Abstract
Anthrax is a worldwide zoonotic disease caused by the spore-forming bacterium Bacillus anthracis. Primarily a disease of herbivores, human infections often result from direct contact with contaminated animal products (cutaneous and inhalational anthrax) or through consumption of infected meat (gastrointestinal anthrax). The genetic near neighbor, Bacillus cereus biovar anthracis (Bcbva), causes an anthrax-like illness in the wildlife and livestock of west and central Africa due to the presence and expression of B. anthracis-specific virulence factors in this background. While Bcbva infections have not been reported in humans, a recent seroprevalence study detected Bcbva antibodies in the rural population around Taï National Park. This work describes the development of new TaqMan multiplex PCRs for the simultaneous detection of B. anthracis and Bcbva. The assays are designed to amplify Ba-1, capB, and lef markers in B. anthracis and genomic island IV (GI4), capB, and lef in Bcbva. Our assays allow for the rapid discrimination of B. anthracis and Bcbva and will provide insights into the molecular epidemiology of these two important pathogens that share an overlapping geographical range in west and central Africa.
Keywords: Bacillus anthracis, Bacillus cereus biovar anthracis, anthrax, multiplex, Ba-1, Africa
1. Introduction
The Gram-positive spore producing Bacillus anthracis is the causative agent of anthrax, a worldwide zoonosis that primarily affects livestock and herbivores. Human infections are predominantly acquired through contact with or ingestion of infected animal products [1,2]. Cutaneous anthrax, the most common presentation in humans, is estimated to account for 20,000 cases annually and has a 20% mortality rate without treatment [3,4,5]. Another closely related member of the B. cereus group, Bacillus cereus biovar anthracis (Bcbva), has been reported to cause anthrax-like illness in wildlife and the livestock of west and central Africa [6,7,8,9,10,11]. Genotypically, Bcbva forms its own distinct clade and is more closely related to other members of the B. cereus group than to B. anthracis [12,13]. Phenotypically however, Bcbva shares some traits with B. anthracis, including the characteristic Medusa head appearance, the tenacious colony consistency, and the absence of beta-hemolysis [8,12]. Notably, Bcbva harbors the pXO1- and pXO2-like plasmids pBCXO1 and pBCXO2, which like their counterparts in B. anthracis, encode anthrax toxin (pag, protective antigen; lef, lethal factor; cya, edema factor), and the poly-γ-d-glutamate capsule, respectively [12,13]. In addition, the presence of chromosomal genomic islands, most of which are thus far unique to Bcbva, can be used as markers for specific detection of the pathogen [12,13]. While Bcbva anthrax-like infections have not been reported in humans, a recent seroprevalence study detected Bcbva-specific antibodies in the rural population around Taï National Park [14,15]. Improved diagnostics will be essential in uncovering and detecting cases in areas reporting Bcvba in bush meat or livestock.
Currently, no single assay exists for the rapid and simultaneous identification of these two pathogens that share an overlapping geographic distribution in western and central Africa [16,17,18,19,20]. Prompt and concurrent diagnosis is necessary in areas where both B. anthracis and Bcbva circulate and could further aid in monitoring the spread of Bcbva across its currently known geographical range. Our work here describes the development of two independent TaqMan multiplex PCR assays for the simultaneous identification of B. anthracis and Bcbva based on detection of unique chromosomal and plasmid markers. Specifically, the assay targeted the lef (pXO1) and capB (pXO2) virulence markers of B. anthracis, which are also present in the pXO1- and pXO2-like plasmids of Bcbva. The previously described chromosomal marker Ba-1 was first introduced for detection of B. anthracis and used for multiple outbreaks and for species confirmation ahead of genotyping [17,21]; the marker is routinely used to screen field and laboratory strains with high repeatability and is routinely confirmed with multi-locus variable tandem repeat analysis (MLVA) genotyping [17,21]. The Ba-1 marker appears to be unique to B. anthracis and encodes a hypothetical protein of unknown function in Ames (GenBank: AJH92142.1, Ames). For identification of Bcbva, a previously published assay for detection of genomic island IV (GI4) unique to this pathogen was adopted [12]. The assays were optimized across two different platforms, QuantStudio 7 and the LightCycler 2.0 (LC2), and a globally diverse panel of strains were tested for assay validation. These assays are easily adaptable across a range of qPCR platforms and may be useful for the diagnosis of B. anthracis and anthrax-toxin producing B. cereus such as Bcbva in areas with limited sequencing capabilities.
2. Materials and Methods
2.1. Bacterial Strains and Plasmids
For this study, a panel of 26 globally diverse B. anthracis strains that included representatives of each major lineage was selected from the Martin E. Hugh-Jones Bacillus anthracis collection curated at the University of Florida (Table 1). This collection well represents the global diversity and geography of B. anthracis [22], including several low passage wild type strains [23,24]. In addition, five Bcbva isolates from the bones and teeth of deceased monkeys collected from Taï National Park between 1994 and 2010 (unpublished data), were also tested along with various Bacillus cereus and Bacillus thuringiensis strains (both from BEI Resources Repository; www.beiresources.org). Globally, there are few Bcbva strains available in collections. Here, we tested a bone collection used for anthropological study. Briefly, to recover Bcbva, our lab tested bone fragments, teeth, or dried marrow from individual bones collected from Taï Forest, Côte d’Ivoire in West Africa representing Cercocebus atys, Cercopithecus diana, Colobus polykomos, Piliocolobus badius and Procolobus verus (Cercopithecoidea, Primates). Biological materials were bead beat using 0.1 mm beads for 5 min in 1X PBS 0.05% Tween-20 and centrifuged at 233× g for 2 min to remove large debris. The supernatant was centrifuged for 10 min at 3724× g to pellet bacterial spores. The pellet was cultured directly on sheep blood agar (SBA) or first incubated in 70% ethanol for 1 h then cultured on SBA. Non-hemolytic suspect colonies were sub-cultured for DNA extraction on SBA and confirmatory PCR (data not shown) was performed using singleplex qPCR assays targeting Ba-1, GI4, lef (lethal factor), and capB (capsule). For further confirmation, one of our isolates, Bc0001, was sequenced on the Illumina MiSeq platform and compared to the Bcbva type strain in GenBank (BioSample accession SAMN02603256). Additionally, a GI4 positive DNA control was constructed by cloning a 1297-bp region of Bcbva DNA encompassing GI4 sequences, into Blue Heron pUCminusMCS vector (pGI4) (Custom design, BlueHeron Biotech, Bothell, WA, USA).
Table 1.
Diversity panel of Bacillus cereus group used to validate multiplex PCR assays in this study.
| A List/ Original ID |
UF ID | Species | Strain | Lineage * | Strain Details |
|---|---|---|---|---|---|
| A0987 | UF00175 | B. anthracis | A.Br.005.006 | Botswana | |
| A0020 | UF00552 | B. anthracis | Ames | A3b | CAMR/Porton |
| A0537 | UF00965 | B. anthracis | A.Br.001/002 | China | |
| N/A | UF01137 | B. anthracis | WNA | A1.a, A.Br.WNA | Colorado, domestic cow, 2012 |
| A0897 | UF00727 | B. anthracis | A.Br.008/009 | Ethiopia | |
| A0389 | UF00930 | B. anthracis | A.Br.001/002 | Indonesia | |
| A0084 | UF00980 | B. anthracis | Vollum 1 | A4, A.Br.Vollum | South Africa |
| A2075 | UF01105 | B. anthracis | Ames | A.Br.005.006 | Tanzania |
| A0462 | UF00738 | B. anthracis | Ames | A3b | |
| A2017 | UF01114 | B. anthracis | Sterne | A.Br.001/002 | Texas, white-tailed deer, 2009 |
| A2076 | UF01106 | B. anthracis | Ames | A3b | Texas, white-tailed deer 2009 |
| A2006 | UF01096 | B. anthracis | Vollum | A4, A.Br.Vollum | Texas, white-tailed deer 2009 |
| A2064 | UF01063 | B. anthracis | WAG | Nigeria | |
| A2067 | UF01075 | B. anthracis | WAG | Nigeria | |
| UF01052 | B. anthracis | WAG | Nigeria | ||
| A0402 | UF00926 | B. anthracis | B.Br.CNEVA | France | |
| A0333 | UF00621 | B. anthracis | B.Br.CNEVA | Germany | |
| A0451 | UF00438 | B. anthracis | B.Br.001/002 | Mozambique | |
| A1088 | UF00910 | B. anthracis | B.Br.CNEVA | Poland | |
| A0104 | UF00839 | B. anthracis | B.Br.001/002 | South Africa | |
| A1055 | UF00603 | B. anthracis | C.Br.A1055 | USA | |
| A0530 | UF00878 | B. anthracis | A.Br.005/006 | Botswana | |
| A1202 | UF00049 | B. anthracis | Argentina | ||
| HHG80 | UF01135 | B. anthracis | Etosha Natl Park (ENP), Namibia | ||
| A1073 | UF00232 | B. anthracis | Chile | ||
| A1075 | UF00242 | B. anthracis | A.Br.003/004 | Chile | |
| Bc0001 | Bcbva | Côte d’Ivoire (Taï Natl Park) | |||
| Bc0002 | Bcbva | Côte d’Ivoire (Taï) | |||
| Bc0007 | Bcbva | Côte d’Ivoire (Taï) | |||
| Bc0009 | Bcbva | Côte d’Ivoire (Taï) | |||
| Bc0011 | Bcbva | Côte d’Ivoire (Taï) | |||
| B. cereus | FDA 5 | ||||
| B. cereus | Gibson 971 | ||||
| B. cereus | NRS 201 | ||||
| B. cereus | G9241 | ||||
| B. thuringiensis | Konkukian 97-27 | ||||
| B. thuringiensis | NRS 996 | ||||
| B. thuringiensis | AD-1 | ||||
| B. thuringiensis | HD-1 | ||||
| B. thuringiensis | Bt HD522 |
2.2. Multiplex qPCR Assays
Previous TaqMan assays for the detection of B. anthracis [21] were adapted to the QuantStudio 7 Flex (Applied Biosystems, Foster City, CA, USA) and the LightCycler 2.0 (Roche, Indianapolis, IN, USA) instruments. For Bcbva, we adapted the GI4 marker and tested with plasmid targets (capB and lef) from Blackburn et al. [21]. The QuantStudio 7 assay consisted of a four-dye reaction for simultaneous detection of the plasmid markers capB and lef, as well as the chromosomal markers Ba-1 and GI4, unique to B. anthracis and Bcbva, respectively. PCR was carried out in a 20-µL reaction using 1 µL of template, 1 × PrimeTime Gene Expression Master Mix (1055772, IDT, Coralville, IA, USA), and primers and probes as described in Table 2. Cycling conditions were as follows: 95 °C for 3 min, and 45 cycles of 95 °C for 20 s and 60 °C for 30 s.
Table 2.
Gene targets, primers and probes used in multiplex on the QuantStudio 7 * platform to detect B. anthracis and B. cereus biovar anthracis (Bcbva) using real-time PCR.
| Target | Oligo | Primer/Probe Sequence (5′–3′) | Final Concentration (nM) |
|---|---|---|---|
| Ba-1 | Forward | GTACATCTTCTAGCTGTTGCAA | 900 |
| Reverse | ACGTAGGAAGACCGTTGATTA | 900 | |
| Probe | VIC-CGTTGTTGTGTATTTG-MGB | 250 | |
| capB | Forward | TAAGCCTGCGTTCTTCGTAAATG | 600 |
| Reverse | GTTCCCAAATACGTAATGTTGATGAG | 600 | |
| Probe | NED-TTGCAGCGAATGAT-MGB | 300 | |
| lef | Forward | CACTATCAACACTGGAGCGATTCT | 600 |
| Reverse | AATTATGTCATCTTTCTTTGGCTCAA | 600 | |
| Probe | Cy5-AGCTGCAGATTCC-MGB | 250 | |
| GI4 | Forward | GGAGATATTAACAAGAGATGGATTGGA | 700 |
| Reverse | CAGTAGGCTTGTCTGCTCTAATAAAATT | 600 | |
| Probe | FAM-ACATGCCAGCGTTTTTTGCCTCTACACA-BHQ1 | 150 |
* QuantStudio 7 excitation filter wavelengths in nm: 470 ± 15, 520 ± 10, 549.5 ± 10, 580 ± 10, 640 ± 10; emission filter wavelengths: 520 ± 15, 558 ± 12, 586.5 ± 10, 623 ± 10, 682 ± 10, 662 ± 10.
On the LC2 platform, two separate duplex assays were designed for simultaneous detection of FAM- and VIC-labeled probes (Table 3). Duplex one contained primers and probes for detection of Ba-1 and GI4 markers, species detection markers. Duplex two was used for detection of virulence markers lef and capB found in pXO1 and pXO2 plasmids (or pXO1- and pXO2-like), respectively. PCR was similarly carried out in a 20-µL reaction using 1 µL of template, 1x PrimeTime Gene Expression Master Mix (1055772, IDT, Coralville, IA, USA), and primers and probes as described in Table 3. Spectral overlap between fluorescent channels from the LC2 instrument were corrected by performing color compensation experiments using FAM and VIC probes according to the manufacturer’s instructions. The resulting color compensation file was applied to data obtained from the LC2 duplex assays. Cycling conditions were as follows: 95 °C for 3 min, and 45 cycles of 95 °C for 20 s and 60 °C for 30 s.
Table 3.
Gene targets, primers and probes used in duplex PCR for the LightCycler 2.0 * platform to detect B. anthracis and Bcbva.
| Target | Oligo | Primer/Probe Sequence (5′–3′) | Final Concentration (nM) |
|
|---|---|---|---|---|
| Duplex 1 | Ba-1 | F-primer | GTACATCTTCTAGCTGTTGCAA | 600 |
| R-primer | ACGTAGGAAGACCGTTGATTA | 600 | ||
| Probe | VIC-CGTTGTTGTGTATTTG-MGB | 250 | ||
| GI4 | F-primer | GGAGATATTAACAAGAGATGGATTGGA | 700 | |
| R-primer | CAGTAGGCTTGTCTGCTCTAATAAAATT | 600 | ||
| Probe | FAM-ACATGCCAGCGTTTTTTGCCTCTACACA-BHQ1 | 600 | ||
| Duplex 2 | lef | F-primer | CACTATCAACACTGGAGCGATTCT | 400 |
| R-primer | AATTATGTCATCTTTCTTTGGCTCAA | 400 | ||
| Probe | VIC-AGCTGCAGATTCC-MGB | 250 | ||
| capB | F-primer | TAAGCCTGCGTTCTTCGTAAATG | 600 | |
| R-primer | GTTCCCAAATACGTAATGTTGATGAG | 600 | ||
| Probe | FAM-TTGCAGCGAATGAT-MGB | 250 |
* LightCycler 2.0 excitation by blue LED light source with maximum emission of 470 nm. Detection channels: 530, 560, 610, 640, 640, 705.
All assays were tested on all 26 B. anthracis strains using ~1.7 × 105 genome equivalents (GE) of DNA (~1 ng). In addition, DNA from Bcbva, Bacillus thuringiensis, and B. cereus were included to test for specificity.
2.3. Limit of Detection of Multiplex Assays
To establish sensitivities, 10-fold serial dilutions of B. anthracis Ames (UF01106) DNA and a plasmid carrying GI4 sequences were tested in triplicate. Specifically, Ames DNA was used to establish limit of detection for the Ba-1, lef, and capB markers. pXO1 and pXO2 plasmid concentrations were estimated in Ames by the absolute quantification method using Ba-1 chromosomal marker as reference. To establish the sensitivity of the Island 4 marker, pGI4, a plasmid carrying GI4 sequences from Bcbva, was used as positive control for this marker. Sensitivities were established for each marker in the Quantstudio7 multiplex assay and both LC2 duplex assays.
2.4. Whole Genome Sequencing of Bcbva Isolate
Nextera XT DNA Library Preparation Kit was used to prepare a Whole Genome Sequencing library of Bc0001. The sample was barcoded using dual indexing with Nextera XT Index Kit v2. The library was quantified with a Qubit 3.0. Paired end sequencing was performed on an Illumina MiSeq. Quality filtration was performed on the samples to trim sequencing adapters, low quality and unknown nucleotides using CLC Genomics Workbench 12.0.2 “Trim Sequences” module. The files were then taxonomically classified using CLC Genomics Workbench 12.0.2 “Taxonomic Profiling” module against an optimized reference Microbial Reference Genome Database (June 2019) with all available B. cereus reference sequences additionally included. Additionally, the assembled genome and selected reference Bacillus spp. genomes underwent whole genome single nucleotide polymorphism (SNP) alignment with RAxML phylogenetic inference and bootstrapping using the PhAME software suite developed at Los Alamos National Labs [28]. The sequencing data are available in NCBI with BioSample accession SAMN15804163.
3. Results
3.1. Level of Detection of Duplex and Multiplex Assays
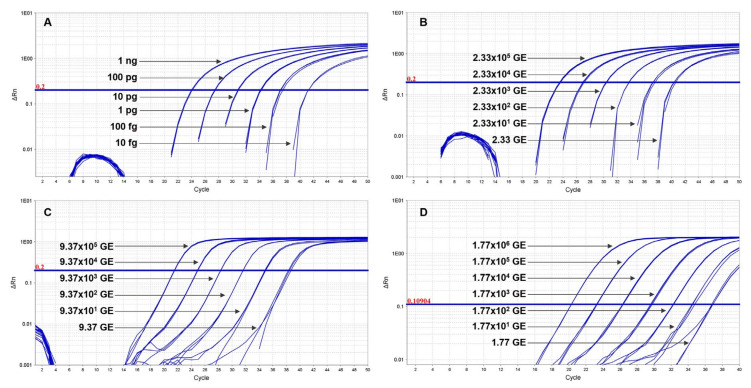
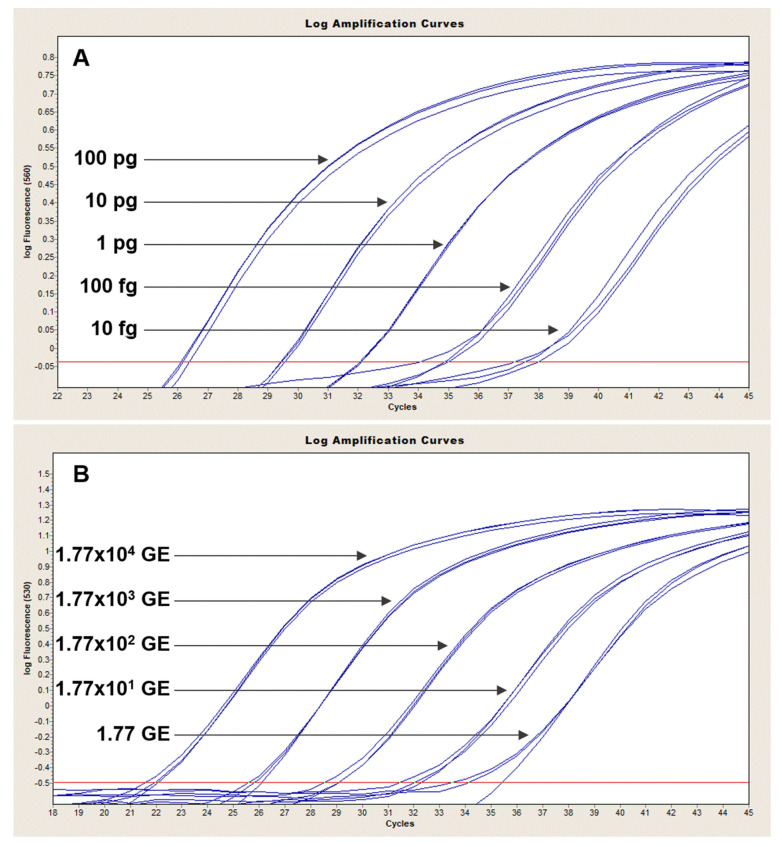
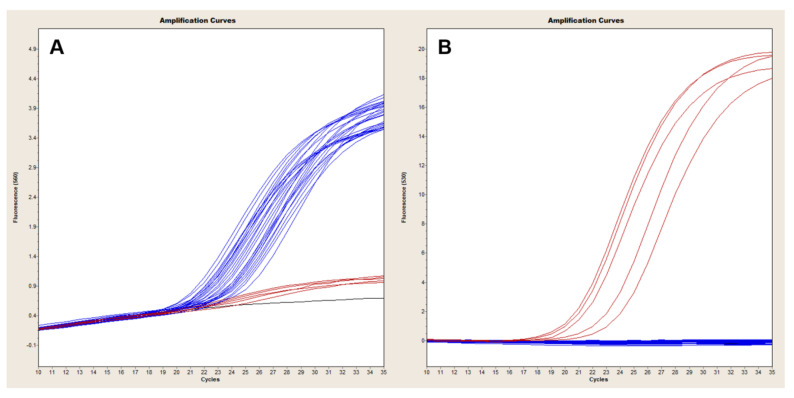
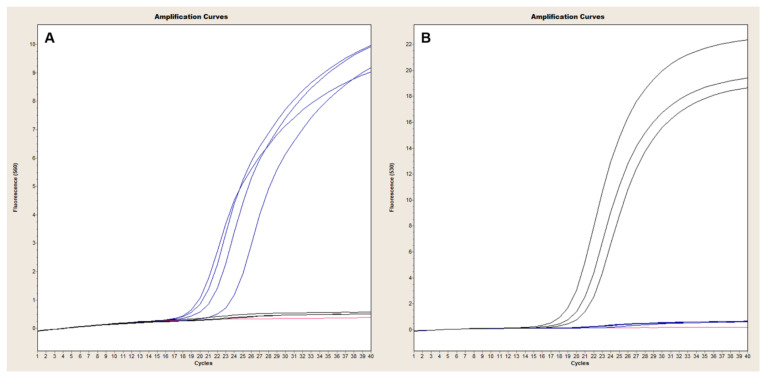
The Ba-1 marker displayed a limit of detection of 100 fg in both platforms with 10 fg-levels of DNA producing only sporadic amplification Figure 1A and Figure 2A). Similarly, the GI4 marker was reliably detected with 17.7 GE of pGI4 but not consistently at the 1.77 GE level (Figure 1D and Figure 2B). For the QuantStudio 7, capB and lef were consistently detected with ~2 and 9 GE of pXO2 and pXO1, respectively (Figure 1B,C), whereas reproducible detection on the LC2, necessitated at least ~2E1 and ~9E1 GE of pXO2 and pXO1, respectively (Figure 3A,B).
Figure 1.
Sensitivity of TaqMan multiplex in QuantStudio. Ten-fold serial dilutions of Ames (Panels (A), (B) and (C)) or control plasmid carrying GI4 from Bcbva (Panel (D)) were tested in triplicate to establish the limit of detection of each primer pair and corresponding probe. The B. anthracis genome specific marker Ba-1 was consistently detected at 100 fg of genomic DNA, with sporadic amplification at the 10-fg level (Panel (A)). capB (Panels B) and lef (Panels (C)) targets were detected with as little as ~2 and 9 GE of pXO2 and pXO1, respectively, but could not be amplified at a lower 10-fold dilution (Panels (B) and (C)). GI4 was reliably detected with at least 17.7 GE of pGI4 (Panel (D)). The standard curve plots displayed R2 and slopes values as follows: Ba-1, R2 = 1, slope = −3.3793; capB, R2 = 0.9986, slope = −3.3337; lef, R2 = 1, slope = −3.3519; GI4, R2 = 0.9996, slope = −3.1776.
Figure 2.
Sensitivity of TaqMan Ba-1-GI4 duplex in LightCycler 2.0. Ten-fold serial dilutions of Ames (Panel (A)) or control plasmid carrying GI4 from Bcbva (Panel (B)) were tested in triplicate to establish the limit of detection of B. anthracis Ba-1 and Bcbva GI4 chromosomal markers. Ba-1 displayed a sensitivity of 100 fg with inconsistent amplification at the 10-fg level (Panel (A)). About 17.7 copies of pGI4 were needed for reliable and reproducible amplification of GI4. The standard curve plots displayed R2 and slopes values as follows: Ba-1, R2 = 0.998, slope = −2.989; GI4, R2 = 0.9972, slope = −3.313.
Figure 3.
Sensitivity of TaqMan capB and lef duplex in LightCycler 2.0. Ten-fold serial dilutions of an Ames strain carrying pXO1 and pXO2 plasmids were tested in triplicate to establish the limit of detection of capB and lef markers. capB and lef were consistently detected with ~2 × 101 and ~9 × 101 GE of pXO2 (Panel (A)) and pXO1 (Panel (B)), respectively. The standard curve plots displayed R2 and slopes values as follows: capB, R2 = 0.976, slope = −3.4404; lef, R2 = 0.9594, slope = −3.486.
3.2. Four-Dye Multiplex in QuantStudio
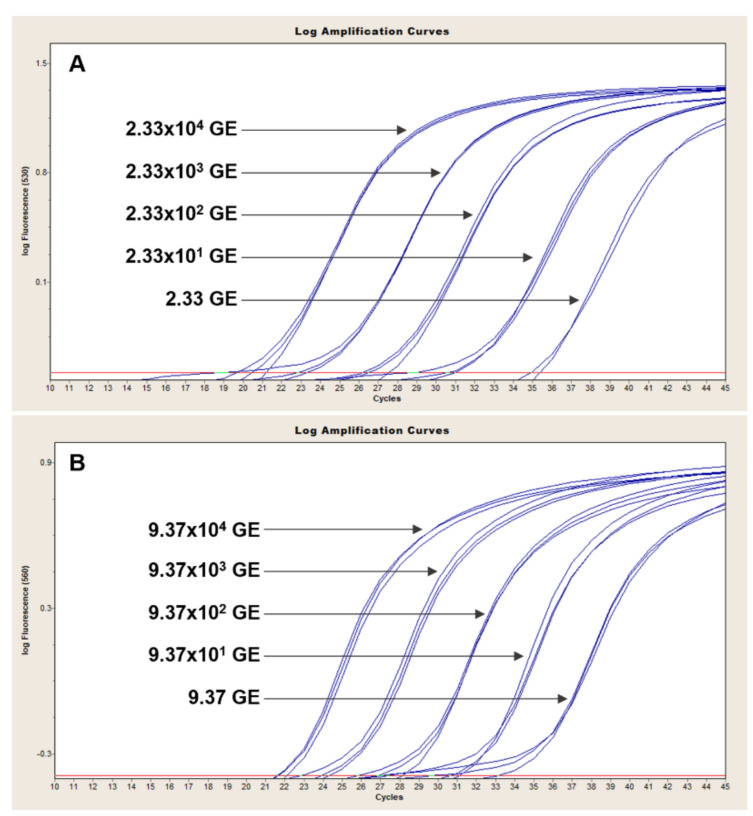
The QuantStudio 7 multiplex assay is based on the simultaneous detection of B. anthracis and Bcbva-specific markers. We validated our assay with 26 B. anthracis strains of known marker status (any of the three markers; 19/26 positive for all three), as well as five Bcbva strains and closely related representatives of the B. cereus group. All 19 B. anthracis isolates known to be positive for capB, lef and Ba-1 markers produced clear and reproducible amplification curves of all three markers (Figure 4A and Table 4). The GI4 marker was specific to Bcbva (Figure 4B) and was not amplified in any other strains tested (Table 4). The five different Bcbva isolates tested showed strong amplification of capB, lef and GI4 while failing to amplify the B. anthracis-specific Ba-1 marker (Figure 4B). The specificity of capB and lef assay was illustrated with capB- and lef- negative strains. Specifically, the four different B. anthracis capB negative strains tested produced strong lef and Ba-1 signals (Figure 4C) whereas only Ba-1 and capB were amplified in lef-negative strains (Figure 4D).
Figure 4.
Evaluation of 4-color qPCR assay in QuantStudio. A collection of B. anthracis strains previously known to carry pXO1 and pXO2 produced consistent amplification of Ba-1 (red), capB (black) and lef (blue) markers (Panel (A)). The GI4 marker (grey) was specifically amplified in Bcbva backgrounds (Panel (B)) that were also strongly positive for capB (black) and lef (blue). Panel (C) illustrates amplification of Ba-1 (red) and lef (blue) markers in capB-negative B. anthracis isolates. Conversely, lef-negative B. anthracis only amplified Ba-1 (red) and capB (black) markers (Panel (D)).
Table 4.
Evaluation of B. cereus sensu lato panel with LC2 and QuantStudio 7 TaqMan assays. Average cycle thresholds are shown.
| LightCycler 2.0 | QuantStudio 7 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Species | ID | Ba-1 | capB | lef | GI4 | Ba-1 | capB | lef | GI4 |
| Ba a Ames | UF00738 | 25.14 | 20.37 | 20.95 | Und. | 24.35 | 23.67 | 21.90 | Und. |
| Ba Vollum 1 | UF00980 | 24.69 | 32.12 | 32.45 | Und. | 25.85 | 37.52 | 36.08 | Und. |
| Ba Ames | UF01105 | 25.49 | 20.06 | 20.49 | Und. | 23.09 | 22.25 | 20.60 | Und. |
| Ba Ames | UF01106 | 26.17 | 20.46 | 20.89 | Und. | 24.69 | 23.73 | 21.92 | Und. |
| Ba Vollum (A4) | UF01096 | 25.36 | 20.68 | 20.73 | Und. | 24.55 | 23.84 | 21.83 | Und. |
| Ba WNA (A1.a) | UF01137 | 25.02 | 19.95 | 20.40 | Und. | 23.83 | 23.06 | 21.26 | Und. |
| Ba | UF00175 | 25.31 | 20.84 | 20.77 | Und. | 24.74 | 24.13 | 21.91 | Und. |
| Ba | UF01063 | 23.85 | 18.90 | 19.31 | Und. | 23.08 | 21.98 | 20.17 | Und. |
| Ba | UF01075 | 24.36 | 20.06 | 20.33 | Und. | 24.73 | 23.73 | 21.89 | Und. |
| Ba | UF01052 | 25.53 | 20.12 | 19.99 | Und. | 24.23 | 23.25 | 21.15 | Und. |
| Ba | UF00049 | 25.93 | 20.11 | 19.80 | Und. | 24.40 | 23.31 | 21.02 | Und. |
| Ba | UF01135 | 23.69 | 18.50 | 18.79 | Und. | 22.35 | 21.28 | 19.65 | Und. |
| Ba | UF00438 | 23.82 | 17.15 | 17.84 | Und. | 21.75 | 20.31 | 18.89 | Und. |
| Ba | UF00603 | 23.73 | 17.50 | 18.24 | Und. | 21.86 | 20.97 | 19.48 | Und. |
| Ba | UF00727 | 23.83 | 18.26 | 17.94 | Und. | 22.40 | 22.17 | 19.86 | Und. |
| Ba | UF00910 | 23.99 | 18.62 | 18.94 | Und. | 22.51 | 21.46 | 19.77 | Und. |
| Ba | UF00926 | 23.39 | 18.01 | 18.34 | Und. | 21.98 | 21.25 | 19.42 | Und. |
| Ba | UF00930 | 23.08 | 18.78 | 18.64 | Und. | 21.45 | 21.28 | 19.22 | Und. |
| Ba | UF00965 | 23.69 | 17.97 | 18.48 | Und. | 22.09 | 20.99 | 19.49 | Und. |
| Ba Sterne | UF01114 | 26.96 | Und. | 22.69 | Und. | 26.21 | Und. | 23.58 | Und. |
| Ba | UF00839 | 23.79 | Und. | 18.93 | Und. | 23.39 | Und. | 20.47 | Und. |
| Ba | UF00878 | 24.39 | Und. | 19.38 | Und. | 23.00 | Und. | 20.05 | Und. |
| Ba | UF00232 | 25.35 | Und. | 20.35 | Und. | 24.59 | Und. | 21.26 | Und. |
| Ba | UF00242 | 23.95 | 18.70 | Und. | Und. | 22.95 | 21.97 | Und. | Und. |
| Ba | UF00502 | 24.59 | 19.71 | Und. | Und. | 23.65 | 22.89 | Und. | Und. |
| Ba | UF00621 | 22.90 | 17.35 | Und. | Und. | 21.35 | 20.64 | Und. | Und. |
| Bcbva | Bc0001 | Und. | 19.33 | 20.01 | 21.22 | Und. | 20.75 | 19.50 | 20.16 |
| Bcbva | Bc0002 | Und. | 17.81 | 18.54 | 18.53 | Und. | 20.47 | 19.27 | 19.83 |
| Bcbva | Bc0007 | Und. | 17.56 | 18.39 | 17.60 | Und. | 20.36 | 19.12 | 19.56 |
| Bcbva | Bc0009 | Und. | 20.59 | 21.31 | 20.97 | Und. | 23.07 | 21.92 | 22.46 |
| Bcbva | Bc0011 | Und. | 17.91 | 18.74 | 18.90 | Und. | 20.92 | 19.77 | 20.14 |
| Bt b 97-27 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bt NRS 996 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bt AD-1 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bt HD-1 | Und. | Und. | 38.30 | Und. | Und. | Und. | 37.36 | Und. | |
| Bt HD522 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bc c FDA 5 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bc Gibson 971 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bc NRS 201 | Und. | Und. | Und. | Und. | Und. | Und. | Und. | Und. | |
| Bc G9241 | Und. | Und. | 20.12 | Und. | Und. | Und. | 16.22 | Und. | |
a Ba = Bacillus anthracis, b Bt = Bacillus thuringiensis, c Bc = Bacillus cereus. Und. = Undetermined, no amplification was detected.
3.3. Duplex Assays in LightCycler 2.0
The LightCycler assays are based on the detection of chromosomal B. anthracis and Bcbva markers in one reaction and detection of plasmid markers in a second duplex reaction. Ba-1 signal was readily detected in all B. anthracis isolates tested (Figure 5A) and was specific up to 35 cycles of amplification with sporadic late cycle amplification appearing in non-Ba-1 backgrounds thereafter. Conversely, GI4 signal was only observed in Bcbva (Figure 5B) with low background signal for this marker observed in non-Bcbva isolates (Figure 5A).
Figure 5.
Evaluation of Ba-1-GI4 duplex PCR in LightCycler 2.0. A collection of B. anthracis and Bcbva strains were evaluated with the Ba-1 and GI4 TaqMan duplex PCR using 1 ng of genomic DNA. All B. anthracis strains tested (blue, panel (A)) showed clear amplification with the Ba-1 marker in the 560 channel, which detects signal from the VIC-labeled Ba-1 probe. Conversely, signal from GI4 was only observed for Bcbva (red, panel (B)) in the 530 channel, which detects signal from the FAM-labeled GI4 probe.
In the duplex assay for detection of capB (530 nm channel) and lef (560 nm channel), capB-negative strains exhibited strong signal in the 560 nm channel (Figure 6A, blue signal), corresponding to amplification of lef, that was absent from the 530 nm channel (Figure 6B). Similarly, lef-negative isolates produced signal only in the 530 nm channel corresponding to amplification of capB (Figure 6B, black signal). Both markers were readily detected in B. anthracis and Bcbva carrying pXO1, pXO2 and pXO1-like and pXO2-like plasmids (Table 4).
Figure 6.
Evaluation of capB-lef duplex PCR in LightCycler 2.0. A collection of B. anthracis and Bcbva strains were evaluated with the capB and lef TaqMan duplex PCR using 1 ng of genomic DNA (Table 4). Amplification of lef in capB-negative B. anthracis strains is illustrated in Panel (A) (blue signal), with little to no lef background signal detected in isolates lacking pXO1 (Panel (A), black signal). Conversely, capB signal was readily detected in strains harboring pXO2 (Panel (B), black signal), but absent from capB-negative isolates (Panel (B), blue signal).
3.4. Specificity
To test specificity, various representatives of the B. cereus group were also tested in triplicate in both platforms. Ba-1, capB and GI4 markers, could not be detected in any these backgrounds (Table 4). The lef marker, however, produced reproducible late cycle amplification in B. thuringiensis serovar Kurstaki HD1. This strain carries a plasmid which displays 90% homology to pXO1 over an area that covers 16% of its sequence. lef was also strongly amplified in B. cereus G9241, which carries a pXO1-like plasmid harboring the genes for anthrax toxin subunits.
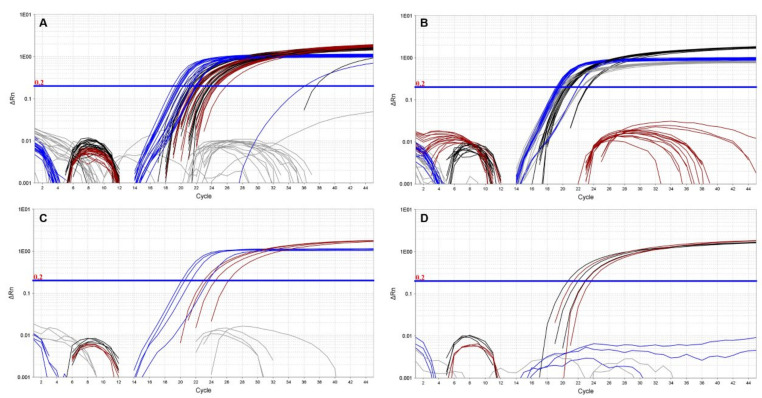
3.5. Whole Genome Sequencing of Bcbva Isolate Bc0001
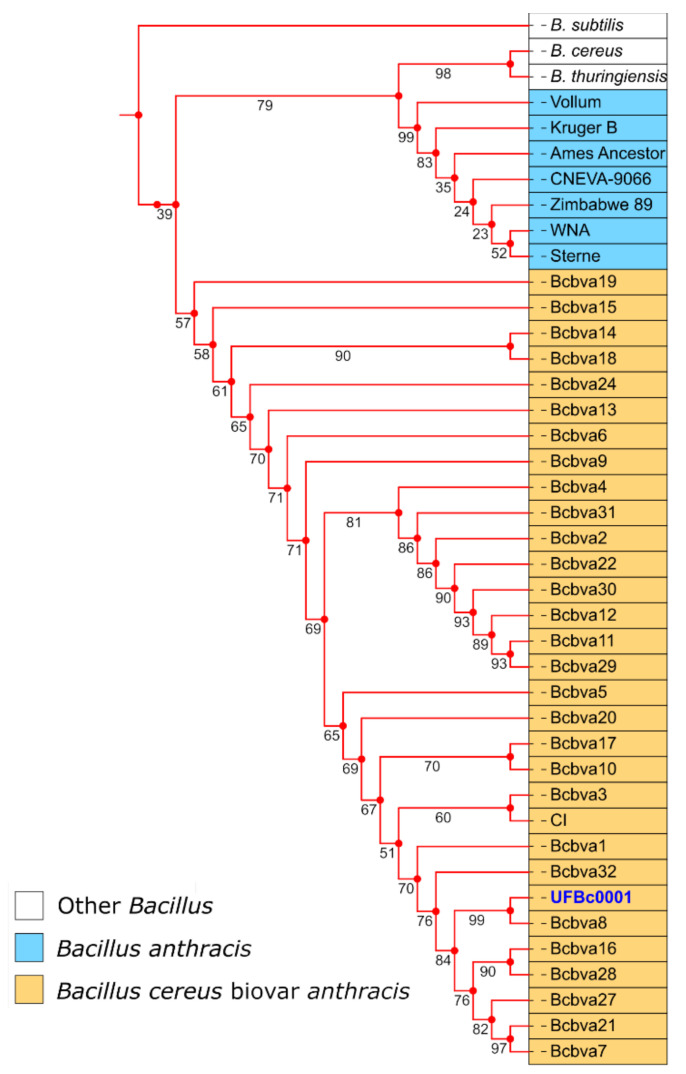
Although the goal of this study was to develop qPCR assays for simultaneous detection of B. anthracis and Bcbva, we undertook whole genome sequencing of one of the Bcbva strains isolated in our lab to provide further confirmation of its identity. Isolate Bc0001 was sequenced on the Illumina MiSeq platform (BioSample accession SAMN15804163) and differed from the Bcbva type strain in GenBank (BioSample accession SAMN02603256) by 65 SNPs. Bc0001 contigs aligned with 99.58% identity to the Bcbva CI genome. Analysis by PATRIC (Pathosystems Resource Integration Center) estimated a genome length of 5,295,704 bp, an average G+C content of 35.21%, and a total of 5,640 protein coding sequences for Bc0001. A phylogenetic tree was constructed using various other Bcbva isolates from Taï National Park (Cote d’Ivoire) that were recently sequenced [10], as well as other members of the Bacillus genus. As expected, Bc0001 is closely related to other Bcbva isolates from Taï National Park, Cote d’Ivoire (Figure 7).
Figure 7.
Phylogenetic tree illustrating relatedness of UFBc0001 (blue font) to Tai National Park isolates (orange boxes) and other members of the Bacillus genus (blue and white boxes) based on whole genome SNP alignments. Boot strapping values are shown on the tree branches.
4. Discussion
The aim of this work was to develop and optimize a diagnostic assay for accurate, simultaneous, and differential detection of B. anthracis, the causative agent of anthrax, and Bcbva, which causes anthrax-like disease in non-human primates, wildlife, livestock, and possibly humans. Limited diagnostics have likely hindered the detection of human Bcbva infections. To that end, we have developed a four-color multiplex assay that can be readily applicable across 4-plex hydrolysis probes platforms (e.g., QuantStudio 3–12, StratageMx4000, BioRad iCycler IQ, ABI7900HT, etc.), and a two-reaction two-color assay for the LC2 capillary based format, which is an aging but commonly used platform worldwide (LightCycler). The LC2 assay is also adaptable to any 2-plex hydrolysis probes platforms. Our four-dye multiplex assay simultaneously detects capB and lef plasmid markers shared by both B. anthracis and Bcbva, as well as chromosomal markers that are unique to each pathogen. The capillary based assay requires two different 2-color reactions for detection of plasmid markers in one and chromosomal markers in the other. Although GI4 and Ba-1 markers serve as the primary difference between B. anthracis and Bcbva, it was important for us to have an assay that could ascertain the plasmid status of the strain and thus pathogenicity.
The GI4 marker was highly specific to Bcbva and could not be detected in any of the B. cereus sensu lato strains tested even at 50 cycles of amplification. Using the QuantStudio 7 multiplex assay, Ba-1 was specific to B. anthracis and absent from all Bcbva, B. cereus, and B. thuringiensis tested, with sporadic late cycle amplification of marker occurring in the LC2 duplex assays after 35 cycles of amplification. Although we tested specificity of the capB and lef markers in non-B. anthracis B. cereus sensu lato, the existence of B. cereus isolates with toxin and/or cap genes have been previously reported in humans [29,30,31,32,33,34]. Indeed, our assay was able to quickly detect the presence of lef in a B. cereus G9241 background known to carry pXO1 (Average Ct = 16.22). Nonetheless, capsule and toxin markers were highly specific in B. anthracis yielding no amplification in strains lacking either capB or lef.
The TaqMan assays described in this work provide a rapid diagnostic tool for simultaneous detection of B. anthracis and Bcbva. Bcbva is an emerging pathogen that circulates in western and central Africa and a collective review of recent studies of both suggest overlap across much of the region [10,12,17,18,19,20,35]. Anthrax remains and important and underreported disease in this region and many of the classical microbiology techniques for differentiating B. anthracis from B. cereus do not work to differentiate Bcbva. Thus far reported in sylvatic animals, human impact is currently unknown. Bcbva is expected to be pathogenic in humans given that clinical manifestation in animals resemble classical anthrax. Recent work has identified serological tools that may further assist in human case detection [15]. Coupling those studies with these PCR assays in regional diagnostics labs could greatly improve our understanding of the epidemiology of anthrax (or anthrax like) disease caused by both pathogens. The Ba-1 and GI4 markers, thus far unique to B. anthracis and Bcbva respectively, are the basis for differentiation of these two pathogens in these qPCR assays. Aside from querying the organism specific genome markers, our assay can also establish the presence of lef and capB markers which are an integral part of the virulence machinery of B. anthracis and Bcbva.
Acknowledgments
Thanks to Huy Quang Nguyen and staff for interpretation support at NIHE. Skeletal material from Taï National Park was transported under the following permits: CITES export permits # 2352, 000704, 000705 and 001809.
Author Contributions
Conceptualization, D.Z., M.H.N. and J.K.B.; methodology: D.Z., M.H.N., G.G., K.K. and T.H.; investigation, D.Z., B.K., O.C., T.T.H.H., M.H.N., G.G., K.K. and J.K.B.; writing—original draft preparation, D.Z., M.H.N. and J.K.B.; writing: review and editing, D.Z., M.H.N., J.K.B., B.K., G.G., K.K., T.H., O.C., T.T.H.H., D.J.D. and J.K.; funding acquisition J.K.B., M.H.N., W.S.M., D.J.D. and J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially funded by the US Defense Threat Reduction Agency’s Biological Threat Reduction Program in Vietnam and HDTRA-12010003 to J.K. Blackburn, the US National Science Foundation (NSF #BCS--0921770, -0922429, -1440278 and -1440532.) to D.J. Daegling and W.S. McGraw, and the Bone Chemistry Lab, Department of Anthropology, University of Florida. We thank the Emerging Pathogens Institute at the University of Florida for additional support.
Conflicts of Interest
None of the investigators has any financial interest or financial conflict with the subject matter or materials discussed in this report.
Ethics Statement
All work in this study was approved by the Institutional Biosafety Committee at the University of Florida. All bacterial samples were available in the Martin E. Hugh-Jones Bacillus anthracis Collection.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Inglesby T.V., O’Toole T., Henderson D.A., Bartlett J.G., Ascher M.S., Eitzen E., Friedlander A.M., Gerberding J., Hauer J., Hughes J., et al. Anthrax as a Biological Weapon, 2002 Updated Recommendations for Management. JAMA. 2002;287:2236–2252. doi: 10.1001/jama.287.17.2236. [DOI] [PubMed] [Google Scholar]
- 2.Goel A.K. Anthrax: A Disease of Biowarfare and Public Health Importance. World J. Clin. Cases WJCC. 2015;3:20–33. doi: 10.12998/wjcc.v3.i1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamal S.M., Rashid A.K.M.M., Bakar M.A., Ahad M.A. Anthrax: An Update. Asian Pac. J. Trop. Biomed. 2011;1:496–501. doi: 10.1016/S2221-1691(11)60109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anthrax. [(accessed on 6 December 2019)]; Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/anthrax.
- 5.Hendricks K.A., Wright M.E., Shadomy S.V., Bradley J.S., Morrow M.G., Pavia A.T., Rubinstein E., Holty J.-E.C., Messonnier N.E., Smith T.L., et al. Centers for Disease Control and Prevention Expert Panel Meetings on Prevention and Treatment of Anthrax in Adults. Emerg. Infect. Dis. 2014;20 doi: 10.3201/eid2002.130687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leendertz F.H., Yumlu S., Pauli G., Boesch C., Couacy-Hymann E., Vigilant L., Junglen S., Schenk S., Ellerbrok H. A New Bacillus Anthracis Found in Wild Chimpanzees and a Gorilla from West and Central Africa. PLoS Pathog. 2006;2:e8. doi: 10.1371/journal.ppat.0020008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leendertz F.H., Lankester F., Guislain P., Néel C., Drori O., Dupain J., Speede S., Reed P., Wolfe N., Loul S., et al. Anthrax in Western and Central African Great Apes. Am. J. Primatol. 2006;68:928–933. doi: 10.1002/ajp.20298. [DOI] [PubMed] [Google Scholar]
- 8.Klee S.R., Ozel M., Appel B., Boesch C., Ellerbrok H., Jacob D., Holland G., Leendertz F.H., Pauli G., Grunow R., et al. Characterization of Bacillus Anthracis-like Bacteria Isolated from Wild Great Apes from Cote d’Ivoire and Cameroon. J. Bacteriol. 2006;188:5333–5344. doi: 10.1128/JB.00303-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zimmermann F., Köhler S.M., Nowak K., Dupke S., Barduhn A., Düx A., Lang A., De Nys H.M., Gogarten J.F., Grunow R., et al. Low Antibody Prevalence against Bacillus Cereus Biovar Anthracis in Taï National Park, Côte d’Ivoire, Indicates High Rate of Lethal Infections in Wildlife. PLoS Negl. Trop. Dis. 2017;11:e0005960. doi: 10.1371/journal.pntd.0005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann C., Zimmermann F., Biek R., Kuehl H., Nowak K., Mundry R., Agbor A., Angedakin S., Arandjelovic M., Blankenburg A., et al. Persistent Anthrax as a Major Driver of Wildlife Mortality in a Tropical Rainforest. Nature. 2017;548:82–86. doi: 10.1038/nature23309. [DOI] [PubMed] [Google Scholar]
- 11.Zohdy S., Schwartz T.S. Shoo Fly Don’t Bother Me: Flies Track Social Primates and Carry Viable Anthrax. Mol. Ecol. 2019;28:4135–4137. doi: 10.1111/mec.15215. [DOI] [PubMed] [Google Scholar]
- 12.Antonation K.S., Grützmacher K., Dupke S., Mabon P., Zimmermann F., Lankester F., Peller T., Feistner A., Todd A., Herbinger I., et al. Bacillus Cereus Biovar Anthracis Causing Anthrax in Sub-Saharan Africa-Chromosomal Monophyly and Broad Geographic Distribution. PLoS Negl. Trop. Dis. 2016;10:e0004923. doi: 10.1371/journal.pntd.0004923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klee S.R., Brzuszkiewicz E.B., Nattermann H., Brüggemann H., Dupke S., Wollherr A., Franz T., Pauli G., Appel B., Liebl W., et al. The Genome of a Bacillus Isolate Causing Anthrax in Chimpanzees Combines Chromosomal Properties of B. Cereus with B. Anthracis Virulence Plasmids. PLoS ONE. 2010;5:e10986. doi: 10.1371/journal.pone.0010986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dupke S., Schubert G., Beudjé F., Barduhn A., Pauly M., Couacy-Hymann E., Grunow R., Akoua-Koffi C., Leendertz F.H., Klee S.R. Serological Evidence for Human Exposure to Bacillus Cereus Biovar Anthracis in the Villages around Taï National Park, Côte d’Ivoire. PLoS Negl. Trop. Dis. 2020;14:e0008292. doi: 10.1371/journal.pntd.0008292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dupke S., Barduhn A., Franz T., Leendertz F.H., Couacy-Hymann E., Grunow R., Klee S.R. Analysis of a Newly Discovered Antigen of Bacillus Cereus Biovar Anthracis for Its Suitability in Specific Serological Antibody Testing. J. Appl. Microbiol. 2019;126:311–323. doi: 10.1111/jam.14114. [DOI] [PubMed] [Google Scholar]
- 16.Carlson C.J., Kracalik I.T., Ross N., Alexander K.A., Hugh-Jones M.E., Fegan M., Elkin B.T., Epp T., Shury T.K., Zhang W., et al. The Global Distribution of Bacillus Anthracis and Associated Anthrax Risk to Humans, Livestock and Wildlife. Nat. Microbiol. 2019;4:1337–1343. doi: 10.1038/s41564-019-0435-4. [DOI] [PubMed] [Google Scholar]
- 17.Blackburn J.K., Odugbo M.O., Van Ert M., O’Shea B., Mullins J., Perreten V., Perrenten V., Maho A., Hugh-Jones M., Hadfield T. Bacillus Anthracis Diversity and Geographic Potential across Nigeria, Cameroon and Chad: Further Support of a Novel West African Lineage. PLoS Negl. Trop. Dis. 2015;9:e0003931. doi: 10.1371/journal.pntd.0003931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kracalik I.T., Kenu E., Ayamdooh E.N., Allegye-Cudjoe E., Polkuu P.N., Frimpong J.A., Nyarko K.M., Bower W.A., Traxler R., Blackburn J.K. Modeling the Environmental Suitability of Anthrax in Ghana and Estimating Populations at Risk: Implications for Vaccination and Control. PLoS Negl. Trop. Dis. 2017;11:e0005885. doi: 10.1371/journal.pntd.0005885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilo P., Rossano A., Bamamga H., Abdoulkadiri S., Perreten V., Frey J. Bovine Bacillus Anthracis in Cameroon. Appl. Environ. Microbiol. 2011;77:5818–5821. doi: 10.1128/AEM.00074-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romero-Alvarez D., Peterson A.T., Salzer J.S., Pittiglio C., Shadomy S., Traxler R., Vieira A.R., Bower W.A., Walke H., Campbell L.P. Potential Distributions of Bacillus Anthracis and Bacillus CereusBiovar Anthracis Causing Anthrax in Africa. PLoS Negl. Trop. Dis. 2020;14:e0008131. doi: 10.1371/journal.pntd.0008131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blackburn J.K., Van Ert M., Mullins J.C., Hadfield T.L., Hugh-Jones M.E. The Necrophagous Fly Anthrax Transmission Pathway: Empirical and Genetic Evidence from Wildlife Epizootics. Vector Borne Zoonotic Dis. Larchmt. N. 2014;14:576–583. doi: 10.1089/vbz.2013.1538. [DOI] [PubMed] [Google Scholar]
- 22.Van Ert M.N., Easterday W.R., Huynh L.Y., Okinaka R.T., Hugh-Jones M.E., Ravel J., Zanecki S.R., Pearson T., Simonson T.S., U’Ren J.M., et al. Global Genetic Population Structure of Bacillus Anthracis. PLoS ONE. 2007;2:e461. doi: 10.1371/journal.pone.0000461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leiser O.P., Blackburn J.K., Hadfield T.L., Kreuzer H.W., Wunschel D.S., Bruckner-Lea C.J. Laboratory Strains of Bacillus Anthracis Exhibit Pervasive Alteration in Expression of Proteins Related to Sporulation under Laboratory Conditions Relative to Genetically Related Wild Strains. PLoS ONE. 2018;13:e0209120. doi: 10.1371/journal.pone.0209120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Norris M.H., Zincke D., Leiser O.P., Kreuzer H.W., Hadfield T., Blackburn J.K. Laboratory Strains of Bacillus Anthracis Lose Their Ability to Rapidly Grow and Sporulate Compared to Wildlife Outbreak Strains. PLoS ONE. 2020;15:e0228270. doi: 10.1371/journal.pone.0228270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sahl J.W., Pearson T., Okinaka R., Schupp J.M., Gillece J.D., Heaton H., Birdsell D., Hepp C., Fofanov V., Noseda R., et al. A Bacillus Anthracis Genome Sequence from the Sverdlovsk 1979 Autopsy Specimens. mBio. 2016;7 doi: 10.1128/mBio.01501-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marston C.K., Allen C.A., Beaudry J., Price E.P., Wolken S.R., Pearson T., Keim P., Hoffmaster A.R. Molecular Epidemiology of Anthrax Cases Associated with Recreational Use of Animal Hides and Yarn in the United States. PLoS ONE. 2011;6:e28274. doi: 10.1371/journal.pone.0028274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Derzelle S., Aguilar-Bultet L., Frey J. Comparative Genomics of Bacillus Anthracis from the Wool Industry Highlights Polymorphisms of Lineage A.Br.Vollum. Infect. Genet. Evol. 2016;46:50–58. doi: 10.1016/j.meegid.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 28.Shakya M., Ahmed S.A., Davenport K.W., Flynn M.C., Lo C.-C., Chain P.S.G. Standardized Phylogenetic and Molecular Evolutionary Analysis Applied to Species across the Microbial Tree of Life. Sci. Rep. 2020;10:1723. doi: 10.1038/s41598-020-58356-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoffmaster A.R., Ravel J., Rasko D.A., Chapman G.D., Chute M.D., Marston C.K., De B.K., Sacchi C.T., Fitzgerald C., Mayer L.W., et al. Identification of Anthrax Toxin Genes in a Bacillus Cereus Associated with an Illness Resembling Inhalation Anthrax. Proc. Natl. Acad. Sci. USA. 2004;101:8449–8454. doi: 10.1073/pnas.0402414101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoffmaster A.R., Hill K.K., Gee J.E., Marston C.K., De B.K., Popovic T., Sue D., Wilkins P.P., Avashia S.B., Drumgoole R., et al. Characterization of Bacillus Cereus Isolates Associated with Fatal Pneumonias: Strains Are Closely Related to Bacillus Anthracis and Harbor B. Anthracis Virulence Genes. J. Clin. Microbiol. 2006;44:3352–3360. doi: 10.1128/JCM.00561-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Avashia S.B., Riggins W.S., Lindley C., Hoffmaster A., Drumgoole R., Nekomoto T., Jackson P.J., Hill K.K., Williams K., Lehman L., et al. Fatal Pneumonia among Metalworkers Due to Inhalation Exposure to Bacillus Cereus Containing Bacillus Anthracis Toxin Genes. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007;44:414–416. doi: 10.1086/510429. [DOI] [PubMed] [Google Scholar]
- 32.Marston C.K., Ibrahim H., Lee P., Churchwell G., Gumke M., Stanek D., Gee J.E., Boyer A.E., Gallegos-Candela M., Barr J.R., et al. Anthrax Toxin-Expressing Bacillus Cereus Isolated from an Anthrax-like Eschar. PLoS ONE. 2016;11:e0156987. doi: 10.1371/journal.pone.0156987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cachat E., Barker M., Read T.D., Priest F.G. A Bacillus Thuringiensis Strain Producing a Polyglutamate Capsule Resembling That of Bacillus Anthracis. FEMS Microbiol. Lett. 2008;285:220–226. doi: 10.1111/j.1574-6968.2008.01231.x. [DOI] [PubMed] [Google Scholar]
- 34.Wright A.M., Beres S.B., Consamus E.N., Long S.W., Flores A.R., Barrios R., Richter G.S., Oh S.-Y., Garufi G., Maier H., et al. Rapidly Progressive, Fatal, Inhalation Anthrax-like Infection in a Human: Case Report, Pathogen Genome Sequencing, Pathology, and Coordinated Response. Arch. Pathol. Lab. Med. 2011;135:1447–1459. doi: 10.5858/2011-0362-SAIR.1. [DOI] [PubMed] [Google Scholar]
- 35.Tamborrini M., Bauer M., Bolz M., Maho A., Oberli M.A., Werz D.B., Schelling E., Zinsstag J., Seeberger P.H., Frey J., et al. Identification of an African Bacillus Anthracis Lineage That Lacks Expression of the Spore Surface-Associated Anthrose-Containing Oligosaccharide. J. Bacteriol. 2011;193:3506–3511. doi: 10.1128/JB.00078-11. [DOI] [PMC free article] [PubMed] [Google Scholar]