Abstract
The foundation of controlling hypertension is adherence to antihypertensive medication adherence. This systematic review and meta-analysis aimed to assess the magnitude and associated factors of adherence to antihypertensive medication among adult hypertensive patients in Ethiopia. A comprehensible bibliographic searching was conducted from PubMed, EMBASE, Scopus, and Web of Science core collection. All published and unpublished studies that had been accessible before 31 May 2020, and written in English were eligible. Joanna Briggs Institute assessment tool was used to evaluate the quality of the findings of the included studies. Stata software 16.0 was used to analyze the data. Study-specific estimates were pooled to determine the overall prevalence estimate across studies using a random-effects meta-analysis model. Publication bias and heterogeneity were checked. Fourteen studies with a total of 4938 hypertensive patients were included in the final systematic review and meta-analysis. The pooled prevalence of medication adherence among hypertensive patients in Ethiopia was 65.41% (95% confidence interval: 58.91–71.91). Sub-group analysis shown that the pooled prevalence of medication adherence was the highest (69.07%, 95% confidence interval: 57.83–80.31, I2 = 93.51) among studies using questionnaire technique whereas the lowest in Morisky Medication Adherence Scale eight-items (60.66%, 95% confidence interval: 48.92–72.40, I2 = 97.16). Moreover, medication adherence was associated with the presence of comorbidities (pooled odds ratio = 0.23, 95% confidence interval: 0.07–0.38, p = 0.030, I2 = 54.9%) and knowledge about the disease and its management (pooled odds ratio = 2.98, 95% confidence interval: 1.72–4.24, p = 0.04, I2 = 55.55%) but not with place of residence (pooled odds ratio = 1.22, 95% confidence interval: 0.51–1.93, p = 0.00, I2 = 76.9%). Despite a lack of uniformity among included studies, adherence to antihypertensive medication among the hypertensive population in Ethiopia was moderate. The presence of comorbidities and/or complications reduced the odds of adherence whereas having good knowledge about the disease increased chance of medication adherence among hypertensive patients.
Keywords: Adherence, antihypertensive medication, hypertension, Ethiopia
Introduction
Hypertension (raised or elevated blood pressure (BP)) is defined as “systolic BP equal to or above 140 mm Hg and/or diastolic BP equal to or above 90 mm Hg.”1,2 It is a serious global public health problem that attributes to heart, brain and kidney diseases, and leads to heart attacks and strokes.1–3 Hypertension is considered as the leading cardiovascular risk factor as well as the principal attributing factor for global deaths.1 Moreover, it is also a major cause of premature death worldwide.3
Globally, hypertension affects about 1.13 billion people, and two-thirds of them are living in low- and middle-income countries.2,3 Every year, hypertension kills about 9 million people worldwide.2 The prevalence of hypertension is significant increasing in Sub-Saharan Africa (SSA) over the past two to three decades. The number of adults with hypertension in SSA was approximately 80 million in 2000 and it is projected that 150 million will have hypertension by 2025.4 Based on a systematic review (SR), the prevalence of hypertension in SSA ranged from 14.7% to 69.9% with the pooled prevalence of 30% (95% confidence interval (CI): 27%–34%).5
The exact prevalence of hypertension in Ethiopia is not known. Based on a study conducted among federal ministry civil servants, the prevalence of hypertension was 27.3% (95% CI: 23.3%–31%).6 In addition, a community-based study showed that the prevalence of hypertension among adults in Eastern Ethiopia was 24.43% (95% CI: 21.57–27.28). This study also stated that 51.64% adult hypertensive patients did not know their disease status.7
A multifactorial approach which requires to manage patients with hypertension can classified into pharmacological therapy and lifestyle modifications. The main components of lifestyle modification are sodium restriction (diet), exercise, moderation of alcohol consumption, smoking cessation, and weight control.8 Antihypertensive medication adherence is the foundation for attaining hypertension control and the reduction of its complications.8,9 One of the growing global health concerns is non-adherence to pharmacological therapy which creates a major obstacle to safe, cost-effective, and effective use of drugs.10,11 A comprehensive meta-analysis (MA) indicated that nearly half (45.2%) of hypertensive patients did not adhere to their antihypertensive medication and 83.7% of patients had uncontrolled BP.12 In developing countries, the prevalence of medication non-adherence among the hypertensive population ranged from 23% to 67.6% with the mean being 47.34%.13
Medication adherence or compliance refers “to the act of conforming to the recommendations made by the provider with respect to timing, dosage, and frequency of medication taking.” It can be defined as “the extent to which a patient acts in accordance with the prescribed interval and dose of a dosing regimen.” Adherence is measured over a period of time and reported as a percentage.8,14,15 Multiple factors are playing a significant role in determining the level of adherence to medication among hypertensive patients. These factors can be grouped into a five main domains such as socioeconomic factors, healthcare service–related factors, disease-related factors, therapy-related factors, and patient-related factors.10,13
Since the nature and character of adherence and its associated factors are very complex, a complete understanding is required in order to develop interventional strategies aimed at the improvement of medication adherence. This kind of compressive national information can be obtained by doing a SR and MA. However, there is no SR of the prevalence and factors associated with adherence to antihypertensive medication in Ethiopia. Therefore, the aim of this SR and MA was to determine the overall adherence to antihypertensive medication and the factors associated with medication adherence among adult’s hypertensive patients in Ethiopia.
Methods
Information sources and searching strategies
This SR and MA was registered in PROSPERO with registration number CRD42020159353. A comprehensible bibliographic searching was conducted to identify relevant published research works on the adherence to antihypertensive medications and associated factors among hypertensive patients in Ethiopia. The relevant studies were searched from the databases of PubMed, Excerpta Medica Database (EMBASE), Scopus, and Web of Science Core collection until 31 May 2020. In addition, a manual search was performed to retrieve unpublished studies and gray literature via Google Scholar and other sources like repositories of Ethiopian public universities. After the potential abstracts of the study were reviewed, their full texts were retrieved. In addition, the reference lists of the identified studies were also examined to identify other relevant articles not captured during our search. The search was done using the following search keywords and medical subject headings (MeSH): “adherence,” “compliance,” “Non-adherence,” “associated factors,” “anti-hypertensive medications,” “anti-hypertensive drugs,” “anti-hypertensive agents,” “Hypertension,” and “Ethiopia.”
Eligibility criteria
The included studies were observational studies (cross-sectional, case–control, and cohort studies) that reported the prevalence and factors associated with adherence to antihypertensive medication among adult hypertensive patients in Ethiopia. All published and unpublished studies that had been accessible before 31 May 2020, and written in English were eligible. The excluded studies were studies with poor quality, letters to the editor, reviews, commentaries, editorials, and case series/reports. Moreover, duplicate studies and studies with incomplete data were also excluded. When duplicate studies were encountered, the most comprehensive and/or recent study with the largest sample size was considered.
Description of the outcomes
The outcome variables were adherence and factors associated with adherence to antihypertensive medication. Adherence to antihypertensive medication was defined as “the extent to which a patient acts in accordance with the prescribed interval and dose of a dosing regimen.”8,14,15 If the included study reported the adjusted odds ratios (AORs) of being non-adherent, we transformed them into AORs of adherence using 1/AOR formula.
The selection process of studies
All search articles were exported to the EndNote X9 citation manager and duplicated studies were excluded. In order to guide the study selection process, the first tool was developed according to eligibility criteria. Then, studies were screened through by careful reading of the title and abstract.
The three authors (L.D.R., B.S.T., and A.B.W.) screened and evaluated studies independently. Studies that mentioned the outcome of the review (antihypertensive medication adherence) in their titles and abstracts were further evaluated. Then, the full text of the studies was further evaluated based on objectives, methods, participants/population, and key findings. The three authors (L.D.R., B.S.T., and A.B.W.) independently evaluated the quality of the studies against the checklist. The authors compared their results in each step of the selection process. Any discrepancy was resolved through discussion or through asking a fourth reviewer (B.T.M.) if consensus could not be reached. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement flow diagram is used to present the overall study selection process.
Critical appraisal of studies
Joanna Briggs Institute (JBI)16 quality assessment tool for observational studies was used to assess the overall quality of the findings of the included studies. The quality of the study was evaluated by three authors (L.D.R., B.S.T., and A.B.W.) independently using the checklist. Then, based on their point, the studies were categorized as high (score above 80%), moderate (between 60% and 80%), and low (below 60%) quality. The minimum point to be included into the SR was greater than or equal to 60%. The main reason of critically appraising these studies was to assess the internal validity (systematic error) and external validity (generalizability) of studies and to reduce the risk of biases.
Data extraction and recording
The two investigators (A.T.G. and N.L.) extracted the data independently using a data extraction template from the included studies. The extracted items were the last name of the first author, year of the study conducted and published, study design, study setting (rural vs urban), study type (community-based vs hospital-based), the method used to assess medication adherence (self-report (using tools such as Brief Medication Questionnaire, Eight-Item Morisky Medication Adherence Scale (MMAS), and Medication Adherence Report Scale), or pill count, electronic monitoring, pharmacy records, prescription claims, and biological assay), data collection techniques (face-to-face interview vs self-administered), sample size, the total number of cases adherent to antihypertensive medication, mean or median doses taken, mean or median age and age range in years, and the male proportion in the respective studies will also be obtained. In addition, the measure of association (odds ratio (OR) or relative risk with their respective CIs) for each associated factor was extracted and specification made if obtained from a bivariate or multivariate analysis. The accuracy of the data extraction was verified by comparing the results with the data extraction by the remaining three investigators (L.D.R., B.S.T., and A.B.W.), who independently extracted the data in a randomly selected subset of papers (30% of the total).
Risk of bias
Two authors (A.T.G. and B.S.T.) independently screened and evaluated studies using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement checklist.17 Visual inspection of the funnel plot was used to explore the publication bias. Besides, Egger’s regression test was carried out to check the symmetry of the funnel plot.
Statistical analysis
The raw numerical data from each study were extracted and recorded on a Microsoft Word, and then exported to an Excel Spreadsheet. Stata software 16.0 was used to analyze the extracted data. An MA of observational studies was conducted, based on recommendations made by Higgins and Thompson18 The pooled prevalence of adherence to antihypertensive medications was determined using an MA of the findings from similar studies. Study-specific estimates were pooled to determine the overall prevalence estimate across studies using a random-effects MA model.
Heterogeneity between the included studies was examined using the I2 statistic.18 I2 values of 25%, 50%, and 75% represented low, medium, and substantial heterogeneity, respectively. Therefore, the presence of heterogeneity between studies was assumed if the I2 statistic is greater than 75%. The source of heterogeneity among the include studies was verified using sensitivity analysis, sub-group analyses, and meta-regressions. Sub-group analysis was performed in case of substantial clinical and/or methodological heterogeneity using selected variables. A difference between sub-groups was considered significant if the p-value is below 5%. Finally, funnel plots and Egger’s test were used to assess the presence of publication bias. The presence of publication bias was confirmed using a p-value < 10% on Egger’s test.
Presentation and reporting of results
The entire process of study screening, selection, and inclusion was depicted with the aid of a flow diagram using the PRISMA guidelines. The PRISMA checklist was also published alongside the final review. First, a narrative synthesis was written to present the main findings of the included studies. Study descriptions and summary (author-year, country, aim, design and population, sample size, and key findings) were compiled using the Microsoft Word. The prevalence of adherence to antihypertensive medication was reported according to the selected variables. In addition, tables and narrative summaries were used to report the risk of bias for every eligible study. Moreover, available data on the identified factors associated with adherence to antihypertensive medication were summarized in tabular form accompanied by a narrative discussion.
Results
Selection of the studies
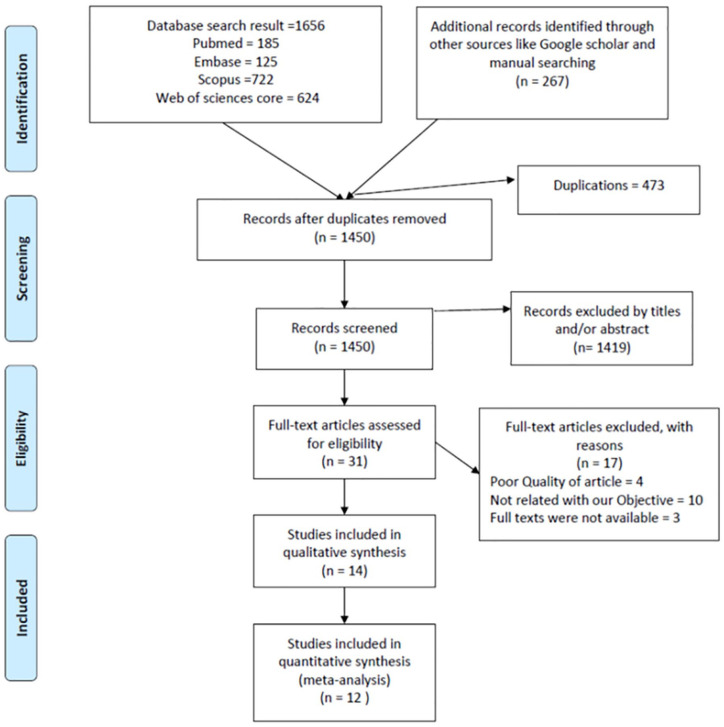
A total of 1923 articles were screened from the five scientific databases (PubMed = 185, Scopus = 722, EMBASE = 125, Web of Science Core = 624, and Google Scholar = 267) of which 473 duplicate articles were excluded. The titles and abstracts of 1450 articles were reviewed according to the inclusion criteria and 1419 articles were not related to the topic and were excluded. The full-text papers of 31 articles were retrieved and reviewed for inclusion which resulted in a total of 18 studies eligible for the methodological quality assessment. After excluding four studies with reasons mainly a weak quality score, 14 studies were included in the final SR (qualitative synthesis)19–32 and 12 of them were also included in MA (Figure 1).
Figure 1.
PRISMA flow diagram of selecting and including studies in systematic review and meta-analysis of adherence to antihypertensive medications and associated factors among hypertensive patients in Ethiopia.
Baseline characteristics of studies
The selected studies were published between 2012 and 2019. Regarding the geographical part of the country, one study was conducted in the north,19 four studies were in the northwest,20,27,30,31 one study was in the northeast,24 three studies were in the central,26,29,32 two studies were in the western,22,23 one study was in the southern,28 and two studies were in the southwest.21,25
Except for the study in Hawassa28 which was an unmatched case–control study, all other studies were hospital-based cross-sectional quantitative in type. Except for the study in Adama,29 the source population were adult hypertensive patients on antihypertensive medication for at least 1 month. But all hypertensive patients on antihypertension medication were included in the Adama study. The sample size of studies was ranged from 10024 to 160028 subjects, and the total sample sizes included for this review were 4938. Systematic random sampling was the main sampling technique which was used by six studies,20,26,28–30,32, while six studies were included all adult hypertensive patients visiting the chronic follow-up clinic during data collection.19,21,22,24,25,27
Face-to-face interviews with chart review were the main data collection technique used by eight studies19–21,23,25,26,28,30 while five studies22,24,29,31,32 used interview (non-specific) technique and only one study27 used self-administered questionnaires to assess adherence. The overview of the baseline characteristics of the 14 studies are presented in Table 1 (author, region, publication year, study design, study population, sample size, sampling technique, and data collection methods).
Table 1.
The baseline characteristics of the primary studies included in systematic review and meta-analysis on adherence to antihypertensive medications and associated factors among hypertensive patients in Ethiopia, 2020.
| Authors | Study area | Geographical region | Publication year | Study design | Study population (hypertensive patients who were) | Sample size | Sampling technique | Data collection technique |
|---|---|---|---|---|---|---|---|---|
| Ali et al.19 | Northern Ethiopia | Northern | 2014 | Prospective cross-sectional study | Adults and on anti HPT med for at least 6 months | 121 | All (convenient) | Face-to-face interview with document review |
| Ambaw et al.20 | Gondar | Northwest | 2012 | Institution-based cross-sectional study | Aged ⩾18 years and on anti-HPT med | 384 | Systematic random sampling technique | Face-to-face interview with document review |
| Asgedom et al.21 | JUSH | Southwest | 2018 | Cross-sectional study | Aged ⩾18 years on anti-HPT med for at least 12 months | 280 | All (convenient) | Face-to-face interview with document review |
| Bekele22 | Gimbi | Western | 2019 | A hospital-based cross-sectional study | Aged ⩾15 years attending medical OPD (all patients) | 127 | A convenience sampling | Interview |
| Berisa and Dedefo23 | Nedjo | Western | 2018 | Cross-sectional study | Aged ⩾18 years on anti-HPT med for at least 12 months | 172 | Consecutive sampling technique | Face-to-face interview with document review |
| Chelkeba and Dessie24 | Dessie | Northeast | 2013 | Cross-sectional convenient study | Aged ⩾18 years and on anti-HPT med for at least 3 months | 100 | All | Interview (not clearly described) |
| Dego and Bobasa25 | Jimma town | Southwest | 2016 | Prospective cross-sectional | Aged ⩾18 years without any comorbidity and on an anti-HPN drug, for at least 3 months | 120 | All non-comorbid HPT patients | Face-to-face interview with document review |
| Demisew et al.26 | Debre Berhan | Central | 2018 | Cross-sectional study | On anti-HPN drugs follow-up at least 6 months | 270 | Systematic random sampling method | Face-to-face interview |
| Gebreyohannes et al.27 | UoG | Northwest | 2019 | Institution-based cross-sectional study | Aged ⩾18 years and on anti-HPT med for at least 3 months | 249 | All (convenient) | Self-administered and chart review |
| Getenet et al.28 | Hawassa | Southern | 2019 | Institution-based unmatched case–control study | Aged ⩾18 years on anti-HPT treatment at least 1 month | 1600* | Systematic random sampling | Face-to-face interview |
| Hareri et al.29 | Adama | Central | 2014 | Facility-based cross-sectional study | Adult on anti-HPN medication (all patients) | 365 | Systematic sampling method | Interview |
| Mekonnen et al.30 | Northwest | Northwest | 2017 | An institution-based cross-sectional quantitative study | Aged ⩾18 years and on anti-HPN drugs for at least for a month | 409 | Systematic random sampling | Face-to-face interview with document review |
| Teshome et al.31 | Debre Tabor | Northwest | 2017 | Hospital-based cross-sectional study | Aged ⩾18 years and on anti-HPT med for at least 3 months | 337 | Simple random sampling | Interviewer-administered questionnaire with document review |
| Tibebu et al.32 | Addis Ababa | Central | 2017 | Institutional-based cross-sectional study | Aged ⩾18 years and on anti-HPT med for at least 6 months | 404 | Systematic random sampling | Interviewer-administered questionnaire with document review |
HPN: hypertension; anti-HPT: antihypertensive; JUSH: Jimma University Specialized Hospital; UoG: University of Gondar; OPD: out-patient department.
This sample size was used to assess the overall adherence level of all patients in the Hawassa Referral Hospital (HRH) by conducting a hospital-based census. Then based on this finding, cases and controls were identified. The sample size for the case–control study was 289 (96 cases and 193 controls).
Reported adherence to antihypertensive treatment
Methods of assessing adherence
The aim of eight studies was to assess the magnitude of adherence to antihypertensive medication and associated factors among hypertensive patients,20,21,25,26,29–32 while three studies were aimed to assess the proportion of non-adherence to antihypertensive medication and associated factors among hypertensive patients,19,23,24 one study22 was aimed to assess the patient compliance and associated factors of antihypertensive treatments, another study28 was designed to assess the determinants of adherence to antihypertensive medication, and the remaining study27 was intended to measure the contribution of adverse effects on antihypertensive medications adherence.
The main medication adherence measurement method was MMAS eight-item scale which was used by six studies,19,21,23,26,28,30 MMAS four-item which was used by three studies,20,31,32 and questionnaire technique by five studies.22,24,25,27,29 Some studies which assessed adherence using questionnaire-based technique were also use other additional methods like pill count24 and a questionnaire-based Morisky Green test.25 Based on the medication adherence measurement methods being used, the adherence level was defined in different ways in these studies.
Five studies did not calculate the sample size.19,21,22,24,27 For studies which calculated the sample size, the response rates were ranged from 93.5%23 to 100%.20,25,30 The proportion of female hypertensive patients in these studies was ranging from 29.76%28 to 63.3%25 with an overall proportion of 49.63%. Three studies22,28,29 did not report the mean age of the participants. The mean age of the patients in the remaining 11 studies was ranging from 51.5 (±standard deviation (SD) 12.1) to 58.3 years (±SD 13.7) with the overall mean age of 55.13 years. The methods of assessing adherence and reported adherence of these 14 studies are presented in Table 2 (research objective, measurement of adherence, definition of adherence, response rate, sex distribution, and mean age ± SD).
Table 2.
The methods of assessing adherence and reported adherence of studies included in SR and MA on adherence to antihypertensive medications and associated factors among hypertensive patients in Ethiopia, 2020.
| Authors | The objective of the study | Adherence measure method | Definition of adherence | Response rate | Male: female, N (%) | Mean age with a range in years | Quality assessment (%) |
|---|---|---|---|---|---|---|---|
| Ali et al.19 | To assess antihypertensive medication non-adherence and its determinants among patients on follow-up in Ayder Referral Hospital (ARH) and Mekelle General Hospital (MGH) | MMAS 8 | Not clearly stated | No SSC | 46 (38%): 75 (62%) | Mean = 54.7 ± 12.7 (no range) | 83.4% |
| Ambaw et al.20 | To assess adherence to antihypertensive therapy and associated factors among HPN patients on follow-up at the University of Gondar Referral Hospital | MMAS 4 | MMAS mean score ⩾3 | 100% | 142 (37%): 242 (63%) | Mean = 56.9 ± 12.8 (no range) | 83.4% |
| Asgedom et al.21 | To assess antihypertensive medication adherence and associated factors among adult hypertensive patients | MMAS 8 | MMAS 8 score was ⩾6 | No SSC | 149 (53.2%): 131 (46.8%) | Mean = 55.0 ± 12.7 years | 79.1% |
| Bekele22 | To assess the patient compliance and associated factors of antihypertensive treatments in hypertensive patients visiting the Gimbi General Hospital | Questionnaire | Not clearly stated | No SSC | 52 (40.9%): 75 (59.1%) | Not calculated | 83.4% |
| Berisa and Dedefo23 | To assess non-adherence-related factors to antihypertensive medications among hypertensive patients on follow-up at the Nedjo General Hospital | MMAS 8 | MMAS 8 score = 8 | 93.50% | 76 (44.2%): 96 (55.8%) | Mean: 51.5 + 12.1 years | 79.1% |
| Chelkeba and Dessie24 | To assess the magnitude of adherence and the factors associated with non-adherence to antihypertensive medication | Questionnaires (plus pill count) | 80% was considered as adherence | No SSC | 69 (69%): 31 (31%) | Mean: 53.88 ± 10.12 (30–72 years) | 83.4% |
| Dego and Bobasa25 | To assess adherence to antihypertensive medication and contributing factors among non-comorbid hypertensive patients in two hospitals of Jimma town, southwest Ethiopia | Questionnaire (Morisky Green test) | Adherence: MGT score of >3 | 100% | 44 (36.7%): 76 (63.3%) | Mean: 53.85 ± 12.00 years | 83.4% |
| Demisew et al.26 | To assess the prevalence of adherence to antihypertensive treatment and associated factors among hypertensive patients | MMAS 8 | MMAS 8: score ⩾8 | 99.60% | 142 (52.4%): 128 (47.4%) | Mean age of 53.7 ± 1.47 years | 79.1% |
| Gebreyohannes et al.27 | To measure the contribution of adverse effects on antihypertensive medication adherence | Questionnaire | >80 medication | No SSC | 117 (47%): 132 (53%) | Mean: 56.51 ± 11.00 years | 83.4% |
| Getenet et al.28 | To assess the determinants of adherence to antihypertensive medication among hypertensive patients on follow-up in the Hawassa Referral Hospital | MMAS 8 | MMAS 8 score was ⩾6 | 100% | 203 (70.24%): 86 (29.76%) | Not calculated | 83.4% |
| Hareri et al.29 | To assess the magnitude of adherence and associated factors with antihypertensive treatment among adults on follow-up at the Adama Hospital, 2013 G.C. | Questionnaire | Scored above mean for medication adherence | 94% | 178 (48.8%): 187 (51.2%) | Not calculated | 68.8% |
| Mekonnen et al.30 | To assess adherence level and its determinants for antihypertensive medications among adult hypertensive patients attending the chronic illness clinics of the referral hospitals in northwest Ethiopia | MMAS 8 | Scored ⩾6 points | 100% | 236 (57.7%): 173 (42.3%) | Mean: 54.5 ± 13.58 years | 83.4% |
| Teshome et al.31 | To assess adherence to antihypertensive medications and identify associated factors at the Debre Tabor General Hospital, northwest Ethiopia | MMAS 4 | MMAS mean score ⩾3 | 97.4% | 163 (48.4%): 174 (51.6%) | Mean = 58.3 + 13.7 years, ranging (23–88) | 83.4% |
| Tibebu et al.32 | To assess adherence to prescribed antihypertensive medications and its associated factors | MMAS 4 | MMAS 4: >3 = low adherence; 1 or 2 = medium adherence, and 0 = high adherence | 97% | 210 (52%): 194 (48%) | Mean: 54 ± 10.77 years | 71.9% |
SR: systematic review; MA: meta-analysis; MMAS: Morisky Medication Adherence Scale; SSC: sample size calculation; MGT: Morisky Green test; HPN: hypertension.
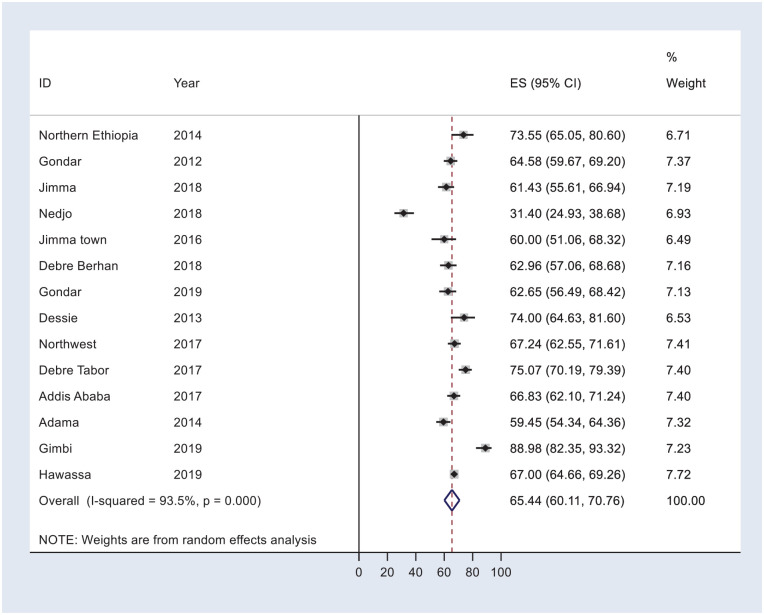
The pooled prevalence of medication adherence
The percentage of medication adherence among hypertensive was wide ranging across reports of primary studies in Ethiopia. The smallest prevalence of mediation adherence was 31.4% as reported by the Nedjo study23 while the highest prevalence (89.98%) was reported from Gimbi.22 The overall pooled prevalence of medication adherence among hypertensive patients in Ethiopia was 65.41% (95% CI: 58.91–71.91; Figure 2).
Figure 2.
Forest plot for the pooled prevalence of antihypertensive medication adherence in Ethiopia.
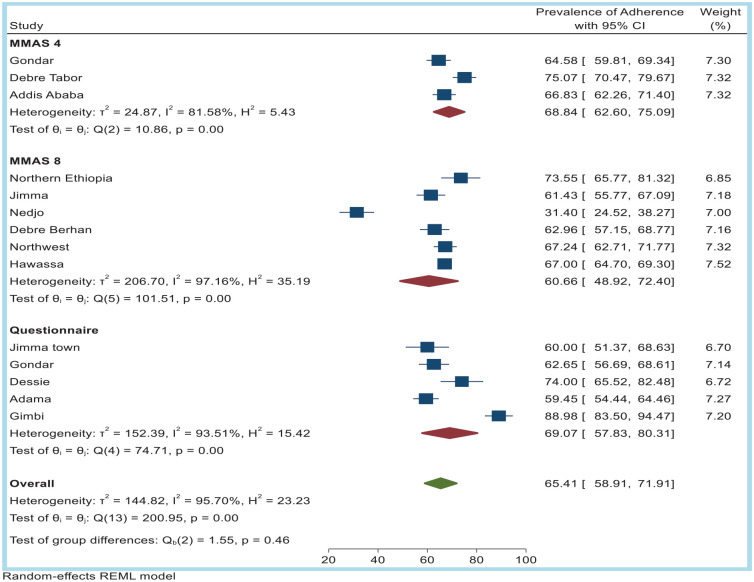
Sub-group analysis based on the adherence measurement methods
Sub-group analysis was computed to assess variability in the level of medication adherence in relation to methods used to measure adherence. The medication adherence measurement methods used by primary studies were categorized into MMAS eight-item, MMAS four-item, and questionnaire technique. According to this sub-group analysis, the magnitudes of medication adherence were substantial variable between the primary studies depending on the difference in methods used to measure medication adherence (I2 = 95.70%). The highest pooled prevalence of medication adherence was observed among studies using questionnaire technique (69.07%, 95% CI: 57.83–80.31, I2 = 93.51), followed by studies using MMAS four-items 68.84% (95% CI: 62.60–75.09, I2 = 81.58). The lowest prevalence (60.66%) was observed among studies using MMAS eight-items to measure medication adherence (95% CI: 48.92–72.40, I2 = 97.16; Figure 3).
Figure 3.
Sub-group analysis showing the pooled prevalence of antihypertensive medication adherence based on tools used to assess medication adherence in Ethiopia, 2020.
Factors associated with adherence
A total of 12 studies reported AORs for factors affecting adherence or non-adherence. According to World Health Organization (WHO) recommendation,11 the identified factors associated with medication adherence in the reviewed studies were categorized into five sets of factors or dimensions which included social and economic factors, therapy-related factors, patient-related factors, condition-related factors, and healthcare system–related factors.
Social and economic factors
The social and economic factors that showed significant association with medication adherence in these studies were age, sex, level of education, place of residence, monthly income, and absence of family support (Table 3).
Table 3.
Social and economic factors that showed significant association with antihypertensive medication adherence among hypertensive patients in Ethiopia, 2020.
| Authors | Area | Outcome variable | Socioeconomic factors affecting adherence to antihypertensive medication (AOR and 95% CI) |
|---|---|---|---|
| Ali et al.19 | Northern Ethiopia | Adherence to antihypertensive medication | Living in Mekelle city (AOR = 0.184, 95% CI: 0.024–0.597) less adherent to medication Absence of family support (AOR = 0.170, 95% CI: 0.030–0.905) less adherent to medication |
| Ambaw et al.20 | Gondar | Adherence to antihypertensive medication | Male (AOR = 0.48, 95% CI: 0.28–0.82) less adherent to medication |
| Berisa and Dedefo23 | Nedjo | Antihypertensive medication non-adherence | Greater than 55 years of age (AOR = 0.10, 95% CI: 0.01–0.85) more non-adherent to medication Elementary level of education (AOR = 21.62, 95% CI: 3.17–147.38) more non-adherent to medication Monthly income less than 500 birr (AOR = 18.51, 95% CI: 1.95–176.06) more non-adherent to medication |
| Dego and Bobasa25 | Jimma town | Antihypertensive medication adherence | No multivariable analysis (only p-value) Middle-aged (41–60 years old) patients: more likely to adhere to medication (p-value = 0.01) |
| Getenet et al.28 | Hawassa | Adherence toward antihypertensive treatment | Age: 18–44 (AOR = 3.80, 95% CI: 1.08–13.31) and 45–54 years (AOR = 2.79, 95% CI: 1.01–7.78) more adherent to medication Urban residence (AOR = 6.84, 95% CI: 3.05–15.36) more adherent to medication |
| Hareri et al.29 | Adama | Adherence status | Middle (46–55 years) age (AOR = 0.30, 95% CI: 0.142–0.640) more non-adherent to medication |
| Teshome et al.31 | Debre Tabor | Adherence toward antihypertensive treatment | Urban residence (AOR = 2.10, 95% CI: 1.15–3.85) more adherent to medication Age >60 years (AOR = 0.33, 95% CI: 0.11–0.98) more non-adherent to medication |
| Tibebu et al.32 | Addis Ababa | Adherence to prescribed antihypertensive medications | Female (AOR = 2.18, 95% CI: 1.33–3.58) more adherent to medication Middle-aged and older adults (AOR = 3.15, 95% CI: 1.34–7.37) and (AOR = 4.09, 95% CI: 1.47–11.39) more adherent to medication |
AOR: adjusted odds ratio; 95% CI: 95% confidence interval.
Out of 11 studies19,23–32 that assess the association of hypertensive patient’s age with medication adherence, six studies found an association.23,25,28,29,31,32 But the studies did not use the same-age categories. Generally, those studies revealed that older hypertensive patients were more likely to adhere to their medication than younger patients. According to a study in Nedjo,23 the odds of adherence were 10 times (AOR = 10.0, 95% CI: 1.18–100.0) more likely among older patients (age >55 years) than the young patients (age 18–34 years). The study in Addis Ababa32 also reported that older (>60 years) and middle-aged (40–59 years) hypertensive patients were found more likely (AOR = 4.09, 95% CI: 1.47–11.39) and (AOR = 3.15, 95% CI: 1.34–7.37) to be adherent than young adults (21–39), respectively. The study in Adama town29 showed that middle-aged (46–55 years) patients were 70% less likely (AOR = 0.30, 95% CI: 0.142–0.640) to be adherent to their medication in comparison with older age (age >55 years) patients. But a study by Dego and Bobasa25 found that middle-aged (41–60 years old) patients were more likely to adhere to their medication compared with participants with older (>60 years) patients (p-value = 0.01). On the contrary, the Debre Tabor study31 stated that older age patients (>60 years) were 67% less likely (AOR = 0.33, 95% CI: 0.11–0.98) to be adherent in compared to younger (age 18–40 years) patients. Similarly, the Hawassa study28 also reported that young age (18–44 years) and middle-aged patients (45–54 years) were three times (AOR = 3.80, 95% CI: 1.08–13.31) and 2.78 times (AOR = 2.79, 95% CI: 1.01–7.78) more adherent as compared to elderly people (>65). In contrary, studies in northern Ethiopia,19 Dessie,24 Debre Berhan,26 University of Gondar,27 and northwest Ethiopia30 showed that there was no statistically significant association between age and medication adherence.
Three studies indicated that sex had an association with medication adherence.20,25,32 All of these studies indicated that female patients were more adherent than males. A study in Addis Ababa32 stated that female hypertensive patients were two times (AOR = 2.18, 95% CI: 1.33–3.58) more likely to be adherent than male patients. Similarly, a study by Ambaw et al.20 at Gondar revealed that the odds of adherence to antihypertensive treatment were 52% less likely (AOR = 0.48, 95% CI: 0.28–0.82) among male patients than the female patients. However, studies in northern Ethiopia,19 Debre Berhan,26 Adama,29 and Dessie24 found no significant association between gender and medication adherence among hypertensive patients.
Two studies showed the relationship between education status and medication adherence.23,25 Illiterate and elementary grade hypertensive patients in Nedjo were 85% (AOR = 0.148, 95% CI: 0.022–0.990) and 95% (AOR = 0.046, 95% CI: 0.007–0.855) less likely to be adherent to medications than those who were college and university graduates, respectively.23 A similar finding was also reported in Jimma.25 Studies in northwest Ethiopia,19 Gondar,20 Debre Berhan,26 Hawassa,28 Adama,29 northern Ethiopia,30 Debre Tabor,31 and Addis Ababa32 found that the educational level was not a significant contributing factor to adherence.
Three studies showed an association between place of residence and medication adherence.19,28,31 The study in Debre Tabor31 shown that respondents who lived in urban areas were two times (AOR = 2.10, 95% CI: 1.15–3.85) more likely to adhere to their antihypertensive medication compared to those who lived in rural areas. Similarly, Hawassa’s study28 also reported that patients living in urban areas were six times (AOR = 6.84, 95% CI: 3.05–15.36) more likely to be adherent than those living in a rural area. But a study in northern19 found that living in the city had an inverse relation with adherence (AOR = 0.184, 95% CI: 0.024–0.597). Many of the reviewed studies, however, stated that there was no association between place of residence and medication adherence.20,23,25,26,30
In Nedjo, those hypertensive patients with low monthly income (<500 Ethiopian birrs) were less likely (AOR = 0.054, 95% CI: 0.006–0.513) to be adherent to their medications than patients with higher monthly income.23 But studies in Gondar,20 Jimma,25 Debre Berhan,26 Adama,29 and northwest Ethiopia30 revealed that the monthly income of the patients had no association with their medication adherence.
Studies in northern Ethiopia also indicated that family support was an important factor associated with medication adherence.19 Hypertensive patients who did not get support from family were more likely to have lower adherence to medication as compared to those who have family support (AOR = 0.170, 95% CI: 0.030–0.905). But according to the study in Addis Ababa, having social support had no association with medication adherence.32 Except for a study in Jimma,25 which showed a statistically significant association between marital status and medication adherence (p-value < 0.05), no study in Ethiopia shown an association between antihypertensive medication adherence and occupational or marital status of the patients.19,20,23,26,29,30,32
Disease/condition-related factors
Nine studies found significant associations between disease-related factors like comorbidities, complication, stage of hypertension, BP controlled, having symptoms (muscle pain, tiredness, poor sleep) and forget the fullness of their drugs to adherence with antihypertensive medication19–21,26–31 (Table 4).
Table 4.
Disease condition–related factors that showed significant association with antihypertensive medication adherence among hypertensive patients in Ethiopia, 2020.
| Study ID | Area | Outcome variable | Disease condition–related factors affecting adherence to antihypertensive medication (AOR and 95% CI) |
|---|---|---|---|
| Ali et al.19 | Northern Ethiopia | Adherence to antihypertensive medication | Being at the pre-hypertension class of BP (AOR = 0.052, 95% CI: 0.003–0.242) less adherent to medication Hypertensive heart disease (AOR = 21.737, 95% CI: 1.568–418.428) more non-adherent to medication |
| Ambaw et al.20 | Gondar | Adherence to antihypertensive medication | Controlled hypertension (AOR = 2.93, 95% CI: 1.73–4.96) more adherent to medication Without comorbidity (AOR = 2.50, 95% CI: 1.01–6.21) more adherent to medication Have only one comorbidity (AOR = 2.68, 95% CI: 1.07–6.71) more adherent to medication |
| Asgedom et al.21 | JUSH | Antihypertensive medication adherence | Comorbidity (AOR = 0.083, 95% CI: 0.033–0.207) more likely to be non-adherent |
| Dego and Bobasa25 | Jimma town | Antihypertensive medication adherence | No multivariable analysis (only p-value) |
| Demisew et al.26 | Debre Berhan | Adherence toward antihypertensive treatment | Comorbid heart disease (AOR = 0.043, 95% CI: 0.03–0.7) less adherent to medication Forget fullness of their drugs (AOR = 0.014, 95% CI: 0.02–0.116) less adherent to medication |
| Gebreyohannes et al.27 | UoG | Level of adherence to antihypertensive medications | Feel tiredness (AOR = 3.802, 95% CI: 1.723–8.391) more non-adherent to medication Muscle pain (AOR = 5.199, 95% CI: 1.407–19.214) more non-adherent to medication Poor sleep (AOR = 4.89, 95% CI: 1.578–15.160) more non-adherent to medication Symptoms caused them to change their antihypertensive drug taking behavior (AOR = 16.104, 95% CI: 4.164–62.290) more non-adherent to medication |
| Getenet et al.28 | Hawassa | Adherence toward antihypertensive treatment | No comorbidities (AOR = 3.14, 95% CI: 1.48–6.67) more adherent to medication Controlled BP (AOR = 2.35, 95% CI: 1.15–4.81) more adherent to medication |
| Hareri et al.29 | Adama | Adherence status | Comorbidities (AOR = 0.50, 95% CI: 0.290–0.893) less adherent to medication |
| Mekonnen et al.30 | Northwest | Adherence toward antihypertensive treatment | No comorbidity (AOR = 4.36, 95% CI: 1.34–14.11) more adherent to medication |
AOR: adjusted odds ratio; 95% CI: 95% confidence interval; JUSH: Jimma University Specialized Hospital; UoG: University of Gondar.
Five studies indicated that the presence of comorbidities affected the extent of antihypertensive medication adherence.20,21,28–30 This finding was, however, non-conclusive. Hypertensive patients with comorbid conditions were 50% less likely (AOR = 0.50, 95% CI: 0.290–0.893) to be adherent compared to patients without comorbidity in Adama.29 Similarly in Jimma University Specialized Hospital (JUSH) patients with comorbidities were 91.7% less likely (AOR = 0.083, 95% CI: 0.033–0.207) to be adherent compared to patients without comorbidities.21 The Hawassa study also reported that hypertensive patients without comorbidity were three times (AOR = 3.14, 95% CI: 1.48–6.67) more likely to adhere to their medication than patients with comorbidity.28 However, a study in northwest indicated that hypertensive patients without comorbidity were four times (AOR = 4.36, 95% CI: 1.34–14.11) more likely to adhere to antihypertensive medications than their counterparts.30 Likewise, a study in Gondar found that patients without comorbidity and patients with only one comorbidity were 2.5 (AOR = 2.50, 95% CI: 1.01–6.21) and almost three (AOR = 2.68, 95% CI: 1.07–6.71) times more likely to be adherent to their medication than patients with two or more comorbidities, respectively.20 Two studies also indicated that the presence of hypertension-related complications such as heart diseases was associated with medication adherence among hypertensive patients.19,26 Hypertensive patients with hypertensive heart disease were 95.4% less likely (AOR = 0.046, 95% CI: 0.002–0.638) to adhere to their antihypertensive therapy than patients without the complication.19 The Debre Berhan study also revealed that hypertensive patients with comorbid heart disease were 95.7% less likely (AOR = 0.043, 95% CI: 0.03–0.7) to adhere to their antihypertensive treatment than patients without comorbid heart disease.26 However, a study in Debre Tabor indicated that having comorbidities like diabetes, cardiovascular disease (CVD), or asthma had no association with medication adherence.31
The study in northern Ethiopia19 found that patients at the pre-hypertension level (BP between 120/80 and 140/90 mm Hg) were 94.8% less likely (AOR = 0.052, 95% CI: 0.003–0.242) to be adherent to their medications than patients with higher BP (>160/100 mm Hg). Those hypertensive patients with controlled BP were three times (AOR = 2.93, 95% CI: 1.73–4.96) higher chance of being adherent to their treatment in Gondar.20 In Hawassa, similar finding was reported as patients with controlled BP were two times more likely (AOR = 2.35, 95% CI: 1.15–4.81) adherent than those with uncontrolled BP value.28 But the study in northwest Ethiopia stated that adherence to antihypertensive medication is not associated with BP control.30
There was a significant relationship between forgetfulness and medication adherence among hypertensive patients. A study in Debre Berhan found that hypertensive patients who experienced forgetfulness of their drugs were 98.6% less likely (AOR = 0.014, 95% CI: 0.02–0.116) to be adherent.26 A study at the University of Gondar27 found that the presence of some symptoms significantly decreased the chance of adherence to hypertensive medication. Hypertensive patients who always or usually feel tiredness, muscle pain, and poor sleep were 74% (AOR = 0.263, 95% CI: 0.119–0.580), 81% (AOR = 0.192, 95% CI: 0.052–0.711), and 80% (AOR = 0.204, 95% CI: 0.066–0.634) less likely to be adherent to their antihypertensive medication, respectively. Moreover, this study also reported that the presence of symptoms caused hypertensive patients to change their antihypertensive medication–taking behavior and make them less adherent to their medication (AOR = 16.104, 95% CI: 4.164–62.290).
Therapy-related factors
Eight studies reported significant associations between therapy-related factors and adherence to antihypertensive medications21,23–25,27,30–32 (Table 5).
Table 5.
Therapy-related factors that showed significant association with antihypertensive medication adherence and among hypertensive patients in Ethiopia, 2020.
| Study ID | Area | Outcome variable | Therapy-related factors affecting adherence to antihypertensive medication (AOR and 95% CI) |
|---|---|---|---|
| Asgedom et al.21 | JUSH | Antihypertensive medication adherence | Combination of antihypertensive medications (AOR = 0.32, 95% CI: 0.144–0.712) more non-adherent to medication |
| Berisa and Dedefo23 | Nedjo | Antihypertensive medication non-adherence | Long duration on treatment (>5 years) (AOR = 5.41, 95% CI: 1.08–27.22) more non-adherent to medication |
| Chelkeba and Dessie24 | Dessie | Non-adherence to antihypertensive medication | Experiencing side effect of the medication (AOR = 4.00, 95% CI: 3.567–6.223) more non-adherent to medication |
| Dego and Bobasa25 | Jimma | Antihypertensive medication adherence | No multivariable analysis (only p-value) |
| Gebreyohannes et al.27 | UoG | Level of adherence to antihypertensive medications | Believing symptoms are caused by antihypertensive medications (AOR = 3.249, 95% CI: 1.248–8.456) more non-adherent to medication |
| Mekonnen et al.30 | Northwest | Adherence toward antihypertensive treatment | On medications for 3 and more years (AOR = 1.89, 95% CI: 1.10–3.35) more adherent to medication |
| Teshome et al.31 | Debre Tabor | Adherence toward antihypertensive treatment | Taking less than two drugs per day (AOR = 3.04, 95% CI: 1.53–6.06) more adherent to medication |
| Tibebu et al.32 | Addis Ababa | Adherence to prescribed antihypertensive medications | Taking more than two types of anti-HPN med (AOR = 0.315, 95% CI: 0.118–0.845) less adherent to medication |
AOR: adjusted odds ratio; 95% CI: 95% confidence interval; JUSH: Jimma University Specialized Hospital; UoG: University of Gondar; HPN: hypertension.
Studies in Debre Tabor31 and JUSH21 found that the number of antihypertensive pills a day had a significant association with adherence. Debre Tabor study found that antihypertensive medication adherence was three times (AOR = 3.04, 95% CI: 1.53–6.06) more likely among hypertensive patients with fewer drugs (<2) per day in compared with patients with more drugs.31 Similarly, patients who are taking only one drug in JUSH were three times (AOR = 3.125, 95% CI: 1.40–6.94) more likely to be adherent than those who take more than one drug.21 However, many studies revealed that medication adherence had no association with the number of pills patients took per day.19,20,23,25–27,30 A study in Addis Ababa reported that patients who are prescribed with two or less types of antihypertensive medications were three times (AOR = 3.17, 95% CI: 1.18–8.47) more likely to be adherent than those who took more than two types of medications.32
A couple of studies reported that the duration of therapy was associated with antihypertensive medication adherence.23,30 Patients who were on antihypertensive medication for three or more years were two times (AOR = 1.89, 95% CI: 1.10–3.35) more likely to adhere to treatment than those who had been diagnosed for less than 3 years in northwest Ethiopia.30 On the contrary, the Nedjo study23 found that patients with longer duration (>5 years) on antihypertensive medication were less likely to be adherent to their treatment (AOR = 0.185, 95% CI: 0.037–0.926). But large numbers of studies in Ethiopia found that there was no statistically significant association between duration of therapy and medication adherence.19–21,25–27,32 Hypertensive patients who experienced side effects of their medications were 75% less likely (AOR = 0.250, 95% CI: 0.161–0.280) to be adherent to their medication than those who did not experience side effects in Dessie.24
Patient-related factors
Eleven studies found significant associations between patient-related factors with adherence to antihypertensive medication.20,21,23,25–32 These patient-related factors were as follows: knowledge about hypertension and its treatment, attitude about antihypertensive treatment, lack of information about their medication, regular physical exercise, and alcohol intake (Table 6).
Table 6.
Patient-related factors that showed significant association with antihypertensive medication adherence and among hypertensive patients in Ethiopia, 2020.
| Study ID | Area | Outcome variable | Patient-related factors affecting adherence to antihypertensive medication (AOR and 95% CI) |
|---|---|---|---|
| Ambaw et al.20 | Gondar | Adherence to antihypertensive medication | Being knowledgeable (AOR = 6.21, 95% CI: 3.22–11.97) more adherent to medication Favorable attitude (AOR = 3.23, 95% CI: 1.31–7.97) more adherent to medication |
| Asgedom et al.21 | JUSH | Antihypertensive medication adherence | Taking alcohol (AOR = 0.011, 95% CI: 0.002–0.079) more non-adherent to medication |
| Berisa and Dedefo23 | Nedjo | Antihypertensive medication non-adherence | No knowledge about HPT and treatment (AOR = 7.67, 95% CI: 2.48–23.73) more non-adherent to medication Inactive physical activity (AOR = 34.51, 95% CI: 4.66–255.89) less adherent to medication |
| Dego and Bobasa25 | Jimma | Antihypertensive medication adherence | No multivariable analysis (only p-value) |
| Demisew et al.26 | Debre Berhan | Adherence toward antihypertensive treatment | Perceives hypertension as a somehow less severe disease (AOR = 0.018, 95% CI: 0.01–0.37) less adherent to medication |
| Gebreyohannes et al.27 | UoG | Level of adherence to antihypertensive medications | Perform regular physical exercise (AOR = 5.88, 95% CI: 2.49–13.89) more adherent to medication |
| Getenet et al.28 | Hawassa | Adherence toward antihypertensive treatment | Have good knowledge (AOR = 3.13, 95% CI: 1.43–6.82) more adherent to medication |
| Hareri et al.29 | Adama | Adherence status | Lack of information about their medication (AOR = 0.12, 95% CI: 0.258–0.583) less adherent to medication |
| Mekonnen et al.30 | Northwest | Adherence toward antihypertensive treatment | Favorable attitude about antihypertensive treatment (AOR = 9.88, 95% CI: 5.34–18.27) more adherent to medication |
| Teshome et al.31 | Debre Tabor | Adherence toward antihypertensive treatment | Being knowledgeable (AOR = 8.86, 95% CI: 4.67–16.82) more adherent to medication |
| Tibebu et al.32 | Addis Ababa | Adherence to prescribed antihypertensive medications | Have good knowledge (AOR = 3.378, 95% CI: 1.971–5.789) more adherent to medication |
AOR: adjusted odds ratio; 95% CI: 95% confidence interval; JUSH: Jimma University Specialized Hospital; UoG: University of Gondar.
Out of six studies20,23,28,30–32 which assessed the relationship between medication adherence and knowledge about hypertension and its treatment, five of them20,23,28,31,32 found a positive association. The study in Addis Ababa,32 Debre Tabor,31 Gondar,20 and Hawassa28 revealed that hypertensive patients who had good knowledge of hypertensive and its treatment were three times (AOR = 3.378, 95% CI: 1.971–5.789), nine times (AOR = 8.86, 95% CI: 4.67–16.82), six times (AOR = 6.21, 95% CI: 3.22–11.97), and three times (AOR = 3.13, 95% CI: 1.43–6.82) more likely to adhere to their antihypertensive medication, respectively. Similarly, a study in Nedjo found that hypertensive patients with poor knowledge on hypertension and treatment were 86.9% (AOR = 0.131, 95% CI: 0.042–0.403) less likely to be adherent to their medication in comparison with those with good knowledge.23 But studies in northwest Ethiopia reported that there was no statistically significant association between medication adherence and the knowledge status of the patient.30 Hypertensive patients who did not have information about their medication were 88% less likely to be adherent to their prescribed medications in Adama (AOR = 0.12, 95% CI: 0.258–0.583).29
Another important factor associated with medication adherence was the attitude about antihypertensive treatment. Studies in Gondar20 and northwest30 reported that hypertensive patients who had favorable attitude were three times (AOR = 3.23, 95% CI: 1.31–7.97) and 10 times (AOR = 9.88, 95% CI: 5.34–18.27) more likely to adhere to antihypertensive medications than those who had unfavorable attitude, respectively.
Performing physical activity regularly was also associated with antihypertensive medication adherence. A study in the University of Gondar27 reported that patients who regularly perform physical exercise were six times more likely to be adherent to their medication (AOR = 5.88, 95% CI: 2.49–13.89). Similarly, those physically inactive hypertensive patients were less likely to be adherent to their antihypertensive medications, as found in a study in Nedjo (AOR = 0.029, 95% CI: 0.004–0.215).23
The association between alcohol consumption and medication adherence among hypertensive patients was not conclusive. JUSH study reported that patients with a habit of alcohol consumption were 89% less likely (AOR = 0.011, 95% CI: 0.002–0.079) to be adherent to antihypertensive treatment.21 In contrast, a study in Debre Tabor did not found any significant association between alcohol consumption and medication adherence among hypertensive patients.31
Healthcare system–related factors
Five studies found an association between adherence with antihypertensive medication and healthcare-related factors like distance from the hospital, patient–provider relationship, and cost of medication20,21,24,25,30 (Table 7).
Table 7.
Healthcare system-related factors that showed a significant association with antihypertensive medication adherence and among hypertensive patients in Ethiopia, 2020.
| Study ID | Area | Outcome variable | Healthcare system–related factors affecting adherence to antihypertensive medication (AOR and 95% CI) |
|---|---|---|---|
| Ambaw et al.20 | Gondar | Adherence to antihypertensive medication | Distance from the hospital (AOR = 2.02, 95% CI: 1.19–3.43) more adherent to medication |
| Asgedom et al.21 | JUSH | Antihypertensive medication adherence | Getting medications freely (AOR = 0.020, 95% CI: 0.003–0.12) more adherent to medication |
| Chelkeba and Dessie24 | Dessie | Non-adherence to antihypertensive medication | Poor patient–physician interaction (AOR = 2.0, 95% CI: 1.05–4.20) more non-adherence to medication |
| Dego and Bobasa25 | Jimma | Antihypertensive medication adherence | No multivariable analysis (only p-value) Believed health professionals and conditions at health institutions good more compliant |
| Mekonnen et al.30 | Northwest | Adherence toward antihypertensive treatment | Got the medication/s free of charge or with low cost (AOR = 2.06, 95% CI: 1.13–3.76) more adherent to medication Good patient–provider relationship (AOR = 4.27, 95% CI: 2.32–7.86) more adherent to medication |
AOR: adjusted odds ratio; 95% CI: 95% confidence interval; JUSH: Jimma University Specialized Hospital
Distance from the hospital had an inconclusive relationship with medication adherence. A study in Gondar20 reported that as the distance from the hospital decreased, the adherence to medication got improved (AOR = 2.02, 95% CI: 1.19–3.43). Whereas studies in Jimma,25 Adama,29 and northwest30 reported that distance from the hospital had no association with medication adherence.
Another healthcare-related factor that shows significant association with adherence was patient–provider relationships. Study in the northwest shown that patients who had good patient–provider relationships were four times (AOR = 4.27, 95% CI: 2.32–7.86) more likely to have good adherence to antihypertensive medication.30 However, patients who had a poor interaction with the physician were 50% (AOR = 0.50, 95% CI: 0.238–0.957) less likely to adhere to their antihypertensive medications in Dessie.24 Moreover, a study in Jimma shown that patients who believed the goodness of health professionals and conditions at health institutions were more compliant than those who did not.25 This association was not seen in the Gondar study.20
Another non-conclusive health-related factor associated with adherence was medication cost or charge. Study in northwest revealed that patients who had got their medications free of charge or with the low cost was two times (AOR = 2.06, 95% CI: 1.13–3.76) more likely to adhere to the medication than those who had got the medication/s with high cost.30 Similarly, those patients who get medications freely were 50 times (AOR = 50.0, 95% CI: 8.55–333.33) more likely to be adherent to their medication in JUSH.21 But the study in northern,19 Gondar,20 Debre Berhan,26 and Hawassa28 found that medication adherence had no association with medication cost or charge
An MA of ORs
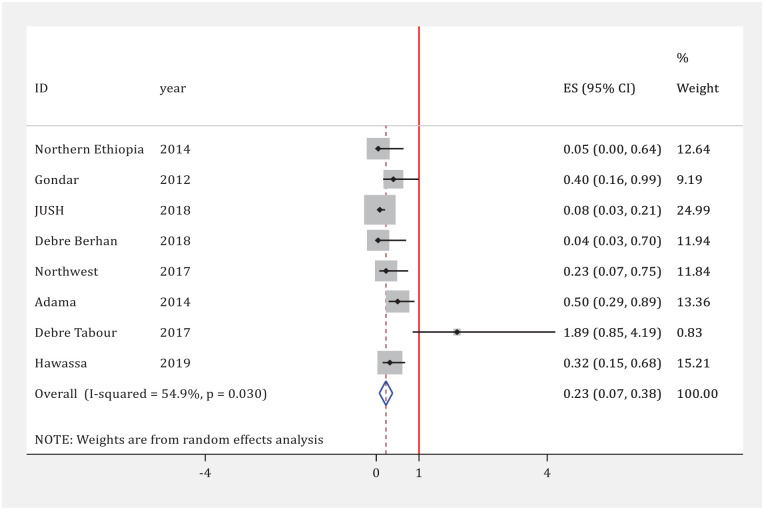
Association between comorbidities and medication adherence
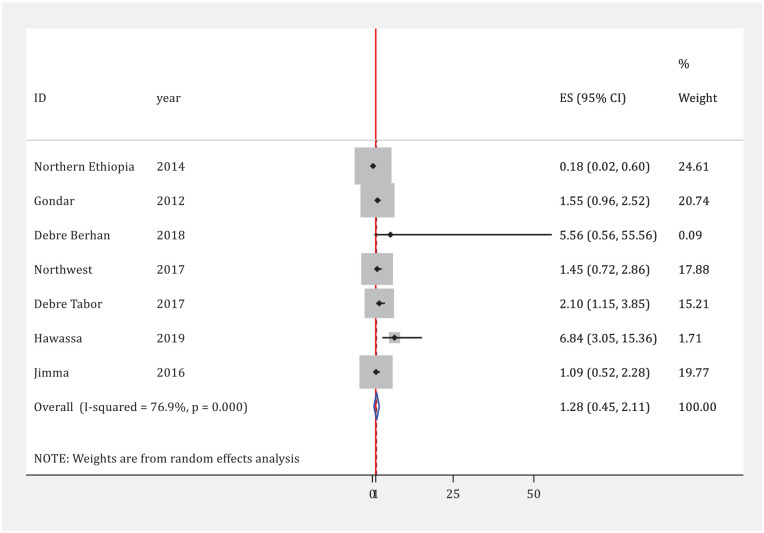
Eight studies have tried to assess the association between adherence to medication and comorbidities and/or complications in hypertensive patients.19–21,26,28–31 Based on these studies, the presence of comorbidities and complications was significantly associated with antihypertensive medication adherence. As indicated in the forest plot in blow, the confidence intervals of seven studies did not cross the line-of-no-effect (OR = 1), meaning that there are no significant differences. Similarly, the confidence interval of the summary estimate (diamond shape) lies entirely to the left of the line-of-no-effect representing a significantly lower adherence among hypertensive patients with comorbidities and complications (p = 0.030). Overall, hypertensive patients with comorbidities and/or complications had 77% lower odds of adherence to antihypertensive medications than patients without comorbidities and/or complications (pooled OR = 0.23, 95% CI: 0.07–0.38, p = 0.030, heterogeneity I2 = 54.9%; Figure 4)
Figure 4.
Meta-analysis of the association between medication adherence and comorbidities in hypertensive patients, 2020.
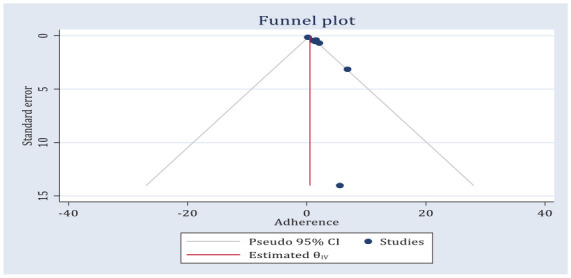
Since funnel plot is symmetric, the observed association between adherence to medication and comorbidities in hypertensive patients was not due to publication bias (Figure 5). The Egger regression asymmetry test also demonstrated no statistically significant publication biases (Egger’s test; b = 1.66, p = 0.0.143).
Figure 5.
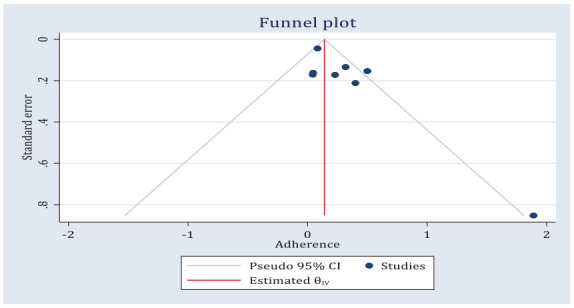
Funnel plot of the odds of the association between medication adherence and comorbidities among hypertensive patients, 2020.
Association between knowledge and medication adherence
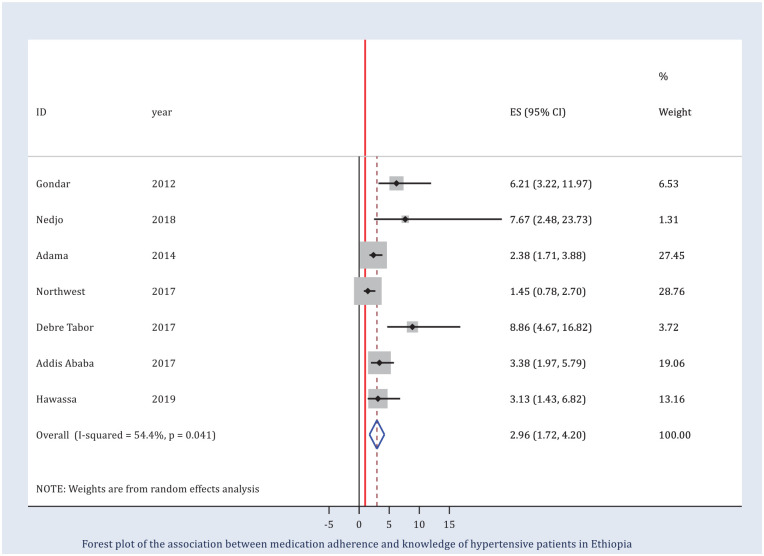
The association between medication adherence and knowledge of hypertensive patients was assessed by seven studies.20,23,28–32 The MA of these seven studies demonstrated an increased odds of adherence to medication among hypertensive patients with good knowledge about their disease and its management. Six of the seven studies independently reported an OR greater than 1. The odds of adherence to antihypertensive medication were three times increased among patients with a good level of knowledge as compared to those with a poor level of knowledge (pooled OR = 2.98, 95% CI: 1.72–4.24, p = 0.04, heterogeneity I2 = 55.55%; Figure 6). The funnel plot appeared asymmetrical (Figure 7) and an Egger’s regression was significant (b = 2.13, p = 0.07).
Figure 6.
Meta-analysis of the association between medication adherence and knowledge of hypertensive patients, 2020.
Figure 7.
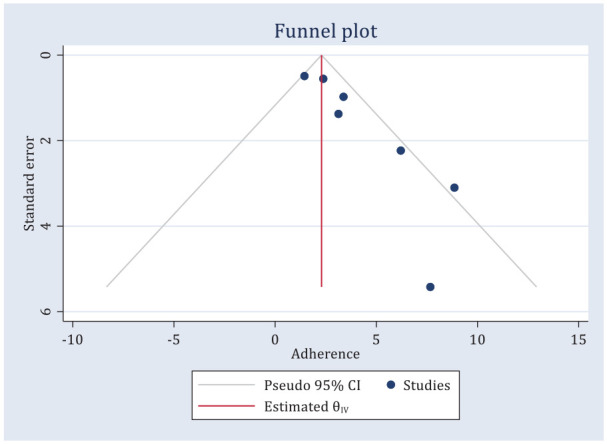
Funnel plot of the odds of the association between medication adherence and knowledge of hypertensive patients in Ethiopia, 2020.
Association between the place of residence and medication adherence
Seven studies reported the association between adherence to medication and place of residence of hypertensive patients.19,20,25,26,28,30,31 Two of the seven studies28,31 individually reported an OR greater than 1 while one study19 reported an OR less than 1. However, the overall pooled OR suggested that there was no significant association between medication adherence and place of residence (pooled OR = 1.22, 95% CI: 0.51–1.93, p = 0.00). There was also evidence of substantial heterogeneity (I2 = 76.9%) (Figure 8). There was evidence of publication bias on both visual inspections of the funnel plot (Figure 9) and from the result of Egger’s test (Egger’s test; b = 2.37, p = 0.020).
Figure 8.
Meta-analysis of the association between medication adherence and place of residence of hypertensive patients, 2020.
Figure 9.
Funnel plot of the odds of an association between medication adherence and knowledge of hypertensive patients in Ethiopia, 2020.
Discussion
Nowadays, addressing medication adherence is considered a major issue in hypertension management that needs to emphasize and get special attention.33 Due to this reason, several studies are carried out to assess the magnitude and associated factors of medication adherence among hypertensive patients in Ethiopia in recent years. After thorough searching and critically evaluating all these studies, we selected 14 studies with a total number of 4938 hypertensive patients. Therefore, this SR and MA synthesized findings of 14 studies that examined the prevalence and factors associated with antihypertensive medication adherence among hypertensive patients in Ethiopia. As per our knowledge, this is the first SR and MA on this topic in Ethiopia. The result of this review has the utmost significance to improve the quality of care for hypertensive patients by showing the summarized magnitude of adherence and suggesting possible strategies to improve the adherence level.
The percentage of medication adherence among hypertensive patients was varied considerably across reports of primary studies that ranged from 31.4% to 89.98%. The overall pooled prevalence of medication adherence in Ethiopia was 65.41% (95% CI: 58.91–71.91). This finding was higher compared with previous SR and MA in developing countries which stated that 47.34% of the hypertensive population were non-adherent to their medication.13 This variation might be due to the difference in medication assessment tools in primary studies included in reviews. Half of the included studies in our review were used as a self-reported questionnaire-based to measure adherence. People may exaggerate their medication adherence while using self-report as a measuring instrument.
One of the main findings of this review was the considerable differences in the adherence percentages due to the methods applied. Considerable variations (I2 = 95.70%) were found in the prevalence of antihypertensive medication adherence based on the type of adherence measurement used in the reviewed studies. For studies using the researcher’s designed questionnaire technique, the pooled prevalence of medication adherence was 69.07% (95% CI: 57.83–80.31, I2 = 93.51). Whereas for studies using MMAS four-items and MMAS eight-items, the pooled prevalence was 68.84% (95% CI: 62.60–75.09, I2 = 81.58) and 60.66% (95% CI: 48.92–72.40, I2 = 97.16), respectively. This MA found that the lowest pooled prevalence was observed among studies using MMAS eight-items. The same result was also reported from an SR and MA of non-adherence to antihypertensive medication in low- and middle-income countries.34 This SR and MA reported a higher non-adherence rate among studies using MMAS eight-item scale with a pooled percentage of 63.35% (95% CI: 38.78–87.91) than studies using the 80% and 90% cut-off scales with a pooled percentage of 25.45% (95% CI: 17.23–33.67). Yet another SR of 25 studies using MMAS eight-items from 15 countries has reported that 45.2% (95% CI: 34.4–56.1, p < 0.001) of hypertensive patients were non-adherence to antihypertensive medications.12
This difference between tools used for adherence measuring might be due to using different cut points in defining the adherence level. Researchers designed questionnaires might have not been sufficiently standardized as MMAS eight-items. The MMAS eight-item scale makes it possible to obtain a more nuanced picture of the adherence, where the participant does not feel forced to claim to be adherent.34 However, the MMAS eight-item scale has been developed in high-income countries which might need to evaluate its reliability and validity before applying in developing countries. MMAS 8 is one of the most widely used self-reported tools for assessing medication adherence among hypertensive patients.35–38 This is because it is simple, cost-effective, and easy to administer in clinical practice.38 Even if it is the widely used self-reported adherence measurement scale, research on its validation and use in the local context is required.39 Due to this requirement, MMAS 8 has been validated in various countries throughout the world.35,37,40–43
Even though, different authors designed and used different types of questionnaires to measure medication adherence in hypertensive patients, there is no internationally accepted gold standard questionnaires.39,44,45 This lack of universally accepted and validated medication adherence measurement can call for the need of conducting research.45 Moreover, each medication adherence scale has advantage and disadvantage. Selecting a suitable adherence scale should depend on the reliability, practicality, cost-effectiveness, acceptability, and convenience to the patient.39,46 Since there is no a perfect adherence measurement scale, using of combination of methods may provide more precise and accurate assessment.46
A holistic assessment of the five dimensions of adherence is crucial to have a comprehensive understanding of factors contributing to sub-optimal adherence in a given country. This comprehensive understanding is mandatory to design, implement, and improve more effective interventions.33 The review found that only a few of the included studies tried to assess all of the five dimensions of adherence. Particularly, the association between medication adherence and healthcare-related factors (distance from the hospital, patient–provider relationship, and cost of medication) was assessed only by a few studies.20,21,24,25,30 Even if a weak health system is one of the major obstacles to tackle hypertension in developing countries, little attention has been given to assess the role of local health systems in the delivery of care for the control of hypertension.13
Factors associated with antihypertensive medication adherence reported in studies included in this review were diverse and described in different ways across the studies. Since only a limited number of studies reporting comparable factors, it was not possible to make an MA for the main factors affecting adherence. Due to this reason, we only included three selected factors such as place of residence, presence of comorbidity and/or complications, and knowledge about hypertension and its management in our MA. These factors were selected because they were reported by many of the included studies in comparable way.
One of the findings of this review was the effect of age on medication adherence which showed conflicting results. Generally, the reviewed studies reported that older patients had more chances to be adherent to their medication than younger patients, but this finding was not conclusive. The same result was also reported in an SR from developing countries which stated that adherence was significantly lower among younger age hypertensive patients in India, Pakistan, and Palestine.13 Whereas elderly patients in Serbia had a significantly lower level of adherence.13 Similarly, older aged hypertensive patients were more adherent than the younger one based on an SR and MA of non-adherence to antihypertensive medication in low- and middle-income countries.34 This association between age and adherence might be related to other factors like knowledge, durations of illness, and the presence of comorbidities that are directly related to age.
This study revealed that the presence of comorbidity and/or complications reduced the likelihood of medication adherence whereas having good knowledge about hypertension and its management increased the chance of medication adherence in hypertensive patients. However, this review revealed that there was no significant association between medication adherence and place of residence (pooled OR = 1.22, 95% CI: 0.51–1.93).
The presence of comorbidities and/or complications was one of the potential barriers that significantly associated with antihypertensive medication adherence. In this study, hypertensive patients with comorbidities and/or complications had 77% lower odds of adherence to antihypertensive medications than patients without comorbidities and/or complications (pooled OR = 0.23, 95% CI: 0.07–0.38). Another SR based on 25 studies from 15 countries also reported that hypertensive patients with comorbidities were significantly non-adherent to antihypertensive medications 31.6% (95% CI: 10.2–97.5, p = 0.045, I2 = 99.1%).12 Similarly, other studies also stated that hypertensive patients with comorbidities have lower chance of adherence to their antihypertensive medications.47–50 The presence of comorbidity influences the medication adherence due to the nature of the comorbidity itself or the medication taken for the comorbidity.50 When hypertensive patients have comorbidities, they are expected to take more medication. This leads to higher pill burden, drug–drug interaction, and medication side effects that can attribute to reduce the chance of medication adherence. Some comorbidities like depression can impair cognitive function of the patients which in turn affects drug-taking behavior.
Knowledge on hypertension is one of the most crucial components of hypertension management among hypertensive patients. The findings of our review also pointed out that the knowledge of hypertensive patients was one of the factors associated with medication adherence. Hypertensive patients with good knowledge had increased odds of adherence to medication (pooled OR = 2.98, 95% CI: 1.72–4.24, p = 0.04). An SR and MA from developing countries stated that being knowledgeable was correlated with an increased likelihood of being adherent.34 Many studies also revealed that knowledge on hypertension is a strong and independent determinant of good medication adherence among hypertensive patients.36,38,47,48,51–57 These studies stated that those hypertensive patients with good knowledge on the disease have higher odds of being adherent to their antihypertensive medication than those with poor knowledge. This might be due to those patients with good knowledge have better understanding about the management of the disease, advantage and importance adherence, and consequences of non-adherence.
Implications for policymakers and clinicians
Our SR and MA provides evidence-based information on the magnitude and factors associated with medication adherence among hypertensive patients in Ethiopia. This knowledge is essential for policymakers, healthcare professionals, patients, and researchers who are interested in enhancing antihypertensive medication adherence.
This article could inform policymakers about the current situation of antihypertensive medication adherence in the country which can help to make evidence-based decisions to improve medication adherence and to tackle factors that negatively affect adherence among hypertensive patients. The findings of this review could help healthcare professionals (nurses, physicians, and pharmacists) to identify factors associated with adherence and to develop well-organized interventions to enhance antihypertensive medication adherence in their practice.
The positive association between level of knowledge and adherence implies the need of continuous educational programs in order to improve hypertensive patients’ awareness about the nature of the disease. Healthcare providers should pay special attention to establish a strong relationship with patients in order to increase knowledge regarding risk factors, complications, and management of hypertension. Therefore, training on communication and counseling skills should be provided to the healthcare workers who provide care for hypertensive patients.
Researchers could use the findings of this review to design appropriate medication adherence assessment methods and techniques which can help them to conduct other research works on the same topic. In addition, this review can give insight to researchers in order to assess the effect or impact of each individual factor on antihypertensive medication adherence. Hypertensive patients are also benefited from this review.
Strengths and weaknesses of the review
The comprehensive search strategy was used to identify relevant studies in the main database like PubMed, Scopus, EMBASE, and Web of Science Core. The PRISMA reporting guidelines were strictly followed for identifying, reporting, and synthesizing this SR and MA. The quality of the included studies was also assessed using standardized measurement, and all articles meet the specified criteria.
We have included 14 studies with a total of 4938 hypertensive patients from all parts of the country except the eastern part which can make this review representative of all patients in the country and the conclusions of this review can be generalizable to the whole population of the country. Through pooling the finding of each of the included studies, this MA provides stronger evidence about the magnitude of antihypertensive medication adherence in Ethiopia. The review assessed all the five dimensions of adherence which can give a comprehensive understanding of factors associated with medication adherence in the country. This can help us to identify a large number of factors associated with antihypertensive medication adherence.
Our review has some methodological limitations. First, we limited our literature search to English languages because English is the medium of communication in higher educational institutions in the country and most of the researchers published their studies in English. Still, it is possible that some suitable studies published in other languages may have been missed. Second, among the selected studies, only one case–control study was found. More case–control studies were desirable to identify more important factors associated with medication adherence. Moreover, all of the included studies were health institution–based studies that may not actually reflect the adherence problem in the community. Since all of the included studies were observational studies, our results were prone to selection bias which is inherent to them.
Third, only half of the included studies were used systematic or simple random sampling techniques while the remaining seven studies selected their study participants using a consecutive sampling technique. This can limit the generalizability of the finding of this review to all hypertensive patients in the country. Fourth, some important factors like sex, educational status, income, social support, BP control level, forgetfulness, alcohol consumption, types of medication, patient–provider relationship, distance from the hospital, and cost of medication were exempted from analysis because they were examined only by a few studies. In addition, the classification of numeric variables like age, number of pills per day, and number of comorbidities was not uniformly across the studies. As a consequence, the effects of these factors in medication adherence may have not been clearly indicated. Finally, heterogeneity in important aspects of the methodology of the selected studies limits the results that can be drawn from the synthesis of the data.
Conclusion
The antihypertensive adherence level among the hypertensive population in Ethiopia was moderate as only two-thirds of patients were adhering to their medication. This SR and MA provide us very crucial insight into factors associated with medication adherence among hypertensive patients. Generally, the reviewed studies showed that hypertensive patients with older age, females, higher educational status, without comorbidities or complications, taking few pills a day, good knowledge about hypertension, and its treatment and favorable attitude had a higher chance to be adherent to their medication. Since all of the included factors showed a positive, negative, and neutral association with adherence, no conclusive relationship could be established between them and antihypertensive medication adherence in Ethiopia.
This MA also provides evidence that the presence of comorbidities and/or complications reduced the odds of adherence whereas having good knowledge about the disease increased chance of adherence to medication among hypertensive patients in Ethiopia. Health service providers and policymakers should take these factors into account to design appropriate intervention strategies to enhance adherence among hypertensive patients. There is also a lack of uniformity of medication adherence assessment methods and techniques across studies in Ethiopia that make it very difficult to synthesize and understand all necessary factors associated with medication adherence in the country. Therefore, we highly recommended for the adoption of validated, contextualized, and standardized medication adherence screening tools with a common definition of adherence.
Footnotes
Author contributions: A.T.G. contributed to the development of the study concept, designing and running electronic literature search, study selection, data extraction, data synthesis, writing manuscript, and final approval of the version submitted. L.D.R. contributed to the development of the study concept, study selection, risk of bias assessment, revision of the manuscript, and final approval of the version submitted. A.B.W. contributed to the study selection, risk of bias assessment, revision of the manuscript, and final approval of the version submitted. B.T.M. contributed to the study selection, risk of bias assessment, revision of the manuscript, and final approval of the version submitted. N.L. contributed to the study selection, revision of the manuscript, and final approval of the version submitted. B.S.T. contributed to the study selection, risk of bias assessment, revision of the manuscript, and final approval of the version submitted. All the authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was not sought for this study because this was a review article and did not involve any patients.
Informed consent: Informed consent was not sought for this study because this was a review article and did not involve any subjects.
ORCID iD: Assefa Tola Gemeda  https://orcid.org/0000-0002-2155-6097
https://orcid.org/0000-0002-2155-6097
Data availability: All data generated or analyzed during this study are included in this published article.
References
- 1. WHO. Global non-communicable diseases target: reduce high blood pressure. Geneva, Switzerland: World Health Organization, 2016. [Google Scholar]
- 2. WHO. A global brief on hypertension: silent killer, global public health crisis: world health day 2013. Geneva, Switzerland: World Health Organization, 2013. [Google Scholar]
- 3. WHO. Hypertension. Geneva, Switzerland: World Health Organization, 2019. [Google Scholar]
- 4. van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa—Consultative review for the 6th session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J 2013; 16: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ataklte F, Erqou S, Kaptoge S, et al. Burden of undiagnosed hypertension in Sub-Saharan Africa: a systematic review and meta-analysis. Hypertension 2015; 65(2): 291–298. [DOI] [PubMed] [Google Scholar]
- 6. Angaw K, Dadi AF, Alene KA. Prevalence of hypertension among federal ministry civil servants in Addis Ababa, Ethiopia: a call for a workplace-screening program. BMC Cardiovasc Disord 2015; 15(1): 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roba HS, Beyene AS, Mengesha MM, et al. Prevalence of hypertension and associated factors in dire Dawa city, Eastern Ethiopia: a community-based cross-sectional study. Int J Hypert 2019; 2019: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gosmanova EO, Kovesdy CP. Adherence to antihypertensive medications: is prescribing the right pill enough? Nephrol Dial Transpl 2014; 30(10): 1649–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abebe SM, Berhane Y, Worku A, et al. Prevalence and associated factors of hypertension: a crossectional community based study in Northwest Ethiopia. PLoS ONE 2015; 10(4): e0125210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Agbor VN, Takah NF, Aminde LN. Prevalence and factors associated with medication adherence among patients with hypertension in sub-Saharan Africa: protocol for a systematic review and meta-analysis. BMJ Open 2018; 8(3): e020715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sabaté E. Adherence to long-term therapies: evidence for action. Geneva, Switzerland: World Health Organization, 2003. [Google Scholar]
- 12. Abegaz TM, Shehab A, Gebreyohannes EA, et al. Nonadherence to antihypertensive drugs a systematic review and meta-analysis. Medicine 2017; 96(4): e5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dhar L, Dantas J, Ali M. A systematic review of factors influencing medication adherence to hypertension treatment in developing countries. Open J Epidemiol 2017; 07: 211–250. [Google Scholar]
- 14. Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health 2008; 11(1): 44–47. [DOI] [PubMed] [Google Scholar]
- 15. Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 2012; 73(5): 691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. Am J Nurs 2014; 114(6): 47–52. [DOI] [PubMed] [Google Scholar]
- 17. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014; 12(12): 1495–1499. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21(11): 1539–1558. [DOI] [PubMed] [Google Scholar]
- 19. Ali M, Bekele M, Teklay G. Antihypertensive medication non-adherence and its determinants among patients on follow up in public hospitals in Northern Ethiopia. Int J Clin Trials 2014; 1: 95. [Google Scholar]
- 20. Ambaw AD, Alemie GA, Yohannes SM, et al. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health 2012; 12: 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Asgedom SW, Atey TM, Desse TA. Antihypertensive medication adherence and associated factors among adult hypertensive patients at Jimma University Specialized Hospital, southwest Ethiopia. BMC Res Notes 2018; 11(1): 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bekele F. Non-compliance and its associated factors among hypertensive patients taking anti-hypertensive treatment visiting Gimbi general hospital Western Ethiopia: cross-sectional study. J Pharm Pharm 2019; 6(2): 65–71. [Google Scholar]
- 23. Berisa HD, Dedefo MG. Non-adherence related factors to antihypertensive medications among hypertensive patients on follow up at Nedjo General Hospital in west Ethiopia. Open Public Health J 2018; 11: 62–71. [Google Scholar]
- 24. Chelkeba L, Dessie S. Antihypertension medication adherence and associated factors at Dessie Hospital, North East Ethiopia, Ethiopia. Int J Res Med Sci 2013; 1(3): 101–107. [Google Scholar]
- 25. Dego TR, Bobasa EM. Adherence to anti-hypertensive medication and contributing factors among non-comorbid hypertensive patients in two hospitals of Jimma town, south west Ethiopia. Gulhane Medical Journal 2016; 58(1): 060–066. [Google Scholar]
- 26. Demisew T, Mahmud S, Kechalew T. A cross sectional study to observe adherence to antihypertensive treatment and associated factors among hypertensive patient on follow up in Debre Berhan Referral Hospital, North Shoa, Ethiopia, 2017. J Cardiovasc Dis Diagnos 2018; 06: 1000321. [Google Scholar]
- 27. Gebreyohannes EA, Bhagavathula AS, Abebe TB, et al. Adverse effects and non-adherence to antihypertensive medications in University of Gondar Comprehensive Specialized Hospital. Clin Hypertens 2019; 25: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Getenet A, Tesfa M, Ferede A, et al. Determinants of adherence to anti-hypertensive medications among adult hypertensive patients on follow-up in Hawassa Referral Hospital: A case–control study. JRSM Cardiovasc Dis 2019; 8: 2048004019892758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hareri H, Gedefaw M, Simeng B. Original research article assessment of prevalence and associated factors of adherence to anti-hypertensive agents among adults on follow up in Adama Referral Hospital, East Shoa, Ethiopia-cross sectional study. Int J Curr Microbiol App Sci 2014; 3: 760–770. [Google Scholar]
- 30. Mekonnen HS, Gebrie MH, Eyasu KH, et al. Drug adherence for antihypertensive medications and its determinants among adult hypertensive patients attending in chronic clinics of referral hospitals in Northwest Ethiopia. BMC Pharmacol Toxicol 2017; 18(1)27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Teshome DF, Bekele KB, Habitu YA, et al. Medication adherence and its associated factors among hypertensive patients attending the Debre Tabor General Hospital, northwest Ethiopia. Integr Blood Press Control 2017; 10: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tibebu A, Mengistu D, Bulto LN. Adherence to prescribed antihypertensive medications and associated factors for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Int J Health Sci 2017; 11(4): 47–52. [PMC free article] [PubMed] [Google Scholar]
- 33. Burnier M, Egan B. Adherence in hypertension: a review of prevalence, risk factors, impact, and management. Circ Res 2019; 124: 1124–1140. [DOI] [PubMed] [Google Scholar]
- 34. Nielsen JO, Shrestha AD, Neupane D, et al. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens 2017; 31(1): 14–21. [DOI] [PubMed] [Google Scholar]
- 35. de Oliveira-Filho AD, Morisky DE, Neves SJ, et al. The 8-item Morisky medication adherence scale: validation of a Brazilian–Portuguese version in hypertensive adults. Res Social Adm Pharm 2014; 10(3): 554–561. [DOI] [PubMed] [Google Scholar]
- 36. Shankar SP, Suman Babu ISS, Ramya N. A study on usefulness of modified medication adherence scale in assessing adherence among hypertensive patients. Perspect Clin Res 2019; 10(4): 163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Labaran K, Mohammed S, Maiha B, et al. Validity evidence of adapted Hausa version of 8-item Morisky medication adherence scale in patients with hypertension in North-Western Nigeria. Bayero J Pure Appl Sci 2018; 11(1): 244–250. [Google Scholar]
- 38. Jankowska-Polanska B, Uchmanowicz I, Dudek K, et al. Relationship between patients’ knowledge and medication adherence among patients with hypertension. Patient Prefer Adherence 2016; 10: 2437–2447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nguyen La, Caze A, Cottrell N. What are validated self-report adherence scales really measuring?: a systematic review. Br J Clin Pharmacol 2014; 77(3): 427–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Perez-Escamilla B, Franco-Trigo L, Moullin JC, et al. Identification of validated questionnaires to measure adherence to pharmacological antihypertensive treatments. Patient Prefer Adherence 2015; 9: 569–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Al-Qazaz HK, Hassali MA, Shafie AA, et al. The eight-item Morisky Medication Adherence Scale MMAS: translation and validation of the Malaysian version. Diabetes Res Clin Pract 2010; 90(2): 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Asilar RH, Gozums S, Capik C, et al. Reliability and validity of the Turkish form of the eight-item Morisky medication adherence scale in hypertensive patients. Anadolu Kardiyol Derg 2014; 14(8): 692–700 [DOI] [PubMed] [Google Scholar]
- 43. Lee GK, Wang HH, Liu KQ, et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PLoS ONE 2013; 8(4): e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Plakas S, Mastrogiannis D, Mantzorou M, et al. Validation of the 8-item Morisky Medication Adherence Scale in chronically ill ambulatory patients in rural Greece. Open J Nurs 2016; 6(03): 158. [Google Scholar]
- 45. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int 2015; 2015: 217047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hawkshead J, Krousel-Wood MA. Techniques for measuring medication adherence in hypertensive patients in outpatient settings. Dis Manag Health Out 2007; 15(2): 109–118. [Google Scholar]
- 47. Algabbani FM, Algabbani AM. Treatment adherence among patients with hypertension: findings from a cross-sectional study. Clin Hypertens 2020; 26: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ghembaza MA, Senoussaoui Y, Tani MK, et al. Impact of patient knowledge of hypertension complications on adherence to antihypertensive therapy. Curr Hypertens Rev 2014; 10(1): 41–48. [DOI] [PubMed] [Google Scholar]
- 49. Monane M, Bohn RL, Gurwitz JH, et al. The effects of initial drug choice and comorbidity on antihypertensive therapy compliance: results from a population-based study in the elderly. Am J Hypertens 1997; 10(7 Pt 1): 697–704. [DOI] [PubMed] [Google Scholar]
- 50. Saadat Z, Nikdoust F, Aerab-Sheibani H, et al. Adherence to antihypertensives in patients with comorbid condition. Nephrourol Mon 2015; 7(4): e29863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Abu H, Aboumatar H, Carson KA, et al. Hypertension knowledge, heart healthy lifestyle practices and medication adherence among adults with hypertension. Eur J Pers Cent Healthc 2018; 6(1): 108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Boima V, Ademola AD, Odusola AO, et al. Factors associated with medication nonadherence among hypertensives in Ghana and Nigeria. Int J Hypertens 2015; 2015: 205716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hashmi SK, Afridi MB, Abbas K, et al. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS ONE 2007; 2(3): e280–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lulebo AM, Mutombo PB, Mapatano MA, et al. Predictors of non-adherence to antihypertensive medication in Kinshasa, Democratic Republic of Congo: a cross-sectional study. BMC Res Notes 2015; 8: 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Mekonnen GB, Gelayee DA. Low medication knowledge and adherence to oral chronic medications among patients attending community pharmacies: a cross-sectional study in a low-income country. Biomed Res Int 2020; 2020: 4392058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Najjar A, Amro Y, Kitaneh I, et al. Knowledge and adherence to medications among Palestinian Geriatrics Living with chronic diseases in the West Bank and East Jerusalem. PLoS ONE 2015; 10(6): e0129240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Salama A, Yasin AE-R, Elbarbary W. Medication knowledge as a determinant of medication adherence in geriatric patients, Serse Elian City, Menoufia Governorate, Egypt. Menoufia Med J 2017; 30(1): 63–68. [Google Scholar]