Abstract
Anaemia and underweight or overweight/obesity are major public health problems driving maternal and child mortality in low- and middle-income countries. While the burden of these conditions is recognised, the evidence for the co-occurrence of these conditions is fragmented and mixed, especially at the individual level. Further, many studies have focused on families and communities. The different pathways for the occurrence of anaemia and BMI challenges indicate that an individual can potentially live with both conditions and suffer the complications. This study examined the prevalence and factors associated with the co-occurrence of anaemia and BMI challenges among a cohort of women in Ghana. Data from the 2014 Ghana Demographic and Health Survey were used. The sample size was 4 337 women aged 15–49 years who were not pregnant during the survey. Women who suffered simultaneously from underweight or overweight/obesity and anaemia were considered as having the double burden of malnutrition. The data were analysed using descriptive statistics, Chi-square test and logistic regression in STATA. One-fifth of the participants were overweight (21%), 4% were underweight and about one-tenth were obese (12%). The prevalence of anaemia was 41%. Only one in three women had normal weight and was not anaemic (34%). About 14% of the women experienced the double burden of malnutrition. Being overweight and anaemic (57%) was the most common form of this double burden. Age, marital status, parity, and wealth were t key risk factors associated with the double burden of malnutrition. The findings from this study show that women experience multiple nutritional challenges concurrently and that only a few women had healthy nutritional status. This information is particularly important and can be introduced into health education programmes to help address misconceptions about body weight and health.
Introduction
Several countries are facing a double burden of nutrition-related diseases, namely the coexistence of undernutrition or overnutrition and micronutrient deficiency in the same individual, household, community and population [1]. Anaemia is known to be one of the major micronutrient deficiencies [2]. Anaemia is associated with high maternal and infant mortality and reduced productivity [3, 4]. While the prevalence of stunting is decreasing significantly, overweight/obesity in all age groups is increasing [5]. The double burden of malnutrition causes great economic and health stress for governments, households and individuals [3]. Most countries are struggling with addressing the double burden of anaemia and underweight or overweight/obesity, as reported by the 2018 Global Nutrition Report [6].
Women have a higher burden of anaemia and underweight or overweight/obesity compared to men [7, 8]. Many women experience anaemia due to malaria, helminthic infection, pregnancy and nursing [9, 10]. Anaemia prevalence among women attending antenatal clinics ranged from 22% in Uganda [9] to 66% in the Dangme East area of Ghana [11]. In South Africa, 68% of women were overweight/obese compared to 41% of men [12]. This gender difference in malnutrition is further worsened by the effects of age, parity, wealth and urbanisation [13].
Previous studies have reported a strong correlation between body mass index (BMI) status and anaemia among women [14, 15]. While underweight is positively related to anaemia, the results of the relationship between overweight/obesity and anaemia are mixed. Among Indonesian and Ghanaian pregnant women, those with a high BMI were less likely to be anaemic [16], but in Mexico, obese women were more likely to be anaemic [17]. In Iran, there was no association between overweight/obesity and anaemia [18]. However, evidence of the association between BMI status and anaemia among non-pregnant women is non-existent in the Ghanaian context. Therefore, this study was conducted to examine the coexistence of anaemia and underweight or overweight/obesity in Ghana.
The prevalence of anaemia among women is high in Ghana [19]. In the Ashanti region, more than half of women are anaemic [20]. At the same time, overweight and obesity have been increasing in the country. Using the World Health Organization Study on AGEing and adult health (SAGE) data, it was estimated that about 20% and 10% were overweight and obese in 2007/08, respectively. In 2014/15, the proportion who were overweight and obese among this sample had increased to 24% and 16%, respectively [21].
However, research and intervention concerning anaemia and BMI challenges have been condition specific [22, 23]. Little attention has been given to the coexistence of these nutritional challenges among women, even though many women are reported to suffer from both anaemia and a BMI that is too low or high. Due to the preference for large body size in certain cultures, some women may be unaware of the micronutrient deficiencies that they may be suffering from [24]. This complex double burden underscores the importance of understanding how underweight or overweight/obesity and anaemia coexist among vulnerable populations. Also, the study of the double burden of malnutrition has primarily focused on the household level by examining the co-occurrence of overnutrition among mothers and undernutrition among their children [1]. This study examined the coexistence of anaemia and BMI challenges among women using the 2014 Ghana Demographic and Health Survey. The findings are essential for tracking efforts towards achieving the 2025 global nutrition targets.
Methods
Source of data
Cross-sectional data were retrieved from the 2014 Ghana Demographic and Health Survey, a nationally representative household survey of Ghana. The survey was carried out by the Ghana Statistical Service, the Ghana Health Service and the National Public Health Reference Laboratory of the Ghana Health Service. The protocol of the study, including the biomarker component, was reviewed and approved by the Ghana Health Service Ethical Review Committee and the Institutional Review Board of ICF International.
The 2014 Ghana Demographic and Health Survey used a two-stage sampling approach. The first stage selected 427 enumeration areas identified from the 2010 Ghana Population and Housing Census [25]. The households in the enumeration areas were listed. About 30 households were randomly selected from the enumeration areas. Field work for the survey was carried out from September to December 2014. The survey collected data on the fertility, socioeconomic status, health status and nutritional status of participating households and individuals using the Demographic and Health Survey Phase VI core questionnaire. All women aged 15–49 from the selected households were eligible to be interviewed. Data on anthropometry (weight and height) and haemoglobin were gathered for 4 528 women who consented. In this study, the sample was limited to 4 337 women who had complete data for all the variables of interest and were not pregnant at the time of the survey.
Measurements
During the survey, blood samples were collected from women via finger prick. Haemoglobin concentration was analysed using a battery-operated portable HemoCue analyser. Participants with altitude-adjusted Hb < 120 g/dl were classified as anaemic, while those with Hb > 120 g/dl were classified as not anaemic. Besides, height and weight were measured. The BMI of the women was computed by dividing weight in kilograms by height in metres squared (kg/m2). Using the standard World Health Organization’s cut-off points, BMI categories were defined as underweight (< 18.5 kg/m2), normal weight (18.5–24.99.0 kg/m2), overweight (25.0–29.9 kg/m2) and obese (≥ 30.0 kg/m2) [26]. A dependent variable called nutritional status was created using anaemia and BMI status. Women who simultaneously were anaemic and underweight or overweight/obesity were considered as having the double burden of malnutrition. This included women who were 1) both anaemic and underweight; 2) both anaemic and overweight; and 3) both anaemic and obese. Women who were only 1) not anaemic; 2) underweight; 3) normal weight; 4) overweight; and 5) obese were classified as not having the double burden of malnutrition.
The covariates that were examined in this study included age, place of residence, educational attainment, ethnicity, marital status, parity, household wealth, breastfeeding status and fruit and vegetable intake. The age of respondents was categorised into 10-year age groups: 15–24, 25–34, 35–44 and 45–49 years. Place of residence was defined as urban or rural. Educational attainment was categorised as none (no formal education), primary, secondary and higher. Ethnicity was defined as Akan, Ga-Dangme, Ewe, Mole-Dagbani or other. Marital status was categorised as never married, currently married or formerly married. The parity of women was defined as the number of children ever borne. Household wealth was determined from household asset data using principal component analysis. The list of household assets used included household assets (such as television, bicycle, and iron) as well as characteristics of the dwelling place such as source of drinking water, sanitation facilities and type of flooring material. Household wealth was equally divided into five groups to create wealth quintiles, namely poorest, poor, middle, richer and richest. The number of days per week that participants had fruit and vegetables to eat was recorded as 0–7.
Analysis
Descriptive statistics including means, frequencies and percentages were computed for all the variables. Cross-tabulations with Chi-square tests were used to show variation in nutritional status and the independent variables. To examine the independent effect of the covariates, we conducted a logistic regression. Odds ratios were calculated to examine the probability of experiencing the double burden of malnutrition, controlling for other factors. The odds ratios, confidence intervals and P-values were reported. The level of significance was set at P < 0.05. The data were weighted before analysis using the Demographic and Health Surveys women’s individual sample weights. The survey weight in STATA was set up using the generated weighting variable, primary sampling unit and strata. These were then applied in all the analyses. Multicollinearity was tested for using the variance inflation factor (VIF) and tolerance. The results of the VIF test are shown in S1 File. None of the VIF values is greater than 10, and the tolerance values are less than 0.1; therefore, there are no signs of multicollinearity. The analysis was conducted in STATA.
Results
Characteristics of respondents
A total of 4 337 women were involved in this study. The mean age was 30 ± 9.9 years, and about half of them (50%) lived in urban areas (Table 1). About half of them had a secondary school education (52%). The majority of the respondents were currently married (56%), and two thirds were Akan (44%). About one-fifth of the participants belonged to households in the richest wealth quintiles (17%). The number of children ever born ranged between 0 and 13 among the women (2.49±2.47).
Table 1. Sociodemographic characteristics of respondents.
| Variable | Frequency | Percent |
|---|---|---|
| Age | ||
| 15–24 | 1 570 | 36.2 |
| 25–34 | 1 258 | 20.0 |
| 35–44 | 1 092 | 25.2 |
| 45–49 | 417 | 9.6 |
| Place of residence | ||
| Urban | 2 138 | 49.3 |
| Rural | 2 199 | 50.7 |
| Level of education | ||
| No education | 1 050 | 24.2 |
| Primary | 829 | 19.1 |
| Secondary | 2 240 | 51.7 |
| Higher | 218 | 5.0 |
| Marital status | ||
| Never married | 1 447 | 33.4 |
| Currently married | 2 442 | 56.3 |
| Formerly married | 448 | 10.3 |
| Ethnicity | ||
| Akan | 1 905 | 43.9 |
| Ga-Dangme | 238 | 5.5 |
| Ewe | 511 | 11.8 |
| Mole-Dagbani | 1 607 | 37.0 |
| Other | 76 | 1.8 |
| Wealth quintile | ||
| Poorest | 1 105 | 25.5 |
| Poorer | 792 | 18.3 |
| Middle | 893 | 20.6 |
| Richer | 813 | 18.7 |
| Richest | 734 | 16.9 |
| Parity (mean) | 2.49 (± 2.47) | |
| Fruit consumption, days per week (mean) | 3.45 (± 2.56) | |
| Vegetable consumption, days per week (mean) | 3.42 (± 2.41) | |
| Total | 4 337 | 100.0 |
Nutritional status of respondents
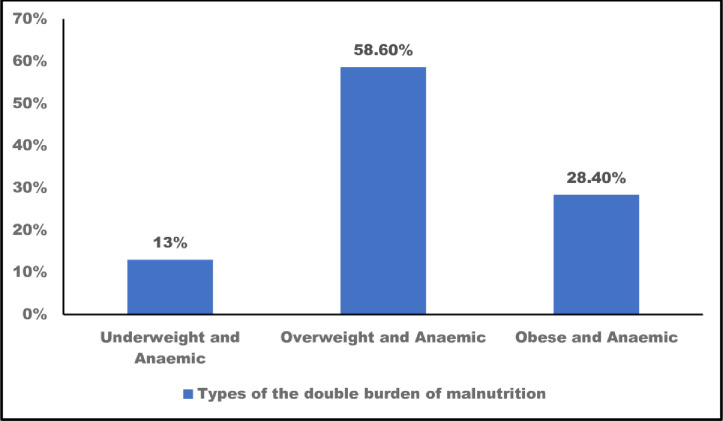
The nutritional status of respondents is shown in Table 2. About two-fifths of the respondents were anaemic (41%). Based on the BMI classification, 61% were of normal weight and about 4% were underweight. About one in five of the women was overweight (23%), and 12% were obese. Only one in three women was normal weight and not anaemic (34%). Slightly more than 14% of the women had the double burden of malnutrition. As shown in Fig 1, being overweight and anaemic was the most common form of this double burden (59%),
Table 2. Nutritional status of respondents.
| Nutritional status | Percent | Frequency |
|---|---|---|
| Anaemia status | ||
| Anaemic | 41.4 | 1 795 |
| Not anaemic | 58.6 | 2 542 |
| Body mass index | ||
| Underweight | 3.6 | 158 |
| Normal weight | 61.1 | 2 650 |
| Overweight | 22.8 | 990 |
| Obese | 12.4 | 539 |
| Nutritional status | ||
| Double burden | 14.2 | 616 |
| No double burden | 85.8 | 3 721 |
| Nutritional status (breakdown) | ||
| Underweight and not anaemic | 1.8 | 78 |
| Underweight and anaemic | 1.8 | 80 |
| Normal weight and not anaemic | 33.9 | 1 471 |
| Normal weight and anaemic | 27.2 | 1 179 |
| Overweight and not anaemic | 14.5 | 629 |
| Overweight and anaemic | 8.3 | 361 |
| Obese and not anaemic | 8.4 | 364 |
| Obese and anaemic | 4.1 | 175 |
| Total | 100 | 4 337 |
Fig 1. Types of the double burden of malnutrition among women in Ghana (n = 616).
Distribution of nutritional status by background characteristics
Table 3 displays the percent distribution of the double burden of malnutrition according to background characteristics among women in Ghana. Particularly, older women showed a significantly higher prevalence of the double burden compared with younger individuals. For example, about 9% of the 15-24-year-old women showed no double burden compared to 19% of those aged 35–44 years (P = 0.000). The proportion of women who had the double burden was higher in urban areas (17%) than in rural areas (11%). Higher education did not have a protective effect on nutritional status. The proportion of women living with the double burden increased from 11% among those with no education to 17% among those with higher education. The double burden was higher among formerly married (22%) women than among those who had never married (9%) and those who were currently married (15%). Regarding wealth, women from poor households had a lower proportion of respondents with double burden (8%) than those from richer households (20%). The mean number of children ever born was higher among women with the double burden (2.8 ± 2.4) compared to their counterparts (2.4 ± 2.5). The mean number of days per week of fruit and vegetable consumption was similar among the women.
Table 3. Percent distribution of the double burden of malnutrition.
| Variable | Double burden | No double burden | P-value |
|---|---|---|---|
| Age | |||
| 15–24 | 8.8 | 91.2 | 0.000 |
| 25–34 | 15.9 | 84.1 | |
| 35–44 | 19.3 | 80.7 | |
| 45–49 | 16.1 | 83.9 | |
| Place of residence | 0.000 | ||
| Urban | 17.1 | 82.9 | |
| Rural | 11.4 | 88.6 | |
| Level of education | 0.008 | ||
| No education | 11.0 | 88.9 | |
| Primary | 14.6 | 85.4 | |
| Secondary | 15.2 | 84.8 | |
| Higher | 17.4 | 82.6 | |
| Currently breastfeeding | 0.140 | ||
| No | 14.6 | 85.3 | |
| Yes | 12.8 | 87.2 | |
| Marital status | 0.000 | ||
| Never married | 9.2 | 90.8 | |
| Currently married | 15.6 | 84.4 | |
| Formerly married | 22.5 | 77.5 | |
| Ethnicity | 0.000 | ||
| Akan | 16.1 | 83.9 | |
| Ga-Dangme | 19.8 | 80.2 | |
| Ewe | 17.6 | 82.4 | |
| Mole-Dagbani | 9.8 | 90.2 | |
| Other | 18.4 | 81.6 | |
| Wealth quintile | 0.000 | ||
| Poorest | 7.6 | 92.4 | |
| Poorer | 13.4 | 86.6 | |
| Middle | 15.7 | 84.3 | |
| Richer | 16.7 | 83.3 | |
| Richest | 20.4 | 79.6 | |
| Parity | 2.1 ± 1.69 | 1.8 ± 1.69 | 0.000 |
| Fruit consumption, days per week | 3.4 ± 2.6 | 3.4 ± 2.6 | 0.400 |
| Vegetable consumption, days per week | 3.4 ± 2.40 | 3.4 ± 2.49 | 0.449 |
Correlates of nutritional status
The correlates of the double burden of malnutrition are presented in Table 4. After controlling for other factors, the variables that were significantly related to nutritional status were age, marital status, wealth and parity. The odds of having the double burden of malnutrition was significantly higher for women aged 35–44 years compared to those aged 15–24 years (OR = 1.54; 95% CI = 1.09, 2.12). Compared with women who had never married, women who were formerly married were twice as likely to have the double burden of malnutrition (OR = 2.03; 95% CI = 1.37, 3.01). Household wealth was associated with the double burden of malnutrition–women who belonged to households of the middle (OR = 2.10; 95% CI = 1.44, 3.06), richer (OR = 2.14, 95% CI = 1.38, 3.32) and richest (OR = 2.75; 95% CI = 1.73–4.37) wealth quintiles had significantly higher odds of experiencing the double burden of malnutrition. Every additional birth also increased the odds of the double burden of malnutrition (OR = 1.06; 95% CI = 1.00–1.12).
Table 4. Correlates of the double burden of malnutrition among women in Ghana.
| Variable | Odds ratio | 95% Confidence interval | P-value |
|---|---|---|---|
| Age | |||
| 15–24 (ref) | |||
| 25–34 | 1.39 | 1.05–1.86 | 0.022 |
| 35–44 | 1.54 | 1.09–2.12 | 0.013 |
| 45–49 | 1.13 | 0.71–1.82 | 0.597 |
| Place of residence | |||
| Urban (ref) | |||
| Rural | 1.01 | 0.84–1.43 | 0.497 |
| Level of education | |||
| No education (ref) | |||
| Primary | 1.14 | 0.85–1.53 | 0.367 |
| Secondary | 1.20 | 0.92–1.56 | 0.179 |
| Higher | 1.18 | 0.73–1.91 | 0.488 |
| Currently breastfeeding | |||
| No (ref) | |||
| Yes | 0.89 | 0.70–1.15 | 0.393 |
| Marital status | |||
| Never married (ref) | |||
| Currently married | 1.42 | 1.05–1.92 | 0.020 |
| Formerly married | 2.03 | 1.37–3.01 | 0.000 |
| Ethnicity | |||
| Akan (ref) | |||
| Ga-Dangme | 1.32 | 0.95–1.84 | 0.900 |
| Ewe | 1.30 | 0.97–1.75 | 0.075 |
| Mole-Dagbani | 0.93 | 0.71–1.22 | 0.616 |
| Other | 1.20 | 0.59–2.44 | 0.595 |
| Wealth quintile | |||
| Poorest (ref) | |||
| Poorer | 1.72 | 1.26–2.35 | 0.001 |
| Middle | 2.10 | 1.44–3.06 | 0.000 |
| Richer | 2.14 | 1.38–3.32 | 0.001 |
| Richest | 2.75 | 1.73–4.37 | 0.000 |
| Parity | 1.06 | 1.00–1.12 | 0.045 |
| Fruit consumption, days | 0.99 | 0.95–1.03 | 0.793 |
| Vegetable consumption, days | 0.99 | 0.96–1.04 | 0.959 |
ref: Reference group.
Discussion
The double burden of anaemia and underweight or overweight/obesity affects women disproportionately. However, research interventions have not focused on the co-occurrence of anaemia and BMI challenges among women. This study examined the co-occurrence of anaemia and BMI challenges and the associated risk factors among women in Ghana. The overall prevalence of anaemia was 41% and that of obesity was 12%. Only 34% of women had normal weight and were not anaemic. The findings indicate that 14% of women had the double burden of malnutrition. Among these women, being overweight and anaemic was the most common situation. The prevalence of the double burden of malnutrition was strongly correlated with age, marital status, parity and wealth.
It has been reported that the prevalence of the double burden of malnutrition at the household level is high in low- and middle-income countries, especially in sub-Saharan Africa [5]. The prevalence of the within-person double burden of underweight or overweight/obesity and anaemia found in this study (14%) was lower than what had been estimated for Kenya (19%) [27] and India (23%) [28]. Even though the prevalence of the individual-level double burden reported in this study is relatively low, about half of the women were overweight and anaemic. This indicates that a high proportion of women are experiencing both undernutrition and overnutrition simultaneously.
In studies that focused on predicting either obesity or anaemia, age, marital status, wealth and parity have been reported as risk factors [12, 20, 29]. These variables are biological and demographic risk factors as well as indicators of socioeconomic status. Age and parity are leading risk factors of maternal malnutrition. Pregnancy and the postpartum period result in substantial demands for iron, which accounts for the biological vulnerability of women to anaemia. For example, during pregnancy, enlargement of red-cell mass and the development and maintenance of the placenta increase iron requirements substantially from 0.8 mg per day in the first trimester to 7.5 mg per day in the third trimester [30]. At the same time, pregnancy and postpartum food cultures increase the risk of obesity among women. Wealthy individuals have access to a wider diversity of nutrient-limited foods and report high intake of fat-rich and sugar-rich diets. In Nigeria, women from rich households consume fast foods at least twice a week [31].
Furthermore, weight management practices among women can explain the results of the study. Weight loss is one of the negative effects of anaemia [32]. For cultural reasons, women often attach great importance to appearance and are preoccupied with their weight at a very early age. In some cultures, the plump woman is idealised, as it is perceived to be preferred by men [33]. In African countries, including Ghana, a plump woman is considered as wealthy and happy [24, 34]. As a result, weight gain has minimal negative connotations and is a cultural solution to anaemia [35, 36]. In an attempt to treat anaemia, the majority of women resort to weight management practices such as intake of appetite-stimulating supplements that predispose them to overweight and obesity [37]. However, gaining additional body fat may prevent iron homeostasis and increase the risk of anaemia. It is reported that obese individuals have an impaired ability to absorb iron. Among women in Chile, it was reported that obese women (20%) had lower iron absorption levels compared to normal-weight women (33%) [15].
To the best of our knowledge, this study is the first of its kind to provide empirical evidence of the within-person double burden of malnutrition with nationally representative data from Ghana. The findings also highlight the risk factors that predispose women to the double burden of malnutrition. Although this study used a nationally representative dataset and controlled for other factors, the findings should be interpreted in the light of its limitations. Firstly, this study was cross-sectional and collected data at a single time point. We cannot make a causal claim about the observed associations between anaemia and underweight or overweight/obesity and the concomitant risk factors. Secondly, detailed dietary consumption data were not collected for women during the 2014 survey as was the case in the 2008 survey [38, 39]. The only available information was the number of days per week of consuming vegetables and fruit; the type and quantity of fruit and vegetables consumed were not measured. We recommend that future versions of the Ghana Demographic and Health Survey include detailed questions on fruit and vegetable intake among women.
Conclusion
There is a gap in research on the prevalence of and the factors that influence the within-person double burden of malnutrition among African women. Our study suggests that Ghanaian women simultaneously experience underweight or overweight/obesity and anaemia and that only a few have a healthy nutritional status. The co-occurrence of overweight and anaemia was the most common form of the double burden of malnutrition. Age, marital status, parity and wealth were the key risk factors associated with the double burden of malnutrition. The pathways through which these risk factors influence the double burden of malnutrition are unhealthy lifestyles, especially poor diet, physical inactivity and inadequate weight management behaviours. These factors are potentially modifiable through educational efforts targeting women and social norms. Future research should focus on addressing beliefs about body weight and anaemia. Such research can develop culturally sensitive educational content on pregnancy and breastfeeding food beliefs. Also, these interventions should be delivered at the individual and community level. Lastly, such research can investigate the impact of these efforts on body weight and anaemia outcomes.
Supporting information
(DOCX)
Acknowledgments
The authors are grateful to the Demographic and Health Survey programme and the Ghana Statistical Service for giving us access to the 2014 Ghana Demographic and Health Survey data. The authors are grateful to the reviewers and academic editors for their critical comments.
Data Availability
Data are available from the Measure Demographic and Health Survey program (visit https://www.dhsprogram.com/data/) for researchers who meet the criteria for access to confidential data. The data is labeled Ghana: Standard DHS, 2014 and can be found through the following link: https://dhsprogram.com/methodology/survey/survey-display-437.cfm.
Funding Statement
Sandra Boatemaa Kushitor was supported by the Dean’s Division, Faculty of AgriSciences, Stellenbosch University, Stellenbosch, South Africa.
References
- 1.Kimani-Murage EW, Muthuri SK, Oti SO, Mutua MK, van de Vijver S, Kyobutungi C. Evidence of a double burden of malnutrition in urban poor settings in Nairobi, Kenya. PLoS One. 2015;10: e0129943 10.1371/journal.pone.0129943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Nutrition Report. 2020 Global Nutrition Report: Action on equity to end malnutrition. Bristol UK; 2020. Available: https://globalnutritionreport.org/
- 3.Ezzati M, Lopez AD, Rodgers AA, Murray C. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva, Switzerland:; 2015. Available: https://apps.who.int/iris/handle/10665/42770
- 4.Horton S, Ross J. The economics of iron deficiency. Food Policy. 2003;28: 51–75. [Google Scholar]
- 5.Onyango AW, Jean-Baptiste J, Samburu B, Mahlangu TLM. Regional overview on the double burden of malnutrition and examples of program and policy responses: African Region. Ann Nutr Metab. 2019;75: 127–130. 10.1159/000503671 [DOI] [PubMed] [Google Scholar]
- 6.IFPRI. Global nutrition report 2018. New York; 2019. Available: https://globalnutritionreport.org/reports/global-nutrition-report-2018/executive-summary/
- 7.Swinburn B a, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378: 804–14. 10.1016/S0140-6736(11)60813-1 [DOI] [PubMed] [Google Scholar]
- 8.Minicuci N, Biritwum RB, Mensah G, Yawson AE, Naidoo N, Chatterji S, et al. Socio demographic and socioeconomic patterns of chronic non-communicable disease among the older adult population in Ghana. Glob Health Action. 2014;7: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Obai G, Odongo P, Wanyama R. Prevalence of anaemia and associated risk factors among pregnant women attending antenatal care in Gulu and Hoima Regional Hospitals in Uganda: A cross sectional study. BMC Pregnancy Childbirth. 2016;16: 1–7. 10.1186/s12884-015-0735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gedefaw L, Ayele A, Asres Y, Mossie A. Anaemia and associated factors among pregnant women attending antenatal care in clinic Wolayita Soso town, Southern Ethiopia. Ethiop J Heal Sci. 2015;25: 10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tay SCK, Nani EA, Walana W. Parasitic infections and maternal anaemia among expectant mothers in the Dangme East District of Ghana. BMC Res Notes. 2017;10: 1–9. 10.1186/s13104-016-2345-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agyemang C, Boatemaa S, Agyemang G, de-Graft Aikins A. Obesity in Sub-Saharan Africa. In: Ahima R, editor. Metabolic syndrome Cham: Springer International Publishing; 2015. pp. 41–53. 10.1007/978-3-319-12125-3 [DOI] [Google Scholar]
- 13.Kodaman N, Aldrich MC, Sobota R, Asselbergs FW, Poku KA, Brown NJ, et al. Cardiovascular disease risk factors in Ghana during the rural-to-urban transition: A cross-sectional study. PLoS One. 2016;11: 1–20. 10.1371/journal.pone.0162753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aigner E, Feldman A, Datz C. Obesity as an emerging risk factor for iron deficiency. Nutrients. 2014;11: 3587–3600. 10.3390/nu6093587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mujica-Coopman MF, Brito A, López D, Roma D, Pizarro F, Olivares M. Body mass index, iron absorption and iron status in childbearing age women. J Trace Elem Med Biol. 2015;30: 215–219. 10.1016/j.jtemb.2014.03.008 [DOI] [PubMed] [Google Scholar]
- 16.Mocking M, Savitri AI, Uiterwaal CSPM, Amelia D, Antwi E, Baharuddin M, et al. Does body mass index early in pregnancy influence the risk of maternal anaemia? An observational study in Indonesian and Ghanaian women. BMC Public Health. 2018;18: 1–9. 10.1186/s12889-018-5704-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cepeda-Lopez CA, Osendarp SK, Melse-Boonstra A, Aeberli I, Gonzalez-Salazar F, Fesken E, et al. Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity-related inflammation rather than by differences in dietary iron intake. Am J Clin Nutr. 2011;93: 977–983. 10.3945/ajcn.110.005439 [DOI] [PubMed] [Google Scholar]
- 18.Arshad M, Arshad M, Jaberian S, Pazouki A, Riazi S. Iron deficiency anemia and megaloblastic anemia in obese patients. Rom J Intern Med. 2016;55: 1–5. 10.1515/rjim-2016-0046 [DOI] [PubMed] [Google Scholar]
- 19.Wegmüller R, Bentil H, Wirth JP, Petry N, Tanumihardjo SA, Allen L, et al. Anemia, micronutrient deficiencies, malaria, hemoglobinopathies and malnutrition in young children and non-pregnant women in Ghana: Findings from a national survey. PLoS One. 2020;15: e0228258 10.1371/journal.pone.0228258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayensu J, Annan R, Lutterodt H, Edusei A, Peng LS. Prevalence of anaemia and low intake of dietary nutrients in pregnant women living in rural and urban areas in the Ashanti region of Ghana. PLoS One. 2020;15: 1–15. 10.1371/journal.pone.0226026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lartey ST, Magnussen CG, Si L, Boateng GO, de Graaff B, Biritwum RB, et al. Rapidly increasing prevalence of overweight and obesity in older Ghanaian adults from 2007–2015: Evidence from WHO-SAGE Waves 1 & 2. PLoS One. 2019;14: e0215045 10.1371/journal.pone.0215045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Otoo GE, Lartey AA, Perez-Escamilla R. Perceived incentives and barriers to exclusive breastfeeding among periurban Ghanaian women. J Hum Lact. 2009;25: 34–41. 10.1177/0890334408325072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ng M, Fleming T, Robinson M, Thomson BA, Graetz N, Margono C, et al. Global, regional and national prevalence of overweight and obesity in children and adults 1980–2013: A systematic analysis. Lancet. 2014;384: 766–781. 10.1016/S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Appiah CA, Otoo GE, Steiner-Asiedu M. Preferred body size in urban ghanaian women: Implication on the overweight/obesity problem. Pan Afr Med J. 2016;23: 1–9. 10.11604/pamj.2016.23.1.8442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghana Statistical Service. 2010 Population and housing census: National analytical report. Accra; 2013.
- 26.World Health Organisation. Obesity: preventing and managing global epidemic. Report of a WHO Expert Consultation. WHO Technical Report Series No 894. Geneva; 2000. [PubMed]
- 27.Fongar A, Gödecke T, Qaim M. Various forms of double burden of malnutrition problems exist in rural Kenya. BMC Public Health. 2019;19: 1–9. 10.1186/s12889-018-6343-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Little M, Humphries S, Dodd W, Patel K, Dewey C. Socio-demographic patterning of the individual-level double burden of malnutrition in a rural population in South India: A cross-sectional study. BMC Public Health. 2020;20: 1–14. 10.1186/s12889-020-08679-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pereko KK a, Setorglo J, Owusu WB, Tiweh JM, Achampong EK. Overnutrition and associated factors among adults aged 20 years and above in fishing communities in the urban Cape Coast Metropolis, Ghana. Public Health Nutr. 2013;16: 591–5. 10.1017/S1368980012002698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Milman N. Iron and pregnancy a delicate balance. Ann Hematol. 2006;85: 559–565. 10.1007/s00277-006-0108-2 [DOI] [PubMed] [Google Scholar]
- 31.Olutayo AO, Akanle O. Fast food in Ibadan: An emerging consumption pattern. Africa (Lond). 2009;79: 207–226. 10.3366/E0001972009000692 [DOI] [Google Scholar]
- 32.Mugisha JO, Kuper H, Seeley J. Older people’s perception of anemia in rural southwest Uganda. J Aging Health. 2014;26: 316–332. 10.1177/0898264313516165 [DOI] [PubMed] [Google Scholar]
- 33.de-Graft Aikins A. Culture, diet and the maternal body: Ghanaian women’s perspectives on food, fat and childbearing. In: Unnithan-Kumar M, Tremayne S, editors. Fatness and the maternal body: Women’s experiences of corporeality and the shaping of social policy. Oxford: Berghahn Books; 2011. [Google Scholar]
- 34.Rudatsikira E, Muula AS, Mulenga D, Siziya S. Prevalence and correlates of obesity among Lusaka residents, Zambia: A population-based survey. Int Arch Med. 2012;5: 1–6. 10.1186/1755-7682-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biritwum R, Gyapong J, Mensah G. The epidemiology of obesity in Ghana. Ghana Med J. 2005;39: 82–85. [PMC free article] [PubMed] [Google Scholar]
- 36.Kandala N, Stranges S. Geographic variation of overweight and obesity among women in Nigeria: A case for nutritional transition in Sub-Saharan Africa. PLoS One. 2014;9 10.1371/journal.pone.0101103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de-Graft Aikins A. Food beliefs and practices during pregnancy in Ghana: implications for maternal health interventions. Health Care Women Int. 2014;35: 954–972. 10.1080/07399332.2014.926902 [DOI] [PubMed] [Google Scholar]
- 38.Amugsi DA, Mittelmark MB, Oduro A. Association between maternal and child dietary diversity: An analysis of the Ghana Demographic and Health Survey. PLoS One. 2015;10: 1–12. 10.1371/journal.pone.0136748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amugsi DA, Lartey A, Kimani E, Mberu BU. Women’s participation in household decision-making and higher dietary diversity: findings from nationally representative data from Ghana. J Health Popul Nutr. 2016;35: 16 10.1186/s41043-016-0053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data are available from the Measure Demographic and Health Survey program (visit https://www.dhsprogram.com/data/) for researchers who meet the criteria for access to confidential data. The data is labeled Ghana: Standard DHS, 2014 and can be found through the following link: https://dhsprogram.com/methodology/survey/survey-display-437.cfm.