Abstract
Introduction:
The World Health Organization’s Eastern Mediterranean Office (EMRO) developed a school mental health program (SMHP) to help reduce the regional burden of child and youth mental health problems. Designed in collaboration with international consultants, the SMHP draws on evidence-based interventions to train school personnel to identify students in need, respond therapeutically, and engage families in seeking care.
Methods:
Teams from Pakistan, Egypt, Iran, and Jordan collaborated with WHO EMRO and British and US universities to form the School Health Implementation Network: Eastern Mediterranean Region (SHINE), an NIMH-funded global mental health hub. SHINE partners used a “theory of change” process to adapt the SMHP to be more readily taken up by school personnel and spread with fidelity. The adapted SMHP more directly addresses teachers’ priorities and uses technology to facilitate training.
Results:
A cluster-randomized implementation-effectiveness trial enrolling 960 children ages 8–13 in 80 Pakistani schools will test the adapted SMHP against the original. Children who screen positive on first the teacher and subsequently the parent Strengths and Difficulties Questionnaires (SDQs) will be enrolled and tracked for 9 months. The primary trial outcome is reduction in parent-rated SDQ total difficulties scores. Secondary outcomes include children’s wellbeing, academics, absenteeism, stigma; parent-teacher interaction; teachers’ self-efficacy, subjective well-being; and school environment. Implementation outcomes include change in teachers’ behaviour and sense of program acceptability, cultural appropriateness, and feasibility as well as penetration and sustainability.
Next steps:
The trial began in October, 2019 with expected completion in July, 2021. Outcomes will inform dissemination of the SMHP in Pakistan and other countries.
Trial Identifier:
NCT04091633 (ClinicalTrials.gov; registered September 17th, 2019)
Keywords: child mental health, school based mental health programs, LMICs, public schools, technology assisted teachers’ training program, school psychosocial environment
Introduction
10–20% of children are affected by socio-emotional problems globally, and the majority of these children live in low- and middle-income countries (LMICs) (1). Despite this tremendous burden and the widespread recognition of the importance of early identification and intervention, most of these children do not receive mental health services (2). Expanding services requires a life-course approach and integrating interventions into existing social and health systems to which children already have access (1, 2). Schools are part of one such system that serves children and youth across a wide age range and offers the opportunity to promote mental health in the context of promoting academic and social outcomes as well (3–6). School-based programs also offer opportunities to identify and address problems early when they are easier and less costly to ameliorate (5).
Child mental health has been identified as a priority by the World Health Organization’s Eastern Mediterranean Regional Office (WHO EMRO). Following consultations with international and regional experts and stakeholders, WHO EMRO developed a School Mental Health Program (SMHP) based on behavioural and socio-emotional learning theories (4) and endorsed by its member countries. The SMHP is designed to train school personnel – primarily teachers – to better identify and respond to the needs of children who demonstrate emotional or behavioural problems. A pilot trial of the SMHP, conducted in the Pakistani city of Lahore, found that it increased teachers’ mental health literacy and their confidence in addressing student mental health problems. A significant improvement in school’s psychosocial environment was also observed (7).
Key challenges and design solutions
As a signatory country of WHO, the federal and provincial health departments in Pakistan made recommendations for a pilot phased implementation of the WHO SMHP in the rural Rawalpindi district of Punjab Province, beginning in 10 public schools in the Kallar Syedan sub-district in April 2016. This phased implementation provided an opportunity to link our research with conventional implementation plans. The Pakistan SHINE team used the theory of change (ToC) methodology to engage stakeholders in revising the SMHP’s content and methods of delivery (8). A series of meetings and three structured workshops included 90 stakeholders, including policy makers from education and health departments, mental health specialists, researchers, head teachers, classroom teachers and other community stakeholders including representatives of non-governmental organizations. The ToC process identifies preconditions, assumptions and hypothesized pathways by which an intervention is implemented and has its impact on desired outcomes. The process identified a number of potential implementation challenges and made suggestions to address them. Broadly, these included the need to adapt existing components of the intervention to the local context and to develop sustainable mechanisms for delivery of quality training and supervision. Informed by the ToC workshops, SHINE adapted the conventional SMHP (cSMHP) to create an enhanced SMHP (eSMHP). Enhancements occurred at two levels: a) Content enhancements and b) Technological enhancements (Box 1).
Box 1: Key Challenges, Advantages and Design Solutions.
Key Challenges
Need to operationalize and adapt the existing components of the School Mental Health Program to the local context and mental health needs
Need to develop sustainable mechanisms for delivery of quality training and supervision in School Mental Health Program
Need to develop a mechanisms for ensuring programme quality at-scale
Key Advantages
Buy-in from Federal Ministry of Health, Pakistan
The federal and provincial health departments in Pakistan made recommendations for a phased implementation of the School Mental Health Program in a pilot district
Design Solutions
- Enhancement to content and delivery of School Mental Health Program
- Content enhancements: Addition of teacher’s motivation and wellbeing module; a collaborative care model for engaging parents/primary caregivers, and; simplification and operationalization of the School Mental Health Program’s individual clinical intervention strategies to facilitate teachers to implement these strategies in classroom settings.
- Technological enhancements: Adaptation of the School Mental Health Program training manual for delivery using an online teacher training platform, and a ‘Chat-bot’ to aid the implementation of intervention strategies in classroom settings.
Objectives and hypotheses
The objective of the SHINE trial is to evaluate the effectiveness of the eSMHP in reducing children’s socio-emotional difficulties compared to the cSMHP. We hypothesize that enhanced training of teachers will improve an intermediate program outcome, i.e., the teachers’ implementation behaviour, which in turn will lead to children’s improved socioemotional wellbeing. The primary outcome will be reduction in parent-rated Strengths and Difficulties Questionnaire (SDQ) total difficulties scores assessed 9 months after intervention delivery (9). Additional hypotheses related to children include that the eSMHP will be superior in reducing both externalizing and internalizing problems; improving child functioning, well-being, and academic performance; reducing child absenteeism, self-reported stigma; and increasing parent-teacher collaboration. Our exploratory implementation hypotheses are that the eSMHP will lead to improved teacher competency and fidelity to the training, greater teacher self-efficacy and wellbeing, and improvements in school environment and parental involvement. Figure 1 summarizes the model that relates teacher training to subsequent child outcomes.
Figure 1:
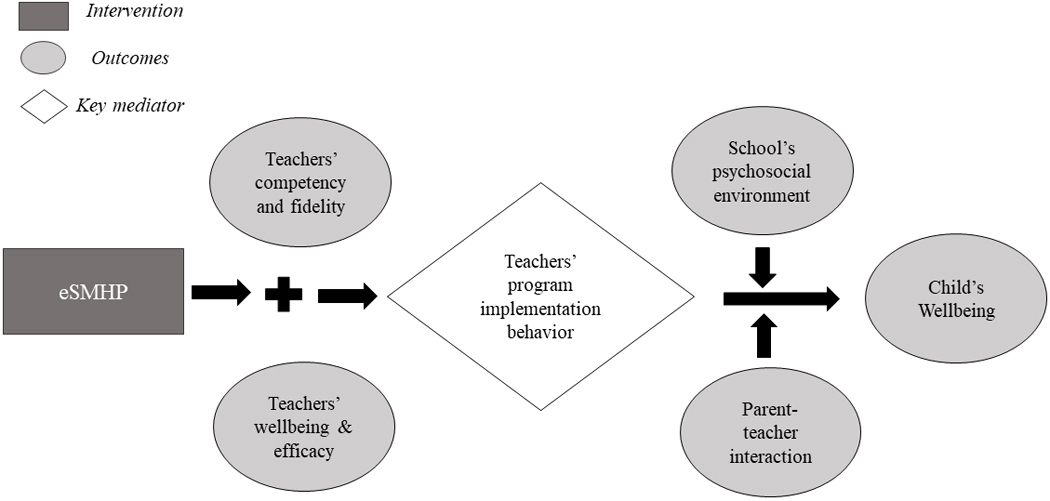
Conceptual Framework of Enhanced School Mental Health Program (eSMHP) Implementation
Methods
Overview
The study has obtained approval from Ethics Review Committee of University of Liverpool, UK and the institutional review board of the Human Development Research Foundation, Islamabad, Pakistan.
Study Sites
In each Pakistani province education is the responsibility of a provincial Ministry of Education operating in collaboration with the federal Ministry. Within provinces, district education departments are administrative hubs for schools. The school system in Pakistan is organised in three levels: primary (grades 1–5); middle (grades 6–8) and high school (grades 9–10). Federal and provincial health and education departments jointly sponsored a five-year phased implementation of the cSMHP in two sub-districts (Kallar Syedan and Gujar Khan) of Rawalpindi district, overseen by the Pakistani Institute of Psychiatry WHO Collaborating Center (IoP-WCC). Implementation of the cSMHP includes in-person teacher training workshops, supervision of teachers in schools, and program monitoring and evaluation conducted by specialist community mental health professionals from the IoP-WCC. This phased implementation of the cSMHP provided an opportunity to study the eSMHP.
The SHINE trial takes place in Gujar Khan, a semi-rural sub-district (approximate population 1,000,000) with an economy largely dependent on subsistence farming. Families get additional support from the earnings of adult male members employed in public or private sector services or industry in nearby Rawalpindi City, or serving in the armed forces. The human development indicators of Gujar Khan are typical of a low-income developing economy, with an infant mortality rate of 55 per thousand live births and a mortality rate among children under 5 of 82 per 1,000 live births (10).
Gujar Khan has 497 public schools (323 primary, 89 middle, and 85 high schools): 231 schools for boys and 266 schools for girls. Teachers specialize in one or more subjects and teach across multiple grades. For each grade level, one teacher is also responsible for managing administrative matters, such as developing students’ annual academic performance report card and holding meetings with parents/primary caregivers. Studies of school-aged children in similar settings in Pakistan have found prevalence rates of socio-emotional problems ranging from 25–35% (11).
Study procedures
The study is a parallel arm, single-blind cluster randomized controlled trial (cRCT) (12). A clustered design is appropriate when the nature of the intervention requires it to be implemented for a group of individuals at once, and to avoid the possibility that group members could be exposed to both the intervention and control conditions (13). These circumstances are pertinent to SMHP which was designed for use with groups of children in classroom settings and at the school level. Single schools are the unit of analysis and are allocated 1:1 stratified by girls’ and boys’ schools. Of the 174 middle and high schools, 80 (40 boys’ and 40 girls’) will be nominated by the district education department and randomly assigned to either the eSMHP arm or the cSMHP arm. To participate, schools will need to have 80–150 students ages 8–13 and 7–10 teachers.
Participants
Child and parent research participants and eligibility
Nine hundred sixty children, ages 8–13 years, who screen positive on both the teacher and parent/primary caregiver-rated SDQ will be recruited to evaluate the impact of the two versions of the SMHP. SDQ total difficulties scores of teacher-rated and parent-rated SDQs will be used as screening criteria (≥12 and ≥ 14, respectively) (9). The SDQ has previously been translated into the local language and used in the region (14). Children will not be eligible if they are thought to be at high risk of abuse or harm to self or others as reported by the students themselves, teachers or parents/primary caregivers, or are identified as such by the assessment team during screening. Children will also not be eligible if they are felt to require immediate or on-going in-patient medical or psychiatric care, are deaf, blind, or have speech difficulties or developmental disorders as defined by the WHO Mental Health Gap Action Programme intervention guide. Exclusion from the evaluation will not impact care received since participating schools will be targeting all of their students independently of enrolment in the trial.
Parents/primary caregivers of the recruited children will also be invited to take part in the trial. Parents/caregivers will not be eligible if they do not live with and have primary caregiving responsibilities for the child.
One head teacher from each of the participating schools (n=80) will be invited to take part in the trial along with an average of four classroom teachers per school (N=320), who will have appointments for the duration of the study. Classroom teachers will be individuals who have appointments for the duration of the study; they will be nominated by head teachers to receive the form of SMHP training to which their school is assigned. Teachers will not be eligible if they report having ongoing health problems that require periods of leave or if they report planning to leave their posts prior to the end of the trial.
Intervention
The SMHP is a universal, early intervention program, that aims to empower educators to understand the importance of mental health in school settings, enhance their understanding of child development and allow them to identify and support children manifesting socio-emotional problems (such as anxiety, reactions to trauma, depression, hyperactivity, disruptive behaviours and conduct problems) in school settings. The WHO SMHP is informed by developmental, behavioural, social and cognitive theories (4). The intervention targets teachers’ self-efficacy and their ability to implement and generalize skills at the classroom and school levels. The SMHP also includes practical steps enabling teachers to identify children at risk, provide appropriate support, and refer children for further care when required. These steps include; a) periodic use of screening questionnaires in the classroom, b) comparing socioemotional development of an identified child to his/her age cohort and c) observing children’s behaviour carefully before referring for further evaluation.
In the SHINE trial, both study arms will involve cascading training and supervision (15). cSMHP training (the control arm) will be conducted by trainers based at the IoP-WCC who have, in turn, been trained by WHO master trainers. The IoP-WCC trainers have a psychology or psychiatry degree. Training for cSMHP involves 3 days of didactic and interactive activities and follow-up supervision once in every 3-months that addresses basic theoretical knowledge related to mental health in schools and specific classroom and individual intervention strategies. Trainers will be encouraged to use interactive learning techniques such as group activities. After training in cSMHP, the nominated teachers from each school are expected to train all other teachers in their school.
The eSMHP (intervention arm) was based on the core content of the cSMHP, modified according to findings from the ToC process. Changes to the training format included converting the initial in-person training into a 4–5 hour, self-paced online training course, which participating teachers will be asked to complete within 3 days. Progress from module to module in the online training is conditional upon passing post-module mental health literacy quizzes (16). Next, the nominated teachers from each school will work as a group on interactive activities and role plays, supported online and in-person by study trainers. These teachers will then apply the training in their respective schools by helping other teachers to register and complete the online training course. While both cSMHP and eSMHP teachers will receive follow-up supervision once in every 3-months to reinforce their training, eSMHP teachers will also have continuous access to a smartphone-based “chat bot” that provides information summarizing recommended responses to common child emotional and behavioral problems.
Content modifications in the eSHMP include enhanced material on child development, counselling skills, and engaging parents. Whereas the cSMHP trains teachers to identify and respond to types of mental illness, the eSMHP trains them to respond to commonly occurring problems and avoids illness labels that could be stigmatizing. The eSMHP also includes an enlarged module addressing teacher wellness. Table 1 outlines the main areas of contrast between the two SMHP versions.
Table 1:
Comparison of cSMHP and eSMPH
| Intervention components | Conventional | Enhanced |
|---|---|---|
| Training methods | Lecture with role plays, monthly supervision | On-line training, self-paced, interactive, multi-media; Monthly supervision plus “chat bot” |
| Knowledge of child development | Lectures, theoretical descriptions | Pictures and narratives |
| Counselling skills | Descriptions and role plays | Adds video examples |
| Parent involvement | Discussed | Expanded material and guidelines |
| Specific interventions | Illness oriented | Trans-diagnostic without stigmatizing labels; specific implementation guidelines |
| Teacher wellness | Brief discussion and voluntary reading | Specific stress management skills module |
In both study arms, the trainers will perform live competency rating of the teachers using an adapted version of ENhancing Assessment of Common Therapeutic factors (ENACT) for SMHP (ENACT Plus) (17) to measure their knowledge and skills regarding SMHP. Only the competent teachers (having a mean score of at least 2 on each domain of ENACT Plus) will be allowed to train and supervise the teachers of their respective schools. In both study arms, trainers will rate 20% of training sessions conducted by nominated teachers in their respective schools using ENACT Plus. Teachers who score less than 2 on any ENACT domain will be provided with additional support in their 3-monthly supervision meetings to ensure fidelity of program delivery.
Study trainers will supervise nominated teachers in both study arms on a 3-monthly basis (2–2.5 hours). The structured supervision meetings will cover aspects of the SMHP implementation i.e. review of teachers` own wellbeing; review of any challenges faced in the implementation of intervention and discussion to mitigate those challenges; use of the Chat-bot in managing socio-emotional problems of children (eSMHP arm only); collecting program implementation data and referrals and information on success stories.
Each nominated teacher will provide peer supervision to other teachers of their respective schools on 3-monthly basis (2–2.5 hours). The agenda and structure of peer supervision meetings will be similar to the supervision meetings conducted by trainers with the nominated teachers. As far as possible the peer supervision meetings will be integrated into the school routine.
Recruiting and consent procedures
The ‘gatekeeper consenting body’ for schools is the District Education Department of Rawalpindi, which has already approved embedding the study within the on-going implementation of the cSMHP in Gujar Khan. After ethics and Data Safety Monitoring Board (DSMB) approval, schools that meet size criteria will be randomly assigned to a treatment arm, and their Head Teachers asked for consent for their participation and the participation of their respective schools, teachers, and students. Head teachers will then nominate 4–5 teachers from their schools to receive direct training from the study team. The nominated teachers will be also asked to provide consent and given the opportunity to discuss their participation in the program with the assessment team.
All children in Gujar Khan schools will be involved with, but a sample will be recruited, using a multi-stage process, to assess the differential impact of the two SMHP versions. In the first stage, teacher-level screening, parent/primary caregiver consent will first be obtained. Parent/primary caregiver consent forms will be distributed to all children within the age range of 8–13 years by the head teachers in each school. Parents/primary caregivers will have two business days to return the signed form to the class teachers. The consent form explains the study features, principles and limits of confidentiality for study participants. Parents’/primary caregivers’ and children’s ongoing participation will be voluntary. A decision to withdraw from the study will have no consequence on the usual academic activities of the child in the school. This approach to seek parent consent is informed by school-based trials (13, 18, 19), where initial parent/primary caregiver consent is obtained by school head teachers.
After obtaining parent/caregiver consent for teacher-level screening, the assessment team will seek assent for this stage from children. To prevent possible coercion from the parents/primary caregivers, informed assent from children will be sought in privacy at home or in school. Children who do not give assent will not be involved in any research procedure.
If the child screens positive in the first teacher screening, a second parent/primary caregiver level screening with the parent-rated SDQ will be carried out after parent/primary caregiver consent is sought by the assessment team. If the child screens positive on both the teacher- and parent-rated SDQ, parent/primary caregiver consent for enrollment in the trial will be sought by the assessment team in a third stage, consent for enrollment in the trial. All assessments with teachers and parents about the child will take place after the child assents to participate.
Measures
Baseline and follow-up assessments of the sample of children, teachers and head teachers will be conducted by a trained research assessment team blind to the allocation status of the trial participants. The assessment will be conducted in the setting of the participant’s choice (home/school settings).
Primary outcome -Strengths and Difficulties Questionnaire (SDQ):
Our primary outcome is reduction in total difficulties scores on parent-rated SDQ (20) in children at 9 months after commencing intervention delivery. The SDQ is a brief, valid (9) and reliable measure of socio-emotional competence that is widely used to assess socioemotional difficulties in childhood. The parent-rated version of SDQ will be used in the study because it has demonstrated greater sensitivity for detecting socio-emotional problems of children as compared to teacher- and self-rated reports (20). The SDQ has 25 items and consists of sub-scales to measure emotional symptoms, conduct problems, hyperactivity, peer problems and prosocial behaviour. Items are rated on a three-point Likert scale (0= not true, 1= somewhat true, 2=certainly true). A total difficulty score is calculated by summing the responses of each item in all domains except for the pro-social behaviour items (5 items) (9). Table 2 shows the full list of study outcomes, when they are measured, and with which assessments.
TABLE 2:
Outcome measures and corresponding time-points of cSMHP and eSMHP in Pakistana
| Time of assessment | |||
|---|---|---|---|
| Outcome | Measure | Baseline | 9 months |
| Child | |||
| Socioemotional problems | Parent-rated SDQ (20) | X | X |
| Externalizing socioemotional problems | Parent-rated SDQ (20) | X | X |
| Internalizing socioemotional problems | Parent-rated SDQ (20) | X | X |
| Functioning | Parent-rated WHODAS-Child (32) | X | X |
| Quality of life | Parent-rated PedsQL (33) | X | X |
| Psychosocial functioning and well-being | Child-rated PSYCHLOPS-Kids (34) | X | X |
| Annual academic performance and classroom attendance | Teacher-rated student academic achievement and attendance record form | X | X |
| Self-rated-stigma | Self-rated PaedS (35) | X | X |
| Teacher | |||
| Self-efficacy | Teacher-rated Efficacy Scale (36) | X | X |
| Objective well-being | Teacher-rated SRQ (37) | X | X |
| Change in program implementation behavior | DIBQ (22) | X | |
| Parents | |||
| Parent-teacher interaction | Parent-rated PTIQ (38) | X | X |
| Project financial data | |||
| Cost of teachers’ training and behavior change | Project cost of intervention and cost to families (CSRI) (39, 40) | X | X |
| School | |||
| Psychosocial profile of the school | Teacher-rated Psychosocial Environment Profile (41) | X | X |
cSMHP, conventional school mental health program; CSRI, Client Service Receipt Inventory; DIBQ, Determinants of Implementation Behavior Questionnaire; eSMHP, enhanced school mental health program; PaedS, Pediatric Self-Stigmatization Scale; PedsQL, Pediatric Quality of Life Inventory; PSYCHLOPS, Psychological Outcome Profiles; PTIQ, Parent-Teacher Involvement Questionnaire; SDQ, Strengths and Difficulties Questionnaire; SRQ, Self-Reporting Questionnaire; WHODAS, World Health Organization Disability Assessment Schedule.
Implementation outcome measures
Proctor and colleagues’ (21) framework will be used to evaluate acceptability, adoption, appropriateness (including cultural appropriateness), feasibility, penetration, sustainability and cost in both study arms. The Determinants of Implementation Behaviour Questionnaire (DIBQ) (22) will be used to measure the change in teachers’ behaviour as they implement the SMHP in school and classroom settings. An adapted version of the DIBQ, based on 12 domains (knowledge, skills, social, professional role and identity, beliefs about capabilities, beliefs about consequences, memory, attention and decision processes, environmental context and resources, social influences, emotion, behavioural regulations and nature of behaviours) will be used post-intervention to assess the change in teachers’ behaviour regarding implementation of SMHP.
Analysis strategy
Primary data analyses will be based on the intention-to-treat principle. For analysis of the primary outcome, a linear mixed model will be employed with treatment, time, interaction between treatment and time as fixed effect, the baseline value of the SDQ total difficulties score as a covariate; and school cluster as a random effect. In addition, an adjusted linear mixed model analysis will be performed with the pre-specified covariates (age groups 8–10 and 11–13, socio-economic status and parent/primary caregivers’ education) measured at baseline being added into the above mixed model. The crude and adjusted mean differences in the primary outcome together with their 95% confidence intervals will be derived from the mixed models. In addition, subgroup analysis of the primary endpoint will be performed using the above pre-specified covariates.
The assessment team will also follow up with children who drop out or are expelled from school during the study period. The per-protocol analyses will also be performed as a supplemental analysis. Adjusted analysis and subgroup analysis will be based on covariates at baseline without missing values (23). No interim analysis of outcomes is planned.
Mediation analysis
An exploratory analysis will be conducted to understand the potential mediating effects of teacher’s program implementation behaviour on the relationship between the SMHP and SDQ scores at 9 months after commencing intervention delivery. We will estimate direct and indirect effects of the intervention using a model-based mediation package by Imai (24). All analyses will be exploratory given limited power for detecting these interaction effects and difficulties in interpreting mediational effects as causal (25)).
Moderator analysis
An exploratory moderator analysis will be conducted to help clarify for whom and under what circumstances (potential moderators) the SMHP works. We will assess modification of treatment effect with potential, a priori-defined modifiers/covariates (age group, socio-economic status, parent/primary caregivers’ education, baseline severity of socioemotional problems, school environment and parents/primary caregivers’ interaction with their child’s teacher, by fitting an appropriate interaction term in the linear mixed model.
Process evaluation:
We will conduct mixed-methods research to assess assumptions underlying the intervention and implementation strategies such as acceptability, feasibility, appropriateness (including cultural appropriateness) and adoption (26). In-depth Interviews (IDIs) and Focus Group Discussions (FGDs) will be conducted with participants of both arms at their preferred. Sampling for qualitative interviews will be purposive so that individuals with knowledge of and exposure to the SMHP will be included for each category of respondent. Sampling may be extended on the basis of emerging results. Sampling for in-depth interviews will continue until theoretical saturation has been reached. We anticipate 8 – 15 interviews with each category of respondent to reach theoretical saturation. Data analysis will be based on the framework analysis approach (27). Quantitative implementation outcome measures will be used to explore program’s acceptability, feasibility, appropriateness, adoption, and cost (28).
Results
The trial is expected to yield considerable information about feasible methods for engaging school systems, teachers, and families in implementing mental health programs at scale. Most importantly, it will provide information about how implementation methods – both in planning and actual training phases -- relate to the impact of the program on students. In many low resource communities it is not possible to employ dedicated mental health professionals in schools, and even then, consultation by students may be limited by stigma, insurance status, or lack of parental consent (29). In these communities school personnel themselves need to be able to respond therapeutically to students who are experiencing emotional or behavioural problems, but those personnel must come to feel that taking on a therapeutic role will enhance rather than compete with their roles as educators. The SHINE trial will test whether a redesign of the WHO SMHP based, on specific input from school personnel, will lead to teachers’ more consistently and effectively helping students in distress. Thus the trial results will have implications for both specific aspects of the content and training that encourage teacher use, but also for the process by which school mental health interventions are introduced into school systems and adapted for those systems’ unique needs.
We expect that suggestions will emerge for further changes to both the SMHP content and implementation process that could enhance its effectiveness; these will be shared with SHINE and WHO EMRO stakeholders, including the SHINE partners from Iran, Egypt, and Jordan, and will influence further use of the SMHP itself and similar or complementary programs. Some of the most interesting results may be whether the SMHP seems to help some children more than others, and what modifications may be necessary to identify and help those for whom the program has limited impact. We also strongly suspect that students’ improvement will be moderated or mediated by parental involvement, a factor that has historically been a barrier to school-based mental health programs (30). It may be that in some communities school mental health programs require explicit investment in personnel who can encourage family participation in all facets of their children’s educational experiences (31).
Next steps:
The SHINE trial will test whether a careful process of stakeholder collaboration (in this case through a series of “theory of change” workshops) can help adapt a school mental health program so that it is more completely embraced by teachers and ultimately is more effective in reducing symptoms among students. The trial began in October, 2019 with expected completion in July, 2021. Outcomes will inform dissemination of the SMHP in Pakistan and other countries.
Highlights:
The Pakistan National Ministry of Health Services is sponsoring a five-year phased implementation of a WHO School Mental Health Program (SMHP) in two subdistricts of Rawalpindi district.
To learn more about scaling up the SMHP, workshops with parents, educators, and health officials led to changes in content and delivery including greater emphasis on teacher well-being and parent-teacher interaction, a problem-oriented trans-diagnostic approach to mental health, and digitally-assisted training.
A cluster-randomized trial in Pakistan will examine whether the changes result in better student outcomes and greater teacher use of program material.
Trial results will provide information on ways to provide and scale up school mental health interventions in low-resource settings through the direct engagement of teachers and other school personnel.
acknowledgments:
The authors are grateful to the World Health Organization’s Eastern Mediterranean Regional Office, the authors of the office’s original school mental health program and manual, representatives of partner countries (Egypt, Iran, and Jordan), and the many stakeholders involved in the workshops that developed the final design for this trial.
The authors alone are responsible for the views expressed in this article, which do not necessarily represent the decisions, policy, or views of the NIMH.
Grant information
This work was funded by the National Institute of Mental Health (NIMH) (U19MH109998). This article is part of a series of protocols of NIMH-funded research partnership grants focused on scaling up mental health interventions in low and middle-income countries.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
Contributor Information
Syed Usman Hamdani, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, United Kingdom and Institute of Psychiatry, World Health Organization Collaborating Centre for Mental Health Research and Training, Rawalpindi, Pakistan.
Zill-e-Huma, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, United Kingdom and Human Development Research Foundation, Islamabad, Pakistan.
Azza Warraitch, Human Development Research Foundation, Islamabad, Pakistan.
Nadia Suleman, Human Development Research Foundation, Islamabad, Pakistan.
Naila Muzzafar, Human Development Research Foundation, Islamabad, Pakistan.
Fareed Aslam Minhas, Institute of Psychiatry, WHO collaborating centre for mental health research and training, Rawalpindi, Pakistan.
Asad Tameezuddin Nizami, Institute of Psychiatry, WHO collaborating centre for mental health research and training, Rawalpindi, Pakistan.
Siham Sikander, Human Development Research Foundation, Islamabad, Pakistan.
Beverly Pringle, National Institute of Mental Health, Bethesda, Maryland, USA.
Ashley Kennedy, National Institute of Mental Health, Bethesda, Maryland, USA.
Holly Campbell-Rosen, National Institute of Mental Health, Bethesda, Maryland, USA.
Hesham M. Hamoda, Department of Psychiatry, Boston Children’s Hospital and Harvard Medical School, Boston, Massachusetts, USA.
Duolao Wang, Department of Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, United Kingdom.
Atif Rahman, Department of Primary Care and Mental Health, University of Liverpool, Liverpool, United Kingdom.
Lawrence S Wissow, Department of Pscyhiatry and Behavioral Sciences, University of Washington, Seattle, Washington, USA.
References
- 1.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet 2011;378:1515–1525 [DOI] [PubMed] [Google Scholar]
- 2.Thapar A, Collishaw S, Pine DS, et al. Depression in adolescence. Lancet 2012;379:1056–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langford R, Bonell C, Jones H, et al. The World Health Organization’s Health Promoting Schools framework: a Cochrane systematic review and meta-analysis. BMC Public Health 2015;15:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Durlak JA, Weissberg RP, Dymnicki AB, et al. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev 2011;82:405–432 [DOI] [PubMed] [Google Scholar]
- 5.Arango C, Díaz-Caneja CM, McGorry PD, et al. Preventive strategies for mental health. Lancet Psychiatry 2018;5:591–604 [DOI] [PubMed] [Google Scholar]
- 6.Fazel M, Patel V, Thomas S, et al. Mental health interventions in schools in low-income and middle-income countries. Lancet Psychiatry. 2014;1:388–398 [DOI] [PubMed] [Google Scholar]
- 7.Imran N, Rahman A, Chaudhry N. Effectiveness of the World Health Organization’s “School Mental Health Manual” intervention for promoting mental health literacy among teachers in Lahore, Pakistan: A randomized, controlled trial. J Am Acad Child Adolescent Psychiatry. 2019;58(10S):S22. [Google Scholar]
- 8.Breuer E, Lee L, De Silva M, et al. Using theory of change to design and evaluate public health interventions: a systematic review. Implement Sci 2016;11:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J Am Acad Child Adol Psych. 2009;48:400–403 [DOI] [PubMed] [Google Scholar]
- 10.Multiple Indicator Cluster Survey, Punjab. Lahore, Pakistan, Pakistan Bureau of Statistics, 2003
- 11.Syed EU, Hussein SA, Mahmud S. Screening for emotional and behavioural problems amongst 5–11-year-old school children in Karachi, Pakistan. Soc Psychiatry Psychiatr Epidemiol 2007;42:421–7 [DOI] [PubMed] [Google Scholar]
- 12.Curran GM, Bauer M, Mittman B, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012;50:217–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Björklund K, Liski A, Samposalo H, et al. “Together at school”--a school-based intervention program to promote socio-emotional skills and mental health in children: study protocol for a cluster randomized controlled trial. BMC Public Health 2014;14:1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Samad L Hollis C, Prince M, et al. Child and adolescent psychopathology in a developing country: testing the validity of the Strengths and Difficulties Questionnaire (Urdu version). Int J Meth Psych Res 2005;14:158–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Murray LK, Dorsey S, Bolton P, et al. Building capacity in mental health interventions in low resource countries: an apprenticeship model for training local providers. Int J Mental Health Systems 2011;5:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamdani SU, Muzaffar N, Huma Z, et al. Using technology to advance school mental health: experience from the Eastern Mediterranean region. J Am Acad Child Adol Psychiatry 2019;58:S22 [Google Scholar]
- 17.Kohrt BA, Jordans MJ, Rai S, et al. Therapist competence in global mental health: Development of the ENhancing Assessment of Common Therapeutic factors (ENACT) rating scale. Behav Res Ther 2015;69:11–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford T, Edwards V, Sharkey S, et al. Supporting teachers and children in schools: the effectiveness and cost-effectiveness of the Incredible Years teacher classroom management programme in primary school children: a cluster randomised controlled trial, with parallel economic and process evaluations. BMC Public Health 2012;12:719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eaton J, McCay L, Semrau M, et al. Scale up of services for mental health in low-income and middle-income countries. Lancet 2011;378:1592–1603 [DOI] [PubMed] [Google Scholar]
- 20.Stone LL, Otten R, Engels RC, et al. Psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire for 4- to 12-yearolds: a review. Clin Child Fam Psychol Rev 2010;13:254–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Proctor E, Silmere H, Raghavan R et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huijg JM, Gebhardt WA, Dusseldorp E, et al. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement Sci 2014;9:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Enders CK. Applied missing data analysis. New York, Guilford Press, 2010 [Google Scholar]
- 24.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychological Methods 2010;15:309–334 [DOI] [PubMed] [Google Scholar]
- 25.Jo B. Causal inference in randomized experiments with mediational processes. Psychological Methods 2008;13:314–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Proctor EK, Landsverk J, Aarons G, et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health 2009;36:24–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess B, editors. Analyzing Qualitative Data; London: Routledge, 1994: 173–194 [Google Scholar]
- 28.Haroz E, Bolton P, Nguyen A, et al. Measuring implementation in global mental health: validation of a pragmatic implementation science measure in eastern Ukraine using an experimental vignette design. BMC Health Serv Res 2019;19:262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Massey OT, Armstrong K, Boroughs M, et al. Mental health services in school: a qualitative analysis of challenges to implementation, operation, and sustainability. Psychology in Schools 2005;42:361–372 [Google Scholar]
- 30.Parikh R, Michelson D, Sapru M, et al. Priorities and preferences for school-based mental health services in India: a multi-stakeholder study with adolescents, parents, school staff, and mental health providers. Glob Ment Health (Camb) 2019;6:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sugai G, Horner RH. Responsiveness-to-intervention and school-wide positive behavior supports: Integration of multi-tiered system approaches. Exceptionality 2009;17:223–237 [Google Scholar]
- 32.Janca A, Kastrup M, Katschnig H, et al. The World Health Organization Short Disability Assessment Schedule (WHO DAS-S): a tool for the assessment of difficulties in selected areas of functioning of patients with mental disorders. Soc Psychiatry Psychiatr Epidemiol 1996;31:349–354. [DOI] [PubMed] [Google Scholar]
- 33.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800–812 [DOI] [PubMed] [Google Scholar]
- 34.Godfrey E, Aubrey M, Crockford S, et al. The development and testing of PSYCHLOPS Kids: a new child‐centred outcome measure. Child and Adolescent Mental Health 2019;24:54–65 [DOI] [PubMed] [Google Scholar]
- 35.Khalil A, Gondal F, Imran N, et al. Self-Stigmatization in Children Receiving Mental Health Treatment in Lahore, Pakistan. Asian J Psychiatr 2020;47:S223–S224 [DOI] [PubMed] [Google Scholar]
- 36.Tschannen-Moran M, Hoy AW. Teacher efficacy: Capturing an elusive construct. Teaching and Teacher Education 2001;17:783–805 [Google Scholar]
- 37.Beusenberg M, Orley J. A User’s guide to the Self Reporting Questionnaire (SRQ) Geneva, World Health Organization Division of Mental Health, 1994 [Google Scholar]
- 38.Kohl GO, Lengua LJ, McMahon RJ and the Conduct Problems Prevention Research Group. Parent involvement in school: conceptualizing multiple dimensions and their relations with family and demographic risk factors. Journal of School Psychology 2000;38:501–523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johns B, Baltussen R, Hutubessy R. Programme costs in the economic evaluation of health interventions. Cost Eff Resour Alloc. 2003;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sleed M, Beecham J, Knapp M, et al. Assessing services, supports, and costs for young families under stress. Child: Care, Health and Development 2006;32:101–110 [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Creating an environment for emotional and social well-being: an important responsibility of a Health-Promoting and Child-Friendly School. WHO Information Series on School Health; Document 10. Geneva, 2003 [Google Scholar]


