Abstract
Objective
Mobile apps can only increase access to alcohol treatment if patients actively engage with them. Peers may be able to facilitate such engagement by providing supportive accountability and instruction and encouragement for app use. We developed a protocol for peers to support engagement in the Stand Down app for unhealthy alcohol use in veterans and tested the acceptability and utility of the protocol.
Method
Thirty-one veteran primary care patients who screened positive for unhealthy alcohol use and were not currently in addiction treatment were given access to Stand Down for four weeks and concurrently received weekly phone support from a Department of Veterans Affairs (VA) peer specialist to facilitate engagement with the app. App usage was extracted daily, and pre/post treatment assessments measured changes in drinking patterns, via the Timeline Follow-Back interview, and satisfaction with care, via quantitative and qualitative approaches.
Results
A priori benchmarks for acceptability were surpassed: time spent in the app (M=93.89 minutes, SD=92.1), days of app use (M=14.05, SD=8.0), and number of daily interviews completed for tracking progress towards a drinking goal (M=12.64, SD=9.7). Global satisfaction, per the Client Satisfaction Questionnaire, was high (M=26.4 out of 32, SD=4.5). Pre to post, total standard drinks in the prior 30 days (MPre=142.7, MPost=85.6), Drinks Per Drinking Day (MPre=5.4, MPost=4.0), and Percent Heavy Drinking Days (MPre=35.3%, MPost=20.1%) decreased significantly (ps<.05).
Conclusions
Findings indicate that Peer-Supported Stand Down is highly acceptable to veteran primary care patients and may help reduce drinking in this population. A larger controlled trial of this intervention is warranted.
Keywords: Smartphone application, unhealthy alcohol use, Primary Care, Veteran, Peer Support
Unhealthy alcohol use refers to a spectrum of drinking behaviors ranging from hazardous drinking (drinking above recommended levels) to an alcohol use disorder (AUD) (Saitz, 2005; United States Preventive Services Task Force, 2018). Unhealthy alcohol use complicates medical treatment, increases the likelihood of chronic medical conditions, increases health care utilization, and incurs numerous costs for society (Whiteford et al., 2010). However, most patients who engage in unhealthy alcohol use receive little to no treatment. For example, within the Veterans Health Administration (VHA), 15–30% of veterans who are seen in primary care screen positive for unhealthy alcohol use based on the Alcohol Use Disorder Identification Test for Consumption (AUDIT-C; Bradley et al., 2007). However, less than 30% of those who screen positive receive brief counseling to reduce drinking during the primary care visit (Burman et al., 2004; Williams et al., 2014).
Mobile Applications for Alcohol Use Self-Management: Promises and Pitfalls
Mobile applications (apps) offer an innovative and low-cost means of expanding access to care for patients who engage in unhealthy alcohol use but are unwilling or unable to attend treatment. Apps provide a private and self-directed care option that can surmount the stigma and negative attitudes that many patients experience regarding in-person alcohol treatment (Rapp, 2006). Further, with mobile apps, costs associated with in-person appointments are eliminated, yielding savings for patients as well as the healthcare system. This includes travel time, a cost which can be particularly salient for veterans, who are over-represented among individuals living in rural areas in the US and may have geographical barriers to in-person care (Holder, 2017).
Emerging evidence from randomized controlled trials (RCT) of smartphone apps such as the Addiction Comprehensive Health Enhancement Support System (A-CHESS; Gustafson et al., 2014) and Step Away (Gonzalez & Dulin, 2015) suggest that these tools can help reduce problem drinking. Further, in a single-arm prospective study of Veteran primary care patients who served in Iraq and Afghanistan, use of Step Away was associated with significant reductions in total standard drinks and heavy drinking days over six months (Hawkins et al., 2019). Despite the expanding evidence base of mobile apps for unhealthy alcohol use, poor patient engagement remains their Achilles’ heel (Attwood, Parke, Larsen, Morton, & 2017; Bertholet, Daeppen, McNeely, Kushnir, & Cunningham, 2017). For example, in a large RCT of a general population sample, individuals with unhealthy alcohol use (i.e., AUDIT-C scores ≥8 and ≥15 drinks per week) were recruited through an online portal and randomized to receive (or not receive) access to a mobile app focused on risk assessment, personalized feedback and self-monitoring. Only 57% of those assigned to the app condition downloaded the app (Bertholet, Godinho, & Cunningham, 2019). The study concluded that while the app significantly improved drinking outcomes among those who downloaded and used it, simply providing access to an app is insufficient to lead to changes in drinking and that additional methods are necessary to enhance patient uptake.
Using Peers to Enhance Patient Engagement in Mobile Apps for Alcohol Use Self-Management
Use of peer support to facilitate behavioral change has a long history in addiction treatment (Reif et al., 2014). Such support is central in mutual-help organizations and is rooted in evidence that shared experiences create a strong alliance which strengthens individuals’ readiness for change and willingness to seek help for addiction (Kelly, Humphreys, & Ferri, 2020). Peer support can also take the form of peer-based recovery services delivered by a coach who has received specialized training to provide services to support an individual’s recovery efforts. This role tends to be more structured than peer support provided by mutual-help groups, though both rely on the shared experiences of peers and are viewed as a potentially cost-effective option in the treatment of addictions (Bassuk, Hanson, Greene, Richard, & Laudet, 2016). In VHA, peer specialists are veterans who are in recovery from substance use and/or mental health problems and are trained to use their lived experience to provide services to other veterans who are currently struggling with such problems (Goldberg, 2017). This role includes providing patients with emotional support, serving as role models for self-management of one’s health problems, and helping patients navigate the health care system.
The peer role has traditionally been limited to behavioral health settings. Recently, however, several health care organizations have expanded this role to primary care settings (Chinman et al., 2017; Daaleman & Fisher, 2015; Swarbrick, Tunner, Miller, Werner, & Tiegreen, 2016). For example, in VHA, peers in primary care often engage in health coaching to support patients’ self-management of health problems, with implementation of the peer role in these settings supported by external facilitation strategies (Chinman et al., 2017). Given this, as well as the central role of peer support in addiction treatment, peers may be ideally positioned to facilitate primary care patients’ engagement with mobile apps for self-management of unhealthy alcohol use. Such support could entail orienting patients to apps, encouraging use of them for self-management of health problems, providing assurance that they are secure, and coaching patients on how to apply the app content to their real-life problems (Ray, Kemp, Hubbard, & Cucciare, 2017). This approach aligns with the supportive accountability model in which adherence to e-health interventions is enhanced through accountability to a coach who is seen as trustworthy, benevolent, and having legitimacy in terms of expertise and/or experience with the intervention (Mohr, Cuijpers, & Lehman, 2011). The feasibility of this approach is supported by research on use of peers to increase adherence to web-based interventions (Possemato et al., 2019), and a survey of peers and primary care providers in VHA (Miller et al., 2019), and a recent implementation trial of a mobile health system for addiction treatment in primary care (Quanbeck et al., 2018).
The Current Study
Using the supportive accountability model, we developed a protocol for VA peer specialists that is aimed at facilitating a patient’s engagement with an app for unhealthy alcohol use – Stand Down: Think Before You Drink (Blonigen et al., 2020). This app is a veteran version of Step Away––a mobile app for individuals who want to reduce or abstain from drinking but are unwilling or unable to engage in in-person care (Dulin, Gonzalez, King, Giroux, & Bacon, 2013). The app is intended for alcohol use self-management, is applicable to individuals with a range of alcohol use severity, and is grounded in the empirically-supported interventions of motivational enhancement (Miller & Rollnick, 2013) and cognitive-behavioral therapies (Magill & Ray, 2009).
In the current study, patients engaging in unhealthy alcohol use were given access to Stand Down for four weeks and concurrently received weekly phone support from a peer to facilitate engagement with the app. Using a single-arm, pre/post interventional design, we (1) tested the acceptability of Peer-Supported Stand Down by measuring levels of app engagement and overall satisfaction with the intervention relative to a priori benchmarks, (2) evaluated the utility of Peer-Supported Stand Down by estimating the magnitude of within-person change in drinking and associated outcomes, and (3) identified facilitators and barriers to patients’ engagement with both the Stand Down app and its integration with peer phone support.
Methods
Participants
VHA administrative data were used to identify patients at a single VA medical center who (i) had a positive AUDIT-C screen (scores of ≥ 4 for women and ≥ 5 for men; Bradley et al., 2007) during a primary care visit in the past month, (ii) did not receive any outpatient, inpatient, or residential care for alcohol use in the month after their positive AUDIT-C, and (iii) had no active diagnoses of a psychotic-spectrum disorder, such as schizophrenia, or a cognitive disorder, such as dementia. Eligible patients (n = 498) were recruited between September 2018 and April 2019 with study invitation letters sent by mail. Patients who did not respond to the letter were called one week later. A total of 267 patients (53.6%) opted out of the study, and 159 patients (31.9%) were unable to be reached by phone. Seventy-two patients (14.5%) either opted in or when contacted by phone expressed interest in the study. A phone screen was conducted to verify that these patients currently met study inclusion criteria. Patients who no longer had a positive AUDIT-C or who reported no alcohol use in the past 30 days were ineligible. Twenty-nine patients were ineligible, yielding a pool of 43 patients who were eligible to participate in the study.
Out of the pool of eligible patients, quota sampling was used to ensure representation of demographic categories that are underrepresented among veteran primary care patients – i.e., < age 50, non-White/Caucasian, and female. Quotas corresponded to their proportions in the population of veteran primary care patients who screen positive for unhealthy drinking – i.e., < age 50 (40%), non-White/Caucasian (30%), and female (10%) (Bradley et al., 2017). The quota for < age 50 was prioritized. After enrolling 32 patients, this quota was filled (41.9%) and the quota for non-White/Caucasian was exceeded (61.3%), but the quota for female patients was not (6.5%). We elected not to enroll any of the remaining eligible patients as none of them were women and they were predominantly from the quota categories that were already met. One participant was subsequently withdrawn after it was determined that they had been recently diagnosed with alcohol-induced dementia. The final sample size was 31 patients. All participants indicated that they were comfortable using a smartphone and all but one indicated that they owned one. Sample characteristics are shown in Table 1. Participants were predominantly male (93.5%) and reported their race/ethnicity as White/Non-Hispanic (38.7%) or Hispanic (35.5%). On average, participants were 54.6 years old (SD=17.3), with the majority being over the age of 50 (n=18, 58.1%). Most participants had at least some college or vocational training (71.0%) and were not employed at the time of enrollment (83.9%) with the majority of these being retired or a full-time student. Most participants (71.0%) were not currently married. Most participants (80.6%) met criteria for past-year AUD, with the average symptom count indicating a moderate level of AUD severity. Lifetime attendance in a mutual-help group or a treatment program for alcohol or other drugs was each endorsed by nearly 40% of the sample.
Table 1.
Sample characteristics
| Variable | N (%) or M (SD) |
|---|---|
|
| |
| Gender | |
| Male | 29 (93.5%) |
| Female | 2 (6.5%) |
| Race/Ethnicity | |
| White (Non-Hispanic) | 12 (38.7%) |
| Hispanic | 11 (35.5%) |
| Black/African American | 3 (9.7%) |
| Other | 5 (16.1%) |
| Age (M, SD) | 54.6 (17.3) |
| Education (highest level) | |
| High School Diploma/GED | 9 (29.0%) |
| At least some college or vocational training | 22 (71.0%) |
| Job status | |
| Employed (full- or part-time) | 5 (16.1%) |
| Unemployed | 5 (16.1%) |
| Student, retired, or other | 21 (67.7%) |
| Marital status | |
| Married | 10 (32.3%) |
| Not married | 21 (67.7%) |
| Drinking problems | |
| AUDIT-C total score (out of 12), M (SD) | 7.8 (2.7) |
| AUD diagnosis (past year) | 25 (80.6%) |
| AUD symptom count (out of 11); M (SD) | 4.6 (2.8) |
| Treatment history | |
| Ever attended a mutual-help group (AA or NA) | 12 (38.7%) |
| Ever attended treatment for an alcohol or drug problem | 12 (38.7%) |
Note. N = 31. AA = Alcoholics Anonymous. NA = Narcotics Anonymous
Procedures
After providing informed consent, participants completed a baseline interview to obtain information on sociodemographics, drinking problems and patterns, other psychoactive substance use, substance use treatment history, interest in receiving help for drinking, readiness to change alcohol use, and health status. A research assistant helped the participant download the Stand Down app to their iPhone or a study-provided iPod Touch. At the time of this study, the app was only available on the iOS platform. Only 12 participants (38.7%) used their personal iPhone during the study, with the majority (61.3%; n = 19) borrowing a study-provided iPod Touch (in almost all cases this was because they owned a smartphone on the Android platform). Participants were instructed to use the Stand Down app for four weeks and informed that they would receive weekly phone support from a peer specialist to “help them get the most out of the app.” Participants were given the name of the peer that they would be working with and informed that they would receive a phone call from this peer in approximately one day. After four weeks, participants were re-interviewed by phone to measure changes in drinking and associated outcomes since baseline, and to obtain global feedback on their perceptions of the individual components of Peer-Supported Stand Down and their overall satisfaction with the intervention. The post-treatment interview was completed by 29 of the 31 participants (93.5% retention). Participants received $25 for each interview. All study procedures were approved by the local institutional review board.
Stand Down application
Stand Down comprises 10 modules: Drinking Patterns (assessment and personalized, norm-based feedback on an individual’s alcohol use), Goals (choosing moderation or abstinence as a drinking goal), Rewards (setting up rewards for meeting a drinking goal), Cravings (information on alcohol cravings and coping strategies to manage them), Strategies (behavioral strategies for relapse prevention), Support Persons (identifying and sharing progress towards a drinking goal with family and/or friends), Reminders (creating self-generated verbal and visual reminders of reasons to change drinking), High-Risk (providing alerts when a high-risk time for drinking is approaching), Moods (assessment of mood levels relative to norms and information on the impact of alcohol use on mood), and New Activities (scheduling nondrinking activities in lieu of drinking). After downloading the app, users are first prompted to complete the Drinking Patterns module and are then prompted to complete the Goals module. In addition, users are prompted to complete Daily Interviews to monitor their drinking and are provided with weekly feedback on progress towards their drinking goal.
Peer phone sessions
The weekly phone sessions with peer specialists were scheduled for 15–30 minutes and were initiated by the peers. The key components of these sessions entailed peers (1) inquiring about use of the app, (2) providing suggestions on how app content could be applied to participants’ lives to reach their drinking goal, (3) offering technical support to navigate the app and understand its functionality, and (4) encouraging ongoing utilization of the app and suggesting action plans tailored to their needs (Ray et al., 2017). Phone sessions were provided by three peers employed by VHA, all of whom had lived experience with alcohol use problems and were in recovery. Consistent with their training, peers were also encouraged to share their lived experience of substance use problems, provide emotional support, and facilitate engagement in health care services, as needed. The protocol for these sessions was detailed in a manual, which was adapted from other guides developed for peer-supported web-based programs for veterans with mental health problems (Possemato et al., 2019). Before recruitment, peers participated in a day-long training led by the first author to review the study procedures, the app, and the peers’ role in the intervention. One week prior to the training, peers were asked to download the app to their personal phones and to use it regularly to become familiar with its features and functionality. Although the peers were already in recovery from alcohol use, this trial period using Stand Down allowed them to gain expertise in the app and to consider how it could have been used to support their past recovery efforts. Phone sessions were audio-recorded with participants’ permission. Throughout the study, peers attended a weekly, one-hour long fidelity monitoring call with the first author to receive clinical supervision and feedback on their phone sessions from the past week.
A total of 79 sessions were completed with participants. On average, participants completed 2.55 sessions (SD=1.4). Almost all participants completed at least one session with a peer (n = 30; 96.8%), and 10 participants (32.3%) completed four or more sessions (three participants requested to have a fifth session with the peer). Out of the 79 sessions that were completed, 64 (81%) were recorded and evaluated for fidelity to the protocol using a 4-item checklist. Checklist items corresponded to the key components described above (i.e., inquiring about app use, applying app content, technical support, and encouraging ongoing utilization) and were rated 0 (not addressed), 1 (somewhat addressed), or 2 (fully addressed). Sessions lasted 12.59 minutes, on average (SD = 5.37). The average total score on the fidelity checklist was 7.16 (SD = 1.51) out of 8.
Measures
Intervention engagement and satisfaction
Data on engagement with Stand Down (i.e., number of modules launched, time spent in the app, number of days used, number of Daily and Weekly Interviews completed) were extracted from the app during the four-week intervention period. Due to limited Wi-Fi availability, 9 participants who borrowed an iPod Touch did not have their app usage data uploaded to the Cloud-based system where these data were being tracked. Therefore, data on app usage was available for 22 of the 31 participants.
At post-treatment, participants used a 5-point scale to rate the helpfulness of the phone sessions with peer specialists (1 = not at all helpful, 5 = very helpful) in terms of receiving instructions on how to use the app, discussing app content to better understand it, discussing app content to help participants apply it to their own lives, and reducing drinking. The extent to which the peer phone sessions helped participants understand and use the skills taught by the app were rated on 4-point scale (1 = not all, 4 = a lot). The ideal frequency of the phone sessions was rated on a 4-point scale (1 = every four weeks, 2 = every two weeks, 3 = weekly, 4 = twice per week). Global satisfaction with Peer-Supported Stand Down was assessed with the 8-item Client Satisfaction Questionnaire (CSQ; Attkisson & Zwick, 1982). Items were rated on a 4-point scale and measured whether the intervention aligned with participants’ goals for managing their drinking. Higher scores indicated more satisfaction with the intervention (α = .91). The perceived flexibility of the intervention in meeting participants’ needs and drinking goals was rated on a 4-point scale (1 = not at all, 4 = very).
Drinking problems
The 3-item AUDIT-C was administered at baseline. This reliable and valid measure of problem drinking focuses on questions of alcohol consumption in the past year (Bradley et al., 2007). Total scores can range from 0 to 12, with higher scores indicating more drinking problems and higher likelihood of an AUD. Participants’ average score at baseline indicated a moderate level of drinking problems (M = 7.8, SD = 2.7). DSM-5 based diagnoses and symptom counts of past-year AUD were assessed at baseline using items from the National Institute on Alcohol Abuse and Alcoholism (NIAAA, 2016).
Drinking patterns
The Timeline Follow-Back interview (TLFB; Sobell, Brown, Leo, & Sobell, 1996) is a retrospective, calendar-based method of gathering daily information on quantity and frequency of alcohol use. The TLFB was administered at baseline and post-treatment to calculate the following drinking variables in the 30 days prior to each assessment: Total standard drinks, percent days abstinent (PDA), drinks per drinking day (DPDD), and percent heavy drinking days (PHDD). Heavy drinking days were defined as five or more standard drinks for men and four or more standard drinks for women.
Other psychoactive substance use
The World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) is a brief and validated measure of psychoactive substance use for patients in primary care and general medical settings (Humeniuk et al., 2010). A modified version of the ASSIST was administered at baseline to assess lifetime (0 = No, 1 = Yes) use of nicotine (90.3%), cannabis (74.2%), sedatives/tranquilizers (29.0%), hypnotics (12.9%), steroids (16.1%), amphetamines (prescribed [6.5%], non-prescribed [22.6%]), cocaine (38.7%), hallucinogens (32.3%), inhalants (6.5%), and opiates (prescribed [58.1%], non-prescribed [9.7%]). Past month use (days) of these substances was also assessed at pre- and post-treatment.
Substance use treatment history and interest in help for drinking
At baseline, items from the Addiction Severity Index (McLellan et al., 1992) were used to assess participants’ history of attending mutual-help groups (e.g., Alcoholics Anonymous; AA) and treatment (i.e., inpatient/residential, outpatient) for an alcohol or drug use problem. At baseline and post-treatment, participants were also asked to separately rate their interest in attending an AA meeting and a treatment program for drinking problems on a 4-point scale (1 = not interested, 4 = very interested).
Readiness to change alcohol use
The Readiness Ruler (Miller & Rollnick, 2013) was administered at baseline and post-treatment and asked participants to indicate how ready they were to make a change (quit or cut down) in their use of alcohol at this time. Responses were rated on a 1 (not ready to change) to 10 (trying to change) scale. Higher readiness to change scores have been shown to predict better drinking outcomes in longitudinal studies (Gaume, Bertholet, & Daeppen, 2017).
Health status
The Veterans RAND 12-item (VR-12) survey was administered at baseline and post-treatment. Two composites scores can be created from this measure to assess participants’ mental and physical health status: Mental Component Score (MCS) and Physical Component Score (PCS) (Spiro, Rogers, Qian, & Kazis, 2004). These composites were standardized using a T-score metric (M = 50, SD = 10) and scores calculated in reference to norms for the US population from 2000–2002 (Selim et al., 2009).
Perceptions of Peer-Supported Stand Down
At post-treatment, open-ended questions were used to query participants on their experiences with the app, the peer phone sessions, and the integration of these two components. For example, participants were queried on their general impression of Peer-Supported Stand Down, how they used the app, what they found most (and least) helpful about the app, what they found most (and least) helpful about the phone sessions with peers, and suggestions for improvements. Questions were adapted from a feedback interview used in prior studies of peer-supported web-based interventions (Kuhn et al., 2014; Possemato et al., 2019). Participants’ feedback was used to identify facilitators and barriers to engagement with the app and integrating the app with peer phone support.
Data Analysis
Descriptive statistics were used to quantify various metrics of intervention engagement and satisfaction (e.g., app usage, CSQ total scores). The primary outcomes were acceptability and utility of Peer-Supported Stand Down. A priori benchmarks for acceptability were as follows: (1) For app usage, at least 3 modules launched and 7 daily interviews completed. These benchmarks represent the low end of engagement of the parent app–Step Away–over a four-week period based on prior research (P. Dulin, personal communication). (2) For patient satisfaction, for each of the 8 CSQ items (4-point response format) a response of 3 or higher indicates at least some satisfaction with an intervention. Thus, an average CSQ total score of 24 was selected as our benchmark for acceptability. These benchmarks were listed in the grant proposal that was submitted to the funding agency. Utility was operationalized in terms of within-person reductions, per Cohen’s d effect sizes, in total standard drinks, PDA, DPDD, and PHDD. This study was not powered to detect significant changes in these outcomes but rather to estimate their magnitude of change pre- to post-treatment. Nonetheless, we conducted repeated measures ANOVAs to explore whether the within-person changes on the drinking outcomes and other continuous measures were significant. McNemar’s chi-square test was also conducted to explore if there was significant change pre- to post-treatment in any drug use in the past month.
Responses to the open-ended questions from the post-treatment phone interview were analyzed using a modified version of Rapid Identification of Themes from Audio-Recordings (Neal et al., 2015). After each interview, two research assistants listened to the audio-recordings and took detailed notes using a template to summarize responses to each interview question and document preliminary themes related to facilitators and barriers to engagement with the app and its integration with peer phone support. Interview notes were then copied into an Excel matrix to compare the preliminary themes for each question (columns) across participants (rows). The matrix was organized such that a summary of participants’ response to the question and the preliminary theme were entered into each cell. The first author and a Master’s level qualitative analyst (JSS) then independently reviewed the matrix to identify global themes across the interview questions related to facilitators and barriers to engagement in the intervention. These individuals then met to review their independently-derived lists of themes and engaged in a consensus process to rectify disagreements and finalize the themes.
Results
Intervention engagement and satisfaction
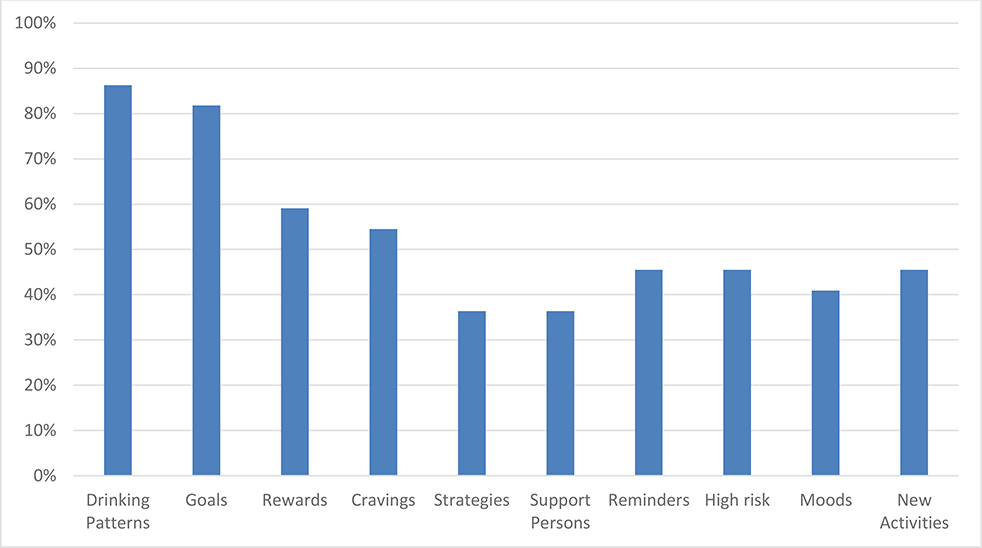
In terms of usage of the Stand Down app, all participants used the app at least once, and 91% used it more than once. By week 4, 82% of participants were still using the app. Participants used the app an average of 14.05 days (SD = 8.0) during the four-week period, with total time spent in the app ranging from < 1 to 407.08 minutes (M = 93.89, SD = 92.1, Median = 63.79). The mean and median number of seconds spent in the app per launch was 149.93 (SD = 437.03) and 60.9, respectively. On average, participants launched 5.23 (SD = 3.9) of the 10 app modules, with majorities of participants launching the Drinking Patterns, Goals, Rewards, and Cravings modules at least once (see Figure 1). Out of 18 participants who launched the Goals module, 15 chose a path of ‘moderation’ and three did not choose a path; no participants chose ‘abstinence’ as a drinking goal. On average, participants completed 12.64 (SD = 9.7) Daily Interviews for monitoring alcohol use and moods, and 1.64 (SD = 1.36) Weekly Interviews, which provides users with feedback on progress towards their drinking goals. Eighty-six percent of the sample completed at least one of the Daily Interviews, and 81% completed more than one.
Figure 1.
Percentage of participants who launched each module of the Stand Down app.
Regarding peer phone support, on a scale of 1 (‘not at all’) to 5 (‘very’), mean ratings of the helpfulness of these sessions were high in terms of receiving instructions on how to use the app (M = 4.16, SD = 1.2), discussing app content to better understand it (M = 4.12, SD = 1.5) and apply it to participants’ lives (M = 4.08, SD = 1.5), and reducing drinking (M = 4.00, SD = 1.4). On a scale of 1 (‘not at all’) to 4 (‘a lot’), the mean rating of how much peer sessions helped participants understand and use the skills taught in the app was 3.41 (SD = 1.0). Seventy-nine percent of participants rated the ideal frequency of the peer phone sessions as being at least weekly. In terms of participants’ global satisfaction with Peer-Supported Stand Down, the mean CSQ total score was 26.41 (SD = 4.5), which is above the benchmark for success (i.e., total score of 24, out of 32) and 76% of participants had a total score above this benchmark. On a scale of 1 (‘not at all’) to 4 (‘very’), the mean rating of the flexibility of the intervention in meeting participants’ needs and drinking goals was 3.55 (SD = 0.8).
Within-person changes in drinking and associated outcomes
In terms of quantity and frequency of alcohol use in the past 30 days, total standard drinks, DPDD, and PHDD decreased from pre to post, while PDA increased. Effect size estimates were moderate in magnitude for total standard drinks and small-to-moderate for PDA, DPDD, and PHDD. These magnitudes of change corresponded to approximately a 40% reduction in total standard drinks, a 10% increase in days abstinent, 1.5 fewer drinks per drinking day, and a 15% decrease in heavy drinking days. Within-person changes were significant for total standard drinks, DPDD, and PHDD (see Table 2).
Table 2.
Within-person changes in drinking and associated outcomes (pre/post-treatment).
| Pre-treatment |
Post-treatment |
Repeated Measures ANOVA |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) | Median (Min, Max) | Mean (SD) | Median (Min, Max) | Cohen’ d (95% CI) | F (df) | p |
|
| |||||||
| Drinking patterns (past 30 days) a | |||||||
| Total Standard Drinks | 142.69 (150.3) | 92.0 (8.0, 630) | 85.64 (73.3) | 75.0 (0.0, 300.0) | −0.48 (−1.00, 0.05) | 6.08* (1,28) | .020 |
| Percent Days Abstinent | 20.9 (28.7) | 0.0 (0.0, 87.0) | 30.2 (36.4) | 13.3 (0.0, 100.0) | 0.28 (−0.24, 0.80) | 1.60 (1,28) | .216 |
| Drinks Per Drinking Day | 5.42 (4.7) | 3.8 (1.07, 21.0) | 4.03 (2.3) | 3.0 (1.50, 10.00) | −0.37 (−0.89, 0.16) | 4.23* (1,27) | .049 |
| Percent Heavy Drinking Days | 35.3 (41.5) | 13.3 (0.0, 100.0) | 20.1 (35.9) | 0.0 (0.0, 100.0) | −0.39 (−0.91, 0.13) | 4.42* (1,28) | .045 |
| Other drug use (days in past month) b | 6.52 (11.9) | 0.0 (0.0, 30.0) | 6.31 (12.3) | 0.0 (0.0, 30.0) | −0.02 (−0.53, 0.50) | 0.02 (1,28) | .879 |
| Interest in help for drinking c | |||||||
| AA | 1.55 (0.9) | 1.0 (1.0, 4.0) | 1.72 (1.1) | 1.0 (1.0, 4.0) | 0.17 (−0.35, 0.68) | 1.99 (1,28) | .169 |
| AUD treatment | 1.69 (0.9) | 1.0 (1.0, 4.0) | 1.66 (0.9) | 1.0 (1.0, 4.0) | −0.04 (−0.55, 0.48) | 0.88 (1,28) | .769 |
| Readiness to change alcohol use d | 5.77 (2.3) | 6.0 (1.0, 10.0) | 6.58 (3.3) | 7.0 (1.0, 10.0) | 0.28 (−0.27, 0.82) | 1.35 (1,25) | .256 |
| Health status e | |||||||
| Physical health (PCS) | 41.13 (8.6) | 41.31 (15.21, 52.02) | 42.55 (12.2) | 46.32 (12.54, 61.11) | 0.13 (−0.38, 0.65) | 0.81 (1,28) | .375 |
| Mental health (MCS) | 42.63 (12.3) | 43.05 (18.08, 61.52) | 41.29 (14.6) | 41.45 (11.51, 67.09) | −0.10 (−0.61, 0.42) | 0.60 (1,28) | .445 |
Note.
= Assessed using the Timeline Follow-Back interview.
= Assessed using the Alcohol, Smoking, and Substance Involvement Screening Test. AA = Alcoholics Anonymous. AUD = Alcohol Use Disorder.
Items were rated on a 4-point scale (1 = not interested, 4 = very interested).
Rated with the Readiness Ruler using a 10-point scale (1 = not ready to change, 10 = trying to change).
= Assessed using the Veterans RAND 12-item survey. PCS = Physical Component Score. MCS = Mental Component Score.
Regarding other outcomes, there was almost no change in the average number days of other drug use in the past month; however, the number of participants who reported any drug use in the past month at baseline (n = 13; 42%) was reduced by nearly half (n = 7; 24%) (p = .06; OR = 2.40; 95% Confidence Intervals = 1.23 – 4.69). In terms of help-seeking, five participants reported attending either a mutual-help group or outpatient substance use treatment in the follow-up period (per the inclusion criteria, no participants received treatment in the 30 days prior to baseline). However, ratings of interest in receiving help for drinking changed minimally over the four weeks. Readiness to change alcohol increased over time, with effect size estimates small-to-moderate in magnitude. However, this magnitude of change corresponded to less than a 1-point increase on the Readiness Ruler. Health status was largely unchanged from pre to post, with average T-scores at both time points indicating that the sample was nearly 1 SD lower than the norm-referenced sample of veterans in terms of physical and mental health.
Facilitators and barriers to engagement with Stand Down
Among facilitators to engagement with the Stand Down app, participants highlighted the ability to track drinking patterns and progress towards goals through the Daily Interviews, reminders of high-risk times for drinking, ease of navigation, and personalized feedback, which raised participants’ awareness of drinking patterns and consequences (see Table 3). In terms of barriers to engagement, participants highlighted the app not being available on the Android platform and the limitations of having to use a study-provided iPod Touch (e.g., challenges with remembering to use a separate device; device would freeze; app would crash or be slow to load; unable to make calls from the device). Some participants also felt that the Daily Interview reminders were too frequent and suggested that an option for customizing the frequency of these reminders should be available for those who need or want less monitoring of their drinking.
Table 3.
Facilitators and barriers to engagement with the Stand Down app
| Facilitator themes | Sample quotations |
|
| |
| Tracking drinking patterns and progress towards goals |
“I liked the way that you can track what you drink every day. I liked when it analyzed how much I drank that week to give me an idea of what my average alcohol content was for that week.”
“The daily questions. It would say how many drinks I had. So today I would think about what I had yesterday. It was good for me to compare on a daily basis.” |
| Reminders of high-risk times for drinking |
“It’s nice to have something that reminds you, [that] this is the time of the night that you might be sensitive to drinking so you might want to think about it before you open that bottle of wine or can of beer.”
“It was helpful to have a recurring alert that a peak [time for drinking] was coming.” |
| Ease of navigation |
“Easy access. Everything on the menu was easy to find and easy to get to. All of the steps were either at the bottom or you could scroll from left to right and complete things.”
“I think it is very customer friendly. I think it is easy to use. It feels like it is your assistant.” |
| Personalized feedback |
“Raising awareness of goals for stopping drinking. Pointing out money saved.”
“The chart in the beginning that shows reasons for drinking and consequences of drinking provides good incentive to use the app. Liked the information about calories and money spent on alcohol.” |
|
| |
| Barrier themes | Sample quotations |
|
| |
| App not available on the Android platform |
“It wasn’t on the Android so that made it more complicated to keep up with the daily check-ins.”
“I would probably use it more if it was on Android. I am more familiar with android than I am with iPhone because that is what I have.” |
| Frequency of the reminders to check-in with the app |
“Tone down the reminders. Make it easier to modify the frequency.”
“The only thing I didn’t like was the reminder every day. I didn’t need that many. I think some people do need it but for me it was not necessary.” |
When asked, “Do you think the app will help Veterans reduce the amount they drink or how often they drink?”, 26 of 29 (89.7%) participants answered yes, with many adding that it would depend on whether the veteran was internally motivated or had support from someone to keep them accountable – e.g., “It will help if you are internally motivated to change”; “It will help as long as it’s used in conjunction with the peer coach to keep you accountable.” When asked, “How likely are you to continue using Stand Down if it were available on your personal phone?”, 26 of 29 (89.7%) participants also answered affirmatively – e.g., “I would say very likely”; “I will continue using the app”; “I will probably use it every day.”
Facilitators and barriers to integrating the app with peer phone support
Open-ended feedback on the integration of the app with peer phone support was uniformly positive. Regarding facilitators to this, themes included the practical benefits of the peer in terms of providing supportive accountability for using the app, and assistance with navigating the app and understand its functionality. In addition, participants noted the more general benefits they experienced from receiving peer support, separate from any benefits related to engagement with the app. For example, participants highlighted the ability to receive support from a fellow veteran with ‘lived experience’ in addiction, and emotional support beyond their issues with alcohol use. In terms of barriers to integration of peer phone support, female participants highlighted a preference for a female peer. Participants also noted some limitations to only receiving support from the peer by phone and a desire for opportunities to meet with the peer in person (see Table 4).
Table 4.
Facilitators and barriers to integrating the app with peer phone support.
| Facilitator themes | Sample quotations |
|
| |
| Supportive accountability for using the app. |
“Having that human support reinforces using the app.”
“Having [the peer] being on hand helps. Makes it easier to regulate yourself when someone else is holding you accountable.” |
| Assistance with navigating the app and understand its functionality. |
“He helped me along with the app. He helped me in telling me where I could go to for different things [in the app].”
“What was helpful were tips on how to use the app... what sections were going to be helpful for using the app to modify behavior.” |
| Support from fellow veteran with ‘lived experience’ with addiction. |
“What was helpful was the way he relayed his experiences. He used good phrasing. He was real”
“Whenever he would give me an example of something that happened to him or a friend of his that made me feel like I wasn’t really alone in my struggle.” |
| Emotional support beyond their alcohol use. |
“He gave me an opportunity to talk about other things going on in my life.”
“He was giving me the room I needed to move forward because I felt he recognized that I wasn’t really read to jump in 100% yet.” |
|
| |
| Barrier themes | Sample quotations |
|
| |
| Lack of a female peer specialist for female veteran patients. |
“It’d nice to talk to somebody that is the same gender.”
“It would be easier to talk with a woman.” |
| Lack of opportunities for in-person sessions with the peer. |
“It would be helpful to have in-person meetings so that they could help you more.”
“I would integrate peer support hang out sessions to keep vets away from using alcohol. This would be a way to keep vets busy.” |
When asked, “Did the peer phone support increase your willingness to use the app?”, 21 of 29 (72.4%) participants answered yes. The other 8 participants reported that the phone sessions neither helped nor hurt their willingness to use the app and suggested this component of the intervention be optional – e.g., “I would have liked it to be an option and not a mandatory thing to have a peer coach. It would be a great idea for those who would want a coach, but I did not need one.”
Discussion
We developed a protocol for peers to support engagement in the Stand Down app for unhealthy alcohol use in veterans and tested the acceptability and utility of the protocol. Acceptability of Peer-Supported Stand Down was high, with levels of app usage and ratings of satisfaction surpassing our a priori benchmarks. Whether peers per se enhanced app engagement cannot be concluded, given the lack of an app-only control condition. Nevertheless, app usage among participants in this study was higher than in many other studies of apps for alcohol use self-management. For example, “Alcooquiz” is an app for unhealthy alcohol use, which contains similar content as Stand Down. In a prior study of this app, 77% of participants used the app at least once, 64% used it more than once, 76% launched the personalized feedback module, and 41% launched the self-monitoring tool (e.g., completion of a drinking diary) (Bertholet et al., 2017). In the current study, all participants used Stand Down at least once, 91% used it more than once, 86% launched the personalized feedback module (i.e., Drinking Patterns), and 86% launched the self-monitoring tool (i.e., Daily Interviews). Further, in the Hawkins et al. (2019) study of veteran primary care patients who were given access to Step Away – the parent app of Stand Down – 54% of participants were still using the app by week 4, whereas 82% of participants in the current study were still using Stand Down by week 4. These comparisons notwithstanding, future research on Peer-Supported Stand Down should include an app-only condition to more directly test whether the peer phone protocol enhances app usage.
The potential utility of the intervention was indicated by effect size changes for most of the drinking outcomes that were moderate in magnitude. These changes must also be qualified by the lack of a control condition in this study, which limits conclusions regarding the efficacy of the intervention. Nevertheless, the clinical significance of these changes should be given consideration. For example, given the mean number of standard drinks consumed by participants in the 30 days prior to enrollment (142.69 drinks), a 40% reduction in this amount over four weeks is notable. While treatment for AUD has traditionally focused on abstinence as the primary outcome, this may not be the typical focus of alcohol use treatment in primary care. Further, non-abstinent drinking patterns may still be associated with successful treatment outcomes long-term (Witkiewitz et al., 2017).
Implications for Implementation of Mobile apps for Unhealthy Alcohol Use
Peer-Supported Stand Down has the potential to address a major barrier to implementation of mobile health tools for unhealthy alcohol use – low patient uptake and engagement (Attwood et al., 2017). This intervention represents a novel application of Mohr and colleagues’ (2011) supportive accountability model for e-health engagement and builds on other research demonstrating the feasibility and acceptability of using peers to support engagement in a web-based cognitive-behavioral intervention for patients with comorbid PTSD and unhealthy alcohol use (Possemato et al., 2019). As in the current study, participants in the Possemato et al. (2019) study reported liking that they were held accountable by someone for using the program, particularly someone who had similar life experiences with whom they could better relate. Peers may fulfill the relational factors that are essential to the supportive accountability model in terms of a coach that is viewed as trustworthy, benevolent, and legitimate (Mohr et al., 2011). The current study extends these findings to the role of peers in providing supportive accountability for engagement in an app for unhealthy alcohol use.
From a cost standpoint, the low-intensity and brief duration of Peer-Supported Stand Down may also have benefits, given the resource constraints of capitated healthcare systems such as VHA. That is, the protocol for the current study involved an average of 2–3 completed sessions (typically 12–13 minutes long) between the peer and participant. This accords well with the typical number of appointments for behavioral health providers in primary care (Possemato, Ouimette, & Lantiga, 2011). Therefore, the peer phone protocol represents a potentially low-cost option for healthcare systems to prime patients’ engagement in an app for unhealthy alcohol use.
The qualitative data also provided insights into what participants liked about Stand Down that promoted their engagement with this app. The most robust facilitator theme was the ability of the app to track participants’ drinking patterns and progress towards their drinking goals via the Daily and Weekly Interviews. In prior research with the parent app, Step Away, this feature has also been reported by users as being most helpful in reducing their drinking (Giroux, Bacon, King, & Dulin, 2014; Hawkins et al., 2019). Interestingly, other qualitative research on engagement with an alcohol-harm reduction app suggests that the most common type of users are not motivated by a desire to cut down on their drinking but rather to monitor their use to increase awareness of drinking habits and the potential for problems (Milward, Deluca, Drummond, & Kimergård, 2018). For these users, app engagement is limited primarily to use of daily diary features with limited exploration of other app features or tools.
Limitations and Future Directions
Several limitations of this study should be acknowledged. First, due to the small sample size there was insufficient power to identify significant changes in outcomes for effect sizes that were small in magnitude. Thus, the replicability of the within-person changes in drinking and associated outcomes needs to be established in future studies. Second, the generalizability of the findings may be limited by the use of quota sampling, the sample being drawn from a single VA medical center and comprising mostly middle-aged men, and the low response rate to the recruitment letters which may have introduced selection factors. Future studies of Peer-Supported Stand Down should expand to multiple sites, enrich recruitment of younger and/or female patients, and expand recruitment efforts using random sampling methods. The generalizability of the intervention to real-world app users may have been further limited by the fact that most participants did not use their own smartphone and a research assistant helped download the app. Given that a lack of digital literacy may be a limitation to app-based interventions in general, future work could explore using peers to assist patients with downloading the app. Third, the four-week intervention period provided only a short-term assessment of outcomes; thus, app engagement and utility will need to be established over longer follow-up periods in future trials. Finally, given the lack of a control condition, the current findings cannot attest to the efficacy of the intervention in terms of either enhancing app engagement or improving drinking outcomes. Nevertheless, the findings are promising and support conducting a larger RCT.
Conclusions
Mobile apps, such as Stand Down, may offer a low-cost means of enhancing access to care for patients who engage in unhealthy alcohol use but are unable or unwilling to seek care in person. Supportive accountability by peers is a novel approach to support patient engagement in such apps and was found to be highly acceptable to veteran primary care patients and may help reduce drinking in this population. A full-scale RCT of Peer-Supported Stand Down is warranted and ideally would employ a design that can test if this approach is superior to the app alone in terms of engaging users and improving outcomes, as well as elucidate for whom peer phone support is most beneficial.
Public Health Significance.
This study suggests that peers may help boost a patient’s acceptance and use of mobile apps that are designed to help them reduce their alcohol use.
Acknowledgments
This work was supported by a VA Health Services Research & Development (HSR&D) grant awarded to Daniel M. Blonigen (PPO 16-305). Christine Timko and Keith Humphreys were supported by Senior Research Career Scientist Awards from VA HSR&D (RCS-00-001 and RCS-14-141, respectively). The views expressed are those of the authors and do not necessarily reflect those of the Veterans Health Administration. Patrick L. Dulin is the primary owner of Here & Now Systems, LLC – the company that developed the Step Away and Stand Down mobile applications.
Footnotes
There are no other conflicts to report.
References
- Attkisson CC, & Zwick R (1982). The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5(3), 233–237. [DOI] [PubMed] [Google Scholar]
- Attwood S, Parke H, Larsen J, & Morton KL (2017). Using a mobile health application to reduce alcohol consumption: A mixed-methods evaluation of the drinkaware track & calculate units application. BMC Public Health, 17(1), 394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Richard M, & Laudet A (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. doi: 10.1016/j.jsat.2016.01.003. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, McNeely J, Kushnir V, & Cunningham JA (2017). Smartphone application for unhealthy alcohol use: A pilot study. Substance Abuse, 38(3), 285–291. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Godinho A, & Cunningham JA (2019). Smartphone application for unhealthy alcohol use: Pilot randomized controlled trial in the general population. Drug and Alcohol Dependence, 195, 101–105. [DOI] [PubMed] [Google Scholar]
- Blonigen DM, Harris-Olenak B, Kuhn E, Humphreys K, Timko C, & Dulin P (2020). From “Step Away” to “Stand Down”: Tailoring a Smartphone Application for Self-Management of Hazardous Drinking for Veterans. JMIR mHealth and uHealth, 8(2): e16062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, & Kivlahan DR (2007). AUDIT-C as a brief screen for alcohol misuse in primary care. Alcoholism: Clinical and Experimental Research, 31, 1208–1217. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Ludman EJ, Chavez L, Bobb JF, Ruedebusch SJ, Achtmeyer CE, … Kivlahan DR (2017). Patient-centered primary care for adults at high risk for AUDs: The Choosing Healthier Drinking Options In Primary Care (CHOICE) trial. Addiction Science & Clinical Practice, 12:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burman ML, Kivlahan D, Buchbinder M, Broglio K, Zhoum XH, Merrill JO, … Bradley KA (2004). Alcohol-related advice for Veterans Affairs primary care patients: Who gets it? Who gives it? Journal of Studies on Alcohol, 65, 621–630. [DOI] [PubMed] [Google Scholar]
- Chinman M, Daniels K, Smith J, McCarthy S, Medoff D, Peeples A, & Goldberg R (2017). Provision of peer specialist services in VA patient aligned care teams: Protocol for testing a cluster randomized implementation trial. Implementation Science; IS, 12, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daaleman TP, & Fisher EB (2015). Enriching patient-centered medical homes through peer support. Annals of Family Medicine, 13, S73–S78. 10.1370/afm.1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulin PL, Gonzalez VM, King DK, Giroux D, & Bacon S (2013). Development of a smartphone-based, self-administered intervention system for alcohol use disorders. Alcoholism Treatment Quarterly, 31, 321–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaume J, Bertholet N, & Daeppen J-B. (2017). Readiness to change predicts drinking: Findings from 12-month follow-up of alcohol use disorder outpatients. Alcohol and Alcoholism, 52(1), 65–71. [DOI] [PubMed] [Google Scholar]
- Giroux D, Bacon S, King DK, Dulin P, & Gonzalez V (2014). Examining perceptions of a smartphone-based intervention system for alcohol use disorders. Telemedicine Journal and e-health, 20(10): 923–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg R (2017). Increasing the role of peer specialists in primary care settings. VA Recovery Update 5:1. [Google Scholar]
- Gonzalez VM, Dulin PL (2015). Comparison of a smartphone app for alcohol use disorders with an Internet-based intervention plus bibliotherapy: A pilot study. Journal of Consulting and Clinical Psychology, 83, 335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG, … Shah D (2014). A smartphone application to support recovery from alcoholism: A randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins E, Danner A, Lott A, Malte C, Dulin P, Fortney J, Sayre G, & Baer J (2019). Evaluating the Usability of a Mobile Application for Self-management of Unhealthy Alcohol Use. In Garets M, Archer S, Kitchens C, Cochran G, Gordon AJ The 2019 Addiction Health Services Research Conference: Insights, review, and abstracts. Substance Abuse, 40(4): 469–472 (Supp 113). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder KA (2017). Veterans in Rural America: 2011–2015, American Community Survey Reports, ACS-36. Washington, D.C. Retrieved on Nov 1, 2018 from www.census.gov/content/dam/Census/library/publications/2017/acs/acs-36.pdf [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J … Simon S (2008). Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction, 103(6), 1039–1047. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Humphreys, & Ferri M (2020). Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews, Issue 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn E, Greene C, Hoffman J, Nguyen T, Wald L, Schmidt J, Ramsey KM, & Ruzek J (2014). A preliminary evaluation of PTSD Coach, a smartphone app for posttraumatic stress symptoms. Military Medicine, 179(1), 12–18. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. (1992). The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9, 199–213. [DOI] [PubMed] [Google Scholar]
- Magill M, & Ray LA (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies of Alcohol and Drugs, 70, 516–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KE, Kuhn E, Yu J, Owen JE, Jaworski BK, Taylor K, Blonigen DM, & Possemato K (2019, April 15). Use and Perceptions of Mobile Apps for Patients Among VA Primary Care Mental and Behavioral Health Providers. Professional Psychology: Research and Practice. Advance online publication. 10.1037/pro0000229 [DOI] [Google Scholar]
- Miller WR, & Rollnick S (2013). Motivational interviewing (3rd ed.). New York, NY: Guilford Press. [Google Scholar]
- Milward J, Deluca Drummond, C., & Kimergård A (2018). Developing typologies of user engagement with the BRANCH alcohol-harm reduction smartphone app: Qualitative study. JMIR mHealth uHealth, 6(12): e11692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miner A, Kuhn E, Hoffman JE, Owen JE, Ruzek JI, & Taylor CB (2016). Feasibility, acceptability, and potential efficacy of the PTSD Coach app: A pilot randomized controlled trial with community trauma survivors. Psychological Trauma: Theory, Research, Practice, and Policy, 8(3), 384–392. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Cuijpers P, & Lehman K (2011). Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. Journal of Medical Internet Research, 13(1): e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (2016). Alcohol use disorder: A comparison between DSM–IV and DSM–5. NIH Publication No.13–7999. Retrieved on Nov 1, 2018 from: http://pubs.niaaa.nih.gov/publications/dsmfactsheet/dsmfact.htm.
- Neal JW, Neal ZP, Van Dyke E, & Kornbluh M (2014). Expediting the analysis of qualitative data in evaluation: A procedure for the rapid identification of themes from audio recordings (RITA). American Journal of Evaluation, 36, 118–132. [Google Scholar]
- Possemato K, Johnson EM, Emery JB, Wade M, Acosta MC, Marsch LA, Rosenblum A, & Maisto SA (2019). A pilot study comparing peer supported web-based CBT to self-managed web CBT for primary care veterans with PTSD and hazardous alcohol use. Psychiatric Rehabilitation Journal, 42(3), 305–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Possemato K, Ouimette P, Lantinga LJ, et al. (2011). Treatment of Department of Veterans Affairs primary care patients with posttraumatic stress disorder. Psychological Services, 8(2), 82–93. [Google Scholar]
- Quanbeck A, Gustafson DH, Marsch LA, Chih M-Y, Kornfield R, McTavish F … Shah DV (2018). Implementing a mobile health system to integrate the treatment of addiction into primary care; A hybrid implementation-effectiveness study. Journal of Medical Internet Research, 20(1), e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapp RC (2006). Treatment barriers identified by substance abusers assessed at a centralized intake unit. Journal of Substance Abuse Treatment, 30(3), 237–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray JM, Kemp LL, Hubbard A, & Cucciare MA (2017). Developing a peer support protocol for improving veterans’ engagement to computer-delivered cognitive behavioural therapy. Behavioural and Cognitive Psychotherapy, 45, 253–265. [DOI] [PubMed] [Google Scholar]
- Reif S, Braude L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, … Delphin-Rittmon ME (2014). Peer recovery support for individuals with substance use disorders: Assessing the evidence. Psychiatric Services, 65, 853–861. [DOI] [PubMed] [Google Scholar]
- Saitz R (2005). Unhealthy alcohol use. New England Journal of Medicine, 352, 596–607. [DOI] [PubMed] [Google Scholar]
- Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, & Kazis LE (2009). Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12). Quality of Life Research, 18(1), 43–52. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Brown J, Leo GI, & Sobell MB (1996). The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug and Alcohol Dependence, 42, 49–54. [DOI] [PubMed] [Google Scholar]
- Spiro A, Rogers W, Qian S, & Kazis L (2004). Imputing Physical and Mental Summary Scores (PCS and MCS) for the Veterans SF-12 Health Survey in the Context of Missing Data, Sept. 2004, Report submitted to CMS.
- Swarbrick M, Tunner TP, Miller DW, Werner P, & Tiegreen WW (2016). Promoting health and wellness through peer-delivered services: Three innovative state examples. Psychiatric Rehabilitation Journal, 39, 204–210. 10.1037/prj0000205 [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force (2018). Unhealthy Alcohol Use in Adolescents and Adults: Screening and Behavioral Counseling Interventions. Retrieved on March 22, 2020 from: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/unhealthy-alcohol-use-in-adolescents-and-adults-screening-and-behavioralcounseling-interventions.
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine CJ, … Vos T (2013). Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet, 382, 1575–1586. [DOI] [PubMed] [Google Scholar]
- Williams EC, Rubinsky AD, Chavez LJ, Lapham GT, Rittmueller SE, Achtmeyer CE, & Bradley KA (2014). An early evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction, 109, 1472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Roos CR, Pearson MR, Hallgren KA, Maisto SA, Kirouac M, … Heather N (2017). How much is too much? Patterns of drinking during alcohol treatment and associations with post-treatment outcomes across three alcohol clinical trials. Journal of Studies of Alcohol and Drugs, 78, 59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]