Abstract
Background: The proportion of recurrences after discharge among patients with coronavirus disease 2019 (COVID-19) was reported to be between 9.1% and 31.0%. Little is known about this issue, however, so we performed a meta-analysis to summarize the demographical, clinical, and laboratorial characteristics of non-recurrence and recurrence groups. Methods: Comprehensive searches were conducted using eight electronic databases. Data regarding the demographic, clinical, and laboratorial characteristics of both recurrence and non-recurrence groups were extracted, and quantitative and qualitative analyses were conducted. Results: Ten studies involving 2071 COVID-19 cases were included in this analysis. The proportion of recurrence cases involving patients with COVID-19 was 17.65% (between 12.38% and 25.16%) while older patients were more likely to experience recurrence (weighted mean difference (WMD)=1.67, range between 0.08 and 3.26). The time from discharge to recurrence was 13.38 d (between 12.08 and 14.69 d). Patients were categorized as having moderate severity (odds ratio (OR)=2.69, range between 1.30 and 5.58), while those with clinical symptoms including cough (OR=5.52, range between 3.18 and 9.60), sputum production (OR=5.10, range between 2.60 and 9.97), headache (OR=3.57, range between 1.36 and 9.35), and dizziness (OR=3.17, range between 1.12 and 8.96) were more likely to be associated with recurrence. Patients presenting with bilateral pulmonary infiltration and decreased leucocyte, platelet, and CD4+ T counts were at risk of COVID-19 recurrence (OR=1.71, range between 1.07 and 2.75; WMD=−1.06, range between −1.55 and −0.57, WMD=−40.39, range between −80.20 and −0.48, and WMD=−55.26, range between −105.92 and −4.60, respectively). Conclusions: The main factors associated with the recurrence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) after hospital discharge were older age, moderate severity, bilateral pulmonary infiltration, laboratory findings including decreased leucocytes, platelets, and CD4+ T counts, and clinical symptoms including cough, sputum production, headache, and dizziness. These factors can be considered warning indicators for the recurrence of SARS-CoV-2 and might help the development of specific management strategies.
Keywords: Recurrence case, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Risk factor, Meta-analysis
1. Introduction
Subsequent to the first report of coronavirus disease 2019 (COVID-19) in December 2019, this disease has spread rapidly worldwide (Chen NS et al., 2020). We know that the clinical spectrum of COVID-19 ranges widely from asymptomatic infections to death (Zhang et al., 2020). As we have developed a deeper understanding of COVID-19, progress has been made in treatment. In China, 83 022 cases were reported as of June 4, 2020, and 78 319 of these were cured and patients were discharged (National Health Commission of the People’s Republic of China, 2020). According to the World Health Organization’s guidelines and scheme of diagnosis and treatment of COVID-19 (Trial 7th Edition), patients who meet discharge criteria should have at least two consecutive negative nucleic acid test results conducted over an interval of at least 24 h (Medical Administration and Hospital Authority, 2020; Rothan and Byrareddy, 2020). The recurrence of a positive severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA test result was found in some discharged patients (Chen DB et al., 2020; Hoang et al., 2020). This phenomenon raises the concern that discharged patients may be at risk of viral reactivation and should be considered potential sources of SARS-CoV-2 infection.
The proportion of recurrence cases after discharge among patients with COVID-19 is between 9.09% and 30.77% (Li YJ et al., 2020; Xiao et al., 2020; Ye et al., 2020). The short inter-episode period from discharge to first recurrence was 5 d in these cases (Yuan et al., 2020). The reasons why SARS-CoV-2 RNA has been re-detected in some discharged patients remain unclear. A number of studies have explored the factors involved in this phenomenon. Zhuo et al. (2020) reported that fever on admission is as an independent risk factor that can be used to predict recurrence outcome. A number of demographical and clinical factors including age, body mass index (BMI), and low levels of some blood parameters have been found to be driving forces in a recurrence prediction model (Huang et al., 2020). Data show that specific characteristics exhibit substantial differences between non-recurrence and recurrence groups (Jiang et al., 2020). We therefore performed a systematic review and meta-analysis to summarize data on demographic characteristics, clinical features, and laboratory findings in non-recurrence and recurrence groups as well as to explore critical factors associated with COVID-19 recurrence. These might provide more evidence for implementing preventive and controllable strategies for recurrence cases.
2. Methods
2.1. Search strategy and selection criteria
Studies published between May 1st, 2020 and May 29th, 2020 were comprehensively interrogated via the Web of Science, PubMed, medRxiv, bioRxiv, China National Knowledge Infrastructure (CNKI), SinoMed, VIP, and Wangfang databases. Search terms were “COVID-19,” “2019-nCoV,” “SARS-CoV-2,” “severe acute respiratory syndrome coronavirus 2,” “recurrence,” “reinfection,” “reactivation,” “re-positive,” and related terms. Details are presented in Table S1.
2.2. Inclusion and exclusion criteria
The inclusion criteria used in this analysis were: (1) negative on two consecutive reverse transcriptase-polymerase chain reaction (RT-PCR) tests at least 24 h apart before being discharged and later presented with recurrence of SARS-CoV-2; (2) recurrence of SARS-CoV-2 among patients with COVID-19 as confirmed using RT-PCR; (3) studies with sufficient data to describe epidemiological and clinical characteristics of both recurrence and non-recurrence cases.
The exclusion criteria used in this analysis were: (1) studies with recurrence cases only; (2) duplicated publication data; (3) studies missing key data; (4) case reports, reviews, and studies lacking original data.
2.3. Data extraction and quality assessment
The following information was extracted from each study: first author, title, journal name, publication date, study periods, regions, sample size, demographic data (e.g., gender, age), chronic medical conditions (e.g., comorbidities, smoking history), clinical features (e.g., fever, headache), laboratory results (e.g., leukocytes, neutrophils), and radiographical features (e.g., ground-glass opacity, bilateral pulmonary infiltration). Three components, including selection, comparability, and exposure or outcome, were assessed for each study using the Newcastle-Ottawa Scale (Jaiswal et al., 2018; Xu and Lu, 2019). This consisted of eight items with a full score of nine stars (Stang, 2010). EndNote (Version X9) was used to manage the articles and citations.
2.4. Statistical analysis
The online tool developed by Luo et al. (2018) was used to convert median and interquartile range (IQR)/range to mean and standard deviation for continuous variables. Statistical differences between continuous variables were then evaluated using the weighted mean difference (WMD) and a 95% confidence interval (95% CI), while the odds ratio (OR) and its 95% CI were calculated to estimate whether, or not, categorical variables increased the risk of SARS-CoV-2 recurrence. Heterogeneity amongst each study was then assessed using I 2; thus, when I 2>50%, a random-effect model was chosen, otherwise a fixed effect model was used (Ades et al., 2005). Potential publication bias was appraised using a funnel plot and Egger weighted regression (Peters et al., 2006). The software R (Version 3.2.3) was used for data clearing and analyses.
3. Results
3.1. Search results
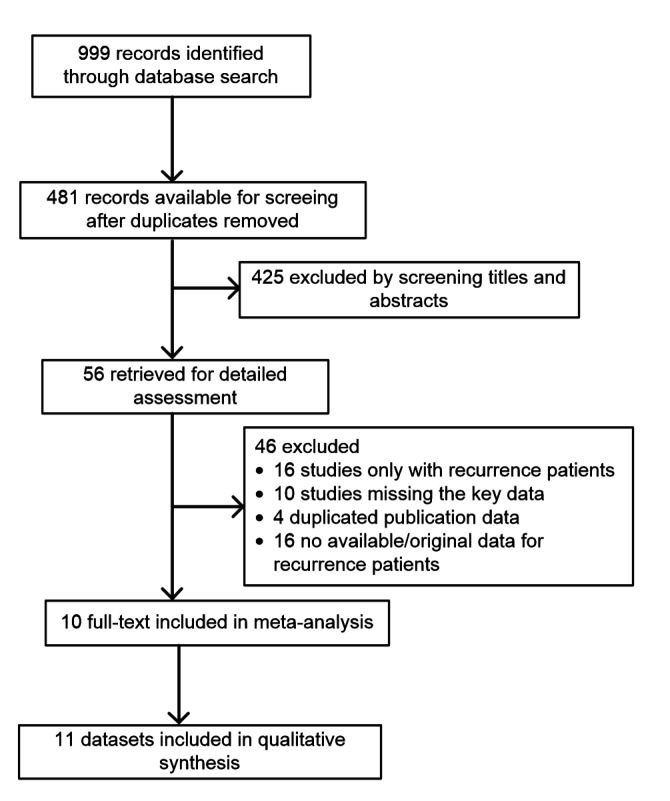
A total of 999 records were identified via a database search. Titles and abstracts of 481 published studies were then screened after discarding duplicates and 56 articles were selected for detailed assessment. Subsequent to applying exclusion criteria, 10 studies consisting of 1803 non-recurrence and 268 recurrence cases were included in a meta-analysis (Fig. 1). Details are presented in Table 1.
Fig. 1.
Flow diagram of the study selection process for meta-analysis
Table 1.
Studies and characteristics of COVID-19 patients included in this meta-analysis
| Study | Journal name | Study period (year-month-day) | Region | Sample size | Quality |
| Chen J et al., 2020 | Aging | 2020/02/24–2020/04/15 | Wuhan, China | 1067 | 6 |
| Jiang et al., 2020 | Journal of Infection | 2020/01/28–2020/03/13 | Henan, China | 35 | 4 |
| An et al., 2020 | Annals of Translational Medicine | 2020/01/23–2020/02/25 | Guangdong, China | 242 | 6 |
| Zhuo et al., 2020 | The Journal of Practical Medicine | 2020/01/23–2020/03/03 | Guangdong, China | 34 | 5 |
| Li Q et al., 2020 | Chongqing Medicine | 2020/01/18–2020/03/15 | Chongqing, China | 20 | 6 |
| Wong et al., 2020 | Journal of Medical Virology | 2020/01/01–2020/04/12 | Darussalam, Brunei | 106 | 6 |
| Huang et al., 2020 | medRxiv | 2020/01/11–2020/04/23 | Shenzhen, China | 414 | 6 |
| Hu et al., 2020 | JAMA Network Open | 2020/01/25–2020/02/26 | Guizhou, China | 69 | 6 |
| Zhao et al., 2020 | Clinical Pediatrics | 2020/01/21–2020/04/18 | Beijing, China | 14 | 5 |
| Xiao et al., 2020 | Journal of Medical Virology | 2020/01/21–2020/02/12 | Wuhan, China | 70 | 6 |
3.2. Demographical and time interval features of recurrence cases
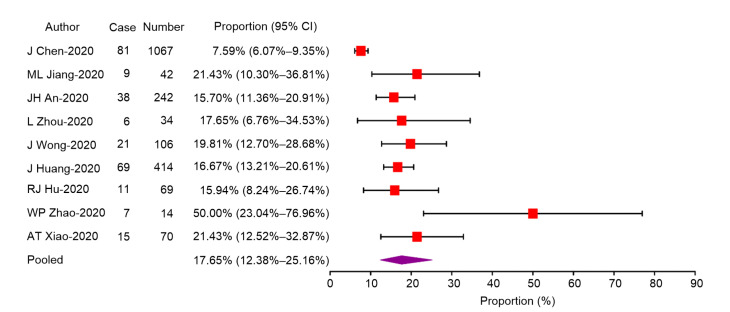
The overall proportion of recurrence cases of SARS-CoV-2 among the patients with COVID-19 was 17.65% (95% CI: range between 12.38% and 25.16%; Figs. S1 and S2). Patients in recurrence cases were found to be older than those in non-recurrence cases (WMD=1.67, 95% CI: range between 0.08 and 3.26), Data show that BMI was lower in recurrence than in non-recurrence cases (WMD=−1.20, 95% CI: range between −2.05 and −0.35). No statistical differences were seen in the time from onset to negative SARS-CoV-2 RNA test results between recurrence and non-recurrence groups. The time from discharge to recurrence of SARS-CoV-2 was 13.38 d (95% CI: range between 12.08 and 14.69 d; Table 2).
Table 2.
WMD and 95% CI of demographical and time interval between recurrence and non-recurrence of COVID-19 patients
| Demographical and time interval | Number of studies | WMD/OR (95% CI) | Heterogeneity, I 2 (%) |
| Age (year) | 8 | 1.67 (0.08, 3.26) | 0 |
| BMI (kg/m2) | 2 | −1.20 (−2.05, −0.35) | 0 |
| Time from onset to RNA negative (d) | 4 | 2.32 (−3.61, 8.25) | 92.10 |
| Time from discharge to recurrence (d) | 2 | 13.38 (12.08, 14.69) | 0 |
WMD, weighted mean difference; CI, confidence interval; OR, odds ratio; BMI, body mass index
Fig. 2.
Overall proportion of recurrence cases among the COVID-19 patients
3.3. Clinical data on recurrence cases
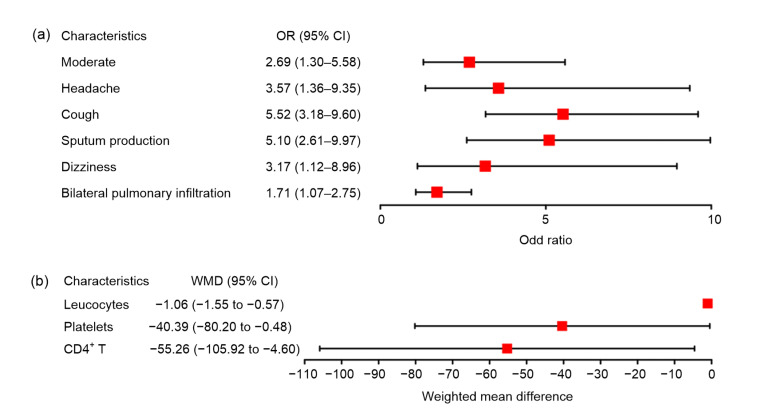
Patients were categorized as having moderate severity conditions (OR=2.69, 95% CI: range between 1.30 and 5.58) while those with clinical symptoms including cough (OR=5.52, 95% CI: range between 3.18 and 9.60), sputum production (OR=5.10, 95% CI: range between 2.61 and 9.97), headache (OR=3.57, 95% CI: range between 1.36 and 9.35), and dizziness (OR=3.17, 95% CI: range between 1.12 and 8.96) were more likely to experience recurrence. Patients who presented with bilateral pulmonary infiltration were also at risk of recurrence (OR=1.71, 95% CI: range between 1.07 and 2.75; Figs. S2a and 3a). Laboratory findings show that leucocytes (WMD=−1.06, 95% CI: range between −1.55 and −0.57), platelets (WMD=−40.39, 95% CI: range between −80.20 and −0.48), and CD4+ T (WMD=−55.26, 95% CI: range between −105.92 and −4.60) all decreased in recurrence cases (Figs. S2b and 3b). The publication bias of the recurrence case proportion among the COVID-19 patients was illustrated in Fig. S3.
Fig. 3.
Clinical characteristic and laboratory findings associated with recurrence cases
OR, odds ratio; CI, confidence interval; WMD, weighted mean difference
4. Discussion
Subsequent to the outbreak of SARS in 2002 and Middle East respiratory syndrome (MERS) in 2012, coronavirus (CoV) transmission between animals and humans has been confirmed (Cauchemez et al., 2013; Cui et al., 2019). This is important because as CoVs are an emerging infectious agent, a number of notable studies have been conducted to explore the biological, epidemiological, and clinical characteristics of the new CoV (Khose et al., 2020; Li TS et al., 2020; Radzikowska et al., 2020). Throughout the early COVID-19 epidemic, the recurrence of positive SARS-CoV-2 RNA test results after hospital discharge appeared in at least seven provinces in China while approximately 14% of discharged patients in Guangdong Province experienced recurrences (Li and Huang, 2020). A comprehensive understanding of this phenomenon is lacking, however.
Patient outcomes are often influenced by numerous factors. The proportion of recurrence cases among patients with COVID-19 was 17.65% while the median time between discharge and the recurrence of a positive SARS-CoV-2 RNA test result was 13.38 d. In order to detect recurrence cases early, the diagnosis and treatment of COVID-19 (Trial 7th Edition) should follow a revised management strategy of the discharged patient from “should continue 14 d self-health condition monitoring” to “continue 14 d isolation management and health condition monitoring” (Li and Huang, 2020). Results show that older aged people are at higher risk of positive SARS-CoV-2 RNA recurrence. Previous research has shown that older people are more likely to develop severe COVID-19 and even die (Wu and McGoogan, 2020). Thus, due to poor self-health status, lower immunity, and chronic medical conditions, older patients have relatively weak virus clearance rates and tolerance, and may lead to recurrence. Moderate severity cases easily developed into recurrence cases, a conclusion supported by previous work (Xiao et al., 2020). Data show statistical differences between cough and sputum production both recurred and did not in the study of Huang et al. (2020). These cases are associated with a higher risk of recurrence. Headaches and dizziness are the most common neurological manifestations associated with COVID-19; however, detailed mechanisms have yet not to be reported and so further research is needed (Ahmad and Rathore, 2020). Integrated into larger-scale sample sizes from each research, headaches and dizziness were also associated with recurrence. Thus, in the study of Chen J et al. (2020), elevated interleukin-6 (IL-6) levels and increased lymphocytes were also shown to be risk factors associated with recurrence. In our study, patients with bilateral pulmonary infiltration and decreased leucocyte, platelet, and CD4+ T counts were more likely to experience recurrence. Indeed, in multivariate regression analysis, patients who presented with bilateral pulmonary infiltration turned out to be at serve recurrence risk for positive SARS-CoV-2 RNA. Chen J et al. (2020) assumed that these results may be attributed to potentially undetectable amount of SARS-CoV-2 which persists in respiratory epithelia during patient recovery. SARS-CoV-2 infection can also lead to a severe dysfunctional immune response (Hui et al., 2020). Studies have also shown that patients with abnormal, over-activated immunity and “cytokine storms,” characterized as immune cell infiltration and elevated pro-inflammatory cytokine release, are also at high risk (Liu S et al., 2020; Song et al., 2020). Immune cells such as white blood cells enable the body to defend itself against external infections and play an important role in response to viruses (Liu W et al., 2020). Guo et al. (2019) previously reported that CD3+ T, CD3+CD4+ T, and CD3+CD8+ T cells significantly decreased in fatal COVID-19 cases (Guo et al., 2019; Zhou et al., 2020). Over-activated T and T-cell inhibitory factor expression may also lead to decreased T cell exhaustion (Altmann and Boyton, 2020; Bellesi et al., 2020; Remy et al., 2020). Decreased cellular immune function might also lead to incomplete virus clearance and recurrences. Indeed, in study of Lippi et al. (2020), a lower platelet count was significantly correlated with severe COVID-19 and death cases while thrombocytopenia in COVID-19 implies serious organ malfunction or physiologic decompensation. The progression of COVID-19 promotes the activation of platelets and alters their function, which means that SARS-CoV-2 interacts with platelets during the infection process (Hottz et al., 2020). These results may explain the lower platelet count, also found in recurrence cases.
Several other possible factors could also induce a SARS-CoV-2 recurrence. Firstly, false-negative RT-PCR results are due to sample sources, sampling procedures, and sensitivity/specificity of a test kit (Yang et al., 2020). Secondly, SARS-CoV-2 RNA shed in feces from at least two weeks to more than one month, and up to a maximum of 83 d has also been reported (Cai et al., 2020; Li N et al., 2020). Thirdly, when the body is infected with a virus, a specific antibody is produced and therefore a body will have a certain period of protection against secondary infections. It remains unknown whether, or not, recovered patients will be immune when exposed again to the virus.
5. Conclusions
A total of 1803 cases of non-recurrence as well as 268 recurrences were included in this study to analyze the factors contributing to SARS-CoV-2 reappearances. Older age, moderately severe cases, and clinical manifestations including cough, sputum production, headache, and dizziness are all recurrence risk factors. Radiographic signs and laboratory findings including bilateral pulmonary infiltration as well as decreased numbers of leucocytes, platelets, and CD4+ T cells are more likely associated with SARS-CoV-2 recurrences. These factors should be considered as early warning signs for recurrence. It is therefore necessary to self-quarantine for 14 d after discharge, while process management from diagnosis, isolation, and treatment to discharge requires strict control.
List of electronic supplementary materials
Search strategy of the recurrence cases with COVID-19
Forest plots of meta-analysis on the proportion of the asymptomatic individuals among the COVID-19 infections
Forest plots of meta-analysis on clinical characteristics and laboratory findings of the recurrence cases among the COVID-19 infections
Funnel plot assessing publication bias in studies reporting proportion of recurrence cases among the COVID-19 patients
Footnotes
Project supported by the National Science and Technology Major Project of China (Nos. 2018ZX10302206 and 2017ZX10202203) and the Zhejiang University Academic Award for Outstanding Doctoral Candidates (No. 2020052), China
Contributors: Zhi CHEN, Meng-qi YAO, and Qiu-xian ZHENG designed the analysis. Meng-qi YAO, Qiu-xian ZHENG, and Jia XU finished the analysis and prepared the manuscript. Jing-wen DENG, Tian-tian GE, Hai-bo ZHOU, and Feng-tian WU prepared the figures and tables. Xin-yu GU, Qin YANG, Yan-li REN, and Gang WANG prepared the tables and edited this manuscript. Zhi CHEN supervised the study. All authors reviewed and approved the final version of the manuscript.
Electronic supplementary materials: The online version of this article (https://doi.org/10.1631/jzus.B2000304) contains supplementary materials, which are available to authorized users
Compliance with ethics guidelines: Meng-qi YAO, Qiu-xian ZHENG, Jia XU, Jing-wen DENG, Tian-tian GE, Hai-bo ZHOU, Feng-tian WU, Xin-yu GU, Qin YANG, Yan-li REN, Gang WANG, and Zhi CHEN declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Ades AE, Lu G, Higgins JPT. The interpretation of random-effects meta-analysis in decision models. Med Decis Making. 2005;25(6):646–654. doi: 10.1177/0272989x05282643. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad I, Rathore F. Neurological manifestations and complications of COVID-19: a literature review. J Clin Neurosci. 2020;77:8–12. doi: 10.1016/j.jocn.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altmann DM, Boyton RJ. SARS-CoV-2 T cell immunity: specificity, function, durability, and role in protection. Sci Immunol. 2020;5(49):eabd6160. doi: 10.1126/sciimmunol.abd6160. [DOI] [PubMed] [Google Scholar]
- 4.An JH, Liao XJ, Xiao TY, et al. Clinical characteristics of the recovered COVID-19 patients with re-detectable positive RNA test. Ann Transl Med. 2020;8(17):1–12. doi: 10.21037/atm-20-5602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellesi S, Metafuni E, Hohaus S, et al. Increased CD95 (Fas) and PD-1 expression in peripheral blood T lymphocytes in COVID-19 patients. Br J Haematol. 2020;191(2):207–211. doi: 10.1111/bjh.17034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai JH, Xu J, Lin DJ, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020;71(6):1547–1551. doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cauchemez S, van Kerkhove MD, Riley S, et al. Transmission scenarios for Middle East respiratory syndrome coronavirus (MERS-CoV) and how to tell them apart. Euro Surveill. 2013;18(24):20503. [PMC free article] [PubMed] [Google Scholar]
- 8.Chen DB, Xu WX, Lei ZY, et al. Recurrence of positive SARS-CoV-2 RNA in COVID-19: a case report. Int J Infect Dis. 2020;93:297–299. doi: 10.1016/j.ijid.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen J, Xu XP, Hu J, et al. Clinical course and risk factors for recurrence of positive SARS-CoV-2 RNA: a retrospective cohort study from Wuhan, China. Aging. 2020;12(17):16675–16689. doi: 10.18632/aging.103795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen NS, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/s0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo LX, Wei D, Zhang XX, et al. Clinical features predicting mortality risk in patients with viral pneumonia: the MuLBSTA score. Front Microbiol, 10:2752. 2019 doi: 10.3389/fmicb.2019.02752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoang VT, Dao TL, Gautret P. Recurrence of positive SARS-CoV-2 in patients recovered from COVID-19. J Med Virol. 2020;92(11):2366–2367. doi: 10.1002/jmv.26056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hottz ED, Azevedo-Quintanilha IG, Palhinha L, et al. Platelet activation and platelet-monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136(11):1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu RJ, Jiang ZX, Gao HM, et al. Recurrent positive reverse transcriptase-polymerase chain reaction results for coronavirus disease 2019 in patients discharged from a hospital in China. JAMA Netw Open. 2020;3(5):e2010475. doi: 10.1001/jamanetworkopen.2020.10475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang J, Zheng L, Li Z, et al. Recurrence of SARS-CoV-2 PCR positivity in COVID-19 patients: a single center experience and potential implications. medRxiv, preprint; 2020. [DOI] [Google Scholar]
- 17.Hui KPY, Cheung MC, Perera RAMP, et al. Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: an analysis in ex-vivo and in-vitro cultures. Lancet Respir Med. 2020;8(7):687–695. doi: 10.1016/s2213-2600(20)30193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaiswal S, Liu XB, Wei QC, et al. Effect of corticosteroids on atrial fibrillation after catheter ablation: a meta-analysis. J Zhejiang Univ-Sci B (Biomed & Biotechnol) 2018;19(1):57–64. doi: 10.1631/jzus.B1600529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang ML, Li Y, Han ML, et al. Recurrent PCR positivity after hospital discharge of people with coronavirus disease 2019 (COVID-19) J Infect. 2020;81(1):147–178. doi: 10.1016/j.jinf.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khose S, Moore JX, Wang HE. Epidemiology of the 2020 pandemic of COVID-19 in the state of Texas: the first month of community spread. J Community Health. 2020;45(4):696–701. doi: 10.1007/s10900-020-00854-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li LQ, Huang SL. Whether the repositive rate of 14% of discharged patients in guangdong is infectious is not clear. Caixin (in Chinese). http://china.caixin.com/2020-02-25/ 101520334.html.2020. [Google Scholar]
- 22.Li N, Wang X, Lv TF. Prolonged SARS-CoV-2 RNA shedding: not a rare phenomenon. J Med Virol. 2020;92(11):2286–2287. doi: 10.1002/jmv.25952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Q, Zhang H, Deng SY, et al. Expression and morphological analysis of peripheral blood lymphocytes subsets in patients with 2019 noval coronavirus. Chongqing Med, online. 2020 (in Chinese) [Google Scholar]
- 24.Li TS, Lu HZ, Zhang WH. Clinical observation and management of COVID-19 patients. Emerg Microbes Infect. 2020;9(1):687–690. doi: 10.1080/22221751.2020.1741327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li YJ, Hu YY, Yu YY, et al. Positive result of Sars-Cov-2 in faeces and sputum from discharged patient with COVID-19 in Yiwu, China. J Med Virol. 2020;92(10):1938–1947. doi: 10.1002/jmv.25905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu S, Zhi YX, Ying S. COVID-19 and asthma: reflection during the pandemic. Clin Rev Allergy Immunol. 2020;59(1):78–88. doi: 10.1007/s12016-020-08797-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu W, Tao ZW, Wang L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133(9):1032–1038. doi: 10.1097/cm9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luo DH, Wan X, Liu JM, et al. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods in Med Res. 2018;27(6):1785–1805. doi: 10.1177/0962280216669183. [DOI] [PubMed] [Google Scholar]
- 30.Medical Administration, Hospital Authority. National Health Commission’s COVID-19 Diagnosis and Treatment Protocol (Trial Version 7) (in Chinese) 2020 (Available from: http://www.nhc. gov.cn/yzygj/s7652m/202003/a31191442e29474b98bfed5579d5af95.shtml)
- 31.National Health Commission of the People’s Republic of China. Update on COVID-19 as of 24:00, March 17 (in Chinese) 2020 (Available from: http://www.nhc.gov.cn/xcs/yqtb/202003/97 b96f03fa3c4e8d8d0bf536271a10c0.shtml)
- 32.Peters JL, Sutton AJ, Jones DR, et al. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 33.Radzikowska U, Ding M, Tan G, et al. Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy. 2020;75(11):2829–2845. doi: 10.1111/all.14429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Remy KE, Mazer M, Striker DA, et al. Severe immunosuppression and not a cytokine storm characterizes COVID-19 infections. JCI Insight. 2020;5(17):e140329. doi: 10.1172/jci.insight.140329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun, 109:102433. 2020 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Song JW, Zhang C, Fan X, et al. Immunological and inflammatory profiles in mild and severe cases of COVID-19. Nat Commun. 2020;11(1):3410. doi: 10.1038/s41467-020-17240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 38.Wong J, Koh WC, Momin RN, et al. Probable causes and risk factors for positive SARS-CoV-2 test in recovered patients: evidence from Brunei Darussalam. J Med Virol. 2020;92(11):2847–2851. doi: 10.1002/jmv.26199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu ZY, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1342. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 40.Xiao AT, Tong YX, Zhang S. False negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J Med Virol. 2020;92(10):1755–1756. doi: 10.1002/jmv.25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu YG, Lu YQ. Systematic review and meta-analysis of the efficacy and safety of immunosuppressive pulse therapy in the treatment of paraquat poisoning. J Zhejiang Univ-Sci B (Biomed & Biotechnol) 2019;20(7):588–597. doi: 10.1631/jzus.B1800640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Y, Yang MH, Shen CG, et al. Laboratory diagnosis and monitoring the viral shedding of SARS-CoV-2 infections. Innovation. 2020;1(3):100061. doi: 10.1016/j.xinn.2020.100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ye GM, Pan ZY, Pan YB, et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J Infect. 2020;80(5):e14–e17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yuan J, Zou RR, Zeng LJ, et al. The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res. 2020;69(6):599–606. doi: 10.1007/s00011-020-01342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang BC, Zhou XY, Qiu YR, et al. Clinical characteristics of 82 cases of death from COVID-19. PLoS ONE. 2020;15(7):e0235458. doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao WP, Wang Y, Tang YF, et al. Characteristics of children with reactivation of SARS-CoV-2 infection after hospital discharge. Clin Pediatr. 2020;59(9-10):929–932. doi: 10.1177/0009922820928057. [DOI] [PubMed] [Google Scholar]
- 47.Zhou L, Liu K, Liu HG. Cause analysis and treatment strategies of “recurrence” with novel coronavirus pneumonia (COVID-19) patients after discharge from hospital. Chin J Tuberc Respir Dis. 2020;43(4):281–284. doi: 10.3760/cma.j.cn112147-20200229-00219. (in Chinese) [DOI] [PubMed] [Google Scholar]
- 48.Zhuo L, Wei FF, Zhou JQ, et al. Factors influencing the outcome of 34 patients with COVID-19. J Pract Med. 2020;36(14):1861–1865. (in Chinese) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy of the recurrence cases with COVID-19
Forest plots of meta-analysis on the proportion of the asymptomatic individuals among the COVID-19 infections
Forest plots of meta-analysis on clinical characteristics and laboratory findings of the recurrence cases among the COVID-19 infections
Funnel plot assessing publication bias in studies reporting proportion of recurrence cases among the COVID-19 patients