Abstract
Purpose:
Since the declaration of the lockdown due to COVID-19, the usage of digital devices has gone up across the globe, resulting in a challenge for the visual systems of all ages. The purpose of this study is to assess the impact of the lockdown on digital device usage, and consequently, the ocular surface health implications and circadian rhythm abnormalities related to digital eye strain.
Methods:
An open online survey was sent through various social media platforms and was open for a period of 2 weeks.
Results:
A total of 407 usable responses were obtained; the average age of respondents was 27.4 years. Typically, 93.6% of respondents reported an increase in their screen time since the lockdown was declared. The average increase in digital device usage was calculated at about 4.8 ± 2.8 h per day. The total usage per day was found to be 8.65 ± 3.74 hours. Sleep disturbances have been reported by 62.4% of people. Typically, 95.8% of respondents had experienced at least one symptom related to digital device usage, and 56.5% said that the frequency and intensity of these symptoms increased since the lockdown was declared.
Conclusion:
The study highlighted the drastic increase in use of digital devices after the initiation of the COVID-19 lockdown, and along with it, the slow deterioration of ocular health across all age groups. Awareness about prevention of digital eye strain should be stressed, and going forward, measures to bring these adverse effects to a minimum should be explored.
Keywords: Computer vision syndrome, COVID-19, digital eye strain, ocular surface health
With time and the advent of technology, the usage of computers, laptops, tablets, and smartphones has seen a steady increase in the past few years. These digital devices require to be held at a distance that is intermediate between near and distance vision, thereby causing strain on the visual system, which is designed for comfortable near and distant vision. The emergence of the COVID-19 pandemic and the worldwide lockdown was immediately followed by a drastic increase in the amount of time spent on these gadgets.
According to the American Optometric Association, as little as two hours of continuous digital device usage per day is enough to bring about the development of an array of eye and vision related problems, and is referred to as digital eye strain.[1] Prolonged usage of these devices is not only a stressor on the visual system but also causes musculoskeletal strain[2,3,4] and circadian disturbances,[2,5,6] and these make up the umbrella diagnosis of computer vision syndrome (though the terms digital eye strain and computer vision syndrome are often used interchangeably throughout the literature).
This study has been conducted to evaluate the impact of the worldwide lockdown on the duration of usage of these devices, and consequently, its effect on ocular surface health and circadian rhythm. The studies so far on this subject have dealt with the student population, or targeted working professionals in a single field. This is the first study of its kind that targets the general population and includes people in all walks of life, since digital device usage is not restricted to just one demographic.
Pathophysiology of digital eye strain
Digital eye strain is a manifestation of evaporative dry eye[7] caused by decreased and incomplete blink rate leading to ocular surface compromise, and asthenopic symptoms[8] caused by a visual system in a constant state of accommodation and convergence. Other environmental factors, such as poor ergonomics, improper lighting, glare, decreased humidity in air-conditioned rooms,[9] are all contributing factors for worsening of these symptoms. Uncorrected refractive errors,[10] contact-lens wearers,[11] people with a history of ocular illnesses,[12] diabetics,[13] female gender,[13] and autoimmune diseases are at risk for the development of more and severe symptoms than their age-matched counterparts.
Digital device usage causes the blink rate to fall significantly,[14,15] and because of this, the meibomian glands are not mechanically stimulated as often to release a proper lipid layer, and there is a fall in the rate of replenishment of the tear film. While working on computers, the gaze angle tends to be higher[8] than what normal near work usually demands, the palpebral aperture is vertically larger, leading to faster evaporation and incomplete blinking. Incomplete blinking fails to distribute the tear film properly, resulting in an unstable tear film,[16] which, coupled with an inadequate lipid layer, presents with dryness of eyes, grittiness or foreign body sensation, burning, and itching of eyes.
The other component is the strain on the ocular muscles, both internal and external. The constant near work demands the eye to always be in a state of accommodation, while the accompanying required convergence taxes the extraocular muscles. When this state is maintained for extensive periods of time, the fluidity of the visual motor system is fatigued[8] and causes eye strain and headache.
Blurring of vision and double vision can be explained by eye fatigue, dry eye symptoms, or an inability of accommodation to relax, causing difficulty in focusing at varied distances.[17] Increased sensitivity to light, glare, colored halos around bright light are caused due to a disparity in the air–tear film refractive interface.
The continuous exposure to blue light emitted by these devices, though not proven to be hazardous, has raised concerns regarding cumulative phototoxicity. Light exposure causes disturbances in the secretion of melanin by melanocytes in the pineal gland, which are controlled by melanopsin-containing photosensitive ganglion cells of the retina. These cells are sensitive to light in the wavelength of 482 nm, falling within the blue light spectrum.[17]
Methods
The survey was aimed at individuals above the age of 18 who used digital devices. Exclusion criteria included people on treatment for glaucoma,[18] contact lens wearers,[19] and people who had undergone LASIK or other ocular surgeries that may affect ocular surface health. Using the formula 4 pq/d2, taking prevalence as 80%, and d as 5% of prevalence, sample size was calculated as 400.
On being approved by the Institutional Human Ethics Committee, an open online survey using Google Forms was sent to people on social media platforms (WhatsApp, Facebook, Instagram). Different demographics of people were targeted so as to get a sample representative of each of the subgroups – students, medical and paramedical staff, nonmedical working professionals, and others. The link to the survey was sent to the personal WhatsApp numbers of medical students, engineering and arts college students, employees of IT companies, engineers, doctors, interns, nurses and posted on a few WhatsApp groups frequented by homemakers; they were all encouraged to send it forward.
Informed consent included the minimum age for participation in the study, why the study was conducted and assurance of confidentiality of the data. It consisted of 14 questions and was open for a period of two weeks. Multiple responses could not be submitted from the same IP address. Only completed questionnaires (2.6MB, pdf) were considered for the study. Data was analyzed using SPSS software version 13. Pearson's correlation was used to find the association between variables. Chi-square test was applied on categorical variables. A value of P ≤ 0.05 was considered significant.
Results
A total number of 520 responses were recorded, out of which 407 were considered for the study after applying exclusion criteria. Out of the 407 people who responded, 55.5% (226/407) were male and 44.5% (181/407) were female. Of the respondents, a majority of 58% (236/407) belonged to the age group 19–26, 24.8% (101/407) belonged to 27–34 years, 11.8% (48/407) were between 35 and 42 years of age, and 5.4% (22/407) were above 42 years of age.
Typically, 36.4% (148/407) of respondents were students including medical undergraduates; 14.5% (59/407) were medical professionals and included interns, residents and higher; 36.9% (150/407) were nonmedical working professionals; and the rest, 12.3% (50/407) included homemakers and a few people who were temporarily unemployed because of the worldwide pandemic.
Of the study population, 45.5% (185/407) of people were already aware of an entity called computer vision syndrome or digital eye strain. Among the people claiming to have prior knowledge of computer vision syndrome, only less than half 41.62% (77/185) were aware that breaks need to be taken every 20 minutes while working on digital devices. The salient findings of the study have been depicted in Figs 1-4.
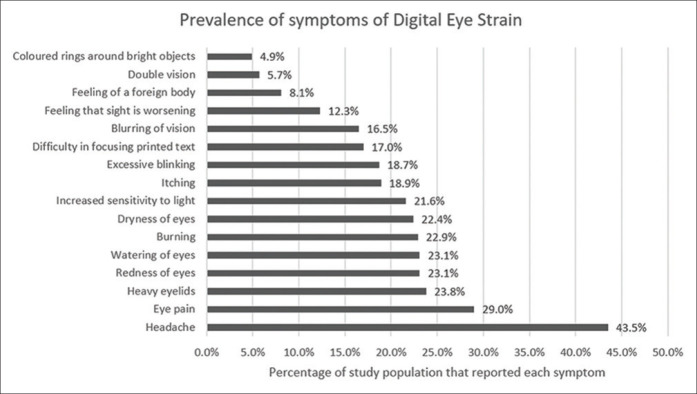
Figure 1.
Comparison of prelockdown and postlockdown digital device usage in all four subsets of study population
Figure 4.
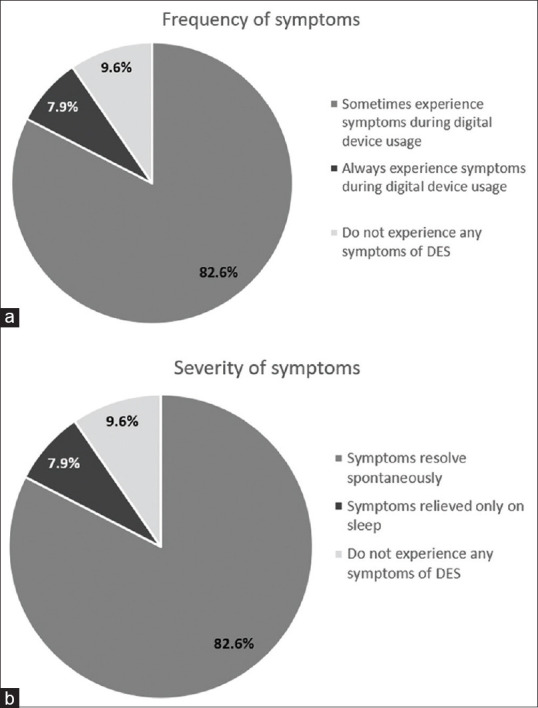
Pie chart depicting the (a) frequency of symptoms, and (b) severity of symptoms of digital eye strain experienced by the study population
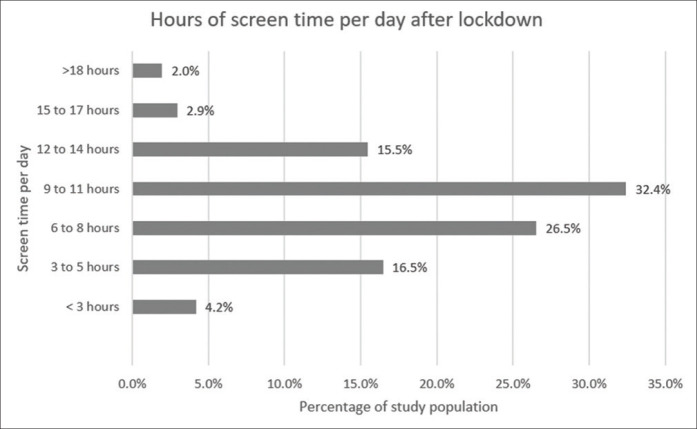
Figure 2.
Graph depicting the frequency with which each symptom of digital eye strain was experienced by the study population
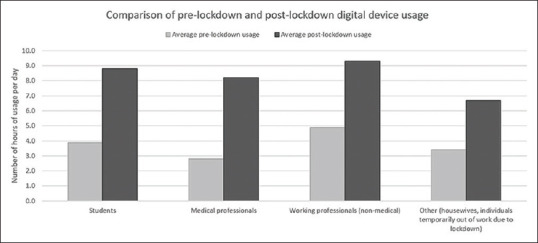
Figure 3.
Graph showing the proportion of study population according to their total screen time per day after lockdown
Effect of the lockdown on screen time
It was noted that 93.6% (381/407) of respondents logged an increase in their digital device usage after the lockdown was initiated. The respondents have logged an average of 4.8 ± 2.8 hours of increase in usage per day, making the total amount of screen time per day 8.65 ± 3.74 hours. It is remarkable that overall digital device usage increased from prelockdown usage by 5 hours or more among 51.1% (208/407) of respondents, of which 40.9% (85/208) were students.
The student population have logged an average increase in usage of 5.18 ± 2.89 hours per day, bringing their daily usage to 8.9 ± 3.63 hours. In total, 49.3% (73/148) of the student population mostly use digital devices for educational purposes (online classes, assignments, webinars).
In total, 62.41% (254/407) of respondents have said that digital device usage prevented them from going to sleep at an optimal time. It is alarming that 65.68% (155/236) people below the age of 26 suffer from sleep pattern disturbances due to digital device usage.
Students are most affected in this regard, with 66.9% (99/148) of the student population reporting an inability to fall asleep on time. This is followed by the working professionals in the nonmedical field, where 64.7% (97/150) suffered from sleep disturbances. This population logged an average of 9.28 ± 3.42 hours of screen time per day, of whom 68% (102/150) claimed that it was work related.
A small fraction of people, 6.63% (27/407), reported no change in their screen time after lockdown. Among these, the majority of this population, 37% (10/27), were understandably homemakers, followed surprisingly closely by the student population 29.6% (8/27), who were already logging around 6 to 7 hours of screen time before the lockdown was declared.
Symptoms of digital eye strain
Sixteen symptoms[20] related to digital eye strain (headache, eye pain, heavy eyelids, redness of eyes, watering of eyes, burning sensation, dryness of eyes, increased sensitivity to light, itching, excessive blinking, difficulty in focusing printed text, blurring of vision, feeling that sight is worsening, feeling of a foreign body or grittiness of eyelids, double vision, colored rings around bright objects) were included in the questionnaire (2.6MB, pdf) . Males reported an average of 2.81 ± 2.54 symptoms, while females reported 3.5 ± 2.78 symptoms, and this difference was found to be statistically significant (P = 0.009).
The correlation between increase in screen time and number of symptoms was found to be statistically significant (P = 0.001). As the screen time increased, there was a statistically significant increase in both frequency of symptoms (P = 0.028) and intensity of symptoms (P = 0.005). Sleep disturbances were increasingly reported by people with a higher screen time, this was also found to be statistically significant (P = 0.001).
In total, 95.8% (368/407) of respondents have experienced at least one symptom related to digital device usage, and 56.5% (230/407) said that the frequency and intensity of these symptoms have increased since the lockdown was declared. The mean usage among this population was 9.3 ± 3.5 hours; and it predominantly consisted of the student community 60% (138/230).
Discussion
The sudden increase in usage of digital devices, and the overall number of hours of screen time logged per day have been due to a shift of professional and social activities to a web-based platform after the advent of the novel coronavirus. This includes online conference calls, meetings, webinars, online classes, assignments done on digital devices, work from home, personal and social video calls, online shopping, leisure, and entertainment.
In total, 90.42% (368/407) of the respondents experienced at least one symptom associated with digital device usage. This is higher than the prevalence reported in previous studies.[21,22] In 2014, a study conducted in Chennai by Logaraj et al.[22] reported a prevalence of 81.9% among engineering students and 78.6% among medical college students. The significant shift can be explained by the increase in duration of digital device usage among the participants of the study. Their study reported less than four hours of screen time per day for 85% of medical students and 46% of engineering students, while the student population in our study have logged an average of 8.9 ± 3.63 hours of usage per day.
In our study, it was noted that females were more affected than males (P = 0.009). This can be attributed to the higher incidence of dry eye in females,[13,23] preponderance of autoimmune conditions associated with dry eyes among females,[24,25] and make-up-related ocular health issues. The association between cosmetic usage and dry eye has revealed a migration of the product onto the surface of the eyes, and this, coupled with the chemistry of compounds used in such preparations, is associated with tear film instability, leading to dry eye.[26] Headache disorders are more commonly seen in females[27] and may account for a few of the symptoms such as sensitivity to light, headache, glare, blurring of vision. The higher incidence of symptoms in females is similar to findings of most of the previous studies.[28,29,30] Interestingly, in the study conducted by Logaraj et al.,[22] males showed a higher prevalence of dry eye.[22]
It was noted that between the student population and the nonmedical working population, despite having comparable total screen time per day with 8.8 ± 3.6 hours, and 9.3 ± 3.4 hours; the former has reported 3.9 ± 3.2 symptoms, while the latter has reported 3.4 ± 2 symptoms. The student population is considerably more symptomatic, and this can be attributed to the abrupt increase in screen time of students, who are previously unaccustomed to spending long consecutive hours on digital devices.
In our study, the most common symptom was headache, affecting 43.5% (177/407) of the population. Headache could be a presentation of eye strain, undiagnosed refractive errors, or simply a result of exposure to continuous bright light for unnatural periods of time. This is on par with the occurrence of headache reported by the study conducted in Chennai in 2014,[22] and significantly higher than the prevalence reported in Ethiopia in 2018.[12]
Eye pain was experienced by 29% (118/407) of people, which can be explained by the undue strain on the intrinsic muscles of accommodation, which cannot fully relax under the viewing distances of digital devices. This is significantly less than the 47.63% prevalence reported by Dessie et al.[12], and this might be explained in part by the fact that contact lens wearers were not excluded from their study. Another factor may be the paucity of breaks in an office environment as compared to usage of devices at home during the lockdown. Office ergonomics might also be implicated.
Blurring of vision has been reported by 16.5% of the population, and this is more than the occurrence reported by Talwar et al., at 13.2%. On the other hand, the study by Logaraj et al.[22] saw 16.4% of medical students and 31.6% of engineering students experiencing this symptom.
In total, 23.8% (97/407) of people said that they experienced heavy eyelids. Besides the obvious fact that heavy eyelids are seen frequently in people with dry eye disease, it is interesting to note that 74.2% (72/97) of this population have sleep disturbances related to digital device usage, and heavy eyelids could be a manifestation of fatigue due to poor sleep pattern. Sleep pattern disruption was more frequent in individuals who reported a longer screen time, as reported by numerous studies.[2,31]
Limitations
The subjects did not undergo refraction and were not examined by an ophthalmologist, and pre-existing refractive errors,[10] ocular surface disorders, and vitamin deficiencies could have contributed to the severity of the symptoms experienced. The study only concentrated on symptoms, and many people with severe dry eye only complain of mild symptoms;[32] hence, leading to underdiagnosis in a self-reported survey. This study only dealt with digital eye strain and the circadian disturbances that arise along with prolonged hours of screen time and does not handle musculoskeletal issues that arise from poor posture that goes hand in hand with these issues.
The survey was aimed at all consenting adults above the age of 18, but with social distancing norms in place, the most affected population have been children in the school going age. These children will have to be followed up for the possible development of myopia resulting from prolonged hours of near work,[33] stressing the developing visual system. The effect of the rays emitted by these devices on the young retina has already raised concerns and needs further evaluation.
Prevention and management of digital eye strain
Digital eye strain or even computer vision syndrome is a classic example of a preventable, lifestyle-induced health issue and measures to curb the symptoms is the need of the hour. A variety of measures can be taken by an individual to limit the impact of digital eye strain on the visual system. The most important one is to voluntarily remember to blink at certain intervals. Forceful blinking during screen time can be encouraged, since this squeezes the meibomian glands, and the lipid layer of the tear film is well formed, which can help with evaporative dry eye. Proper positioning of the desktop, so that it is 4–5 inches below eye level, ensures that most of the globe is protected by the eyelids, and only a small inferior portion is exposed to environmental drying forces.[3]
Focusing on distant objects at intervals decreases the accommodative effort of the eyes for a while and prevents eye pain and headache. A rule of thumb is the 20-20-20 rule, which says that after every 20 minutes of screen time, a person should take a a 20 second break to focus on an object located 20 feet away. For a person who works continuously on the desktop for more than 8 to 10 hours a day, a pair of dedicated “computer glasses” might be the way to go. These are simply a pair of prescription lenses with a small plus power (+0.25D to +0.5D) that a person can wear while working on the desktop that will require a less accommodative effort from the eyes, though these have not yet seen mainstream usage.
The circadian rhythm disturbances can be controlled to an extent using in-built blue light filters in the devices themselves, or plain glasses with a slight yellow tint, called “blue light filter glasses.” These glasses do not need a prescription, since they are plain glasses with a slight yellow tint. The use of these might just be limited to reducing circadian disturbances[17] over anything else. The AAO does not recommend any special eyewear for digital eye strain till date.
Other measures include a warm fomentation followed by a gentle eyelid massage once or twice daily, which can help in healthy functioning of the tarsal glands. A preservative-free artificial tear preparation can be recommended. People who wear contact lenses can be asked to switch to glasses while working on screens as much as possible.
A few apps do exist, both for use on smartphones and desktops, that remind you to take a break at customized fixed intervals, and these could be used to lessen the occurrence of symptoms. For those working from home, a makeshift “office space” with a proper screen positioning, table height, ergonomic seating arrangements, and optimal lighting will lessen the strain on the eyes while also helping to avoid issues caused by bad posture.
Whenever possible, podcasts can be preferred over video classes to eliminate the visual strain. For an avid reader, increasing the font size and improving contrast on any interface will help relieve the eye strain to a great extent. Audiobooks might be a suitable alternative to long hours spent in front of a screen. Television, while it comes with its own list of disadvantages, is, in this case, the lesser of two evils and can be used whenever screen sharing or data transfer is possible.
It is well established that the cause of most of these symptoms is a result of evaporative dry eye caused by a drastic fall in the blink rate, which then leads to a cascade of other issues. Further studies in this field must deal with the question of bringing the blink rate to near-normal values and ensuring a complete blink each time. A Pavlovian technique could be developed, in which subjects are given a mild tactile stimulus which can be conditioned to lead to blinking. Of course, such a development would need months of training to result in a conditioned reflex, but considering the plethora of silent sufferers with digital eye strain, and the fact that this number is only going to increase in the near future, this might be a good place to start.
Conclusion
Our study highlights the increase in use of digital devices after the initiation of the COVID-19 lockdown, and along with it, the slow deterioration of ocular health across all age groups. Measures are warranted to disseminate awareness about the prevention of digital eye strain and minimize the adverse effects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors thank Dr. Deepa Srinivasan for the data analysis.
References
- 1.Computer vision syndrome (CVS) American Optometric Association [Online] Available from: http://wwwaoaorg/x5374xml . Last cited on 2020 Aug 24.
- 2.Patil A, Bhavya, Chaudhury S, Srivastava S. Eyeing computer vision syndrome: Awareness, knowledge, and its impact on sleep quality among medical students. Ind Psychiatry J. 2019;28:68–74. doi: 10.4103/ipj.ipj_93_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loh K, Redd S. Understanding and preventing computer vision syndrome. Malays Fam Physician. 2008;3:128–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Wapa A, Namgyal A. Computer vision syndrome: Affecting young and old alike. Delhi Journal of Ophthalmology. 2018;29:74–5. [Google Scholar]
- 5.Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci USA. 2015;112:1232–7. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenfield M. Computer Vision syndrome aka. Digital Eye Strain Optometry in Practice. 2016;17:1–10. [Google Scholar]
- 7.Akkaya S, Atakan T, Acikalin B, Aksoy S, Ozkurt Y. Effects of long-term computer use on eye dryness. North Clin Istanb. 2018;5:319–22. doi: 10.14744/nci.2017.54036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhootra AK. Basics of Computer Vision Syndrome New Delhi, India: Jaypee Brothers Medical Publishers, 2014 ISBN 978-93-5152-413-7 [Google Scholar]
- 9.Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: A review. Surv Ophthalmol. 2005;50:253–62. doi: 10.1016/j.survophthal.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Rosenfield M. Computer vision syndrome: A review of ocular causes and potential treatments. Ophthalmic Physiol Opt. 2011;31:502–15. doi: 10.1111/j.1475-1313.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- 11.Kojima T. Contact lens-associated dry eye disease: Recent advances worldwide and in Japan. Invest Ophthalmol Vis Sci. 2018;59:DES102–8. doi: 10.1167/iovs.17-23685. [DOI] [PubMed] [Google Scholar]
- 12.Dessie A, Adane F, Nega A, Wami SD, Chercos DH. R Factor-Litvak., editor. Computer vision syndrome and associated factors among computer users in Debre Tabor Town, Northwest Ethiopia Pam. J Environ Public Health. 2018;2018 doi: 10.1155/2018/4107590. 4107590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah S, Jani H. Prevalence and associated factors of dry eye: Our experience in patients above 40 years of age at a tertiary care center. Oman J Ophthalmol. 2015;8:151–6. doi: 10.4103/0974-620X.169910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci. 1991;68:888–92. doi: 10.1097/00006324-199111000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Freudenthaler N, Neuf H, Kadner G, Schlote T. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol. 2003;241:914–20. doi: 10.1007/s00417-003-0786-6. [DOI] [PubMed] [Google Scholar]
- 16.Hirota M, Uozato H, Kawamorita T, Shibata Y, Yamamoto S. Effect of incomplete blinking on tear film stability. Optom Vis Sci. 2013;90:650–7. doi: 10.1097/OPX.0b013e31829962ec. [DOI] [PubMed] [Google Scholar]
- 17.Sheppard AL, Wolffsohn JS. Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang X, Vadoothker S, Munir WM, Saeedi O. Ocular surface disease and glaucoma medications: A clinical approach. Eye Contact Lens. 2019;45:11–8. doi: 10.1097/ICL.0000000000000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guillon M, Maissa C. Dry eye symptomatology of soft contact lens wearers and nonwearers. Optom Vis Sci. 2005;82:829–34. doi: 10.1097/01.opx.0000178060.45925.5d. [DOI] [PubMed] [Google Scholar]
- 20.Seguí M del M, Cabrero-García J, Crespo A, Verdú J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol. 2015;68:662–73. doi: 10.1016/j.jclinepi.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Noreen K, Batool Z, Fatima T, Zamir T. Prevalence of computer vision syndrome and its associated risk factors among under graduate medical students of Urban Karachi. Pak J Ophthalmol. 2016;32:140–6. [Google Scholar]
- 22.Logaraj M, Madhupriya V, Hegde SK. Computer vision syndrome and associated factors among medical and engineering students in Chennai. Ann Med Health Sci Res. 2014;4:179–85. doi: 10.4103/2141-9248.129028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shanti Y, Shehada R, Bakkar MM, Qaddumi J. Prevalence and associated risk factors of dry eye disease in 16 northern West bank towns in Palestine: A cross-sectional study. BMC Ophthalmol. 2020;20:26. doi: 10.1186/s12886-019-1290-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang H, Wang PB, Chen T, Zou J, Li YJ, Ran XF, et al. Analysis of clinical characteristics of immune-related dry eye. J Ophthalmol. 2017;2017:8532397. doi: 10.1155/2017/8532397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matossian C, McDonald M, Donaldson KE, Nichols KK, MacIver S, Gupta PK. Dry eye disease: Consideration for women's health. J Women's Health. 2019;28:502–14. doi: 10.1089/jwh.2018.7041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang MT, Craig JP. Investigating the effect of eye cosmetics on the tear film: Current insights. Clin Optom (Auckl) 2018;10:33–40. doi: 10.2147/OPTO.S150926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmed F. Headache disorders: Differentiating and managing the common subtypes. Br J Pain. 2012;6:124–32. doi: 10.1177/2049463712459691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eyes Overexposed: The Digital Device Dilemma. (2016) Retrieved from Vision Impact Institute. https://visionimpactinstituteorg/wp-content/uploads/2016/03/2016EyeStrain_Report_WEBpdf .
- 29.Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthalmic Physiol Opt. 2012;32:375–82. doi: 10.1111/j.1475-1313.2012.00925.x. [DOI] [PubMed] [Google Scholar]
- 30.Sen A, Richardson S. A study of computer-related upper limb discomfort and computer vision syndrome. J Hum Ergol. 2007;36:45–50. [PubMed] [Google Scholar]
- 31.Yogesh S, Abha S, Priyanka S. Mobile usage and sleep patterns among medical students. Indian J Physiol Pharmacol. 2014;58:100–3. [PubMed] [Google Scholar]
- 32.Messmer EM. The Pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112:71–82. doi: 10.3238/arztebl.2015.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children-A systematic review and meta-analysis. PLoS One. 2015;10:e0140419. doi: 10.1371/journal.pone.0140419. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.