Abstract
Omega-3 polyunsaturated fatty acids (n-3 PUFAs) have been described as positively associated with cognitive functioning. Current meta-analyses have identified eicosapentaenoic acid (EPA) as potentially more effective than docosahexaenoic acid (DHA). An especially vulnerable subgroup that might benefit from these beneficial effects are depressed youths. In this study, we examined associations between red blood cell (RBC) DHA and EPA levels and depression severity and verbal memory performance in a sample of 107 moderately (n = 63) and severely (n = 44) depressed youths. The findings showed that youths with high RBC EPA levels had steeper learning curves compared to those with moderate or low RBC EPA levels (Pillai’s Trace = 0.195, p = 0.027, ηp2 = 0.097). No associations between RBC DHA levels or depression severity and verbal memory performance were observed. Our results further confirm previous findings indicating a more important role of EPA compared to DHA in relation to cognitive functioning. Future research should further investigate the differential role of EPA and DHA concerning cognitive functioning in depressed youths. Evidence supporting beneficial supplementation effects could potentially establish a recommendation for a natural and easily accessible intervention for cognitive improvement or remission.
Keywords: omega-3 polyunsaturated fatty acid, EPA, DHA, depression, depression severity, verbal memory, children, adolescents, cognition
1. Introduction
According to the World Health Organization (WHO), approximately 4.4% of the world’s population suffer from depression [1], with a lifetime prevalence rate of approximately 10%–15% [2,3]. Although the median age of onset lies at around 25 [2], the first symptoms and onset of depression often occur as early as during childhood or adolescence [4], and earlier onset is associated with poorer health outcomes, such as more depressive episodes, more suicide attempts, and poorer functional outcomes [5]. For adolescents, the one-year prevalence rates are estimated to lie around 5% with a large range of approximately 0.2%–17% [6,7,8,9]. Depression is a very severe mental disorder and can lead to suicide, which, in 2015, was the second leading cause of death amongst 15–29-year-olds [10]. In youths, depression has been deemed the leading cause of disability-adjusted life years (DALYs) and years lived with disability (YLD) [11]. Altogether, these findings highlight the burden that this disease poses on today’s youth and the devastating associated consequences.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [12] defines the diagnostic criteria for major depressive disorder (MDD), which include depressed mood, fatigue, and diminished pleasure, as well as cognitive problems such as difficulties concentrating. To meet the diagnostic criteria for MDD, at least five symptoms must have been present for most of the time during the same two-week period. Symptoms must include either depressed mood or loss of interest or pleasure. In children and adolescents, key symptoms also include irritable mood.
Clinical research to date has primarily focused on the emotional symptoms of depression, while problems with cognition can equally impact everyday functioning and subjective quality of life [13,14,15]. Moreover, cognitive deficits have been associated with poorer antidepressant treatment outcome [16,17]. Cognitive impairments could be especially problematic when children and adolescents are affected. At this critical stage in life, problems with concentration and cognition could lead to long-lasting consequences concerning personal life and educational attainment [18,19]. Meta-analyses investigating cognitive deficits in depressed adults have reported moderate impairments in several cognitive domains compared to healthy controls [20,21,22,23,24,25,26]. Evidence from several studies suggests that these cognitive problems remain at least partially present even in the remitted stage [27,28,29]. Although cognitive complaints are equally part of the diagnostic criteria in youths, evidence for impaired cognitive test performance in this subgroup of depressed individuals seems much more heterogeneous. Some meta-analyses have found similar deficits to analyses with adult patients [30,31,32]. A qualitative review by Vilgis et al. [33], however, concluded that while some studies reported cognitive deficits in depressed children and adolescents, the majority did not find any impairments. Günther et al. [34] reported heterogenous results with undisturbed attention, whereas memory impairment was associated with depressive disorders.
In their review, McDermott and Ebmeier [35] reported negative associations between depression severity and cognitive functioning in adults; however, this effect seemed domain-specific. In youths, thus far only tendencies toward a similar association have been reported [36], highlighting the need for further investigation into this subject. In the past few years, cognitive remission has become an important goal for MDD treatment; however, treatment options concerning cognitive symptoms are scarce. Evidence of positive cognitive effects of antidepressant medication has proven rather heterogeneous [37,38,39,40,41,42,43,44].
Since the industrial revolution, nutritional patterns in Western societies have shifted toward foods containing more omega-6 (n-6) compared to omega-3 (n-3) polyunsaturated fatty acids (PUFAs) [45]. These changes have been held responsible for the rise in different civilization diseases such as cardiovascular diseases, but also in psychiatric diseases such as depression [46]. n-3 PUFA deficiency has been associated with depression [47,48,49] and eicosapentaenoic acid (EPA) status has been negatively associated with depression severity [50]. Meta-analytic evidence has further suggested beneficial effects of n-3 PUFA supplementation on depression symptoms [51,52,53,54,55], especially with high doses of EPA [51,52]. Interestingly, symptom severity might moderate this beneficial effect, as some studies have reported stronger effects in more severely depressed patients [56]. However, other meta-analyses in both adults [57] and children and adolescents [58] have revealed no beneficial effect of n-3 PUFAs for the treatment of depressive disorder. In youths, however, only four randomized controlled trials (RCTs) thus far have been included [58]. The anti-inflammatory properties of n-3 PUFAs have mostly been made responsible for their beneficial effects in relation to depression [59]. Proinflammatory cytokines have been shown to play a role in depression [60], and hence n-3 PUFAs have been discussed to counteract these inflammatory processes [61].
n-3 PUFAs are vital for normal brain development [61,62,63,64]. Consequently, the past few years have seen a renewed interest in the investigation of n-3 PUFAs in relation to cognition. Several studies in youths have reported positive associations between reported dietary n-3 PUFA intake and cognitive performance [65,66]. In a study by Montgomery et al. [67], low blood n-3 PUFA status was associated with poorer reading abilities and working memory performance in children. Similarly, Wurff et al. [68] reported better performance on an attention task for adolescents with higher n-3 PUFA status. Meta-analyses of n-3 PUFA supplementation have reported mixed results, depending on the study population investigated [69,70,71,72,73,74,75,76]. It remains unclear whether the specific type of n-3 PUFA ingested might have significantly contributed to these heterogenous study results, as some meta-analyses have suggested beneficial effects of EPA rather than docosahexaenoic acid (DHA) [69,77].
The question remains as to how n-3 PUFAs might affect cognition in depressed individuals, as supplementation studies in depressed populations are very scarce [78]. The results reported by Rogers et al. [79] showed no benefit of n-3 PUFA supplementation on cognition in adult individuals with mild to moderate depression. In youths, however, Vesco et al. [80] reported decreased parent-rated impairments in executive functioning after 12-week supplementation with n-3 PUFAs. To the best of our knowledge, there is as yet no study investigating the associations between EPA and DHA statuses and cognitive performance in depressed children and adolescents.
The aim of the current study was to address the previously mentioned research deficits and to investigate verbal memory performance in depressed children and adolescents in relation to EPA and DHA statuses as well as depression severity. The aforementioned research findings suggest that (1) EPA but not DHA is positively associated with cognitive functioning, (2) depression severity is negatively associated with cognitive functioning, and (3) depression severity might moderate the association between EPA and depression symptoms. We hence hypothesized that patients with a high EPA status would outperform patients with a low EPA status in verbal memory tasks and that this would be especially evident in severely depressed compared to moderately depressed individuals. Furthermore, we hypothesized that moderately depressed patients would outperform severely depressed patients.
If EPA but not DHA were to be identified as being associated with cognitive functioning in depressed children and adolescents, this would prove important, especially for this specific population, as EPA compared to DHA has also been considered to be more effective in the treatment of depression symptoms [51,52]. Consequently, future RCTs could investigate EPA supplementation as an intervention in these individuals, targeting both emotional and cognitive symptoms at the same time.
2. Materials and Methods
The findings reported in this present study were generated from data collected by the “The Omega-3-pMDD trial,” a multi-center placebo-controlled trial aiming to investigate the efficacy of omega-3 fatty acid supplementation in moderately to severely depressed children and adolescents aged 8–17 years. Two hundred and twenty patients across Switzerland will be recruited in order to investigate both the psychopathological and cognitive effects of nine months of n-3 PUFA supplementation. In the present study, we report cross-sectional findings from data collected prior to randomization to a treatment arm, with the exception of intellectual ability that was assessed six weeks post-randomization. Funding was received from the Swiss National Foundation and the private foundations that are listed later in the funding section. No industry funding was received. The clinical trial was registered on www.ClinicalTrials.gov, protocol no. NCT03167307. The clinical trial’s design paper has already been published [81]. The study was approved by the local ethics committee and was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and later amendments. All parents (or legal guardians) provided written informed consent and written or oral assent was obtained from the participating children before entering the study.
2.1. Participants
Participants were recruited from seven different in- and outpatient services across Switzerland. For inclusion, the patients had to meet the diagnostic criteria for MDD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV [82] and had to have reported symptoms of at least moderate severity defined by a Children’s Depression Rating Scale [83] total score of ≥40 [84]. Patients who met the DSM-IV diagnostic criteria for an eating disorder within the last six months or the diagnostic criteria for a lifetime diagnosis of schizophrenia, bipolar affective disorder, or substance dependency were excluded from the trial. Mental retardation, pervasive development disorder, or pre-existing neurological or medical conditions that are likely to be responsible for depression symptoms constituted further exclusion criteria. Antidepressant treatment was allowed at study entry to avoid selection bias toward less severely depressed patients. Lastly, patients regularly supplementing n-3 PUFAs within the last six months (dosage limit set at 600 mg/day) or patients unable to follow the study procedures (e.g., due to a language barrier) were also excluded.
During the screening visit, the inclusion and exclusion criteria were assessed using the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL) [85] and the Children’s Depression Rating Scale revised (CDRS-R) [83]. Patients meeting all inclusion and no exclusion criteria were then included in the lead-in phase of the trial (7–14 days). During the lead-in phase, all participants received a placebo in a single blinded fashion and psychopathological, cognitive, and bloodwork baseline data were collected. Assessment of the inclusion and exclusion criteria was repeated at the end of this phase, after which patients were randomized to a treatment arm in a double-blind fashion. At the time of analysis, the sample consisted of 107 patients that met all of the inclusion and no exclusion criteria at screening and had analyzed PUFA blood sample data. The current article investigated this subsample in a cross-sectional manner using single cognitive and psychopathological assessments from the lead-in phase of the trial.
2.2. Instruments
2.2.1. Sociodemographic Variables
Sociodemographic information and information on treatment history were obtained using the patients’ medical records, as well as patient and parent interviews. Information on the course of illness was collected via patients’ self-reports and parents’ reports. The patients’ medical records were consulted for confirmation of these reports. Patients or parents provided further information where information was missing or incomplete.
2.2.2. Independent Variables
Severity of Depression (CDRS-R)
The CDRS-R is a semi-structured clinical interview assessing the severity of depression using 17 depression symptoms [83]. Patients and parents provide information on 14 of these symptoms which are then rated on a 7- or 5-point Likert scale, depending on the specific symptom. The interviewer then integrates this information and provides a final score for each symptom. Three further nonverbal symptoms are rated by the interviewer only (depressed facial affect, hypoactivity and listless speech). The final scores for each reported symptom, as well as the ratings on nonverbal symptoms are added up to obtain a final score for depression severity. Scores of 30–39 can be interpreted as mild, 40–59 as moderate, and ≥60 as severe symptoms of depression [84]. Validation studies on CDRS-R have reported good validity and reliability for depressed children and adolescents [86].
EPA and DHA Statuses
Venous blood samples were collected. For determination of erythrocyte fatty acid composition, blood was drawn into EDTA tubes, centrifuged, and then the plasma and buffy coat taken off; the erythrocytes were then frozen at −80 °C until analysis. The fatty acid composition of the erythrocytes was analyzed by gas chromatography at Omegametrix GmbH using previously described methods [87]. EPA and DHA statuses are given as a percentage of total fatty acids measured in RBCs.
2.2.3. Outcome Variables
Cognitive Tests—Memory
-
Verbal Memory: VLMT
We used a validated German version (Verbaler Lern- und Merkfähigkeitstest (VLMT) [88]) of the Auditory Verbal Learning Test (AVLT) [89], in which a list of 15 semantically independent words is presented auditorily to an individual and he or she is asked to remember and reproduce as many words as possible. This process is repeated five times. Then, a second list of 15 words (= interference list (I)) is presented and the individual is asked to remember and reproduce as many words as possible from the second list. In the next step, the individual is asked to reproduce the words from the first list. After 20–30 min, he or she is once again asked to reproduce the first list of words. In the last step, the individual is asked to recognize the words from a list of 50 semantically or phonetically related and unrelated words. The test measures declarative verbal memory capacity. Short-term verbal memory is characterized by the number of words correctly reproduced by the individual in each of the five rounds (T1, T2, T3, T4, and T5). The long-term memory parameters are T7, which is the number of words from the first list recalled after 20–30 min, and T5–T7, which is the difference between the number of words recalled at T5 and T7. The interference score is I, which represents the number of correctly reproduced words from the interference list, T6, which is the number of words from the first list recalled after interference, and T5–6, which is the difference between the number of words reproduced from the first list before and after interference. Lastly, recognition (W) is the number of words correctly identified as belonging to the first list, and W–F is the correctly identified words minus the words wrongly attributed to the first list.
-
Numeric Memory: WISC-IV Digit Span
The digit span subtest from the Wechsler Intelligence Scale for Children—Fourth Edition (WISC-IV) [90] consists of two parts, namely, forward and backward. In the first part, the individual has to reproduce sequences of digits of increasing length. In the second part, the individual is instructed to repeat a sequence of digits in reverse order. The test measures numeric short-term memory and working memory.
2.2.4. Control Variables
IQ: Reynolds Intellectual Assessment Scales and Screening (RIAS)
The RIAS is an intelligence test for individuals between 3 and 99 years of age, mostly used for research purposes [91]. It includes two subtests, the results of which are added to form a verbal intelligence index (VIX) and two subtests to form the nonverbal intelligence index (NIX). These are then integrated into the global intelligence index (GIX). Reliability of the RIAS is high (Cronbach α = 0.95 for the global index) [92,93].
C-Reactive Protein (CRP)
High-sensitive CRP was measured in the plasma in an accredited medical laboratory using a commercial assay with a coefficient of variation of 1.3% at 3.6 mg/L, to be used as a marker for low-grade inflammation and as a stratification parameter for randomization. Values above 10 were excluded from analysis, as they could have indicated infection.
Body Mass Index (BMI)
The BMI was calculated using weight (kg)/height (cm)2. BMI was not obtained in some cases because of missing measurement tools and devices.
2.3. Statistical Analysis
Statistical Package for the Social Sciences (SPSS) software version 26 was used for all statistical analyses. Descriptive statistics are given in order to describe the study sample characteristics. Moderately and severely depressed patient groups were distinguished using a clinical cut-off of the CDRS-R total score (40–59 = moderate; ≥60 = severe) [84]. Three approximately equally sized groups were formed according to the data distribution of EPA and DHA statuses, because the patients’ n-3 PUFA statuses were all low when referring to the currently proposed ideal levels [94]. Hence, the formation of three groups would allow for the investigation of especially low status and rather normal values. Differences between moderately and severely depressed patients and differences between EPA and DHA status groups for the investigation of potential confounding variables were analyzed using chi-square tests, independent t-tests, and one-way ANOVAs, depending on the scale level of the variable investigated. Non-parametric Mann–Whitney U or Kruskal–Wallis tests were only used for strongly skewed data (>1, <(−1)), as in large sample sizes parametric tests should be robust against the violation of normality assumption [95].
In order to investigate differences in memory scores depending on depression severity (moderate vs. severe) and EPA and DHA statuses (low, intermediate, and high), multivariate analyses of covariance (MANCOVAs) were computed to evaluate the VLMT short-term, long-term, and interference parameters separately. Multivariate outliers were checked using Mahalanobis’ distances. Bonferroni correction was applied for the interpretation of between-subjects effects and pairwise comparisons. For digit span parameters, univariate analyses of covariance (ANCOVAs) were used for the forward and backward parameters separately.
Conservative results using Pillai’s Trace instead of Wilk’s Lambda are reported [96]. Pillai’s Trace values range from 0 to 1 with increasing values indicating a stronger contribution of the independent variable to the model. For all MANCOVAs, normal distribution within groups was investigated using Shapiro–Wilk tests and Q-Q plots where n ≤ 25. Box’s tests were used to evaluate the homogeneity of variance–covariance matrices. Levene’s tests were used to assess the equality of error variances, although the results should be robust against violation if none of the standard deviations are more than four times as large as the corresponding smallest standard deviation [97]. The homogeneity of the regression slopes was assessed for all covariates. Significance levels were set at p < 0.05.
3. Results
At the time of analysis, the subsample of patients that met all inclusion and no exclusion criteria and where blood samples were available consisted of 107 patients. For one patient, the WISC digit span scores were missing due to the fact that the test had not been done with this individual. RIAS scores for seven patients were missing, because IQ testing was done six weeks post-randomization and these patients had not yet reached week six of the study.
3.1. Descriptive Statistics
Patients achieved average mean normative scores for both the VLMT total learning parameter (∑T-15) (T-score, M = 49.15, SD = 9.21), as well as the WISC digit span score (scaled score metric, M = 9.57, SD = 2.43). However, a significant proportion of patients achieved below average scores, with 24 patients (22.42%) with T-scores < 40 for the VLMT; moreover, 24 patients (22.64%) achieved scaled metric scores <8 for the digit span test. There was one outlier for the long-term memory scores, with a Mahalanobis’ distance of 25.72 (critical value = 13.82); however, it was decided not to exclude this participant because all other memory parameters were within normal range. Only 5.8% achieved recognition normative scores below average and 67% recognized all 15 words from the list. The skewness of the recognition data was −2.32 (SE = 0.23) and kurtosis was 6.51 (SE = 0.47). A total of 46.2% of the participants reached maximum recognition scores even when subtracting interference or false positive mistakes (skewness of −1.691 (SE = 0.25) and kurtosis of 2.96 (SE = 0.47)). Hence, it was decided to investigate depression severity and EPA/DHA group differences concerning recognition scores using nonparametric Kruskal–Wallis and Mann–Whitney U tests instead of MANCOVAs.
Severity group formation resulted in a group of 63 moderately depressed patients and a group of 44 severely depressed patients. The sociodemographic information, IQ, physiological parameters, and psychopathology data are summarized in Table 1 for both severity groups. Severely depressed patients were over proportionally female compared to moderately depressed patients; hence, gender was later entered as a covariate for the ANCOVA and MANCOVA analyses. No other group differences except CDRS-R score differences presented between severity groups. Importantly, no differences concerning antidepressant use were found.
Table 1.
Descriptive statistics for sociodemographic information, biological parameters, IQ, psychopathology.
| Sample Characteristics | Variable Specifics | n | M (SD) | Min | Max | Moderate Depression M (SD) |
Severe Depression M (SD) |
t/χ2/U | p |
|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic information | Age | 107 | 15.50 (1.89) | 8.67 | 18.00 | 15.25 (2.09) | 15.85 (1.51) | −1.630 | 0.106 |
| Sex: %female | 107 | 67% | 57% | 82% | 7.166 | 0.007 ** | |||
| Physiological parameters | BMI | 99 | 22.35 (4.87) | 14.00 | 39.80 | 21.86 (4.35) | 23.06 (5.52) | 1285.0 | 0.454 |
| CRP | 105 | 0.79 (1.26) | 0 | 6.6 | 0.65 (0.81) | 0.99 (1.69) | 1220.0 | 0.410 | |
| IQ | |||||||||
| RIAS | VIX | 100 | 101.73 (9.93) | 79 | 129 | 102.58 (10.18) | 100.51(9.61) | 1.019 | 0.102 |
| NIX | 100 | 106.33 (8.93) | 70 | 123 | 107.71 (8.61) | 104.34 (9.12) | 1.879 | 0.310 | |
| GIX | 100 | 104.52 (9.35) | 76 | 128 | 105.78 (9.32) | 102.68 (9.21) | 1.651 | 0.102 | |
| Depression severity | |||||||||
| CDRS-R | Total score | 107 | 57.73 (7.76) | 42 | 79 | 52.37 (4.18) | 65.41 (4.54) | −15.331 | <0.001 *** |
| Severe % a | 44 | 41.1% | - | - | - | - | |||
| Course of illness | |||||||||
| Mean duration of depression (months) | Months | 104 | 14.71 (11.69) | 1 | 84 | 13.45 (9.76) | 16.43 (13.84) | 1503.0 | 0.228 |
| Total number of episodes | 105 | 1.46 (0.95) | 1 | 8 | 1.44 (1.10) | 1.48 (0.70) | 1490.0 | 0.230 | |
| Recurrent depression | Yes | 104 | 31% | 26% | 38% | 1.775 | 0.183 | ||
| Use of antidepressant medication | Yes | 102 | 37% | 35% | 40% | 0.317 | 0.573 |
Note: ** p < 0.01, *** p < 0.001. CRP, C-reactive protein; BMI, body mass index; VIX, verbal intelligence index; NIX, nonverbal intelligence index; GIX, global intelligence index; RIAS, Reynolds Intellectual Assessment Scales and Screening; CDRS-R, Children’s Depression Rating Scale revised. a CDRS-R severity scores: 40–59 = moderate, ≥60 = severe.
EPA group formation resulted in three groups (n1 = 34, n2 = 39, and n3 = 34) with group means of M1 = 0.34 (SD = 0.05), M2 = 0.46 (SD = 0.04), M3 = 0.66 (SD = 0.11). No gender (χ2 = 0.172, p = 0.918), age (F(2,104) = 0.816, p = 0.445), IQ (F(2,97) = 2.317, p = 0.104), BMI (H(2) = 2.950, p = 0.229), CRP (H(2) = 2.771, p = 0.250) differences or differences concerning antidepressant use (χ2 = 0.866, p = 0.649) presented between the three groups. DHA group formation resulted in three groups (n1 = 36, n2 = 35, and n3 = 36) with group means of M1 = 2.89 (SD = 0.22), M2 = 3.48 (SD = 0.20), and M3 = 4.54 (SD = 0.61). Moreover, between these groups, no gender (χ2 = 0.468, p = 0.791), age (F(2,104) = 0.774, p = 0.464), IQ (F(2,97) = 0.924, p = 0.401), (H(2) = 0.987, p = 0.611), CRP (H(2)= 0.539, p = 0.764) differences or differences concerning antidepressant use (χ2 = 0.527, p = 0.768) were found.
As shown in Table 2, severely depressed patients had higher DHA and total omega-3 status compared to moderately depressed patients. No significant differences concerning EPA status were observed.
Table 2.
Fatty acid status for moderately and severely depressed patients.
| Total | Moderate MDD (n = 63) | Severe MDD (n = 44) | t | p | |
|---|---|---|---|---|---|
| Fatty acid | M (SD) | M (SD) | M (SD) | ||
| EPA | 0.49 (0.15) | 0.47 (0.14) | 0.51 (0.16) | −1.515 | 0.133 |
| DHA | 3.63 (0.79) | 3.50 (0.71) | 3.82 (0.87) | −2.077 | 0.040 * |
| All n-6 | 34.37 (1.32) | 34.45 (1.26) | 34.32 (1.40) | 0.512 | 0.609 |
| All n-3 | 6.45 (1.0) | 6.26 (0.93) | 6.71 (1.06) | −2.318 | 0.022 * |
| AA/EPA | 35.10 (11.27) | 36.08 (11.21) | 33.74 (11.60) | 1.045 | 0.298 |
Note: * p < 0.05. EPA, eicosapentaenoic acid; DHA, docosahexaenoic; n-6, omega-6; n-3, omega-3; AA, arachidonic acid.
3.2. Main Analysis—EPA Status and Depression Severity in Relation to Memory
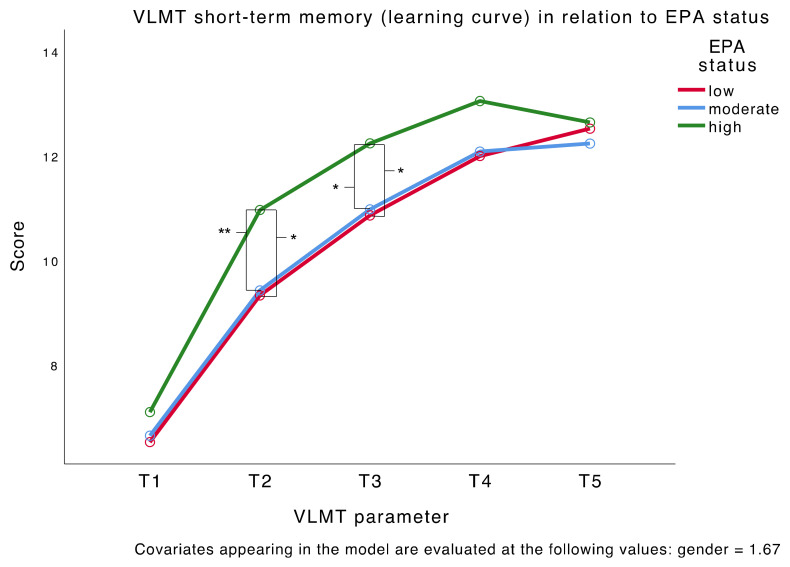
The MANCOVA results for the short-term memory VLMT parameters resulted in a significant main effect for EPA status (F(10,194) = 2.094, p = 0.027) but not for depression severity (F(5,96) = 0.622, p = 0.684). The between-subjects effects of EPA status were significant for the second trial (T2) (F(2,100) = 6.096, p = 0.003) and reached borderline significance for T3 (F(2,100) = 4.825, p = 0.010) after Bonferroni correction of the significance level (p < 0.01). Pairwise comparisons showed that patients with a high EPA status (M = 10.96, SE = 0.37) outperformed patients with a moderate (M = 9.42, SE = 0.35, p = 0.009) or low (M = 9.32, SE = 0.40, p = 0.010) EPA status in T2. The same results presented for T3, where patients with a high EPA status (M = 12.23, SE = 0.35) outperformed patients with a moderate (M = 10.97, SE = 0.33, p = 0.027) or low (M = 10.86, SE = 0.37, p = 0.023) EPA status. The VLMT short-term memory score profiles for the three EPA status groups are shown in Figure 1. The results indicate that patients with a high EPA status had steeper learning curves compared to those with a moderate or low EPA status. No main effect of either EPA status or depression severity presented for interference, long-term memory parameters, and the parameters of the digit span test. All results are summarized in Table 3. Independent samples Kruskal–Wall tests showed no effect of EPA status for either the uncorrected (H(2) = 0.893, p = 0.640) or the corrected (H(2) = 2.239, p = 0.326) recognition parameter; there was also no significant effect of depression severity (U = 1370.500, p = 0.901 U = 1274.000, p = 0.580). Further analyses concerning potential confounding group differences revealed no significant IQ differences between the six EPA/severity groups.
Figure 1.
VLMT learning curve in relation to EPA status. N = 107. * p < 0.05, ** p < 0.01.
Table 3.
Multivariate analysis of covariance (MANCOVA) and univariate analysis of covariance (ANCOVA) results for Verbaler Lern- und Merkfähigkeitstest (VLMT) and digit span parameters. EPA status and depression severity entered as factors and gender as a covariate.
| MANCOVA EPA status (EPA) Depression Severity (S) Interaction Severity * EPA Status (I) Covariate: Gender (G) |
||||||||
|---|---|---|---|---|---|---|---|---|
| VLMT short-term memory parameters |
EPA: F(10,194) = 2.094, p = 0.027 *, ηp2 = 0.097 S: F(5,96) = 0.622, p = 0.684, ηp2 = 0.031 I: F(10,194) = 0.910, p = 0.525, ηp2 = 0.045 G: F(5,96) = 1.287, p = 0.276, ηp2 = 0.063 |
|||||||
| Moderate depression N = 63 M (SD) |
Severe depression N = 44 M (SD) |
F p ηp2 |
Pairwise | p | ||||
| EPA | S | I | G | |||||
| T1 score | ||||||||
| Low EPA | 6.52 (0.33) | 6.55 (0.53) | 1.044 | 0.816 | 0.415 | 0.6 | NS | NS |
| Moderate EPA | 7.00 (0.35) | 6.29 (0.46) | 0.356 | 9.369 | 0.661 | 0.44 | ||
| High EPA | 7.11 (0.40) | 7.06 (0.42) | 0.02 | 0.008 | 0.008 | 0.006 | ||
| T2 score | ||||||||
| Low EPA | 9.74 (0.52) | 8.91 (0.69) | 6.096 | 1.577 | 2.03 | 0 | EPA: h > m EPA: h > l |
p = 0.009 **
p = 0.010 * |
| Moderate EPA | 10.14 (0.56) | 8.71 (0.46) | 0.003 * | 0.212 | 0.137 | 0.997 | ||
| High EPA | 10.67 (0.26) | 11.25 (0.44) | 0.109 | 0.016 | 0.039 | 0 | ||
| T3 score | ||||||||
| Low EPA | 11.43 (0.40) | 10.36 (0.64) | 4.825 | 1.674 | 1.366 | 2.47 | EPA: h > m EPA: h > l |
p = 0.027 *
p = 0.023 * |
| Moderate EPA | 11.27 (0.52) | 10.71 (0.45) | 0.010 ° | 0.199 | 0.26 | 0.119 | ||
| High EPA | 11.94 (0.38) | 12.50 (0.52) | 0.088 | 0.016 | 0.027 | 0.024 | ||
| T4 score | ||||||||
| Low EPA | 12.17 (0.38) | 10.91 (0.64) | 2.652 | 0.944 | 0.082 | 3.069 | NS | NS |
| Moderate EPA | 12.32 (0.50) | 11.88 (0.70) | 0.075 | 0.334 | 0.921 | 0.083 | ||
| High EPA | 13.00 (0.33) | 13.06 (0.42) | 0.05 | 0.009 | 0.002 | 0.03 | ||
| T5 score | ||||||||
| Low EPA | 12.57 (0.38) | 12.55 (0.51) | 0.41 | 0.103 | 0.059 | 2.101 | NS | NS |
| Moderate EPA | 12.32 (0.50) | 12.18 (0.58) | 0.665 | 0.749 | 0.942 | 0.15 | ||
| High EPA | 12.50 (0.41) | 12.75 (0.37) | 0.008 | 0.001 | 0.001 | 0.021 | ||
| VLMT interference parameters | EPA: F(6,198) = 1.426, p = 0.206, ηp2 = 0.041 S: F(3,98) = 1.056, p = 0.372, ηp2 = 0.031 I: F(6,198) = 0.102, p = 0.996, ηp2 = 0.003 G: F(3,98) = 0.869, p = 0.460, ηp2 = 0.026 |
|||||||
| I | ||||||||
| Low EPA | 6.43 (0.40) | 6.18 (0.62) | 1.671 | 2.28 | 0.079 | 1.414 | NS | NS |
| Moderate EPA | 6.41 (0.44) | 5.71 (0.58) | 0.193 | 0.134 | 0.924 | 0.237 | ||
| High EPA | 7.33 (0.71) | 6.63 (0.52) | 0.032 | 0.022 | 0.002 | 0.014 | ||
| T6 | ||||||||
| Low EPA | 11.96 (0.59) | 11.55 (0.56) | 2.364 | 0.68 | 0.134 | 1.917 | NS | NS |
| Moderate EPA | 11.36 (0.56) | 10.94 (0.70) | 0.101 | 0.411 | 0.875 | 0.169 | ||
| High EPA | 12.28 (0.43) | 12.44 (0.48) | 0.045 | 0.007 | 0.003 | 0.019 | ||
| T5–6 | ||||||||
| Low EPA | 0.61 (0.43) | 1.00 (0.54) | 2.556 | 0.756 | 0.075 | 0.107 | NS | NS |
| Moderate EPA | 0.95 (0.24) | 1.24 (0.36) | 0.083 | 0.387 | 0.928 | 0.744 | ||
| High EPA | 0.22 (0.31) | 0.31 (0.37) | 0.049 | 0.008 | 0.001 | 0.001 | ||
| VLMT long-term memory parameters | EPA: F(4,200) = 0.604, p = 0.660, ηp2 = 0.012 S: F(2,99) = 0.055, p = 0.946, ηp2 = 0.001 I: F(4,200) = 0.093, p = 0.984, ηp2 = 0.002 G: F(2,99) = 1.123, p = 0.330, ηp2 = 0.022 |
|||||||
| T7 | ||||||||
| Low EPA | 11.78 (0.54) | 11.82 (0.48) | 1.1 | 0.091 | 0.157 | 1.832 | NS | NS |
| Moderate EPA | 11.55 (0.67) | 11.18 (0.69) | 0.337 | 0.763 | 0.855 | 0.179 | ||
| High EPA | 12.00 (0.46) | 12.44 (0.58) | 0.022 | 0.001 | 0.003 | 0.001 | ||
| T5–7 | ||||||||
| Low EPA | 0.78 (0.36) | 0.73 (0.41) | 0.774 | 0.007 | 0.123 | 0.128 | NS | NS |
| Moderate EPA | 0.77 (0.44) | 1.00 (0.39) | 0.464 | 0.934 | 0.884 | 0.721 | ||
| High EPA | 0.50 (0.31) | 0.31 (0.44) | 0.015 | 0 | 0.002 | 0.001 | ||
| Moderate depression N = 62 M (SD) |
Severe depression N = 44 M (SD) |
|||||||
| Digits forward | ||||||||
| Low EPA | 8.68 (0.44) | 8.64 (0.41) | 0.654 | 0.018 | 0.019 | 0.043 | NS | NS |
| Moderate EPA | 8.45 (0.37) | 8.29 (0.49) | 0.522 | 0.894 | 0.981 | 0.837 | ||
| High EPA | 8.89 (0.40) | 8.88 (0.52) | 0.013 | 0 | 0 | 0 | ||
| Digits backward | ||||||||
| Low EPA | 8.09 (0.41) | 7.64 (0.49) | 0.556 | 1.016 | 0.188 | 0.151 | NS | NS |
| Moderate EPA | 8.41 (0.47) | 7.88 (0.36) | 0.575 | 0.316 | 0.829 | 0.699 | ||
| High EPA | 8.33 (0.43) | 8.31 (0.27) | 0.011 | 0.01 | 0.004 | 0.002 | ||
Note: ηp2 = 0.01 (small), 0.06 (medium), and 0.14 (large). l, low EPA; m, moderate EPA; h, high EPA. Group sizes (n): Moderately depressed with a low EPA status = 23; moderately depressed with a moderate EPA status = 22; moderately depressed with a high EPA status = 18; severely depressed with a low EPA status = 11; severely depressed with a moderate EPA status = 17; severely depressed with a high EPA status = 16. Multivariate effects, pairwise comparisons: ° borderline significant, * p < 0.05 ** p < 0.01. Between-subjects effects: ° borderline significant, * p < 0.010 (short-term memory), * p < 0.017 (interference), and * p < 0.025 (long-term memory) after Bonferroni correction of the significance level. Significant effects are marked in bold. T1–7, trials 1–7; NS, not significant.
3.3. Main Analysis—DHA Status and Depression Severity in Relation to Memory
The same analyses were run using DHA instead of EPA status as a factor. A significant interaction effect for long-term memory parameters was found (F(4,200) = 3.069, p = 0.018). However, in contrast to the EPA analyses where no IQ differences were found between the groups, further analyses revealed significant IQ differences between moderately and severely depressed patients in the moderate DHA status group. Moderately depressed patients had significantly higher GIX scores (M = 106.05, SD = 8.56) compared to severely depressed patients in the moderate DHA status group (M = 97.62, SD = 10.57; t(31) = 2.537, p = 0.016). Hence, the MANCOVA and ANCOVA analyses were rerun entering IQ as a second covariate. A significant main effect for DHA status was found for digits forward scores (F(2,91) = 3.342, p = 0.040). However, pairwise comparisons were no longer significant after Bonferroni correction for multiple comparisons. No significant main effect for depression severity presented for any memory parameter. A borderline significant interaction effect presented for interference parameters of the VLMT (F(6,182) = 2.219, p = 0.052). Between-subjects effects revealed a significant effect for the T6 parameter (F(2,92) = 4.337, p = 0.016) where severely depressed patients with a high DHA status (M = 12.56, SE = 0.50) outperformed severely depressed patients with a moderate DHA status (M = 10.50, SE = 0.61, p = 0.036). Moreover, in the moderate DHA status group, moderately depressed patients (M = 12.34, SE 0.47) outperformed severely depressed patients (M = 10.50, SE = 0.61, p = 0.021). IQ proved a significant covariate for nearly all parameters. All MANCOVA and ANCOVA results are summarized in Table 4. Independent samples Kruskal–Wallis tests showed no effect of DHA status for either the uncorrected (H(2) = 0.522, p = 0.770) or the corrected (H(2) = 2.054, p = 0.358) recognition parameter.
Table 4.
MANCOVA and ANCOVA results for the VLMT and digit span parameters.
| MANCOVA DHA Status (DHA) Depression Severity (S) Interaction Severity * DHA Status (I) Covariates: Gender (G), GIX (IQ) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| VLMT short-term memory parameters | DHA: F(10,178) = 1.323, p = 0.221, ηp2 = 0.069 S: F(5,88) = 0.524, p = 0.758, ηp2 = 0.029 I: F(10,178) = 0.686, p = 0.736, ηp2 = 0.037 G: F(5,88) = 1.218, p = 0.308, ηp2 = 0.065 IQ: F(5,88) = 6.113, p < 0.001 ***, ηp2 = 0.258 |
||||||||
| Moderate depression N = 59 M (SD) |
Severe depression N = 41 M (SD) |
F p ηp2 |
Pairwise | p | |||||
| DHA | S | I | G | IQ | |||||
| T1 score | |||||||||
| Low DHA | 6.65 (1.61) | 6.40 (2.07) | 1.57 | 0.057 | 0.115 | 0.073 | 7.401 | NS | NS |
| Moderate DHA | 7.25 (1.68) | 7.00 (1.41) | 0.214 | 0.812 | 0.892 | 0.788 | 0.008 * | ||
| High DHA | 6.94 (1.61) | 6.78 (1.90) | 0.033 | 0.001 | 0.002 | 0.001 | 0.074 | ||
| T2 score | |||||||||
| Low DHA | 9.87 (2.97) | 8.91 (0.69) | 1.733 | 0.923 | 0.323 | 0 | 14.652 | NS | NS |
| Moderate DHA | 10.85 (2.87) | 9.10 (2.13) | 0.182 | 0.339 | 0.725 | 0.982 | <0.001 * | ||
| High DHA | 10.25 (1.18) | 10.28 (2.63) | 0.036 | 0.01 | 0.007 | 0 | 0.137 | ||
| T3 score | |||||||||
| Low DHA | 11.09 (2.17) | 11.50 (2.72) | 1.096 | 0.184 | 0.641 | 3.039 | 15.105 | NS | NS |
| Moderate DHA | 11.70 (2.06) | 10.38 (2.06) | 0.338 | 0.669 | 0.529 | 0.085 | <0.001 * | ||
| High DHA | 11.75 (2.05) | 11.94 (1.86) | 0.023 | 0.002 | 0.014 | 0.032 | 0.141 | ||
| T4 score | |||||||||
| Low DHA | 11.96 (2.35) | 12.20 (2.20) | 1.769 | 0.1 | 0.913 | 2.062 | 31.252 | NS | NS |
| Moderate DHA | 13.15 (1.73) | 11.54 (3.05) | 0.176 | 0.752 | 0.405 | 0.154 | <0.001 * | ||
| High DHA | 12.63 (1.09) | 13.06 (1.51) | 0.037 | 0.001 | 0.019 | 0.022 | 0.254 | ||
| T5 score | |||||||||
| Low DHA | 12.09 (2.28) | 13.10 (1.60) | 0.038 | 0.366 | 1.816 | 0.881 | 19.51 | NS | NS |
| Moderate DHA | 13.05 (1.79) | 11.77 (1.88) | 0.963 | 0.547 | 0.169 | 0.35 | <0.001 * | ||
| High DHA | 12.44 (1.63) | 12.89 (1.64) | 0.001 | 0.004 | 0.038 | 0.009 | 0.175 | ||
| VLMT interference parameters | DHA: F(6,182) = 0.933, p = 0.472, ηp2 = 0.039 S: F(3,90) = 0.716, p = 0.545, ηp2 = 0.023 I: F(6,182) = 2.219, p = 0.052 °, ηp2 = 0.066 G: F(3,90) = 0.480, p = 0.697, ηp2 = 0.016 IQ: F(3,90) = 8.593, p = < 0.001 ***, ηp2 = 0.223 |
||||||||
| I | |||||||||
| Low DHA | 7.13 (2.70) | 5.90 (2.38) | 0.066 | 0.804 | 0.753 | 1.131 | 16.398 | NS | NS |
| Moderate DHA | 6.60 (1.76) | 5.92 (2.63) | 0.936 | 0.372 | 0.474 | 0.29 | <0.001 * | ||
| High DHA | 6.25 (2.46) | 6.39 (1.91) | 0.001 | 0.009 | 0.016 | 0.012 | 0.151 | ||
| T6 | |||||||||
| Low DHA | 11.43 (2.76) | 12.70 (2.36) | 1.405 | 0.006 | 4.337 | 0.445 | 12.435 | I: s/h > s/m I: m/m > s/m |
p = 0.036 *
p = 0.021 * |
| Moderate DHA | 12.45 (2.21) | 10.00 (2.35) | 0.251 | 0.936 | 0.016 * | 0.506 | 0.001 * | ||
| High DHA | 12.06 (1.95) | 12.61 (1.29) | 0.03 | 0 | 0.086 | 0.005 | 0.119 | ||
| T5–6 | |||||||||
| Low DHA | 0.65 (1.56) | 0.40 (1.58) | 2.621 | 0.613 | 1.959 | 0.017 | 0.006 | NS | NS |
| Moderate DHA | 0.60 (1.60) | 1.77 (1.64) | 0.078 | 0.436 | 0.147 | 0.897 | 0.936 | ||
| High DHA | 0.38 (1.41) | 0.28 (1.32) | 0.054 | 0.007 | 0.041 | 0 | 0 | ||
| VLMT Long-term memory parameters | DHA: F(4,184) = 0.599, p = 0.664, ηp2 = 0.013 S: F(2,91) = 0.181, p = 0.835, ηp2 = 0.004 I: F(4,184) = 1.805, p = 0.130, ηp2 = 0.038 G: F(2,91) = 0.488, p = 0.615, ηp2 = 0.011 IQ: F(2,91) = 11.721, p < 0.001 ***, ηp2 = 0.205 |
||||||||
| T7 | |||||||||
| Low DHA | 11.70 (2.79) | 11.90 (2.51) | 0.804 | 0.151 | 1.598 | 0.744 | 19.794 | NS | NS |
| Moderate DHA | 12.25 (2.95) | 10.62 (2.18) | 0.45 | 0.698 | 0.208 | 0.391 | <0.001 * | ||
| High DHA | 11.69 (2.02) | 13.00 (1.33) | 0.017 | 0.002 | 0.034 | 0.008 | 0.177 | ||
| T5–7 | |||||||||
| Low DHA | 0.39 (1.64) | 1.20 (1.75) | 1.11 | 0.011 | 1.86 | 0.031 | 1.802 | NS | NS |
| Moderate DHA | 0.80 (2.12) | 1.15 (1.46) | 0.334 | 0.916 | 0.161 | 0.86 | 0.183 | ||
| High DHA | 0.75 (1.44) | −0.11 (1.41) | 0.024 | 0 | 0.039 | 0 | 0.019 | ||
| Moderate depression N = 58 M (SD) |
Severe depression N = 41 M (SD) |
||||||||
| Digits forward | |||||||||
| Low DHA | 9.09 (2.18) | 9.90 (1.37) | 3.342 | 0.956 | 1.523 | 0.23 | 25.145 | NS | NS |
| Moderate DHA | 8.45 (1.50) | 7.85 (1.41) | 0.040 * | 0.543 | 0.224 | 0.633 | <0.001 * | ||
| High DHA | 8.69 (1.66) | 8.28 (2.08) | 0.068 | 0.004 | 0.032 | 0.003 | 0.216 | ||
| Digits backward | |||||||||
| Low DHA | 8.64 (2.36) | 8.60 (1.17) | 0.78 | 0.005 | 0.192 | 0.058 | 17.851 | NS | NS |
| Moderate DHA | 8.15 (1.81) | 7.62 (1.26) | 0.461 | 0.942 | 0.826 | 0.81 | <0.001 * | ||
| High DHA | 8.19 (1.64) | 7.89 (1.61) | 0.017 | 0 | 0.004 | 0.001 | 0.164 | ||
Note: GIX, global intelligence index. ηp2 = 0.01 (small), 0.06 (medium), and 0.14 (large). L, low DHA status; m, moderate DHA status; h, high DHA status; m/l, moderately depressed with a low DHA status; m/m, moderately depressed with a moderate DHA status; m/h, moderately depressed with a high DHA status; s/l, severely depressed with a low DHA status; s/m, severely depressed with a moderate DHA status; s/h, severely depressed with a high DHA status. Group sizes (n): m/l = 23; m/m = 20; m/h = 16; s/l = 10; s/m = 13; s/h = 18. Multivariate effects, pairwise comparisons: ° borderline significant * p < 0.05, *** p < 0.001. Between-subjects effects: ° borderline significant, * p < 0.010 (short-term memory), * p < 0.017 (interference), and * p < 0.025 (long-term memory) after Bonferroni correction of the significance level. Significant effects are marked in bold. T1–7, trials 1–7; NS, not significant.
4. Discussion
The current study investigated RBC EPA and DHA levels, as well as depression severity in relation to memory performance in a sample of 107 moderately to severely depressed youths.
Contrary to previous findings that reported inverse associations between oily fish intake and depression severity [98], in our sample severely depressed patients had significantly higher DHA and total omega-3 statuses compared to moderately depressed patients. Whereas negative associations between EPA status and depression severity have been reported [50], we found no significant differences concerning EPA status between moderately and depressed patients.
In our study, we examined potential cognitive deficits in depressed children and adolescents that have been inconsistently found in previous studies [30,31,32,33,34] in contrast to research conducted in adult patient groups, where deficits seem more consistent [20,21,22,23,24,25,26]. Although most patients achieved average normative scores for both the VLMT and the digit span test, over 20% of the patients (compared to an expected 15.9% in a healthy population) achieved below average normative scores. These results indicate a tendency toward impaired verbal memory in depressed youths.
We further aimed at investigating potential negative associations between depression severity and cognitive functioning in depressed youths that so far have mostly been reported in adult patient groups [35,99], with similar tendencies from research conducted in children and adolescents [36]. Contrary to our hypothesis, in our sample we did not find any significant differences in verbal memory performance between moderately and severely depressed patients. Hence, we could not confirm any negative associations between depression severity and cognitive functions previously reported in adult patient groups [35,99].
Most importantly, we were interested in memory performance in relation to EPA and DHA status, because EPA supplementation has mostly been associated with beneficial cognitive effects in youths [69,77], and beneficial cognitive effects would prove especially important in this vulnerable population. Our results indicated that patients with a high EPA status had steeper learning curves across the short-term memory trials of a verbal list learning test, compared to patients with a moderate or low EPA status. Compared to patients with a moderate or low EPA status, those with a high EPA status, seemed to remember more words faster, although they achieved equal scores in the first trial and again in the last two trials. This finding only partly confirmed our hypothesis that patients with a high EPA status would outperform patients with a low EPA status in verbal memory tests, because differences were only observed for the second and third trials and not overall. Moreover, these differences were only found for short-term memory parameters, whereas no significant effect for EPA status presented for any other VLMT parameter or the digit span test. However, we were able to confirm our hypothesis concerning DHA by finding no significant effect of DHA on any verbal memory parameter. Both results are in line with previous findings from meta-analyses on supplementation effects of EPA and DHA that suggested beneficial effects of EPA but not DHA on cognitive functioning [69,77] and effects in clinical rather than healthy populations [69]. In contrast to our hypothesis, we were not able to confirm any superior effects of a high EPA status in severely compared to moderately depressed patients.
A number of limitations should be kept in mind when interpreting the reported results. First, no healthy control group was investigated; hence, no comparison between depressed and healthy children and adolescents could be made. Nevertheless, our data suggested that a somewhat larger proportion of participants than expected in a healthy population achieved below average normative scores in both tests. Importantly, the current study was based on a cross-sectional design. It is hence limited by the impossibility to draw conclusions about any causal relationships. Another methodological limitation lies in the small and unequally sized subgroups formed by the two factors of depression severity and DHA and EPA status. Moreover, for several analyses the Levene’s tests proved significant. However, rather conservative statistical methods for correction were applied throughout the analyses, minimizing the probability of a type-I error.
Our results further contribute to previous findings that reported some impairment considering cognitive functions [30,31,32] and especially memory performance [34] in depressed youths. Future studies should investigate differences between healthy and depressed individuals concerning memory performance in order to be able to further confirm these findings and make recommendations for cognitive assessments in this population. Surprisingly, the analyses of our sample revealed higher DHA and total omega-3 status in severely compared to moderately depressed patients. One explanation for this finding might lie in altered nutritional patterns in severely compared to moderately depressed youths. Moreover, considering the population investigated, low n-3 PUFA levels were expected to begin with, and hence, small ranges were presented. Wider ranges might therefore have produced different results. This explanation is, of course, only speculative. Although the reported analyses with EPA and DHA only contributed associations between RBC levels and verbal memory rather than effects of supplementation, they further corroborate evidence from meta-analyses that confirmed the beneficial supplementation effects of EPA but not DHA. Thus, our findings suggest that an increased dietary intake of EPA might prove beneficial for cognitive improvement or even remission in depressed youths. Based on our findings, future RCTs should investigate the effects of EPA compared to DHA supplementation in depressed children and adolescents to potentially establish a recommendation for a natural and easily accessible intervention for cognitive improvement or remission in depressed youths. Neuroimaging studies have tried to explain differences in supplementation effectivity between DHA and EPA. Bauer et al. [100], for example, reported a reduction in functional activation in the left anterior cingulate cortex and shorter reaction times in the Stroop color–word task following EPA rather than DHA supplementation, which, they argued, might represent stronger neural efficiency in EPA-supplemented compared to DHA-supplemented individuals. Biologically, however, the supplementation advantages of EPA over DHA have yet to be explained, considering EPA is found in much smaller concentrations within the brain compared to DHA [61,101]. As there is also a lack of understanding about the actual absorption and utilization of both EPA and DHA, it would be paramount to investigate the moderating effects of, for example, the microbiome, as differences might be expected, and these again might explain differential effects in different populations.
Acknowledgments
The authors would like to thank all members of the Omega-3 Study team, especially all members of the clinical sites for their help in recruiting patients, namely. Oliver Pick and Alain Di Gallo from the Department of Child and Adolescent Psychiatry, Psychiatric University Hospitals Basel; Stefan Müller from the Child and Adolescent Psychiatric Services Baselland; Simone Heitzer and Maria Dokianaki from the Clienia Littenheid; Amir Yamini from the Child and Adolescent Psychiatric Services Thurgau; Michael Schmid from the Child and Adolescent Psychiatric Services St. Gallen; Ioannis Christodoulakis from the Klinik Sonnenhof. Additionally, the authors would like to thank the Translational Molecular Psychiatry unit of the Department of Child and Adolescent Psychiatry and Psychotherapy, namely, Edna Grünblatt, for their help with storing the collected blood samples. Especially, the authors thank all of their patients and their families for participating in the present study.
Author Contributions
Conceptualization, S.E. (Sophie Emery) and R.D.; methodology, S.E. (Sophie Emery), I.H., G.B., S.W., and R.D.; software, S.E. (Sophie Emery); validation, I.H.; formal analysis, S.E. (Sophie Emery); investigation, S.E. (Sophie Emery), N.B., M.S., M.A., K.N., and I.H.; resources, S.W., K.S., S.E. (Suzanne Erb), S.B., L.W., U.M.-K., B.C.-W., B.R., and M.H; data curation, S.E.; M.H. and I.H.; writing—original draft preparation, S.E.; writing—review and editing, R.D., I.H., and G.B.; visualization, S.E. (Sophie Emery); supervision, R.D., G.B., K.S., S.W., and I.H.; project administration, S.E. (Sophie Emery), I.H., N.B., M.S., M.A., and K.N.; funding acquisition, G.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Swiss National Foundation, grant number 33IC30_166826. Furthermore, the Thalmann Foundation (University of Basel), the Ebnet Foundation, and the Vontobel Foundation supported additional PhD projects. The Research Department of Child and Adolescent Psychiatry, University Hospital of Psychiatry Zurich of the University of Zurich provided infrastructure and administrative staff support. Burgerstein, Antistress AG, and Rapperswil-Jona (SG, Switzerland) provided the study medication for the clinical trial with no restrictions regarding data analysis or publication rights. No additional industrial funding was provided throughout the study.
Conflicts of Interest
G.B. was supported by the Swiss National Science Foundation, the Stanley Foundation, the Gertrud Thalmann Fonds, and the Ebnet Foundation and he has received lecture honoraria from Lundbeck, Opopharma, Antistress AG (Burgerstein) in the last five years. In the last five years, K.S. has received royalties from Springer, Hogrefe, Schattauer, and Vandenhoeck & Ruprecht, as well as a lecture honorarium from Vifor. His work was supported by the Swiss National Science Foundation (SNF), the Swiss Ministry of Justice, the University of St. Gallen, the Botnar Foundation, and Gertrud Thalmann Fonds in the last five years. In the last five years, S.W. has received royalties from Thieme, Hogrefe, Kohlhammer, Springer, and Beltz. In the last five years, her work has been supported by the Swiss National Science Foundation (SNF), diff. EU FP7s, HSM Hochspezialisierte Medizin of the Kanton Zurich, Switzerland, Bfarm Germany, ZInEP, Hartmann Müller Stiftung, and the Olga Mayenfisch, Gertrud Thalmann, Vontobel, Unicentia, and Erika Schwarz Fonds. Outside professional activities and interests are declared under the link of the University of Zurich www.uzh.ch/prof/ssl-dir/interessenbindungen/client/web/. The other authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Depression and Other Common Mental Disorders: Global Health Estimates. WHO; Geneva, Switzerland: 2017. [Google Scholar]
- 2.Kessler R.C., Bromet E.J. The Epidemiology of Depression Across Cultures. Annu. Rev. Public Health. 2013;34:119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler R.C., Sampson N.A., Berglund P., Gruber M.J., Al-Hamzawi A., Andrade L., Bunting B., Demyttenaere K., Florescu S., De Girolamo G., et al. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol. Psychiatr. Sci. 2015;24:210–226. doi: 10.1017/S2045796015000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler R.C., Amminger G.P., Aguilar-Gaxiola S., Alonso J., Lee S., Ustun T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry. 2007;20:359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zisook S., Lesser I., Stewart J.W., Wisniewski S.R., Balasubramani G., Fava M., Gilmer W.S., Dresselhaus T.R., Thase M.E., Nierenberg A.A., et al. Effect of Age at Onset on the Course of Major Depressive Disorder. Am. J. Psychiatry. 2007;164:1539–1546. doi: 10.1176/appi.ajp.2007.06101757. [DOI] [PubMed] [Google Scholar]
- 6.Costello E.J., Mustillo S., Keeler G., Angold A. Mental Health Services: A Public Health Perspective. Oxford University Press; Oxford, UK: 2004. Prevalence of Psychiatric Disorders in Childhood and Adolescence; pp. 111–128. [Google Scholar]
- 7.Costello E.J., Egger H., Angold A. 10-Year Research Update Review: The Epidemiology of Child and Adolescent Psychiatric Disorders: I. Methods and Public Health Burden. J. Am. Acad. Child Adolesc. Psychiatry. 2005;44:972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 8.Costello E.J., Erkanli A., Angold A. Is there an epidemic of child or adolescent depression? J. Child Psychol. Psychiatry. 2006;47:1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 9.Avenevoli S., Swendsen J., Shelli A., Burstein M., Merikangas K.R. Major Depression in the National Comorbidity Survey–Adolescent Supplement: Prevalence, Correlates, and Treatment. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:37–44.e2. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . Depression and Other Common Mental Disorders—Global Health Estimates. IGO; Geneva, Switzerland: 2017. pp. 1–24. Licence: CC BY-NC-SA 3.0. [Google Scholar]
- 11.Erskine H.E., Moffitt T.E., Copeland W.E., Costello E.J., Ferrari A.J., Patton G., Degenhardt L., Vos T., Whiteford H.A., Scott J.G. A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol. Med. 2015;45:1551–1563. doi: 10.1017/S0033291714002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Arlington, VA, USA: 2013. [Google Scholar]
- 13.Knight M.J., Lyrtzis E., Baune B.T. The association of cognitive deficits with mental and physical Quality of Life in Major Depressive Disorder. Compr. Psychiatry. 2020;97:152147. doi: 10.1016/j.comppsych.2019.152147. [DOI] [PubMed] [Google Scholar]
- 14.Cambridge O.R., Knight M.J., Mills N., Baune B.T. The clinical relationship between cognitive impairment and psychosocial functioning in major depressive disorder: A systematic review. Psychiatry Res. 2018;269:157–171. doi: 10.1016/j.psychres.2018.08.033. [DOI] [PubMed] [Google Scholar]
- 15.Hammar Å. Cognitive functioning in major depression—A summary. Front. Hum. Neurosci. 2009;3:26. doi: 10.3389/neuro.09.026.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruder G.E., Alvarenga J.E., Alschuler D.M., Abraham K., Keilp J.G., Hellerstein D.J., Stewart J.W., McGrath P.J. Neurocognitive predictors of antidepressant clinical response. J. Affect. Disord. 2014;166:108–114. doi: 10.1016/j.jad.2014.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Etkin A., Patenaude B., Song Y.J.C., Usherwood T., Rekshan W., Schatzberg A.F., Rush A.J., Williams L.M. A Cognitive–Emotional Biomarker for Predicting Remission with Antidepressant Medications: A Report from the iSPOT-D Trial. Neuropsychopharmacology. 2014;40:1332–1342. doi: 10.1038/npp.2014.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fletcher J.M. Adolescent depression: Diagnosis, treatment, and educational attainment. Health Econ. 2008;17:1215–1235. doi: 10.1002/hec.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morey-Nase C., Phillips L.J., Bryce S., Hetrick S., Wright A.L., Caruana E., Allott K. Subjective experiences of neurocognitive functioning in young people with major depression. BMC Psychiatry. 2019;19:1–9. doi: 10.1186/s12888-019-2197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahern E., Semkovska M. Cognitive functioning in the first-episode of major depressive disorder: A systematic review and meta-analysis. Neuropsychology. 2017;31:52–72. doi: 10.1037/neu0000319. [DOI] [PubMed] [Google Scholar]
- 21.Porter R., Robinson L.J., Malhi G.S., Gallagher P. The neurocognitive profile of mood disorders—A review of the evidence and methodological issues. Bipolar Disord. 2015;17:21–40. doi: 10.1111/bdi.12342. [DOI] [PubMed] [Google Scholar]
- 22.Wagner S., Doering B., Helmreich I., Lieb K., Tadić A. A meta-analysis of executive dysfunctions in unipolar major depressive disorder without psychotic symptoms and their changes during antidepressant treatment. Acta Psychiatr. Scand. 2012;125:281–292. doi: 10.1111/j.1600-0447.2011.01762.x. [DOI] [PubMed] [Google Scholar]
- 23.Rock P.L., Roiser J.P., Riedel W.J., Blackwell A.D. Cognitive impairment in depression: A systematic review and meta-analysis. Psychol. Med. 2014;44:2029–2040. doi: 10.1017/S0033291713002535. [DOI] [PubMed] [Google Scholar]
- 24.Lim J., Oh I.K., Han C., Huh Y.J., Jung I.-K., Patkar A.A., Steffens D.C., Jang B.-H. Sensitivity of cognitive tests in four cognitive domains in discriminating MDD patients from healthy controls: A meta-analysis. Int. Psychogeriatr. 2013;25:1543–1557. doi: 10.1017/S1041610213000689. [DOI] [PubMed] [Google Scholar]
- 25.Snyder H.R. Major depressive disorder is associated with broad impairments on neuropsychological measures of executive function: A meta-analysis and review. Psychol. Bull. 2013;139:81–132. doi: 10.1037/a0028727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee R.S., Hermens D.F., Porter M.A., Redoblado-Hodge M.A. A meta-analysis of cognitive deficits in first-episode Major Depressive Disorder. J. Affect. Disord. 2012;140:113–124. doi: 10.1016/j.jad.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 27.Hasselbalch S.G., Knorr U., Kessing L.V. Cognitive impairment in the remitted state of unipolar depressive disorder: A systematic review. J. Affect. Disord. 2011;134:20–31. doi: 10.1016/j.jad.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 28.Biringer E., Mykletun A., Sundet K., Kroken R., Stordal K.I., Lund A. A longitudinal analysis of neurocognitive function in unipolar depression. J. Clin. Exp. Neuropsychol. 2007;29:879–891. doi: 10.1080/13803390601147686. [DOI] [PubMed] [Google Scholar]
- 29.Semkovska M., Quinlivan L., O’Grady T., Johnson R., Collins A., O’Connor J., Knittle H., Ahern E., Gload T. Cognitive function following a major depressive episode: A systematic review and meta-analysis. Lancet Psychiatry. 2019;6:851–861. doi: 10.1016/S2215-0366(19)30291-3. [DOI] [PubMed] [Google Scholar]
- 30.Wagner S., Müller C., Helmreich I., Huss M., Tadić A. A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. Eur. Child Adolesc. Psychiatry. 2015;24:5–19. doi: 10.1007/s00787-014-0559-2. [DOI] [PubMed] [Google Scholar]
- 31.Brooks B.L., Iverson G.L., Sherman E.M.S., Roberge M.-C. Identifying Cognitive Problems in Children and Adolescents with Depression Using Computerized Neuropsychological Testing. Appl. Neuropsychol. 2010;17:37–43. doi: 10.1080/09084280903526083. [DOI] [PubMed] [Google Scholar]
- 32.Goodall J., Fisher C., Hetrick S., Phillips L., Parrish E.M., Allott K. Neurocognitive Functioning in Depressed Young People: A Systematic Review and Meta-Analysis. Neuropsychol. Rev. 2018;28:216–231. doi: 10.1007/s11065-018-9373-9. [DOI] [PubMed] [Google Scholar]
- 33.Vilgis V., Silk T., Vance A. Executive function and attention in children and adolescents with depressive disorders: A systematic review. Eur. Child Adolesc. Psychiatry. 2015;24:365–384. doi: 10.1007/s00787-015-0675-7. [DOI] [PubMed] [Google Scholar]
- 34.Günther T., Holtkamp K., Jolles J., Herpertz-Dahlmann B., Konrad K. Verbal memory and aspects of attentional control in children and adolescents with anxiety disorders or depressive disorders. J. Affect. Disord. 2004;82:265–269. doi: 10.1016/j.jad.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 35.McDermott L.M., Ebmeier K. A meta-analysis of depression severity and cognitive function. J. Affect. Disord. 2009;119:1–8. doi: 10.1016/j.jad.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 36.Maalouf F.T., Brent D., Clark L., Tavitian L., McHugh R.M., Sahakian B.J., Phillips M.L. Neurocognitive impairment in adolescent major depressive disorder: State vs. trait illness markers. J. Affect. Disord. 2011;133:625–632. doi: 10.1016/j.jad.2011.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenblat J.D., Kakar R., McIntyre R.S. The Cognitive Effects of Antidepressants in Major Depressive Disorder: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int. J. Neuropsychopharmacol. 2016;19:pyv082. doi: 10.1093/ijnp/pyv082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennabi D., Haffen E., Van Waes V. Vortioxetine for Cognitive Enhancement in Major Depression: From Animal Models to Clinical Research. Front. Psychiatry. 2019;10:771. doi: 10.3389/fpsyt.2019.00771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Biringer E., Rongve A., Lund A. A Review of Modern Antidepressants Effects on Neurocognitive Function. Curr. Psychiatry Rev. 2009;5:164–174. doi: 10.2174/157340009788971137. [DOI] [Google Scholar]
- 40.Prado C.E., Watt S., Crowe S.F. A meta-analysis of the effects of antidepressants on cognitive functioning in depressed and non-depressed samples. Neuropsychol. Rev. 2018;28:32–72. doi: 10.1007/s11065-018-9369-5. [DOI] [PubMed] [Google Scholar]
- 41.Skandali N., Rowe J.B., Voon V., Deakin J.B., Cardinal R.N., Cormack F., Passamonti L., Bevan-Jones W.R., Regenthal R., Chamberlain S.R., et al. Dissociable effects of acute SSRI (escitalopram) on executive, learning and emotional functions in healthy humans. Neuropsychopharmacology. 2018;43:2645–2651. doi: 10.1038/s41386-018-0229-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bortolato B., Miskowiak K.W., Köhler C.A., Maes M., Fernandes B.S., Berk M., Carvalho A.F. Cognitive remission: A novel objective for the treatment of major depression? BMC Med. 2016;14:1–18. doi: 10.1186/s12916-016-0560-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zuckerman H., Pan Z., Park C., Brietzke E., Musial N., Shariq A.S., Iacobucci M., Yim S.J., Lui L.M.W., Rong C., et al. Recognition and Treatment of Cognitive Dysfunction in Major Depressive Disorder. Front. Psychiatry. 2018;9:655. doi: 10.3389/fpsyt.2018.00655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shilyansky C., Williams L.M., Gyurak A., Harris A., Usherwood T., Etkin A. Effect of antidepressant treatment on cognitive impairments associated with depression: A randomised longitudinal study. Lancet Psychiatry. 2016;3:425–435. doi: 10.1016/S2215-0366(16)00012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simopoulos A.P. Evolutionary Aspects of Diet: The Omega-6/Omega-3 Ratio and the Brain. Mol. Neurobiol. 2011;44:203–215. doi: 10.1007/s12035-010-8162-0. [DOI] [PubMed] [Google Scholar]
- 46.Simopoulos A.P. The Importance of the Omega-6/Omega-3 Fatty Acid Ratio in Cardiovascular Disease and Other Chronic Diseases. Exp. Biol. Med. 2008;233:674–688. doi: 10.3181/0711-MR-311. [DOI] [PubMed] [Google Scholar]
- 47.Li F., Liu X., Zhang D. Fish consumption and risk of depression: A meta-analysis. J. Epidemiol. Community Health. 2015;70:299–304. doi: 10.1136/jech-2015-206278. [DOI] [PubMed] [Google Scholar]
- 48.Lin P.-Y., Huang S.-Y., Su K.-P. A Meta-Analytic Review of Polyunsaturated Fatty Acid Compositions in Patients with Depression. Biol. Psychiatry. 2010;68:140–147. doi: 10.1016/j.biopsych.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 49.Edwards R., Peet M., Shay J., Horrobin D. Depletion of docosahexaenoic acid in red blood cell membranes of depressive patients. Biochem. Soc. Trans. 1998;26:S142. doi: 10.1042/bst026s142. [DOI] [PubMed] [Google Scholar]
- 50.Adams P.B., Lawson S., Sanigorski A., Sinclair A.J. Arachidonic acid to eicosapentaenoic acid ratio in blood correlates positively with clinical symptoms of depression. Lipids. 1996;31:S157–S161. doi: 10.1007/BF02637069. [DOI] [PubMed] [Google Scholar]
- 51.Sublette M.E., Ellis S.P., Geant A.L., Mann J.J. Meta-Analysis of the Effects of Eicosapentaenoic Acid (EPA) in Clinical Trials in Depression. J. Clin. Psychiatry. 2011;72:1577–1584. doi: 10.4088/JCP.10m06634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grosso G., Pajak A., Marventano S., Castellano S., Galvano F., Bucolo C., Drago F., Caraci F. Role of Omega-3 Fatty Acids in the Treatment of Depressive Disorders: A Comprehensive Meta-Analysis of Randomized Clinical Trials. PLoS ONE. 2014;9:e96905. doi: 10.1371/journal.pone.0096905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hallahan B., Ryan T., Hibbeln J.R., Murray I.T., Glynn S., Ramsden C.E., SanGiovanni J.P., Davis J.M. Efficacy of omega-3 highly unsaturated fatty acids in the treatment of depression. Br. J. Psychiatry. 2016;209:192–201. doi: 10.1192/bjp.bp.114.160242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mocking R.J.T., Harmsen I., Assies J., Koeter M.W.J., Ruhé H.G., Schene A.H. Meta-analysis and meta-regression of omega-3 polyunsaturated fatty acid supplementation for major depressive disorder. Transl. Psychiatry. 2016;6:e756. doi: 10.1038/tp.2016.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liao Y., Xie B., Zhang H., He Q., Guo L., Subramaniapillai M., Fan B., Lu C., Mclntyer R.S. Efficacy of omega-3 PUFAs in depression: A meta-analysis. Transl. Psychiatry. 2019;9:1–9. doi: 10.1038/s41398-019-0515-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Appleton K.M., Rogers P.J., Ness A.R. Updated systematic review and meta-analysis of the effects of n−3 long-chain polyunsaturated fatty acids on depressed mood. Am. J. Clin. Nutr. 2010;91:757–770. doi: 10.3945/ajcn.2009.28313. [DOI] [PubMed] [Google Scholar]
- 57.Bloch M.H., Hannestad J. Omega-3 fatty acids for the treatment of depression: Systematic review and meta-analysis. Mol. Psychiatry. 2012;17:1272–1282. doi: 10.1038/mp.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang L., Liu H., Kuang L., Meng H., Zhou X. Omega-3 fatty acids for the treatment of depressive disorders in children and adolescents: A meta-analysis of randomized placebo-controlled trials. Child Adolesc. Psychiatry Ment. Health. 2019;13:1–9. doi: 10.1186/s13034-019-0296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rapaport M.H., Nierenberg A.A., Schettler P.J., Kinkead B.L., Cardoos A., Walker R.S.W., Mischoulon D. Inflammation as a predictive biomarker for response to omega-3 fatty acids in major depressive disorder: A proof-of-concept study. Mol. Psychiatry. 2016;21:71–79. doi: 10.1038/mp.2015.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Young J.J., Bruno D., Pomara N. A review of the relationship between proinflammatory cytokines and major depressive disorder. J. Affect. Disord. 2014;169:15–20. doi: 10.1016/j.jad.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 61.Bazinet R.P., Layé S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 2014;15:771–785. doi: 10.1038/nrn3820. [DOI] [PubMed] [Google Scholar]
- 62.Koletzko B., Lien E., Agostoni C., Böhles H., Campoy C., Cetin I., Decsi T., Dudenhausen J.W., Dupont C., Forsyth S., et al. The roles of long-chain polyunsaturated fatty acids in pregnancy, lactation and infancy: Review of current knowledge and consensus recommendations. J. Perinat. Med. 2008;36:5–14. doi: 10.1515/JPM.2008.001. [DOI] [PubMed] [Google Scholar]
- 63.Baumgartner J. Handbook of Lipids in Human Function. Elsevier; Amsterdam, The Netherlands: 2016. Effects of Omega-3 Fatty Acid Supplementation on Cognition in Children; pp. 331–375. [Google Scholar]
- 64.Lauritzen L., Brambilla P., Mazzocchi A., Harsløf L., Ciappolino V., Agostoni C. DHA Effects in Brain Development and Function. Nutrients. 2016;8:6. doi: 10.3390/nu8010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lassek W.D., Gaulin S.J. Sex Differences in the Relationship of Dietary Fatty Acids to Cognitive Measures in American Children. Front. Evol. Neurosci. 2011;3:3. doi: 10.3389/fnevo.2011.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Darcey V.L., McQuaid G.A., Fishbein D.H., VanMeter J.W. Dietary Long-Chain Omega-3 Fatty Acids Are Related to Impulse Control and Anterior Cingulate Function in Adolescents. Front. Neurosci. 2019;12:1012. doi: 10.3389/fnins.2018.01012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Montgomery P., Burton J.R., Sewell R.P., Spreckelsen T.F., Richardson A.J. Low Blood Long Chain Omega-3 Fatty Acids in UK Children Are Associated with Poor Cognitive Performance and Behavior: A Cross-Sectional Analysis from the DOLAB Study. PLoS ONE. 2013;8:e66697. doi: 10.1371/annotation/26c6b13f-b83a-4a3f-978a-c09d8ccf1ae2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Van Der Wurff I.S.M., Von Schacky C., Berge K., Zeegers M.P.A., Kirschner P.A., De Groot R.H.M. Association between Blood Omega-3 Index and Cognition in Typically Developing Dutch Adolescents. Nutrients. 2016;8:13. doi: 10.3390/nu8010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Emery S., Häberling I., Berger G., Walitza S., Schmeck K., Albert T., Baumgartner N., Strumberger M., Albermann M., Drechsler R. Omega-3 and its domain-specific effects on cognitive test performance in youths: A meta-analysis. Neurosci. Biobehav. Rev. 2020;112:420–436. doi: 10.1016/j.neubiorev.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 70.Jiao J., Li Q., Chu J., Zeng W., Yang M., Zhu S. Effect of n−3 PUFA supplementation on cognitive function throughout the life span from infancy to old age: A systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2014;100:1422–1436. doi: 10.3945/ajcn.114.095315. [DOI] [PubMed] [Google Scholar]
- 71.Chang J.P.-C., Su K.-P., Mondelli V., Pariante C.M. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacology. 2018;43:534–545. doi: 10.1038/npp.2017.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bloch M.H., Qawasmi A. Omega-3 Fatty Acid Supplementation for the Treatment of Children with Attention-Deficit/Hyperactivity Disorder Symptomatology: Systematic Review and Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatry. 2011;50:991–1000. doi: 10.1016/j.jaac.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cooper R.E., Tye C., Kuntsi J., Vassos E., Asherson P. Omega-3 polyunsaturated fatty acid supplementation and cognition: A systematic review and meta-analysis. J. Psychopharmacol. 2015;29:753–763. doi: 10.1177/0269881115587958. [DOI] [PubMed] [Google Scholar]
- 74.Naderali E.K., Naderali M.-M., Abubakari A.-R. Omega-3 fatty acid supplementation and cognitive function: Are smaller dosages more beneficial? Int. J. Gen. Med. 2014;7:463–473. doi: 10.2147/IJGM.S67065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mazereeuw G., Lanctôt K.L., Chau S.A., Swardfager W., Herrmann N. Effects of omega-3 fatty acids on cognitive performance: A meta-analysis. Neurobiol. Aging. 2012;33:1482.e17–1482.e29. doi: 10.1016/j.neurobiolaging.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 76.Karr J.E., Alexander J.E., Winningham R.G. Omega-3 polyunsaturated fatty acids and cognition throughout the lifespan: A review. Nutr. Neurosci. 2011;14:216–225. doi: 10.1179/1476830511Y.0000000012. [DOI] [PubMed] [Google Scholar]
- 77.Chang J.P.-C., Su K.-P., Mondelli V., Satyanarayanan S.K., Yang H.-T., Chiang Y.-J., Chen H.-T., Pariante C.M. High-dose eicosapentaenoic acid (EPA) improves attention and vigilance in children and adolescents with attention deficit hyperactivity disorder (ADHD) and low endogenous EPA levels. Transl. Psychiatry. 2019;9:1–9. doi: 10.1038/s41398-019-0633-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Knochel C., Voss M., Gruter F., Alves G.S., Matura S., Sepanski B., Stablein M., Wenzler S., Prvulovic D., Carvalho A.F., et al. Omega 3 Fatty Acids: Novel Neurotherapeutic Targets for Cognitive Dysfunction in Mood Disorders and Schizophrenia? Curr. Neuropharmacol. 2015;13:663–680. doi: 10.2174/1570159X13666150630173047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rogers P.J., Appleton K.M., Kessler D., Peters T.J., Gunnell D., Hayward R.C., Heatherley S.V., Christian L.M., McNaughton S.A., Ness A.R. No effect ofn-3 long-chain polyunsaturated fatty acid (EPA and DHA) supplementation on depressed mood and cognitive function: A randomised controlled trial. Br. J. Nutr. 2008;99:421–431. doi: 10.1017/S0007114507801097. [DOI] [PubMed] [Google Scholar]
- 80.Vesco A.T., Young A.S., Arnold L.E., Fristad M.A. Omega-3 supplementation associated with improved parent-rated executive function in youth with mood disorders: Secondary analyses of the omega 3 and therapy (OATS) trials. J. Child Psychol. Psychiatry. 2017;59:628–636. doi: 10.1111/jcpp.12830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Häberling I., Berger G., Schmeck K., Held U., Walitza S. Omega-3 Fatty Acids as a Treatment for Pediatric Depression. A Phase III, 36 Weeks, Multi-Center, Double-Blind, Placebo-Controlled Randomized Superiority Study. Front. Psychiatry. 2019;10 doi: 10.3389/fpsyt.2019.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Arlington, VA, USA: 2000. Text Revision (DSM-IV-TR) [Google Scholar]
- 83.Poznanski E., Mokros H. Children’s Depression Rating Scale–Revised. Volume 12 WPS; Los Angeles, CA, USA: 1996. [Google Scholar]
- 84.Guo Y., Nilsson M.E., Heiligenstein J., Wilson M.G., Emslie G. An Exploratory Factor Analysis of the Children’s Depression Rating Scale—Revised. J. Child Adolesc. Psychopharmacol. 2006;16:482–491. doi: 10.1089/cap.2006.16.482. [DOI] [PubMed] [Google Scholar]
- 85.Kaufman J., Birmaher B., Brent D., Rao U., Flynn C., Moreci P., Williamson D., Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 86.Mayes T.L., Bernstein I.H., Haley C.L., Kennard B.D., Emslie G.J. Psychometric Properties of the Children’s Depression Rating Scale–Revised in Adolescents. J. Child Adolesc. Psychopharmacol. 2010;20:513–516. doi: 10.1089/cap.2010.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Harris W.S., Von Schacky C., Park Y. The Omega-3 Fatty Acid Deficiency Syndrome: Opportunities for Disease Prevention. Nova Science Publishers; Hauppauge, NY, USA: 2013. Standardizing Methods for Assessing Omega-3 Fatty Acid Biostatus; pp. 385–398. [Google Scholar]
- 88.Helmstaedter C., Durwen H.F. Vlmt: Verbaler Lern- Und Merkfahigkeitstest. Ein Praktikables und Differenziertes Instrumentarium zur Prufung der Verbalen Gedachtnisleistungen. Schweiz. Arch. Neurol. Psychiatry. 1990;141:21–30. [PubMed] [Google Scholar]
- 89.Schmidt M. Auditory and Verbal Learning Test. A handbook. Western Psychological Association; Los Angeles, CA, USA: 1996. [Google Scholar]
- 90.Wechsler D. Wechsler Intelligence Scale for Children. 4th ed. The Psychological Corporation; San Antonio, TX, USA: 2003. (WISC-IV) [Google Scholar]
- 91.Hagmann-Von A.P., Grob A. Reynolds Intellectual Assessment Scales and Screening. Deutschsprachige Adaptation der Reynolds Intellectual Assessment Scales (RIAS) & des Reynolds Intellectual Screening Test (RIST) von Cecil R. Reynolds und Randy W. Kamphaus. Huber; Unterschleißheim, Germany: 2014. [Google Scholar]
- 92.Gygi J.T., Arx P.H.-V., Schweizer F., Grob A. The Predictive Validity of Four Intelligence Tests for School Grades: A Small Sample Longitudinal Study. Front. Psychol. 2017;8:8. doi: 10.3389/fpsyg.2017.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Krist H., Kunter M., Nückles M., Pinquart M., Seidel T. Testbesprechung. Z. Entwickl. Padag. Psychol. 2016;48:50–55. [Google Scholar]
- 94.Von Schacky C. Verwirrung um die Wirkung von Omega-3-Fettsäuren. Internist (Berl.) 2019;60:1319–1327. doi: 10.1007/s00108-019-00687-x. [DOI] [PubMed] [Google Scholar]
- 95.Lumley T., Diehr P., Emerson S., Chen L. The Importance of the Normality Assumption in Large Public Health Data Sets. Annu. Rev. Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- 96.Ateş C., Kaymaz O., Kale H.E., Tekindal M.A. Comparison of Test Statistics of Nonnormal and Unbalanced Samples for Multivariate Analysis of Variance in terms of Type-I Error Rates. Comput. Math. Methods Med. 2019;2019:2173638. doi: 10.1155/2019/2173638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Howell D.C. Statistical Methods for Psychology. 7th ed. Wadsworth Cengage Learning; Belmont, CA, USA: 2012. [Google Scholar]
- 98.Bountziouka V., Polychronopoulos E., Zeimbekis A., Papavenetiou E., Ladoukaki E., Papairakleous N., Gotsis E., Metallinos G., Lionis C., Panagiotakos D. Long-Term Fish Intake is Associated with Less Severe Depressive Symptoms Among Elderly Men and Women. J. Aging Health. 2009;21:864–880. doi: 10.1177/0898264309340693. [DOI] [PubMed] [Google Scholar]
- 99.McClintock S.M., Husain M.M., Greer T.L., Cullum C.M. Association between depression severity and neurocognitive function in major depressive disorder: A review and synthesis. Neuropsychology. 2010;24:9–34. doi: 10.1037/a0017336. [DOI] [PubMed] [Google Scholar]
- 100.Bauer I.E., Hughes M., Rowsell R., Cockerell R., Pipingas A., Crewther S., Crewther D. Omega-3 supplementation improves cognition and modifies brain activation in young adults. Hum. Psychopharmacol. Clin. Exp. 2014;29:133–144. doi: 10.1002/hup.2379. [DOI] [PubMed] [Google Scholar]
- 101.Weiser M.J., Butt C.M., Mohajeri M.H. Docosahexaenoic Acid and Cognition throughout the Lifespan. Nutrients. 2016;8:99. doi: 10.3390/nu8020099. [DOI] [PMC free article] [PubMed] [Google Scholar]