Abstract
BACKGROUND & AIMS:
Abdominal pain is the most common gastrointestinal symptom reported in ambulatory clinics, but little is known about its prevalence and burden of illness in the general community. We conducted a population-based survey to determine the epidemiology, clinical characteristics, and healthcare-seeking behavior of persons with abdominal pain.
METHODS:
Using an online survey research firm, we recruited a representative sample of adults (18 years or older) with a history of abdominal pain. The survey included questions about abdominal pain severity as measured by GI PROMIS (a validated patient-reported outcome questionnaire), healthcare-seeking behaviors, and tests performed to evaluate symptoms. We used multivariable regression models to adjust for confounding.
RESULTS:
Overall, 24,929 individuals accessed the survey and 10,300 respondents reported experiencing abdominal pain and completed the questionnaire. Most participants (81.0%) were symptomatic in the past week, as measured by GI PROMIS. Of participants with prior pain, 61.5% sought medical care for their symptoms; non-Hispanic blacks, Latinos, and participants with more education, insurance, a usual source of care, comorbidities, and more severe pain had increased odds for seeking care. Participants who sought care consulted with the following providers: primary care physicians (84.5%), gastroenterologists (39.2%), nurse practitioners or physician assistants (18.6%), obstetricians or gynecologists (8.3%), general surgeons (7.1%), or rheumatologists (3.2%). Moreover, 72.4% of healthcare seekers received tests to evaluate their pain: cross-sectional imaging (54.2%), colonoscopy (52.3%), upper endoscopy (40.8%), exploratory surgery (6.3%), or capsule endoscopy (5.0%).
CONCLUSIONS:
The burden of illness and healthcare use associated with abdominal pain is high in the United States. However, 2 of 5 individuals did not seek care for their symptoms and many of them might have undiagnosed, treatable disorders.
Keywords: abdominal discomfort, acute hepatic porphyria, gastrointestinal, healthcare seeking, patient-reported outcome
INTRODUCTION
Abdominal pain is the leading gastrointestinal (GI) symptom prompting ambulatory visits in the U.S.,1 yet less is known about its prevalence and burden in the general community; most prior studies focused on functional GI disorders such as irritable bowel syndrome (IBS) and functional dyspepsia.2, 3 While there have been some efforts that specifically examined the population prevalence of abdominal pain, these studies were either limited by having predominately non-Hispanic white cohorts, only examining for the presence of upper abdominal pain, excluding participants with physician-diagnosed GI disorders, or were performed decades ago.4–6 These studies also did not assess in detail healthcare utilization and diagnostic testing.4–6
To update our understanding of the prevalence and characteristics of abdominal pain in the community, we performed a survey of nearly 25,000 adults from across the U.S. Namely, we assessed the epidemiology, clinical characteristics, and healthcare seeking of those with pain. Moreover, given the study’s large sample size, we also aimed to investigate whether the prevalence of rare abdominal pain symptom constellations could be ascertained, using acute hepatic porphyria (AHP) as a model phenotype.
METHODS
Study Design
We performed a population-based survey of community-dwelling adults between November 6 to November 25, 2018. Respondents completed an online, self-administered questionnaire that was estimated to take 5–10 minutes to complete. This study was approved by the Cedars-Sinai Institutional Review Board (Pro55392).
A representative sample of Americans ≥18 years old was recruited through Cint, a survey research firm. Cint employs quotas for age, sex, and region based on latest U.S. Census data. They also have measures for preventing multiple responses per user and employ a reward system based on marketplace points, which we describe elsewhere.7, 8 Participants who completed the current survey were awarded points worth $0.62.
Cint research panels sent participants who met Census quota criteria an email inviting them to complete an online survey. Users who clicked the link were then brought to our survey home page, which was generically described as a “national health survey.” Survey invitations were distributed until we reached our sample size goal of approximately 10,000 respondents with abdominal pain, allowing us to create a robust belly pain-focused dataset.
Study Population
All respondents ≥18 years old who accessed the survey were first asked which of the following GI symptoms they had ever experienced (presented in random order): abdominal or belly pain; bloating; bowel incontinence; constipation; diarrhea; difficulty swallowing; heartburn/acid reflux; nausea/vomiting; none of the above. Only those who reported abdominal pain were allowed to continue with the remaining survey. We employed a ‘blinded’ screener listing 8 GI symptoms to increase the likelihood that respondents had abdominal pain in the past and were not simply seeking compensation.
Survey Instrument
To characterize individuals reporting abdominal pain, respondents completed questions on their abdominal pain onset, severity as measured by the National Institutes of Health (NIH) Patient-Reported Outcomes Measurement Information System (PROMIS) abdominal pain questionnaire,8, 9 locus of control using an adapted version of the diabetes locus of control scale,10 disability related to their pain, and perceived etiology of their symptoms. We also examined whether respondents experienced episodes of excruciating abdominal pain that lasted more than one day and required them to seek urgent medical care.
To assess healthcare-seeking behavior, we asked all individuals with abdominal pain: “Have you ever discussed your belly pain with a healthcare provider?” For those who sought care, we determined the provider(s) with whom they consulted and diagnostic tests that were performed specifically to evaluate their pain.
Finally, we measured their physical and mental health using the NIH PROMIS Global Health Short Form Questionnaire.11 We also collected medical comorbidity data and then posed demographic and socioeconomic questions.
Outcomes
The primary outcome measure was whether individuals had experienced abdominal pain in the past, as assessed through the GI symptom screener. We also assessed whether those with pain discussed their symptoms with a healthcare provider.
As the sample size of this study was large, we also investigated whether rare abdominal pain symptom constellations could be identified, using AHP as a model phenotype. AHP is a family of rare genetic diseases (acute intermittent porphyria, hereditary coproporphyria, variegate porphyria, and ALA-dehydratase deficiency porphyria) characterized by potentially life-threatening attacks of severe, diffuse abdominal pain with concomitant neuropsychiatric, neurovisceral, and cutaneous manifestations.12, 13 It is also among a small set of visceral pain conditions recognized by the National Organization for Rare Disorders that can stand out on the basis of patient-reported symptoms, yet can present with symptoms that overlap with common visceral pain conditions, such as IBS or functional abdominal pain. Moreover, as AHP is rare, clinicians may not be aware of and/or routinely assess for concomitant non-GI symptoms in patients with multiple episodes of excruciating pain, leading to missed and delayed diagnosis and treatment.23 The criteria we used to determine the presence of ‘AHP-like’ symptoms are listed in Supplementary Table 1; all respondents were eligible for this analysis, including those previously diagnosed by a physician with another condition.
Statistical Analyses
All descriptive and statistical analyses were performed in Stata 13.1 (StataCorp LP, College Station, TX) and a two-tailed p-value <.05 was considered significant. We used bivariate analyses to compare individuals with abdominal pain who did or did not seek healthcare for their symptoms, as well as those who had or did not have AHP-like symptoms. Continuous variables were compared between groups using either Student’s t-test or the analysis of variance test. Categorical variables were compared using the chi-squared test. For multivariable analyses, we performed logistic regression models to identify independent predictors and to calculate odds ratios (OR) and 95% confidence intervals (CI). The regression models were performed on our outcomes of seeking healthcare for pain and having AHP-like symptoms.
Qualitative Analyses
The survey included an open-ended question asking respondents about their thoughts regarding the etiology of their pain: “In your own words, what do you think is the cause(s) of your belly pain?” A summative content analysis was adopted to examine their perceived abdominal pain etiologies.14 We coded the free texts (word, sentence, and paragraph) and organized them into categories.
RESULTS
Study Population
Overall, 260,613 individuals were invited to complete the survey. Of the 24,929 respondents who accessed the survey, 13,076 (52.5%) did not endorse prior abdominal pain, 993 (4.0%) did not provide consent, and 560 (2.2%) eligible respondents (consented and had prior pain) did not finish the survey. Therefore, our study cohort included 10,300 individuals with a history of abdominal pain; demographics are shown in Table 1 with comparisons to the U.S. population in Supplementary Table 2.
TABLE 1.
Study population demographics (N=10,300).
| Variable | n (%) or mean (standard deviation) |
|---|---|
|
| |
| Age (years): | |
| 18 to 29 | 2,032 (19.7%) |
| 30 to 39 | 2,076 (20.2%) |
| 40 to 49 | 2,100 (20.4%) |
| 50 to 59 | 1,782 (17.3%) |
| ≥60 | 2,310 (22.4%) |
|
| |
| Sex: | |
| Male | 4,252 (41.3%) |
| Female | 6,019 (58.4%) |
| Other | 29 (0.3%) |
|
| |
| Race/ethnicity: | |
| Non-Hispanic white | 7,877 (76.5%) |
| Non-Hispanic black | 765 (7.4%) |
| Latino | 873 (8.5%) |
| Non-Hispanic Asian | 310 (3.0%) |
| Other | 475 (4.6%) |
|
| |
| Marital status: | |
| Married or in a long-term relationship | 6,256 (60.7%) |
| Not married | 4,044 (39.3%) |
|
| |
| Educational attainment: | |
| High school degree or less | 2,235 (21.7%) |
| Some college | 3,408 (33.1%) |
| College degree | 3,398 (33.0%) |
| Advanced graduate degree | 1,259 (12.2%) |
|
| |
| Employment status: | |
| Not employed a | 4,311 (41.9%) |
| Employed or full-time student | 5,989 (58.2%) |
|
| |
| Total household income: | |
| $0 to 50,000 | 4,988 (48.4%) |
| $50,001 to 100,000 | 3,319 (32.2%) |
| $100,001 to 200,000 | 1,356 (13.2%) |
| ≥$200,001 | 180 (1.8%) |
| Prefer not to say | 457 (4.4%) |
|
| |
| U.S. region: | |
| Northeast | 2,255 (21.9%) |
| South | 3,877 (37.6%) |
| Midwest | 1,843 (17.9%) |
| West | 2,325 (22.6%) |
|
| |
| Has health insurance | 9,265 (90.0%) |
|
| |
| Has usual source of care | 7,959 (77.3%) |
|
| |
| Has comorbidity that affects GI tract b | 4,805 (46.7%) |
|
| |
| Abdominal pain locus of control (0–5) c | 2.8 (0.9) |
|
| |
| Abdominal pain PROMIS percentile score d | 31.2 (31.3) |
|
| |
| Physical global health PROMIS T-score e | 45.3 (8.2) |
|
| |
| Mental global health PROMIS T-score e | 46.0 (9.4) |
: includes those who reported being unemployed, unable to work owing to a disability, on leave of absence from work, retired, or a homemaker;
: see Supplementary Table 3 for list of associated physician-diagnosed conditions;
: locus of control measures the extent to which individuals believe they can control events that affect them—higher score corresponds to lower perceived control of events that affect their abdominal pain;
: higher score corresponds to more severe symptoms with 50 being the median among all individuals with abdominal pain;
: higher score corresponds to better health.
Abdominal Pain Characteristics and Perceived Etiologies
The 10,300 participants reported the following when asked when they first started experiencing abdominal pain: ≤5 years ago (6,180, 60.0%); 6–10 years ago (1,524, 14.8%); ≥11 years ago (2,485, 24.1%); unknown (111, 1.1%). We found that 8,344 (81.0%) respondents were symptomatic in the past week as measured by NIH GI PROMIS. Responses for each individual PROMIS item are listed in Table 2. Among the 9,652 individuals who were ever employed, 3,921 (40.6%) reported that their abdominal pain caused difficulty working at a job or business, and 1,101 (11.4%) stated that their pain prevented them from working for at least one year.
TABLE 2.
Abdominal pain severity as measured by NIH GI PROMIS (N=10,300).
| NIH GI PROMIS abdominal pain item | n (%) |
|---|---|
|
| |
| In the past 7 days, how often did you have belly pain? | |
| Never | 3,844 (37.3%) |
| One day | 3,763 (36.5%) |
| 2–6 days | 2,090 (20.3%) |
| Once a day | 297 (2.9%) |
| More than once a day | 306 (3.0%) |
|
| |
| In the past 7 days, at its worst, how would you rate your belly pain? a | |
| Not bad at all | 311 (4.8%) |
| A little bad | 2,032 (31.5%) |
| Somewhat bad | 2,597 (40.2%) |
| Quite bad | 1,175 (18.2%) |
| Very bad | 341 (5.3%) |
|
| |
| In the past 7 days, how much did belly pain interfere with your day-to-day activities? a | |
| Not at all | 988 (15.3%) |
| A little bit | 2,574 (39.9%) |
| Somewhat | 1,771 (27.4%) |
| Quite a bit | 805 (12.5%) |
| Very much | 318 (4.9%) |
|
| |
| In the past 7 days, how much did belly pain bother you? a | |
| Not at all | 146 (2.3%) |
| A little bit | 2,413 (37.4%) |
| Somewhat | 2,090 (32.4%) |
| Quite a bit | 1,351 (20.9%) |
| Very much | 459 (7.1%) |
|
| |
| In the past 7 days, how often did you have discomfort in your belly? | |
| Never | 2,004 (19.5%) |
| Rarely | 2,810 (27.3%) |
| Sometimes | 3,672 (35.7%) |
| Often | 1,514 (14.7%) |
| Always | 300 (2.9%) |
: 3,844 respondents did not answer this question as they did not endorse abdominal pain in the past 7 days via the first PROMIS item.
Of the overall cohort, 3,558 (34.5%) stated that they previously experienced excruciating abdominal pain that lasted more than a day and required urgent medical attention. They reported the following number of episodes of severe pain: 1 (610, 17.1%); 2 (807, 22.7%); 3 (665, 18.7%); 4 (265, 7.5%); ≥5 (1,211, 34.0%). Participants noted that their most recent episode occurred: within last 6 months (1,730, 48.6%); 6–12 months ago (582, 16.4%); 1–2 years ago (416, 11.7%); 2–3 years ago (213, 6.0%); ≥3 years ago (617, 17.3%).
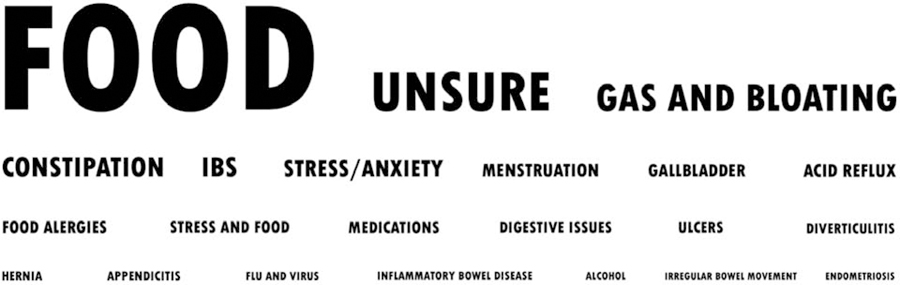
Additionally, 4,805 (46.7%) of 10,300 individuals reported having been diagnosed by a physician with conditions that affect the GI tract or are commonly associated with GI disorders (Supplementary Table 3). Respondents were also asked to comment on the perceived etiology of their pain through a free-text question. Figure 1 shows a word cloud generated from the qualitative content analysis detailing the various triggers reported by the 9,062 (88.0%) participants who provided a response.
FIGURE 1.
Qualitative content analysis of perceived causes of abdominal pain (n=9,062). Note: font size corresponds to prevalence.
Abdominal Pain Healthcare-Seeking Behavior and Diagnostic Studies
Overall, 6,329 (61.5%) respondents discussed their pain with a healthcare professional. They consulted with the following providers: primary care physician/internist (5,349, 84.5%); gastroenterologist (2,483, 39.2%); nurse practitioner or physician assistant (1,180, 18.6%); obstetrician/gynecologist (523, 8.3%); general surgeon (448, 7.1%); rheumatologist (201, 3.2%); neurologist (165, 2.6%); cardiologist (163, 2.6%); hematologist (117, 1.9%); hepatologist (116, 1.8%).
Table 3 presents results from the multivariable regression on abdominal pain healthcare seeking. Non-Hispanic blacks, Latinos, and those in the other race/ethnicity group were more likely to have sought care versus non-Hispanic whites. Individuals with more education, employment, insurance, a usual source of care, comorbidities, lower perceived locus of control, and more severe pain also had increased odds for seeking care. Conversely, better physical health was associated with lower odds for seeking care. No associations were seen for the remaining variables.
TABLE 3.
Predictors of having sought healthcare for abdominal pain (N=10,300).
| Variable | Sought healthcare for abdominal pain (n=6,329) | OR [95% CI] a |
|---|---|---|
|
| ||
| Age (years): | ||
| 18 to 29 | 1,140 (56.1%) | reference |
| 30 to 39 | 1,258 (60.6%) | 1.05 [0.91–1.22] |
| 40 to 49 | 1,300 (61.9%) | 0.91 [0.78–1.06] |
| 50 to 59 | 1,158 (65.0%) | 0.93 [0.79–1.09] |
| ≥60 | 1,473 (63.8%) | 0.88 [0.74–1.04] |
|
| ||
| Sex: | ||
| Male | 2,550 (60.0%) | reference |
| Female | 3,759 (62.5%) | 0.96 [0.87–1.06] |
| Other | 20 (69.0%) | 1.75 [0.72–4.24] |
|
| ||
| Race/ethnicity: | ||
| Non-Hispanic white | 4,795 (60.9%) | reference |
| Non-Hispanic black | 508 (66.4%) | 1.28 [1.06–1.54] |
| Latino | 567 (65.0%) | 1.33 [1.12–1.59] |
| Non-Hispanic Asian | 147 (47.4%) | 0.93 [0.72–1.21] |
| Other | 312 (65.7%) | 1.33 [1.06–1.67] |
|
| ||
| Marital status: | ||
| Married or in a long-term relationship | 3,899 (62.3%) | reference |
| Not married | 2,430 (60.1%) | 0.98 [0.88–1.08] |
|
| ||
| Education level: | ||
| High school graduate or less | 1,337 (59.8%) | reference |
| Some college | 2,150 (63.1%) | 1.21 [1.06–1.37] |
| College graduate | 2,063 (60.7%) | 1.17 [1.02–1.33] |
| Graduate degree | 779 (61.9%) | 1.21 [1.01–1.45] |
|
| ||
| Employment status: | ||
| Not employed | 2,777 (64.4%) | reference |
| Employed or full-time student | 3,552 (59.3%) | 1.12 [1.00–1.25] |
|
| ||
| Total household income: | ||
| $0 to 50,000 | 3,088 (61.9%) | reference |
| $50,001 to 100,000 | 2,025 (61.0%) | 1.05 [0.94–1.17] |
| $100,001 to 200,000 | 847 (62.5%) | 1.11 [0.95–1.30] |
| ≥$200,001 | 117 (65.0%) | 1.27 [0.88–1.85] |
| Prefer not to say | 252 (55.1%) | 1.08 [0.86–1.35] |
|
| ||
| U.S. region: | ||
| Northeast | 1,434 (63.6%) | reference |
| South | 2,398 (61.9%) | 0.90 [0.80–1.02] |
| Midwest | 1,115 (60.5%) | 0.91 [0.78–1.05] |
| West | 1,382 (59.4%) | 0.93 [0.81–1.07] |
|
| ||
| Health insurance status: | ||
| Uninsured | 462 (44.6%) | reference |
| Insured | 5,867 (63.3%) | 1.29 [1.10–1.52] |
|
| ||
| Has a usual source of care: | ||
| No | 759 (32.4%) | reference |
| Yes | 5,570 (70.0%) | 3.90 [3.49–4.37] |
|
| ||
| Has comorbidity that affects GI tract: | ||
| No | 2,406 (43.8%) | reference |
| Yes | 3,923 (81.6%) | 4.26 [3.85–4.72] |
|
| ||
| Abdominal pain locus of control (0–5) b | 2.9 (0.9) | 1.28 [1.20–1.36] |
|
| ||
| Abdominal pain PROMIS percentile score c | 37.5 (32.8) | 1.012 [1.010–1.014] |
|
| ||
| Physical global health PROMIS T-score d | 43.9 (8.2) | 0.985 [0.977–0.993] |
|
| ||
| Mental global health PROMIS T-score d | 45.4 (9.4) | 1.005 [0.998–1.011] |
Data are presented as mean (standard deviation) or n (% of row).
: all variables in the table were included in the multivariable logistic regression model;
: locus of control measures the extent to which individuals believe they can control events that affect them—higher score corresponds to lower perceived control of events that affect their abdominal pain;
: higher score corresponds to more severe symptoms with 50 being the median among all individuals with abdominal pain;
: higher score corresponds to better health.
Of the patients who sought healthcare (n=6,329), 4,582 (72.4%) underwent testing and/or procedures to evaluate their pain. The most common tests were abdominal CT or MRI scan (2,485, 54.2%), colonoscopy (2,394, 52.3%), and upper endoscopy (1,867, 40.8%). Exploratory surgery (288, 6.3%) and capsule endoscopy (229, 5.0%) were used less often.
Among the 3,558 individuals who had excruciating bouts of pain that lasted more than a day, 3,271 (91.9%) sought medical care. Of those who sought care, most went to an emergency room (1,908, 58.3%) or doctor’s office (1,493, 45.6%). This was followed by visits to urgent care (825, 25.2%) and health centers (513, 15.7%). Moreover, 573 (17.5%) participants were hospitalized for their symptoms.
AHP-Like Symptoms—Broad Definition
Due to the study’s large sample size, we also assessed whether the prevalence of rare abdominal pain symptom constellations could be ascertained, using AHP as a model phenotype. We found that 2,413 (23.4%) of the 10,300 respondents noted AHP-like symptoms using our broad definition. Supplementary Table 4 presents demographic data for this subset. The most commonly reported co-occurring symptoms were autonomic (2,358, 97.7%), central (2,328, 96.5%), and peripheral (1,418, 58.8%) nervous system manifestations. We also noted that 527 (21.8%) individuals experienced urine color change to dark red or brown and 159 (6.6%) had skin blisters on sun-exposed areas. In multivariable regression (Table 4), those who identified as Latino or other race/ethnicity and who had a usual source of care, comorbidities, lower perceived locus of control, and more severe pain had higher odds for having AHP-like symptoms. Conversely, increasing age and better physical health were associated with lower odds for reporting such symptoms. We found no associations with the remaining covariates.
TABLE 4.
Predictors of having AHP-like symptoms (N=10,300).
| Variable | AHP-like symptoms: broad definition a (n=2,413) | OR [95% CI]b | AHP-like symptoms: specific definition c (n=734) | OR [95% CI]b | |
|---|---|---|---|---|---|
|
| |||||
| Age (years): | |||||
| 18 to 29 | 545 (26.8%) | reference | 210 (10.3%) | reference | |
| 30 to 39 | 594 (28.6%) | 0.95 [0.81–1.12] | 219 (10.6%) | 0.75 [0.59–0.95] | |
| 40 to 49 | 562 (26.8%) | 0.74 [0.62–0.87] | 157 (7.5%) | 0.47 [0.36–0.60] | |
| 50 to 59 | 404 (22.7%) | 0.55 [0.46–0.65] | 113 (6.3%) | 0.39 [0.29–0.51] | |
| ≥60 | 308 (13.3%) | 0.33 [0.27–0.41] | 35 (1.5%) | 0.12 [0.08–0.19] | |
|
| |||||
| Sex: | |||||
| Male | 945 (22.2%) | reference | 370 (8.7%) | reference | |
| Female | 1,461 (24.3%) | 0.97 [0.87–1.08] | 360 (6.0%) | 0.52 [0.43–0.62] | |
| Other | 7 (24.1%) | 1.09 [0.43–2.77] | 4 (13.8%) | 2.26 [0.71–7.19] | |
|
| |||||
| Race/ethnicity: | |||||
| Non-Hispanic white | 1,715 (21.8%) | reference | 496 (6.3%) | reference | |
| Non-Hispanic black | 217 (28.4%) | 1.16 [0.96–1.40] | 71 (9.3%) | 1.13 [0.84–1.52] | |
| Latino | 282 (32.3%) | 1.43 [1.19–1.71] | 95 (10.9%) | 1.23 [0.94–1.60] | |
| Non-Hispanic Asian | 45 (14.5%) | 0.91 [0.64–1.30] | 18 (5.8%) | 1.29 [0.75–2.20] | |
| Other | 154 (32.4%) | 1.53 [1.21–1.93] | 54 (11.4%) | 1.43 [1.02–2.02] | |
|
| |||||
| Marital status: | |||||
| Married or in a long-term relationship | 1,483 (23.7%) | reference | 456 (7.3%) | reference | |
| Not married | 930 (23.0%) | 0.93 [0.83–1.04] | 278 (6.9%) | 0.97 [0.81–1.17] | |
|
| |||||
| Education level: | |||||
| High school graduate or less | 621 (27.8%) | reference | 182 (8.1%) | reference | |
| Some college | 851 (25.0%) | 1.00 [0.87–1.15] | 250 (7.3%) | 1.15 [0.92–1.44] | |
| College graduate | 712 (21.0%) | 0.91 [0.78–1.05] | 222 (6.5%) | 1.15 [0.90–1.47] | |
| Graduate degree | 229 (18.2%) | 0.93 [0.76–1.16] | 80 (6.4%) | 1.45 [1.03–2.05] | |
|
| |||||
| Employment status: | |||||
| Not employed | 1,059 (24.6%) | reference | 291 (6.8%) | reference | |
| Employed or full-time student | 1,354 (22.6%) | 1.07 [0.95–1.22] | 443 (7.4%) | 1.10 [0.90–1.34] | |
|
| |||||
| Total household income: | |||||
| $0 to 50,000 | 1,314 (26.3%) | reference | 381 (7.6%) | reference | |
| $50,001 to 100,000 | 723 (21.8%) | 1.01 [0.88–1.14] | 234 (7.1%) | 1.22 [0.99–1.50] | |
| $100,001 to 200,000 | 261 (19.3%) | 0.84 [0.69–1.01] | 87 (6.4%) | 0.93 [0.68–1.26] | |
| ≥$200,001 | 40 (22.2%) | 1.19 [0.77–1.83] | 17 (9.4%) | 1.75 [0.92–3.30] | |
| Prefer not to say | 75 (16.4%) | 0.93 [0.70–1.23] | 15 (3.3%) | 0.84 [0.48–1.48] | |
|
| |||||
| U.S. region: | |||||
| Northeast | 518 (23.0%) | reference | 144 (6.4%) | reference | |
| South | 993 (25.6%) | 1.09 [0.95–1.26] | 292 (7.5%) | 1.17 [0.92–1.48] | |
| Midwest | 371 (20.1%) | 1.03 [0.86–1.22] | 126 (6.8%) | 1.50 [1.13–1.98] | |
| West | 531 (22.8%) | 1.10 [0.94–1.29] | 172 (7.4%) | 1.33 [1.02–1.72] | |
|
| |||||
| Health insurance status: | |||||
| Uninsured | 217 (21.0%) | reference | 69 (6.7%) | reference | |
| Insured | 2,196 (23.7%) | 1.03 [0.85–1.24] | 665 (7.2%) | 0.97 [0.72–1.30] | |
|
| |||||
| Has a usual source of care: | |||||
| No | 290 (12.4%) | reference | 92 (3.9%) | reference | |
| Yes | 2,123 (26.7%) | 2.26 [1.94–2.63] | 642 (8.1%) | 1.75 [1.36–2.25] | |
|
| |||||
| Has comorbidity that affects GI tract: | |||||
| No | 720 (13.1%) | reference | 194 (3.5%) | reference | |
| Yes | 1,693 (35.2%) | 2.78 [2.47–3.12] | 540 (11.2%) | 2.26 [1.86–2.75] | |
|
| |||||
| Abdominal pain locus of control (0–5) d | 3.2 (0.9) | 1.73 [1.61–1.85] | 3.5 (0.8) | 1.66 [1.48–1.86] | |
|
| |||||
| Abdominal pain PROMIS percentile score e | 50.0 (34.7) | 1.010 [1.008–1.012] | 64.8 (30.9) | 1.021 [1.018–1.025] | |
|
| |||||
| Physical global health PROMIS T-score f | 40.9 (7.9) | 0.955 [0.946–0.965] | 39.0 (7.4) | 0.948 [0.933–0.963] | |
|
| |||||
| Mental global health PROMIS T-score f | 43.1 (9.3) | 1.002 [0.995–1.010] | 42.1 (9.5) | 1.000 [0.989–1.012] | |
Data are presented as mean (standard deviation) or n (% of row).
: Includes those with ≥2 episodes of excruciating abdominal pain along with ≥2 of the following concomitant symptoms: urine color change, skin blisters, and peripheral (muscle weakness, pain or numbness in arms, legs, or back), central (anxiety, confusion, depression, hallucinations, insomnia, seizures), and autonomic (constipation, hypertension, nausea/vomiting, tachycardia) nervous system manifestations;
: all variables in the table were included in the multivariable logistic regression model;
: includes ≥2 episodes of excruciating abdominal pain along with ≥2 of the following concomitant symptoms: urine color change, skin blisters, and peripheral (muscle weakness, pain or numbness in arms, legs, or back) and central (confusion, hallucinations, seizures) nervous system manifestations;
: locus of control measures the extent to which individuals believe they can control events that affect them—higher score corresponds to lower perceived control of events that affect their abdominal pain;
: higher score corresponds to more severe symptoms with 50 being the median among all individuals with abdominal pain;
: higher score corresponds to better health.
AHP-Like Symptoms—Specific Definition
We also employed a narrow definition that included symptoms more specific to AHP and typically not seen in more common GI conditions. Here, 734 (7.1%) individuals from the overall cohort met this criterion (Supplementary Table 4 lists their demographics). We also noted that PROMIS scores were highest (indicating more severe pain) among this group (64.8 ± 30.9; p<.001) vs. those who only met the AHP-like broad criteria (n=1,679; 43.5 ± 34.3) and those who did not meet either (n=7,887; 25.4 ± 27.7).
The most prevalent concomitant symptoms were peripheral (705, 96.1%) and central nervous system manifestations (540, 73.6%). We also noted that 387 (52.7%) and 149 (20.3%) individuals reported urine color change to dark red or brown and skin blisters on sun-exposed areas, respectively. Results from the regression were comparable to those on the broad definition, save for a few exceptions (Table 4). Males and those with a graduate degree and who lived in the Midwest and West regions were more likely to have AHP-like symptoms using the specific definition. Latinos were also no longer more likely to have AHP-like symptoms vs. non-Hispanic whites.
DISCUSSION
In this large nationwide survey of nearly 25,000 Americans, we found that abdominal pain is common, affecting nearly half of adults at some point in their lives. Comparisons of the prevalence seen in our study to that found in other reports are challenging given the different cohorts, time frames, and definitions used. For example, in the 1990s, Camilleri and colleagues found that 5% of respondents reported upper abdominal pain or discomfort at least once a month over the past 3 months4 while Sandler et al. noted that 22% had pain or discomfort within the past month.5 More recently, as part of the development and validation of the Rome IV questionnaires, Palsson and colleagues found that about 40% of respondents in the general population who did not have physician-diagnosed lower GI disorders had at least some discomfort or pain in the past 3 months.6 In contrast, our study identified those with pain (not discomfort) anywhere in the abdomen at any point in the past and in the last week as well as included all-comers, such as those with physician-diagnosed GI disorders.
Among those with prior abdominal pain, we also determined the proportion that sought medical care for their symptoms; to date, there have been limited studies focused on healthcare-seeking behaviors among all-comers with abdominal pain. In the present cohort, we found that only 61.5% of those in the general population discussed their pain with a healthcare provider. This percentage is higher than that found by Sandler and colleagues, as they noted that 19.1% of respondents with abdominal pain sought care.5 This difference is likely due to the differing time frames noted in the survey questions; we assessed for healthcare-seeking behavior among those who had ever experienced abdominal pain whereas Sandler et al. examined such behavior among those who had symptoms in the past month. In multivariable regression, after adjusting for access to care factors, we found that non-Hispanic blacks and Latinos are more likely to seek care for their pain when compared to non-Hispanic whites. While prior research shows that racial/ethnic minorities, in general, use health services at a lower rate vs. non-Hispanic whites,15 our findings suggest that abdominal pain may disproportionality impact the quality of life for non-Hispanic blacks and Latinos, causing them to be more likely to seek care. It may also reflect cultural factors in reporting specific symptoms to healthcare providers. Given the decrements to quality of life caused by abdominal pain and the potential for serious underlying pathology, further research to better understand individuals’ attitudes and barriers to healthcare seeking are warranted.
Additionally, we found that individuals with lower locus of control (i.e., believe they have less control over events that impact their symptoms) are more likely to seek care for their pain. However, they may be resistant to accepting their physicians’ assessments and recommendations, particularly when diagnosed with a ‘non-organic’, functional disorder. Prior research has shown that patients with IBS that have lower locus of control are less likely to rapidly respond to cognitive behavioral therapy.16 By assessing for the presence of this maladaptive cognition early on (“How much control do you think you have over your belly pain?”17), it may allow for a more tailored approach and perhaps improved patient satisfaction and outcomes.
In this study, we also questioned respondents regarding any diagnostic testing they underwent specifically for evaluation of their pain. Among those who had testing, 52.3% and 40.8% underwent colonoscopy or upper endoscopy, respectively. Colonoscopic evaluation is generally not indicated for abdominal pain,18 and while we did not have access to medical records to determine the indication, our results suggests its possible overuse. As the yield of colonoscopy in isolated abdominal pain is low,19, 20 efforts to reduce its inappropriate use are warranted. Upper endoscopy similarly may be overutilized since national dyspepsia guidelines do not suggest endoscopy for those <60 years old even in the presence of alarm features.21 This recommendation was informed by a meta-analysis that found that only 0.8% of individuals with dyspepsia had cancer and that alarm features have limited predictive utility.22
We also uniquely investigated the proportion of subjects who noted AHP-like symptoms. As AHP is rare, clinicians may not be aware of and/or routinely assess for the presence of concomitant neuropsychiatric, neurovisceral, and cutaneous symptoms among those with multiple episodes of excruciating abdominal pain. This study systematically assessed for these symptoms and found that 23.4% of those with prior abdominal pain have profiles consistent with AHP manifestations. Even when using a more specific definition that excluded central and autonomic symptoms also seen in common GI disorders (e.g., IBS, functional dyspepsia) and conditions that cause dysautonomia (e.g., Ehlers-Danlos syndrome, postural orthostatic tachycardia syndrome, diabetes, Parkinson’s disease), we still noted that 7.1% of individuals have AHP-like symptoms. While most with AHP-like symptoms will likely not have AHP given its low combined prevalence of approximately 5 cases per 100,000 persons, it remains important for clinicians to include it in the differential diagnosis among individuals with recurrent, severe episodes of pain as it leads to significant morbidity and mortality.12, 13 Clinician insight of co-occurring neuropsychiatric, neurovisceral, and cutaneous symptoms may also prompt earlier testing for AHP with low cost, non-invasive testing including urine porphobilinogen or aminolevulinic acid levels,12, 13 thereby decreasing the delay to diagnosis. Prior studies reported an up to 15-year delay from symptom onset to diagnosis of AHP.23 Earlier diagnosis could also lead to sooner access to effective medicines,12, 24 reduced healthcare costs, and improved outcomes.
Our study has strengths and potential limitations. As for strengths, this is one of the largest U.S. studies of participants with abdominal pain, with extensive clinical and healthcare seeking data from over 10,000 Americans from the general population. Another strength is the use of the NIH PROMIS questionnaires, which were rigorously developed under NIH oversight and are a valid and reliable way to assess severity of abdominal pain.9 We also notably assessed for the prevalence and predictors of symptom complexes consistent with AHP manifestations. To our knowledge, this study is the first to examine the prevalence of AHP-like symptoms in a systematic manner, and we found that one-fourth of those with prior abdominal pain have AHP-like symptoms. While AHP is rare, these findings suggest that clinicians should include AHP on the differential diagnosis and take a proactive approach to eliciting for concomitant neurologic, psychiatric, skin, and urologic manifestations when evaluating those with multiple episodes of unexplained severe abdominal pain.
One limitation may be that the data were acquired via an internet-based survey, so there could be concerns about generalizability, particularly among elderly individuals who lack computing skills or online access. However, at the time of the survey in 2018, two-thirds of those ≥65 years old used the internet.25 We also employed age-based quotas for respondents, ensuring an appropriate representation of elderly individuals. As with all observational studies, our findings are also susceptible to residual confounding. There is also risk of recall bias since the symptom and healthcare seeking data were self-reported. Prior studies that assessed the validity of self-reported healthcare seeking found that patients generally under-report their healthcare utilization26; we therefore may have underestimated the prevalence of healthcare seeking for abdominal pain as well as the use of diagnostic testing. Participation and selection bias are also possible as Cint provided a small financial incentive for those who completed the survey. While the demographics of our cohort are largely similar to the U.S. general population, our sample had a higher proportion from lower-income households than expected. Finally, among those with AHP-like symptom complexes, we did not evaluate what proportion truly had AHP with confirmatory testing nor did we assess whether symptoms for those with AHP improved with appropriate treatment; this is worthy of further research.
In conclusion, in this large nationwide survey of nearly 25,000 community-dwelling Americans, we found that the burden of illness and healthcare utilization associated with abdominal pain is high. However, we noted that 2 of 5 of those with abdominal pain have not sought medical care for their symptoms and many of them may have undiagnosed, treatable disorders.
Supplementary Material
WHAT YOU NEED TO KNOW.
BACKGROUND:
Researchers performed a nationwide survey of nearly 25,000 adults to evaluate the epidemiology and healthcare seeking of persons with abdominal pain.
FINDINGS:
The study found that 38.5% of participants with abdominal pain have not sought medical care for their symptoms.
IMPLICATIONS FOR PATIENT CARE:
Almost 40% of Americans do not seek care for their abdominal pain—many of these persons might have undiagnosed, treatable disorders.
Acknowledgments
GRANT SUPPORT: This study was funded by Alnylam Pharmaceuticals, a company involved in the development and testing of treatments for acute hepatic porphyria. The study sponsor did not have a role in the collection, analysis, or interpretation of data, or drafting of the manuscript. The Cedars-Sinai Center for Outcomes Research and Education (CS-CORE) is supported by The Marc and Sheri Rapaport Fund for Digital Health Sciences & Precision Health. Dr. Almario was supported by a career development award from the American College of Gastroenterology. Drs. Almario and Spiegel are supported by a CTSI grant from the NIH/NCATS UL1TR001881-01.
WRITING ASSISTANCE: No medical writing support was received.
ABBREVIATIONS:
- AHP
acute hepatic porphyria
- CI
confidence interval
- GI
gastrointestinal
- IBS
irritable bowel syndrome
- NIH
National Institutes of Health
- OR
odds ratio
- PROMIS
Patient-Reported Outcomes Measurement Information System
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES: Dr. Almario has served as a consultant for Alnylam Pharmaceuticals. Dr. Spiegel has served on advisory boards for and received grant support to his institution from Alnylam Pharmaceuticals. Drs. Lakhoo and Khalil have no relevant disclosures.
REFERENCES
- 1.Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: Update 2018. Gastroenterology 2019;156:254–272.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ford AC, Marwaha A, Sood R, et al. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut 2015;64:1049–1057. [DOI] [PubMed] [Google Scholar]
- 3.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:712–721.e4. [DOI] [PubMed] [Google Scholar]
- 4.Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clin Gastroenterol Hepatol 2005;3:543–52. [DOI] [PubMed] [Google Scholar]
- 5.Sandler RS, Stewart WF, Liberman JN, et al. Abdominal pain, bloating, and diarrhea in the United States: prevalence and impact. Dig Dis Sci 2000;45:1166–71. [DOI] [PubMed] [Google Scholar]
- 6.Palsson OS, Whitehead WE, Van Tilburg MA, et al. Development and validation of the Rome IV diagnostic questionnaire for adults. Gastroenterology 2016;150:1481–1491. [Google Scholar]
- 7.Menees SB, Almario CV, Spiegel BMR, et al. Prevalence of and factors associated with fecal incontinence: results from a population-based survey. Gastroenterology 2018;154:1672–1681.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Almario CV, Ballal ML, Chey WD, et al. Burden of gastrointestinal symptoms in the United States: results of a nationally representative survey of over 71,000 Americans. Am J Gastroenterol 2018;113:1701–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegel BM, Hays RD, Bolus R, et al. Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) gastrointestinal symptom scales. Am J Gastroenterol 2014;109:1804–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferraro LA, Price JH, Desmond SM, et al. Development of a diabetes locus of control scale. Psychol Rep 1987;61:763–70. [DOI] [PubMed] [Google Scholar]
- 11.Hays RD, Bjorner JB, Revicki DA, et al. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res 2009;18:873–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson KE, Bloomer JR, Bonkovsky HL, et al. Recommendations for the diagnosis and treatment of the acute porphyrias. Ann Intern Med 2005;142:439–450. [DOI] [PubMed] [Google Scholar]
- 13.Bissell DM, Wang B. Acute hepatic porphyria. J Clin Transl Hepatol 2015;3:17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
- 15.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med 2003;18:146–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lackner JM, Gudleski GD, Keefer L, et al. Rapid response to cognitive behavior therapy predicts treatment outcome in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2010;8:426–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spiegel BM, Khanna D, Bolus R, et al. Understanding gastrointestinal distress: a framework for clinical practice. Am J Gastroenterol 2011;106:380–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Early DS, Ben-Menachem T, Decker GA, et al. Appropriate use of GI endoscopy. Gastrointest Endosc 2012;75:1127–31. [DOI] [PubMed] [Google Scholar]
- 19.Kueh SH, Zhou L, Walmsley RS. The diagnostic yield of colonoscopy in patients with isolated abdominal pain. N Z Med J 2013;126:36–44. [PubMed] [Google Scholar]
- 20.Morini S, Hassan C, Meucci G, et al. Diagnostic yield of open access colonoscopy according to appropriateness. Gastrointest Endosc 2001;54:175–9. [DOI] [PubMed] [Google Scholar]
- 21.Moayyedi PM, Lacy BE, Andrews CN, et al. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol 2017;112:988–1013. [DOI] [PubMed] [Google Scholar]
- 22.Vakil N, Moayyedi P, Fennerty MB, et al. Limited value of alarm features in the diagnosis of upper gastrointestinal malignancy: systematic review and meta-analysis. Gastroenterology 2006;131:390–401; quiz 659–60. [DOI] [PubMed] [Google Scholar]
- 23.Bonkovsky HL, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyrias consortium. Am J Med 2014;127:1233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sardh E, Harper P, Balwani M, et al. Phase 1 trial of an RNA interference therapy for acute intermittent porphyria. N Engl J Med 2019;380:549–558. [DOI] [PubMed] [Google Scholar]
- 25.Pew Research Center. Internet/broadband fact sheet. 2020. [cited 2020 March 3]; Available from: http://www.pewinternet.org/fact-sheet/internet-broadband/.
- 26.Ritter PL, Stewart AL, Kaymaz H, et al. Self-reports of health care utilization compared to provider records. J Clin Epidemiol 2001;54:136–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.