly COVID-19 cases are : a) PR in COVID-19 inpatients improve breathlessness, anxiety, and depression, physical function and the quality of life; b) no early PR in critically ill patients; c) teleconsultation for PR; d) regular monitoring during PR is required; e) Personnel involved in PR, safety measures should be ensured |
| Thomas et al.[53] | Multinational | Recommendations designed for utilizing physiotherapy workforce, how to determine physiotherapy requirement, physiotherapy treatment modalities including respiratory care and use of PPE in acute care of adult confirmed or suspected COVID-19 |
| Barker-Davies et al.[54] | UK | A panel of seven teams working at the Defense Medical Rehabilitation Centre, Stanford Hall reached a consensus on rehabilitation issues related to COVID-19 including PR based-on Likert scale (0-10) agreement score - (i)Respiratory complications should be considered in post-COVID-19 patients (Level of agreement: mean score 9.38, 95% CI: 8.92 to 9.85), (ii)Initial assessment is recommended in a timely manner depending on the safety issue, degree of dysfunction, normocapnic respiratory failure and patient's physical and mental status (Level of agreement: mean score 9.00, 95% CI: 8.48 to 9.52). (iii)Low-intensity exercise (<3 METs or equivalent) should be considered in patients on oxygen therapy, increase in exercise intensity according to symptoms (Level of agreement: mean score 8.90, 95% CI: 8.23 to 9.57). |
| Kurtai? Aytur et al.[55] | Turkey | Pulmonary rehabilitation recommendations for adult COVID-19 cases considering contagiousness of COVID-19, recommendations on limited contact of a patient with healthcare providers, and the evidence about possible benefits of PR. Mild disease - individualized approach, general health recommendations (avoid smoking, take plenty of fluid, protein, vitamin C and minerals, and fiber-rich diet), special care of people with disability, no PR; pneumonia - individualized PR (single session, at home) in people with productive cough though, take care of people with disability, follow general health recommendations, use of PPE; severe pneumonia - PR (single session) as per physiatrist recommendations, stop PR if the condition gets worse during PR, use PPE; ARDS - no major PR intervention, general rehabilitation care, for example, bed positioning, early mobilization, airway clearance, and joint ROM are to be initiated by healthcare staff in a rehabilitation facility. |
| Zeng et al.[56] | China | WHO Family of International Classifications (WHO-FICs) frame-work to form an expert consensus on the COVID-19 rehabilitation program including PR. Pulmonary rehabilitation includes thorax mobilizing exercise, expectoration therapy, respiratory training to improve patients' symptoms. Patients' body posture influences diaphragm activity, lung ventilation/perfusion in the lung, and ease breathing. Changed body positioning, active breathing, clapping, and thoracic vibration assists cough expectoration. Gradual and graded resistant breathing training improves breathing experience. Electrical stimulation diaphragmatic trainer, electronic biofeedback could also be useful. Exercise training (endurance, resistance, balance, and coordination training). does not only improves the cardiopulmonary muscle unit but also increase the compensatory ability of the noninvolved organs. However, in COVID-19, the above exercises should be judged judicially, for what strong co-operation between physiatrist and physiotherapist is the key. |
| CARM: Chinese Association of Rehabilitation Medicine; Respiratory rehabilitation committee of CARM; Cardiopulmonary rehabilitation Group of CSPMR: Chinese Society of Physical Medicine and Rehabilitation; PR: Pulmonary rehabilitation; PPE: Personal protective equipment; METs: Metabolic equivalent; CI: Confidence interval; ARDS: Acute respiratory distress syndrome; ROM: Range-of-motion; WHO: World Health Organization; FICs: Family of International Classifications. | ||
In a position paper, the Italian Association of Respiratory Physiotherapists (ARIR) described how to perform and manage mechanical ventilation, and what aspects of rehabilitation could be performed, where patients remained stable.[18]
The Respiratory Rehabilitation Committee of the Chinese Association of Rehabilitation Medicine (CARM) and the Cardiopulmonary Rehabilitation Group of the Chinese Society of Physical Medicine and Rehabilitation (CSPMR) issued a set of recommendations to follow while administering inpatient PR to COVID-19 patients.[19,51,52,57] These recommendations can guide clinical practice and form the basis for PR in COVID-19 patients;[51,52]
Pulmonary rehabilitation would relieve the symptoms of dyspnea, anxiety, and depression and eventually improve physical functions and QoL
For critical inpatients, there should be no early PR interventions
For patients in isolation, PR guidance should be conducted through educational videos, instruction manuals, or remote consultation
Assessment and monitoring should be performed throughout the PR process
Appropriately graded personal protective equipment (PPE) should be used following the present guidelines.
In another position paper, by the American Academy of Physical Medicine and Rehabilitation, the conditions (C), actions (A) and needs (N) principles were described to aid physiatrist and physicians and further staff in acute inpatient rehabilitation facility, general measures to limit spread of COVID-19 during stay, to navigate patients’ care during this public health emergency and establish a treatment plan after patients are discharged.[19] These recommendations are not specific regarding pulmonary aspects of rehabilitation.[19]
Thomas et al.[53] further proposed clinical practice recommendations for acute respiratory care to be effective for COVID-19 patients; i.e., maintaining air- borneprecautions,followingcoughetiquetteandhygiene by both patients and staff, and use of disposable PPE. They also recommended treatments such as aerosol- generating PR procedures (cough and huff during treatment), open suction, naso- and oropharyngeal suctioning, and sputum inductions should ideally be performed in a negative pressure room or in a closed-door single-room by a physiotherapist under the guidance of a physician. Physiotherapist-assisted positioning training of gravity-assisted lung clearance to help ICU staff to manage COVID-19 patients is also recommended under the supervision of a medical doctor.[53] Additional measures should be taken for physiotherapists assisting sputum sample collection.[53]
A panel of seven teams consisting of rehabilitation, sports and exercise medicine, rheumatology, psychiatry, general practice, psychology, and pain specialists working at the Defense Medical Rehabilitation Centre, Stanford Hall, United
Kingdom (UK) developed a consensus statement for rehabilitating COVID-19 including PR; compromised respiratory function and functional limitations should be assessed as early as possible, in association with degree of dysfunction, normocapnic respiratory failure and patient’s physical and mental status. Initially, low intensity exercise (≤3 metabolic equivalent of task [METs] or equivalent) should be considered in those patients requiring oxygen therapy. Progression of therapy would be via exercise intensity, which can be increased gradually based on clinical features.[54]
The Turkish Society of Physical Medicine and Rehabilitation has suggested a set of recommendations to be effective for PR in adult COVID-19 cases. In mild disease, those who are asymptomatic, and ARDS, there should be no major pulmonary interventions; however, in patients with pneumonia with productive cough, PR is required taking safety measures preventing infection transmission.[55] Alongside, patient and caregiver education, smoking cessation, peripheral muscle training, bronchial hygiene, adequate nutrition, healthy mind, oxygen therapy are mentioned important improving lung function.[55]
The World Health Organization (WHO)-Family of International Classifications (FICs) framework forms a consensus report regarding a COVID-19 rehabilitation program including PR. They recommend several techniques to be useful in improving lung function; however, these should be judged considering risk-benefit ratio in a cooperative milieu between physiatrist and other rehabilitation team members.[56]
Table 3 summarizes PR strategies to be effective for COVID-19 based on published works.
Table 3. Summary of pulmonary rehabilitation interventions in COVID-19 patients.
| Parameters | Summary |
| Indications!51-551 | COVID-19 pneumonia/severe pneumonia with a productive cough but medically stable should participate in PR; asymptomatic and pneumonia with a non-productive cough should do aerobic exercises and home-based exercise program. |
| Pre-requisites151-531 | With the good general condition, no fever/dyspnea/tachypnea, normal SpO2 (>90%), decreased viral load, a FiO2 <0.6, RR <40 breaths/min, PEEP <10 cmH2O (1 cmH2O =0.098 kPa), no airway problems, SBP >90 and < 180 mmHg, MAP >65 and <110 mmHg, HR >40 and <120 beats/min, no arrhythmia, MI, DVT, & PE, high LA (>4 mmol/L), Richmond Agitation-Sedation Scale score: -2 to +2, low IP. Understanding between a physiatrist and other rehabilitation team members is also vital. |
| What exercises are to do151-53,551 (individualized exercise program designed by a physiatrist in a multidisciplinary facility) |
In-patient (without ventilation support but require oxygen therapy) - Exercise includes respiratory (breathing exercise - slow inhalation and exhalation through the nose and mouth respectively, pursed-lip & diaphragmatic breathing) and peripheral muscle training, breathing exercise (intensity - between 1.0 & 3.0 METs, twice/day, duration - from 15 to 45 mins.), (low-intensity exercise (1-3 METs) should be considered initially particularly for patients who required oxygen therapy), bed mobilization, aerobic exercise, joint ROM (active/passive) & stretching, positioning with pillow support (upright, semi-sitting, forward-leaning depending on SOB) thrice/day, bronchial hygiene techniques (assisted cough, postural drainage, and percussion), clearance of secretion (chest maneuvers - cupping & huffing), transfer to and from bed-chair, and NMES of limb muscles. In-patient program for an intubated patient - aerosol-generating PR procedures (cough and huff during treatment), gravity-assisted drainage techniques (prone positioning for over 12 hours in ARDS), open suctions, naso- and oropharyngeal suctioning, sputum inductions, should ideally be performed in a negative pressure room or a closed-door single-room under the guidance of a medical doctor. In-patient program (extubated and before hospital discharge) - Exercise includes respiratory (breathing exercise - slow inhalation through the nose and slowly exhales through the mouth, pursed-lip & diaphragmatic breathing) and peripheral muscle training, breathing exercise (between 1.0 & 3.0 METs those requires oxygen therapy), aerobic exercise, joint ROM & stretching, posture change (upright, semi-sitting, forward-leaning depending on SOB), bronchial hygiene techniques (chest cupping), postural drainage with or without chest percussion), encourage huffing, ADL training, transfer to and from bed-chair, balance training, resume slow-paced ambulation, & NMES for limb muscles. Out-patient program (after discharge from hospital and within a community) - (1) Patient education - using a booklet, videos, telehealth, advise healthy lifestyle education, encourage family and social activities. (2) Respiratory rehabilitation: (i) aerobic exercises (individualized walking, brisk walking, slow jogging, and swimming programs should start with low intensity, for a short duration, 3-5 sessions/week, each session lasts between 20 & 30 min. Intermittent exercise for fatigue. (ii)Muscle strength training (resistance training) - starts with a reduced load, and in target muscle group repeat it 8-12 times, 1-3 sets/time, with 2-min rest between sets, 2-3 sessions/week for 6 weeks. Load increased around 5 to 10% each week; (iii)balance training: hands-free balance training under balance trainer; (iv) breathing exercise (intentional breathing exercise and airway clearance techniques) - breathing exercise: posture management, adjust breathing rhythm, huffing, thoracic expansion training, mobilization of respiratory muscle groups; airway clearance techniques: first, forced expiratory techniques to expel sputum and reduce coughing and energy consumption; second, positive expiratory pressure to assist forced expiration (3) ADL guidance: (i) basic ADLs (rehabilitation for bed mobility, transfer, ambulation, dressing, toileting, and bathing); (ii) instrumental ADLs. Targeted intervention by an occupational therapist would be worth consideration. |
| Additional supports are required during PR151,52,55,561 | Caregiver training, patient counseling (about disease, available treatment, benefit of regular rest, sufficient sleep, smoking avoidance), diet rich with protein, fiber, Vitamin C, and minerals, take adequate fluid, single-use PPE, psychological intervention (where appropriate), long-term oxygen therapy (if required), care for immobility, neurologic evaluation, care for comorbidities (chronic lung-cardiac disease, senility, obesity, and organ failure). Consider ICU-acquired weakness, maintain cough etiquette as well, behavioral modification strategies, and vocation-specific support. |
| When to do no exercise151-53,551 | No major breathing exercise in mild pneumonia, pneumonia without a productive cough, ARDS, or asymptomatic COVID-19. Pulmonary rehabilitation is not recommended for severely ill patients or in those conditions are deteriorating. Avoid manual hyperinflation in patients under ventilation and inspiratory muscle training if infection transmission risk is high. |
| Monitoring133-35'52-551 | Vital signs (before, during, and after exercise) should be documented. Before and after PR, pulse oximetry (SpO2), exercise-induced symptoms (perceived exertion, chest tightness, dizziness, headache, blurred vision, palpitations, and profuse sweating) should also be checked. Evaluation should also include Spirometry (FEV1/FVC), FiO2, and 6-MWT; 1-MWT & 1-STS are useful when patients are being followed-up on teleconsultation. Chest X-ray and CT scanning of COVID-19 unveil lung changes before and after PR. |
| PR: Pulmonary rehabilitation; RR: Respiratory rate; SpO2: Oxygen saturation; PEEP: Positive end expiratory pressure; SBP: Systolic blood pressure; MAP: Mean arterial pressure; HR: Heart rate; MI: Myocardial infarction; DVT: Deep vein thrombosis; PE: Pulmonary embolism; LA: Lactic acid; IP: Intracranial pressure; METs: Metabolic equivalent; SOB: Shortness of breath; NMES: Neuromuscular electrical stimulation; ARDS: Acute respiratory distress syndrome; ROM: Range-of-motion; ADL: Activities of daily living; PPE: Personal protective equipment; ICU: Intensive care unit; FEV1: Forced expiratory volume in one second; FVC: Forced vital capacity; FiO2: Fraction of inspired oxygen; 1-MWT: 1-Minute walk test; 6-MWT: 6-min walk test; 1-STS: 1-min Sit-to-Stand test; CT: Computed tomography. | |
Discussion
The COVID-19 pandemic has been transmitting rapidly, leaving few possibilities to conduct high-quality, prospective, clinical trials in large series of patients. Therefore, most of the current protocols are based on preliminary results, expert opinions, consensus of professionals, and learning from experience of previous pandemics of the severe acute respiratory distress syndrome (SARS) virus.[18,21,51-56] There is a need to describe the specific details of such protocols.[18,58]
In severe COVID-19 cases, pulmonary function becomes significantly compromised. Among the patients who are hospitalized, an estimated 15% requires ICU support.[59] Currently there is no definite cure for COVID-19; however, empirical use of antiviral, antibacterial, and disease-modifying anti- inflammatory agents appear to be effective in selective cases. Therefore, the preventive recommendations and guidelines remain crucial, particularly social distancing, staying home strategy, hand hygiene and cough etiquette to prevent transmission of COVID-19.[60-62]
Alongside medicinal interventions, PR should be started at the start of inpatient-stay, throughout the entire stay, and continued at outpatient service and in the community. An important step of PR includes the cleaning of airways at regular intervals, otherwise, bronchial secretions may lead to blocked airways resulting in difficulty breathing. Although the cough is usually nonproductive in COVID-19, productive coughing up phlegm can occur at a later stage.[59] According to a retrospective study, severe COPD patients participated in a three-week in-house PR program that included airway drainage, initiation of long-term oxygen therapy, endurance and strength training, high-intensity inspiratory muscle training, and respiratory physiotherapy for breathlessness. This resulted in a significant improvement (p<0.001) of 6MWT, modified Medical Research Council Dyspnea (mMRC) Score, and FEV1 scores).[63] Supervised early PR in COPD also reduced the mortality risk, hospital readmission, hospital stay, and improved HRQoL, and walking distance.[64] Increased aerobic capacity can improve immune and respiratory function.[22] However, outcomes of these interventions in COVID-19 cases are still to be determined and an algorithm of PR for chronic respiratory conditions could be an acceptable alternative, and technology will be used increasingly to mitigate increased patients’ demands.[23,35]
There should be no major PR interventions for critically ill patients, until they become medically stable or if there are signs of progressive deterioration.[18,51-55] The recommendations by the Chinese, Italian, Turkish, UK and multinational rehabilitation professionals can be a guiding document in this regard (Table 2).[18,51-55] When patients remain intubated, even a slight change in body position can adversely affect the ventilation/perfusion ratio, thereby, mismatching the alveolar gas exchange.[51,52] However, in patients who are weaning from the ICU, postural change and prone-lying position can enhance alveolar gas exchange and excretion of pulmonary secretions and, thus, reduce pulmonary infection incidence; in addition, spontaneous deep breathing and early mobilization maximize respiratory and diaphragmatic muscles strength, and promote respiratory function recovery.[24] Crucially, timing of respiratory exercises in patients releasing from ICU is yet to be determined and it varies from patient to patient.[21,25,53] Regarding these aspects, the physiatrists are responsible for examining patients that need to undergo physical therapy, determining appropriate treatment programs, and deciding to what extent it must be taken by the patient, instructing physical therapists of what treatment to give, and keeping track of the patient- treatment record.[55] The role of the physiatrist is to manage a patient’s medical issues as they participate through the rehabilitation process. A physiatrist would assess the patient and assure that the patient is medically stable to participate in therapies.[55] Despite these differences, both therapists and physiatrists collaborate and communicate to ensure that patients are receiving appropriate treatments in the current COVID-19 pandemic.[23,53,55] Preparing the multidisciplinary rehabilitation team to implement the most effective practices for long-term functionality and QoL is also required.[26]
In COVID-19 survivors following discharge, restrictive ventilatory defect and impaired diffusion capacity are associated with disease severity, chest computed tomography and X-ray delineated ground- glass opacity, and residual impaired lung function,[27] particularly in elderly patients. Therefore, spirometry and DLCO should be considered in routine clinical follow-up for them.[28] Pulmonary fibrotic changes could gradually improve with self-rehabilitation; however, patient's physical abilities are significantly hampered by the limited ventilatory efforts and diffusion capacity. Therefore, starting rehabilitation at the earliest possible opportunity, in advance of patients developing severe or limited ventilatory capability, is of utmost importance.[29]
Furthermore, COVID-19 patients recovering from assisted ventilation report impaired lung function.[7] In post-acute COVID-19 Italian patients, Grade 4-5 dyspnea on mMRC, minimal activity shortness of breath, higher inspired oxygen requirement, and impaired 6MWT performance have been documented.[30] Extubated COVID-19 survivors develop ICU-associated inspiratory (diaphragm) and limb muscles weakness (combined myopathy and neuropathy), limited joint ROM, and overall poor physical function.[31,55,56] Poor nutrition with serum hypoalbuminemia is reportedly linked with ARDS.[32,55]
During PR, respiratory muscle performance is scarcely considered.[33] Test of incremental respiratory enduranceandmaximalinspiratory-expiratorypressure devices appear to be useful in measuring respiratory muscle performance, although their reliability and validity are yet to be tested in COVID-19.[33,55] In adverse conditions such as senility, obesity, inactivity, smoking, and viral infection, respiratory muscle strength becomes compromised further and its force- generating capacity is compensated by increased oxygen demand and consumption due to associated high airway resistance and altered chest wall mechanics.[33] Deep breathing exercise is an important component of PR; however, successful PR depends on coordination between diaphragm strength, trunk-limb posture and balance, joint ROM, nutrition and adequate fluid intake.[24,30,32] Therefore, during early PR these factors should be considered.[30,56] Early inpatient rehabilitation includes respiratory care, bed mobilization, bed-to- chair transfer, sit-to-stand training, assisted walking, and neuromuscular electrical stimulation in limb muscles result in improved respiratory function, quadriceps muscle function, and walking capacity measured on Barthel dyspnea index, quadriceps size, and EuroQoL questionnaire.[30,34] Besides, a dynamic patient-guided robotic suspension system assists in developing ambulation, ADL performance, 6MWT, and 10-meter walk test speed.[35] In COVID-19, an eight-segment traditional Chinese PR exercises regime is considered promising, particularly when prescribed with conventional breathing techniques and proprioceptive neuromuscular facilitation.[36] Existing spa-based rehabilitation facility could be used to rehabilitate COVID-19 PR.[37]
Isolated mental health issues or psychological issue as part of PICS, such as post-traumatic stress disorder, anxiety, and depression are documented in COVID-19 infection.[54,38,65,66] A RCT was performed in 72 Chinese patients who recovered from COVID-19 and showed positive outcomes (p<0.05) regarding FEV1/FVC, 6MWT, SAS, QoL, and FIM scores compared to controls.[17] However, in a short-term study, PR interventions appeared to be ineffective in improving depression levels and, hence, long-term studies are required.[17,65,67] The Respiratory Rehabilitation Committee of CARM, and Cardiopulmonary rehabilitation Group of CSPMR suggest that, apart from easing respiratory distress, improving physical function, and QoL, PR programs can be useful in improving both anxiety and depression.[51] In a Letter to Editor, Zhu et al.[24] further demonstrated that PR in association with psychological intervention and sleep promotion may reduce anxiety and depression in COVID-19 patients. The PR further improves ADL and global functional capacity irrespective of the patient’s age.[68] The COVID-19 patients in isolation may benefit from PR through educational videos, instruction manuals, or telehealth.[19,51] When the inpatient program is completed, self-management and PR counseling can be still conducted by telehealth technologies.[39] However, during telemedicine, we cannot evaluate 6MWT, manual muscle test, grip strength, and gait. Instead, we can implement 1-min Sit-to-Stand test (1-STS) to assess exercise capacity and cardiovascular responses, five-times STS test to assess and monitor muscle strength, oxygen saturation status, and prescribed exercises to patients. Telehealth is cost-effective, and neither patients nor physicians require to travel, and it can serve all individuals irrespective of geographical location, although it seems to be unrealistic in developing countries.[39-41] For patients who are unable to participate in a telerehabilitation program and require input for impaired balance, a face-to-face interview is considered an appropriate measure.[42]
In a recent retrospective inception cohort, early PR of COPD patients within 90 days of hospital discharge was associated with a significantly lower death risk over one year (hazard ratio [HR], 0.63, 95% confidence interval [CI]: 0.57 to 0.69 (p <0.001).[34] Additional PR sessions were also associated with a reduced death risk (HR, 0.91, 95% CI: 0.85 to 0.98, p=0.01).[69] Besides, patients who adhere to PR techniques for a long-time, usually require less utilization of healthcare utilization than non-adherent patients. However, longitudinal cohort studies addressing these facts in COVID-19 survivors are still required.[10,70]
Moreover, COVID-19 patients may have simultaneously lung and cardiac problems. Autopsied COVID-19 lung tissue revealed diffuse alveolar damage, bronchial mucosa, focal interstitial thickening, intra-alveolar hemorrhages and intra-alveolar fibrin cluster formation, with compromised respiratory function.[71,72] Besides, COVID patients with previous cardiac problem or COVID-19 associated myocarditis are at an increased risk of hospital morbidity and mortality.[73] Therefore, strategies of PR may not be similar for all COVID-19 survivors, rather these may vary depending on the extent of lung injury and cardiac status. Yeo et al.[74] recommended existing cardiac rehabilitation programs to be continued in COVID- 19 survivors; however cardiovascular comorbidity might adversely affect the magnitude of gains made in PR.[10,75] Therefore, revision of existing cardiac rehabilitation strategies in COVID-19 individuals should be considered and should be matched according to the current cardiac and pulmonary status.[76]
Pulmonary rehabilitation seems to be safe in COVID-19 pneumonia.[64,43] However, it must be individualized and be led by a prudent multidisciplinary approach including a physiatrist, occupational, speech-language, and swallowing therapists, to greatly increase the likelihood of acute and longer-term positive outcomes.[65,43-45,77] Clinically significant, but undiagnosed dysphagia can occur in patients undergoing PR. Dysphagia education and screening as part of a PR program can improve swallowing-related QoL and overall self-management of COPD and dysphagia.[78] Combined resistive inspiratory and expiratory muscle training can improve signs and symptoms of dysphagia as seen in stroke patients.[79] Similarly, personalized occupational therapy consisting of education, breathing control techniques, and breathing exercises is reported to improve FVC and overall survival rate in chronic lung disorders.[80] We are still curious about whether they would be equally effective in COVID-19 survivors with impaired lung function.
The COVID-19 is highly contagious; as PR team members work in close contact with the patients, they remain among the most vulnerable group of individuals, hence any rehabilitation plan should include a plan to make optimal use of a limited rehabilitation workforce. A Business Continuity Plan (BCP), - an organizational strategy, can be one of the best probable approaches. In BCP, splitting the medical team (a physical division of workforce into sub-teams), restricted movement amongst team members (to reduce cross-infection among team members), and work- from-home arrangements are considered useful.[77] To overcome patient load, organizational changes and remodeling of tasks of healthcare professionals are sometimes required, as seen in a Northern Italian rehabilitation hospital;[46] however, in a rehabilitation unit, a physiatrist is the ultimate authority and is responsible for monitoring patients’ nutrition, posture, airway, breathing, oxygen supply, and physical activity; physiatrist‐to‐physician communication in a multidisciplinary setting hasten the decision‐making process regarding patients’ referral to a rehabilitation unit.[47,48,55] The Italian societies of respiratory healthcare professionals promoted a position paper focused on the COVID-19 crisis, stressing that there should be separate PR facilities for both COVID-19 and non-COVID-19 cases.[49] In COVID-19 cases, the field of physical medicine and rehabilitation has been also faced with many challenges and is being acknowledged as an integral part of the healthcare system in the healthcare system of the United States. This includes taking care of patients transferred out of the acute care hospital into rehabilitation beds, thereby, releasing pressure on emergency departments.[49]
An important challenge for physiatrists working in a developing country such as Bangladesh would be the resettling of recovered COVID-19 survivors in their community. Based-on previous study, community-based PR in chronic lung disorders appears to be feasible and effective. Since COVID-19 may remain asymptomatic, survivors can get re-infected, and there is an absence of acknowledged or evidenced cure to date, COVID-19-PR at the community level could be a difficult task for the rehabilitation personnel.[47,81] Community-based rehabilitation for COVID-19 cases with compromised lung function requiring PR should be different from that of non- COVID-19 cases, as recurrences may occur even after complete recovery.[82] The response of society toward the COVID-19 survivors may also complicate community- based PR of COVID-19 cases. However, the ultimate success of COVID-19 PR-program at community would depend on availability and distribution of rehabilitation services in the community, skilled rehabilitation personnel, prudent PR care, sufficient protective measures for both patients and rehabilitation staff, caregiver training, the attitude of society toward
COVID-19, and survivors psychological status, and the state’s policy regarding financing toward COVID-19 PR.[50,83,84]
By adopting the following strategies, healthcare facilities can improve the quality of PR services for COVID-19 patients having respiratory impairment:
Involvement of rehabilitation professionals (physiatrists, respiratory therapists, speech- language and swallowing therapists, occupational, and physical therapists) in the clinical care of COVID-19 patients admitted to ICU to reduce pulmonary complications and to enhance functional recovery.
The rehabilitation team involved in COVID-19 care should consult existing medical guidelines and relevant literature for best evidence, but, at the same time, device own strategies and protocols considering their own resources and patient inf low.
Considering community-based PR of COVID-19 survivors with compromised lung function; it is important to involve politicians, community leaders, professionals, common people, and family members in the process result in positive outcomes.
Conducting further research is needed to generate evidence-based methods for effective PR; focusing on optimal dose, duration, intensity and frequency, specifically designed for COVID-19 patients. In conclusion, growing evidence suggest that PR appears to be useful in COVID-19 survivors. The PR programs starting already in hospital may lead to reduced hospital stay and improved overall respiratory function. Guiding principles have been proposed by the experts from China, Italy, UK, and Turkey. These may be adapted according to local needs and, in this regard global rehabilitation societies, such as the International Society of Physical Medicine, can play an active role. Further prospective clinical studies are needed to unveil which PR programs are safe and effective in COVID-19 survivors, with the goal of improving their QoL beyond their stay within an emergency care facility.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.World Health Organization. Coronavirus disease (COVID-19). Available at: https://covid19.who.int/?gclid=EAIaIQobChMIkofT-PTP6QIViMEWBR2dIAiYEAAYASAAEgLyc_D_BwE . [Accessed: August 10, 2020].
- 2.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khalifa M, Zakaria F, Ragab Y, Saad A, Bamaga A, Emad Y, et al. Guillain-Barré syndrome associated with severe acute respiratory syndrome coronavirus 2 detection and coronavirus disease 2019 in a child. J Pediatric Infect Dis Soc. 2020;9:510–513. doi: 10.1093/jpids/piaa086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331–100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11–11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyer AF, Schoenberg N, Babcock H, McMullen KM, Micek ST, Kollef MH. A prospective evaluation of ventilator- associated conditions and infection-related ventilator- associated conditions. Chest. 2015;147:68–81. doi: 10.1378/chest.14-0544. [DOI] [PubMed] [Google Scholar]
- 8.Muscedere J, Sinuff T, Heyland DK, Dodek PM, Keenan SP, Wood G, et al. The clinical impact and preventability of ventilator-associated conditions in critically ill patients who are mechanically ventilated. Chest. 2013;144:1453–1460. doi: 10.1378/chest.13-0853. [DOI] [PubMed] [Google Scholar]
- 9.Brown SM, Bose S, Banner-Goodspeed V, Beesley SJ, Dinglas VD, Hopkins RO, et al. Approaches to Addressing Post-Intensive Care Syndrome among Intensive Care Unit Survivors. A Narrative Review. Ann Am Thorac Soc. 2019;16:947–956. doi: 10.1513/AnnalsATS.201812-913FR. [DOI] [PubMed] [Google Scholar]
- 10.Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/ European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. e13-64Am J Respir Crit Care Med. 2013;188 doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. CD003793Cochrane Database Syst Rev. 2015;2 doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaunaurd IA, Gómez-Marín OW, Ramos CF, Sol CM, Cohen MI, Cahalin LP, et al. Physical activity and quality of life improvements of patients with idiopathic pulmonary fibrosis completing a pulmonary rehabilitation program. Respir Care. 2014;59:1872–1879. doi: 10.4187/respcare.03180. [DOI] [PubMed] [Google Scholar]
- 13.Menezes KK, Nascimento LR, Ada L, Polese JC, Avelino PR, Teixeira-Salmela LF. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J Physiother. 2016;62:138–144. doi: 10.1016/j.jphys.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 14.Liaw MY, Hsu CH, Leong CP, Liao CY, Wang LY, Lu CH, et al. Respiratory muscle training in stroke patients with respiratory muscle weakness, dysphagia, and dysarthria - a prospective randomized trial. e19337Medicine (Baltimore) 2020;99 doi: 10.1097/MD.0000000000019337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harada H, Yamashita Y, Misumi K, Tsubokawa N, Nakao J, Matsutani J, et al. Multidisciplinary team-based approach for comprehensive preoperative pulmonary rehabilitation including intensive nutritional support for lung cancer patients. e59566PLoS One. 2013;8 doi: 10.1371/journal.pone.0059566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rochester CL, Fairburn C, Crouch RH. Pulmonary rehabilitation for respiratory disorders other than chronic obstructive pulmonary disease. Clin Chest Med. 2014;35:369–389. doi: 10.1016/j.ccm.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract. 2020;39:101166–101166. doi: 10.1016/j.ctcp.2020.101166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR) Monaldi Arch Chest Dis. 2020;90:163–168. doi: 10.4081/monaldi.2020.1285. [DOI] [PubMed] [Google Scholar]
- 19.McNeary L, Maltser S, Verduzco-Gutierrez M. Navigating coronavirus disease 2019 (Covid-19) in physiatry: A CAN report for inpatient rehabilitation facilities. PM R. 2020;12:512–515. doi: 10.1002/pmrj.12369. [DOI] [PubMed] [Google Scholar]
- 20.Smith JM, Lee AC, Zeleznik H, Coffey Scott JP, Fatima A, Needham DM, et al. Home and community-based physical therapist management of adults with post-intensive care syndrome. Phys Ther. 2020;100:1062–1073. doi: 10.1093/ptj/pzaa059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J. Rehabilitation management of patients with COVID- 19: lessons learned from the first experience in China. Eur J Phys Rehabil Med. 2020;56:335–338. doi: 10.23736/S1973-9087.20.06292-9. [DOI] [PubMed] [Google Scholar]
- 22.Mohamed AA, Alawna M. Role of increasing the aerobic capacity on improving the function of immune and respiratory systems in patients with coronavirus (COVID-19): A review. Diabetes Metab Syndr. 2020;14:489–496. doi: 10.1016/j.dsx.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polastri M, Nava S, Clini E, Vitacca M, Gosselink R. COVID-19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J. 2020;55:2001822–2001822. doi: 10.1183/13993003.01822-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu C, Wu Y, Liu H, Ban Y, Ma X, Zhang Z. Early pulmonary rehabilitation for SARS-CoV-2 pneumonia: Experience from an intensive care unit outside of the Hubei province in China. Heart Lung. 2020;49:449–450. doi: 10.1016/j.hrtlng.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehy LM. Considerations for Postacute Rehabilitation for Survivors of COVID-19. e19462JMIR Public Health Surveill. 2020;6 doi: 10.2196/19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rivera-Lillo G, Torres-Castro R, Fregonezi G, Vilaró J, Puppo H. Challenge for rehabilitation after hospitalization for COVID-19. Arch Phys Med Rehabil. 2020;101:1470–1471. doi: 10.1016/j.apmr.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.You J, Zhang L, Ni-Jia-Ti MY, Zhang J, Hu F, Chen L, et al. Anormal pulmonary function and residual CT abnormalities in rehabilitating COVID-19 patients after discharge. e150-e2J Infect. 2020;81 doi: 10.1016/j.jinf.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mo X, Jian W, Su Z, Chen M, Peng H, Peng P, et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020;55:2001217–2001217. doi: 10.1183/13993003.01217-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zha L, Shen Y, Pan L, Han M, Yang G, Teng X, Tefsen B. Follow-up study on pulmonary function and radiological changes in critically ill patients with COVID-19. J Infect. 2020 doi: 10.1016/j.jinf.2020.05.040. S0163-4453(20)30317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curci C, Pisano F, Bonacci E, Camozzi DM, Ceravolo C, Bergonzi R, et al. Early rehabilitation in post-acute COVID- 19 patients: data from an Italian COVID-19 rehabilitation unit and proposal of a treatment protocol. A cross-sectional study. . Eur J Phys Rehabil Med. 2020 doi: 10.23736/S1973-9087.20.06339-X. [DOI] [PubMed] [Google Scholar]
- 31.Estraneo A, Ciapetti M, Gaudiosi C, Grippo A. Not only pulmonary rehabilitation for critically ill patients with COVID-19. J Neurol. 2020:1–3. doi: 10.1007/s00415-020-10077-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brugliera L, Spina A, Castellazzi P, Cimino P, Arcuri P, Negro A, et al. Nutritional management of COVID-19 patients in a rehabilitation unit. Eur J Clin Nutr. 2020;74:860–863. doi: 10.1038/s41430-020-0664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Severin R, Arena R, Lavie CJ, Bond S, Phillips SA. Respiratory muscle performance screening for infectious disease management following COVID-19: A Highly Pressurized Situation. Am J Med. 2020;133:1025–1032. doi: 10.1016/j.amjmed.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pancera S, Galeri S, Porta R, Pietta I, Bianchi LNC, Carrozza MC, et al. Feasibility and efficacy of the pulmonary rehabilitation program in a rehabilitation center: Case report of a young patient developing severe COVID-19 acute respiratory distress syndrome. J Cardiopulm Rehabil Prev. 2020;40:205–208. doi: 10.1097/HCR.0000000000000529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tay SS, Neo EJ, Tan MM, Tan PL. Post-critical care COVID- 19 patient benefits from a robotic patient-guided suspension system for pulmonary rehabilitation. Ann Acad Med Singap. 2020;49:401–404. [PubMed] [Google Scholar]
- 36.Chen JM, Wang ZY, Chen YJ, Ni J. The Application of Eight- Segment Pulmonary Rehabilitation Exercise in People With Coronavirus Disease 2019. Front Physiol. 2020;11:646–646. doi: 10.3389/fphys.2020.00646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Antonelli M, Donelli D. Respiratory rehabilitation for post- COVID19 patients in spa centers: first steps from theory to practice. Int J Biometeorol. 2020;64:1811–1813. doi: 10.1007/s00484-020-01962-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 Infection. Am J Phys Med Rehabil. 2020;99:470–474. doi: 10.1097/PHM.0000000000001443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhutani M, Hernandez P, Bourbeau J, Dechman G, Penz E, Aceron R, et al. Key highlights of the canadian thoracic society's position statement on the optimization of COPD management during the coronavirus disease 2019 pandemic. Chest. 2020;158:869–872. doi: 10.1016/j.chest.2020.05.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bryant MS, Fedson SE, Sharafkhaneh A. Using telehealth cardiopulmonary rehabilitation during the COVID-19 Pandemic. J Med Syst. 2020;44:125–125. doi: 10.1007/s10916-020-01593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iannaccone S, Castellazzi P, Tettamanti A, Houdayer E, Brugliera L, de Blasio F, et al. Role of rehabilitation department for adult individuals with COVID-19: The experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil. 2020;101:1656–1661. doi: 10.1016/j.apmr.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A Proposal for multidisciplinary tele-rehabilitation in the assessment and rehabilitation of COVID-19 survivors. Int J Environ Res Public Health. 2020;17:4890–4890. doi: 10.3390/ijerph17134890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang F, Liu N, Hu JY, Wu LL, Su GS, Zhong NS, et al. Pulmonary rehabilitation guidelines in the principle of 4S for patients infected with 2019 novel coronavirus (2019- nCoV) Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:180–182. doi: 10.3760/cma.j.issn.1001-0939.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 44.Kiekens C, Boldrini P, Andreoli A, Avesani R, Gamna F, Grandi M, et al. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56:323–326. doi: 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- 45.Yang LL, Yang T. Pulmonary rehabilitation for patients with coronavirus disease 2019 (COVID-19) Chronic Dis Transl Med. 2020;6:79–86. doi: 10.1016/j.cdtm.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simonelli C, Paneroni M, Fokom AG, Saleri M, Speltoni I, Favero I, et al. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: an experience from Northern Italy. Monaldi Arch Chest Dis. 2020:90–90. doi: 10.4081/monaldi.2020.1085. [DOI] [PubMed] [Google Scholar]
- 47.Gitkind AI, Levin S, Dohle C, Herbold J, Thomas M, Oh-Park M, et al. Redefining Pathways into Acute Rehabilitation during the COVID-19 Crisis. PM R. 2020;12:837–841. doi: 10.1002/pmrj.12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99:769–774. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vitacca M, Carone M, Clini EM, Paneroni M, Lazzeri M, Lanza A, et al. Joint statement on the role of respiratory rehabilitation in the COVID-19 Crisis: The Italian position paper. Respiration. 2020;99:493–499. doi: 10.1159/000508399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grigoletto I, Cavalheri V, Lima FF, Ramos EMC. Recovery after COVID-19: The potential role of pulmonary rehabilitation. Braz J Phys Ther. 2020 doi: 10.1016/j.bjpt.2020.07.002. S1413-3555(20)30560-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chinese Association of Rehabilitation Medicine; Respiratory Rehabilitation Committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation Recommendations for respiratory rehabilitation of coronavirus disease 2019 in adult. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:308–314. doi: 10.3760/cma.j.cn112147-20200228-00206. [DOI] [PubMed] [Google Scholar]
- 52.Zhao HM, Xie YX, Wang C. Chinese Association of Rehabilitation Medicine; Respiratory Rehabilitation Committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary Rehabilitation Group of Chinese Society of Physical Medicine and Rehabilitation. Recommendations for respiratory rehabilitation in adults with coronavirus disease 2019. Chin Med J (Engl) 2020;133:1595–1602. doi: 10.1097/CM9.0000000000000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66:73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54:949–959. doi: 10.1136/bjsports-2020-102596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kurtaiş Aytür Y, Köseoğlu BF, Özyemişçi Taşkıran Ö, Ordu-Gökkaya NK, Ünsal Delialioğlu S, Sonel Tur B, et al. Pulmonary rehabilitation principles in SARS- COV-2 infection (COVID-19): A guideline for the acute and subacute rehabilitation. Turk J Phys Med Rehabil. 2020;66:104–120. doi: 10.5606/tftrd.2020.6444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zeng B, Chen D, Qiu Z, Zhang M, Wang G, Rehabilitation Group of Geriatric Medicine branch of Chinese Medical Association, division of Management of Medical Rehabilitation Institution of Chinese Hospital Association, Rehabilitation Institution Management division of Chinese Rehabilitation Medical Association, division of Rehabilitation Psychology, Chinese Psychological Association, division of Disability Classification Research, Chinese Association of Rehabilitation of Disabled Persons Expert consensus on protocol of rehabilitation for COVID- 19 patients using framework and approaches of WHO International Family Classifications. Aging Med (Milton) 2020;3:82–94. doi: 10.1002/agm2.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.ISPMR 2020 (International Society of Physical and Rehabilitation Medicine) ISPMR National Societies. Available at: https://www.isprm.org/natsoc/ [Accessed: May 25, 2020].
- 58.Boldrini P, Bernetti A, Fiore P, SIMFER Executive Committee, SIMFER Committee for International Affairs Impact of COVID-19 outbreak on rehabilitation services and Physical and Rehabilitation Medicine physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER) Eur J Phys Rehabil Med. 2020;56:316–318. doi: 10.23736/S1973-9087.20.06256-5. [DOI] [PubMed] [Google Scholar]
- 59.Guimarães F. Approach of the physiotherapist in intensive care units in the context of the COVID-19 pandemic. e0033001Fisioter Mov Curitiba. 2020;33 [Google Scholar]
- 60.Coronavirus COVID-19 Dashboard. 2020 Available at: http://103.247.238.81/webportal/pages/covid19.php. [Accessed: May 25, 2020].
- 61.Coronavirus disease (COVID-19) advice for the public. World Health Organization (WHO) Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. [Accessed: May 25, 2020].
- 62.Hou C, Chen J, Zhou Y, Hua L, Yuan J, He S, et al. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID-19): A well-mixed SEIR model analysis. J Med Virol. 2020;92:841–848. doi: 10.1002/jmv.25827. [DOI] [PubMed] [Google Scholar]
- 63.Greulich T, Koczulla AR, Nell C, Kehr K, Vogelmeier CF, Stojanovic D, et al. Effect of a three-week inpatient rehabilitation program on 544 consecutive patients with very severe COPD: A retrospective analysis. Respiration. 2015;90:287–292. doi: 10.1159/000436979. [DOI] [PubMed] [Google Scholar]
- 64.Ryrsø CK, Godtfredsen NS, Kofod LM, Lavesen M, Mogensen L, Tobberup R, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD- exacerbations: a systematic review and meta-analysis. BMC Pulm Med. 2018;18:154–154. doi: 10.1186/s12890-018-0718-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gracely RH, Ceko M, Bushnell MC. Fibromyalgia and depression. Pain Res Treat. 2012;2012:486590–486590. doi: 10.1155/2012/486590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 67.Khan F, Amatya B. Medical rehabilitation in pandemics: Towards a new perspective. jrm00043J Rehabil Med. 2020;52 doi: 10.2340/16501977-2676. [DOI] [PubMed] [Google Scholar]
- 68.Baltzan MA, Kamel H, Alter A, Rotaple M, Wolkove N. Pulmonary rehabilitation improves functional capacity in patients 80 years of age or older. Can Respir J. 2004;11:407–413. doi: 10.1155/2004/632153. [DOI] [PubMed] [Google Scholar]
- 69.Lindenauer PK, Stefan MS, Pekow PS, Mazor KM, Priya A, Spitzer KA, et al. Association between initiation of pulmonary rehabilitation after hospitalization for COPD and 1-year survival among medicare beneficiaries. JAMA. 2020;323:1813–1823. doi: 10.1001/jama.2020.4437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Donesky D, Citron TL, Hilling L, Cayou C, Milic MM. Additional evidence for the long-term benefits of pulmonary rehabilitation. Respir Care. 2015;60:1120–1129. doi: 10.4187/respcare.03153. [DOI] [PubMed] [Google Scholar]
- 71.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–1014. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 Autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153:725–733. doi: 10.1093/ajcp/aqaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhu H, Rhee JW, Cheng P, Waliany S, Chang A, Witteles RM, et al. Cardiovascular complications in patients with COVID-19: Consequences of viral toxicities and host immune response. Curr Cardiol Rep. 2020;22:32–32. doi: 10.1007/s11886-020-01292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yeo TJ, Wang YL, Low TT. Have a heart during the COVID-19 crisis: Making the case for cardiac rehabilitation in the face of an ongoing pandemic. Eur J Prev Cardiol. 2020;27:903–905. doi: 10.1177/2047487320915665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Troosters T, Remoortel HV. Pulmonary rehabilitation and cardiovascular disease. Semin Respir Crit Care Med. 2009;30:675–683. doi: 10.1055/s-0029-1242637. [DOI] [PubMed] [Google Scholar]
- 76.Triest FJ, Singh SJ, Vanfleteren LE. Cardiovascular risk, chronic obstructive pulmonary disease and pulmonary rehabilitation: Can we learn from cardiac rehabilitation. Chron Respir Dis. 2016;13:286–294. doi: 10.1177/1479972316642367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hoenig H, Koh G. Response to letter regarding “how should the rehabilitation community prepare for 2019-nCoV. ” Arch Phys Med Rehabil. 2020;101:1471–1472. doi: 10.1016/j.apmr.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McKinstry A, Tranter M, Sweeney J. Outcomes of dysphagia intervention in a pulmonary rehabilitation program. Dysphagia. 2010;25:104–111. doi: 10.1007/s00455-009-9230-3. [DOI] [PubMed] [Google Scholar]
- 79.Arnold RJ, Bausek N. Effect of respiratory muscle training on dysphagia in stroke patients - a retrospective pilot study. MedRxiv. 2020.02.08.20021303. Available at: http://medrxiv.org/content/early/2020/02/11/2020.02.08.20021303 . [DOI] [PMC free article] [PubMed]
- 80.Maekura R, Hiraga T, Miki K, Kitada S, Miki M, Yoshimura K, et al. Personalized pulmonary rehabilitation and occupational therapy based on cardiopulmonary exercise testing for patients with advanced chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1787–1800. doi: 10.2147/COPD.S86455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Machado A, Oliveira A, Valente C, Burtin C, Marques A. Effects of a community-based pulmonary rehabilitation programme during acute exacerbations of chronic obstructive pulmonary disease - A quasi-experimental pilot study. Authors’ reply. Pulmonology. 2020;26:112–113. doi: 10.1016/j.pulmoe.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 82.JiangM , LiY , HanM , WangZ , ZhangY , DuX Recurrent PCR positivity after hospital discharge of people with coronavirus disease 2019 (COVID-19) J Infect. 2020;81:147–178. doi: 10.1016/j.jinf.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Negrini S, Ferriero G, Kiekens C, Boldrini P. Facing in real time the challenges of the COVID-19 epidemic for rehabilitation. Eur J Phys Rehabil Med. 2020;56:313–315. doi: 10.23736/S1973-9087.20.06286-3. [DOI] [PubMed] [Google Scholar]
- 84.Bajwah S, Wilcock A, Towers R, Costantini M, Bausewein C, Simon ST, et al. Managing the supportive care needs of those affected by COVID-19. Eur Respir J. 2020;55:2000815–2000815. doi: 10.1183/13993003.00815-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]