Abstract
This study uses National Health Service data to compare the stillbirth rate overall and regionally during the initial April-June 2020 coronavirus lockdown vs the same period in 2019.
Pregnant women have an increased risk of infectious diseases, including respiratory infections such as influenza,1 and are included on the coronavirus disease 2019 (COVID-19) UK clinically vulnerable list.2 Little is known about the risk of COVID-19 to unborn children, with data limited to a case series of 3 stillbirth deliveries in pregnant women with confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection3 and a single London hospital reporting a higher rate of stillbirth deliveries during the pandemic period compared with a prepandemic period.4 To provide more robust data, we used national and regional hospitalization data in England to assess the risk of stillbirths during the COVID-19 pandemic.
Methods
National Health Service hospital admissions in England were assessed from April 1, 2019, to June 30, 2020, using annual Hospital Episode Statistics (HES) data (April 1, 2019, to March 31, 2020) and monthly data available as Secondary Uses Service (April 1 to June 30, 2020). Data for a 5-month (December 2019 to May 2020) crossover period between the 2 data sets were used to validate the consistency of stillbirth recording (eFigure in the Supplement). Stillbirth rates in HES were also compared with Office for National Statistics (ONS) civil deaths registrations for stillbirths during 2016-2019 for validation.
Hospitalization of mothers experiencing a stillbirth (fetal deaths >24 weeks’ gestation) were identified using relevant International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes (Z37.1, Z37.3, Z37.4, Z37.7) in any of the 20 diagnosis fields, with the denominator being hospitalizations with an ICD-10 code for delivery outcome (Z37). National and regional numbers of stillbirths and proportion of deliveries with a recorded stillbirth were analyzed.
In England, the first case of COVID-19 was recorded on January 31, 2020, and lockdown was established between March 23 and June 23, 2020. For ease of calculations, we defined the lockdown period as April to June 2020 and compared stillbirth rates for the same period in 2019 using the incidence rate ratio with a Fisher exact test at a 2-sided .05 significance level (Stata version 15.0 [StataCorp]).
Public Health England has approval to process confidential patient data for health protection purposes without explicit consent under the Health Service (Control of Patient Information) Regulations 2002.
Results
Stillbirth deliveries in HES declined from 4.6 to 4.0 per 1000 deliveries during 2016-2019, which was consistent with ONS data for 2016 (4.6 in HES vs 4.4 in ONS), 2017 (4.2 in HES vs 4.2 in ONS), 2018 (4.3 in HES vs 4.1 in ONS), and 2019 (4.0 in HES vs 3.9 in ONS).
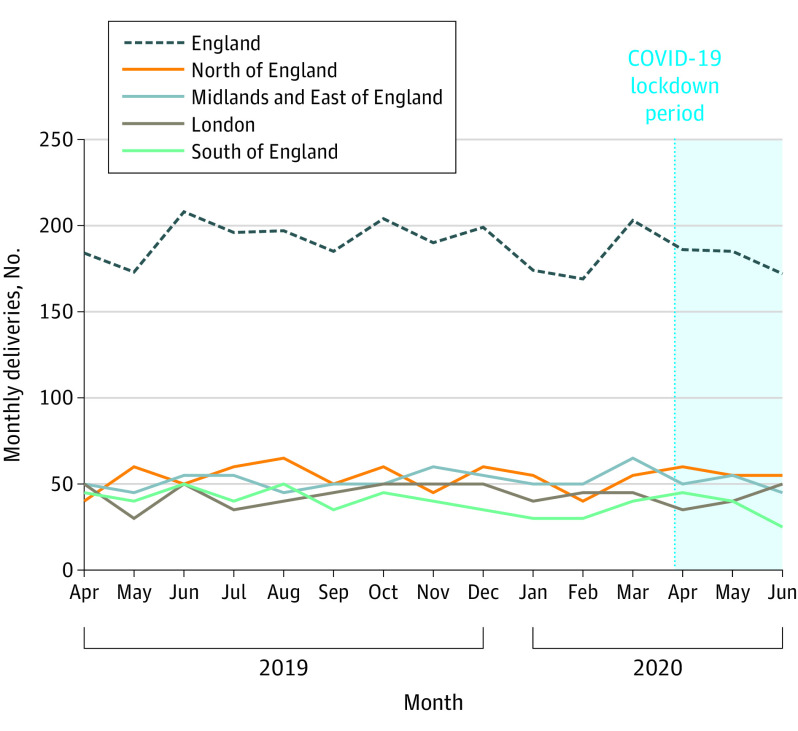
Between April 1, 2019, and June 30, 2020, there were 2825 stillbirths, with the highest proportion of stillbirth deliveries reported in London (145/26 760; 0.54% [95% CI, 0.46%-0.64%]), compared with the other 3 English regions. Nationally, the proportion of deliveries with a recorded stillbirth was similar throughout the surveillance period, and regionally the numbers fluctuated but with no evidence of any increase above baseline during the pandemic period (Figure).
Figure. Monthly Count of Deliveries With a Record of Stillbirth in England and Its Regions, April 2019 to June 2020.
Between April 1, 2020, and June 30, 2020, there were 543 stillbirths (0.41% [95% CI, 0.38%-0.45%]), compared with 565 stillbirths (0.40% [95% CI, 0.37%-0.44%]) for the same period in the previous year (incidence rate ratio, 1.02 [95% CI, 0.91-1.15]; P = .69). Within individual regions, the rate of stillbirth deliveries was not significantly different between the comparison and lockdown periods (Table).
Table. Count and Proportion of Deliveries With a Recorded Stillbirth and Rate Ratio of Periods Before Lockdown and in Lockdown Adjusted by Calendar Montha.
| Prelockdown comparison period (April 2019 to June 2019) | Lockdown period (April 2020 to June 2020) | Incidence rate ratio (95% CI) | P valueb | |||||
|---|---|---|---|---|---|---|---|---|
| No. of stillbirths | Total No. with a delivery outcome | Stillbirth rate, % (95% CI) | No. of stillbirths | Total No. with a delivery outcome | Stillbirth rate, % (95% CI) | |||
| All England | 565 | 139 745 | 0.40 (0.37-0.44) | 543 | 131 218 | 0.41 (0.38-0.45) | 1.02 (0.91-1.15) | .69 |
| North of England | 150 | 38 165 | 0.39 (0.33-0.46) | 170 | 35 400 | 0.48 (0.41-0.56) | 1.22 (0.98-1.52) | .07 |
| Midlands and East of England | 150 | 42 220 | 0.36 (0.30-0.42) | 150 | 39 295 | 0.38 (0.32-0.45) | 1.07 (0.86-1.35) | .53 |
| London | 130 | 25 960 | 0.50 (0.42-0.59) | 125 | 24 640 | 0.51 (0.42-0.60) | 1.02 (0.79-1.30) | .90 |
| South of England | 135 | 33 390 | 0.40 (0.34-0.48) | 110 | 31 880 | 0.35 (0.28-0.42) | 0.85 (0.66-1.10) | .21 |
Subnational figures have been rounded to the nearest 5; percentages calculated using rounded counts. Sources: April 2019-March 2020: Hospital Episode Statistics, NHS Digital. Copyright 2020, reused with the permission of NHS Digital. All rights reserved (provisional data). April 2020-June 2020: Secondary Uses Service, NHS Digital. Copyright 2020, reused with the permission of NHS Digital. All rights reserved.
Significance test at the .05 level.
Discussion
There was no evidence of any increase in stillbirths regionally or nationally during the COVID-19 pandemic in England when compared with the same months in the previous year and despite variable community SARS-CoV-2 incidence rates in different regions.5 This contrasts with the findings from a single UK hospital4 and is reassuring given the concerns about patients, including pregnant women, receiving fewer services or being hesitant to access health care during the pandemic.6 Limitations of the study include using a combination of annual and monthly HES data sets and not having data available on SARS-CoV-2 infection status, maternal sociodemographic characteristics, or access to care for the cohort. It will be important to continue to monitor pregnancy outcomes in the future.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
eFigure. Comparison of Delivery Rates With a Recorded Stillbirth in England in HES and SUS, December 2019 to May 2020
References
- 1.Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med. 2014;370(23):2211-2218. doi: 10.1056/NEJMra1213566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pregnancy and coronavirus, 2020. NHS England. Published July 22, 2020. Accessed September 4, 2020. https://www.nhs.uk/conditions/coronavirus-covid-19/people-at-higher-risk/pregnancy-and-coronavirus/
- 3.Knight M, Bunch K, Vousden N, et al. ; UK Obstetric Surveillance System SARS-CoV-2 Infection in Pregnancy Collaborative Group . Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khalil A, von Dedelszan P, Draycott T, Ugwumadu A, O’Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324(7):705-706. doi: 10.1001/jama.2020.12746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coronavirus (COVID-19) in the UK. Public Health England. Accessed September 17, 2020. https://coronavirus.data.gov.uk/cases
- 6.Coronavirus and pregnancy—preserving maternal health across the European Region. World Health Organisation Europe. Published June 30, 2020. Accessed August 14, 2020. https://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/news/news/2020/6/coronavirus-and-pregnancy-preserving-maternal-health-across-the-european-region
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Comparison of Delivery Rates With a Recorded Stillbirth in England in HES and SUS, December 2019 to May 2020