Abstract
Objectives
The use of mobile technologies and handheld computers by physicians has increased worldwide. However, there are limited studies globally regarding training physicians on the use of such devices in clinical practice. In addition, no studies have been conducted previously in Oman addressing this issue among postgraduate medical trainees and trainers. The present study explores the practice and perception of resident doctors and trainers towards the use of mobile technologies and handheld devices in healthcare settings in Oman.
Methods
This cross-sectional study was conducted using a validated questionnaire disseminated via email to all residents and trainers in five major training programs of the Oman Medical Specialty Board (OMSB). The questionnaire explored three main areas; perception, usage, and perceived barriers of handheld devices.
Results
Overall, 61.4% of the residents and 28.3% of the trainers responded to the questionnaire. Both types of participants agreed that the use of such devices positively affects clinical decision-making. In total, 98.8% of the participating residents and 86.7% of the trainers frequently used handheld devices. Both OMSB residents and trainers agreed that lack of time, training, and applications were the most common factors limiting the use of these devices. Participants emphasized the need for constructive training regarding the use of handheld devices as healthcare resources.
Conclusions
Point-of-care devices are positively perceived and frequently used by OMSB trainees and trainers. However, constructive training on the effective usage of these devices in clinical decision-making is needed. Further future studies to evaluate the impact of using such devices in patient care should be conducted.
Keywords: Internship and Residency; Point-of-Care Systems; Cross-Sectional Studies; Clinical Decision-Making; Oman; Computers, Handheld; Training Support
Introduction
The medical field has been making use of fast-developing innovations in mobile technologies and handheld devices among other fields.1 In 2010, 82% of adults in the US reported owning and using a mobile phone or similar device.2 Moreover, approximately one in six people have used a mobile phone to access health-related information.3 Today, smartphones and handheld computers provide access to a wide variety of medical applications to assist physicians at the point of care, also known as point-of-care (POC) devices.4 Recent studies have documented an increase in POC device ownership and usage by medical students, residents, and faculty physicians in various clinical settings.4-9
Having information readily available at the POC can be extremely useful in view of the growing amount of accessible medical information, increased expectations to follow guidelines and formulary restrictions, and the time limitations placed on physicians.1,10 Handheld devices can improve efficiency, and previous studies suggest that they may also reduce medical errors and improve patient outcomes.1,10-13 Numerous applications for both personal and clinical use are now available to assist healthcare providers with many important tasks including information and time management, health record maintenance and access, communication and consulting, reference and information gathering, patient management and monitoring, clinical decision-making, and medical education and training.1,10,14-16
However, there are limited studies globally regarding training physicians on the use of such devices in clinical practice. In addition, no studies have been conducted previously in Oman regarding this trend among postgraduate medical trainees and trainers. Studying this issue in residency training setting will help predict future practice, plan training, and raise awareness regarding POC devices.
Therefore, we sought to explore the perception and usage of mobile handheld devices among Oman Medical Specialty Board (OMSB) residents and trainers. In addition, this study also explored the perceived barriers and the need for formal training related to such devices in healthcare settings.
Methods
OMSB is the postgraduate body responsible for residency training in Oman. Currently, there are 18 postgraduate training programs accommodating 565 residents. This cross-sectional study was conducted using an online questionnaire in Google Docs format, which was disseminated via email to all residents and trainers in five major programs within the OMSB (family medicine, internal medicine, general surgery, obstetrics and gynecology, and pediatrics).
The questionnaire was developed from May to September 2012 by the investigators with the aid of previous research questionnaires related to the topic.2,3,9,11,15,17 Certain questions were utilized from earlier uncompleted research. The questionnaire included different aspects concerning POC device perception, usage, trend, and perceived barriers. Before the data collection, the questionnaire underwent both internal and external validation. First, the questions were reviewed by senior researchers who are experts in the field. Second, they were reviewed and modified by a statistician and an epidemiologist. Third, the questionnaire was subjected to content validation after an initial pilot study involving 15 doctors. A second pilot study (conducted in January 2014) using the online questionnaire was conducted among residents and trainers of the anesthesia program of the OMSB to check response rates, comprehension, and conduct an initial statistical analysis. A different program was chosen to pilot the study to get a wider insight and avoid the chance of having the same participant answering the questionnaire two times.
All residents and trainers of the aforementioned five major programs in OMSB were invited. Residents who were training abroad at the time of data collection were excluded. An ‘other’ specialty option was added to the questionnaire’s demographic questions to identify any residents and trainers of other specialties that might have received the online questionnaire by mistake. Responders of this kind were also excluded from the study. Ethical approval was obtained from the Ethics Committee of the Sultan Qaboos University, Muscat, Oman (MREC#816). Thereafter, approval was obtained from OMSB. All participants indicated their consent online before being able to answer the questions. No personal information was obtained from any of the participants, apart from their email addresses, which was optional.
The data were collected in two stages. In the first stage (from 23 February to 13 April 2014), the online questionnaire was sent to the OMSB training affairs office, where it was in turn sent to the program coordinators of the five training programs. These program coordinators subsequently distributed the online questionnaire by email to all of their residents and trainers. Online reminders to answer the questionnaire were sent three times over a six-week period. The initial response rate was low, so the chief residents of the programs were contacted and requested to encourage residents to participate in the study.
In the second stage (from 13 April to 13 May 2014), hard copy versions of the questionnaire were distributed to trainers and residents of the five specialties currently training at the Sultan Qaboos University Hospital, Royal Hospital, or other local health centers in Muscat. The specialty coordinator at each hospital sent the hard copies to the mailboxes of the doctors who were instructed to distribute them to the residents and trainers during morning meetings and in outpatient departments. Instructions were given to the coordinator to inform the doctors that those who had already responded to the online questionnaire should not participate again.
Data was analyzed using SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) for the statistical analyses. Percentages and means ± standard deviation (SD) were calculated for categorized and continuous variables, respectively. Chi-square test was used to compare groups.
Results
A total of 60.0% of the residents and 15.0% of the trainers responded to the online questionnaire. In addition, 4.0% of the residents and 16.0% of the trainers completed the hard copy version of the questionnaire. Collectively, 61.4% of the residents (175/285 residents) and 28.6% of the trainers (91/318 trainers) completed the questionnaire.
Of the residents who responded, the majority were junior residents (R1 or R2). Most were from the internal medicine and family medicine programs (33.1% and 32.6%, respectively). In total, 79.0% of the residents in the family medicine program participated in the study compared to 60.4% of internal medicine residents, 68.0% of general surgery residents, 56.0% of pediatrics residents, and 23.1% of obstetrics and gynecology residents.
In terms of the trainers, the majority of those who responded were similarly from the family medicine and internal medicine programs (33.0% for both). This can also be attributed to the large number of trainers in those specialties (76 and 80 trainers, respectively, compared to 69, 41, and 52 trainers in the pediatrics, obstetrics and gynecology, and general surgery programs, respectively). Overall, 40.0% of trainers in the family medicine program participated in the study, compared to 38.0% of internal medicine trainers, 27.0% of obstetrics and gynecology trainers, 17.0% of pediatrics, 14.0% of general surgery trainers. Most of the trainers were senior consultants (40.0%) or senior specialists (34.0%) with the remaining trainers being consultants (17.0%), specialists (9%), or associate professors (1.0%).
Among the participants, 56.0% of the residents were female, and 98.0% were Omani. The mean age of the residents was 28.5±2.0 years (range: 25–36 years). There was an almost equal distribution of male and female trainers (46.0% and 54.0%, respectively). As with the residents, most of the trainers were Omani (71.0%). The mean age of the trainers was 42.0±7.5 years (range: 26–64 years).
The vast majority (98.8%) of residents frequently used POC devices (i.e., used the device at least once per week), with 79.5% using their device daily, and 19.3% using their device on a weekly basis. Only two residents (1.1%) had never used handheld devices in clinical practice settings [Figure 1]. The mean duration of device usage was 3.6±2.2 years.
Figure 1.
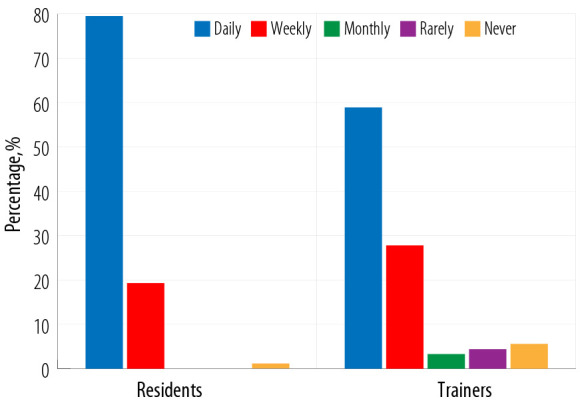
Frequency of usage of handheld devices in clinical practice.
The most frequently used applications for POC devices by residents were: accessing the internet for medical purposes (93.2%), checking their emails (80.7%), and drug references (75.6%). Other applications used frequently by the residents included: taking pictures related to clinical practice (63.1%), reading e-books (60.2%), using medical calculators (60.2%), and accessing data books (50.6%). Only 27.3% of the residents frequently used handheld devices for research purposes [Figure 2].
Figure 2.
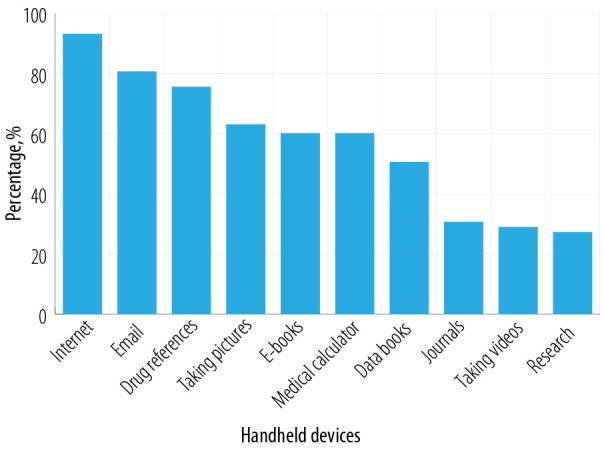
Most common applications of handheld devices in clinical practice by residents.
Most of the residents reported using handheld devices after an encounter with a patient (96.6%), whereas 72.2% of residents used the device before seeing the patient, and only 33.7% used the device during the patient encounter [Figure 3].
Figure 3.
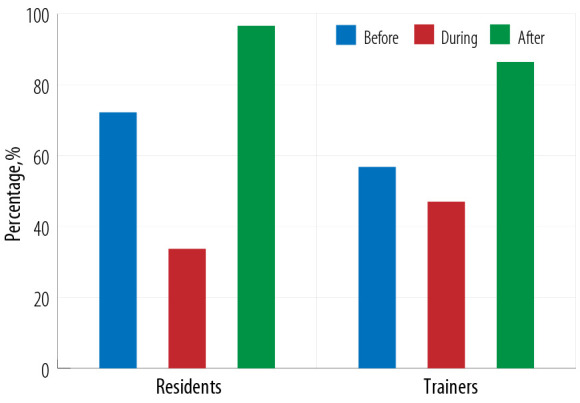
Usage of handheld devices in medical practice in relation to patient encounters.
Regarding the usage of POC devices among trainers, 86.7% used their device at least once per week. Overall, 58.9% used the device daily, 27.8% used it weekly, and 5.6% had never used a handheld device for clinical practice [Figure 1]. The mean duration of device usage was 5.0±3.6 years. None of the trainers < 30 years old were infrequent users (i.e., used the device less than once per week) compared to 3.0% of trainers between 30–39 years old and 20.0% of trainers aged ≥ 40 years old. This difference was statistically significant (p < 0.050). Additionally, 6.0% of Omani trainers were infrequent users compared to 31.0% of non-Omani trainers. This difference was also statistically significant (p < 0.050).
The most common applications of POC devices by trainers involved checking their email (80.0%), accessing the internet (76.7%), and taking pictures related to clinical practice (56.7%). Other applications included: drug references (54.4%), reading medical journals (53.3%), and using medical calculators (50.0%) [Figure 4].
Figure 4.
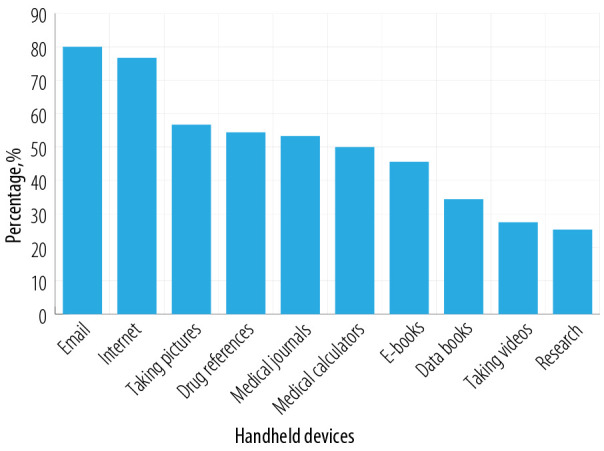
Most common applications of point-of-care devices by trainers.
Most of the trainers used handheld devices after the patient encounter (86.4%), although 56.8% used them before the patient encounter and 47.0% while they were interviewing the patient [Figure 3].
Most residents (88.0%) believed that handheld devices influenced clinical decision-making by helping them to determine diagnoses (74.0%) and avoid ordering unnecessary tests (74.0%). However, only 45.0% thought that using handheld devices shortened the length of hospital stay for the patient.
Residents agreed that a lack of training (23.0%), limited time (21.0%), and the small size of the screen on the device (20.0%) were the factors that most limited their usage of handheld devices as healthcare resources. Other factors identified as barriers included: the lack of applications for their devices (15.0%), the fact that other resources were more helpful (13.0%), and a lack of comfort with the technology (10.0%).
Many of the trainers thought that the use of handheld devices influenced their clinical decision-making (60.0%), particularly by helping to ascertain the diagnosis (57.0%), modify treatments (62.0%), avoid ordering unnecessary tests (47.0%), and shorten the patient’s length of stay (26.0%).
Trainers agreed that certain factors limited their use of handheld devices, particularly lack of time (24.0%), the small size of the screen on the device (24.0%), and lack of training (18.0%). Other limitations included a lack of programs/applications on the device (14.0%), the fact that other resources were considered to be more helpful (14.0%), and concern that the data or the device would be lost (11.0%).
Most of the residents (71.6%) expressed the need for formal training on the use of handheld devices in medical practice [Figure 5]. A total of 89.0% of the residents had been self-trained, and 27.0% had received training from a friend.
Figure 5.
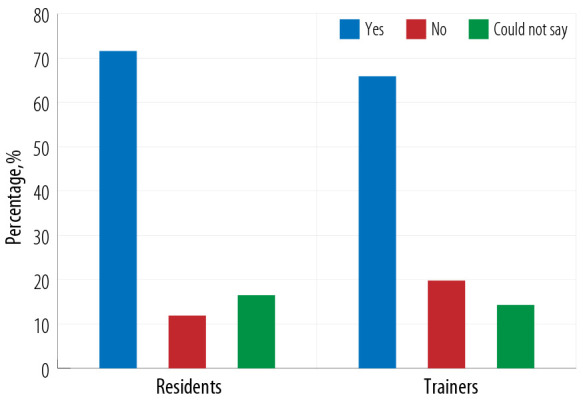
Need for training expressed by residents and trainers.
Direct observed training, interactive training in groups, and self-directed learning were the most preferred training methods by the residents (94.0%, 91.0%, and 91.0%, respectively). Other methods of training preferred by the residents included computer programs (86.0%), lectures/presentations (66.0%), and written instructions/manuals (63.0%). The most preferred format of training was in a small group of fewer than five individuals (91.0%). However, 89.0% and 88.0% of the residents thought that self-training using instructions and face-to-face training with a single trainer would be helpful, respectively, while 62.0% believed training in groups of more than five individuals would be useful.
Most trainers (65.9%) also expressed the need for POC devices training [Figure 5]. Among the trainers, 90.0% had been self-trained and 14.0% had been trained by another person. Regarding the format that they preferred for training, the majority of the trainers felt that face-to-face training with a single trainer (93.0%) and training in small groups (93.0%) would be beneficial; in contrast, fewer trainers believed that self-training using instructions (85.0%) and training in large groups (67.0%) would be helpful. Among trainers, the most preferred methods for training were direct observed training (97.0%) and interactive training in groups (93.0%). Other methods also felt to be helpful included self-directed learning (86.0%), computer programs (82.0%), presentations/lectures (75.0%), and written instructions/manuals (72.0%).
Discussion
Participants in this study believe that POC device use positively affects clinical decision-making. In addition, they appeared to be frequent users of handheld devices in clinical settings. However, both OMSB residents and trainers agreed that lack of time, lack of training, and small size of the screen on the device were the most common factors limiting the use of these devices. There are no organized training programs for the use of POC hand devices in OMSB. The lack of well-known medical applications that can be installed freely to devices of both trainers and trainees can attribute to their usage limitation. The lack of time can be explained by the crowded outpatient department and the increasing number of inpatients that need to be seen in a limited time. So, taking more time on the POC handheld devices can further delay the service. It also can be explained by the multiple tasks assigned for both residents and trainers.
Over the past decade, only 18 empirical studies have been conducted on accepting physician-specific technology.18 This study was the first to evaluate POC handheld device use in medical practice in Oman and explored awareness, usage, and training among OMSB residents and trainers in five major specialties. The results indicated a high frequency of usage of such devices among both residents (98.8%) and trainers (86.7%), which is comparable to the findings of a previous study (96% and 92%, respectively).19 According to another study, individuals with greater clinical experience tend to be less satisfied with technology due to their higher expectations; this might therefore explain why fewer trainers use handheld devices in comparison to residents.20 Another reason that explains the lower usage of these devices among trainers is age. Older age is associated significantly with lower usage among trainers. In the current study, the majority of both residents and trainers had only recently started using their devices in clinical practice (four and five years ago, respectively). This can be considered to indicate a late introduction to such technologies in comparison to other studies.14,19
The study also found that the most frequent applications of POC devices by residents and trainers included accessing the internet for medical purposes, checking emails, drug references, and taking pictures. To some extent, these applications are similar to the most frequent applications of handheld devices reported in other studies, such as drug references, medical calculators, medical references, personal organizers, and making notes/memos.1,14,19,20 Furthermore, this study explored different factors limiting the usage of these devices in Oman. Similar to previous studies,1,18 both OMSB residents and trainers agreed that a lack of time, lack of training, and small size of the screen on the device were the most common barriers to the use of POC devices. This highlights the importance of well-organized training on the use of handheld devices in medical settings.
Both residents and trainers expressed their beliefs that the use of handheld devices affected their clinical decision-making and the management plans of their patients, indicating the importance of such devices in clinical care. Despite this, there was a general lack of training on the use of handheld devices. The study showed that majority of residents and trainers had trained themselves on the use of these devices. These figures are similar to data reported in previous research.19,20 This indicates a global lack of formal training on these devices. This study also explored the formats and methods of training most preferred by both residents and trainers. According to their responses, training in small groups of less than five individuals, self-training using instructions, and face-to-face training with a single trainer were the preferred training types. These findings are similar to preferred methods and formats in other studies.2,3,9,11,15,21
The study was limited by the low response rate of OMSB trainers, which may prevent the generalization of the results to all trainers at OMSB. Another limitation is that this study included residents and trainers from only five specialty training programs in OMSB, limiting the generalization of the results to other residents and trainers in the OMSB and other physicians in Oman.
Conclusion
This is the first study in Oman exploring the usage and perception of postgraduate medical trainees and trainers towards POC devices in clinical practice. Although the frequency and perception of the use of POC devices among OMSB residents and trainers were high, there was a lack of formal training on the use of these devices in medical practice in Oman. Well-organized training programs are highly recommended. However, further studies are needed to evaluate the pattern of handheld device use among residents and trainers in other residency programs and other non-OMSB physicians in Oman. Future studies may also address the impact of the usage of such devices on patients’ care.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank Prof. Heming for his assistance in reviewing our manuscript, Dr. Ibrahim Inawa for providing us with some questions from his incomplete study, and the statistician Dr. Sayed Rizvi for helping us with the initial validation of the questionnaire. We are also grateful to the OMSB and all residents and trainers who participated in this study.
References
- 1.Embi PJ. Information at hand: using handheld computers in medicine. Cleve Clin J Med 2001. Oct;68(10):840-842, 845-846, 848-849 passim. 10.3949/ccjm.68.10.840 [DOI] [PubMed] [Google Scholar]
- 2.Criswell DF, Parchman ML. Handheld computer use in U.S. family practice residency programs. J Am Med Inform Assoc 2002. Jan-Feb;9(1):80-86. 10.1136/jamia.2002.0090080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kho A, Henderson LE, Dressler DD, Kripalani S. Use of handheld computers in medical education. A systematic review. J Gen Intern Med 2006. May;21(5):531-537. 10.1111/j.1525-1497.2006.00444.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torre DM, Wright SM. Clinical and educational uses of handheld computers. South Med J 2003. Oct;96(10):996-999. 10.1097/01.SMJ.0000051732.86014.5B [DOI] [PubMed] [Google Scholar]
- 5.Dee CR, Teolis M, Todd AD. Physicians’ use of the personal digital assistant (PDA) in clinical decision making. J Med Libr Assoc 2005. Oct;93(4):480-486. [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll AE, Christakis DA. Pediatricians and personal digital assistants: what type are they using? AMIA Annu Symp Proc 2003;2003:130-134. [PMC free article] [PubMed] [Google Scholar]
- 7.Baumgart DC. Personal digital assistants in health care: experienced clinicians in the palm of your hand? Lancet 2005. Oct;366(9492):1210-1222. 10.1016/S0140-6736(05)67484-3 [DOI] [PubMed] [Google Scholar]
- 8.Gillingham W, Holt A, Gillies J. Hand-held computers in healthcare: what software programs are available? N Z Med J 2002. Sep;115(1162):U185. [PubMed] [Google Scholar]
- 9.Bennett NL, Casebeer LL, Kristofco RE, Strasser SM. Physicians’ Internet information-seeking behaviors. J Contin Educ Health Prof 2004;24(1):31-38. 10.1002/chp.1340240106 [DOI] [PubMed] [Google Scholar]
- 10.Rothschild JM, Lee TH, Bae T, Bates DW. Clinician use of a palmtop drug reference guide. J Am Med Inform Assoc 2002. May-Jun;9(3):223-229. 10.1197/jamia.M1001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rothschild JM, Lee TH, Bae T, Yamamoto R, Horsky J, Bates DW. Survey of physicians’ experience using a handheld drug reference guide. Proc AMIA Symp 2000;•••:1125. [Google Scholar]
- 12.Rosenbloom MJ, Adams J. Patient care efficiency and medical error reduction using PDA-based medical information. Acad Emerg Med 2001;8:587-588. [Google Scholar]
- 13.Fischer S, Stewart TE, Mehta S, Wax R, Lapinsky SE. Handheld computing in medicine. J Am Med Inform Assoc 2003. Mar-Apr;10(2):139-149. 10.1197/jamia.M1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T 2014. May;39(5):356-364. [PMC free article] [PubMed] [Google Scholar]
- 15.McAlearney AS, Schweikhart SB, Medow MA. Doctors’ experience with handheld computers in clinical practice: qualitative study. BMJ 2004. May;328(7449):1162. 10.1136/bmj.328.7449.1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McAlearney AS, Schweikhart SB, Medow MA. Organizational and physician perspectives about facilitating handheld computer use in clinical practice: results of a cross-site qualitative study. J Am Med Inform Assoc 2005. Sep-Oct;12(5):568-575. 10.1197/jamia.M1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grasso MA, Yen MJ, Mintz ML. Survey of handheld computing among medical students. Comput Methods Programs Biomed 2006. Jun;82(3):196-202. 10.1016/j.cmpb.2006.03.005 [DOI] [PubMed] [Google Scholar]
- 18.Yarbrough AK, Smith TB. Technology acceptance among physicians: a new take on TAM. Med Care Res Rev 2007. Dec;64(6):650-672 . 10.1177/1077558707305942 [DOI] [PubMed] [Google Scholar]
- 19.Morris CG, Church L, Vincent C, Rao A. PDA usage and training: targeting curriculum for residents and faculty. Fam Med 2007. Jun;39(6):419-424. [PubMed] [Google Scholar]
- 20.Jamal A, Temsah MH, Khan SA, Al-Eyadhy A, Koppel C, Chiang MF. Mobile Phone Use Among Medical Residents: A Cross-Sectional Multicenter Survey in Saudi Arabia. JMIR Mhealth Uhealth 2016. May;4(2):e61. 10.2196/mhealth.4904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McLeod TG, Ebbert JO, Lymp JF. Survey assessment of personal digital assistant use among trainees and attending physicians. J Am Med Inform Assoc 2003. Nov-Dec;10(6):605-607. 10.1197/jamia.M1313 [DOI] [PMC free article] [PubMed] [Google Scholar]


