Abstract
Early diagnosis and treatment of deep vein thrombosis (DVT) is a main issue in the Emergency setting. With the aim of assisting clinicians in the diagnosis and the subsequent management of DVT in the Emergency Departments, a Nominal Group Technique (NGT) study was conducted. A panel of 5 Italian experts developed 21 consensus statements based on available evidence and their clinical experience. The agreed consensus statements may assist clinicians in applying the results of clinical studies and clinical experience to routine care settings, providing guidance on all aspects of the risk assessment, prophylaxis, early diagnosis and appropriate treatment of DVT in the EDs.
Keywords: venous thromboembolism, deep vein thrombosis, emergency department, clinical algorithms, clinical decision rules, D-dimer, pre-test probability
Introduction
Venous thromboembolism (VTE), which refers to a diagnosis of deep vein thrombosis (DVT) and/or pulmonary embolism (PE), is a common, often preventable life-threatening complication in the Emergency Department (ED) patients.1,2 Indeed, early diagnosis and treatment of DVT and PE remains challenging to ED due to the presence of ambiguous clinical signs and symptoms and the potential for a fatal outcome.3
During the last few years, the therapeutic armamentarium of VTE has been enriched with the introduction of direct oral anticoagulants (DOACs) that are associated with additional benefits in emergency situations where monitoring methods are limited,4 including a lower risk of major hemorrhage such as intracranial hemorrhage.5–7
Because of the above evidence, International guidelines encourage early discharge of low risk PE patients and outpatient management of low risk DVT patients.8,9
Currently, most cases of VTE are diagnosed in the ED3 and a significant number of patients (>50%) continue to be managed as in-patients, including those potentially suitable for out of hospital management.3,10
Although several diagnostic algorithms have been developed,11,12 there are no clear indications for the diagnosis and the subsequent management of DVT and PE in the ED. Until such indications will be available, a structured consensus technique appears a well-suited method to develop consensus statements, which reflect the collective diagnostic and management patterns of experts with considerable knowledge and experience in the current management of VTE in the Italian EDs.
In this study, a Nominal Group Technique (NGT)13 aimed to providing advice to ED physicians on all aspects of the risk assessment, prophylaxis, early diagnosis and appropriate treatment of VTE based upon the best available information, including situations where the actual evidences are limited. This is the first of 2 papers on the study, providing indications on diagnosis and management of DVT in the ED. A second paper will present the study’s results on the diagnosis and treatment of PE in the emergency setting.
Methods
Design of the Study
The 3 most common consensus methods used for medical and health services research are the Delphi method, the consensus development conference, and the NGT.13–15 The NGT, that was the method selected in the present study, is a structured, facilitated, multistep, group meeting technique used to generate and prioritize responses to specific questions by a group of experts.16
The NGT meeting usually comprises the following steps:17
Introduction: the facilitator illustrates the purpose of the meeting and, eventually, summarizes the results of recent research on studied topics.
Silent generation: each expert notes individually his “ideas” on the subject.
Sharing: each expert shares his notes in turn and the facilitator registers them.
Discussion: the facilitator leads the discussion and give the experts an equal opportunity to contribute their personal views during the discussion by presenting their own list of “ideas”. At the end of the discussion, the experts come to a shared list of ideas.
Ranking: participants express their level of agreement with respect to the list of ideas. The facilitator consolidates the results and presents them to the group.
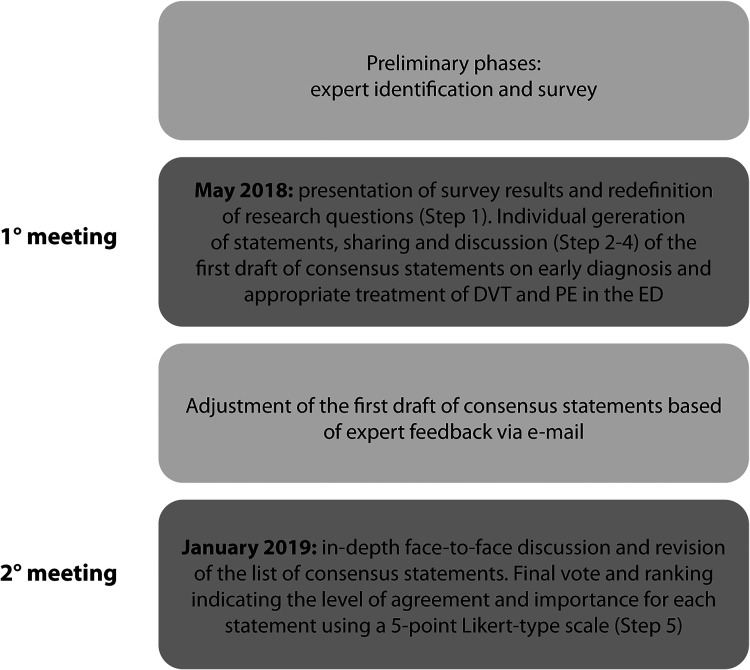
In our study, from May 2018 to January 2019, two NGT meetings were conducted in order to reach a consensus statement on early diagnosis and appropriate treatment of DVT and PE in the ED.
Preliminary Phases: Expert Identification and Survey
Experts were purposively selected to participate in the NGT: all experts had at least 15 years’ experience in ED and 2 peer-reviewed publications on Emergency Medicine within the last 10 years. Five experts—that are the authors of this paper—agreed to participate in the study.
Before the NGT process, a survey was carried out in order to investigate pathways to VTE diagnosis in the Italian ED, with a particular focus on the processes, events, and factors influencing treatment pathways and clinical outcomes.
Based on the available evidence on the diagnosis and management of VTE, items of a closed-ended questionnaire were defined by research team members (2 psychologists and 1 sociologist with extensive experience in standardized consensus methods). Using a dedicated online platform, a sample of 98 Italian ED physicians were asked to answer individually to the questionnaire. The survey platform was online for 10 weeks. Ultimately, 21 physicians answered to the questionnaire (response rate 21.9%). Results of the survey were analysed by research team members. Descriptive statistical analyses were performed using SPSS ver. 25.
NGT Meetings
The first NGT was held in Rome on the 9 May 2018. Phases and steps of the NGT meetings are showed in Figure 1. At the start of the meeting, an overview of the study was presented, and the aim of the NGT and NGT process were briefly explained to the experts by the facilitator (Step 1: introduction). Then results of the survey were presented, while emphasizing the low response rate, followed by discussion among experts. Then research questions were presented and redefined with the help of the experts: considering the characteristics of the 2 pathological conditions, it was decided to evaluate separately for DVT and PE, the aspects related to the risk assessment, prophylaxis, early diagnosis and appropriate treatment in the ED.
Figure 1.
NGT meetings and steps.
In step 2 (silent generation), experts were given 45 minutes to think and generate individually items in response to research questions. Then, each expert was asked to comment individually his statements (Step 3: sharing). During the discussion (Step 4) experts were invited to include comments. At the end of the first NGT meeting, participants generated 24 consensus statements for DVT and 28 for PE.17
Following the meeting, the research team reviewed all the materials and defined a list of consensus statements topically organized that was circulated among the experts by e-mail. Experts were invited to include comment and indicate statements to be discarded or modified and literature on statements that they considered acceptable.
The second meeting was held in Rome on the 28 January 2019. During the meeting, all statements were discussed in depth taking into account updated evidence on diagnosis and treatment of DVT and PE. Overall, during the final discussion, 33 statements (15 for DVT and 18 for PE) were reformulated or merged; for the remaining ones, only minor linguistic modifications were agreed.
During the final voting phase (Step 5: ranking), experts were invited to rate individually each statement on a 5-point Likert-type scale indicating their level of “agreement” and the “importance” of each statement. At the end of the meeting, results were communicated to the whole group.
The definition of the consensus was determined before the analysis and was set at ≥75% agreement.
Results
The final list included 21 consensus statements for DVT. The statements regarding DVT were grouped into the following 4 categories: 1) From clinical suspicion to diagnosis; 2) Patient management with DVT; 3) Treatment of DVT in the acute phase.
The complete list of statements on DVT that reached the consensus is provided in Tables 1.
Table 1.
Consensus Statements on DVT.
| DVT—From clinical suspicion to diagnosis | |
| 1 | It is desirable that the diagnostic work-up of the DVT should be completed in the Emergency Department (ED) with a multidisciplinary approach that can be variable depending on levels of care of the ED. |
| 2 | The clinical manifestations of DVT are not specific: the diagnostic process must be guided by the pre-test clinical probability. |
| 3 | The dichotomized Wells score proved to be accurate in stratifying the pre-test probability of DVT in ED, therefore it is necessary to acquire the information to calculate it before any further investigation. |
| 4 | The determination of D-dimer and the use of non-invasive study of the veins of the lower limbs such as CUS (compressive ultrasonography) is recommended in the DVT diagnostic work-up. |
| 5 | It is recommended that each laboratory has a specific reference cut-off for d-dimer test and it is necessary an age-correction during the interpretation of this value. |
| 6 | In a patient with Wells pre-test score “unlikely” and negative D-Dimer, the diagnosis of DVT can be reasonably excluded. |
| 7 | If Wells score is “unlikely” for DVT and D-Dimer test is positive it is recommended to perform CUS; if CUS is negative it is indicated to perform complete venous ultrasound (US) evaluation (preferably in 48-72 hours); if venous US is negative, the diagnosis is reasonably excluded. If US is not available, it is indicated to perform a second CUS at 5-7 days. |
| 8 | If Wells score is “likely” for DVT it is recommended to perform CUS; if CUS is negative, it is indicated to perform a complete venous US evaluation (preferably in 48-72 hours) to rule out isolated distal DVT, if available, or, if not, repeat CUS at 5-7 days. |
| 9 | If Wells score is “likely” for DVT with a positive CUS evaluation, it is recommended to start anticoagulant therapy. |
| 10 | If the patient has a positive CUS and a positive D-Dimer test the diagnosis of DVT is confirmed regardless of Wells pre-test probability. |
| 11 | In pregnant women with significant edema in one or both the lower limbs or with clinical suspected deep venous thrombosis of other vascular districts, evaluation performing venous Ultrasound (US) is mandatory. |
| 12 | It is not recommended the use of invasive or expensive tests such as phlebography, CT or MRI for the diagnosis of DVT. |
| 13 | In patients with DVT, further investigations are not necessary to exclude Pulmonary Embolism (PE) in absence of specific symptoms. |
| Patient management with DVT | |
| 14 |
|
| 15 | It is recommended that all EDs refer to shared protocols for the out of hospital management and follow-up of patient with an ED diagnosis and initial treatment of DVT. |
| Treatment of DVT in the acute phase | |
| 16 | Prompt initiation of anticoagulant therapy after a diagnosis of DVT is mandatory. |
| 17 | Anticoagulant therapy should begin in the ED right after the diagnosis of DVT, regardless of the patient’s subsequent destination. |
| 18 | While awaiting for the result of diagnostic evaluation of patient with likely DVT (according to the dichotomized Wells score), anticoagulant therapy can also be considered after weighing both thrombotic and hemorrhagic risk. |
| 19 | The choice of the anticoagulant drug must take into account not only the common criteria of good clinical practice, but also patient renal and hepatic function, comorbidities, compliance, preferences and opportunity of early discharge. |
| 20 | DOACs (Direct Oral AntiCoagulants) represent the better anticoagulant approach especially for patients discharge directly, or after a brief observation, from ED |
| 21 | Vena cava filters placement or endovascular procedures are indicated in patients with DVT and contraindications to anticoagulant therapy, depending on hospital skills and availability. |
Most statements were revised during the second NGT meeting. Ultimately, all statements included in the final list reached the defined level of consensus as ≥75% of participants, indicated by a score of 4 (agree) or 5 (strongly agree) (Figure S1-online-only supplementary materials).
Discussion
In this study, NGT method was used to build consensus among a panel of 5 experts who had substantial experience in the current management of DVT in the ED.
In this section, we present final consensus statements (Table 1), with supplementary comments that reflect reasoning behind them, based on experts’ discussion, supported by references where appropriate.
Consensus Statements
1. From clinical suspicion to diagnosis
It is desirable that the diagnostic work-up of the DVT should be completed in the ED with a multidisciplinary approach that can be variable depending on levels of care of the ED.
The clinical manifestations of DVT are not specific: the diagnostic process must be guided by the pre-test clinical probability.
The dichotomized Wells score proved to be accurate in stratifying the pre-test probability of DVT in ED, therefore it is necessary to acquire the information to calculate it before any further investigation.
The determination of D-dimer and the use of non-invasive study of the veins of the lower limbs such as CUS (extended or limited compressive ultrasonography) is recommended in the DVT diagnostic work-up.
It is recommended that each laboratory has a specific reference cut-off for d-dimer test and it is necessary an age-correction during the interpretation of this value.
In a patient with Wells pre-test score “unlikely” and negative D-Dimer, the diagnosis of DVT can be reasonably excluded.
If Wells score is “unlikely” for DVT and D-Dimer test is positive it is recommended to perform CUS; if CUS is negative it is indicated to perform complete venous ultrasound (US) evaluation (preferably in 48-72 hours); if venous US is negative, the diagnosis is reasonably excluded. If US is not available, it is indicated to perform a second CUS at 5-7 days.
If Wells score is “likely” for DVT it is recommended to perform CUS; if CUS is negative, it is indicated to perform a complete venous US evaluation (preferably in 48-72 hours) to rule out isolated distal DVT, if available, or, if not, repeat CUS at 5-7 days.
If Wells score is “likely” for DVT with a positive CUS evaluation, it is recommended to start anticoagulant therapy.
If the patient has a positive CUS and a positive D-Dimer test the diagnosis of DVT is confirmed regardless of Wells pre-test probability.
In pregnant women with significant edema in one or both the lower limbs or with clinical suspected deep venous thrombosis of other vascular districts, evaluation performing venous Ultrasound (US) is mandatory.
It is not recommended the use of invasive or expensive tests such as phlebography, Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) for the diagnosis of DVT.
In patients with DVT, further investigations are not necessary to exclude Pulmonary Embolism (PE) in absence of specific symptoms.
Supplementary Comments
Statement 1-3: The assessment of the pretest probability is the base for correct management of DTV.8,18 A low pre-test probability together with a negative D-Dimer test, allows the exclusion of DVT without further investigation.19 A review of clinical trials that investigated the prevalence of DVT as a function of pretest probability (with or without D-Dimer determination), concluded that diagnostic accuracy increases if the pretest probability is estimated before the diagnostic tests.20 In the ED, the panel of experts recommends the use of dichotomized pretest probability (DVT “unlikely” or “likely”).21
Statement 4: CUS, an extremely accurate and non-invasive test for the diagnosis of DVT,22 can be easily performed in the ED by a trained emergency physician.23,24
The CUS, that can be “2-points” (also called “limited”, that investigate popliteal and common femoral veins) or “3-points” (also called “extended”, that investigate popliteal, common femoral and superficial femoral veins).22,25,26
Statement 5: Elderly patients have physiologically higher D-Dimer values.27 Age-Adjustment of D-Dimer reduces the number of diagnostic tests performed to exclude or confirm DVT without reducing its sensitivity.28,29
Statement 6: The combination of an “unlikely” Wells score and a negative age-adjusted D-dimer excludes the presence of DVT in both outpatients and inpatients of both sexes with a 1.2% failure rate (95% CI: 0.7% to 1.8%).21 However, in patients with malignancy or suspected DVT recurrence the original Wells rule is less safe because of higher failure rate (2.2%).21,30,31
Statement 7-11: Complete or whole-leg duplex venous ultrasound (US) is the gold-standard test for the diagnosis of DVT. For this reason, in doubtful cases CUS is recommended.32 If CUS is not available or difficult to perform in reasonable time, the panel of experts suggests to perform a second CUS at 5-7 days, starting anticoagulant therapy if the patient’s bleeding risk is not excessive.33
According to the Panel of experts, the anticoagulant treatment for isolated distal DVT should be considered in patients characterized by a high risk of thrombosis extension.34 Risk factors for DVT extension are: positive D-dimer test, severe symptoms, extended thrombosis (>5 cm in length, >7 mm in diameter or involving multiple veins), thrombosis localized nearly a proximal circulation vein, absence of removable risk factors, history of previous DVT or active cancer and in-patients status.35 On the other hand, for patients at high risk for bleeding, monitoring with CUS is more appropriate that starting anticoagulation therapy, even for patients at high risk of DVT extension.
Statement 11: Neither D-dimer alone nor clinical prediction rules should be used to rule out VTE in pregnant women without objective testing.36, 37 The LEFt score replaces the Wells score in the pregnancy setting: it attributes one point in the case of left (“L”) leg suspicion, one point for edema (“E”) and one point if the suspicion occurred during the first trimester (“Ft”) of pregnancy. The DVT probability is “unlikely” with score 0 (risk of DVT 0%) and “likely” with score ≥1 (risk of DVT 11.7%).38
Statement 12: The use of expensive and/or invasive tests such as venography, Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) is not indicated for the diagnosis of DVT in the Emergency setting. The 2012 ACCP guidelines include the use of MRI, iliac vein doppler and phlebography (grade 2 C) only in pregnant women with suggestive symptoms of isolated iliac vein thrombosis with a negative CUS exam, rather than serial CUS evaluation.34
Statement 13: In a cohort of 103 patients with deep vein thrombosis of lower limbs, the prevalence of asymptomatic PE was 66%. Furthermore, no significant recurrence rate of thrombotic events was observed in the asymptomatic PE group during the follow-up; the authors concluded that, in absence of specific symptoms, further investigations for the diagnosis of PE were not necessary, as no short- or long-term clinical or therapeutic consequences were expected.39
2. Management of DVT
14. The management of DVT should be as outpatients except in presence of one of them:
ongoing bleeding or high bleeding risk (VTE BLEED risk score);
severe renal failure (eVFG < 30 ml/min);
metastatic cancer
Massive DVT, involving iliac femoral vein, caval vein or severely symptomatic patients (phlegmasia dolens);
Inadequate home-care setting.
15. It is recommended that all EDs refer to shared protocols for the out of hospital management and follow-up of patient with an ED diagnosis and initial treatment of DVT.
Supplementary Comments
Statement 14: According to Lozano and al,40 patients treated as outpatient have an equal recurrence rate of venous thromboembolic events and lower rate of major bleeding than those managed as inpatient. Similarly, a Cochrane review suggests that patients treated at home with LMWH are less likely to have recurrence of VTE with no clear differences in major or minor bleeding, nor in mortality than those treated as inpatients.41
On the other hand, the proportion of patients with DVT currently managed as outpatients in clinical practice is still very low: in an analysis of RIETE registry was 31-38%.42
Statement 15: The development of out-of-hospital pathways for the management of patients with an ED diagnosis of DVT requires well-organized outpatient resources and infrastructures.43
3. DVT treatment in the acute phase
16. Prompt initiation of anticoagulant therapy after a diagnosis of DVT is mandatory.
17. Anticoagulant therapy should begin in the ED right after the diagnosis of DVT, regardless of the patient’s subsequent destination.
18. While awaiting for the result of diagnostic evaluation of patient with likely DVT (according to the dichotomized Wells score), anticoagulant therapy can also be considered after weighing both thrombotic and hemorrhagic risk.
19. The choice of the anticoagulant drug must take into account not only the common criteria of good clinical practice, but also patient renal and hepatic function, comorbidities, compliance, preferences and opportunity of early discharge.
20. DOACs (Direct Oral Anti-Coagulant) represent the better anticoagulant approach especially for patients discharge directly, or after a brief observation, from ED.
21. Vena cava filters placement or endovascular procedures are indicated in patients with DVT and contraindications to anticoagulant therapy, depending on hospital skills and availability.
Supplementary Comments
Statement 16-18: Bleeding risk should be evaluated before the initiation of anticoagulant therapy and periodically during the treatment, using a specific and validated risk score.44 According to the American College of Chest Physicians (ACCP) 2016 guidelines,9 the bleeding risk score should be rapid and easy to use in the ED.
Statement 19-20: Anticoagulant therapy represents the mainstay of medical therapy for DVT. Treatment may include subcutaneous, weight adjusted low-molecular weight heparin (LMWH), fondaparinux, unfractionated heparin (UFH) and DOACs.
In case of obesity and renal failure, unfractionated heparin continuous intravenous infusion or subcutaneous injections represents of treatment of choice.45 In case of pregnancy, treatment of choice is currently LMWH 46 A rapid anticoagulant effect can be achieved with a DOAC, whose efficacy is widely confirmed and non-inferior to Vitamin K antagonist, while counting on a minor bleeding risk, easier administration and fewer interactions with other drugs and foods.47,48 In the absence of contraindications, DOACs (apixaban, dabigatran, edoxaban, rivaroxaban) should be considered as the first line anticoagulant therapy in non-cancer patients with DVT.8 Edoxaban and rivaroxaban should be considered as a valid alternative to LMWH for the management of cancer-related DVT, while considering the higher bleeding risk in patients with gastro-intestinal cancer.49
As for apixaban, the Caravaggio trial50 compared daltheparin and apixaban efficacy and safety; the study is ongoing but data derived from ADAM-VTE study (small study comparing apixaban vs daltheparin) suggest a lower major bleeding risk and VTE recurrence in patients treated with apixaban.51 DOACS must be avoided in patient suffering from severe renal failure, antiphospholipidic syndrome, DVT in atypical districts, and in patients with vena cava filters.47
Statement 21: ACCP 201234 and European Society of Cardiology (ESC) 2018 guidelines8 recommend vena cava filter placement only in patients with proximal DVT and absolute contraindication to anticoagulant therapy. Filters must be removed as soon as bleeding risk allows anticoagulant treatment.34,9,8
Conclusions
The assessment of the pretest probability is necessary in the emergency setting, and it is the base for correct management of DVT. An effective DVT management in the ED requires:
DVT risk stratification through a validated and easy to use CPR
An age adjusted d-dimer cut off
Bedside CUS testing performed directly in the ED
Furthermore, when appropriate outpatient management of DVT is considered safe and effective and beneficial to the healthcare system alike.52 For this purpose, it is necessary to develop out-of-hospital pathways in order to ensure opportunities for follow-up, patient education and communication between primary and secondary care.53
Dentali et al,42 examined Italian patient enrolled in RIETE registry with a diagnosis of DVT, showing that 53.7% of patients were treated as outpatients. This rate was higher in other cohorts, reaching out of 80%.54
A 2018 American College of Emergency Physician (ACEP) clinical policy on DVT states DOACs as a safe, more easily administered, and effective treatment in patients with DVT.55 DOACs, especially those with single drug approach (i.e. DOACS not requiring bridge therapy using LMWH), allow the patient to be directly discharged from the ED,56 ensuring an easy out of hospital management.57 Moreover, apixaban and rivaroxaban offer the added benefit of monotherapy from the beginning of anticoagulation, and are also associated with a lower risk of bleeding compared to the standard LMWH/ VKA combination.58,59 In the AMPLIFY study—which compares immediate administration of apixaban 10 mg twice a day for 7 days followed by 5 mg twice a day vs enoxaparin followed by warfarin in 5395 patient with acute VTE (of which 3532 had isolated DVT) randomly assigned—no difference emerged in outcomes events (RR: 0.84; 95%CI 0.60-1.18) while major bleeding and major/ CNRM bleeding were lower in apixaban cohort (RR: 0.31: 95%CI 0.17-0.55 and RR: 0.44, 95%CI 0.36-0.55 respectively).60
The EINSTEIN DVT randomized study compared immediate administration of rivaroxaban 15 mg twice a day for 3 weeks followed by 20 mg once a day vs enoxaparin followed by warfarin in 3449 patient with acute symptomatic DVT; no difference emerged in the outcome events (HR: 0.68; 95%CI 0.44-1.04) and major bleedings (HR: 0.65; 95%CI 0.33-1.30).61
Furthermore, although the risk of bleeding appears lower, the reversal agents now available (idarucizumab for dabigatran and andexanet alfa for factor Xa inibitors) are a further security in daily practice.62,63
Strengths and Limitations of the Study
Our study has several strengths. We adopted strict criteria to help ensure that the panel of experts comprised leader experts on the management of VTE in the ED. Furthermore, face-to-face meeting allowed experts to explain and defend ideas, which might improve the quality of the final list of statements. Consensus statements are based on existing evidence and on experts’ experience. However, further research is required to further support some of the issues mentioned in the statements.
Supplemental Material
supplementary_material for Diagnosis and Treatment of Deep Vein Thrombosis in the Emergency Department: Results of an Italian Nominal Group Technique Study by Aldo Salvi, Cinzia Nitti, Andrea Fabbri, Paolo Groff, Enrico Giuseppe Ruggiero and Giancarlo Agnelli in Clinical and Applied Thrombosis/Hemostasis
Acknowledgments
Content Ed Net provided organizational and methodological support for the conduction of the study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article. This project was supported by Bristol Meyer Squibb, Italy. Bristol Meyer Squibb had no role in study design, collection of evidence, interpretation of data, writing the manuscript, or decision to publish.
ORCID iD: Aldo Salvi  https://orcid.org/0000-0002-5601-8790
https://orcid.org/0000-0002-5601-8790
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Singer AJ, Thode HC, Jr, Peacock WF. Admission rates for emergency department patients with venous thromboembolism and estimation of the proportion of low risk pulmonary embolism patients: a US perspective. Clin Exp Emerg Med. 2016;3(3):126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vinson D, Berman D. Outpatient treatment of deep venous thrombosis: a clinical care pathway managed by the emergency department. Ann Emerg Med. 2001;37(3):251–258. [DOI] [PubMed] [Google Scholar]
- 3. Jimenez S, Ruiz-Artacho P, Merlo M, et al. Risk profile, management, and outcomes of patients with venous thromboembolism attended in Spanish emergency departments. Medicine. 2017;96(48):e8796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Takatsuki S, Kimura T, Sugimoto K, et al. Real-world monitoring of direct oral anticoagulants in clinic and hospitalization settings. SAGE Open Med. 2017;5:2050312117734773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vinogradova Y, Coupland C, Hill T, Cox JH. Risks and benefits of direct oral anticoagulants versus warfarin in a real world setting: cohort study in primary care. BMJ. 2018;362:k2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Granger CB, Alexander J, McMurray J, et al. ; On the behalf of ARISTOTLE Committees and investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. [DOI] [PubMed] [Google Scholar]
- 7. Imberti D, Barillari G. Real life management of venous thromboembolsim with rivaroxaban: results from experience VTE, an Italian Epidemiological Survey. Clin Appl Thromb. 2017;24(2):241–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mazzolai L, Aboyans V, Ageno W, et al. Diagnosis and management of acute deep vein thrombosis: a joint consensus document from the European Society of Cardiology Working Groups of aorta and peripheral circulation and pulmonary circulation and right ventricular function. Eur Heart J. 2018;39(47):4208–4218. [DOI] [PubMed] [Google Scholar]
- 9. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–352. [DOI] [PubMed] [Google Scholar]
- 10. Pollack CV, Schreiber D, Goldhaber SZ, et al. Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). J Am Coll Cardiol. 2011;57(6):700–706. [DOI] [PubMed] [Google Scholar]
- 11. Jakobsson C, Jiménez D, Gómez V, Zamarro C, Mean M, Aujesky D. Validation of a clinical algorithm to identify low-risk patients with pulmonary embolism. J Thromb Haemost. 2010;8(6):1242–1247. [DOI] [PubMed] [Google Scholar]
- 12. Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35(43):3033–3069. [DOI] [PubMed] [Google Scholar]
- 13. Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Durand MA, Chantler R. Consensus Groups in Principles of Social Research. Open University Press/McGraw-Hill Education Berkshire; 2014:64–66. [Google Scholar]
- 15. Fink A, Kosecoff J, Chassin M, Brook RH. Consensus methods: characteristics and guidelines for use. Am J Public Health. 1984;74(9):979–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health. 1972;62(3):337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38(3):655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kitchen L, Lawrence M, Speicher M, Frumkin K. Emergency department management of suspected calf-vein deep venous thrombosis: a diagnostic algorithm. West J Emerg Med. 2016;17(4):384–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lim W, Le Gal G, Bates SM, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: diagnosis of venous thromboembolism. Blood Adv. 2018;2(22):3226–3256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wells PS, Owen C, Doucette S, Fergusson D, Tran H. Does this patient have deep vein thrombosis? JAMA. 2006;295(2):199–207. [DOI] [PubMed] [Google Scholar]
- 21. Geersing G, Zuithoff N, Kearon C, et al. Exclusion of deep vein thrombosis using the Wells rule in clinically important subgroups: individual patient data meta-analysis. BMJ 2014;348:g1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Herman RZ, Dangur IA, Berant R, et al. Comparison between two-point and three-point compression ultrasound for the diagnosis of deep vein thrombosis. J Thromb Thrombolysis. 2018;45(1):99–105. [DOI] [PubMed] [Google Scholar]
- 23. Kory P, Pellecchia C, Shiloh A, Mayo P, Di Bello C, Koenig S. Accuracy of ultrasonography performed by critical care physicians for the diagnosis of DVT. Chest. 2011;139(3):538–542. [DOI] [PubMed] [Google Scholar]
- 24. Pedraza G, Valle A, Ceballos G, Rodríguez F, López MA, Villanueva MM. Comparison of the accuracy of emergency department-performed point-of-care-ultrasound (pocus) in the diagnosis of lower-extremity deep vein thrombosis. J Emerg Med. 2018. May;54(5):656–664. [DOI] [PubMed] [Google Scholar]
- 25. Lee J, Lee S, Yun S. Comparison of 2-point and 3-point point-of-care ultrasound techniques for deep vein thrombosis at the emergency department a meta-analysis. Medicine. 2019;98(22):e15791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hamper U, DeJong M, Scoutt L. Ultrasound evaluation of the lower extremity veins. Radiol Clin North Am. 2007;45(3):525e47. [DOI] [PubMed] [Google Scholar]
- 27. Leger R, Bryant S, Edwards K, et al. An age distribution of D-dimer values in normal healthy donor population: an indirect verification of the age-adjusted D-dimer cutoffs for VTE exclusion. Blood. 2016;128(22):1432. [Google Scholar]
- 28. Riva N, Camporese G, Lotti M, et al. Age-adjusted D-dimer to rule out deep vein thrombosis: findings from the PALLADIO algorithm. J Thromb Haemost. 2018;16(2):271–278. [DOI] [PubMed] [Google Scholar]
- 29. Farm M, Siddiqui AJ, Onelöv L, et al. Age-adjusted D-dimer cut-off leads to more efficient diagnosis of venous thromboembolism in the emergency department: a comparison of four assays. J Thromb Haemost. 2018;16(5):866–875. [DOI] [PubMed] [Google Scholar]
- 30. Lee A. VTE in patients with cancer-diagnosis, prevention, and treatment. Thromb Res. 2008;123:(1):S50–S54. [DOI] [PubMed] [Google Scholar]
- 31. Schutgens RE, Beckers MM, Haas FJ, Biesma DH. The predictive value of D-dimer measurement for cancer in patients with deep vein thrombosis. Haematologica. 2005;90(2):214–219. [PubMed] [Google Scholar]
- 32. Needleman L, Cronan J, Lilly M, et al. Ultrasound for lower extremity deep venous thrombosis multidisciplinary recommendations from the Society of Radiologists in Ultrasound Consensus Conference. Circulation. 2018;137(14):1505–1515. [DOI] [PubMed] [Google Scholar]
- 33. Guanella R, Righini M. Serial limited versus single complete compression ultrasonography for the diagnosis of lower extremity deep vein thrombosis. Semin Respir Crit Care Med. 2012;33(2):144–150. [DOI] [PubMed] [Google Scholar]
- 34. Kearon C, Akl E, Comerota A, et al. Antithrombotic therapy for VTE disease antithrombotic therapy and prevention of thrombosis 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2):e419S–e494S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Streiff M, Agnelli G, Connors J, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. 2016;41(1):32–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chan W, Rey E, Kent N, et al. Venous thromboembolism and antithrombotic therapy in pregnancy. J Obstet Gynaecol Can. 2014;36(6):527–553. [DOI] [PubMed] [Google Scholar]
- 37. Bates SM, Jaeschke R, Stevens SM, et al. Diagnosis of DVT: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e351S–e418S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Le Moigne E, Genty C, Meunier J, et al. Validation of the LEFTt score, a newly proposed diagnostic tool for deep vein thrombosis in pregnant women. Thromb Res. 2014;134(3):664–667. [DOI] [PubMed] [Google Scholar]
- 39. García-Fuster MJ, Fabia MJ, et al. Should we look for silent pulmonary embolism in patients with deep venous thrombosis? BMC Cardiovasc Disord. 2014;14(1):178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lozano F, Santos JT, Barrón M, et al. Home versus in-hospital treatment of outpatients with acute deep venous thrombosis of the lower limbs. J Vasc Surg. 2014;59(5):1362–1367. [DOI] [PubMed] [Google Scholar]
- 41. Othieno R, Okpo E, Forster R. Home versus in-patient treatment for deep vein thrombosis. Cochrane Database Syst Rev. 2018;1(1):CD003076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dentali F, Di Micco G, Pierfranceschi MG, et al. Rate and duration of hospitalization for deep vein thrombosis and pulmonary embolism in real-world clinical practice. Ann Med. 2015;47(7):546–554. [DOI] [PubMed] [Google Scholar]
- 43. Kelliher S, Hall P, Kevane B, et al. Implementation of an acute DVT ambulatory care pathway in a large urban centre: current challenges and future opportunities. Thrombosis J. 2019;17:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bartholomew JR. Venous Thromboembolism (Deep Venous Thrombosis & Pulmonary Embolism). 2018. [Google Scholar]
- 45. Smythe M, Priziola J, Dobesh P, Wirth D, Cuker A, Wittkowsky A. Guidance for the practical management of the heparin anticoagulants in the treatment of venous thromboembolism. J Thromb Thrombolysis. 2016;41(1):165–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bates SM, Rajasekhar A, Middeldorp S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018;2(22):3317–3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Becattini C, Agnelli G. Treatment of venous thromboembolism with new anticoagulant agents. J Am Coll Cardiol. 2016;67(16):1941–1955. [DOI] [PubMed] [Google Scholar]
- 48. van der Hulle T, Kooiman J, den Exter P, Dekkers O, Klok F, Huisman M. Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and metanalysis. J Thromb Haemost. 2014;12(3):320–328. [DOI] [PubMed] [Google Scholar]
- 49. Ay C, Westendorf JB, Pabinger I. Treatment of cancer-associated venous thromboembolism in the age of direct oral anticoagulants. Ann Oncol. 2019;30(6):897–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Agnelli G, Becattini C, Bauersachs R, et al. Apixaban versus dalteparin for the treatment of acute venous thromboembolism in patients with cancer: The Caravaggio Study. Throm Haemost. 2018;118(9):1668–1678. [DOI] [PubMed] [Google Scholar]
- 51. McBane R, Wysokinski W, Rademacher JL, et al. Apixaban and dalteparin in active malignancy associated venous thromboembolism: the ADAM VTE trial. J Thromb Haemost. 2019;18(2):411–421. [DOI] [PubMed] [Google Scholar]
- 52. Bishop B, Wilson AG, Post D, Howard L, Ruehlen L. A pilot study of home treatment of deep vein thrombosis with subcutaneous once-daily enoxaparin plus warfarin. J Manag Care Pharm. 2006;12(1):70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Weeda E, Butt S. Systematic review of real-world studies evaluating characteristics associated with or programs designed to facilitate outpatient management of deep vein thrombosis. Thrombosis Hemostasis. 2018;24(9_Suppl):301S–313S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mansour S, Alotaibi G, Wu C, McMurtry M. Trends in admission rates and in-hospital stay for venous thromboembolism. Thromb Res. 2017;156:149–154. [DOI] [PubMed] [Google Scholar]
- 55. American College of Emergency Physicians Clinical Policies Subcommittee on Thromboembolic Disease; Wolf S, Hahn S, Nentwich L, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected acute venous thromboembolic disease. Ann Emerg Med. 2018;71(5):e59–e109. [DOI] [PubMed] [Google Scholar]
- 56. Kahler Z, Beam D, Kline J. Cost of treating venous thromboembolism with heparin and warfarin versus home treatment with rivaroxaban. Acad Emerg Med. 2015;22(7):796–802. [DOI] [PubMed] [Google Scholar]
- 57. Wolf S, Hahn S, Nentwich L, Raja A, Silvers S, Brown M. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected acute venous thromboembolic disease. Ann Emerg Med. 2018;71(5):e59–e109. [DOI] [PubMed] [Google Scholar]
- 58. Burnett A, Mahan C, Vazquez S, Oertel L, Garcia D, Ansell J. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. J Thromb Thrombolysis. 2016;41(1):206–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mantha S, Ansell J. Indirect comparison of dabigatran, rivaroxaban, apixaban and edoxaban for the treatment of acute venous thromboembolism. J Thromb Thrombolysis. 2015;39(2):155–165. [DOI] [PubMed] [Google Scholar]
- 60. Agnelli G, Büller H, Cohen SA, et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(9):799–808. [DOI] [PubMed] [Google Scholar]
- 61. The Einstein Investigators. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–2510. [DOI] [PubMed] [Google Scholar]
- 62. Almarshad F, Alaklabi A, Bakhsh E, Pathan A, Almegren M. Use of direct oral anticoagulants in daily practice. Am J Blood Res. 2018;8(4):57–72. [PMC free article] [PubMed] [Google Scholar]
- 63. Crowther M, Cuker A. How can we reverse bleeding in patients on direct oral anticoagulants? Kardiol Pol. 2019;77(1):3–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
supplementary_material for Diagnosis and Treatment of Deep Vein Thrombosis in the Emergency Department: Results of an Italian Nominal Group Technique Study by Aldo Salvi, Cinzia Nitti, Andrea Fabbri, Paolo Groff, Enrico Giuseppe Ruggiero and Giancarlo Agnelli in Clinical and Applied Thrombosis/Hemostasis