Abstract
The COVID-19 pandemic has resulted in widespread hospitalisations and deaths around the world. As patients with rheumatic diseases generally have increased risk of infections and complications, understandably, there is significant concern of the impact of SARS-CoV-2 on these patients. However, there is a paucity of data in rheumatic patients. We review mechanisms through which SARS-CoV-2 results in infection, including ACE2 receptor, and complications (including immune dysregulation, thrombosis and complement activation). We assess these pathways in patients with rheumatic disease and those on immune modulating therapy. Although data thus far does not appear to show worse outcomes in rheumatic patients as a whole, given alterations in the underlying immune pathways in certain diseases (such as systemic lupus erythematosus), we posit that the risk is not equal in all rheumatic patients. We also discuss the benefit of underlying disease control with respect to COVID-19 risk reduction and potential increased risk of disease flares following viral infection from an immune standpoint.
Introduction
By late October 2020, severe acute respiratory coronavirus 2 (SARS-CoV-2) has infected over 43 million people globally, with over 1.1 million deaths and thousands more hospitalisations for direct complications from COVID-19 [1]. Prevalence of COVID-19 is equal between the genders, although men are at higher risk for severe outcomes and death [2]. This is particularly concerning as there are no proven therapies for this infection as of yet and vaccine developments are still underway. Many immunocompromised patients, particularly in rheumatic diseases, may theoretically develop increased complications from COVID-19, although preliminary studies have been inconclusive [3–6]. Using knowledge of the immunopathogenesis of rheumatic diseases and the expanding knowledge of COVID-19 immune responses, we aim to describe some of the similarities between the immune dysregulation in rheumatic diseases and COVID-19. We also aim to summarise the risk of developing severe COVID-19 in rheumatic disease and to therapies utilised for rheumatic diseases, in addition to how these therapies can be utilised to target the inflammatory complications associated with COVID-19.
COVID-19 viral entry in aging and rheumatic diseases
In many patients with rheumatic diseases (e.g. rheumatoid arthritis and systemic lupus erythematosus), there is a documented higher risk of severe infectious complications compared to the general population, which may relate to the degree of disease activity [7, 8]. There is little data however that patients with rheumatic conditions as a whole may have an increased risk for contracting COVID-19, although evidence is limited. Like other viruses, SARS-CoV-2 requires entry into cells in order to replicate. This, in turn, results in cellular responses aimed at quelling the viral infection. The primary cellular receptors for SARS-CoV-2 which bind the viral spike protein is angiotensin-converting enzyme 2 (ACE2), and its co-receptor, transmembrane serine protease 2 (TMPRSS2) [9, 10]. Patients with co-morbidities for cardiovascular disease including obesity, hypertension and chronic kidney disease have higher levels of circulating ACE2 [11, 12]. These patients have been shown to have more severe COVID-19. These co-morbidities are present more frequently in patients with rheumatic diseases. Interestingly, both ACE2 and TMPRSS2 are transcriptionally expressed at higher levels in respiratory epithelial cells in elderly patients [13]. ACE2 is also hypomethylated and overexpressed in lupus [14]. Apolipoprotein E, a known inducer of ACE2, is present in higher levels in patients with rheumatic and cardiovascular diseases [15, 16], suggesting that ACE2 levels are likely elevated in rheumatic patients. This theoretically increases the risk of contracting COVID-19 in patients with rheumatic diseases. Moreover, cytokines that are elevated in patients with rheumatic diseases (e.g. TNFα) may promote the expression of ACE2 [17], and disease modifying therapies (e.g. hydroxychloroquine), may reduce their expression [18]. This suggests that maintaining adequate control of rheumatic diseases may be important in reducing the risk of infection. This notion is supported by recent data from prospective cohorts showing that the incidence of COVID-19 infections in patients receiving disease modifying therapies (e.g. TNF alpha inhibitors or JAK inhibitors) for inflammatory conditions (e.g. inflammatory arthritis or inflammatory bowel disease) was comparable to that of the general population [4, 19].
Immune dysregulation in COVID-19, aging and rheumatic diseases
In both active rheumatic diseases (such as systemic lupus erythematosus, systemic sclerosis and myositis) and anti-viral immune response, there is generation of a robust type I interferon (IFN) response. IFN responses are important in limiting intracellular viral replication and in the generation of the appropriate immune response required for proper host defense. In many rheumatic diseases, elevated disease activity is associated with increased IFN signals [20]. Based on the role of IFN responses in viral infection, the increased IFN signals in active rheumatic diseases may be theorised to assist with viral clearance during an infection. Intriguingly, aging results in diminished type I interferon responses intracellularly [21]. Recently, inborn errors against type I interferon immunity [22] and autoantibodies against type I interferon [23] have been detected in patients with severe COVID-19 in contrast to patients with mild/asymptomatic disease, suggesting that impaired interferon response plays a key role in disease pathogenesis.
In patients with severe COVID-19, there is a prominent cytokine release syndrome (CRS or cytokine storm). Acute respiratory distress syndrome, which is a consequence of the cytokine storm and clinically presents as respiratory and/or heart failure, is a frequent cause of mortality in patients hospitalised with COVID-19 [24]. Cytokine storm stems from the infected individual’s response to SARS-CoV-2 in the absence of negative counter-balancing signals as was suggested by the presence of CRS in patients infected with SARS-CoV-1 (which is structurally related to SARS-CoV-2) who had minimal viral titres [25, 26]. In COVID-19, CRS results in unbalanced cytokine responses and elevated levels of inflammatory mediators including IL-6, IL1b and TNF-a [27–29]. Elevated IL-6 levels have been associated with poor outcomes in COVID-19, including mechanical ventilation and mortality in hospitalized patients [30].
One of the primary mechanisms for the loss of immune homeostasis, with subsequent CRS, in patients with COVID-19 stems from the increased activation of the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome and reduced anti-viral type I interferon response [31]. This imbalance results in increased levels of IL-1β and IL-18 generated by an activated NLRP3 inflammasome [32]. These cytokines promote the release of other inflammatory signals including IL-6 and TNFα. Downstream, the pro-inflammatory cytokines promote the release of additional inflammatory signals such as those from activated monocytes, and TH17 cells [33]. Natural killer (NK) cells normally counteract these inflammatory signals by killing viral-infected cells, activated monocytes and T cells, thereby acting to reduce the inflammatory response [34, 35]. In COVID-19, however, NK cell number and function are reduced in patients with severe disease, thereby potentiating the CRS [36].
Patients with cardiovascular co-morbidities, such as diabetes, hypertension, obesity and increased age, are at increased risk for COVID-19 complications [37], suggesting that some of the relevant signals important in maintaining immune homeostasis to counterbalance inflammatory cytokine release are less functional in these patients. These co-morbidities are often more prevalent in patients with rheumatic diseases and there may be an increased risk of cytokine storm in rheumatic patients. Aging is associated with the development of chronic inflammation and a general reduction in immune diversity [38]. The aged innate immune response is characterized by increased secretion of pro-inflammatory cytokines (TNF, IL-6 and IL-1β) and a decrease in the number and function of dendritic cells (DCs) and macrophages. This leads to poor priming of T cells and diminished clearance of infectious agents and apoptotic cells through phagocytosis [39, 40]. Cell-mediated immunity suffers a loss of naïve lymphocytes in the aged population, with an increased expansion of antigen-specific memory lymphocytes, leading to an inadequate immune response to newly encountered antigens and an increased susceptibility to infection [39–41]. NK cells as mediators of immune regulation play a pivotal role in this immune senescence. NK cell production and proliferation are reduced in aging, though the absolute number of NK cells is higher, likely due to the accumulation of long-lived NK cells [42]. The expression of natural cytotoxicity receptor (NCR) NKp30 is also reduced in aging. This not only decreases granule-mediated cytotoxicity but also negatively impacts the adaptive immune response through obstructed NK-DC crosstalk [43]. Neutrophil apoptosis by NK cells is mediated through death receptor ligation by NCR NKp46. Finally, both NKp30+ and NKp46+ NK cell expression is reduced in older individuals [44] which further impairs the elimination of virally infected cells and infected monocytes releasing inflammatory cytokines.
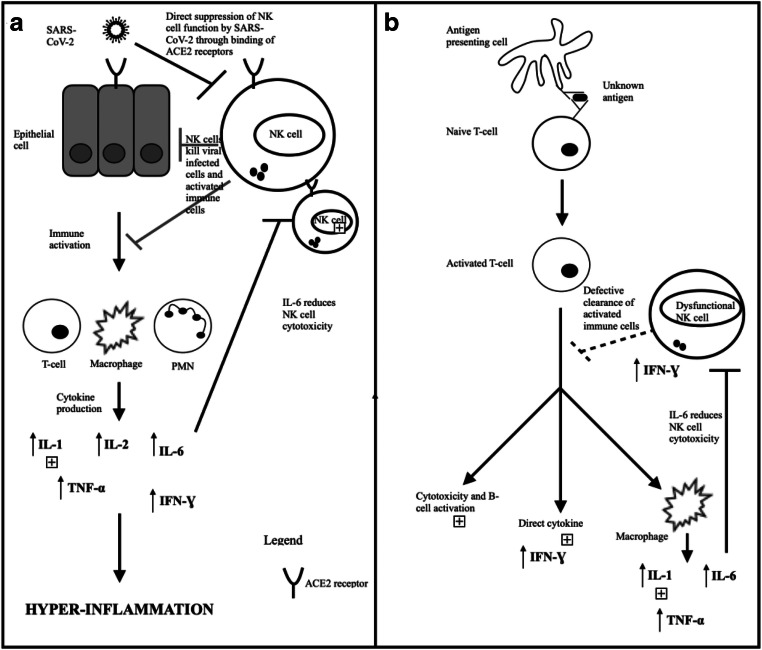
Similarly, in many patients with rheumatic diseases (e.g. systemic lupus erythematosus, Sjogren’s syndrome, systemic sclerosis and systemic juvenile idiopathic arthritis), there is a disparity in negative signals that counterbalance CRS. For example, systemic lupus erythematosus (SLE) patients have a numerical deficit and reduced cytotoxicity of their NK cells. In addition, SLE patients may foster autoantibodies to both HLA class I–binding receptors (NKG2A, NKG2C) and multiple killer cell immunoglobulin-like receptors, which results in the dysregulation of self/non-self-recognition [45, 46]. Although numerical deficits are less frequent in patients with Sjogren’s syndrome and systemic sclerosis (SSc), both groups of patients have reduced NK cell cytotoxicity [47]. Likewise, in patients with chronic lung diseases secondary to rheumatic diseases, NK cell functions are also diminished. Patients with juvenile idiopathic arthritis (JIA) and rheumatoid arthritis–related macrophage activation syndrome also harbour diminished NK cell cytolytic activities [48]. Figure 1 illustrates the similarities in the reduction of NK cell function between SARS-CoV-2 infection and SLE, ultimately leading to hyper-inflammation and organ dysfunction from cytokine release. Hence, patients with rheumatic diseases (especially SLE) may be at increased risk for COVID-19, particularly if their diseases are not adequately controlled.
Fig. 1.
a SARS-CoV-2 directly suppressed NK cell function through binding of ACE2 receptors on the cell surface. This reduces NK cell ability to kill both viral-infected cells and activated immune cells, increasing the production of pro-inflammatory cytokines and contributing to the development of hyper-inflammation. b Similarly, in rheumatic diseases, dysfunctional NK cells are not effective at clearing the immune cells which are activated by the binding of an unknown antigen (via an antigen presenting cell) to a naive T cell. Downstream, this leads to production of pro-inflammatory cytokines, which ultimately lead to organ damage
COVID-19 associated thrombosis, complement activation and relevance to rheumatic diseases
It is well-established that coagulation is intricately linked with inflammation, particularly as elevated IL-6 levels and C-reactive protein (CRP) may be associated in promoting the formation of thrombosis. Postmortem analysis of patients with COVID-19 have shown evidence of thrombotic microangiopathy and neo-angiogenesis from both renal and lung samples, without evidence for vasculitis [49, 50]. Lupus anticoagulants are elevated in 50% of patients with severe COVID-19 and in 91% of patients with severe disease and a prolonged activated partial thromboplastin time (aPTT) [51, 52]. Although these antibodies are associated with thrombosis normally, the presence of these antibodies does not appear to correlate with the risk of thrombosis in COVID-19, as significant antiphospholipid antibodies were not present in patients with COVID-19 and venous thromboembolism [53]. Bikdeli et al. recently highlighted the development of thromboembolic disease as a severe manifestation of SARS-CoV-2 infection [54]. Thrombotic complications were found to be present in more than 30% of cases in COVID-19 patients admitted to intensive care. Similarly, elevated mannose–binding lectin (MBL), which is known to activate the lectin pathway in the complement system, promotes thrombosis. Localised activation of other complement pathways such as the classical or lectin pathways may also result in increased risk of thrombosis in areas of tissue damage, such as the lungs [55].
Like patients with COVID-19, patients with uncontrolled rheumatic diseases have increased risk for thrombosis. This is most notable in patients with SLE [56], although it has also been described in patients with ANCA vasculitis [57] and Sjogren’s syndrome [58]. The thrombotic risks appear to improve once the diseases are more quiescent, although persistent and increased hypercoagulability has been demonstrated in patients during disease remission [59] and may be associated with activation of the alternative pathway and NETosis [60]. Similarly, thrombosis stemming from circulating lupus anticoagulants may be exacerbated by inflammatory insults, such as acute infections. Although this has not been directly shown in patients with SLE and COVID-19, patients with SLE and COVID-19 appear to have more severe courses of hospitalization compared to other patients with rheumatic conditions [61].
COVID-19-associated immune dysregulation
With the unbalanced immune response in COVID-19 patients with vascular co-morbidities, it is conceivable to suspect that patients with rheumatic diseases may be at increased risk for immune dysregulation–related complications as they are more likely to have increased vascular co-morbidities. COVID-19 infection may also lead to underlying flare of rheumatic disease. This is most likely in disease subsets of inflammatory arthritis [62] and ANCA-associated vasculitis [63], where exposure to viral infections has been shown to predispose these patients to disease flares [62]. It is also seen in different forms of reactive arthritis that may be self-limited (e.g. parvovirus B19, hepatitis B, rubella) or longer lasting (e.g. chikungunya and hepatitis C). In contrast to these other viruses, coronaviruses are usually associated with arthralgia, but not frank arthritis [64]. It is unknown, however, if SARS-CoV-2-related arthralgia is self-limited or if it may result in a more chronic inflammatory arthritis. Indeed, exposure to viruses, such as coronavirus and parainfluenza, may increase the likelihood for developing rheumatoid arthritis [65]. Thus far, there have been three reports of patients presenting with a reactive arthritis–like pattern following SARS-Co-V-2 infection [66–68]. Like arthralgia, myalgias are also common in patients with COVID-19 [66] and rarely, myositis can ensue in patients with COVID-19 [69]. As the anti-viral response in patients without a CRS may promote pathways associated with a disease relapse, it would not be farfetched to suspect that certain patients, particularly those with a connective tissue disease (e.g. SLE, Sjogren’s syndrome, inflammatory myositis), may develop a disease flare. However, this has not yet been thoroughly described in patients in relation to SARS-CoV-2 infection.
Lung complications, such as interstitial lung disease, are common in patients with rheumatic illness, particularly in connective tissue diseases [70]. This is clinically challenging, particularly as patients infected with SARS-CoV-2 may also develop lower respiratory infections and pulmonary thrombosis. In a case series of 17 patients with SLE diagnosed with COVID-19 by Mathian et. al., a majority of them (76%) developed respiratory complications [71]. Similarly, in a cohort of patients with rheumatic diseases, a disproportionately larger number of patients with required mechanical ventilation and a prolonged hospitalisation, compared to patients with other rheumatic diseases [3]. It is difficult to determine if the respiratory complications in these SLE patients developed in these studies stemmed primarily from the SARS-CoV-2 infection, SLE flare or a combination of COVID-19 potentiating a respiratory SLE flare. Unfortunately, many of the clinically available biomarkers that are reported to be associated with COVID-19 are also abnormal in rheumatic diseases (e.g. NK cell dysfunction, elevated IL-6, CRP, hypocomplementemia), and they do not always parallel the disease activity in these patients [72–74]. Hence, biomarkers that can distinguish rheumatic disease flares from COVID-19 are desperately needed.
The potential risk of disease flare or complications of COVID-19 with active rheumatic disease supports the notion that patients with rheumatic conditions should be monitored more closely during the pandemic.
Infectious risks associated with therapies in rheumatic diseases
Corticosteroids are commonly used in patients with rheumatic diseases; however, they may increase the risk of contracting COVID-19. Corticosteroids, particularly at increased doses, reduce innate, cell-mediated and humoral immune responses to infection and increase the risk of opportunistic infections [75]. In patients with other severe coronavirus infections, such as SARS and MERS, some studies suggested that high doses of corticosteroids resulted in increased mortality [76]. In a large retrospective cohort of patients with inflammatory bowel disease (IBD), the use of high-dose corticosteroids (prednisone > 20 mg/day) was associated with severe COVID-19 and increased mortality [77]. Prednisone > 10 mg/day was associated with increased COVID-19 severity in patients with rheumatic illnesses [5]. It is unclear if the increased risk is conferred from corticosteroid use or from the dysregulated immunity stemming from rheumatic disease activity. Regardless, corticosteroids increase risk of secondary infections. Many patients with COVID-19 are at risk of developing co-infections, which in turn increases their risk of developing complications including increased hospitalization periods and/or mortality [78]. However, it has been recently postulated that acute corticosteroid use in patients with a CRS related to COVID-19 may be beneficial [79]. It is important, therefore, to weigh the potential benefits (e.g. treating the severe CRS associated with COVID-19 and/or the inflammatory component of rheumatic diseases in the acute setting with the risk of infections) with the risk of long-term corticosteroids.
Many therapies utilised in the treatment of rheumatic diseases were initially thought to be associated with an increased risk of complications from COVID-19, but they are now being investigated as potential therapeutic strategies in the treatment of COVID-19-related cytokine storms. For example, mice deficient in TNFα or its receptor were protected from a severe form of a SARS-CoV infection [80]. This is not surprising and is likely applicable to SARS-CoV-2 as TNFα levels are elevated in patients with COVID-19 [27, 28], and elevated levels of TNFα promotes the expression of ACE2, which increases viral entry into cells [81]. Therapies targeting this pathway have been suggested to potentially treat patients with severe COVID-19 [82]. Therefore, it is no surprise that patients with rheumatic diseases (e.g. rheumatoid arthritis and psoriatic arthritis), and related immune-mediated inflammatory conditions (e.g. IBD) which utilise higher doses of agents targeting this pathway do not appear to have an increased risk of COVID-19 [83]. Similar findings have been observed in COVID-19 patients with agents targeting other pathways used in rheumatic diseases (e.g. anti-IL-17 and anti-IL-12/23 therapies). Indeed, therapies used for treating rheumatic conditions that target cytokine pathways elevated in severe COVID-19 (e.g. IL-6 and IL-1β) have been shown to be beneficial in small single-arm studies [83, 84]. Larger comparative studies assessing the efficacy of these agents are currently underway [85]. Table 1 summarises available information on COVID19 outcomes in patients with rheumatic diseases on immunomodulatory therapies.
Table 1.
Summary of select published studies assessing SARS-CoV-2 infection in patients with rheumatic diseases
| Reference | Jurisdiction | Study type | Patient population | Outcomes |
|---|---|---|---|---|
| Avouac, et al 2020 [86] | France/Italy | Case series | 3 patients with SSc on rituximab (including 1 with ILD) |
Deaths: 0 Mechanical ventilation: 0 At reporting, 1 patient discharged, 2 on general ward All patients had complete B cell depletion |
| Favalli, Monti, et al, 2020 [87] | Italy | Retrospective cohort (survey) |
Baseline: 955 patients on bDMARD or tsDMARD 6 confirmed cases (3 RA, 2 SpA, 1 sarcoidosis; 5 TNF-i, 1 abatacept) 144 suspected cases |
Confirmed cases: 3 Hospitalisations (supplemental oxygen): Deaths: 0 Mechanical ventilation: 0 Suspected cases: Deaths: 0 Mechanical ventilation: 0 |
| Favalli, Agape, et al, 2020 [56] | Italy | Retrospective cohort (survey) |
Baseline: 123 patients with CTD. 60% of patients on csDMARDs. Mean steroid dose 5.3 mg daily. bDMARDs: 18 belimumab, 5 rituximab, 2 IL-6 1 confirmed case (SSc with ILD on rituximab + HCQ) 14 suspected cases |
Confirmed case: Death: 1 Suspected cases: Deaths: 0 Mechanical ventilations: 0 |
| Fredi et al, 2020 [88] | Italy | Retrospective cohort + case-control study (hospitalised COVID-19 with/without COVID-19) |
Baseline: 1525 rheumatic patients at single centre 65 confirmed cases: 43 on glucocorticoid (average 35 mg weekly). 27 bDMARDs (including 4 rituximab) 52 suspected cases |
Confirmed cases: 72% Hospitalisations. 15% deaths (CV co-morbidities in majority) Deaths: 4% Suspected cases: 0 Case control: No difference in hospitalised patients with COVID19 with and without rheumatic diseases |
| Gianfrancesco et al, 2020 [5] | Global | Retrospective cohort |
600 patients from COVID19 Global Rheumatology Alliance physician-reported registry including: rheumatic diseases: 230 RA, 85 SLE, 74 PsA, 48 SpA, 44 vasculitis Medications: 231 on bDMARDs or tsDMARDs; 11 on prednisone > 10 mg/day |
Hospitalisations: 46% Deaths: 9% Hospitalisations: -No difference with rheumatic diseases -Increased with co-morbidities (HTN, lung disease, DM, CVD, CKD) -Increased OR with prednisone > 10 mg/day (OR 2.05) -Reduced with TNF-i (OR 0.40) Patients on TNF-I had reduced odds of hospitalisation (OR 0.40) Patients on prednisone > 10 mg/day had increased odds of hospitalisation (OR 2.05) No differences with other medications |
| Gisondi et al, 2020 [89] | Italy | Retrospective cohort |
Baseline: 5206 patients with PsO on bDMARDs 6 confirmed cases |
Hospitalisations: 4 Mechanical ventilation: 1 Death: 0 -3 had co-morbidities (HTN, DM, CKD, obesity) |
| Haberman et al 2020 [18] | USA | Case series | 86 patients with immune-mediated inflammatory diseases on therapy |
Hospitalisations: 14 ICU: 7 Death: 1 50% hospitalised on bDMARDs/tsDMARDs. 76% ambulatory on bDMARDs/tsDMARDs Hospitalised patients more likely to have co-morbidities (HTN, DM, and obstructive lung disease) |
| Moiseev et al, 2020 [90] | Russian Federation | Retrospective cohort |
Baseline: 902 patients in ICU with COVID19 10 had rheumatic disease (5 RA, 1 PsA, 1 SpA, 1 SLE, 2SSc) Baseline medications not reported |
Deaths: 5 (all had co-morbidities; 2 RA, 1 SpA, 2 SSc) ICU: 3 (all had co-morbidities; 2 RA, 1 SLE) Recoveries: 2 (both had HTN; 1 RA, 1 PsA) |
| Monti et al, 2020 [91] | Italy | Retrospective cohort |
Baseline: 320 RA/PsA patients on bDMARDs/tsDMARDs 4 confirmed cases 4 suspected cases |
Confirmed cases: 1 hospitalisation (supplemental oxygen) Suspected cases: Hospitalisations: 0 Deaths:4 |
| Sanchez-Piedra et al, 2020 [92] | Spain | Cohort |
Baseline: 6600 rheumatic disease patients on bDMARDs/tsDMARDs in BIOBADASER database41 COVID-19 cases at 15 hospitals in the registry 31 confirmed cases 10 suspected cases |
Deaths: 3 ICU: 6 Hospitalisations: 28 Deaths in: 63M RA on anakinra + pred 5 mg/day (smoker, BMI 34.6); 56F SpA on secukinumab (past smoker, BMI 28.4); 91F vasculitis on rituximab + pred 5 mg/day |
| Tomelleri et al, 2020 [93] | Italy | Retrospective cohort |
Baseline: 162 LVV patients (95 GCA; 67 TA)—medications: steroid, MTX, TNF-i, IL-6, JAKi 4 confirmed cases |
Hospitalisations: 2 Deaths: 0 -79M GCA/HTN on prednisone 17.5 mg; 79M GCA/CVD/CKD on pred 7.5 mg |
| Wallace et al, 2020 [94] | USA | Cohort | 5 SLE (80% on HCQ) vs. 31 rheumatic patients with COVID-19 |
SLE: 80% hospitalised; 60% mechanical ventilation; 20% death Overall cohort: 64% Hospitalised: 19% Mechanical ventilation: 13% Death: 0 |
Finally, several groups have suggested that agents targeting anti-CD20, which depletes a large proportion of circulating B cells, may pose an increased risk in patients with COVID-19 [95]. These conclusions are based on the idea that humoral immunity provided by B cells may be important in reducing the viral titres targeting SARS-CoV-2, and potentially promoting the elimination of infected cells via cell-mediated immunity and antibody dependent cellular toxicity (ADCC) [96]. However, there does not appear to be an increased risk of severe COVID-19 in patients with X-linked agammaglobulinemia, or patients treated with anti-CD20 agents who have rheumatic or other inflammatory conditions (e.g. multiple sclerosis) [97–99]. In contrast, patients with combined forms of common variable immune deficiency with both impaired cell-mediated and impaired humoral immunity may be more affected. Arguably, cell-mediated immunity may be more important in reducing the risk of severe CRS and COVID-19. Interestingly, a report of a COVID-19 in a patient with ANCA-associated vasculitis treated with rituximab showed mild symptoms [100]. It is clear, however, that patients treated with these agents have an increased risk of developing other infections (e.g. encapsulated bacteria). Hence, careful monitoring of total immunoglobulin levels (IgG) to ensure that they are in the therapeutic range (7–10 g/L) are important to minimise these risks.
Conclusion and future perspective
Like many other viruses, SARS-CoV-2 poses its own unique challenges, particularly in patients with rheumatic diseases as they also carry a predisposition for immune dysregulation. Careful interpretation is required when assessing disease biomarkers, many of which may indicate either a rheumatic flare or an elevation in COVID-19 disease severity. Most studies suggest that patients with rheumatic disease are not at increased risk for acquiring COVID-19, but that their COVID-19 symptoms may be more severe. However, there is granularity in assessing this issue, as patients with systemic lupus erythematosus may be at increased risk of severe COVID-19. Importantly, there is accumulating evidence that COVID-19 may result in flares of rheumatic disease. Therefore, focus in the case of rheumatic diseases should thus be on making sure that the patient’s underlying disease is well managed and that their symptoms and immune dysfunction are being well regulated, as this may help protect them from an aggravated onslaught of immune dysregulation brought on by COVID-19.
Compliance with ethical standards
Disclosures
None.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WorldHealthOrganization. Coronavirus disease (COVID-19) Pandemic. 2020 [cited 2020 October]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2.Jin J-M, Bai P, He W, Wu F, Liu X-F, Han D-M, Liu S, Yang J-K (2020) Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 10.1101/2020.02.23.20026864 [DOI] [PMC free article] [PubMed]
- 3.D'Silva KM, Serling-Boyd N, Wallwork R, Hsu T, Fu X, Gravallese EM, Choi HK, Sparks JA, Wallace ZS (2020) Clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and rheumatic disease: a comparative cohort study from a US ‘hot spot’. Ann Rheum Dis [DOI] [PMC free article] [PubMed]
- 4.Huang Y, Chen Z, Wang Y, Han L, Qin K, Huang W, Huang Y, Wang H, Shen P, Ba X, Lin W, Dong H, Zhang M, Tu S (2020) Clinical characteristics of 17 patients with COVID-19 and systemic autoimmune diseases: a retrospective study. Ann Rheum Dis [DOI] [PMC free article] [PubMed]
- 5.Gianfrancesco MA, Hyrich KL, Gossec L, Strangfeld A, Carmona L, Mateus EF, Sufka P, Grainger R, Wallace Z, Bhana S, Sirotich E, Liew J, Hausmann JS, Costello W, Robinson P, Machado PM, Yazdany J, Committee C-GRAS (2020) Rheumatic disease and COVID-19: initial data from the COVID-19 Global Rheumatology Alliance provider registries. Lancet Rheumatol [DOI] [PMC free article] [PubMed]
- 6.So H, Mak JWY, Tam LS (2020) No systemic lupus erythematosus with COVID-19 in Hong Kong: the effect of masking? J Rheumatol [DOI] [PubMed]
- 7.Doran MF, Crowson CS, Pond GR, O'Fallon WM, Gabriel SE. Predictors of infection in rheumatoid arthritis. Arthritis Rheum. 2002;46:2294–2300. doi: 10.1002/art.10529. [DOI] [PubMed] [Google Scholar]
- 8.The Corrona® RA Registry. Available from: https://www.corrona.org/registry/rheumatoid-arthritis
- 9.Hoffmann M, Kleine-Weber H, Schroeder S, Kruger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Muller MA, Drosten C, Pohlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280 e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H (2020) Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol [DOI] [PMC free article] [PubMed]
- 11.Kuba K, Imai Y, Penninger JM. Angiotensin-converting enzyme 2 in lung diseases. Curr Opin Pharmacol. 2006;6:271–276. doi: 10.1016/j.coph.2006.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uri K, Fagyas M, Kertesz A, Borbely A, Jenei C, Bene O, Csanadi Z, Paulus WJ, Edes I, Papp Z, Toth A, Lizanecz E (2016) Circulating ACE2 activity correlates with cardiovascular disease development. J Renin-Angiotensin-Aldosterone Syst 17 [DOI] [PMC free article] [PubMed]
- 13.Chow JH, Mazzeffi MA, McCurdy MT. Angiotensin II for the treatment of COVID-19-related vasodilatory shock. Anesth Analg. 2020;131:102–105. doi: 10.1213/ANE.0000000000004825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sawalha AH, Zhao M, Coit P, Lu Q (2020) Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. medRxiv [DOI] [PMC free article] [PubMed]
- 15.Song L-J, Liu W-W, Fan Y-C, Qiu F, Chen Q-L, Li X-F, Ding F. The positive correlations of apolipoprotein E with disease activity and related cytokines in systemic lupus erythematosus. Diagn Pathol. 2013;8:175. doi: 10.1186/1746-1596-8-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vogt LM, Kwasniewicz E, Talens S, et al. Apolipoprotein E triggers complement activation in joint synovial fluid of rheumatoid arthritis patients by binding C1q. J Immunol. 2020;204:2779–2790. doi: 10.4049/jimmunol.1900372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahley RW. Apolipoprotein E: from cardiovascular disease to neurodegenerative disorders. J Mol Med (Berl) 2016;94:739–746. doi: 10.1007/s00109-016-1427-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hodis HN, Quismorio FP, Jr, Wickham E, Blankenhorn DH. The lipid, lipoprotein, and apolipoprotein effects of hydroxychloroquine in patients with systemic lupus erythematosus. J Rheumatol. 1993;20:661–665. [PubMed] [Google Scholar]
- 19.Haberman R, Axelrad J, Chen A, Castillo R, Yan D, Izmirly P, Neimann A, Adhikari S, Hudesman D, Scher JU. Covid-19 in immune-mediated inflammatory diseases - case series from New York. N Engl J Med. 2020;383:85–88. doi: 10.1056/NEJMc2009567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muskardin TLW, Niewold TB. Type I interferon in rheumatic diseases. Nat Rev Rheumatol. 2018;14:214–228. doi: 10.1038/nrrheum.2018.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen HJ, Tas SW, de Winther MPJ (2020) Type-I interferons in atherosclerosis. J Exp Med 217 [DOI] [PMC free article] [PubMed]
- 22.Zhang Q, Bastard P, Liu Z et al (2020) Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 10.1126/science.abd4570 [DOI] [PMC free article] [PubMed]
- 23.Bastard P, Rosen LB, Zhang Q et al (2020) Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 10.1126/science.abd4585 [DOI] [PMC free article] [PubMed]
- 24.Ruan S. Likelihood of survival of coronavirus disease 2019. Lancet Infect Dis. 2020;20:630–631. doi: 10.1016/S1473-3099(20)30257-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, Rollin PE, Dowell SF, Ling AE, Humphrey CD, Shieh WJ, Guarner J, Paddock CD, Rota P, Fields B, DeRisi J, Yang JY, Cox N, Hughes JM, LeDuc JW, Bellini WJ, Anderson LJ, Group SW A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 26.Peiris JS, Chu CM, Cheng VC, Chan KS, Hung IF, Poon LL, Law KI, Tang BS, Hon TY, Chan CS, Chan KH, Ng JS, Zheng BJ, Ng WL, Lai RW, Guan Y, Yuen KY, Group HUSS Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Z, Hu J, Zhang Z, Jiang S, Han S, Yan D, Zhuang R, Hu B, Zhang Z (2020) Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. medRxiv pre-print
- 28.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, Xie C, Ma K, Shang K, Wang W, Tian DS (2020) Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis [DOI] [PMC free article] [PubMed]
- 30.Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, von Bergwelt-Baildon M, Klein M, Weinberger T. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146:128–136 e124. doi: 10.1016/j.jaci.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schmidt RL, Lenz LL. Distinct licensing of IL-18 and IL-1beta secretion in response to NLRP3 inflammasome activation. PLoS One. 2012;7:e45186. doi: 10.1371/journal.pone.0045186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zheng Y, Sun L, Jiang T, Zhang D, He D, Nie H. TNF alpha promotes Th17 cell differentiation through IL-6 and IL-1beta produced by monocytes in rheumatoid arthritis. J Immunol Res. 2014;2014:385352. doi: 10.1155/2014/385352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schuster IS, Coudert JD, Andoniou CE, Degli-Esposti MA. “Natural Regulators”: NK cells as modulators of T cell immunity. Front Immunol. 2016;7:235. doi: 10.3389/fimmu.2016.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nat Immunol. 2008;9:503–510. doi: 10.1038/ni1582. [DOI] [PubMed] [Google Scholar]
- 36.Osman M, Faridi RM, Sligl W, Shabani-Rad M-T, Dharmani-Khan P, Parker A, Kalra A, Tripathi MB, Storek J, Tervaert JWC, Khan FM. Impaired natural killer cell counts and cytolytic activity in patients with severe COVID-19. Blood Adv. 2020;4(20):5035–5039. doi: 10.1182/bloodadvances.2020002650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15:505–522. doi: 10.1038/s41569-018-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gubbels Bupp MR, Potluri T, Fink AL, Klein SL. The Confluence of sex hormones and aging on immunity. Front Immunol. 2018;9:1269. doi: 10.3389/fimmu.2018.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ponnappan S, Ponnappan U. Aging and immune function: molecular mechanisms to interventions. Antioxid Redox Signal. 2011;14:1551–1585. doi: 10.1089/ars.2010.3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aiello A, Farzaneh F, Candore G, Caruso C, Davinelli S, Gambino CM, Ligotti ME, Zareian N, Accardi G. Immunosenescence and its hallmarks: how to oppose aging strategically? A review of potential options for therapeutic intervention. Front Immunol. 2019;10:2247. doi: 10.3389/fimmu.2019.02247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang Y, Wallace DL, de Lara CM, Ghattas H, Asquith B, Worth A, Griffin GE, Taylor GP, Tough DF, Beverley PC, Macallan DC. In vivo kinetics of human natural killer cells: the effects of ageing and acute and chronic viral infection. Immunology. 2007;121:258–265. doi: 10.1111/j.1365-2567.2007.02573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hazeldine J, Lord JM. The impact of ageing on natural killer cell function and potential consequences for health in older adults. Ageing Res Rev. 2013;12:1069–1078. doi: 10.1016/j.arr.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hazeldine J, Hampson P, Lord JM. Reduced release and binding of perforin at the immunological synapse underlies the age-related decline in natural killer cell cytotoxicity. Aging Cell. 2012;11:751–759. doi: 10.1111/j.1474-9726.2012.00839.x. [DOI] [PubMed] [Google Scholar]
- 45.Hagberg N, Theorell J, Hjorton K, Spee P, Eloranta ML, Bryceson YT, Ronnblom L. Functional anti-CD94/NKG2A and anti-CD94/NKG2C autoantibodies in patients with systemic lupus erythematosus. Arthritis Rheum. 2015;67:1000–1011. doi: 10.1002/art.38999. [DOI] [PubMed] [Google Scholar]
- 46.Segerberg F, Lundtoft C, Reid S, Hjorton K, Leonard D, Nordmark G, Carlsten M, Hagberg N. Autoantibodies to killer cell immunoglobulin-like receptors in patients with systemic lupus erythematosus induce natural killer cell hyporesponsiveness. Front Immunol. 2019;10:2164. doi: 10.3389/fimmu.2019.02164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schleinitz N, Vely F, Harle JR, Vivier E. Natural killer cells in human autoimmune diseases. Immunology. 2010;131:451–458. doi: 10.1111/j.1365-2567.2010.03360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crayne CB, Albeituni S, Nichols KE, Cron RQ. The immunology of macrophage activation syndrome. Front Immunol. 2019;10:119. doi: 10.3389/fimmu.2019.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, Frank S, Turek D, Willi N, Pargger H, Bassetti S, Leuppi JD, Cathomas G, Tolnay M, Mertz KD, Tzankov A (2020) Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology [DOI] [PMC free article] [PubMed]
- 50.Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, Yi F, Yang HC, Fogo AB, Nie X, Zhang C. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Harzallah I, Debliquis A, Drenou B (2020) Frequency of lupus anticoagulant in Covid-19 patients. J Thromb Haemost [DOI] [PMC free article] [PubMed]
- 52.Pineton de Chambrun M, Frere C, Miyara M, Amoura Z, Martin-Toutain I, Mathian A, Hekimian G, Combes A (2020) High frequency of antiphospholipid antibodies in critically ill COVID-19 patients: a link with hypercoagulability? J Intern Med [DOI] [PMC free article] [PubMed]
- 53.Galeano-Valle F, Oblitas CM, Ferreiro-Mazon MM, Alonso-Munoz J, Del Toro-Cervera J, di Natale M, Demelo-Rodriguez P. Antiphospholipid antibodies are not elevated in patients with severe COVID-19 pneumonia and venous thromboembolism. Thromb Res. 2020;192:113–115. doi: 10.1016/j.thromres.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quere I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH (2020) COVID-19 and Thrombotic or Thromboembolic Disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol [DOI] [PMC free article] [PubMed]
- 55.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, Baxter-Stoltzfus A, Laurence J (2020) Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res [DOI] [PMC free article] [PubMed]
- 56.Bazzan M, Vaccarino A, Marletto F. Systemic lupus erythematosus and thrombosis. Thromb J. 2015;13:16. doi: 10.1186/s12959-015-0043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stassen PM, Derks RP, Kallenberg CG, Stegeman CA. Venous thromboembolism in ANCA-associated vasculitis--incidence and risk factors. Rheumatology (Oxford) 2008;47:530–534. doi: 10.1093/rheumatology/ken035. [DOI] [PubMed] [Google Scholar]
- 58.Chung WS, Lin CL, Sung FC, Hsu WH, Chen YF, Kao CH. Increased risks of deep vein thrombosis and pulmonary embolism in Sjogren syndrome: a nationwide cohort study. J Rheumatol. 2014;41:909–915. doi: 10.3899/jrheum.131345. [DOI] [PubMed] [Google Scholar]
- 59.Hilhorst M, Winckers K, Wilde B, Oerle RV, Cate HT, Tervaert JWC. Patients with antineutrophil cytoplasmic antibodies associated vasculitis in remission are hypercoagulable. J Rheumatol. 2013;40:2042–2046. doi: 10.3899/jrheum.130200. [DOI] [PubMed] [Google Scholar]
- 60.Middleton EA, He X-Y, Denorme F, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gendebien Z, von Frenckell C, Ribbens C, Andre B, Thys M, Gangolf M, Seidel L, Malaise MG, Malaise O (2020) Systematic analysis of COVID-19 infection and symptoms in a systemic lupus erythematosus population: correlation with disease characteristics, hydroxychloroquine use and immunosuppressive treatments. Ann Rheum Dis [DOI] [PubMed]
- 62.Franklin J, Lunt M, Bunn D, Symmons D, Silman A. Risk and predictors of infection leading to hospitalisation in a large primary-care-derived cohort of patients with inflammatory polyarthritis. Ann Rheum Dis. 2007;66:308–312. doi: 10.1136/ard.2006.057265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kemna MJ, Tervaert JWC, Broen K, Timmermans SA, Paassen PV, Damoiseaux JG. Seasonal influence on the risk of relapse at a rise of antineutrophil cytoplasmic antibodies in vasculitis patients with renal involvement. J Rheumatol. 2017;44:473–481. doi: 10.3899/jrheum.160066. [DOI] [PubMed] [Google Scholar]
- 64.Joob B, Wiwanitkit V. Arthralgia as an initial presentation of COVID-19: observation. Rheumatol Int. 2020;40:823. doi: 10.1007/s00296-020-04561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Joo YB, Lim YH, Kim KJ, Park KS, Park YJ. Respiratory viral infections and the risk of rheumatoid arthritis. Arthritis Res Ther. 2019;21:199. doi: 10.1186/s13075-019-1977-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Saricaoglu EM, Hasanoglu I, Guner R (2020) The first reactive arthritis case associated with COVID-19. J Med Virol. 10.1002/jmv.26296 [DOI] [PMC free article] [PubMed]
- 67.Yokogawa N, Minematsu N, Katano H, Suzuki T (2020) Case of acute arthritis following SARS-CoV-2 infection. Ann Rheum Dis. 10.1136/annrheumdis-2020-218281 [DOI] [PubMed]
- 68.Ono K, Kishimoto M, Shimasaki T, Uchida H, Kurai D, Deshpande GA, Komagata Y, Kaname S (2020) Reactive arthritis after COVID-19 infection. RMD Open. 10.1136/rmdopen-2020-001350 [DOI] [PMC free article] [PubMed]
- 69.Guan WJ, Zhong NS. Clinical characteristics of Covid-19 in China. Reply. N Engl J Med. 2020;382:1861–1862. doi: 10.1056/NEJMc2005203. [DOI] [PubMed] [Google Scholar]
- 70.Doyle TJ, Dellaripa PF. Lung manifestations in the rheumatic diseases. Chest. 2017;152:1283–1295. doi: 10.1016/j.chest.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Favalli EG, Agape E, Caporali R. Incidence and clinical course of COVID-19 in patients with connective tissue diseases: a descriptive observational analysis. J Rheumatol. 2020;47:1296. doi: 10.3899/jrheum.200507. [DOI] [PubMed] [Google Scholar]
- 72.Mathian A, Mahevas M, Rohmer J, Roumier M, Cohen-Aubart F, Amador-Borrero B, Barrelet A, Chauvet C, Chazal T, Delahousse M, Devaux M, Euvrard R, Fadlallah J, Florens N, Haroche J, Hie M, Juillard L, Lhote R, Maillet T, Richard-Colmant G, Palluy JB, Pha M, Perard L, Remy P, Riviere E, Sene D, Seve P, Morelot-Panzini C, Viallard JF, Virot JS, Benameur N, Zahr N, Yssel H, Godeau B, Amoura Z. Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine. Ann Rheum Dis. 2020;79:837–839. doi: 10.1136/annrheumdis-2020-217566. [DOI] [PubMed] [Google Scholar]
- 73.Cruz-Gonzalez DJ, Gomez-Martin D, Layseca-Espinosa E, Baranda L, Abud-Mendoza C, Alcocer-Varela J, Gonzalez-Amaro R, Monsivais-Urenda AE. Analysis of the regulatory function of natural killer cells from patients with systemic lupus erythematosus. Clin Exp Immunol. 2018;191:288–300. doi: 10.1111/cei.13073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lin SJ, Hsu CY, Kuo ML, Lee PT, Hsiao HS, Chen JY. Phenotypic and functional characterization of natural killer cells in rheumatoid arthritis-regulation with interleukin-15. Sci Rep. 2020;10:5858. doi: 10.1038/s41598-020-62654-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Skapenko A, Leipe J, Lipsky PE, Schulze-Koops H. The role of the T cell in autoimmune inflammation. Arthritis Res Ther. 2005;7(Suppl 2):S4–S14. doi: 10.1186/ar1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cohn LA. The influence of corticosteroids on host defense mechanisms. J Vet Intern Med. 1991;5:95–104. doi: 10.1111/j.1939-1676.1991.tb00939.x. [DOI] [PubMed] [Google Scholar]
- 77.Lee N, Allen Chan KC, Hui DS, Ng EK, Wu A, Chiu RW, Wong VW, Chan PK, Wong KT, Wong E, Cockram CS, Tam JS, Sung JJ, Lo YM. Effects of early corticosteroid treatment on plasma SARS-associated Coronavirus RNA concentrations in adult patients. J Clin Virol. 2004;31:304–309. doi: 10.1016/j.jcv.2004.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brenner EJ, Ungaro RC, Gearry RB, Kaplan GG, Kissous-Hunt M, Lewis JD, Ng SC, Rahier JF, Reinisch W, Ruemmele FM, Steinwurz F, Underwood FE, Zhang X, Colombel JF, Kappelman MD (2020) Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an International Registry. Gastroenterology [DOI] [PMC free article] [PubMed]
- 79.Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Inf Secur. 2020;81:266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Group RC, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ (2020) Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med
- 81.Channappanavar R, Fehr AR, Vijay R, Mack M, Zhao J, Meyerholz DK, Perlman S. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Haga S, Yamamoto N, Nakai-Murakami C, Osawa Y, Tokunaga K, Sata T, Yamamoto N, Sasazuki T, Ishizaka Y. Modulation of TNF-alpha-converting enzyme by the spike protein of SARS-CoV and ACE2 induces TNF-alpha production and facilitates viral entry. Proc Natl Acad Sci U S A. 2008;105:7809–7814. doi: 10.1073/pnas.0711241105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Feldmann M, Maini RN, Woody JN, Holgate ST, Winter G, Rowland M, Richards D, Hussell T. Trials of anti-tumour necrosis factor therapy for COVID-19 are urgently needed. Lancet. 2020;395:1407–1409. doi: 10.1016/S0140-6736(20)30858-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cavalli G, De Luca G, Campochiaro C, Della-Torre E, Ripa M, Canetti D, Oltolini C, Castiglioni B, Tassan Din C, Boffini N, Tomelleri A, Farina N, Ruggeri A, Rovere-Querini P, Di Lucca G, Martinenghi S, Scotti R, Tresoldi M, Ciceri F, Landoni G, Zangrillo A, Scarpellini P, Dagna L. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2020;2:e325–e331. doi: 10.1016/S2665-9913(20)30127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kewan T, Covut F, Al-Jaghbeer MJ, Rose L, Gopalakrishna KV, Akbik B. Tocilizumab for treatment of patients with severe COVID-19: a retrospective cohort study. EClinicalMedicine. 2020;24:100418. doi: 10.1016/j.eclinm.2020.100418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Avouac J, Airó P, Carlier N, Matucci-Cerinic M, Allanore Y (2020) Severe COVID-19-associated pneumonia in 3 patients with systemic sclerosis treated with rituximab. Ann Rheum Dis [DOI] [PubMed]
- 87.Favalli EG, Monti S, Ingegnoli F, Balduzzi S, Caporali R, Montecucco C (2020) Incidence of COVID-19 in patients with rheumatic diseases treated with targeted immunosuppressive drugs: what can we learn from observational data? Arthritis Rheum [DOI] [PMC free article] [PubMed]
- 88.Fredi M, Cavazzana I, Moschetti L, Andreoli L, Franceschini F, Airò P et al (2020) COVID-19 in patients with rheumatic diseases in northern Italy: a single-centre observational and case–control study. Lancet Rheumatol [DOI] [PMC free article] [PubMed]
- 89.Gisondi P, Facheris P, Dapavo P, Piaserico S, Conti A, Naldi L et al (2020) The impact of the COVID-19 pandemic on patients with chronic plaque psoriasis being treated with biological therapy: the Northern Italy experience. Br J Dermatol [DOI] [PMC free article] [PubMed]
- 90.Moiseev S, Avdeev S, Brovko M, Yavorovskiy A, Novikov PI, Umbetova K et al (2020) Rheumatic diseases in intensive care unit patients with COVID-19. Ann Rheum Dis [DOI] [PubMed]
- 91.Monti S, Balduzzi S, Delvino P, Bellis E, Quadrelli VS, Montecucco C. Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis. 2020;79(5):667–668. doi: 10.1136/annrheumdis-2020-217424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sanchez-Piedra C, Diaz-Torne C, Manero J, Pego-Reigosa JM, Rúa-Figueroa Í, Gonzalez-Gay MA, et al. Clinical features and outcomes of COVID-19 in patients with rheumatic diseases treated with biological and synthetic targeted therapies. Ann Rheum Dis. 2020;79(7):988–990. doi: 10.1136/annrheumdis-2020-217948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tomelleri A, Sartorelli S, Campochiaro C, Baldissera EM, Dagna L (2020) Impact of COVID-19 pandemic on patients with large vessel vasculitis in Italy: a monocentric survey. Ann Rheum Dis [DOI] [PMC free article] [PubMed]
- 94.Wallace B, Washer L, Marder W, Kahlenberg JM (2020) Patients with lupus with COVID-19: University of Michigan experience. Ann Rheum Dis [DOI] [PMC free article] [PubMed]
- 95.Baker D, Roberts CAK, Pryce G, Kang AS, Marta M, Reyes S, Schmierer K, Giovannoni G, Amor S (2020) COVID-19 vaccine-readiness for anti-CD20-depleting therapy in autoimmune diseases. Clin Exp Immunol [DOI] [PMC free article] [PubMed]
- 96.Boross P, Leusen JH. Mechanisms of action of CD20 antibodies. Am J Cancer Res. 2012;2:676–690. [PMC free article] [PubMed] [Google Scholar]
- 97.Soresina A, Moratto D, Chiarini M, Paolillo C, Baresi G, Foca E, Bezzi M, Baronio B, Giacomelli M, Badolato R (2020) Two X-linked agammaglobulinemia patients develop pneumonia as COVID-19 manifestation but recover. Pediatr Allergy Immunol [DOI] [PMC free article] [PubMed]
- 98.Meca-Lallana V, Aguirre C, Beatrizdel R, Cardenoso L, Alarcon T, Vivancos J. COVID-19 in 7 multiple sclerosis patients in treatment with ANTI-CD20 therapies. Mult Scler Relat Disord. 2020;44:102306. doi: 10.1016/j.msard.2020.102306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Quinti I, Lougaris V, Milito C, Cinetto F, Pecoraro A, Mezzaroma I, Mastroianni CM, Turriziani O, Bondioni MP, Filippini M, Soresina A, Spadaro G, Agostini C, Carsetti R, Plebani A. A possible role for B cells in COVID-19? Lesson from patients with agammaglobulinemia. J Allergy Clin Immunol. 2020;146:211–213 e214. doi: 10.1016/j.jaci.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Suárez-Díaz S, Morán-Castaño C, Coto-Hernández R, Mozo-Avellaneda L, Suárez-Cuervo C, Caminal-Montero L (2020) Mild COVID-19 in ANCA-associated vasculitis treated with rituximab. Ann Rheum Dis. 10.1136/annrheumdis-2020-218246 [DOI] [PubMed]