Abstract
Introduction:
Patients with hip fractures can become cold during the perioperative period despite measures applied to maintain warmth. Poor temperature control is linked with increasing complications and poorer functional outcomes. There is generic evidence for the benefits of maintaining normothermia, however this is sparse where specifically concerning hip fracture. We provide the first comprehensive review in this population.
Significance:
Large studies have revealed dramatic impact on wound infection, transfusion rates, increased morbidity and mortality. With very few studies relating to hip fracture patients, this review aimed to capture an overview of available literature regarding hypothermia and its impact on outcomes.
Results:
Increased mortality, readmission rates and surgical site infections are all associated with poor temperature control. This is more profound, and more common, in older frail patients. Increasing age and lower BMI were recognized as demographic factors that increase risk of hypothermia, which was routinely identified within modern day practice despite the use of active warming.
Conclusion:
There is a gap in research related to fragility fractures and how hypothermia impacts outcomes. Inadvertent intraoperative hypothermia still occurs routinely, even when active warming and cotton blankets are applied. No studies documented temperature readings postoperatively once patients had been returned to the ward. This is a point in the timeline where patients could be hypothermic. More studies need to be performed relating to this area of surgery.
Keywords: anesthesia, fragility fractures, geriatric trauma, systems of care, trauma surgery
Introduction
Around 76,000 patients sustain a hip fracture annually and it remains the most common, serious injury that an older person can sustain. Each year hip fractures cost the United Kingdom (UK) Health Service and social care an estimated £2 billion ($2.6 billion) and take up 1.8 million hospital bed days. The UK has an increasing aging population with nearly 12 million people aged 65 or above,1 a trend mirrored globally. This trend continues inexorably and by 2030 more than one fifth of the population will be over the age of 65.2 Given the growing geriatric population, the number of hip fracture injuries is expected to rise substantially, hence the need for betterment of care.
The National Hip Fracture Database (NHFD) and performance related care through Best Practice Tariffs (BPTs) allow for quality monitoring and drives reimbursement rates based on outcomes. Variables measured include baseline demographics as well as length of stay, final discharge destination, inpatient hip fracture rates, pressure ulcer numbers, reoperation rates, crude and adjusted 30-day mortality rates. This performance monitoring encourages hip fracture programs to provide best practice in both acute care and secondary fracture avoidance. BPT result in hospitals being reimbursed more money for the care of hip fracture patients based on 7 characteristics such as time to surgery, assessment by a geriatrician within 72 hours, nutrition assessment etc. These targets allow for a more streamlined, structured process for helping hip fracture patients and also provide a time incentive for orthopedic departments.3 Since the implementation of the NHFD and BPTs, hip fracture care has continually improved. For example during the NHFDs inception year, 30-day mortality stood at 10.9%, while in the NHFD 2019 report that mortality figure had decreased to 6.1%.4
One variable which is not recorded within the NHFD is temperature monitoring. From the moment a patient experiences a hip fracture, they are exposed to a multitude of environmental challenges, which works against their innate ability to maintain normothermia. This includes long lie hip fracture patients arriving hypothermic in the Emergency Department, varying temperature control within theaters, loss of heat from washout fluids and skin preparation for surgery and the dysregulation of central temperature control via general anesthetic.5-8 Equally of importance is understanding that the temperature challenge (or inability to maintain core temperature) is phased. Early heat loss is through redistribution throughout the body from the core to the cooler periphery. The effect of the environment is a second phase following this redistribution and an equilibrium phase then occurs. Neuraxial and general anesthesia both contribute to temperature loss. The latter, sometimes perceived more “temperature protective” may actually have a similar impact due to the effect of major conduction blockade on vasomotor and shivering responses.9
Hypothermia is a small, easily measurable, auditable and changeable element that may impact patient outcomes. It affects wound infection risk, transfusion rates and increases mortality.9-12 Due to a paucity of hip fracture specific evidence in this domain, we provide an overview of applicable literature in similar populations regarding hypothermia and its impact on outcomes.
Materials and Methods
A comprehensive literature search was undertaken using the “Ovid” search system. Databases searched include MEDLINE, Embase, the Cochrane library and NICE evidence search. Search terms (“Normothermia” or “Hypothermia”) and (“Fragility Fracture” or “Hip Fracture” or “Hip Surgery” or “Fractured Neck of Femur” or “Osteoporotic Fracture”) were used to search titles, abstracts and subject headings. Further method details can be found in the supplementary information section.
After initial screening of titles and abstracts, any papers not relevant (not regarding above criteria) were excluded. Some papers were excluded for the same reason at 2 different points due to a variety of reasons, namely misleading titles and Scopus filters not removing review papers, allowing these papers to make it through the first round of exclusion. Similarly, on full text review, outcomes may not have fallen in line with the review criteria, such as research only comparing 2 warming types and not considering any type of postoperative complication.
Remaining papers were analyzed full text using set criteria:
1. Pertains to hip fracture care
2. Primary research
3. Investigates post-operative outcome, for example:
a. Mortality
b. 30-day readmission
c. Length of stay
d. Wound infection
e. Bleeding times
f. Lactate levels
Results
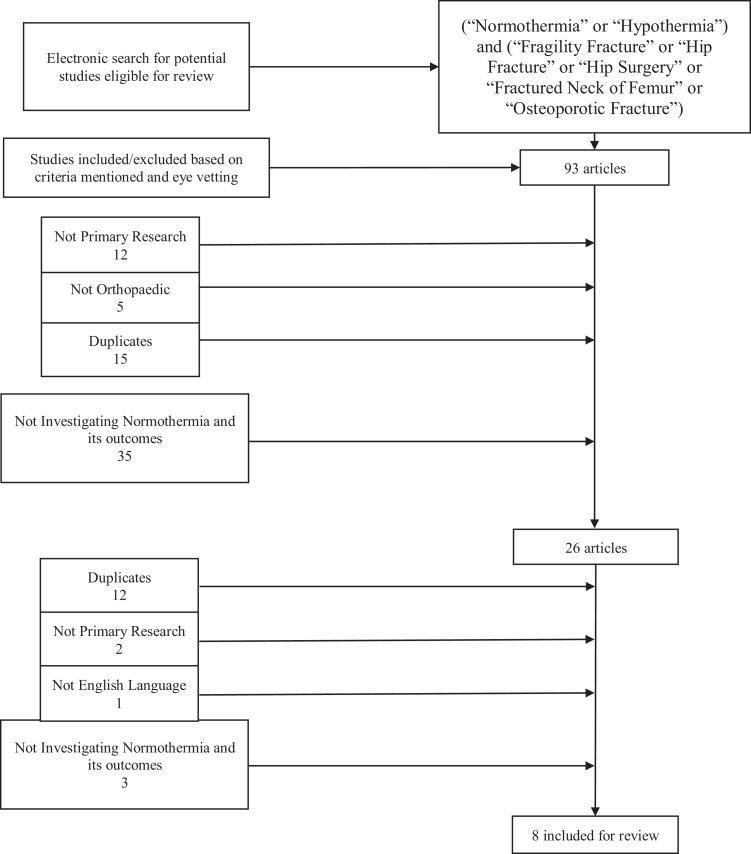
94 articles were screened for inclusion based upon titles and abstract (Figure 1). 27 papers were identified for full text review. 7 papers fulfilling the inclusion criteria are discussed along several key themes. A comprehensive table contained in the supplementary information section contains a summary of all studies discussed (Supplementary Table 1).
Figure 1.
How papers were included/excluded from the review.
Hypothermia Is Associated With Increased Serum Lactate
A large-scale multi-center retrospective cohort study by Faizi et al13 stratified 1162 patients into groups based on body temperature (>37.5°C pyrexial, 36.5-37.5°C euthermic, <36.5°C low body temperature). Temperature data was taken via tympanic thermometers which were regularly calibrated by the units’ medical physics department. The same brand of thermometer was used across all patients. There was a statistically significant higher lactate in the low temperature group (2.2 mmol/L) vs euthermic range (2.0 mmol/L). However, there was no progressive increase in serum lactate levels when the body temperature continued to drop. One limitation of the study is that they classed low body temperature as <36.5°C, although in National Institute for Health and Care Excellence (NICE) guidelines and most other references, hypothermia is classed as <36°C.14
Hypothermia May Increase Readmission and Mortality
A single-center retrospective cohort study by Williams et al 15 assessed how hypothermia impacted 929 hip fracture patients aged > 65. Outcomes included length of stay, 30-day readmission, and mortality rates. Risk factors for hypothermia were also investigated. Temperature measurements were obtained by tympanic or axillary thermometers. 10% of patients were hypothermic (<36°C), with these individuals being significantly older (87.1 yrs. ± 7.8) than the normothermic patients (84.7 yrs. ± 7.8). Hypothermic patients preoperatively were twice as likely to enter recovery <36°C than patients who were normothermic, illustrating a need for careful temperature control along the patient’s pathway at all stages, as hypothermia in preoperative periods can lead to further problems post-surgery. 30-day mortality rates in the did not reach a statistical significance between the groups. There was a statistically significant difference in 30-day re-admission with a rate of 9.8% for the hypothermic cohort vs 2.3% in normothermic patients. Log rank tests were performed to analyze the impact of length of stay and mortality, this was also not significant.
A prospective cohort study by Uzoigwe et al 16 included 781 patients, investigating mortality rates and demographic details of hip fracture patients. Tympanic thermometers that were calibrated regularly were used for temperature data, and the same model of thermometer was used across the department. 38% patients had a body temperature <36.5°C and 14% of patients had a body temperature <36°C. The full cohort showed mortality rates of 9.3% at 30 days, for those with low body temperature <36.5°C, there was a greater 30-day mortality which was statistically significant; 15.3% compared to 5.1% for those with normal body temperature. Those with a temperature <36.5°C had a 2.8-fold increase in 30-day mortality. Even when adjusted for ASA grade and time to surgery, body temperature was still a predictor of mortality.
A later follow up study17 with an additional 285 patients, found that 407/1066 (38.2%) were <36.5°C. Adjusted for the 7 most potent prognostic indicators for mortality, they found that body temperature <36.5°C increased risk of death by 2.1 times, reinforcing the need for careful and aggressive temperature control. These 2 studies are the first of their kind, investigating how low body temperature impacts outcomes.
Hypothermia Is Common During Hip Fracture Surgery, Especially in Post-Anesthesia Care Unit
A prospective cohort study by Gurunathan et al18 outlines a patient’s journey from ward—holding bay—theater—Post-anesthetic care unit (PACU). Measurements were recorded via tympanic thermometers which were calibrated and kept in the same rooms before use. Reporting only 87 patients, there was a significant decrease of temperature of 0.7°C between holding bay until PACU arrival. Furthermore, the temperature difference between the holding bay and first recorded temperature in the operating room was 0.2°C less. Ambient temperatures were consistent throughout the patient’s journey, with around 30% of patients arriving in PACU hypothermic. In this work, almost 8% of patients arrived at the operating room hypothermic despite using routine practice of normothermia maintenance—using 2 cotton blankets in the waiting room. This suggests that patients lose heat through the journey from ward to operating room, where they are subjected to the negative hypothermic impact of anesthetic agents intraoperatively.
Although a small sample size, this study is very representative of a “normal” surgical patient’s journey from ward to PACU and illustrates that current temperature management protocols can be improved. However, there were no further measurements of temperature post-operatively, leaving a gap in the timeline, as patients could potentially become hypothermic when returned to the ward.
Hypothermia May Be Associated With Increased Rates of Surgical Site Infections
A retrospective cohort study by Frisch et al19 looked at; postoperative length of stay, 30-day readmission and postoperative complications (superficial and deep SSI, non-SSI, deep vein thrombosis, pulmonary embolism, myocardial infarction and stroke). There were a total of 1525 patients warmed using the BairHugger system. Overall incidence of intraoperative hypothermia was 17%, with the patients on average being older than normothermic individuals. Lower BMI also showed a significant association with risk of hypothermia.
Univariate analysis of postoperative complications revealed no significant associations with hypothermia or complications including infection, transfusion requirement, cardiac, thromboembolic complications, length of stay or 30-day readmission. Overall infection rates were 1.2% for deep SSI, 1.5% for superficial SSI and 4.6% for non- SSI-similar to found by Kumin et al.20 However, multivariate logistic regression analysis adjusted for risk factors of infection revealed that deep SSI had a significant association with hypothermia. This conclusion may disagree with that shown in Kumin et al,20 however, Kumin et al did not perform uni/multivariate analysis. 15.8% of patients who had BairHugger warming experienced hypothermia, highlighting the rate of hypothermia despite active warming.
Drawbacks of this study are that there was only a 6 week follow up which could lead to exclusion of longer-term complications and that any patients who attended a different hospital for complications will have not been recognized. Additionally, the operating room temperature in the hospital were not standardized and the authors noted no standardized measurement of temperature—they described typically that pre and post operation temperature is measured by skin probes, and intraoperatively many factors contribute to the type of temperature measurement.
Different Methods of Patient Warming May Affect Rates of Surgical Site Infections
A randomized pilot study by Kumin et al20 compared forced air warming (FAW) using the Bair Hugger, and resistive fabric warming (RFW) on the rates of deep surgical site infections (SSIs), superficial SSIs and inadvertent perioperative hypothermia (<36°C). These measurements were followed postoperatively within 90 days of arthroplasty surgery. 6 hospitals participated in this pilot spread across the UK. 515 were randomized to FAW (n = 255) or RFW (n = 260). Deep SSI occurred in 4/223 (1.8%) of FAW patients and 3/221 (1.4%) of RFW patients. These SSIs were determined by local principal investigators and all patients who developed an infection received antibiotic prophylaxis. Superficial SSI occurred in 3.5%in the FAW cohort and 0.5% in the RFW cohort.
37 patients in total were hypothermic at the last available temperature measurement, 7.5% and 9.7% in the FAW and RFW group, respectively. Limitations of this study include not specifying the method of temperature collection and not including information on PACU temperatures. Furthermore, this is the only study in the review which investigated hip arthroplasty, which likely involved elective operations thus making it less relatable to emergency hip fracture care, additionally, the authors did not specify if arthroplasty surgery was emergency or not. This study was also funded by 3 M—the company which produces the BairHugger, this was the only paper in this review funded by the industry.
Discussion
Inadequate temperature control is an important and under emphasized variable within the care of hip fracture patients. Routine inadvertent intraoperative hypothermia occurs despite active warming routines applied perioperatively.21
The literature base from which guidance can be drawn is heterogeneous for hip fracture groups. Methodology differs markedly between studies and when similar outcomes are studied in similar populations with similar interventions, different results are reported. Some studies noted statistically significant increases in mortality and in 30-day readmission rates16,17 while others noted no difference at all. This makes it difficult to draw reliable conclusions or choose best future direction due to the contradicting, heterogeneous evidence available. One factor that remained constant across all studies was that significant numbers of patients are colder than they should be at all time points of the perioperative episode despite active warming regimens. As could be expected, increasing age and decreasing BMI are flagged as risk factors for hypothermia in this population.
There is a link between hypothermia and poor outcome—whist the studies reviewed are often contradictory of which outcome measure is most affected, they all demonstrate a negative association with periods of lower temperatures in the hip fracture population. Increasing serum lactate and its link to poor outcome,13 unplanned admission and mortality are all demonstrated to be impacted by lower body temperatures. Interestingly, the literature supports a view that there is more than one opportunity for cooling to be reversed and opportunities to correct temperature control exist at all parts of the patient episode. Patients entering operating theaters with low body temperature for example are almost twice as likely to be hypothermic when the temperature is routinely recorded in post-operative recovery units.15 Hypothermia has been suggested to contribute significantly in the rates of deep wound infection in one study19 but there were no other studies available to compare this to, other than a hip arthroplasty pilot study—which found no difference.20 Outside of hip fracture care and in general surgery, there is a significantly higher transfusion rate in hypothermic patients when compared to their normothermic cohort.21 Other negative postoperative outcomes such as wound healing and infection rates are significantly higher in hypothermic groups.10
While the literature base is heterogeneous, there is considerable evidence, and it is common clinical sense, that avoiding hypothermia will improve patient outcomes. Better practice in maintaining normothermia might be the next step to further better hip fracture care via a marginal gains approach, starting with more vigilant auctioning of temperature fluctuations and a more proactive rather than reactive structure.
As with all assessment of uncontrolled clinical studies, there are limitations of this review. These include its non-systematic nature due to the large variety in evidence, methodology and lack of applicable studies, making it difficult to pool results. There is a gap in research within this area of fragility fracture care and more studies are required to strengthen the evidence base. Multiple variables such as; age, gender, BMI, ASA grade, injury type, frailty, cognition and hip fracture specific scores need to be considered, imputed and their impact noted. Operation type, 30-day readmission, 30-day mortality, surgical site infection rate, blood transfusion rates, blood loss and lactate levels are all variables that can be measured to unify outcome assessments. Furthermore, temperature monitoring should continue to follow patients on return to the ward as there is a complete lack of research studying postoperative temperature measurements at this point. Another recommendation would be encouragement of combined active and passive warming techniques throughout the patient episode and not just isolated, reactionary measures as is common practice now. Active and passive warming systems are readily available at many points of the patient journey. We feel what is needed is a system to enable this improvement in culture around patient warming or at least maintenance of heat, proactively. Specifically, within the hip fracture timeline, transfer to and from the ward has been noted as a point where core temperature significantly drops, highlighting an area to focus on when considering the improvement of patient warming and instigation of a culture of warming. There may be considerable marginal gains by using warming spacer blankets or more substantial active warming to be continued on the ward. Hopefully through application of these simple measures, normothermia will become the accepted state for these patients and not hypothermia.
Supplemental Material
Supplemental Material, table for Too Cool? Hip Fracture Care and Maintaining Body Temperature by James Arkley, Suhib Taher, Ján Dixon, Gemma Dietz-Collin, Stacey Wales, Faye Wilson and William Eardley in Geriatric Orthopaedic Surgery & Rehabilitation
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James Arkley  https://orcid.org/0000-0002-9806-9166
https://orcid.org/0000-0002-9806-9166
Ján Dixon, MBBS  https://orcid.org/0000-0003-0445-3026
https://orcid.org/0000-0003-0445-3026
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Giannoudis P, Einhorn TA. Surgical and Medical Treatment of Osteoporosis: Principles and Practice. CRC Press; 2020. [Google Scholar]
- 2. Age UK. Later Life in the United Kingdom 2019. Published 2019. Accessed June 22, 2020 https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/later_life_uk_factsheet.pdf
- 3. NHS Improvement. 2019/20 National Tariff Payment System—A consultation notice: Annex DtD Guidance on best practice tariffs. 2019:85.
- 4. National Hip Fracture Database. Annual Report 2019 Published 2019. Accessed May 9, 2020 https://www.nhfd.co.uk/files/2019ReportFiles/NHFD_2019_Annual_Report_v101.pdf
- 5. Díaz M, Becker DE. Thermoregulation: physiological and clinical considerations during sedation and general anesthesia. Anesth Prog. 2010;57(1):25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2012;45(1):38–43. [DOI] [PubMed] [Google Scholar]
- 7. Lenhardt R. The effect of anesthesia on body temperature control. Front Biosci (Schol Ed). 2010;2:1145–1154. [DOI] [PubMed] [Google Scholar]
- 8. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109(2):318–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events: a randomized clinical trial. JAMA. 1997;277(14):1127–1134. [PubMed] [Google Scholar]
- 10. Qadan M, Gardner SA, Vitale DS, Lominadze D, Joshua IG, Polk HCJ. Hypothermia and surgery: immunologic mechanisms for current practice. Ann Surg. 2009;250(1):134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Michelson A, Macgregor H, As K, Barnard M, Rohrer M. Reversible hypothermia-induced inhibition of human platelet activation in whole blood in vitro and in vivo. Blood. 1992;78:47. [Google Scholar]
- 12. Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108(1):71–77. [DOI] [PubMed] [Google Scholar]
- 13. Murtuza F, Farrier AJ, Venkatesan M, et al. Is there an association between body temperature and serum lactate levels in hip fracture patients? Ann R Coll Surg Engl. 2015;97(7):513–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NICE. Hypothermia: prevention and management in adults having surgery. Published 2016. Accessed May 9, 2020 https://www.nice.org.uk/guidance/cg65/chapter/Recommendations [PubMed]
- 15. Williams M, Ng M, Ashworth M. What is the incidence of inadvertent hypothermia in elderly hip fracture patients and is this associated with increased readmissions and mortality? J Orthop. 2018;15(2):624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Uzoigwe CE, Khan A, Smith RP, et al. Hypothermia and low body temperature are common and associated with high mortality in hip fracture patients. Hip Int. 2014;24(3):237–242. [DOI] [PubMed] [Google Scholar]
- 17. Faizi M, Farrier AJ, Venkatesan M, et al. Is body temperature an independent predictor of mortality in hip fracture patients? Injury. 2014;45(12):1942–1945. [DOI] [PubMed] [Google Scholar]
- 18. Gurunathan U, Stonell C, Fulbrook P. Perioperative hypothermia during hip fracture surgery: an observational study. J Eval Clin Pract. 2017;23(4):762–766. [DOI] [PubMed] [Google Scholar]
- 19. Frisch NB, Pepper AM, Jildeh TR, Shaw J, Guthrie T, Silverton C. Intraoperative hypothermia during surgical fixation of hip fractures. Orthopedics. 2016;39(6):e1170–e1177. [DOI] [PubMed] [Google Scholar]
- 20. Kümin M, Deery J, Turney S, et al. Reducing Implant Infection in Orthopaedics (RIIiO): results of a pilot study comparing the influence of forced air and resistive fabric warming technologies on postoperative infections following orthopaedic implant surgery. J Hosp Infect. 2019;103(4):412–419. [DOI] [PubMed] [Google Scholar]
- 21. Sun Z, Honar H, Sessler DI, et al. Intraoperative core temperature patterns, transfusion requirement, and hospital duration in patients warmed with forced air. Anesthesiology. 2015;122(2):276–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, table for Too Cool? Hip Fracture Care and Maintaining Body Temperature by James Arkley, Suhib Taher, Ján Dixon, Gemma Dietz-Collin, Stacey Wales, Faye Wilson and William Eardley in Geriatric Orthopaedic Surgery & Rehabilitation