Highlights
-
•
Quality improvement requires a comprehensive integrated approach.
-
•
Clinical standards are a vital first step in improving outcomes for LMICs.
-
•
Capacity building needs a range of educational courses from basic to advanced.
-
•
Evaluation tools are needed to measure progress.
Keywords: Quality improvement, Service improvement, Low and middle-income countries
Abstract
Consistent evidence has emerged over many years that the mortality and morbidity outcomes for burn patients in low and middle-income countries (LMICs) lag behind those in more resource rich countries. Interburns is a charity that was set up with the aim of working to reduce the disparity in the number of cases of burns as well as the outcomes for patients in LMICs. This paper provides an overview of a cyclical framework for quality improvement in burn care for use in LMICs that has been developed using an iterative process over the last 10 years. Each phase of the process is outlined together with a description of the tools used to conduct a gap analysis within the service, which is then used to frame a programme of capacity enhancement. Recent externally reviewed projects have demonstrated sustained improvement with the use of this comprehensive and integrated approach over a three-year cycle. This overview paper will be supported by further publications that present these results in detail.
1. Introduction
The prevention and management of burn injuries in resource–poor environments has historically been extremely challenging due to numerous factors, including limited resources, gaps in training, a lack of awareness of the extent of the problem and a tendency for the issue to fall between the various development goals. For instance, whilst most burn deaths are due to infection [1], burns are not an infectious disease and whilst burns are the most common cause of mortality in women aged 15–35 in India [2] (i.e. child-bearing age), it is not a maternal health issue. The change from the eight Millennium Development Goals (MDGs) [3] to the seventeen Sustainable Development Goals (SDGs) will hopefully help to overcome this as the death, disability, social and economic hardship and subsequent educational and employment impact resulting from burns can be linked to several of the SDGs, such as reduced inequalities, good health and well-being and partnerships for the goals [4].
Burn care and prevention in high-income countries has made enormous progress over the last 50 years. There has been a significant reduction in the number of injuries and greatly improved patient outcomes, enabling the focus to shift from survival to quality of life [5], [6], [7]. However, burn injuries are related to poverty and consequently the majority of the burden of disease is borne by people in the lowest socio-economic groups living in the poorest countries and yet there been little significant change in either the incidence or the outcomes in these regions [8], [9].
Where any sort of specialist burn services are available in low and middle-income countries (LMICs), they are frequently in the capital cities, and receive patients from across the country who need to travel significant distances to access care. These patients frequently struggle to pay for the necessary surgery, dressings, and drugs required in modern burn treatment. Whilst the centralisation of burns services into specialist units has been an appropriate development in high resource settings where the number of significant burn injuries is low, the opposite is true in many low resource settings where the incidence remains high [10]. Here a policy of decentralisation is needed, as centralised services get totally overwhelmed with patients arriving from all over the country. The development of effective burn services in secondary cities would ensure timely and equitable access to simple, safe, affordable care delivered by well-trained and motivated staff.
The authors visited and/or worked in numerous burn services in many countries across Asia, the Middle East and Sub-Saharan Africa and are acutely aware of the problems they experience in terms of being understaffed and under resourced. We have seen first-hand the differences in access to care, mortality and morbidity outcomes as outlined in the literature [6], [11]. Working within the constraints of a LMIC will inevitably put pressure on a service to demonstrate excellence in all six key components of quality in healthcare: safety, effectiveness, patient-centred, timely, efficient and equitable [12]. Over many decades modern burn care in high-income countries has developed to become highly technological and expensive; it will require equivalent years of development before most services in low-income countries can achieve the same level of care.
Interburns (International Network for Training, Education and Research in Burns), established in 2006 as an NGO and registered charity, is a global network of burn care professionals who have been working to address the enormous and unacceptable discrepancies in burn care and prevention across the world. In 2012 Interburns hosted an international consensus meeting attended by participants from 10 countries to agree standards for burn care services in LMICs as a first step to improving burn services in some of the poorest countries in the world. It is critical to understand that this process was not intended to create a dual system, one for rich countries and one for poor, but to ensure that the minimal standards that are achievable in a low resource environment are available (www.interburns.org).
The next challenge was how to develop a simple practical system that would enable the assessment of services against these agreed standards and to develop a comprehensive, integrated programme to support quality improvement and capacity building tailored to the specific needs of an individual service. Through an iterative process of action research involving a wide range of participants from multiple countries over a number of years, Interburns has developed a comprehensive, systems-based framework based on these standards. The approach combines an assessment of individual services followed by gap analysis and contextualised capacity building through education, training and research, leading to measurable improvement in service delivery.
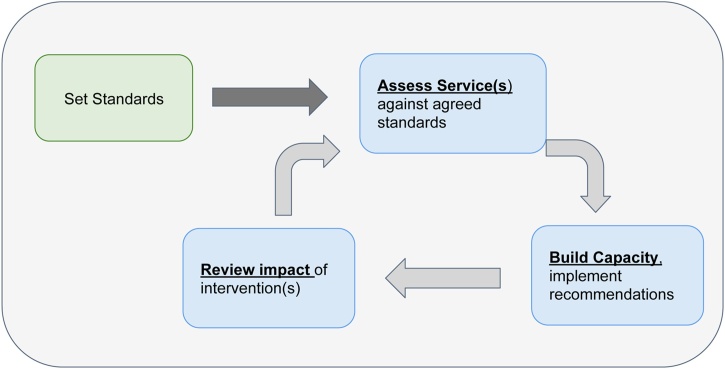
The framework, includes the following stages (see Fig. 1):
Stage 1. Define standards
Stage 2. Service evaluation and gap analysis
Stage 3. Tailored capacity building
Stage 4. Impact assessment
Fig. 1.
Cyclic nature of the framework.
The framework can be used to support recommendations at regional and national levels to seek solutions to issues that are beyond the scope of an individual service. The framework itself is also subject to regular review based on user feedback and has been refined on three occasions over a period of 5 years. This paper provides an overview of the quality improvement framework, its development and initial information on its use to date.
2. The quality improvement framework
2.1. Stage 1 – Setting and defining the standards
Twenty-nine experienced multi-disciplinary participants with leadership roles in a range of burn services from across the globe met for an international consensus meeting in Nepal in January 2012 (for full list, see Acknowledgements). The aim of the meeting was to agree a set of standards, which would support the transformation of burn care while ensuring that they would be appropriate and achievable for resource poor contexts. Although participants recognised the importance of burn prevention and pre-hospital care, including first aid, in reducing morbidity and mortality, it was agreed that these standards should focus on the care of the injured patient who required treatment in a health facility. The standards were developed as a tool to address the secondary and tertiary prevention of injury-related death and disability [13].
Over a four-day period of intense work, the group worked to:
-
•
Agree generic operational standards for burns services.
-
•
Define three different levels of burn care service (Basic, Intermediate and Advanced), including guidelines on the resources and activities necessary to ensure optimal outcomes for patients at each level.
-
•
Develop a framework for training and education programmes in burn care, to provide staff working in LMICs with the skills and knowledge necessary to meet the agreed operational standards.
The methods used included a range of participatory workshops, group presentations with immediate feedback and critique, review and amendment of proposals and summary sessions with joint reflections. Following the consensus meeting, there was a further period of 7 months during which statements were fine-tuned and schematics produced for final agreement and signed off by all participants.
Twenty-five operational standards were agreed, which are appropriate and achievable in LMICs taking into account the volume of patients and the limited resources available (see Table 1).
Table 1.
Operational standards agreed at the consensus meeting in Nepal.
| 1. | Burn patients should be assessed and treated by health care workers who had had training appropriate to the level of service their facility provides (Basic, Intermediate or Advanced). |
| 2. | Where a facility is unable to provide the required skill level, burn patients should be transferred to a facility able to offer the appropriate treatment. Burn patients should receive immediate treatment that is safe and effective before they are transferred. |
| 3. | Burn patients with other significant co-existing trauma should be managed according to WHO trauma guidelines [18]. |
| 4. | Burn patients with deep burns should be treated in a healthcare facility that can offer skin grafting. |
| 5. | Where appropriate, early excision and grafting is strongly encouraged. |
| 6. | All burn patients should receive adequate pain control from the first contact with the healthcare professional. |
| 7. | Burn patients should receive holistic treatment, which addresses all their needs in including surgical, nursing, physiotherapy, occupational therapy, dietary, psychological and medico-legal support. This is best provided by a multi-disciplinary team. |
| 8. | The provision of advanced care includes access to reconstructive surgery, advanced diagnostic facilities, blood bank, critical care, anaesthetists, hospital specialists and other services. |
| 9. | All burn care providers should ensure burn patients are mobilised, positioned and splinted as appropriate as soon as possible to minimise disability. |
| 10. | All burn care providers should ensure that burn patients receive optimal nutrition to maximise early wound healing. |
| 11. | Paediatric care and therapy should be appropriate to the unique needs of the child. |
| 12. | Burn care should be delivered according to the agreed Consensus Burn Care Clinical Guidelines [13]. |
| 13. | There should be a lead person with overall responsibility for burn care in each facility who is responsible for ensuring that the Guidelines are adhered to. |
| 14. | Facilities providing advanced care should have a designated area that is allocated only for burn patients. |
| 15. | Burn patients should be followed up by burn professionals to ensure holistic scar management, rehabilitation (physical and psychosocial) and access to reconstructive surgery following discharge from the health care facility. |
| 16. | Facilities treating burn patients should be adequately resourced, equipped and staffed to provide such care. |
| 17. | Specialist burn units should offer training and on-going support to health care professionals managing burns in other facilities within their region/district |
| 18. | Specialist burn units should participate in research programmes where appropriate. |
| 19. | Burn patient data should be recorded at all levels of health care and a national Burn Register is recommended. |
| 20. | There should be a system for on-going inspection, quality control and quality improvement for burn care facilities. |
| 21. | Health care professional involved in burn care at all levels should be engaged in burn injury prevention activities. Community involvement should be encouraged. |
| 22. | Specialist burn units and health care professionals should be engaging in policy-makers and health planners at all levels to ensure appropriate provision and delivery of burn care and burn prevention programmes. |
| 23. | The Ministry of Health should be responsible for ensuring that every burn patient in their country has access to the appropriate level of burn care to ensure equitable burn care provision. |
| 24. | The international burn care community has a critical role to play in recognising and supporting the implementation of these essential standards for burn care. |
| 25. | Burn injury disproportionately affects the poor. Fund-raising and advocacy for burn patients is essential to ensure access to appropriate care for all burn patients. Appropriate and timely burn care had been shown to significantly reduce the massive social and financial impact of burn injury. |
All standards are based on the principle that every burn patient has the right to safe and effective care, irrespective of location. The group also developed a Burn Care Resource Matrix (see Table 2) outlining the knowledge, skills and physical resources (infrastructure, equipment and supplies) required to ensure that the Operational Standards can be met at each level of facility; this is an important resource which serves as the basis for the detailed assessment of a given burn service. The levels outlined in the table are pyramidal in nature, i.e., all that is mentioned in Level 1 is included in Level 2, with Level 3 including items listed for Levels 1 and 2.
Table 2.
Burn care resource matrix.
| Capability | Knowledge | Skills | Facilities/Equipment |
|---|---|---|---|
| Level 1 Service – Basic | |||
| Prevention | • Local epidemiology of burns • Available community support (e.g., Schools, NGOs, Local Media) • Basics of primary prevention and secondary prevention |
Communication, ability to motivate local community | • Basic communication facilities, poster, banners. Etc. • Standardised paper/electronic registry form |
| First aid | • Stop, drop and roll • Application of clean cool water to the wounds • Awareness of dangerous/bad practices |
Ability to demonstrate principles of first aid | Simple props for demonstrations, such as a bucket of water |
| Assessment of burn injured patient | • History taking • ABC of immediate burn care • Assessment of other injuries • Symptoms and signs of inhalation injury • Clinical assessment of depth and surface area of burn |
• Appropriate history and clinical examination. Ability to prioritise airway (with c spine control), breathing and circulation • Ability to accurately assess size and depth of burn wound and presence of other injuries, including inhalation |
Basic medical/nursing notes. Stethoscope, blood pressure cuff |
| Simple emergency procedures | Basic airway management | • Jaw thrust, chin tilt, insertion of guedal airway, use of bag and mask • Insertion of IV cannula |
Guedal airway, bag and mask, IV fluids (saline or ringers lactate) |
| Clear communication and documentation | • Local legal requirements • Availability of local, regional burn service and contact phone numbers |
• SBAR (Situation, Background, Assessment, Response) • Clear, accurate and legible documentation |
Telephone |
| Safe transport | Local transport options, local burns services | Patient preparation for safe transport | Access to transport (taxi, rickshaw, ambulance. etc.) |
| Care of minor burns | • Analgesia, cleaning and dressing wounds • Correct positioning • Recognition of burn depth and the progression of changes in appearance • Signs and symptoms of infection |
• Basic antisepsis, hand washing • Cleaning wound and applying a dressing. Correct positioning. Assess wound for signs of infection |
• Oral and injectable analgesics • Antiseptic fluids and topical antimicrobials • Simple dressings, POP |
| Level 2 Service–Intermediate | |||
| Advanced emergency procedures | Advanced airway management, central venous catheterization, escharotomy and fasciotomy | Intubation, insertion of central line. Surgical decompression | • Laryngoscope, suction, bougey, selection of ETTs, oxygen supply • Central line kits, basic surgical set, access to theatre |
| Fluid management | Fluid resuscitation formula and maintenance fluids | Implementing and monitoring fluid balance. Insertion of urinary catheter | Urinary catheters, catheter bags, monitoring charts |
| In-patient care of minor and moderate burns | • Indications for excision and grafting of burns and prioritising areas • Management of infected burns and delayed presentations • Basics of nutrition and rehabilitation therapy • Psychosocial/social support • Specific requirements of children |
• Tangential excision and skin grafting of small/moderate surface area burns • Debridement of infected burns • Pre- and post-operative management of burns • NG feeding and nutritional supplementation • Simple contracture release and burn reconstruction • Physio-, socio- and psychotherapies • Distraction and play therapy |
• Specific ward or area of ward for patients • Watson knife, mesher • Laboratory support and blood transfusion facility • NG tubes, nutritional supplements • Specific physiotherapy area and equipment • Play area for children |
| Training of level 1 staff | Appropriate education material | Simple teaching skills and ability to motivate staff | Laptop computer, printed materials, flip chart |
| Level 3 Service–Advanced | |||
| Comprehensive management of complicated and extensive burns | • Advanced pathophysiology of burns • Inhalation injury management • Critical and intensive care • Advanced wound coverage modalities • Sophisticated nutritional supplementation • Complex reconstruction • Long term and comprehensive rehabilitation |
• Critical/intensive care skills for adults and children • Advanced Plastic and Reconstructive Surgery skills (including micro surgery) • Burns specific rehabilitation skills |
• Specialised physical plant • Designated critical care area • Dedicated burns operating theatre • Access to other specialities (e.g., renal, cardiology) • Post discharge rehabilitation facilities |
| Training of Level 2 staff | Appropriate education material | • Advanced teaching skills • Ability to motivate staff |
Digital camera, projector, lecture theatre/seminar room |
| Research and Audit | • Principles of research methodology and use of evidence informed practice • Quality improvement framework • Importance of general and targeted audit |
• Ability to design, develop and implement research projects and audit • Ability to lead quality improvement initiatives |
• IT equipment (internet access, data management software) • Data collection support • Library |
| Policy & National Planning | • Health service structure, government and non-governmental initiatives relevant to burns • Familiarity with regional burn care resources |
• Develop working relationship with health/planning ministries • Develop strategic level national framework plans • Collaboration with other burn centres in the region |
• Access to data • Administrative support |
N.B. The levels outlined in the table are pyramidal in nature, i.e., all that is mentioned in Level 1 is included in Level 2, with Level 3 including items listed for Levels 1 and 2.
2.2. Stage 2 – service assessment and gap analysis
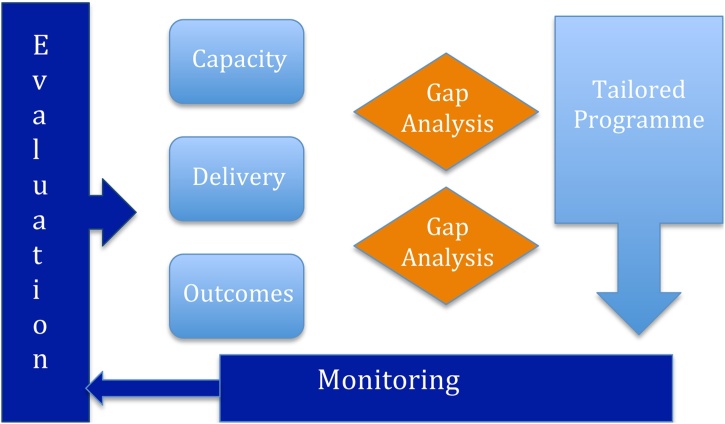
Fig. 2 summarises the participatory action research approach we use when assessing an individual service, region or country. The emphasis is on ensuring that the key personnel at each site are fully engaged with the process, and that the researchers are flexible in their approach to ensure that the local context fully informs the interpretation of the findings. Assessment considers the following key questions: – does the facility have the capacity to deliver care? Does it actually deliver quality care? What are the outcomes?
Fig. 2.
The participatory approach to service review.
A number of tools have been designed to collect the relevant information, which have been revised and refined over the last 6 years. The assessment of a service includes a Gap Analysis against the Standards, which informs a tailored programme of improvement that is put in place. Once improvement activities have taken place, the service is re-evaluated.
To ensure consistency in approach, each site undergoes an initial assessment/evaluation using a Primary Assessment Tool (PAT), based on the operational standards for burn services. The PAT collates information relating to the hospital as a whole as well as the burn service specifically, including staffing levels, training, equipment, resources and numbers for inpatient and outpatient services. The PAT provides the background information to inform and contextualise subsequent service assessment.
The main tool for evaluation of a burn service against the standards is the Delivery Assessment Tool (DAT). Interburns is now working with version 4 of the tool, following several evolutions in response to local staff in Ethiopia, Nepal, Bangladesh and the Occupied Palestinian Territories, putting a greater emphasis on discussion and participation. The process for conducting the DAT is through facilitated group discussions with members of the multidisciplinary burn team that incorporates verification of data (e.g. referencing theatre logbooks) when deemed necessary. Facilitators are trained to ensure everyone present feels confident in contributing to the discussion and giving their honest opinion.
The DAT consists of 10 sections, each covering a specific aspect of a burn service and scored on a scale from 0 to 10. The scoring in each section is based on a number of sub-sections, each of which contains a variable number of items depending on the weighting/importance attributed to that sub-section. The 10 areas are outlined in Table 3.
Table 3.
Ten subsections in the Delivery Assessment Tool.
| 1. | Policies and procedures: referral, transfer, burn ward/beds, clinical guidelines and protocols, discharge planning and follow-up, non-survivable burns and palliative care, operational and management issues |
| 2. | Burn service activities: burn prevention activities, training delivered to other services, research, and sustainability of key activities |
| 3. | Burn care team: clinical lead, multi-disciplinary team, overall team capacity, access to other specialities, team communication/team meetings, training levels of burn care team. |
| 4. | Surgery: surgical capacity, delivery of emergency surgery, early excision and skin grafting, reconstructive surgery. |
| 5. | Nursing care and assessment: nursing capacity, assessment of the burn wound, infection control, dressings and wound care, paediatric care |
| 6. | Treatment options: emergency care, critical care, pain management, nutrition, fluid resuscitation |
| 7. | Rehabilitation services: physical rehabilitation capacity, anti-contracture positioning, mobilisation, splinting, scar management, access to therapy, therapy follow-up, contractures |
| 8. | Patient support: psychosocial care, financial support for patients, social work and legal support for patients, support and consumables |
| 9. | Outcomes and data capacity: documentation data collection and management, quality improvement and audit, mortality and morbidity, patient outcome measures, patient experience outcomes, capacity for data and outcomes collection |
| 10. | Equipment and Facilities: this is a 52-item checklist of key equipment and facilities, based on the physical resources identified in the standards for each of the 3 levels of service. |
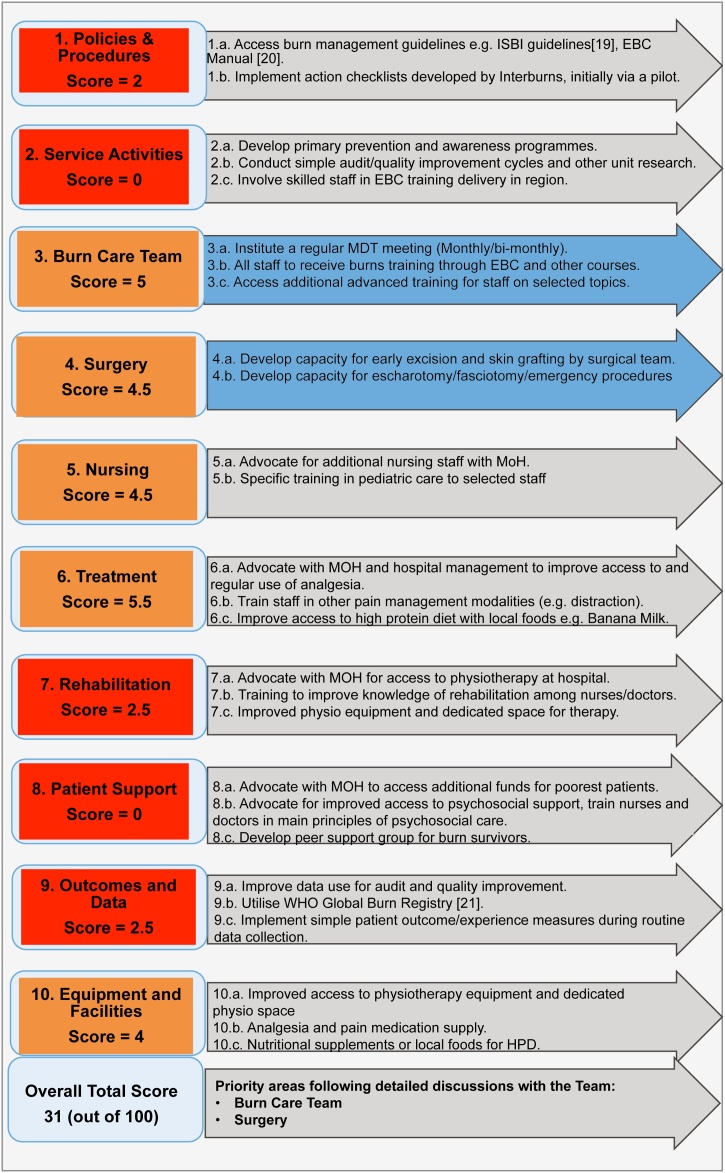
Each service receives an aggregate score out of 100, based on the scores of 0–10 in each of the 10 service areas. A summary scorecard for each service is produced that uses a coloured traffic light system, providing an accessible visual aid that allows team members to quickly identify strengths and weaknesses, and prioritise areas for quality improvement that are under their direct control. Fig. 3 gives an example how scoring in a subsection is set out: this example illustrates the scoring and traffic light system as applied to Surgery, which covers 4 key areas:
Emergency surgery – escharotomy and fasciotomy (maximum score = 2).
Early excision and skin grafting (maximum score = 4).
Burn reconstructive surgery (maximum score = 2).
Surgical capacity (maximum score = 2).
Fig. 3.
An example of scoring a subsection of DAT: subsection 4 (surgery).
Fig. 4 provides an example of a completed score card with the associated recommendations for action across all 10 subsections; this particular example reflects a facility where there are multiple areas for improvement. The scorecard is then used for discussion amongst the team members to review the findings and, more importantly, to decide what changes are within their sphere of influence and agree priorities for action. The example in Fig. 4 highlights the two key areas that were prioritised for action, these being Section 3: Burn care and Section 4: Surgery. The associated actions become the focus for service improvement, including contextualised education and training, and form the basis of the re-evaluation, which is the final stage of the process.
Fig. 4.
Example DAT gap analysis and action plan from a Regional Hospital [19], [20], [21].
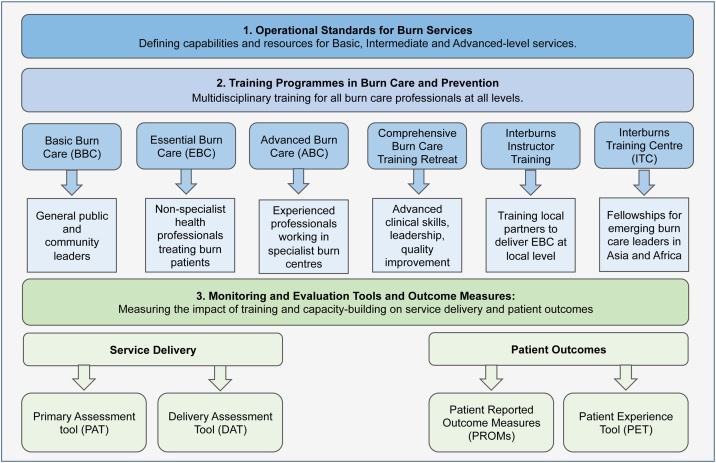
2.3. Stage 3 – Capacity building through education and training
Following initial assessment of a service and as part of the recommendations, the range of education and training opportunities are reviewed to address the areas of need. We strongly believe in the importance of appropriate education and training in order to build capacity and competence for both individual facilities and countries to improve their services [14], [15]. Interburns has developed and evaluated a range of educational courses that are both clinical and non-clinical, face-to face and online, and range from short courses on basic burn care through to residency programme as part of Clinical Fellowships (see Fig. 5). These courses have been substantially informed from the ground up and modified continuously in response to feedback. They, therefore, utilise content and delivery modes that have been developed to match the needs of the relevant audience.
Fig. 5.
Overview of the range of courses offered.
For example, parts of our Basic Burn Care© (BBC) course have been further developed in Nepal as part of a Community Burn Care and Prevention programme; local participants were involved in co-creating ways in which the content could be context specific and appeal to local communities. The Essential Burn Care© (EBC) course has been delivered in Ethiopia, Ghana, Malawi, India, Bangladesh, Cote D'Ivoire, Pakistan, Palestine and Nepal. At the more technical level, there are currently three Advanced Burn Care© (ABC) courses all of which have been delivered on more than one occasion in an LMIC (one each for surgeons, nurses and therapists: ABC Surgery, ABC Nursing and ABC Rehabilitation). Each of these courses is a 5-day modular programme designed to be highly interactive with an emphasis on participants gaining practical experience through active involvement, simulation exercises and direct patient contact. All courses have a strong emphasis on putting knowledge into action.
Following a series of international training-of-the-trainers programmes, a faculty of local instructors lead the training delivery to ensure that learning is contextualised appropriately and can be cascaded effectively to remote areas of their countries. We are increasingly working on a range of delivery methods to support these courses, such as educational videos and enhanced digital platforms, so that attendees can use the materials provided to cascade the learning to their own wider network(s) and scale up the capacity building within their own services.
We have taken a different approach by establishing International Training Centres (ITCs) that provide placements for burn-care health professionals lasting from 1 to 6 months. These ITCs are not based in the UK, but in India, Nepal and South Africa and allow all professional groups to experience a hands-on active, relevant experience. Staff from other countries and regions, e.g., Ethiopia, Uganda, Tanzania, Afghanistan and the Middle East, have already benefited from these structured placements, which include the development of a skills portfolio and a small research project. The leads from the ITCs met in November 2019 to establish an overarching framework of working that ensures that trainees have a high-quality experience, with similar opportunities for relevant experience and skill development.
Acknowledging that successful service development requires additional non-clinical skills [16], [17] we have developed a 5-day Quality Improvement and Implementation Science course, for those working in burn centres. The first of these took place in January 2019 in the UK with an international group of attendees who are required to undertake a small scale QI project in their home unit to put their skills into practice. A 15- month programme specifically designed for nurses has been held for eight nurses from Malawi and Ethiopia who attended two 5-day teaching sessions followed by small scale projects presented in a final 3-day session. These staff will be actively encouraged to present their projects to international audiences via conference opportunities.
2.4. Stage 4 – Impact evaluation
The final stage of the process is to complete an Impact Evaluation of the service after an agreed amount of time. This is carried out post activities using the same PAT and DAT tools and scorecards as used in the initial assessment. This allows facilities to track their progress against the standards. It also allows for the true cyclic nature of the framework to start, as a new gap analysis is then conducted, and a new improvement plan is made. This iterative process allows facilities to refocus attention on areas that the team agree should be the next set of priorities. As the facility team become increasingly proficient in using the tools, they can develop an annual cycle of review with ‘spot checks’ from an external or partner institution.
3. Results using the framework
The Interburns Delivery Assessment Tool was first developed, piloted and used at scale as part of a 6-year quality improvement programme in both Bangladesh and Nepal, from 2013 to 2019. The programme was funded through two consecutive UK Department for International Development (DFID) grants under the Global Poverty Action Fund and Aid Direct Fund. From 2013 to 2016, the programme covered 14 hospitals, seven each in Bangladesh and Nepal. From 2016 to 2019, 11 hospitals were covered, including eight hospitals from the previous 3 years and three new facilities. The majority of these services are intermediate and advanced-level inpatient burn services at secondary and tertiary level facilities, ranging from small regional hospitals in rural cities with fewer than 10 beds, to one of the largest burn units in the world with 400–500 inpatients.
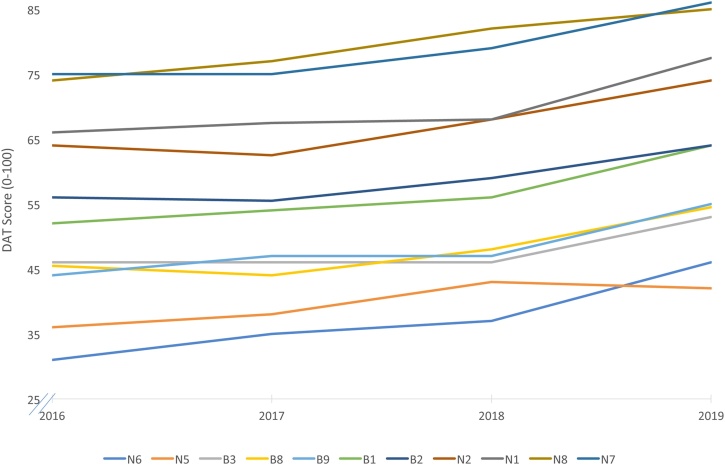
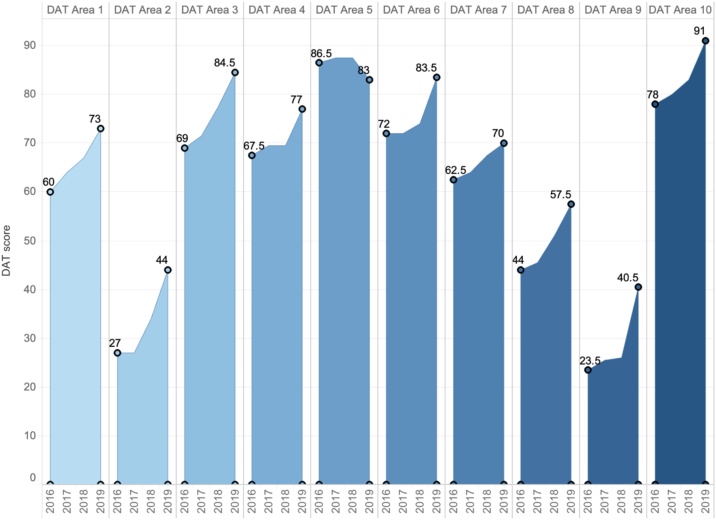
Fig. 6 illustrates some of the overall improvements that were presented in an unpublished external review of this work (commissioned by DFID). The quality of burn care provision improved in all of the project's health facilities according to the DAT scoring: the average change per burn unit was 10.4 points, with the most significant change recorded being 15.5 points, and the least improvement identified as a 6.5 points improvement. Fig. 7, from the same unpublished report, illustrates the average improvements across each of the individual sections of the DAT. The lowest scores correspond to areas 2 (Burn Service Activities) and 9 (Patient Outcome and Data Management), but these sub-sections also experienced the biggest improvements (increase of 17 points). All sections improved between 2016 and 2019, except for Section 5 on Nursing Care. Seven out of the 11 project health facilities (all six in Bangladesh and one in Nepal) scored section 5 between 0.5 and 2 points lower in 2019 compared to 2016. The reason behind this score reduction was the staff turnover or new recruitment before appropriate training had been put in place. It is clear from Fig. 6, Fig. 7 that progress can take time and is not always linear; the local context and the extent to which clinical staff can influence every sub-domain of the DAT can vary considerably. Strong leadership at national, hospital and community level are needed in order to maintain motivation to improve services. However, these projects have demonstrated tangible and measurable improvements across all supported services with a large inpatient population and will be the focus of a more detailed paper on the project, which is currently in preparation.
Fig. 6.
Overall Improvement in DAT scores. Legend: These scores give the baseline and annual cyclical review scores for hospitals in Nepal and Bangladesh over the initial and follow up implementation projects; the scores for the overall DAT range from 0 to 100.
Fig. 7.
Improvement in each of the subsections of DAT over a three-year cycle. Legend: These scores give the average baseline and final review scores over all participating facilities in Nepal and Bangladesh for each of the subsections of the DAT (scores range from 0 to 100).
4. Conclusion
This paper encompasses the work of many people over a 10-year period, who have worked together to build a framework which is comprehensive and robust, specifically addressing quality improvement in burn services which is appropriate and achievable in resource poor settings. This framework ensures that there is an unwavering focus on improving service delivery for the benefit of patients, whilst ensuring there is sustainable capacity building through appropriately designed education and training. Such a programme is constantly under review, and we are starting to see the benefits through the large numbers who have experienced this approach. We intend to publish further papers detailing the data we have collected which demonstrate improvements in knowledge, skills and attitudes to prevention and treatment. Some of our country partners are now in a position to work with their national governments to ensure that burn care – prevention, treatment and monitoring – is part of their national strategy. These are exciting developments, which bear witness to the need to use a comprehensive approach when interventions are aimed at initiating change.
The next challenge will be to consider the options for scaling up this approach across the many regions that currently lack well resourced, organised and equitably distributed burns services. As well as Nepal and Bangladesh, Interburns has worked with partners in Afghanistan, Ghana, Ethiopia, Gaza and West Bank and Sierra Leone using this framework to encourage local service development, as well as using the information gathered to support national strategy development. Scale-up of any intervention is determined by a number of factors including the intervention itself and whether it is credible, relevant, easy to undertake and provides a relative advantage. Additionally, the environment in which the intervention is to be introduced, the end user organisation, the resource organisation and the strategy devised are all key [22]. We have based our work on implementation science, endeavouring to understand the inner and outer setting, the process, the characteristics of individuals and the intervention itself as defined by the Consolidated Framework for Implementation Research [23]. This has enabled us to develop an approach that is ideally suited to the real-world environment of resource stretched and overburdened health systems in poorer countries. To facilitate scale up, taking into account the limited financial resources available, we would like to ensure that all our resources supporting service self-evaluation are made available on-line as a free tool, that we increase the availability of on line learning and continue to disseminate training of trainers to allow local delivery of both Basic Burn Care© and Essential Burn Care© as well as seek further funding to continue to develop and deliver Advanced Burn Care© training. Finally, we would urge others involved in helping to improve burn care services in some of the poorest countries in the world to utilise this approach.
Conflict of interests
There are no conflicts of interest for any of the authors.
Funding
This project was funded by:
DFID Global Poverty Action Fund, Innovation Window. GPAF-INN-034 ‘Improving outcomes for 10,000 burn patients in Bangladesh and Nepal’ (2013–2016).
DFID Aid Direct, Community Partnerships Window. UKAD-INN-079 ‘Reducing mortality and morbidity from burn injuries by transforming national programmes of burn care and prevention in Bangladesh and Nepal’ (2016–2019).
DFID Small Charities Challenge Fund. ‘Implementing a comprehensive national strategy for burn care and prevention in Ethiopia’ (2018–2020).
Wales for Africa grant: ‘Improving national burn care and prevention in Ghana’ (in partnership with Korle-Bu Teaching Hospital, Accra) (2015–2016).
The National Institute for Health Research (NIHR), NIHR Global Health Research Group on Burn Trauma, Grant Reference 16/137/110. The views expressed are those of the authors and not necessarily those of the NIHR of the Department of Health and Social Care.
Acknowledgements
The authors would like to thank the following people who attended the original consensus meeting in Nepal in January 2012, their work was fundamental to the development of the Standards:
India
Dr Shobha Charmania, General Surgeon
Dr Rajeswari Dharmarajan, Burns Surgeon
Dr Sachin Jamma, Plastic Surgeon
Professor Sazzad Khondoker, Plastic Surgeon
Bangladesh
Professor A.J.M. Salek, Plastic Surgeon
Ms Monira Rahman, Executive Director, Acid Survivors Foundation
Dr Kishor Kuma Das, Plastic Surgeon
Canada
Dr Tim Spoule, Plastic Surgeon
Dr Redouane Bouali, Critical Care Specialist
Dr Shala Yekta, Senior Researcher
Egypt
Dr Amr Moghazy, Plastic Surgeon
Nepal
Dr Keshav Das Joshi, General Surgeon
Dr Khima Nand Joshi, General Surgeon
Ms Pernilla Ardeby, Paerdiatric Nurse
Ms Nara Devi Bariya, Burns Nurse
Dr Ramnandan Prasad Chaudhary, Paediatric Surgeon, Nepal
Dr Shankar Rai, Plastic Surgeon, Nepal
Mr Stephen Knoble, Medical training Consultant, Nepal
Pakistan
Dr Shariq Ali, Emergency Medicine
Nigeria
Dr Richard Nnabuko, Plastic Surgeon
South Africa
Dr Elbie Van der Merwe, Burns Surgeon, South Africa
United Kingdom
Dr Bruce Richard, Paediatric Plastic Surgeon
Dr Sian Falder, Paediatric Plastic Surgeon
Professor Patricia Price, Health Psychologist
RuthAnn Fanstone, Physiotherapist
Richard Bendell, Director of Operations, Interburns
Dr Tom Potokar, Plastic Surgeon and Director Interburns
Mr Greg Healey, Businessman, Interburns
United States of America
Dr Michael Peck, Burns Surgeon
The authors would like to thank everyone who has given so generously of their time through their participation and enthusiasm for the project, in each of the countries where we have worked.
References
- 1.Lachiewicz A.M., Hauck C.G., Weber D.J., Cairns B.A., van Duin D. Bacterial infections after burn injuries: impact of multidrug resistance. Clin Infect Dis. 2017;65(12):2130–2136. doi: 10.1093/cid/cix682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanghavi P., Bhalla K., Das V. Fire-related deaths in India in 2001: a retrospective analysis of data. Lancet. 2009;373(9671):1282–1288. doi: 10.1016/S0140-6736(09)60235-X. [DOI] [PubMed] [Google Scholar]
- 3.The World Health Organisation millennium development goals. https://www.who.int/topics/millennium_development_goals/about/en/ [accessed 15.05.20].
- 4.The World Health Organisation sustainable development goals. https://www.who.int/sdg/en/ [accessed 15.05.20].
- 5.Pereira C., Murphy K., Herndon D. Outcome measures in burn care. Is mortality dead? Burns. 2004;30(8):761–771. doi: 10.1016/j.burns.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 6.Smolle C., Cambiaso-Daniel J., Forbes A.A., Wurzer P., Hundeshagen G., Branki L.K. Recent trends in burn epidemiology worldwide: a systematic review. Burns. 2016;43(2):249–257. doi: 10.1016/j.burns.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spronk I., Legemate C., Oen I., van Loey N., Polinder S., van Baar M. Health related quality of life in adults after burns: a systematic review. PLOS ONE. 2018;13(5):e0197507. doi: 10.1371/journal.pone.0197507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization, 2015. Burns. http://www.who.int/violence_injury_prevention/other_injury/burns/en/ [accessed 19.11.19].
- 9.Golshan A., Patel C., Hyder A.A. A systematic review of the epidemiology of unintentional burn injuries in South Asia. J Public Health. 2013;35(3):384–396. doi: 10.1093/pubmed/fds102. [DOI] [PubMed] [Google Scholar]
- 10.Meara J.G., Leather A.J.M., Hagander L., Alkire B.C., Alonso N., Ameh E.A. Global Surgery 2030: evidence and solutions for achieving health, welfare and economic development. Lancet Comm. 2015;386(9993):569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 11.Stokes M.A.R., Johnson W.D. Burns in the third world: an unmet need. Ann Burns Fire Disasters. 2017;30(4):243–246. [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organisation . World Health Organisation; Geneva: 2006. Quality of care: a process for making strategic choices in health systems. ISBN 92 4 156324 9 (NLM classification: W 84.1) ISBN 978 92 4 156324 6. [Google Scholar]
- 13.Potokar T., editor. Setting standards for burn care services in low and middle income countries. Interburns ©; 2013. https://aidstream.org/files/documents/Interburns%20Standards%20Report%202013.pdf. [Google Scholar]
- 14.Burdick W., Morahan P.S., Norcini J.J. Capacity building in medical education and health outcomes in developing countries: the missing link. Educ Health. 2007;20(3):65. PMID: 18080954. [PubMed] [Google Scholar]
- 15.Kerry V.B., Ndung’u T., Walensky R.P., Lee P.T., Kayanja V.F.I.B., Bangsbery Managing the demand for global health education. PLoS Med. 2011;8(11):e1001118. doi: 10.1371/journal.pmed.1001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beane A., Wagstaff D., Abayadeera A., Wijeyarante M., Ranasinghe G., Mirando S. A learning health systems approach to improving the quality of care for patients in South Asia. Global Health Action. 2019;12:1587893. doi: 10.1080/16549716.2019.1587893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones B., Vaux E., Olsson-Brown A. How to get started in quality improvement. BMJ. 2019;364:k5408. doi: 10.1136/bmj.k5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mock C., Lormand J.D., Goosen J., Joshipura M., Peden M. World Health Organization; Geneva: 2004. Guidelines for essential trauma care. ISBN 92 4 154640 9. [Google Scholar]
- 19.ISBI Practice Guidelines Committee ISBI practice guidelines for burn care. Burns. 2016;42(5):953–1021. doi: 10.1016/j.burns.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 20.Essential Burn Care Manual. Available from: www.interburns.org/trainnig.
- 21.World Health Organisation: Global burn registry. Available from: https://www.who.int/violence_injury_prevention/burns/gbr/en/.
- 22.Simmons R., Fajans P., Ghiron L., editors. Scaling up health service delivery from pilot innovations to policies and programmes. World Health Organisation; Geneva: 2007. [Google Scholar]
- 23.Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]