Abstract
Objective:
To evaluate perceptions regarding cell phone use in a teaching hospital setting among health care providers, residents, medical students, and patients.
Methods:
Fifty-three medical students, 41 resident physicians, 32 attending physicians, and 46 nurses working at University Hospital completed a questionnaire about cell phone use practices and their perceptions of cell phone use in the hospital. Forty-three inpatients admitted to medical/surgical units at University Hospital were surveyed at bedside about their perceptions regarding physicians’ cell phone use.
Results:
All health care providers identified cell phones as a risk to patient confidentiality with no specific group significantly more likely to attribute risk than another. Practitioners were identified as either primarily as inpatient or outpatient practitioners. Inpatient practitioners were significantly more likely to rate cell phones as beneficial to patient care than outpatient practitioners. Physicians were statistically more likely to rate mobile phones as beneficial to patient care as compared to nurses. Among the patient population surveyed, one quarter noted that their physician had used a cell phone in their presence. The majority of those patients observing practitioner cell phone use had reported a beneficial or neutral impact on their care. Significance: Perceived risk of cell phones to patient confidentiality was equal across health care providers surveyed. Physician and medical students were significantly more likely to rate cell phones as beneficial to patients’ care than nurse providers. Patients indicated that their physicians used cell phones in their presence at low rates and reported that the use was either neutral or beneficial to the care they received.
Keywords: technology, clinician–patient relationship, education, interprofessional education, cell phone
Introduction
Since their introduction nearly 40 years ago, cell phones have become ubiquitous in both personal and professional settings. In the practice of medicine, cell phones have become increasingly commonplace, with an estimated 87% of physicians using a smartphone or tablet at their workplace (1). As within the general population, cell phones now serve a vital role within the health care community, from patient monitoring to communication with colleagues as well as a more convenient access to online medical information. The “smartphone” particularly has revolutionized the practice of medicine, with documented evidence of improvement in hospital communication and workflow efficiency (2). The use of smartphones can positively impact clinical training and remote patient management through applications (“apps”) designed specifically for physician use (3,4). These devices also allow for easy and fast access to the information available on the internet, providing health care providers with current relevant resources to support their clinical decision-making and direct patient care (5). The pervasive use of smartphones in the health care setting, however, has also presented unique challenges. Previous studies have noted significant distraction among health care providers due to frequent smartphone notifications that led to missing important patient information (6). Additionally, there are pervasive concerns regarding unprofessional behavior when using smartphones, and risks to patient privacy when using these devices to communicate patient information (7,8). Text messages between providers may be misinterpreted or ambiguous (9). Additionally, cell phones may increase the risk of nosocomial infection through cross contamination when potentially contaminated cell phones are handled post hand washing (10). Despite their ubiquity, there is a notable lack of literature regarding patient and health care provider attitudes about cell phones being used in the clinical setting. Therefore, this study examined both perceptions regarding cell phone use and the impact of mobile phones among health care providers and patients, by characterizing (a) the difference in perceptions toward smartphone use in clinical settings between physicians, trainees, and nurses, (b) perceptions around the benefits of mobile phones and their perceived risk to patient confidentiality, and (c) patients’ attitudes about their physician’s cellular device use. For the purposes of this study, smart phones is a term used to describe any of the cell phones used in this study by participants which included multiple types but all of which enabled data storage, web access ability, Text enabled, and voice communication.
Methods
Study Population
The study sample was obtained via convenience sampling and included both health care providers and patients. The provider participants included attending physicians, resident physicians, medical students, and nurses working at University Hospital in Newark, New Jersey. The patient population was comprised of adult patients and adult guardians of pediatric patients who were hospitalized on the inpatient medical, surgical, and pediatric units at University Hospital during the time of the study.
Study Design and Data Collection
This was a cross-sectional, survey-based study in which a single page paper survey was administered to attending physicians, residents, medical students, nurses, and patients. Questions on each survey were tailored based on the role of the respondent. From March 12, 2017, to July 25, 2018, the survey was distributed in resident and physician lounges, the hospital cafeteria, and all patients were inpatient and were administered the questionnaire in the units at University Hospital they were admitted to. All study procedures were approved by the Rutgers New Jersey Medical School Institutional Review Board. No participant identifiers were obtained.
Eligibility criteria included all patients over 18 or adult guardian of pediatric patients admitted to medical, surgical, and pediatric units at University Hospital who were English or Spanish speaking. All participants were required to have been alert and conscious enough to obtain a verbal informed consent.
Predictors
We examined 7 possible predictors of attitudes about the impact of cell phones on clinical care. Demographic variables included age (20-29, 30-39, 40-49, 50-59, 60-69, >70), professional role (medical student, resident physician, attending physician, nurse), and location of provider (inpatient, outpatient). Cell phone use patterns were ascertained via questions investigating what types devices were used in the hospital, the purpose of use (personal, clinical, or both), the location of use, and whether the provider used their phone in the presence of patients.
Outcome measures
The primary outcome measures collected were perceptions regarding the impact of cell phones on risk to patient confidentiality. They were ascertained by inquiring “Do you believe that cell phone use can potentially compromise patient confidentiality?” Response options included “Yes,” “No,” and “Potentially, based on location of use”. “Yes” and “Potentially, based on location of use” were merged to dichotomize the responses to “yes/potentially” and “no”.
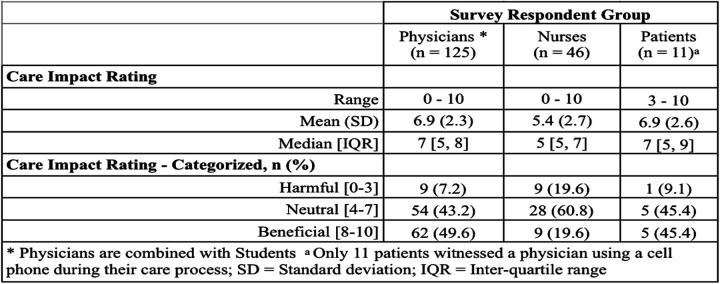
The secondary outcomes were provider attitudes regarding the benefit of cell phones in the health care setting. They were ascertained by inquiring “How would you rate the impact of cell phone use on the quality of patient care” with a numerical scale ranging from 0 to 10. Responses from 0 to 3 were demarcated as having a “Harmful” impact on patient care, responses from 4 to 7 were demarcated as having a “Neutral” impact on patient care, and responses from 8 to 10 were demarcated as being “Beneficial” to patient care.
Statistical analysis methods
Study data and outcomes were first characterized using summary statistics for each of the respondent groups (physicians, nurses, and patients). Comparisons of outcome measures between the respondent groups were performed using Pearson’s χ2, Fisher’s exact, and Wilcoxon Rank Sum tests. All statistical tests were 2-sided and a P value less than .05 was considered statistically significant.
Results
Between March 12, 2017, and July 25, 2018, a total of 214 surveys were collected. The respondents were comprised of medical students (n = 52), resident physicians (n = 41), attending physicians (n = 32), nurses (n = 46), and patients (n = 43) admitted to the University Hospital. Three provider surveys were later excluded from analysis as the respondents had completed less than half of the survey questions.
Cell Phone Use Patterns
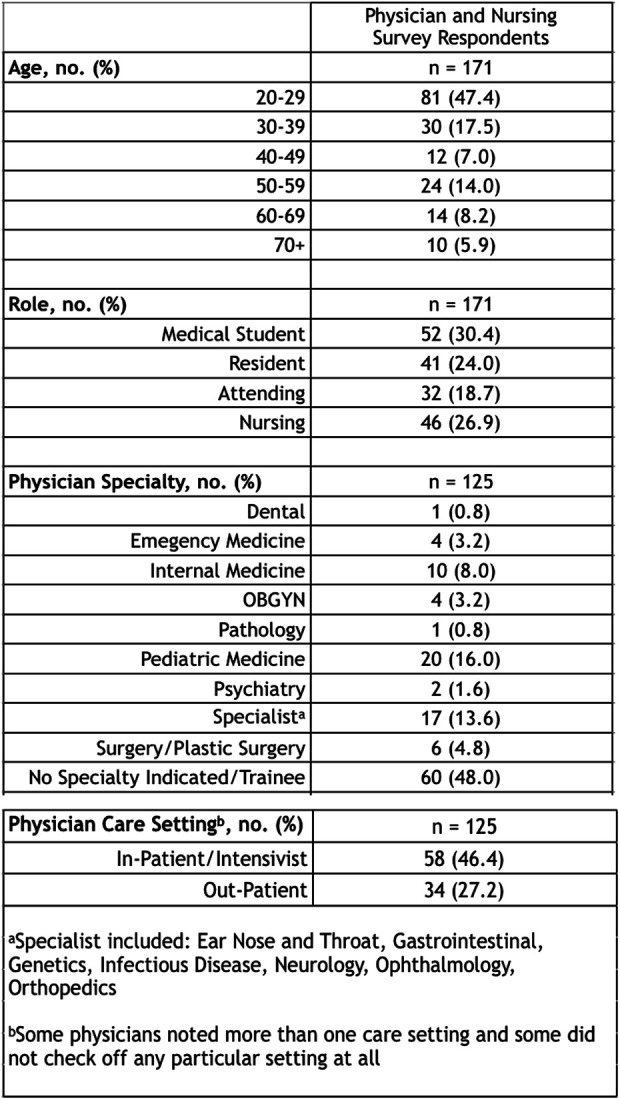
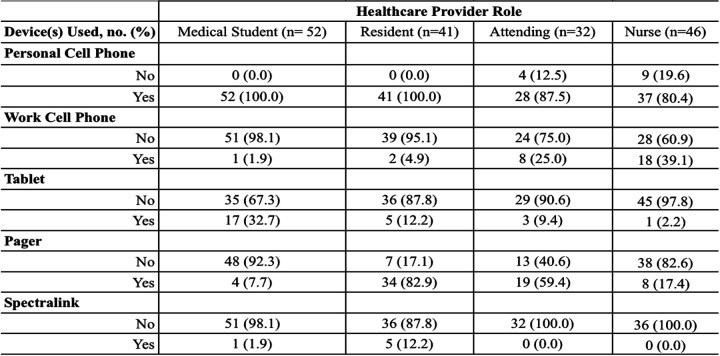
As part of the survey, table 1 included basic demographics (age, professional status of respondent and site of services) and whether the devices that health care providers used in the hospital were self-provided, employer-issued, or if they used both personal and employer issued devices. Attending physicians (24.1%) were significantly more likely than resident physicians (4.9%) and medical students (1.9%) to report using both a personal and employer-issued cell phone, while nearly all (96.8%) of the trainees (medical students and resident physicians) reported using only their personal cell phones. We also inquired about the types of technological devices that health care providers used in the hospital, including pagers, cell phones, tablets, and other. Overall, attending physicians were also significantly less likely to use a personal cell phone in a clinical setting, compared to medical students and residents (87.5% vs 100.0% vs 100.0%, P = .004). Residents (82.9%) were the most likely to report using a pager device in the hospital compared with medical students (7.7%) and attending physicians (59.4%). Residents (12.2%) and medical students (32.7%) reported using tablets at significantly higher rates than attendings (9.4%; see Table 2).
Table 1.
Provider Demographics.
|
Table 2.
Device Use by Health Care Provider Role.
|
Nurses also reported considerable rates of cell phone use in the clinical setting. While 80% of nurses reported using their own personal cell phone, an additional 30% reported also using an employer provided cell phones. Nurses were also surveyed regarding their observations of physician cell phone utilization (see Table 2). Sixty-one percent of nurses reported observing physicians using a cell phone in the presence of a patient.
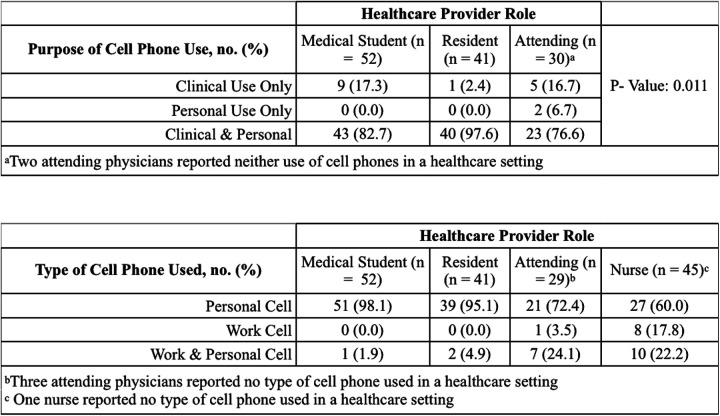
We also inquired as to whether health care providers used their devices in the hospital setting for clinical purposes (such as communicating with other providers or looking up clinical data), for personal purposes (such as communicating with family members), or both clinical and personal purposes. Attending physicians, resident physicians, and medical students reported using their phones for clinical purposes at nearly equal rates; however, medical students (82.7%) and resident physicians (97.6%) were significantly more likely than attending physicians (76.6%) to report combined clinical and personal use (P = .01; see Table 3).
Table 3.
A, Purpose of Cell Phone Use Among Health Care Providers. B, Type of Phone Used by Providers.
|
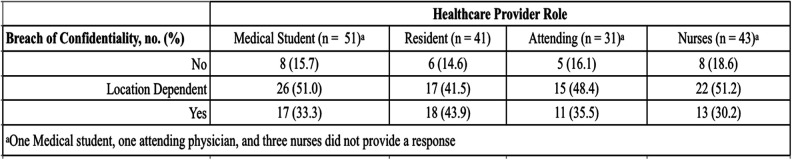
Perceived Risk of Cell Phones for Patient Confidentiality
Attendings (83.9%), residents (85.3%), and medical students (85%) acknowledge equally that cell phone use in clinical spaces impose potential risk to patient confidentiality (responses include %location dependent or yes) with cell phone use, with no group endorsing significantly higher perception of the risk. Nurses (81.4%) also identify a potential risk to patient confidentiality with increased clinical use of cell phones (see Table 4).
Table 4.
Perceptions of Risk of Cell Phone Use by Providers
|
Perceived Impact of Cell Phones
In general, all respondents acknowledge that cell phones are potentially beneficial to health care, (attendings 50%, residents 56%, medical students 44%) without any significant difference between provider roles. However, attendings physicians (13%) were more likely to report that cell phones were potentially harmful to patient care compared to resident physicians (7%) and medical students (4%). Additionally, there was a significant difference between the perceptions among physicians and nurses. Only 19% of nurse respondents (vs 50% physicians and trainees) indicated that they thought cell phones were beneficial to patient care. There was no significant difference in perceived benefit of cell phones between physicians and patients or between nurses and patients. Physicians who practice inpatient medicine (58.6%) were significantly more likely to report that cell phone use was beneficial to care compared with physicians who practice exclusively in the outpatient setting (30%; see Table 5).
Table 5.
Provider Perceived Impact of Cell Phones on Care.
|
Patient Perspective
Forty-three patients were surveyed regarding their physician’s cell phone use. Patient ages ranged from 20 to 70+ with a median age-group of 50 to 59 years old. Seven (16.5%) patients were provided surveys in Spanish. Of the patients surveyed, 25.6% endorsed that their physician had used a cell phone in their presence. Of those patients, 45.5% felt that cell phones contribute beneficially to their care, 45.5% felt that the impact of their physician’s cell phone use on their care was neutral, while only 9% felt that their physician’s cell phone use was harmful to their care.
Discussion
This is the first systematic investigation of attitudes and perceptions regarding the impact of cell phones on clinical care and patient confidentiality among both health care providers and patients. Congruent with national data, we found that the health care providers we surveyed endorsed using cell phones in clinical settings at high rates (1). Attending physicians were least likely of all health care providers to use their cell phone in the clinical setting, while resident physicians and medical students reported high rates of use for both personal and professional purposes. The reason underpinning these use patterns are likely multifactorial. First, seasoned attending physicians likely find cell phones unnecessary to carrying out their daily clinical decision-making. They are familiar with guidelines for care and have refined clinical judgement. As such they likely rely less on standardized scales and recommendation calculators than younger physicians whose training has been technology-oriented. Second, in recent years resident and student education has been revolutionized by dozens of teaching apps and online modules focused on medical education (6). They are used to support clinical decision-making, provide risk calculations, and optimize care (9). As cell phones become integral to physician training, their use in clinical settings has been adopted at much higher rates among younger physicians and trainees. In addition, attending physicians were significantly more likely than resident physicians and medical students to indicate that they perceived cell phones as potentially harmful to patient care, which is consistent with their reduced rates of use in clinical settings.
Considering the ubiquity of cell phones, we assessed provider perceptions of potential risks that they pose to patient care. We specifically assessed perceived risk to patient confidentiality, since cell phones often store sensitive patient data that requires careful protection. Providers uniformly reported perceptions that cell phones pose a risk to confidentiality of protected health information. All health care providers regardless of role are required to undergo Health Insurance Portability and Accountability Act (HIPPA) certified training annually. This training likely imparts an awareness of guidelines for protecting patient confidentiality among all providers. While the differences were not statistically significant, medical students and residents endorsed the highest perceived risk of cell phones to confidentiality compared with other providers. Our findings are consistent with previous studies which have also identified that medical students understand the risk that cell phone communication pose to patient confidentiality (11). However, students and physicians continue to use nonsecure devices to communicate patient health information (PHI) with colleagues, indicating further need for education around proper use and implementation of policy around cell phone use for clinical purposes (11).
We also assessed perceived impact of cell phones on patient care among providers and patients. We found that attending physicians, resident physicians, and medical students reported that they perceived cell phone as beneficial to patient care at similar rates. In addition, physicians and medical students were significantly more likely to perceive cell phones as beneficial to patient care than nurses. This difference is explained in part by the tendency of medical students and residents to use cell phones for educational purposes. Numerous apps have been designed for medical education and health care–related use that were shown to improve patient care (12). As evidence-based medicine curriculums become more commonplace in medical schools, cell phone use among practitioners will likely increase for the purpose of incorporating national guidelines and current recommendations into patient care (4). Finally, resident physicians hold the responsibility of communicating with attending physicians, consulting physicians, auxiliary staff, and medical students on the team to manage and direct care for each patient on their service (13,14). This responsibility likely accounting for their higher rates of cell phone use and higher perceived benefit of cell phones on patient care.
Attending physicians practicing within the inpatient setting were significantly more likely to perceive cell phones as beneficial to patient care compared with attending physicians practicing solely in outpatient offices. Inpatient medicine has been impacted by the advent of cell phone technology, allowing for rapid communication with consulting physicians and immediate access to laboratory results (15,16), which are often absent in office-based medicine. Additionally, though attending physicians indicated that they believed cell phones to be overall beneficial to patient care, they were more likely to perceive cell phones as harmful to patient care compared with resident physicians and medical students.
Finally, a small minority of our patients sampled reported that a physician had used a cell phone in their presence during their current admission to the hospital. Of the patients who endorsed physician phone use, almost all those individuals reported that they perceived their physician’s cell phone use to be beneficial or neutral to the medical care they received. Previous studies of patient perceptions of physician cell phone use have shown patient tolerance of cell phones in the clinical setting, if they are used for work-related purposes (17). Of note, our patient population is composed of a proportion of non-English speakers and many of the patients who endorsed physician phone use noted that the device was employed for translation services. As such, it was unsurprising that patients perceived cell phones to be beneficial to their care, as they functioned to aid the patients’ communication with their physician.
There are several limitations to this study. We employed convenience sampling and while there were no participants who refused to complete the survey, there is a risk that those surveyed differ from the general provider population in their cell phone utilization and attitudes. We also relied on self-reported data regarding cell phone use patterns. Since there was no direct observation of use, the self-reported patterns could potentially fail to reflect true practices of health care providers. In addition, our patient population was composed of many Spanish-speaking patients and their family members. These individuals could potentially regard cell phones as more beneficial to their care due to the convenience of obtaining interpreter services through cell phones, causing them to underestimate the potentially detrimental impact of cell phones on patient care.
We were able to demonstrate in this study that cell phones, when used appropriately, can be a vital asset in improving patient care, facilitating communication, and improving medical education. Nevertheless, it is important that as these new tools of communication become commonplace in the practice of medicine that health care providers and patients alike remain cognizant of maintaining the traditional patient–physician relationship, marked by confidentiality, compassion, and trust.
Acknowledgments
The authors would like to acknowledge and thank the faculty, staff, students, residents, and patients cared for at University Hospital for their support and participation in this study that has enabled them to examine and evaluation the impact of technology on clinical care.
Author Biographies
Courtney Caminiti earned her MD from New Jersey Medical School and an MPH degree from Columbia University Mailman School of Public Health. She is currently a first-Year pediatrics resident at the Children's Hospital at Montefiore.
Lily Deng is working with Rutgers Biomedical and Health Sciences.
Patricia Greenberg is administrative manager & senior biostatistician for RUBIES in Department of Biostatistics & Epidemiology.
Anthony Scolpino is currently working with Rutgers New Jersey Medical School.
Catherine Chen is currently a Second-Year studying Biomedical Engineering at Northwestern University. She has earned an associate degree from Raritan Valley Community College in 2018 and is planning to matriculate to Northwestern University Feinberg School of Medicine in 2021 through Northwestern's 7-Year HonorsProgram in Medical Education program. She currently serves as a research project lead for the Competition for Undergraduate Regenerative Engineering (CURE) investigating quick-gelling, anti-bacterial catechol-based hydrogels for applications in wound healing. Catherine plans to continue her scientific endeavors this upcoming summer through the Summer Undergraduate Research Fellowship at the Mayo Clinic working with Dr. Bradley Erickson on computer-aided diagnostics.
Ellen Yang is working with Rutgers Biomedical and Health Sciences.
James M Oleske is currently working with François-Xavier Bagnoud Distinguished Professor of Pediatrics Emeratus, Rutgers New Jersey Medical School, Newark, New Jersey.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James M Oleske, MD, MPH  https://orcid.org/0000-0003-2305-5605
https://orcid.org/0000-0003-2305-5605
References
- 1. Chase J. iPad and other drugs Medical Marketing & Media: The Interactive Guide; 2013:10–11. [Google Scholar]
- 2. Soto RG, Chu LF, Goldman JM, Rampil IJ, Ruskin KJ. Communication in critical care environments: mobile telephones improve patient care. Anesth Analg. 2006;102:535–41. [DOI] [PubMed] [Google Scholar]
- 3. Derbyshire SW, Burgess A. Use of mobile phones in hospitals. BMJ. 2006;333:767–8. doi:10.1136/bmj.38995.599769.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Westbrook JI, Gosling AS, Coiera E. Do clinicians use online evidence to support patient care? A study of 55,000 clinicians. J Am Med Inform Assoc. 2004;11:113–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Katz-Sidlow RJ, Ludwig A, Miller S, Sidlow R. Smartphone use during inpatient attending rounds: prevalence, patterns and potential for distraction. J Hosp Med. 2012;7:595–9. [DOI] [PubMed] [Google Scholar]
- 6. Wu RC, Lo V, Morra D, Wong BM, Sargeant R, Locke K, et al. The intended and unintended consequences of communication systems on general internal medicine inpatient care delivery: a prospective observational case study of five teaching hospitals. J Am Med Inform Assoc. 2013;20:766–77. doi:10.1136/amiajnl-2012-001160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robinson T, Cronin T, Ibrahim H, Jinks M, Molitor T, Newman J, et al. Smartphone use and acceptability among clinical medical students: a questionnaire-based study. J Med Syst. 2013;37:9936 doi:10.1007/s10916-013-9936-5 [DOI] [PubMed] [Google Scholar]
- 8. Wu RC, Morra D, Quan S, Lai S, Zanjani S, Abrams H, et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5:553–9. [DOI] [PubMed] [Google Scholar]
- 9. 6 pitfalls of texting for hospitals: how to avoid them. 2016. Retrieved from:http://www.healthcarebusinesstech.com/hospital-texting-pitfalls
- 10. Redelmeier DA, Detsky AS. Pitfalls with smartphones in medicine. J Gen Intern Med. 2013;28:1260–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tran K, Morra D, Lo V, Quan SD, Abrams H, Wu RC. Medical students and personal smartphones in the clinical environment: the impact of confidentiality of personal health information and professionalism. J Med Internet Res. 2014;16:e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ventola CL. Mobile devices and apps for healthcare professionals: uses and benefits. PT. 2014;39:356–64. [PMC free article] [PubMed] [Google Scholar]
- 13. Coiera E, Tombs V. Communication behaviors in a hospital setting: an observational study. BMJ. 1998;316:673–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hortwitz LI, Detsky AS. Physician communication in the 21st century: to talk or to text? JAMA. 2011;305:1128–9.15. [DOI] [PubMed] [Google Scholar]
- 15. Angarita FA. Incorporating smartphones into clinical practice. Ann Med Surg (Lond). 2015;4:187–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu R, Rossos P, Quan S, Reeves S, Lo V, Wong B, et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed methods study. J Med Internal Res. 2011;13: e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Alexander SM, Nerminathan A, Harrison A, Phelps M, Scott KM. Prejudices and perceptions: patient acceptance of mobile technology use in health care. Inter Med J. 2015;45:1179–81. [DOI] [PubMed] [Google Scholar]


