Abstract
Objectives
The purpose of the study is to assess the effectiveness of fracture liaison service (FLS) after 5-year implementation to close the secondary fracture care gap, ensuring that patients receive osteoporosis assessment, intervention, and treatment, therefore, reducing the fracture risk at Police General Hospital (PGH).
Methods
A prospective cohort study was conducted. We studied male and female, ≥ 50 years old who presented with a fragility hip fracture and participated in PGH’s FLS from April 1, 2014–March 31, 2019 (5 years implementation). The sample size was 353 patients, with 1-year follow-up. The data were compared with a previous study, before the commencement of the FLS.
Results
After 1-year follow up, the mortality rates were 5.95% and there were only 8 patients who had secondary fractures (2.93%), which showed a decrease of 30% from before FLS implementation. Post-injury bone mineral density (BMD) rates were increased from 28.33% to 85.84%, osteoporosis treatment rates were increased from 40.8% to 89.38%, and the time to surgery and hospitalization decreased from 7.9 to 5.0 days, and 23.2 to 19.6 days, respectively, all with statistical significance (P < 0.001). However, the 1-year mortality rates were not significant when compared to the previous study.
Conclusions
Patients with fragility hip fractures participating in FLS after 5-year implementation at PGH had significantly higher post-injury BMD and osteoporosis treatment rates and significantly shorter in time to surgery and hospitalization. This showed that secondary fracture rates were lower than before the project at 1-year of follow up.
Keywords: Fracture liaison service, Osteoporosis, Fragility hip fracture, Thailand
1. Introduction
Osteoporosis is a generalized skeletal disorder of low bone mass and deterioration in its architecture, causing susceptibility to fragility fracture, especially in postmenopausal women and elderly men [1]. Currently, the prevalence of osteoporosis is still increasing exponentially both nationally in Thailand and globally. Untreated osteoporosis leads to a higher risk of having a subsequent fragility fracture, termed the “fracture cascade” [2,3]. To ensure that the “osteoporosis treatment gap” is addressed, a robust proactive system needs to be applied to the healthcare system of osteoporotic patients, and the fracture liaison service (FLS) has been proposed as the most effective model of care [[4], [5], [6]].
At Police General Hospital (PGH) in Thailand, although there are clinical practice guidelines (CPG) for osteoporosis treatment according to the Thailand Osteoporotic Foundation (TOPF) 2016 guidelines, a multidisciplinary approach has not been previously implemented. Following a study in 2015 done by Amphansap et al it was seen that the first year mortality rates in fragility fracture patients were 9.2%, the incidence of the second fracture at 1-year was 30%, the rates of bone mineral density (BMD) testing were only 28.33% and medical treatment initiation for calcium and vitamin D supplements, non-bisphosphonate and bisphosphonate drugs were 12.5%, 3.33%, and 6.67%, respectively, and decreased to 0.83%, 1.67%, and 0.83%, respectively, when the patients were followed up 1 year later [7]. This reflects the ineffectiveness of the previously used guidelines in managing patients with fragility fractures.
The purpose of this study is to assess the effectiveness of FLS after implementation for the last 5 years in Police General Hospital, which is a program that aims to prevent secondary fracture, reduce 1-year mortality rates, and increase the number of patients receiving BMD testing and initiating anti-osteoporotic treatment.
2. Methods
2.1. Program description
Police General Hospital is currently one of the major tertiary trauma centers in Bangkok, Thailand. A 900-bed hospital serves a population of approximately 320,000 people. The Police General Hospital’s Fracture Liaison Service (PGH’s FLS) has been implemented since 2014 as a physician-led intervention and interdisciplinary support program that identifies, investigates, and treats fragility fracture patients. All patients that were included were scheduled for full workup at the FLS clinic, at which investigations for osteoporosis and secondary causes of osteoporosis were done, lifestyle and dietary education was provided, and treated for osteoporosis when appropriate. The PGH’s FLS was awarded the Gold Level standard of the Capture the Fracture programmed by International Osteoporosis Foundation in 2016.
2.2. Ethical considerations
This study was approved by the Ethics review committee for Human research in Police General Hospital. (COA No.14/2018).
2.3. Data collection
A prospective single-center cohort study was conducted in all male and female patients aged 50 years or older who were admitted at Police General Hospital with low-energy fragility fractures of the hip from April 1, 2014 to March 30, 2019. After informing the patients about the FLS, all of them participated in PGH’s FLS. Exclusion criteria included patients who had fractures due to high-energy trauma, bone tumors, and atypical femoral fractures.
Demographic data were collected from a standardized questionnaire containing gender, age, underlying disease, previous fragility fracture, type of fracture, history of previous BMD evaluation, pre-injury ambulatory status, pre-injury number of falling, 25(OH) vitamin D levels, and type of osteoporosis.
The primary outcomes that were evaluated included secondary fragility fracture rates, and the mortality rates at 1-year follow-up after 5 years of PGH’s FLS implementation. Secondary outcomes were as follows: type of treatment, time to surgery, length of hospital stay, the number of patients who had follow up BMD testing, the number of patients were treated for osteoporosis by medications at 1 year, post-injury ambulatory status at 1 year, post-injury number of falls at 1 year, the cause of loss of follow up, and the cause of death. The data from this study were compared to a previous study done by Amphansap et al [7].
2.4. Statistical analysis
All statistical analysis was performed using STATA version 15 and statistical significance was set at a P-value of < 0.05 with a 95% confidence interval. Continuous data were presented as a maximum, minimum, mean, and standard deviation. Categorical data were presented as frequency and percentage.
3. Results
There were 353 osteoporotic hip fracture patients who participated in PGH’s FLS within the duration of 5 years. After 1 year, 62 patients (17.56%) were excluded from the study due to loss of follow-up.
3.1. Demographic data
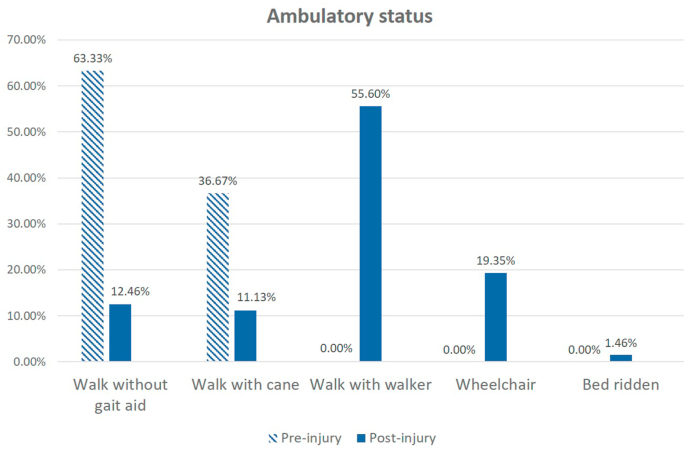
The patients’ demographic data are summarized in Table 1. There were 260 females (73.65%) and 93 males (26.35%) with an average age of 78.9 years and a maximum and minimum age of 97 and 50 years, respectively. The most common chronic underlying illness was hypertension (248 patients, 70.25%). The types of fractures found in this study included femoral neck fractures (167 patients, 47.31%), intertrochanteric fractures (176 patients, 49.86%), and subtrochanteric fractures (4 patients, 1.13%). There were 37 patients (10.48%) with a history of fragility fracture and 28 patients (7.93%) who had a previous BMD measurement. All the parameters were compared with the data from the historical control done by Amphansap et al [7] and found no statistically significant differences between each parameter in the demographic data (P > 0.05), except dyslipidemia and diabetes mellitus. Regarding the pre-injury ambulatory status (Fig. 1), most patients could walk without gait aid (64%) and the remaining patients relied on assistive walking devices (36%). We evaluated the pre-injury number of falls within 1 year which was found to be an average 1.52-fold with a minimum number of 1 time and a maximum number of 5-fold. More than half of the patients had vitamin D deficiency (< 20 ng/ml) (183 patients, 57.37%), 93 patients were identified as having vitamin D insufficiency (20–29 ng/ml) (29.15%), and the remaining had normal vitamin D levels (≥ 30 ng/ml) (43 patients, 13.48%). Most of the patients (327 patients, 92.63%) were diagnosed with primary osteoporosis.
Table 1.
Comparison of demographic data before and after Police General Hospital’s Fracture Liaison Service implementation.
| Variable | Before project [7] (n = 120) | After project (n = 353) | P-value |
|---|---|---|---|
| Sex | 0.945 | ||
| Male | 32 (26.7%) | 93 (26.35%) | |
| Female |
88 (73.3%) |
260 (73.65%) |
|
| Age, year | 0.665 | ||
| ≤ 80 | 68 (56.6%) | 192 (54.40%) | |
| > 80 | 52 (43.3%) | 161 (45.60%) | |
| Underlying disease | |||
| Hypertension | 84 (70%) | 248 (70.25%) | 0.958 |
| Dyslipidemia | 33 (27.5%) | 132 (37.39%) | 0.049∗ |
| Diabetes mellitus | 21 (17.5%) | 124 (35.13%) | < 0.001∗ |
| Type of fracture | |||
| Femoral neck | 55 (45.8%) | 167 (47.31%) | 0.78 |
| Intertrochanteric | 63 (52.5%) | 176 (49.86%) | 0.617 |
| Subtrochanteric | 2 (1.7%) | 4 (1.13%) | 0.646 |
| Other (isolated greater or lesser trochanter) |
0 (0.0%) |
6 (1.70%) |
0.345 |
| Previous fractures |
12 (10%) |
37 (10.48%) |
0.881 |
| Pre-injury BMD evaluation rates |
8 (6.7%) |
28 (7.93%) |
0.652 |
| Pre-injury falls within 1 year (time) |
No data |
1.52 (Min 1, Max 5) |
NA |
| 25(OH) vitamin D level | No data | NA | |
| < 20 ng/ml | 183 (57.37%) | ||
| ≥ 20 to < 30 ng/ml | 93 (29.15%) | ||
| ≥ 30 ng/ml |
43 (13.48%) |
||
| Type of osteoporosis | No data | NA | |
| Primary osteoporosis | 327 (92.63%) | ||
| Secondary osteoporosis | 26 (7.37%) | ||
| CKD-MBD | 20 (5.67%) | ||
| Primary hyperparathyroidism | 3 (0.85%) | ||
| Multiple myeloma (no direct involvement) | 3 (0.85%) | ||
Values are presented as number (%).
NA, not assessed; Min, minimum; Max, maximum, ∗statistically significant.
Fig. 1.
Comparison of ambulatory status at pre-injury versus 1-year follow up post-injury.
3.2. Primary and secondary outcomes
As shown in Table 2, Table 3, the majority of patients (320 patients, 90.65%) had undergone operative treatment based on their fracture types and configuration, which included arthroplasty (147 patients, 41.64%) and fixation (173 patients, 49.01%). Among the fixation cases, there were 142 cephalomedullary nail fixations (40.23%), 27 plate fixations (7.65%), and 4 multiple screw fixations (1.13%). For the arthroplasty cases, there were 138 hemiarthroplasty operations (39.09%), and 9 total hip replacements (2.55%). In contrast, the remaining 33 patients (9.35%) were treated non-operatively due to severe status of their underlying medical condition. For patients who had undergone surgical treatment, the average time to surgery was 5.2 ± 2.8 days (5.4 ± 3.5 days in the arthroplasty group and 5.0 ± 1.5 days in the fixation group). The length of hospitalization was classified into surgical patients at 19.6 ± 8.4 days and non-surgical patients at 24.1 ± 6.8 days. The BMD monitoring at follow up was done in 303 patients (85.84%), and the results showed 142 (47%) patients with osteoporosis, 118 (39%) with osteopenia, and 43 (14%) patients with normal BMD. There was a 100% rate of evaluation for secondary osteoporosis and fall risks. There were 4 (1.13%), deceased patients within 30 days of injury, 11 deceased patients within 90 days (3.12%), 17 patients deceased within 6 months (4.82%), and 21 (5.95%) patients who deceased within 1 year after the injury, respectively. Listed causes of death were pneumonia (33.3%), septicemia (19.05%), and infected pressure sores, acute myocardial infarction, and gastrointestinal hemorrhage (9.52% of each).
Table 2.
Comparison of outcomes before and after Police General Hospital’s Fracture Liaison Service implementation.
| Variable | Before project [7] (n = 120) | After project (n = 353) | P-value |
|---|---|---|---|
| Type of treatment | 0.015∗ | ||
| Conservative | 21 (17.5%) | 33 (9.35%) | |
| Surgery | 99 (82.5%) | 320 (90.65%) | |
| Arthroplasty | |||
| Hemiarthroplasty | 39 (32.5%) | 138 (39.09%) | |
| Total hip arthroplasty | 4 (3.3%) | 9 (2.55%) | |
| Fixation | |||
| Cephalomedullary nail | 41 (34.2%) | 142 (40.23%) | |
| Plate | 12 (10.0%) | 27 (7.65%) | |
| Multiple screws |
3 (2.5%) |
4 (1.13%) |
|
| Time to surgery, day | No data | 5.2 ± 2.8 | NA |
| Arthroplasty | 7.9 | 5.4 ± 3.5 | < 0.001∗ |
| Fixation |
7.9 |
5.0 ± 1.5 |
< 0.001∗ |
| Hospitalization, day | No data | 21.2 ± 5.6 | NA |
| Surgery | 23.2 | 19.6 ± 8.4 | <0.001∗ |
| Conservative |
25.9 |
24.1 ± 6.8 |
0.002∗ |
| Post-injury BMD evaluation rates |
34 (28.3%) |
303 (85.84%) |
< 0.001∗ |
| 2nd osteoporosis and fall risks assessment | No data | 353 (100.0%) | NA |
| Cumulative death | |||
| 30-day mortality | No data | 4 (1.13%) | |
| 90-day mortality | No data | 11 (3.12%) | |
| 180-day mortality | No data | 17 (4.82%) | |
| 1-year mortality |
11 (9.2%) |
21 (5.95%) |
0.225 |
| Cause of death | No data | NA | |
| Pneumonia | 7 (33.33%) | ||
| Septicemia | 4 (19.05%) | ||
| Infected pressure sore | 2 (9.52%) | ||
| Acute myocardial infarction | 2 (9.52%) | ||
| Gastrointestinal hemorrhage | 2 (9.52%) | ||
| Multiple myeloma | 1 (4.77%) | ||
| Other (Unidentified cause) | 3 (14.29%) | ||
Values are presented as mean ± standard deviation or number (%).
NA, not assessed; Min, minimum; Max, maximum.
∗statistically significant.
Table 3.
Outcomes at 1-year follow up.
| Variable | Before project at 1 year [7] (n = 120) | After project at 1 year (n = 273) | P-value |
|---|---|---|---|
| Secondary fractures | 36 (30.0%) | 8 (2.93%) | < 0.001∗ |
| Post-injury osteoporotic medications | |||
| No | 71 (59.2%) | 29 (10.62%) | < 0.001∗ |
| Yes | 49 (40.8%) | 244 (89.38%) | |
| Calcium or vitamin D | 0 (0.0%) | 26 (9.53%) | |
| Calcium and vitamin D | 25 (20.8%) | 225 (82.42%) | |
| Bisphosphonate | 18 (15.0%) | 15 (5.49%) | |
| Denosumab | 0 (0.0%) | 78 (28.57%) | |
| Teriparatide | 6 (5.0%) | 29 (10.63%) | |
| Others (Vit K2, Calcitonin) |
0 (0.0%) |
7 (2.57%) |
|
| Post-injury falls, time | NA | 0.1 (Min 0, Max 1) | NA |
Values are presented as number (%).
NA, not assessed; Vit, vitamin; ∗statistically significant.
Only 8 patients (2.93%) had secondary fragility fractures within 1 year of follow-up. There were 244 patients (89.38%) who received osteoporotic medications. No incidence of osteonecrosis of the jaw or atypical femoral fracture was reported. After the post-injury falls at 1-year post-injury follow-up were evaluated, only an average of 0.1 falls were recorded (minimum 0 vs maximum 1). For ambulatory status at 1-year post-injury, most patients ambulated with gait aid assistance (235 patients, 86.08%) with the rest of the patients walking without gait aid (34 patients, 12.46%), with only 4 patients bedridden (1.46%)(Fig. 1) We classified causes of loss of follow-up for this study for the 62 patients (17.57%) by medical problems in 28 patients (45%), by patients’ inconvenience in 27 patients (44%), and 7 patients were unable to be contacted (11%).
There was a statistically significant decrease in secondary fracture rates from 30% to 2.93% (P < 0.001), a statistically significant increase in the rates of post-injury BMD evaluation from 28.3% to 85.84% (P < 0.001), a statistically significant increase in post-injury osteoporotic medications rates from 40.8% to 89.38% (P < 0.001) and a statistically significant decrease in time to surgery and hospitalization (P < 0.001). However, the first year mortality rates change were not statistically significant (P = 0.225).
4. Discussion
According to a study done by Jennings LA et al prior to the FLS project implementation, out of 51 346 patients who were hospitalized for osteoporotic hip fractures, only 7% received an anti-osteoporotic medication. The highest morbidity and mortality rates were seen in the first year following the fracture [8]. From the study done by Amphansap et al regarding hip fracture patients in Police General Hospital, Thailand, it was found that first-year mortality rates, secondary fracture rates, and post-injury BMD intervention rates were 9.2%, 30%, and 28.3%, respectively. The data also showed that osteoporotic treatment rates at 1-year post-fracture with calcium and vitamin D, non-bisphosphonate drugs, and bisphosphonate drugs were 20.8%, 15%, and 5%, respectively. The 1-year follow-up rates were less than 2% [7]. This issue of missed diagnosis and under-treatment of osteoporotic fractures is a problem both nationally and worldwide.
FLS is likely to improve multidisciplinary care by allowing better communication between healthcare professionals through a systematic coordination. This is done by assessment and evaluation of laboratory investigations to rule out secondary osteoporosis and to keep as a baseline for further treatment. FLS is associated with improved outcomes in terms of reducing future fractures as well as morbidity and mortality, which is a result of the improved investigation, detection, and treatment of osteoporosis. It has also been shown to improve the care of osteoporotic fractures. Many studies have shown that the diagnosis, BMD testing, and treatment initiation of osteoporosis occur more frequently in patients who underwent acute low-intensity trauma fractures followed by FLS implementation as compared to before the project was implemented [4,9,10].
PGH’s FLS has been operating since 2014, in which the team had collected data from hip fracture patients and followed up for 1 year. After implementing the FLS, it was found that there was approximately 58% increase in BMD evaluation, up to 49% increase in osteoporotic medications at 1 year, and 27% decrease in secondary fractures, with all of this data being statistically significant. From the data of Walter et al the FLS model was associated with a reduction in re-fractures risk (HR 0.18–0.67 over 2–4 years) [11], and from the study done by de Bruin IJA et al FLS can reduce subsequent non-vertebral fractures in the first year after primary fracture (HR 0.84) [12]. This was consistent with the study done by Aubry-Rozier et al that showed the re-fracture rate in the FLS group as 3% [13]. Reduction of secondary fracture in this study may be a result of a reduction in falls by an average 1.52-fold in 1-year pre-injury (maximum 5, minimum 1) to 0.1-fold in 1-year post-injury (maximum 1, minimum 0). According to the Cochrane review for fall prevention, several combination exercises led to an approximately 30% reduction, and home environment adjustment achieved about a 20% reduction in the incidence of falls [14].
The first-year mortality rates in this study decreased from 9.2% to 5.95%, which were lower than a study performed by Phadunkiet et al which showed the first-year mortality rates of osteoporotic hip fractures in Chiang Mai, Thailand, to be approximately 18–20% [15]. In our study, the majority of the deceased patients (17/21, 80.95%) passed away within 180 days after the index injury, 85.72% of which were caused by complications related to conservative treatment. The finding was similar to the data seen in a study by Ha Yc et al who had a rate of mortality due to hip fracture at the 180-day mark as 10.8% [16].
Even though medications or supplements were prescribed in 89.38% of patients at 1 year, only 47.27% of patients received pharmacologic anti-osteoporotic treatment. This discrepancy can be partially explained by the cost of treatment not covered by health care systems or insurance. In Thailand, there are 3 universal health care systems that will affect the availability of the intervention and treatment the patients can get. The Civilian Welfare system will receive full coverage for their BMD intervention and anti-osteoporotic medications, whereas the Social Security for private employees and Universal Coverage Scheme for all other Thai nationals will only be able to receive calcium and vitamin D supplements. The data from the International Osteoporosis Foundation (IOF) in 2013 showed that reimbursement varied greatly across the region in Asia-pacific, ranging from 0 to 100% reimbursement for the most commonly prescribed medications. There were also differences between public and private insurance, with only partial reimbursement being offered, or restrictive criteria applied, such as age or history of fracture. Furthermore, BMD testing is not fully reimbursed in many countries, which serves as another barrier to access osteoporotic intervention and treatment [17].
Standardized BMD evaluation following the WHO criteria by dual X-ray absorptiometry (DXA) was used. The patients were diagnosed with osteoporosis when the T-score is ≤ −2.5. This study showed about 53% of fragility hip fracture patients had normal BMD or osteopenia, similar to the data from Switzerland that showed 49.7% of osteoporotic hip fracture patients being in the normal and osteopenia group [13]. Although elderly patients had non-osteoporotic BMD according to the WHO criteria, nearly half of the patients who had fragility hip fractures due to osteoporotic fracture did not depend on only BMD but also clinical risk factors [18].
In this study, we found that 86.52% of patients had vitamin D inadequacy (< 30 ng/ml). The finding was consistent with a study done by Phusunti et al in a Thai population in which 78.4% of fragility hip fracture patients had vitamin D inadequacy [19]. Similarly, a study in Singapore found 92% of osteoporotic hip fracture patients with vitamin D inadequacy [20]. The possible explanations for this large proportion of patients are the sedentary lifestyles in elderly people with the majority of activities being in-door, and poor nutritional intake of calcium and vitamin D. Another study showed reduced physical performance such as the speed of gait, speed of rising from a chair, and balance adjustments that were noted in patients with vitamin D levels of less than 20 ng/ml [21]. Patients with mean serum 25(OH)D ≥ 33 ng/ml had a substantially greater likelihood of maintenance of bisphosphonate response [22]. From this reasoning, patients who are at risk of hip fractures should receive vitamin D supplements and keep their serum 25(OH)D at normal levels.
Although the advancement in orthopedic interventions has led to a great improvement in the outcomes of hip fracture, the recovery remains slower than expected and rehabilitation can be a lengthy process [23,24]. From Fig. 1, it is seen that the pre-injury ambulatory status of this group of patients was ambulatory without assistance in 64%, and with gait aid in 36%. When compared to post-injury ambulatory status at 1-year follow up, it can be seen that only 12.46% were able to ambulate without assistance and more than half required a walker for ambulation, with up to 20% of patients requiring a wheelchair. These results are similar to those of Osnes et al who found that loss of function and independence among survivors was profound, with 40% unable to walk independently and 60% requiring assistance a year later [25]. Because of these losses, 33% were totally dependent or in a nursing home in the year following a hip fracture [26]. Some patients may need life-long gait aid for ambulatory support, and fewer than half of people who survive a hip fracture will walk unaided again [27]. Therefore, primary prevention of falls before having a hip fracture is much more important than the treatment planning after a hip fracture.
A loss to follow-up has been a major challenge in patients with fragility fractures. A large number of these patients are elderly who rely on their relatives for a hospital visit and long-term continuity of care. Both patients and their relatives need to understand the importance of follow-up and anti-osteoporotic medications. After the implementation of PGH’s FLS, the rate of loss to follow-up at 1 year markedly decreased from 98% to 17.56%. The result confirmed that the FLS raised the acknowledgment for the need for long-term osteoporosis management to achieve treatment goals. The reason for the patients who had a loss of follow-up was 89% from awareness of patient’s conditions, and 44% was from the patients’ inconvenience such as the patients not being able to come or from their relatives not bringing them for follow up. Another 45% was from medical problems such as multiple underlying illnesses, on many medications, and scared of drug interactions or side effects from osteoporotic medications. Analysis of previous data showed that over 50% of patients defaulted follow-up due to poor understanding of their medical conditions; they refused to receive treatment as they did not understand why it is needed. Besides, 10% of patients reported having gastrointestinal side effects arising from oral medication, and approximately 8% reported having to take several drugs for other underlying illnesses [28].
There are strengths seen in this study. This prospective cohort study is the first of its kind in Thailand, with the FLS project being implemented for 5 years in Thailand. This study also had a 100% rate of evaluation of fall risks and ruling out secondary osteoporosis in all patients participating in the project. This study also has some limitations. The population in the study was comprised of Thai nationals only. Due to this, the findings may not be generalizable to other racial or ethnic groups. The authors compared the current data with a previous study (historical comparison) that collected data regarding fragility hip fractures of patients occurring before the implementation of the FLS in Police General Hospital.
5. Conclusions
Patients with fragility hip fractures participating in the FLS after a 5-year implementation at Police General Hospital had significantly higher post-injury BMD and osteoporosis medical treatment rates and significantly shorter time to surgery and hospitalization. This showed secondary fracture rates that were lower than before the project at 1-year of follow up. Multifaceted and intensive FLS has improved and closed the osteoporosis hip fracture care gaps in Police General Hospital.
CRediT author statement
Tanawat Amphansap: Conceptualization, Methodology, Formal analysis, Writing-original draft, Writing-review & editing, Project administration. Nitirat Stitkitti: Data curation, Validation, Visualization. Alisara Arirachakaran: Writing-review & editing.
Conflicts of interest
The authors decalre no competing interests.
Acknowledgments
The authors would like to thank Dr. Lertkong Nitiwarangkul for biostatistics assistance and Atiporn Therdyothin for language editing assistance. ORCID Tanawat Amphansap: 0000-0003-2148-3921. Nitirat Stitkitti: 0000-0003-2438-4670. Alisara Arirachakaran: 0000-0002-9174-873X.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.World Health Organization Study Group Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Seer. 1994;843:1–129. [PubMed] [Google Scholar]
- 2.Lindsay R, Pack S, Li Z. Longitudinal progression of fracture prevalence through a population of postmenopausal women with osteoporosis. Osteoporos Int. 2005;16:306–312. doi: 10.1007/s00198-004-1691-5. [DOI] [PubMed] [Google Scholar]
- 3.Melton L.J, 3rd, Amin S. Is there a specific fracture ‘cascade’? BoneKEy Rep. 2013;2:367. doi: 10.1038/bonekey.2013.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akesson K, Marsh D, Mitchell P.J, McLellan A.R, Stenmark J, Pierroz D.D. Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24:2135–2152. doi: 10.1007/s00198-013-2348-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eisman J.A, Bogoch E.R, Dell R, Harrington J.T, McKinney R.E, Jr., McLellan A. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. 2012;27:2039–2046. doi: 10.1002/jbmr.1698. [DOI] [PubMed] [Google Scholar]
- 6.Marsh D, Akesson K, Beaton D.E, Bogoch E.R, Boonen S, Brandi M.L. Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int. 2011;22:2051–2065. doi: 10.1007/s00198-011-1642-x. [DOI] [PubMed] [Google Scholar]
- 7.Amphansap T, Nitiwarangkul L. One-year mortality rate after osteoporotic hip fractures and associated risk factors in Police General Hospital. Osteoporos Sarcopenia. 2015;1:75–79. [Google Scholar]
- 8.Jennings L.A, Auerbach A.D, Maselli J, Pekow P.S, Lindenauer P.K, Lee S.J. Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc. 2010;58:650–657. doi: 10.1111/j.1532-5415.2010.02769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller A.N, Lake A.F, Emory C.L. Establishing a fracture liaison service: an orthopaedic approach. J Bone Joint Surg Am. 2015;97:675–681. doi: 10.2106/JBJS.N.00957. [DOI] [PubMed] [Google Scholar]
- 10.Wu C.H, Tu S.T, Chang Y.F, Chan D.C, Chien J.T, Lin C.H. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone. 2018;111:92–100. doi: 10.1016/j.bone.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Walters S, Khan T, Ong T, Sahota O. Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging. 2017;12:117–127. doi: 10.2147/CIA.S85551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Bruin I.J.A, Wyers C.E, van den Bergh Jpw, Geusens P. Fracture liaison services: do they reduce fracture rates? Ther Adv Musculoskelet Dis. 2017;9:157–164. doi: 10.1177/1759720X17706464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aubry-Rozier B, Stoll D, Gonzalez Rodriguez E, Hans D, Prudent V, Seuret A. Impact of a fracture liaison service on patient management after an osteoporotic fracture: the CHUV FLS. Swiss Med Wkly. 2018;148:w14579. doi: 10.4414/smw.2018.14579. [DOI] [PubMed] [Google Scholar]
- 14.Gillespie L.D, Robertson M.C, Gillespie W.J, Sherrington C, Gates S, Clemson L.M. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phadungkiat S, Chariyalertsak S, Rajatanavin R, Chiengthong K, Suriyawongpaisal P, Woratanarat P. Incidence of hip fracture in Chiang Mai. J Med Assoc Thai. 2002;85:565–571. [PubMed] [Google Scholar]
- 16.Ha Y.C, Park Y.G, Nam K.W, Kim S.R. Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Kor Med Sci. 2015;30:483–488. doi: 10.3346/jkms.2015.30.4.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International Osteoporosis Foundation . 2016. Gaps and solutions in bone health: a global framework for improvement; pp. pp24–pp25. [Google Scholar]
- 18.Eriksen E.F. Treatment of osteopenia. Rev Endocr Metab Disord. 2012;13:209–223. doi: 10.1007/s11154-011-9187-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phusunti S, Suthutvoravut W, Unnanuntana A, Chotiyarnwong P. The prevalence of hypovitaminosis D in patient with fragility hip fracture at a single institution in Thailand. J Med Assoc Thai. 2016;99:1233–1238. [PubMed] [Google Scholar]
- 20.Ramason R, Selvaganapathi N, Ismail N.H, Wong W.C, Rajamoney G.N, Chong M.S. Prevalence of vitamin D deficiency in patients with hip fracture seen in an orthogeriatric service in sunny Singapore. Geriatr Orthop Surg Rehabil. 2014;5:82–86. doi: 10.1177/2151458514528952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wicherts I.S, van Schoor N.M, Boeke A.J, Visser M, Deeg D.J, Smit J. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007;92:2058–2065. doi: 10.1210/jc.2006-1525. [DOI] [PubMed] [Google Scholar]
- 22.Carmel A.S, Shieh A, Bang H, Bockman R.S. The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥ ng/ml. Osteoporos Int. 2012;23:2479–2487. doi: 10.1007/s00198-011-1868-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vatansever A, Ozic U, Okcu G. Assessment of quality of life of patients after hemiarthroplasty for proximal femoral fractures. Acta Orthop Traumatol Turcica. 2005;39:237–242. [PubMed] [Google Scholar]
- 24.Takeda H, Kamogawa J, Sakayama K, Kamada K, Tanaka S, Yamamoto H. Evaluation of clinical prognosis and activities of daily living using functional independence measure in patients with hip fractures. J Orthop Sci. 2006;11:584–591. doi: 10.1007/s00776-006-1073-2. [DOI] [PubMed] [Google Scholar]
- 25.Magaziner J, Simonsick E.M, Kashner T.M, Hebel J.R, Kenzora J.E. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45:M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 26.Leibson C.L, Tosteson A.N, Gabriel S.E, Ransom J.E, Melton L.J. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644–1650. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 27.Osnes E.K, Lofthus C.M, Meyer H.E, Falch J.A, Nordsletten L, Cappelen I. Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int. 2004;15:567–574. doi: 10.1007/s00198-003-1583-0. [DOI] [PubMed] [Google Scholar]
- 28.Naranjo A, Ojeda-Bruno S, Bilbao-Cantarero A, Quevedo-Abeledo J.C, Diaz-Gonzalez B.V, Rodriguez-Lozano C. Two-year adherence to treatment and associated factors in a fracture liaison service in Spain. Osteoporos Int. 2015;26:2579–2585. doi: 10.1007/s00198-015-3185-z. [DOI] [PubMed] [Google Scholar]